mental health issues in later life
advertisement

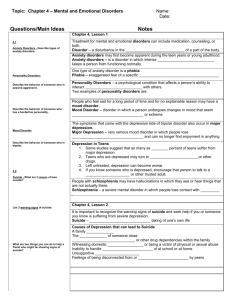
MENTAL HEALTH ISSUES IN LATER LIFE Educational Tool Kit Two 1 Educational Tool Kit 2 Objectives Chapter 1 1. 2. 3. 4. 5. 6. 7. 8. 9. Chapter 2 1. 2. 3. 4. Common Mental Health Disorders To be aware of the prevalence of mental health problems in the older population. To be familiar with symptoms and risk factors for mental health problems. To recognize how mental health is different among older compared to younger adults. To be aware of different treatment options for mental health problems. To be aware of ideas for how natural caregivers can help older adults with mental health problems. To recognize addictions as a mental health problem. To recognize the interactions between substance abuse and other physical and mental health problems. To understand the symptoms and risks factors related to suicide. To understand how a natural caregiver can get help for an older adult contemplating suicide. Diagnosis and Treatment Issues To be able to recognize if someone needs help. To be aware of where to turn for a mental health assessment/diagnosis. To be familiar with barriers to detection and treatment of mental health conditions in the elderly. To be aware of how to share your concerns regarding mental health with others. 2 MENTAL HEALTH ISSUES IN LATER LIFE Chapter 1: 1. 2. 3. 4. 5. 6. 7. 8. 9. 1.1 Common Mental Health Disorders To be aware of the prevalence of mental health problems in the older population. To be familiar with symptoms and risk factors for mental health problems. To recognize how mental health is different among older compared to younger adults. To be aware of different treatment options for mental health problems. To be aware of ideas for how natural caregivers can help older adults with mental health problems. To recognize addictions as a mental health problem. To recognize the interactions between substance abuse and other physical and mental health problems. To understand the symptoms and risks factors related to suicide. To understand how a natural caregiver can get help for an older adult contemplating suicide. What are the common mental health disorders? Older adults may experience many different types of mental health disorders, but some are more common then others. See PowerPoint slides 2­9 for further information regarding common mental health disorders. If you have further questions or believe that someone you know may be experiencing one of these disorders contact your local mental health agency. (The following has been reprinted with permission from Positive Aging Resource Center.) 1.1(a) Depression Begin with Activity # 1 – Ask the attendees to answer the questions found in the Later­Life Depression Quiz. Discuss each answer using the information provided on the Quiz. Depression is a common mental health disorder. Most of us will know someone who has been diagnosed with depression, but we may not fully understand what that diagnosis means. The following will provide basic information. 3 1.1(a)(1) What are the symptoms of depression? Has your friend, family member, or neighbor seemed blue lately? Has he or she lost interest in things that had been important to them in the past? Have they seemed sad for a period of time? It could be depression. Remember however, sadness does not always equal depression, and depression is not always marked by sadness. A person may be depressed if he or she experiences: Sleep changes · Have difficulty falling asleep · Wake up in the middle of the night and not be able to get back to sleep · Sleep more than usual Activity changes · Feel tired all of the time · Feel less energetic than usual · Feel nervous or may not be able to sit still Appetite changes · Have lost his or her appetite · Find that food no longer tastes good · Experience an increased appetite and weight gain Sad feelings · Feel sad or blue most of the day nearly every day · Experience feelings of hopelessness or worthlessness Troubled thoughts · Have trouble making decisions 4 · Wish that he or she was dead · Think about suicide · Have problems with attention or concentration Personality changes · Be irritable · Have lost motivation · Lose his or her temper more easily than usual · Lose interest in things that he or she used to enjoy · If someone you know is experiencing some or all of these changes, he or she may be suffering from depression. You can help him/her by talking about it. 1.1(a)(2) What is the prevalence of depression in older adults? According to Mental Health: Report of the Surgeon General (1999), 3.8% of people over the age of 55 who live independently in the community suffer from major depression in any given year. Of the nearly 35 million Americans age 65 and older, an estimated 2 million have a major depressive illness and another 5 million have depressive symptoms that fall short of meeting full diagnostic criteria for a disorder. 1.1(a)(3) What are the risk factors for depression? Having a chronic medical illness increases a person’s risk of having a depressive disorder. In outpatient medical settings, the prevalence of major depression among older adults is about 12%; in nursing homes, it is about 25%. Other risk factors are: 5 · Family history of: ° Recurrent depression ° Bipolar disorder ° Alcohol abuse or dependence · Personal history of : ° Chronic medical illnesses, especially heart disease, Parkinson’s disease, Alzheimer’s disease, diabetes mellitus, stroke, and cancer. ° Chronic pain ° Loss of physical functioning ° Prior depressive disorders ° Recent significant loss ° Multiple recent stressors (within past 6 months) ° Social isolation 1.1(a)(4) How is depression treated? It has been found that most people respond best with a combination of counseling and medications; antidepressant drugs. This is a decision best made through communication between the physician/mental health counselor and the older adult or a family member if the older adult is incapable of making decisions. 1.1(a)(5) What are commonly prescribed antidepressant drugs? Most antidepressants appear to be equally effective in large populations, so the choice of medication is usually based on: potential side effects that are either helpful or harmful to the older adult, coexisting medical and psychiatric illnesses, prior response to antidepressants in either the adult or close relatives, and possible drug­drug interactions. · Older adults are typically started on the lowest effective dose of medication; the dosage may be increased based on tolerability of side effects and if there has been no response after 1­2 weeks of treatment. · Most side effects to anti­depressant drugs occur in the first few weeks of treatment. Schedule follow­up visits at least 3 times in the first 3 months. · It may take 2­4 weeks of treatment before a person begins to feel better. Other people may experience relief within 2­3 days. 6 · For adults who do not respond to an adequate trial of a particular anti­ depressant, a change to a different medication may be helpful. · Older adults should continue to take anti­depressants even after they feel better because stopping the medicine too soon can result in a relapse. · If this is the first depressive episode, people should continue to take antidepressants for at least 12 months. Then, under the supervision of a doctor, they can gradually taper and try to discontinue the medication, always watching for a recurrence of their symptoms. · If this is the second or more depressive episode in the person’s lifetime, he or she should take antidepressants indefinitely. The medication can treat the acute episode and it can prevent future episodes. Once someone has had 2 or more episodes of depression, the chance of another episode in the future is extremely high (80­90%). · ECT ­ Electroconvulsive therapy is the oldest psychiatric treatment now in use, but modern practice is very different from that of early years. · The technique of stimulation has been refined, and superficial anesthesia with muscular relaxation and oxygenation are in wide use. These changes contribute to a more lenient procedure. 1.1(a)(6) When should people combine counseling with medication? For adults with depression who have been treated with counseling alone, consider medication if symptoms do not improve after 6 weeks or if symptoms continue after 3 months. Medication should always be considered if the older adult has suicidal thoughts, psychotic symptoms (e.g., if he or she is hearing derogatory or other types of voices or having delusions), severe vegetative symptoms (such as refusal to eat or large weight loss), or worsening of symptoms. Continuation treatment ° Acute treatment most often refers to the first three months after the person begins to take antidepressant drugs. The goal of this treatment is to achieve remission of the symptoms of depression. ° Remission refers to minimal residual symptoms (decreases symptoms). 