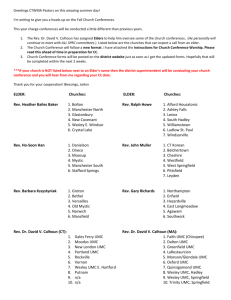
September - UMC Health System
advertisement

UMC Health System September 2015 From Peter’s Desk by Peter Laverty Is your Estate Plan Complete? Let’s check, Will drawn up? Check. Executor named for the estate, advance directives signed, and funeral arrangements specified? Check, check, and check. Not long ago, you would have been finished; you would have taken all the advance planning needed. Not any longer, in the 21st Century your estate planning may need an additional review. You now live in the electronic age. There is one key facet of your estate planning you may have overlooked: your digital estate plan. This plan will lay out your digital assets — both financial (such as online bank and brokerage accounts, utility accounts and download destinations like Amazon, Apple, Netflix, and eBay) and social (like Facebook, eHarmony and twitter accounts) — and provides directions on how to access and handle them upon your death. Until last month when I started looking into digital estate planning I never gave much thought what would happen to them after my death and never once thought to appoint an executor of my electronic files and personal information stored there. When I was setting up my own, I found a lot of information that would need someone to take care of. I had apps to close, payments that needed to be stopped, pictures to be given to my family and my financial records that I only had on line. Then all these digital sites needed sign in names and passwords to open my digital world. Here are five steps to help you create your individual digital estate plan: Step 1: Make an inventory list of your digital assets and how best to access them. • Online sign in name, password and account number for each account. Be careful how you store this list, if hacked it could cause real problems. • Your digital inventory could include the following: • Your Facebook, Twitter, eHarmony, church and other social media accounts. • Bank, credit union, brokerage, retirement plan, credit card, funeral plan, loan, and insurance accounts that you access online. Your accounts could include: • Online retail accounts and apps from stores, flash sale sites or marketplaces like eBay, Amazon, Netflix and iTunes. • Photo- or video-sharing sites • Music sites • PayPal or other online payment accounts • Utility bills you pay online • Any other online accounts such as ones from airline sites with your frequent flier miles, the cloud and hundreds more. If you use a “digital wallet” product on your cell phone — like a prepaid restaurant app that lets you pay from your phone — this too might be worth adding to the list. Update these inventories at least once a year — or, ideally, whenever you change a password, or close or open a digital account. Step 2: Find a safe place to store this information. Since your digital inventories contain personal information that could lead to identity theft and financial losses if it gets into the wrong hands, “you have to be very careful” about where you put them. One option is to store the lists in a safety deposit box at your bank. Alternatively, you might put them in a online site like Password Box or SecureSafe, which securely encrypts and stores all of your account information and passwords in one place. You can also use one of these sites to store copies of important documents such as your wills and trusts, the deed to your house, stock certificates and birth certificates. When you die, your beneficiaries get access to everything you have stored. Both sites have a free program that can be upgraded, for a price, if needed, it will depend on your storage needs. If that makes you nervous, you can also give the lists, or a copy of them, to a trusted person like your spouse, child or best friend, as well as your digital executor. Step 3: Name a “digital executor.” This is the person you designate to carry out your digital estate plan upon your death, ensuring that your end-of-life requests are met. Your digital executor should be impartial and mature, able to handle this sensitive information responsibly, and technologically savvy. Once you have settled on someone who fits that description, name him or her as your digital executor in your will. Step 4: Write out instructions for what should happen to your digital assets after you die. Your will most likely lays out the distribution of all your bank and brokerage accounts, so you probably don’t need a separate written plan for the ones you access online. Make sure the executor of your will and the executor of your digital estate knows how to obtain your list of online financial accounts. Create a to-do list outlining how you want all things digital — from your Facebook and LinkedIn profiles to your Flickr and YouTube accounts — to be handled when you die. Then give this document to your digital executor. The to-do list should answer questions like these: • Do you want your Facebook account deactivated when you die, or do you want it to remain online as a memorial of your life? • Do you want your Picasa photos wiped out or sent to a family members? In general, Facebook will not grant access to an account to anyone other than the account holder (or your digital executor, if you’ve given him or her permission to enter your user name and password). This is not an easy job and will be almost impossible if your executor does not have digital executor power. Step 5: Consider whether you want to post a final message online. Your