Discharge Summary - The ICD
advertisement

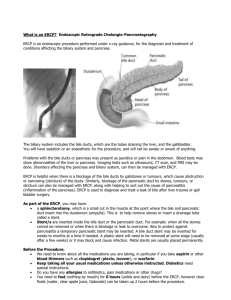
Discharge Summary DISCH ARGE DIAGNOSIS: Cho ledocho lithiasis. C HRON IC DIAGN OSES: I. Dementia. 2. Hyperten sion . CON DITION ON DISCH ARGE: Improved. PROC EDURES AND DIAGNOSTI CS: ERe p with a successfu l sphincterotomy and stone removal HOSPITAL COU RSE: This is an 88-year-old Caucasian female admitted from an outside hospital after developing fevers and tachycardia. After a cho lecystomy and unsuccessful ERC P, she was admitted for a repeat ERCP and sphincterotomy and stone removal for cho ledocholithiasis. I. Cho ledocho lithiasis. Originally thought to be sept ic or infected. Prior to adm ission with fevers reported at an outside fac il ity, however, during her hospitali zation here she was afebril e with no leukocytosis and ERe p was performed with successful sphincterotomy and stone removal and the patient was discharged back to her care facility with a prescription for Levaquin x5 days for a total of antibiotics for 5 days. On admission she did receive erta penem and then vancomycin as an inpatient. 2. Chronic problems of dementia and hypertension were at patient's baseline and home medicati ons including Lotrel and Risperdal were continued. DISPOSITION: The patient was discharged to care physician . MEDICATIONS ON DISCH ARGE: I. Levaquin 500 mg daily x5 days. 2. Lotrel40 mg daily. 3. Risperdal 0.5 mg b.i. d, 4 . Tylenol p.r.n, 5. Metoclopramide 5 mg prior to meal as well. 6. Omeprazo le 40 mg daily. with follow-up by her primary History and Physical C HIEF CO MP LAINT: Abdominal pai n. HISTORY OF PRESENT ILLN ESS: The patient is an 88-year-old Caucasian fema le with dementia who recently visited her primary care provider after havin g refractory nausea, vomi ting, and abdominal pain in her care center. On presentation to her PCP, she did have increased right upper quadrant pain with a white co unt of 17.5 and lipase of 5 1O. At that tim e, physician did order an ultrasoun d which demonstra ted ga llbladder wall thi ckenin g and stones as well as signs of pan creatitis with increased LFTs and abnormal bilirubin. Laparoscopic cholecystectomy was scheduled and proceeded with the next day on with intraoperati ve cholangiogram showing incomplete obstruction distal to the common bile duct, and calculus with moderate dilatati on of the biliary tree and ERe ? was performed on the which was unsuccessful in cannulating th e common bile duct and did show choledocholithiasis. The patient had remain ed fairly stable throughout her hospitalization at outside facility until just prior to transportati on. At which time, she did have a fever of 101.7 and heart rate up to 122. The patient did then receive ertapenem antibiotics for broader coverage of any GI path ogens an d was transferred to the thi s hospital. On arriva l, the patient was quite delirious and unable to respond appropriately to questions; therefore, personal history from the patient was not able to be obtained. REVI EW OF SYSTEMS: The patient is unabl e to co mplete . ME DICAL HISTORY: Inclu des dementia with psychi atric features, pne umon ia, hypertension, and anemia. SURG ICAL HISTORY : Unknown. History and Physical SOCIAL HISTORY : Wid ow in a nu rsing faci lity. ALLERGIES : NONE KNOWN. FAM ILY HISTOR Y: A lso unknown. MEDIC An ON S: At home include Lotre l, Reglan, Risperda l, Tylenol, and Phenergan. H osp ital medications included amlodipine 5 mg, Tylenol 650 mg p.r.n., morphine 2 mg p.r.n., Zofran p.r.n., benazepri VH CI 40, Nex ium 40 mg, risperid one 0.5 mg b.i.d., as we ll as fentanyl, Glucagon, and propofol during the procedures. PHYSICAL EXAMINA T ION: VITAL SIGNS: The patient did have a temperature o f37.4 degre es on admission with the heart rate of 129, blood pressure of 184/94, and respiratory rate of24. She was saturating 92% on 2 L of oxyge n. GENERAL: Th is is a confused Cachectic-appearing elderly wo man in apparent psychiatric distress. HEENT: Nonnocephalic and atraumatic with loss of dentition. Pupils are reactive. Extraocular movements are intact. CARD IAC EXAM: Shows tachycardi c heart with no murmurs, rub s, or ga llop s. RES PIRA TORY EXAM: C lear to ausc ultatio n b ilaterally. ABDOMEN: Soft and nood istended with minimal tenderness to deep palpati on . Bowe l sounds are positive. EXTREM ITIES : Show no cl ubb ing, cyanosis or ede ma with 2+ dorsal ped al and rad ial pulses. LABORATORY DATA: Laboratory was sent from the patient; however, was from w ith the following pertinent exam . White count of 17 and hemo globin 13.5. Alkaline phosphata se of 186, AST of 106, ALT of209, and lipase of 5 1o. ASSESSMEN T AND PLAN: Thi s is an 88-year-o ld Ca uca sian fem ale wi th cho ledoc ho lithia sis status post failed ERCP. History and Physical 1. Cho ledocholith iasis with fever. The pat ient is afebrile wh ile arriving to , however, her increased blood pressures and tachycard ia are concern ing for a septic picture ; there fore, we will broaden spectru m of antibiotics to ertapenem I g da ily and add vancomyci n to this. The patient is scheduled for ERC P th is evening. 