7 ° To prevent a relapse, most people should remain on continuation treatment (at the medication’s full dosage) for 12 months following symptom resolution. Maintenance treatment ° Some adults remain on maintenance therapy following continuation treatment. ° The risk of recurrence of depression increases with each episode of depression. Maintenance treatment is advised for adults who have had 2 or more previous episodes of depression. Discontinuing active treatment Few people like to take medication and people often want to stop taking antidepressants. This is best done gradually. Older adults should be reminded of the symptoms they had when they were first treated for depression. These symptoms are likely to recur and they should watch for them when they begin to lower the dosage of the antidepressant. If the symptoms do begin to reappear, the person should go back to the previous dose of medication that kept the symptoms under control. Abruptly ending treatment can cause short­term reactions in a discontinuation syndrome: Physical symptoms of this syndrome include: ° Gastrointestinal problems (nausea, vomiting, cramping, diarrhea) ° Sleep disturbances ° Headaches, dizziness, and imbalance ° Sweating Psychological symptoms of this syndrome include: ° Anxiety ° Agitation 8 ° Low mood Tapering dosages of anti­depressants, rather than stopping abruptly, can prevent discontinuation syndrome. 1.1(a)(7) How should I talk with someone who may be depressed? Approaching someone who may be depressed can be very helpful. Please see Handout # 1 – “Talking about Depression” for some tips. 1.1(a)(8) How can I help? Be there. · Listen. Be patient and don't interrupt. · Reassure. Phrases like "I love you," "I care about you," and "I am here for you" help. Be helpful. · Assist your friend with small tasks that may seem huge to him or her. Mow the lawn. Go to the grocery store. Cook. · Help your loved one to keep doctor's appointments and to stick to his or her medication plan. Take care of your own emotions. · Remind yourself that you are not responsible for your loved one's depression. Draw a clear line between being supportive and being overprotective. You do not want to make your loved one dependent on you. · Take breaks. Watch a movie or have a cup of tea. · Find a safe haven for expressing your emotions. Having a loved one with depression can wear you out, frustrate you, and add stress to your life. Take solace in a support group or talk with your own therapist. · Don't ignore your own needs. Stick to your routine, and remember to do things for yourself as well as for your loved one. · Give yourself a pat on the back for being strong for a loved one. 9 What not to do Don't be your loved one's counselor. · Don't try to talk him or her out of being depressed. It is not a choice to be depressed. · Don't say, "I know how you feel." Unless you have been depressed, you don't know how your loved one feels. Don't make light of the problem. · Don't offer simple answers. Avoid unhelpful phrases like: · "Cheer up." · "Pull yourself up by your bootstraps." · "Stop feeling sorry for yourself." · "Lots of people are worse off than you are." If your loved one talks about suicide, get help right away. Tell his or her therapist or doctor. If your loved one is threatening to commit suicide, bring him or her to the hospital emergency room. (Positive Aging Resource Center: http://www.positiveaging.org/consumer/depression_howtolove.shtml.) 10 Vignette # 1 People Who Beat Depression Betty: "I thought it was just the blues, but it went on for weeks and weeks. Some nights I could barely sleep—other times I slept until noon. I found I wasn't returning phone calls from friends. My family and friends noticed I wasn't myself. I didn't enjoy things I used to do—my garden, walking in the mornings at the mall with friends, seeing a movie. Was I going to feel this way forever?" What worked for me: "When I went in for my regular check­up, my doctor noticed how down I was. He suggested that I go to see a counselor. I did and I started taking medicine. I had to try a couple of different types of medication before I saw results, but I stuck with it. In a few months, I was back in the swing again." Arlene: "Sure, I knew something was up. My daughter said I was short­tempered and irritable—not like myself. Some days, Lord—getting out of bed was too much. I prayed, thinking that if I had enough faith it would pass. I talked to my minister and he said to have faith, but to get help. He thought I might be depressed." What worked for me: "I saw a doctor who told me my minister was right. He said that depression is a medical illness, but it's treatable. I got help. Now my daughter says I'm the mom she always knew." Alma: "I had an "ataque de nervios." I was crying a lot and I felt angry. I had trouble concentrating. I couldn't even get myself to church. My family was worried about me." What worked for me: "I went to the health clinic a few blocks away. The doctor there was very kind and he listened to me. He told me that this problem is very common in people my age. He prescribed some medicine and I took it faithfully every day. I also talked to a counselor from the health clinic about my worries. After a few months of taking medication and talking with my counselor, I felt much better." Not everyone reacts in the same way when depressed. Some people have many symptoms, and some people have just a few. 1.1(b) Anxiety Anxiety is different than fear. Fear is a response to danger. If you are anxious, you may feel very nervous even without an actual threat. Sometimes people feel both anxious 11 and depressed at the same time. Anxiety can be a helpful emotion. If you are in danger, the anxiety reaction alerts you, makes it easier to run for safety. Anxiety can also make you more alert for times in which you must be at your best such as a public performance or an important test. Sometimes, however, anxiety occurs without actual danger or the anxiety is excessive for the circumstances. This inappropriate or excessive anxiety, an anxiety disorder––can interfere with a person’s ability to function. Recognizing an anxiety disorder is the first step in managing it. 1.1(b)(1) · What are the risk factors for anxiety? Risk factors for anxiety: · Family history of: o Alcohol abuse o Anxiety disorders o Mood disorders · Personal history of: o Depression o Anxiety disorder o Chronic medical illness, especially diabetes mellitus, mitral valve prolapse, Parkinson’s disease, Alzheimer’s disease, congestive heart failure, or hyperthyroidism o Loss of significant person during childhood o Cognitive impairment o Alcohol abuse/dependence o Social isolation · Other factors: o Female gender o Exposure to traumatic event 1.1(b)(2) · · · · · · · What are the symptoms of anxiety? Excess or undue worry or fear Fatigue Disturbed sleep Jumpiness, jitteriness, trembling Muscle aches, tension Dizziness, lightheadedness Gastrointestinal upset 12 · · · · 1.1(b)(3) Dry mouth, sensation of a lump in the throat, choking sensation Clammy hands, sweating Racing heartbeat, chest discomfort Shortness of breath, or the feeling of being smothered What are panic attacks? Panic attacks, an overwhelming feeling of anxiety, can be debilitating. It is important to seek help if you or a loved one is experiencing panic attacks. See Figure # 1 for symptoms. Figure # 1 Symptoms of a Panic Attack Feelings of intense fear or discomfort in which 4 or more of the following symptoms occur abruptly and peak within 10 minutes: o Palpitations o Sweating o Shaking o Shortness of breath, feeling smothering o Choking sensation o Chest pain o Nausea/GI distress o Dizziness o De­realization. A feeling that world feels unreal and unfamiliar o Fear of losing control or going crazy o Fear of dying o Numbness/tingling of hands, mouth, and feet o Chills, hot flashes 13 1.1(b)(4) What causes anxiety? Experts believe that anxiety is caused by a mixture of factors like brain chemistry, genes, life events, and personality. In this way, an anxiety disorder is like many other physical problems like heart disease and diabetes. Have you been feeling anxious? If so, talk to your doctor. This feeling may be a side effect of a medicine (including appetite suppressants or medicines with caffeine) that you are taking for another health problem. 1.1(b)(5) What is the prevalence of anxiety disorders? According to Mental Health: Report of the Surgeon General, 11.4% of the population over the age of 55 suffers from an anxiety disorder in any given year. (U.S. Department of Health and Human Services, 1999). This may be an under representation of the problem because it will often go unreported. 