digital estate plan can also explain how you want to send a final online message (or messages) to friends and family. Whatever you decide to do, be sure your digital estate plan provides specific instructions for your digital executor about any content you want to be posted online upon your death, as well as how and when it should be posted. Seniors Are Special is a service of UMC Health System and Texas Tech University Health Sciences Center 602 Indiana Ave • Lubbock, TX 79415 • 806-775-8760 Seniors are Special News – September 2015 2 Medicare Premiums May Jump for Some in 2016 But not so for Social Security Benefits Retirees are facing a double-whammy next year: no inflation adjustment in their Social Security benefits and a whopping 52 % jump in certain Medicare premiums, stated a report by Mark Miller writing for Ruetgers on August 6, 2015. Miller states the Medicare premium hikes will hit only 30 % of beneficiaries – those who are not protected from a “hold-harmless” provision in federal law that prohibits any premium hike that produces a net reduction in Social Security benefits. However, the likely increases suggest strongly that the recent trend of moderate healthcare inflation is ending. Let’s start with the Social Security news. Final figures for 2016 will not be available until the fall, but the recent annual report of Social Security’s trustees projects that there will not be any cost-of-living adjustment (COLA) next year. The COLA is determined by averaging together third-quarter inflation as measured by the Consumer Price Index for Urban Wage Earners and Clerical Workers (CPI-W). Inflation has been flat due to collapsing oil prices. On the healthcare front, renewed cost pressures are pointing toward much higher Medicare premiums starting next year, according to the Medicare trustees’ annual report. Consider the monthly premium for Part B (outpatient services), which has stayed at $104.90 for the past three years. The Medicare trustees projected that the premium will jump 52 %, to $159.30 for beneficiaries who are not protected by the hold harmless provision. That would include anyone enrolled in Medicare who is not yet taking Social Security benefits due to a decision to delay enrollment. It also would include new enrollees in Medicare next year. (The increase also would be applied to lowincome beneficiaries whose premiums are paid by state Medicaid programs). High-income retirees – another group that is not protected by the hold-harmless provision – also will be hit hard if the trustee projections hold. Affluent seniors already pay more for Medicare Part B and also Part D for prescription-drug coverage. This year, for example, higher-income seniors pay between $146.90 and $335.70 monthly for Part B, depending on their income, rather than $104.90. The Medicare trustees now project that to jump even more. Higher costs for the affluent look like a trend that could accelerate further. The recently passed “doc fix” legislation (which corrects long-standing problems with reimbursement rates to physicians) shifts a higher percentage of costs to higher-income seniors starting in 2018. Seniors with incomes of $133,000 to $160,000 would pay 65 % of total premium costs, rather than 50 % today. Seniors with incomes between $160,000 and $214,000 would pay 80 %, as they do today. (Note this has not been confirmed by CMS as of 8/20/16) Physical Therapist's Role in Peripheral Neuropathy by Theresa Heflin, PT Peripheral Neuropathy (PN) is a condition that develops as a result of damage to the peripheral nervous system, which is a network of nerves that transfers information from your brain/spinal cord to the rest of the body. Symptoms can range from numbness or tingling, to pricking sensations, burning pain (especially at night), muscle wasting/weakness and hypersensitivity. Although the symptoms of PN can cause discomfort and loss of function, there is evidence that PN may improve over time. Treatment by a physical therapist can help reduce symptoms and improve an individual’s quality of life. PN may be either inherited or developed because of a disease process or trauma. Trauma is the most common cause of the nerve injuries (i.e. auto accidents, falls, sports related activities and surgical procedures). Diseases or disorders and their related processes (such as inflammation) can be associated with peripheral neuropathy. Diabetes is the leading cause of peripheral neuropathy in the US. About 60-70% of people with diabetes have mild to severe forms of nervous system damage that can affect the ability to feel sensation and/or the ability to move parts of your body. Problems with circulation, autoimmune diseases, kidney disorders, cancers, neuromas and infections can also cause PN. Exposure to toxins such as medication toxicity, environmental or industrial toxins and heavy alcohol consumption may damage nerves and cause PN as well. Physical therapists play a vital role in helping individuals improve and maintain function that may be limited by PN. Your physical therapist will work with you to develop a treatment plan to help address your specific needs and goals. For example, nerve gliding activities allow the nerves to move more easily as you bend and straighten your joint. This can help with single nerve injuries such as carpel tunnel syndrome. Modalities such as TENS (transcutaneous electrical nerve stimulation) can help with pain management. Moderate intensity exercises can help improve strength and physical