CPY Document - Unified Court System
advertisement
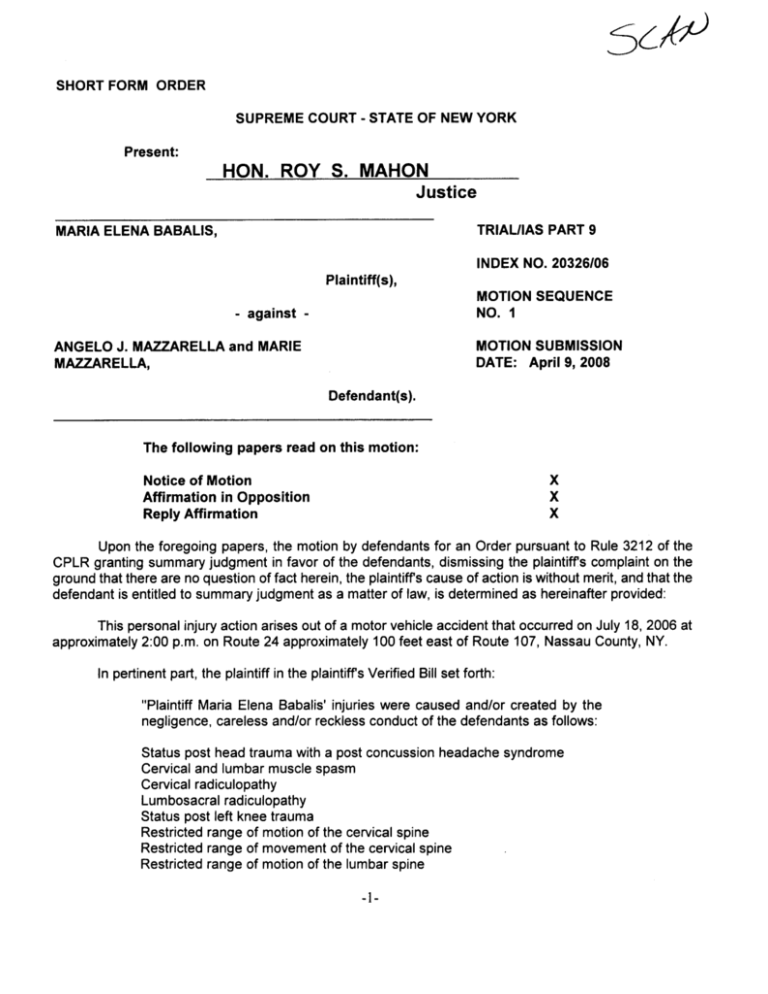
SclP SHORT FORM ORDER SUPREME COURT - STATE OF NEW YORK Present: HON. ROY S. MAHON Justice TRIAUIAS PART 9 MARIA ELENA BABALlS, INDEX NO. 20326/06 Plaintiff(s), MOTION SEQUENCE NO. - against ANGELO J. MAZRELLA and MARIE MOTION SUBMISSION MAZRELLA, DATE: April 9, 2008 Defendant(s). The following papers read on this motion: Notice of Motion Affirmation in Opposition Reply Affirmation Upon the foregoing papers , the motion by defendants for an Order pursuant to Rule 3212 of the CPLR granting summary judgment in favor of the defendants , dismissing the plaintiffs complaint on the ground that there are no question of fact herein , the plaintiffs cause of action is without merit , and that the defendant is entitled to summary judgment as a matter of law , is determined as hereinafter provided: This personal injury action arises out of a motor vehicle accident that occurred on July 18 , 2006 at approximately 2:00 p. m. on Route 24 approximately 100 feet east of Route 107 , Nassau County, NY. In pertinent part , the plaintiff in the plaintiffs Verified Bill set forth: Plaintiff Maria Elena Babalis ' injuries were caused and/or created by the negligence , careless and/or reckless conduct of the defendants as follows: Status post head trauma with a post concussion headache syndrome Cervical and lumbar muscle spasm Cervical radiculopathy Lumbosacral radiculopathy Status post left knee trauma Restricted range of motion of the cervical spine Restricted range of movement of the cervical spine Restricted range of motion of the lumbar spine Restricted range of movement of the lumbar spine The above injuries are accompanied by severe pain , tenderness , swelling, stiffness , discomfort , distress , weakness , stress , restriction of motion, degeneration of the underlying soft tissue , blood vessels , bones , nerves tendons , ligaments and musculature and all of the natural consequences flowing therefrom. Plaintiff has further suffered and continues to suffer severe pain and difficulty with prolonged sitting, standing, walking, bending, climbing stairs, lifting or carrying heavy objects , performing strenuous activities and finding a comfortable position sleeping. disruption and diffic81ty with daily activities , way of life and enjoyment of life including Plaintiff has and will continue to experience impairment , significant impairment of numerous daily activities that plaintiff had previously taken for granted. Any and all of the above injuries wil result in traumatic arthritis and/or onset of arthritis , osteoarthritic involvement , osteoporosis and/or necrosis at an earlier age , at an accelerated rate and with greater severity than would have otherwise occurred. All of the above injuries are permanent in nature. The defendants, amongst other things, in support of the defendants ' application submit the June 27 2007 deposition transcript of the plaintiff; an affirmed letter report dated August 24 2007 of Michael J. Katz , an orthopedist of an August 24 2007 orthopedic evaluation of the plaintiff; an August 30, 2007 affirmed letter report of Island Neurological Associates , PC by John Kelemen , MD , a neurologist of an August 30 2007 neurological examination of the plaintiff and an August 20 , 2007 affirmed letter report of Allan Rothpearl , MD, a radiologist of a review of a December 12 , 2006 MRI of the plaintiffs cervical spine. The rule in motions for summary judgment has been succinctly re-stated by the Appellate Division Second Dept. , in Stewart Title Insurance Company, Inc. v. Equitable Land Services, Inc., 207 AD2d 880, 616 NYS2d 650 , 651 (Second Dept., 1994): It is well established that a party moving for summary judgment must make a prima facie showing of entitlement as a matter of law , offering sufficient material issues of fact 853 487 N. (Winegrad v. New York Univ. Med. Center 49 N. 2d 557 , 562 Zuckerman v. City of New York 316, 476 N. E.2d 642; 2d 595 , 404 N. E.2d 718). Of course , summary judgment is a 427 N. drastic remedy and should not be granted where there is any doubt as to the evidence to demonstrate the absence of any 64 N. existence of a triable issue 2d 851 (State Bank of Albany v. McAuliffe 97 A.D. 2d 607 2d 944), but once a prima facie showing has been made , the burden