1.1(b)(6) What else should I know about anxiety disorders? The symptoms, frequency, and intensity of anxiety and the behaviors that result from an anxiety disorder vary among individuals. Only a physician can determine whether there is a medical cause for the anxiety symptoms. Sometimes an older adult really is having a heart attack––not a panic attack! Some people, especially those who have a combination of panic disorders and depression, may also require evaluation for: · · · 1.1(b)(7) Medical problems Psychological issues Substance abuse How are Anxiety Disorders managed? Management of anxiety disorders may include medication therapy, psychotherapy, or both. 14 Medication Several types of medications are effective in managing anxiety. Factors that are considered in choosing a medication include the person’s age, coexisting medical and psychiatric illnesses, prior response to medications, and possible drug interactions. Psychotherapy Psychosocial interventions for anxiety disorders include cognitive behavioral therapy (CBT), group therapy (such as marital and family therapy), and psychodynamic psychotherapy to address coexisting disorders or stressors. Support, reassurance, and education are important elements of each of these interventions. 1.1(b)(8) How can I help someone who is anxious? Provide a comforting setting · Confusion can increase a person's anxiety. Guide your loved one to familiar surroundings. Adding structure to his or her day can create a sense of security. · Sometimes pets can be therapeutic! Talk with their physician or a mental health professional to determine if they are capable of caring for a pet. If so, and your loved one doesn't have a pet already; talk with him or her about adopting a dog or cat. Talk with a vet or animal shelter in your community about local pet adoption programs for seniors. · Make sure that he or she sees a doctor. · Counseling with a therapist, doctor, or a social worker can help. · If your loved one is taking one or more medications, ask his/her doctor if anxiety is a side effect of any of these drugs. · Sometimes conditions like depression can go hand in hand with anxiety. Treatment for the depression can make the anxiety go away. 15 · Help your loved one to get moving. · Regular physical activity may help. · Breathing exercises and yoga can be calming. Rent or borrow a video about yoga from the library and try it together. Who knows? You may feel calmer, too! · Music or relaxation tapes and CDs can also be quite soothing. Try classical music, Gregorian chants, ocean waves breaking on the shore, waterfalls, birds singing, or whales "talking" to each other. Try several kinds and find the one that is most relaxing. Note: For more conversations about anxiety go to http://www.positiveaging.org/consumer/anxiety_conv.shtml. Vignette # 2 Conversations about Anxiety Rosemary and Alice ­ At the Senior Center Rosemary usually meets with her friends at the Reedville Senior Center on Thursdays. This is the first time that Rosemary has been to the center in a few weeks. Rosemary: It's good to be back here. I've missed you all! Alice: We missed you, too. You look great. Jean Ellen said that you were having some health problems. Rosemary: Yes, I had "postural hypotension". I was getting dizzy when I sat up in bed in the morning. I felt so strange and I was very anxious. I've never had a heart attack, but maybe that's what it feels like. My heart was racing. Alice: Did your doctor give you something for that? Rosemary: She did. The medicine helped with the dizziness, but I was still feeling panicky. Alice: Did that feeling ever go away? Rosemary: It did, but only after a lot of trial and error–trying to find out what the problem was. I stopped drinking coffee and that helped a lot. My doctor told me that postural hypotension can bring on anxiety. Caffeine can, too. So I've been taking medicine for the medical problem and I switched to herbal tea, and now I feel much better. 16 1.1(c) Alcohol and Aging It is not uncommon for a person to self­medicate, often using alcohol to dull emotional pain. People drink alcohol to cope with loneliness, grief, boredom, depression, feelings of self­worth, and physical problems. It's normal to seek comfort for these problems, but alcohol will not solve the problem. As people age their bodies become more sensitive to the effects of drinking alcohol. Drinking alcohol can worsen some common problems. Alcohol can add to health problems. It can: · Worsen one's balance and lead to falls and hip fractures. · Further worsen a person's eyesight and reflexes; this can lead to traffic accidents. · Worsen some common medical conditions such as high blood pressure, diabetes, and ulcers. 1.1(c)(1) What is the prevalence of alcohol abuse in older adults? · The prevalence of heavy drinking (12 to 21 drinks per week) in older adults is estimated at 3 to 9 percent (Liberto et al., 1992). · Alcohol abuse and dependence are approximately four times more common among men than among women (1.2 percent vs. 0.3 percent) aged 65 and older (Grant et al., 1994). Although lifetime prevalence rates for alcoholism are higher for white men and women between ages 18 and 29, African American men and women have higher rates among those 65 years and older. The lifetime prevalence rates for alcoholism among Hispanic men were between those of whites and African Americans. Hispanic females had a much lower rate than those for whites and African Americans (Helzer et al., 1991). · The rate of alcohol dependence among older adults (aged 65 and older) who come to the emergency room is almost 15% (Kaplan, 2000). 17 1.1(c)(2) Who is at risk of abusing alcohol? Risk factors for developing an alcohol abuse problem · Having a mental health disorder; half of all individuals with severe mental health problems are also substance abusers. · Having an alcoholic parent. 1.1(c)(3) Does alcohol impact other illnesses? Alcohol abuse can contribute to: · Physical health problems: o o o o o o o o · Mental health problems: o o o o · Anxiety Dementia Depression Suicide Social problems such as: o o o o 1.1(c)(3) Chronic obstructive pulmonary disease Cirrhosis of the liver Hypertension and heart disease Neuropathy Peptic ulcer disease Sleep disorders Cancer Premature death Family problems Financial difficulties Homelessness Violence and victimization What are the symptoms of alcohol abuse? · Increased consumption and frequency of consumption of alcohol · Increased tolerance to the effects of alcohol · Confusion, disorientation, blurred vision · Gastrointestinal problems (nausea, vomiting) 18 · Insomnia, unusual drowsiness · Lack of physical coordination · Malnutrition · Slurred speech · Urinary problems (incontinence, retention) · Withdrawal symptoms (e.g., nausea, headache, anxiety, depression, sleeplessness) when one drinks less than usual 1.1(c)(4) · What are the signs of alcohol abuse? Health, relationship, legal, or work problems because of drinking o o o · Unusual behavior because of drinking o o o o o · Calling restaurants in advance to determine whether they serve alcohol Considering the amount of alcohol that will be available at social events; drinking before parties; asking to mix one’ s own drinks at social gatherings; guarding alcoholic beverages Sleeping during the daytime Discontinuing usual activities Hiding empty containers for alcohol in the garbage or elsewhere Unsafe behavior because of drinking o o 1.1(c)(5) Eviction from place of residence Neglect of grooming and hygiene Withdrawal from friends, family, and neighbors Evidence of unexplained injuries such as bruises, burns, or fractured bones Minor car accidents What is alcohol abuse? The Diagnostic and Statistical Manual (DSM IV) defines an alcohol use disorder as one’s recurrent consumption of alcohol even after one has experienced work, legal, relationship, or physical problems because of drinking: 19 Alcohol Abuse A maladaptive pattern of alcohol use leading to clinically significant impairment or distress, as manifested by one (or more) of the following, occurring within a 12­­month period: 1. 2. 3. 4. Recurrent alcohol use resulting in a failure to fulfill major role obligations at work, school, or home (e.g., repeated absences or poor work performance related to alcohol use; alcohol­related absences, suspensions, or expulsions from school; neglect of children or household) Recurrent alcohol use in situations in which it is physically hazardous (e.g., driving an automobile or operating a machine when impaired by alcohol use) Recurrent alcohol­related legal problems (e.g., arrests for alcohol­related disorderly conduct) Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol (e.g., arguments with spouse about consequences of intoxication, physical fights). Alcohol Dependence A maladaptive pattern of alcohol use, leading to clinically significant impairment or distress, as manifested by three (or more) of the following, occurring at any time in the same 12­ month period: 1. 