function. Balance and coordination activities are extremely important to decrease the risk of falling. PN, (especially diabetic PN) decreases sensation and awareness of where your joint is in space, therefore affecting your ability to sense uneven ground, objects or changes in temperature. Another way your physical therapist can help is by educating you on how to safely manage your PN, be aware of changes in skin color, temperature and making sure your skin is intact. Education can be provided about proper splinting/bracing, modification of the way you perform certain tasks, as well as providing home safety recommendations. Physical therapists are prepared through education and experience to treat conditions, such as PN. General tips when looking for a physical therapist: Get recommendations from family and friends or from other health care providers. When you contact a physical therapy clinic for an appointment, ask about the physical therapists’ experience in helping people with PN. During your first visit with the physical therapist, be prepared to describe your symptoms in as much detail as possible, and keeping a journal highlighting when you experience pain will help the physical therapist identify the best way of approaching care. Because there are many conditions associated with PN, such as diabetes, some basic lifestyle modifications can help reduce the risk of its development. Maintaining an active, healthy lifestyle may help reduce your risk of developing certain types of PN and the complications associated with it. If you suspect symptoms of PN, see your physician for more definitive testing and planning for management and treatment. – written by Theresa Heflin PT, Physical Medicine and Rehab Dept. Facts About Adult Vaccination - Not Just For Kids! 1. People on Medicare Part B can get influenza, pneumococcal, and hepatitis B vaccines at no cost. 2. Pneumococcal vaccination is one-time for adults age 65 years and older. 3. Serious complications of mumps are more common among adults than children. 4. Adults are much more likely than children to die from chickenpox if they get it. 5. Influenza vaccination can reduce physician visits and lost work days, and reduce antibiotic use. 6. The hepatitis B vaccine prevents cancer, specifically primary liver cancer. 7. There are about one million cases of shingles in the US every year. 8. Due to high immunization rates, 50 or fewer cases of tetanus occur each year in the US. 9. By age 50 years, 80 % of women will be infected with human papillomavirus. 10. Hepatitis A is one of the most common vaccine-preventable disease acquired during travel outside the US. Seniors are Special News – September 2015 Are Your Heartburn Medications Killing You? 3 by Dr. Sammer Islam Did you know that ice cream was once linked to causing polio? It was all over the medical journals and it was thought to be a proven fact. Well there was at least a statistical correlation which confirmed this association….right? There has been a lot of information in the press about the possibility of developing a heart attack while on Prilosec or Nexium therapy according to research study that recently was published. When this study first came out, my Facebook account and email was flooded with messages from patients and friends asking me whether they should stop taking these medications. I am in favor of minimizing unnecessary drugs for my patients. If there is not a clinical indication to be on a treatment, then we should try and get you off of it. Proton pump inhibitors or PPIs have helped thousands of patients with treatment of bleeding ulcers, reflux symptoms or indigestion, and overall made people feel better. So should you continue taking these medications in light of this study? Here is what I have to say: What did the study ACTUALLY find: The risk of developing a heart attack was 16%. This sounds scary - but when you look at the data itself it is not as impressive as it may seem. The rate of a heart attack or myocardial infarction (MI) would require treatment of 4000 patients with PPIs to produce just one additional MI. That is a lot of people that need treatment for the possibility of one heart attack. The study methods involve taking data from thousands of patients, mixing it up together, and using a computer model to suggest an association. 2.9 MILLION patients were data mined - which means they were put into this computer to find an association. This is analogous to taking the population of Dallas, seeing which patients had heart-attacks, and finding most of them had taken a bubble-bath in the evening of their heart-attack, therefore concluding bubble-baths cause an MI. Studies of this type cannot prove causality and certainly do not define a mechanism. In the study, the patients who were on PPI therapy may be sicker than those who were not. No one really knows why those patients who were on PPI therapy had this association. Maybe they were sicker overall? Maybe they had other risk factors for MI that were not addressed such as obesity, diabetes, smoking - all risk factors for both heartburn and a heart attack? The point is that there are numerous queries about this patient population that we just don’t know. This raises the question as to whether there were confounding factors involved, limitations the authors of this study acknowledge themselves. Drug dosages were not analyzed Also of contention is the study authors could not stratify which drug dosages are at higher risk. Is it all doses of PPI