2. Hyperten sion . The patient has had elevated blood pressures s ince admiss ion and was started on benazepril HCl40 and amlod ipine 5 mg . We will giv e her bo lus o f 500 mL of IV fluids and hel p regulate hyperten sive medication s as needed. 3. Dementi a. This is chro nic and of unkn own etiology. The pat ient does appea r to have some e leme nt of deli rium, superimposed with dem entia. At this time, we w ill continue Risperdal 0 .5 mg b.i.d, 4 . Fluids, electro lytes and nutrition . The patient is to remain nothin g by mouth for her procedure. We will obtain CSC, CMP, PT, INR, urinary culture and ana lys is for furth er workup of electro lytes and other abnorma lities, Again, the patient will rece ive 500 mL of norm al saline. 5. Proph ylaxis. We will not need prophylax is at this time as the patient will be go ing to procedure. 6 . Code status is full as und ersto od by the patient livin g we ll in chart. Procedure: Indications: Providers: ERCP Filling defect on intraoperative cholangiogram, Suspected bile duct stoners) Referring MD: Requesting Provider: Medicines: General Anesthesia Complications: No immediate complications Procedure: Pre-Anesthesia Assessment - Prior to the procedure, a History and Physical was performed, and patient med ication allergies have been reviewed. The patient's tolerance of previous anesthesia has been reviewed. - The risks and benefits of the procedure and the sedation options and risks were discussed with the palient. All questions were answered and informed consent was obta ined. - Patient identification and proposed procedure were verified prior to the procedure by the physician and the nurse. The procedure was verified in the pre-procedure area. - Pre-procedure physical examination revealed no contraindications to sedation . - ASA Grade Assessment: II - A patient with mild systemic disease. - After reviewing the risks and benefits, the patient was deemed in satisfactory condition to undergo the procedure. - The anesthesia plan was to use moderate sedation/analgesia (conscious sedation). - Immediately prior to administration of medications, the patient was re-assessed for adequacy to receive sedatives. - The heart rate, respi ratory rate, oxygen saturations, blood pressure, adequacy of pulmonary ventilation, and response to care were mon itored throughout the procedu re. - The physical status of the patient was re-assessed after the procedure. After obtaining informed consent from the patient's daughter, the scope was passed under direct vision. Throughout the procedure, the patient's blood pressure, pulse, and oxygen saturations were monitored continuously. The Duodenal Scope was introduced through the mouth, and used to inject contrast into and used to inject contrast into the bile duct. The ERCP was accomplished without difficulty. The patient tolerated the procedure well. Findings: T he scout film was showed surgical clips in RUQ. The esophagus was successfully intubated under direct vision. The scope was advanced to a normal major papilla in the descending duodenum without detailed examination of the pharynx, larynx and associated structures, and upper GI tract. The upper GI tract was grossly normal. The cannulation was straightforward, The bile duct was deeply cannulated with the short-nosed traction sphincterotome and 0.025" wire without the use of contrast and on the first tOUCh. A pancreatogram was neither altempted nor obtained. Contrast was injected . I personally interpreted the bile duct images. There was brisk flow of contrast through the duels. Image quality was excellent. Contrast extended to the entire biliary tree.The lower third of the main bile duct contained one filling defect consistent with a stone, wh ich was 9 mm in diameter. The main bile duct was diffusely dilated . The largest diameter was 10 mm. The intrahepatic branches were not dilated. There were oostoe chances cIw CCY. Biliarv sphincterotomy was made with a monofiiament Autotome sphincterotome using ERBE electrocautery. There was no post-sphincterotomy bleeding. To discover objects, the biliary tree was swept with a 9-12 mm balloon starting at the bifurcation. One stone was removed and no stones were left. The extrahepatic ducts were swept repeatedly until no further stones, debris or sludge was seen. Excellent drainage of bile and contrast was noted both endoscopically and ftouroscopically. At this point the procedure was completed . Add'llmages: o Impression: - The entire main bile duct was moderately dilated. - Choledocholithiasis was found . Complete removal was accomplished by biliary sphincterotomy and balloon sweep. Recommendation: - Avoid aspirin and nonsteroidal anti-inflammatory and anticoagulant medicines for 7 days. - Clear liquid diet today and advance as tolerated tomorrow. - Continue with antibiotic, may consider to switch to oral antibiotic (ciprofloxacin 500 mg bid) .. . ~ .