2. Tolerance, as defined by either of the following: a. a need for markedly increased amounts of alcohol to achieve intoxication or desired effect b. markedly diminished effect with continued use of the same amount of alcohol Withdrawal, as manifested by either of the following: a. the characteristic withdrawal syndrome for alcohol b. the same (or a closely related) substance is taken to relieve or avoid withdrawal symptoms 3. Alcohol is often taken in larger amounts or over a longer period than was intended 4. A persistent desire or unsuccessful efforts to cut down or control alcohol use 5. A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects 20 6. Important social, occupational, or recreational activities are given up or reduced because of alcohol use 7. Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol (e.g., current cocaine use despite recognition of cocaine­ induced depression, or continued drinking despite recognition that an ulcer was made worse by alcohol consumption) (American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, fourth edition, 1994.) 1.1(c)(6) · How is alcohol abuse diagnosed? Screening tools for identifying alcohol abuse in older adults include: o o o 1.1(c)(7) A clinical interview with open­ended questions A drinking history A self­administered screening test that can be distributed during a talk about alcohol and older adults. This form of self­scored test can also be distributed in senior centers and senior housing facilities. What are the treatments for alcohol abuse? Management of alcoholism may include drug therapy, psychotherapy, or both. Medication Several types of drug therapies are effective in managing alcoholism. When choosing a medication the physician will consider the persons age, coexisting medical and psychiatric illnesses, response to medications, and possible drug interactions. Psychotherapy Psychosocial interventions for alcoholism include motivational intervention; cognitive behavioral therapy (CBT); group therapy (such as marital and family therapy); and psychodynamic psychotherapy to address coexisting disorders or stressors. Support, reassurance, and education are important elements 21 of each of these interventions. Other factors that the physician will keep in mind when choosing a particular intervention are: · Older adults may be motivated to stop drinking because of concerns about their health and their desire to remain independent and financially secure. · The most successful interventions include the older adult in decision­making, and these interventions are respectful of the individual’s ethnic and cultural beliefs and experiences. · With the older adult’s permission, the inclusion of family members and other health care providers in the treatment process can also be very helpful. · Both the experience of alcoholism and the stage of addiction may differ among individuals, and one individual may need different types of treatment throughout the course of his or her chronic problem with alcohol. Detoxification Individuals, particularly older adults who stop drinking alcohol, may experience mild symptoms (anxiety, insomnia) to severe symptoms (seizures, delirium tremens) of alcohol withdrawal. Medical monitoring, whether in the hospital or in an outpatient facility, is especially important for those who experience a severe case of withdrawal. Medications can be used to prevent or address these symptoms. 1.1(c)(8) Does alcohol interact with medications? Alcohol can cause problems if a person is taking medication. It can: · Interact badly with many drugs that are commonly prescribed to older adults. · Cause harmful side effects or lessen a medication's effectiveness. 22 1.1(c)(9) Is alcohol abuse ever confused with other illnesses? It is easy to confuse alcohol abuse with another illness because we often do not want to think of a loved one having a substance abuse problem. In addition, many symptoms can be similar or mimic an illness. Common Signs of Dementia · Memory problems · Confusion · Trouble concentrating · Poor coordination Common Signs of Heavy Alcohol Use · Impaired thinking · Problems with judgment · Forgetfulness and confusion · Balance problems Common Signs of Both Dementia and Heavy Alcohol Use · Mood swings · Loss of interest in activities 1.1(c)(10) How can I tell if someone is drinking too much? · Have more than three drinks per day (1 drink = 1 can/bottle of beer, 1 glass of wine, or 1 shot of hard liquor). · Lose interest in food or prefer drinking alcohol to eating meals. · Find that it takes more and more alcohol to become "drunk". Find that alcohol affects your mood. · Drink alcohol to calm or soothe your nerves, forget your troubles, or cheer up. 23 · Become irritable, resentful, or unreasonable when NOT drinking alcohol. Find that alcohol affects your relationships with others. · Hide or lie about drinking habits. · Have medical, family, or financial problems as a result of drinking alcohol. Last, if alcohol is interfering with safety · Drinking alcohol alone. · Neglecting one's home, self, or pets. · Driving a car after drinking alcohol, especially after an arrest for driving under the influence of alcohol. If one or more of the above statements sounds familiar, seek help by talking to a doctor or asking your local health department or social service agency for suggestions. 1.1(c)(11) What support is available for families of people who abuse alcohol? Support groups and 12­step programs can also help people who are dealing with alcohol abuse. Such programs include: · Alcoholics Anonymous: www.alcoholics­anonymous.org · Al­Anon (for families and friends of alcoholics): www.al­ anon.alateen.org People do not become alcoholics because they have done something wrong. Alcoholism is a disease, just as depression and diabetes are diseases. 24 Vignette # 3 Faces of Alcohol Abuse The following people saw alcohol abuse in people they love. Through Al­Anon, they found help for themselves and advice about helping their loved ones. Here are their stories: Jean. My husband Ed started drinking heavily when he retired. He used to have a drink when he got home from work in the evening, but all of a sudden, he was home all the time. He started having that first drink at 5:00, soon it was 3:30, and before I knew it, he was having his first drink of the day at 1:00 P.M. He started skipping his Rotary Club meetings because they were held in the evening. Usually by then he was too drunk to drive. I even heard him calling the other Rotarians on the phone to make excuses for missing the meetings. He told his friends that he was sick or that his old back injury was flaring up. He even blamed me, saying that I was making him stay home to mow the lawn. He never once let on what was really happening. Lou. My wife Marietta lost her mother last year. It was a tough time for her. She is the "organized" one in the family and a lot of the funeral planning and financial issues fell on her shoulders. She always puts everyone and everything else first. At the end of the day, she would be so wound up that she needed a drink to relax. I am embarrassed to say I think that is what got her through. But the drinking kept getting worse and worse­­ when she was unhappy or worried or tired, she would have a drink. When I look back, I see all the warning signs. She tried to hide all the empty bottles in the bottom of the trash, she got very short­tempered when she couldn't have a sherry "to calm her nerves," and she stopped baking bread on the weekends, which was always one of her great pleasures. For more faces of alcohol abuse see: http://www.positiveaging.org/consumer/eh­faces.shtml 1.1(d) Dual Disorders What are co­occurring substance abuse disorders and mental illness in older adults? Dual disorders may include a combination of substance abuse (abuse of alcohol or drugs) and any psychiatric disorder including depression, anxiety, bipolar disorder, and schizophrenia. 1.1(d)(1) · What are the risk factors for developing dual disorders? Having a mental health disorder; half of all individuals with severe mental health problems are also substance abusers 25 · 1.1(d)(2) Having a parent who was a substance abuser and/or a parent who suffered from a mood disorder. How are dual disorders managed? Management of dual disorders may include drug therapy, psychotherapy, or both. The decision to use one treatment method over another may depend in part on: · Other medical or psychiatric illnesses that the patient may have · His or her history of substance use Medication Several types of drug therapies are effective in managing dual disorders. When choosing a medication, the physician will consider the older adults age, coexisting medical and psychiatric illnesses, response to medications, and possible drug interactions. Psychotherapy Psychosocial interventions for dual disorders include motivational intervention; cognitive behavioral therapy (CBT); group therapy (such as marital and family therapy); and psychodynamic psychotherapy to address coexisting disorders or stressors. Support, reassurance, and education are important elements of each of these interventions. 