or only the high-doses? Is it patients who take it every day or as needed? Duration of medication use was also not addressed - if I only take a PPI for 3 months, is my risk higher versus taking it for one year? What if I stop my medications for a couple of weeks and restart again - does my risk change? Additionally, not all of the drugs within the class of PPIs had this association; two of the five drugs studied did NOT show a correlation. Why was that? These are all questions in which the study could not answer, leaving me to wonder how accurate the data might be. All patients, regardless of PPI therapy, need to improve their overall health Regardless if you have heartburn or reflux, or are on PPI therapy, living a heart-healthy lifestyle is best for your overall health. This means exercising, eating right, routine health maintenance, checking your lipid profile, etc. Mitigating risk factors for a heart attack will not only improve your overall health, but will also help with your reflux symptoms. There is nothing in this study which would change my clinical practice For me, if I feel like my patients clinically need a PPI, I would still recommend this to them. If I feel like they do not need a PPI, I would recommend them to stop it, solely based on the fact I truly believe the less medications the better, and NOT based on this study. Very commonly in the medical field, studies come out that seem to show a correlation and immediately a causative effect is assumed. This is a false fallacy. Don’t forget the ice cream and polio effect; correlation does NOT necessarily equal causation. Sameer Islam, MD is a board-certified Gastroenterologist and Hepatologist practicing at Southwest Gastroenterology. For an appointment contact his office (806)-761-0747. You can get more information from his webpage (www. sameerislam.com), Facebook (facebook.com/sameerislamd), Twitter (@sislamMD), or watch his videos on YouTube (youtube.com/sameerislammd). Medicare 101 Peter Laverty, Director Seniors are special will present a morning training seminar on the Basics of Medicare. This seminar is an introduction to Medicare for those that will soon be entering Medicare or those interested in a short refresher course. Saturday, September 12, 2015 | 10:00 AM – Noon | UMC Activities Center, 5217 82nd (RockRidge Shopping Center) This seminar will include: • Basic information about Medicare • Avoiding penalties • Important decisions you need to make • Should I keep/sign up for Part B? • Your choices in health and prescription drug coverage • What about Medicare D? • When to make decisions to ensure coverage You must register ahead of time for the seminar, please note that seating is limited. To register call SAS at 775-8760. This is an information seminar only, no insurance will be sold, nor will insurance agents will be permitted to pass out information including business cards. UMC’s Better Breathers Club to meet at UMC Activities Center The UMC Better Breathers Club is a support group for people with Chronic Lung disease such as COPD, Asthma, Pulmonary Fibrosis and Lung Cancer. Joining is free! Learn to manage your lung disease and live better. The Better Breathers Club meets the second Monday of every month from 6:00 pm to 7:30pm at the UMC Activities Center at 5217 82nd Street, 82nd & Slide in Rockridge Plaza. Our next meeting will be Monday, August 10th. This month’s speakers are Dr. Jessica Nelson and Dr. Medhut Guirguis from TTUHSC Psychology Dept.They will talk on anxiety and depression. For additional information, contact Lori Stroud at 775-8950. Seniors are Special News – September 2015 4 UMC Activities Center – Lewis Walker & Julie Dominguez College football season is finally here, and I for one am very excited! Finally something to watch on TV giving me a reason not to move off the couch on a Saturday afternoons into the evening. Daisy (my dog) will not be excited as she does not like when I watch sports; especially Texas Tech football. She climbs on the couch and wants to cuddle. Daisy gets as close to me as she can. I guess she can sense my anxiety or demeanor changing even before opening kickoff. Being close is her way of calming me down. Daisy is going to spend a lot of time on my lap this football season. This is the first time in four years that I have not had season tickets to Tech football. It is going to be a change for me and Daisy. No more going early to find decent free parking, no more frito pie in the Frazier Alumni Pavilion, and no more feeling the energy of the crowd. And I am completely okay with this change. I may still be able to make a game or two as some friends have season tickets and might let me tag along. But, I was ready for a change, a break from the game day routine I have had for several years. Change can be good! Change can be good, but it can also be challenging. Even things most would consider little changes that only last a day or two can throw us for a loop. They might be little to others but to us, they are awful. I see and hear about changes at the UMC Activities Center often. The parking lot is too busy, the dollar store closed, an instructor makes changes to the class they teach or there is a substitute instructor who teaches different than the regular instructor. The instructor is still providing a great workout that is challenging the class in a different way than before. These changes throw the participants off. The parking lot raises their blood pressure or they can’t run next door to shop