1.1(e) Dementia What is dementia? Dementia is the term used to refer to over 100 different illnesses that lead to cognitive impairment. (See Figure 2). Dementia affects between 5 and 7 percent of adults over age 65 and 40 percent of those over age 85 (American Psychological 26 Association, 1998). It is also important to note that about 10% of older adults who are evaluated for dementia actually have some reversible problem. Figure 2 Examples of Various Types of Dementia · Alzheimer’s disease · Vascular dementia · Huntington’s chorea · Parkinson’s disease 1.1e(1) What are the risk factors for dementia? · Age · Vascular disease · Diabetes mellitus · Female gender · Sedentary lifestyle · Low education level · Race/Ethnicity · Increased risk among African Americans and Latinos, even when controlled for educational level HIV­positive status, especially with co­morbid hepatitis C · History of: o o o o 1.1(e)(2) Cardiovascular accident Alcohol abuse Head trauma What causes dementia? There is a lot of speculation as to what causes dementia, but right now that question can’t be answered definitively. There are some substances that are linked 27 including alcohol and drug abuse, vitamin deficiencies, medications, thyroid problems, and kidney failure. Common Infectious Causes · Neurosyphilis paresis (a syphilitic infection manifested as dementia, seizures, and problems walking and standing) · AIDS/HIV­related disorders · Meningitis · Encephalitis · Creutzfeldt­Jakob disease 1.1(e)(3) What are the symptoms of a dementing illness? · Loss of short­term and long­term memory · Loss of abstract thinking and judgment · Aphasia or word­finding difficulties (particularly nouns) · Apraxia (inability to carry out motor activities despite intact comprehension and motor function) · Agnosia (inability to recognize or identify items despite intact sensory function) · Difficulty with construction (inability to copy three­dimensional figures, assemble blocks, or arrange sticks in specific designs) · Personality change or alteration and accentuation of premorbid traits · “Catastrophic” reactions to misplaced objects · Extreme anxiety if left alone or if caregiver is out of sight · Loss of the ability to attend to activities of daily living 1.1(e)(4) How is dementia diagnosed? Diagnosing can be difficult. Alzheimer’s disease as an example can only be diagnosed with 100% accuracy by performing an autopsy after death, while 28 other dementias are diagnosed at earlier stages. If you believe someone may have dementia it is important that they have a complete physical with testing to rule out infections or negative interactions between medications. 1.1(e)(5) How is dementia managed? Depending on the type of dementia the person is experiencing, the physician may use a combination of medications and therapy. The earlier the diagnosis is given, the greater the likelihood of slowing the progression or limiting the disease. Medication Medications for dementia can be grouped into three categories: 1. Cholinergic neurotransmitter modifying agents such as acetyl cholinesterase inhibitors. 2. Non­cholinergic neurotransmitters/neuropeptide modifying agents. 3. Other pharmacological agents. (Agency for Healthcare Research and Quality, 2004.) Therapy · Behavior modification to help control unacceptable or dangerous behaviors · Rewarding appropriate or positive behaviors Ignoring inappropriate behaviors (within the bounds of safety) Reality orientation to reduce disorientation · Family counseling to strengthen coping skills · Provision of a safe environment o o o o Familiar objects and people Lights left on at night to reduce disorientation 29 · Control of aggressive or agitated behavior · Care of daily needs, may require: o o o o o o Monitoring and assistance in the home In­home care Adult day care Monitoring and assistance in an institutionalized setting Nursing home Visiting nurses or aides, volunteer services, homemakers, or adult protective services 1.1(f) Delirium What is delirium? Delirium (also called acute confusional state and acute brain syndrome) is a potentially life­threatening condition that occurs in 30% of older persons during medical hospitalization and in 10 to 50% of older adults during surgical hospitalization. Also, up to 60% of residents in nursing homes may have delirium. Mariano, C., Gould, E., Mezey, M., et al., (eds.) (1999). 1.1(f)(1) What are the risk factors of delirium? · Drug­drug or alcohol­drug interactions. Toxic effects of (or withdrawal from) alcohol; elicit drugs; prescribed or over­the­ counter drugs (particularly psychoactive drugs, including benzodiazepines) · Benzodiazepine use prior to hospitalization · Infections (e.g., meningitis, encephalitis) · Seizures · Stroke · Subdural hematoma · Tumors · Giant cell arteritis (a chronic inflammatory process involving the extracranial arteries) 30 · Hip fracture · Hydrocephalus (increased fluid in the brain) · Hypercapnia (reduced ventilation often associated with chronic obstructive pulmonary disease) · Infection (e.g., UTI) · Metabolic disturbances (e.g., liver or kidney failure, electrolyte disturbances, hyper­ or hypoglycemia, diabetes, thyroid disorders) · Myocardial infarction (heart attack) · Tumors · Anesthesia · Dehydration · Malnutrition · Sudden environmental changes · Depression Negative outcomes associated with delirium · Complications (such as pneumonia and decubitus ulcers) related to long­term hospital stays · Seizures · Coma · Death 1.1(f)(2) What are the symptoms of delirium? (May occur in any combination and may be intermittent) · Altered awareness, disorientation, clouding of consciousness · Impaired attention, concentration, and memory · Inability to process visual and auditory stimuli · Increased motor activity (e.g., restlessness, plucking, picking) 31 · Anxiety, suspicion, and agitation · Misinterpretation, illusions, delusions, or hallucinations · Speech abnormalities · Reduced wakefulness; sleep disturbance 1.1(f)(3) How is delirium managed? The American Psychiatric Association (1999) Practice Guidelines for the Treatment of Patients with Delirium (Washington, DC: APA) recommends that management should include: · Coordination of care with other physicians · Identification of the cause of delirium · Interventions for acute conditions · Treatment of related disorders · Monitoring of the patient’s safety · Assessment and monitoring of the patient’s psychiatric status · Assessment of the psychological and social characteristics of the patient and family · Establishment and maintenance of alliances among caregivers · Education about the illness · Care for the patient after treatment for delirium 1.1(g) Are there other addictions that can negatively impact older adults? Yes, we can all think of examples of addictions that can negatively impact older adults such as nicotine, narcotics and gambling. Whatever addiction is causing problems; seek help. By treating these addictions older adults can live life to the fullest. 1.1(h) Narcotics 1.1(h)(1) Are older adults addicted to narcotics? 32 There is a lack of data on narcotic use and abuse by older adults. It is thought that older adults who abuse narcotics in late life are simply younger addicts grown old, because very few older adults initiate narcotic drug use in their later years. The number of emergency room visits for heroin or morphine abuse in persons older than 55 in the United States has doubled in the past 10 years, from 1.8% to 3.6%. · Older women are more likely than older men to have problems with prescription drug abuse and dependence because they are more likely to visit physicians and receive prescriptions. · 1.1(h)(2) What are the risk factors for abusing narcotics? · Other primary psychiatric diagnoses (particularly depression) · Chronic medical illness · Cognitive impairment · Social isolation 1.1(h)(3) Why do people misuse or abuse narcotics? · Lack of judgment or misconceptions about drugs · Inability to manage medications because of confusion or cognitive impairment · Insufficient resources for purchasing or storing medications · Self­medication for reasons other than those prescribed; e.g., to: · Sleep · Relax · Alleviate depression or anxiety 1.1(h)(4) What are the symptoms of narcotics abuse? · Sleep disturbances · Impaired cognition · Diminished ability to perform activities of daily living · Irritability · Delusions · Violent behavior · Falls · Constipation 33 1.1(h)(5) How will this addiction be managed? Older patients who are addicted to prescription narcotics should be referred early for appropriate psychiatric, addiction, and pain management services. Education It is important to educate patients that narcotics can be “habit­forming.” Once educated about this fact, many older patients will request discontinuation and medication use can be gradually decreased. Medication To treat withdrawal symptoms, a combination therapy of medications is common. · Psychotherapy Immediately refer patients to a psychiatrist if they abuse narcotics and have any of the following conditions: o Severe anxiety or anorexia o Significant psychomotor agitation or retardation o Psychosis or mania o Suicidal or homicidal thinking Consider referring patients to a psychiatrist if they abuse narcotics and have any of the following disorders: o Depression o Eating disorders o Post­traumatic stress or abuse o Obsessive compulsive disorders or personality disorders (Substance Abuse and Mental Health Services Administration 2002.) 