like they used to. But change is different and that can make some feel angst. I am not immune to not liking change. Several times a week I participate in an exercise class. It is my time to focus on me and not be in charge of the exercise time or be watching individuals form in the class. The instructor for the class will normally post on the internet the night before what the class will be doing. It is usually some combination of higher intensity weight training with cardiovascular exercise. That was until late July when on multiple occasions what was posted online was not what we performed the next morning. The tables had been turned! I was the one now feeling the angst of change. I had mentally prepared myself for what was posted and struggled with the change. Change is like that! It can throw us for a loop and make things extremely difficult. It can make us want to quit, walk away or try to ignore the change. I went through these thought processes that morning when I went to workout and it was not what I was expecting. But, instead I luckily remembered what a member of the UMC Activities Center said one morning: “I don’t have to do it, but I GET to.” I GET TO. Those three little words made all the difference for me. The next time you encounter a change or something you are not keen on. Remember the three little words, “I GET TO,” because one day you may not be physically, emotionally, or mentally able to GET TO. Class Spotlight: The class under the spotlight this month is T’ai Chi Ch’uan with Larry Sava. T’ai Chi Ch’uan is a slow moving activity whose movements are flowing, circular, and weight shifting. It has been described as a soft martial art technique (mind and body) emphasizing health, balance and energy. T’ai Chi Ch’uan can be performed as individual movements or as a series (a Form). Several forms of T’ai Chi Ch’uan are taught in this class these forms may include: WuHao, Yang Short Form (37) and others. Minimum physical requirement: ability to stand for 20 minutes. T’ai Chi Ch’uan with Larry meets on Tuesday and Thursday at 3:00PM. T’ai Chi Ch’uan may be ideal for individuals who are looking to start an exercise routine but are not looking for a “traditional style” of group fitness class that includes a form of cardiovascular exercise and weights. T’ai Chi Ch’uan might also be a good fit for individuals who are “stiff”, suffer from arthritis or fibromyalgia and need gentler movements associated with exercise. Studies conducted by Texas Tech and Texas Tech University Health Sciences Center researchers “have shown that tai chi can be beneficial in decreasing pain and stiffness in those with arthritic knees, as well as reducing stress.” (www.ttuhsc.edu) Individuals who participate in this form of exercise may see an improvement in balance, coordination, strength and wellbeing. Come give it a try! From the Membership: This month we decide to talk to the entire T’ai Chi Ch’uan class and asked them to share their thoughts on the class. They gave us the following information: “We enjoy T’ai Chi Ch’uan for the tranquil and peaceful movements while exercising as a group. T’ai Chi Ch’uan will help increase your balance, flexibility, mobility, focus and overall energy. It helps to reduce stress levels, improve concentration, and strengthen bones and joints. The instructor and substitute instructor are patient and clear. They encourage us and make allowances for our abilities and capacities.” Nutrition Talk at the UMC Activities Center: On Wednesday, September 16th at 3:00PM, the UMC Activities Center will host a Nutrition Talk with Autumn Bollinger, MS, RD, LD. The topic this month will be Sugar vs Sugar Substitutes. Understanding Artificial Sweeteners and Sugar Substitutes - Harm or Help. The lectures are open to anyone so feel free to invite a family member, friend, or neighbor to attend! The UMC Activities Center is located at 5217 82nd Street (SW corner of 82nd & Slide in the RockRidge Plaza). For further information, contact the office at 783-8829. Closed for Labor Day: The UMC Activities Center will be closed on Monday September 7th for Labor Day. Have a safe and happy holiday. Regular hours will resume on Tuesday, September 8th. Seniors Are Special’s Monthly Seminar Wednesday, September 9, 2015 | 3:00 PM – 5:00 PM | McInturff Conference Center at UMC Medical Topic: 3:00 PM | Sarah Hancock, RN, UMC Stroke Educator “UMC Stroke Services” Medical Topic: 4:00 PM Dr. Steven Brooks Department of Surgery TTUHSC Director UMC Geriatric Trauma “Geriatric Trauma” Refreshments are served between speakers. Join us for Seniors are Special’s monthly educational seminars. These seminars meet on the second Wednesday of each month beginning at 3:00 PM in UMC’s McInturff Conference Center. The meetings are free, open to the public, and no reservations are necessary. Please bring a friend. For further information on these meetings, call SAS at 806775-8760. Shuttle transportation service is available from Tech’s southwest parking lot for SAS’s monthly meeting UMC’s Courtesy Shuttle vans provide free shuttle service between 2:30 PM and 3:30 PM and 4:15 PM to 5:15 PM for our seminar guests. The shuttle picks up at the Texas Tech parking lot located SOUTH WEST of the Texas Tech Parkway, off 10th Street. Turn west at the 10th Street & Texas Tech Parkway light. The parking lot is located one block down on your left hand side of the street. Follow the SAS parking signs. You are, however, free to park in any of UMC’s parking lots.