1.1(h)(6) Are older adults abusing Benzodiazepine? Older adults represent only 14% of the U.S. population, yet they receive 27% of all prescriptions for anxiolytic benzodiazepines and 38% of hypnotic benzodiazepines. · 34 Most benzodiazepine prescriptions for older adults in the United States are ordered for anxiety and insomnia, with only 5 percent used as adjuncts for general anesthesia, as muscle relaxants, or as anticonvulsants. · Data from the Veterans Affairs Hospital System suggest that elderly patients may be prescribed inappropriately high doses of medications such as benzodiazepines and may be prescribed these medications for longer periods than are younger adults. · A national survey of approximately 3,000 community­dwelling persons indicated that older persons were over represented among the 1.6 percent who had taken benzodiazepines daily for 1 year or longer: · o 71% > 50 years of age o 33% > 65 years of age 1.1(h)(7) What are the risk factors for benzodiazepine abuse? Medical hospitalization is a significant risk factor for initiation and continuation of benzodiazepines. § As many as 12% of older adults who were given a prescription for benzodiazepines upon discharge from the hospital were prescribed the benzodiazepine at the time of admission, without a specific indication (Surendrakumar D, Dunn M, & Roberts CJC, p. 88.) · As many as 38% of older adults will refill these benzodiazepine prescriptions for an additional 3 or more months following discharge from the hospital (Grad R, Tamblyn R, Holbrook AM, et al., p. 184­88.) Older adults who are at risk of abusing benzodiazepines include those who: · Drink alcohol in light to moderate amounts. · Have abused sedatives and other drugs. · Have taken methadone. Have developed physiological dependence on benzodiazepines after long­term use and are experiencing acute withdrawal effects following abrupt discontinuation. · 35 Most patients who are exposed to long­term, continuous use of benzodiazepines will develop physiological dependence. Continuous use is defined as the daily consumption of at least one dose of benzodiazepines for 4 months or longer. 1.1(h)(8) What are the adverse outcomes associated with benzodiazepine abuse? Adverse effects (sedation, inattention, memory loss, confusion, and lack of motor coordination) and toxicity often result from long­acting benzodiazepines due to poor absorption and metabolism of the drug. Higher doses of oxazepam, flurazepam, and chlordiazepoxide are associated with the greatest risk of injury in older adults. · Poor interactions with other prescription drugs. · Poor interactions with alcohol. Withdrawal symptoms including anxiety, agitation, lethargy, nausea, loss of appetite, insomnia, dizziness, tremor, poor coordination, difficulty concentrating, or confusion. 1.1(h)(9) What are the symptoms of benzodiazepine abuse? · Excessive daytime sedation · Ataxia · Problems with attention and memory · Anxiety, agitation · Impaired psychomotor abilities · Drug­related delirium or dementia (often mistaken for Alzheimer’s disease). Other potential causes of symptoms · Alcohol or other substance abuse · Bipolar illness · Other medication 36 Stressful situation (e.g., loss of a loved one, traumatic incident, major life transition such as retirement) · · Coexisting illness (e.g., diabetes, stroke, cancer) 1.1h(10) How is benzodiazepine abuse managed? Education Occasionally, simply educating patients that benzodiazepines are from a class of medications that are “habit­forming” may be an effective management strategy. Once educated about this fact, many older patients will spontaneously request discontinuation. Psychotherapy Immediately refer patients to a psychiatrist if they abuse benzodiazepines and have any of the following conditions: · Severe anxiety or anorexia · Significant psychomotor agitation or retardation · Psychosis or mania · Suicidal or homicidal thinking Consider referring patients to a psychiatrist if they abuse benzodiazepines and have any of the following disorders: · Depression · Eating disorders · Post­traumatic stress or abuse · Obsessive compulsive disorders or personality disorders 1.1(i) Suicide What is suicide? People can become depressed because of an imbalance of brain chemicals and because of stresses like the loss of a spouse, illness, or disability. Either of these may lead to thoughts of suicide. It's a sad fact, but many older adults are at risk for suicide. In fact, more than 20% of people who commit suicide are over age 65. Although most 37 people who consider suicide are depressed, most people who are depressed are not suicidal. Suicide can be prevented. Whether you have thought about suicide or you know someone who has, it's important to know the warning signs, take those signs seriously, and take action. The problems that sometimes lead to suicide can often be solved. Figure 3 Warning Signs for Suicide 1) Previous suicide attempts. Half of all people who commit suicide have attempted suicide before. 2) Talking about death or suicide. A person who is suicidal may talk about death or say things like "everyone would be better off without me." 3) Planning for suicide. Some people who are thinking about suicide put their affairs in order. They may give away prized possessions, pay off debt, and make changes to a will. 4) Depression. People who commit suicide are usually suffering from depression. Depression is an illness that can worsen because of a loss, retirement, or an illness. A person with five or more of the following symptoms may be suffering from depression that is serious enough to lead to suicide: · Sad mood · Weight loss or weight gain · Increased or decreased appetite · Change in sleeping pattern · Loss of energy, tiredness · Loss of interest in usual activities · Feelings of worthlessness and guilt · Difficulty concentrating and thinking clearly 38 · 1.1(i)(1) Focus on death and the desire to be dead Who is at risk for suicide? · Although they represented only 13 percent of the U.S. population, individuals age 65 and older accounted for 18 percent of all suicide deaths in 2000. · White men age 85 and older had the highest rates of suicide (by gender and race): 59 deaths per 100,000 persons in 2000; this rate was more than five times the U.S. rate of 10.6 per 100,000. Source: Office of Statistics and Programming, http://www.cdc.gov/ncipc/wisqars/default.htm. 1.1(i)(2) · What are the risk factors for suicide among older adults? Male Gender Men are 3 times more likely than women to commit suicide because they usually pick more lethal methods such as guns, hanging, stabbing, or jumping from buildings. Women, who often choose to commit suicide by taking pills, have a greater chance of being rescued. · Ethnicity Among elderly men, Cuban Americans and Caucasians are at greatest risk of committing suicide; native­American men are also at high risk. Among women, Asian Americans have the highest suicide rates. Native­American elders commit suicide less than whites and African­American seniors have the lowest rates of suicide for both men and women. Other Factors: Health concerns: o Multiple chronic illnesses; chronic and/or severe pain that is not appropriately managed or controlled; a cancer diagnosis or fear of having cancer; terminal illness 39 o o Psychiatric disorders: depression, schizophrenia, bipolar disorder, gambling addiction Alcohol abuse or dependence Financial concerns: o Financial difficulties due to business decisions, bankruptcy, excessive gambling debts, or medical bills Family makeup: o o Family history of suicide and/or mental illness Being married and not wanting to be a burden to family members Personal history of: o o o o Psychiatric problems, especially a mood disorder or alcohol abuse, and/or prior suicide attempts; admission to a psychiatric hospital Thinking about or voicing suicidal thoughts Low self­esteem Complicated bereavement Other risk factors: o o o 1.1(i)(3) Protestant, but seldom attends church Residence in an urban area Recent relocation What are the warning signs for suicide among older adults? (See Handout # 2 – “Crisis Intervention”) Overt comments such as: o o o “I wish I were dead.” “I’d like to just go to sleep and never wake up.” “Everyone would be better off without me.” Signs of intention such as: o o o A previous attempt at suicide “Accidents” that may have been suicide attempts (e.g., medication overdoses or noncompliance with drug regimens) Purchasing excessive amounts of medication 40 o Buying a gun Putting one’s “affairs in order”: o o o o o Making or changing a will Giving money or possessions away, especially those with sentimental value Making funeral plans Registering to become an organ donor Interest in or rejection of religion Subtle clues such as: o o o o o 1.1(i)(4) Changes in sleeping and eating patterns Self­neglect; deterioration of health; irritability Difficulty with activities of daily living Breakdown of relationships Doctor & clinic visits for vague symptoms or somatic complaints How will a doctor or mental health professional know if the person is thinking of committing suicide? Older adults who tell friends, family members, or health professionals that they are considering suicide should be taken seriously. A diagnostic interview that is conducted with respect, empathy, and sensitivity can help the health care provider determine the individual‘s intent and risk to himself or others. 1.1(i)(5) What type of treatments are available? If the diagnostic interview reveals the older adult’s intention to commit suicide, management should include referral to a hospital emergency department because the individual may require an acute psychiatric admission. A mental health plan that involves medication and psychotherapy; and/or other services such as support groups may be indicated for those people with suicidal thoughts without intent. These referrals depend on the urgency and degree of risk (e.g., on whether the individual has a specific plan and the means to carry it out) and 41 whether or not the person can agree to a verbal contract for safety. See Figure 4 for additional information. Figure 4 Crisis Intervention Older adults at a high risk for suicide may have: · Made a firm decision to commit suicide. · Lethal means of carrying out the suicide attempt. · High stress levels. · Perceived little family or social support. Older adults who are at high risk for suicide: · Should not be left alone. · And who present immediate safety risks to themselves or others should be referred to a hospital emergency department. · Should not drive themselves to the hospital. Before taking a suicidal older adult to the hospital emergency department: · He or she should be informed about the decision to go there. The professional making the recommendation should explain the primary concern for his or her welfare. It is important to emphasize the individual’s value and entitlement to treatment in order to feel better. · The health care provider and the older adult should consult with a mental health crisis line or a provider within the emergency department of the hospital by telephone. · A family member or friend should be contacted to take the individual to the hospital. · If a family member or friend is not available, the health care provider may need to call 911 to ask a police officer to take the older adult to the emergency room. 42 Other Services Older adults who have been at risk for suicide may benefit from ongoing support. In addition to referrals for medication and psychotherapy, they may be helped by: · Individual or group therapy to teach alternative coping strategies and techniques to deal with stress. · Support groups to allow expression of feelings and concerns in a supportive environment. · Community programs for older adults to minimize the risk of social isolation. 1.1(i)(6) How do I talk to a loved one about suicide? What should you do if you think that a loved one, friend, or neighbor is suicidal? Taking the time to listen and talk with him or her could mean the difference between life and death. See Figure 5 for keys to listening. Figure 5 Listening is Key · · · · Ask what is bothering him or her Be persistent Listen without judgment Listen without interrupting DO: · · · · Ask if the person is thinking about ending his or her life Let the person know you care and that he or she is not alone Say that depression can be treated and problems can be solved Offer to accompany him or her to the doctor or the emergency room DON'T: · · · Argue with the person about or out of suicide Say "you have too much to live for" Say "you will hurt your family" 43 Tips to reach out A kind word can mean a great deal. Here are some tips: · Stop by an older neighbor's house­­especially someone who lives alone or recently experienced a loss. · Call to check in with old friends and family members, just to say "hello". · Strike up a conversation with that lonely looking man you see at the pharmacy every week. 1.1(i)(7) How do I get help for someone who may be contemplating suicide? Suicide can be prevented. Take warning signs seriously, and take action. The risk factors for suicide can often be managed or treated by a professional. Getting Professional Help Encourage older adults who consider suicide to seek help from a doctor, mental health professional, or an emergency room immediately. Offer to drive or accompany the person to get help. Some people cannot seek help on their own. If the person does not have a doctor or does not know of a health care center, help him or her find one. Never leave a person alone if you think he or she is at high risk of attempting suicide. Follow Up After you take a loved one to see a health or mental health professional, help him or her to stay in touch with the doctor: · Ask about follow­up appointments. · Make sure your loved one goes to appointments. · Ask about the person's medication. Make sure he or she is taking the medication. 44 Call or visit your loved one's doctor or mental health provider if you have any concerns. Vignette # 4 Talking about Suicide "My brother still lives where I grew up­­on a reservation for Native Americans in Montana. Last year, his wife left him. He became very depressed and started to drink a lot. Lately he's been talking about wanting to kill himself. At first I had no idea what to say to my brother. I was terrified! Even though I wanted to help him, I was afraid of saying the wrong thing. My friend said I should talk with a mental health counselor to learn more about depression and the risk of suicide. I found a wonderful person at our neighborhood health clinic. She helped me to figure out what to say to my brother and she showed me how to work through my own feelings of helplessness." Thoughts of suicide don't have to lead to tragedy. Read these stories of hope to learn what others have experienced. 45 Vignette # 5 Stories of Hope June ­ Brooklyn, New York I live in a retirement community. My next­door neighbor, Sal, lost his son Joey on 9/11. He had lost his wife several years back, and his son, a firefighter, was his great pride and joy. When he lost Joey, Sal seemed to whither up­­he lost weight, got dark circles under his eyes, and his skin just hung off him. I stopped by one night, just to talk. He said he didn't know what he had to live for now that Joey was gone. I went with him the very next day to see the social worker who visits our complex. She got him help. Now Sal is planning a neighborhood spaghetti supper to raise money for the 9/11 fund. Sienna ­ Las Cruces, New Mexico My sister Darla had a tough year a few years back. She was laid off from the company where she had worked for 19 years. Then she lost her beloved dog and her osteoporosis was so bad that she needed a wheelchair to get around. She seemed so sad all the time, and complained about how unfair life was. She started giving her grandchildren all her kitchenware. She said she didn't need it anymore. Cooking had always been Darla's great pleasure. One day she told me how easy it would be if she could just swallow a few extra pain pills. I stayed over that night and took her to the community health center the next day. They said she was suffering from depression, and she started seeing a specialist. She is back to her old self again and back cooking up a storm! 46 Chapter 2 Diagnostic and Treatment Issues 1. 2. 3. 4. To be able to recognize if someone needs help. To be aware of where to turn for a mental health assessment/diagnosis. To be familiar with barriers to detection and treatment of mental health conditions in the elderly. To be aware of how to share your concerns regarding mental health with others. Introduction Shame and social stigma associated with mental health problems prevent many people, especially the elderly, from seeking professional help. Many older people prefer to see their general practitioner for all of their health concerns. Some general practitioners do not have specialized training in mental health service delivery; this, along with the reluctance to seek help, can lead to undiagnosed and untreated mental health conditions among the elderly. 2.1 How do I know if someone needs help? Certain skills are helpful when dealing with people who are emotionally upset. These include: · Listening · Expressing sincere concern · Demonstrating kindness · Showing respect and courtesy · Using a calm tone of voice and manner · Exhibiting non­judgmental attitudes · Being supportive and gentle · Avoiding arguments or provoking agitated or aggressive behavior · Using reassurance when appropriate but avoiding false reassurance 47 2.2 Where do I turn for a mental health assessment/diagnosis? For many people the initial entry point for assessment of mental health concerns is their primary physician or general practitioner. For others they may feel comfortable accessing, and live in an area that has, specialized mental health centers or clinics that provide assessments, treatment, or referrals. Wherever the entry point, it is important to ask for an assessment if you question a loved ones mental health. The cost of the assessment is often a concern for family members. Can my loved one afford the assessment and subsequent treatment. See Educational Tool Kit 4, Chapter 4 for information regarding financial assistance that may be available. However, if you live in household with a person who has an Employee Assistance Program (EAP) benefit through their employer you may be eligible to see a counselor free of charge through this confidential employer sponsored benefit. In addition, the internet offers a variety of self­assessments that an individual can take in privacy as an initial screening. If you think your results warrant further assessment you can print your results to bring with you to your initial appointment. If you are not sure where to turn, contact your doctor or local clinic for information on how to access mental health care in your region. You do not need to go into detail or reveal your identity to get this information. (See the resource section at the end of this document for more information.) Samples of these assessments can be found in the resource section of this document. 48 Figure 1 Instruments Used to Assess Mental Health Issues in Older Adults 2.3 · Clinical Dementia Rating · Geriatric Depression Scale (GDS) Short Form · Health Screening Survey (HSS) · Index of Activities of Daily Living (ADLs) · Instrumental Activities of Daily Living (IADL) Scale · Mini Mental Status Examination · Michigan Alcoholism Screening Test—Geriatric Version (MAST­G) · The Alcohol Use Disorders identification Test (AUDIT) · The Center for Epidemiologic Studies Depression Scale (CES­D) What are the barriers to detection and treatment of mental health conditions in the elderly? Several barriers may hinder detection of mental health problems in older adults; these factors may also result in underreporting the seriousness of one’s symptoms. The barriers include: · Age­related Changes Signs of depression may look like changes that are often misconstrued as a normal part of aging such as reduced activity level, reduced appetite, changes in sleep patterns, or stooped posture. · Illness Physical illness can mask depression and depression can mimic physical ailments, often leading to misdiagnosis. If depression and/or anxiety co­exists with a physical illness, it often worsens or complicates the physical problem. 49 Several influential factors in the healthcare system (managed care, cost reduction efforts, and so forth) increasingly restrict the amount of time doctors spend in patient care, forcing mental health concerns to compete with general medical conditions. Elderly may not feel comfortable bringing up uncomfortable issues if they feel rushed. · Attitudes of Others Signs of mental illness may be dismissed because of stereotypical beliefs about older people—for example, defining them as “difficult” or irritable, forgetful, complaining about their health, or appearing sad. Providers may be reluctant to inform older patients of a diagnosis due to uncertainty about the diagnosis, reluctance to stigmatize, uncertainty regarding effective treatment, concern about medication interactions, lack of access to psychiatric care, or concerns about the effectiveness or cost­effectiveness of treatment interventions (Surgeon Generals Report, 2001) · Denial Having grown up in a time when “toughing things out” was the approved remedy, older adults may deny their mental illness symptoms as signs of seeming weak or crazy. · Alcohol or Drugs Some people in late life turn to alcohol or drugs to cope with losses. Because these substances can slow the central nervous system, their consumption can intensify depression— and can be lethal in some mental health treatments. · Health Complaints Some older adults tend to somaticize—complain about physical problems, rather than talk about emotional pain. Complaints may center on problems with weakness, constipation, abdominal pains, chest pains or other vague symptoms disguising the underlying mental health condition. 50 · Stigma As long the stigma of mental illness remains, the difficulty of identifying mental health disorders in older adults and providing them with proper care will remain a significant barrier to their ability to reach mental wellness (www.asaging.org). 2.4 How do I share my concerns regarding mental health with others? If someone you cared about were ill and needed help, chances are you would do everything you could to provide assistance. But when that person shows signs of mental illness it’s hard for most people to know what to do or say. It can be hard to know how to discuss your concerns regarding the mental health issues with an older adult. This section will provide some information on how to begin this important discussion. Specific training in counseling or mental health skills is not necessary in order to address your loved one regarding the concerns you have about his/her behavior or mental health. Before talking to the person you are concerned about it might help to consult a professional who is knowledgeable on the needs of older adults such as counselor, psychologist, doctor, minister, or social worker. This person can help you look at the situation more objectively and explore your options. Before consulting with the professional you may want to gather the following information to help with the informal assessment as to what help your loved one might need and how the person should be approached. 51 Figure 2 General guidelines for initiation the conversation • • • • • • • • • • • • Avoid talking to the person if they are upset or under the influence of a substance Be gentle and kind Avoid a confrontational style Avoid using labels since they may carry a heavy stigma Take into consideration the person’s age and ability to understand; you may need to discuss the issue is several sessions rather than one big conversation. Be consistent and patient in your expression of concern without exerting undue pressure Be direct; treat the individual as an adult Give specific examples of behaviors that concern you Use I statements as in “I am concerned about you because I have noticed you wearing the same cloths for several days and have not seen you outside in your garden as you usually are.” Be prepared with information in case the person is willing to seek help Don’t be discouraged if the person is not ready to accept your assistance—you may want to enlist the aid of others who are also concerned or try again on another occasion Don’t worry if you don’t say things perfectly, what is important is that your message of concern is conveyed and your willingness to help is expressed 2.5 Where can I get more information? · In person Talk with your doctor or contact your local mental health agency · Online www.asaging.org www.csat.samhsa.gov www.positiveaging.org www.surgeongeneral.gov www.webmd.com · Telephone Federal Center for Mental health Services – 1­800­789­2647 FirstLink Hotline – (701) 235­7335 National Eldercare Locator – 1­800­677­1116 North Dakota Helpline – 211 · Handouts How to Talk to an Older Person Who Has a Problem With Alcohol or Medications Hazelden 52 1­800­257­7800 www.hazelden.org Fact Sheet #8: Prevention and Treatment of Mental Health Problems Among Older Adults Get Connected! Linking Older Adults with Medication, Alcohol, and Mental Health Resources National Clearinghouse for Alcohol and Drug Information (NCADI) 1­800 53 References: Best nursing practices in care for older adults: Incorporating essential gerontologic content into baccalaureate nursing education (2nd ed, Topic 6, p. 7). New York: The John A. Hartford Foundation Institute for Geriatric Nursing, Division of Nursing, School of Education, New York University.(move citation up) ­729­6686 David Meagher, Delirium: the role of psychiatry, Advances in Psychiatric Treatment (2001) 7: 433­442. 54