shifts to the party opposing the motion for summary judgment to 467 N. produce evidentiary proof in admissible form sufficient to establish material (Alvarez v. Prospect Hosp. , 68 issues of fact which require a trial of the action Zuckerman v. City of 2d 923, 501 N. E.2d 572; 2d 320 , 324 , 508 N. New York, supra 49 N. 2d at 562 427 N. 2d 595 , 404 N. 2d 718). It is noted that the question of whether the plaintiff has made a prima facie showing of a serious injury should be decided by the Court in the first instance as a matter of law (see Licaro v. Ellot, 57 NY2d 230, 455 NYS2d 570, 441 NE2d 1088; Palmerv. Amaker, 141 AD2d 622 , 529 NYS2d 536, Second Dept., 1988; Tipping- Cestari v. Kilhenny, 174 AD2d 663 , 571 NS2d 525, Second Dept. , 1991). In making such a determination , summary judgment is an appropriate vehicle for determining whether a plaintiff can establish prima facie a serious injury within the meaning of Insurance Law Section 5102(d) (see , Zoldas v. Louise Cab Corp., 108 AD2d 378, 381 , 489 NYS2d 468, First Dept., 1985; Wright v. Melendez , 140 AD2d 337, 528 NYS2d 84 , Second Dept., 1988). Serious injury is defined , in Section 5102(d) of the Insurance Law , wherein it is stated as follows: (d) ' Serious injury' means a personal injury which results in death; loss of a fetus; dismemberment; significant disfigurement; a fracture; permanent loss of use of a body organ , ember , function or system; permanent consequential limitation of use of a body organ or member; significant limitation of use of a body function or system; or a medically determined injury or impairment of a non- permanent nature which prevents the injured person from performing substantially all of the material acts which constitute such person s usual and customary daily activities for not less than ninety days during the one hundred eighty days immediately following the occurrence of the injury or impairment." In pertinent part , the report of Dr. Katz sets forth: Examination of the Cervical Spine: There is no tenderness about the cervical spine and there is no paravertebral muscle spasm. Flexion is present to 50 (normal 500 ) and extension is present to 60 (normal 60 ). Lateral flexion is present with right-sided lateral flexion to 45 (normal 450 ) and left-sided lateral flexion to 45 (normal 45 ). Right-sided rotation is present to 80 (normal 800 and left-sided rotation is present to 80 (normal 80 ). Motor strength is present in the C5T1 innervated segments. Sensation is intact in the C5innervated dermatomes. Reflex testing reveals the biceps , triceps , and brachioradialis reflexes to be 2+ and symmetric. Adson s test is negative. Examination of the Lumbosacral Spine: The gait was normal without antalgic or Trendelenburg component. No paravertebral muscle spasm was present. Active range of motion revealed forward flexion to 90 0 (normal 90 ), full extension to 30 (normal 30 ), and full lateral and side bending to 30 (normal ). Straight leg raising test was negative. Sensory examination revealed full sensation to light touch in the L3- S1 dermatomes. Reflexes of the quadriceps , tibialis posterior and Achilles tendon were 2+ and symmetric bilateral. Babinski was negative and there was no demonstrable clonus. Patrick was negative. Examination of the Left Knee: There is normal valgus attitude about the knee in the standing position. There is no swelling about the knee. Range of motion is normal. There is no effusion within the knee. The range of motion is 0- 135 (normal 1350 ) in the flexion/extension arc. The patellar reflex is 2+ There is no medial or lateral joint line tenderness. Lachman s test is negative for anterior/posterior instability. The patellar apprehension test is negative. The motor strength of the Quadriceps is 5/5. The knee is stable to varus and valgus stress. There is a negative pivot shift test. The posterior drawer sign is negative. The posterior sag sign is negative. There is no demonstrable crepitus. The prepatellar bursa is supple and lacks swelling, erythema, or induration. I did the following measurements of the upper extremities: Circumferential measurements about the right upper extremity are 9 inches at the midportion and 9 inches on the left at the midportion. Using a power pinch meter , there was 4 kg of force on the right and 4kg of force on the left. Using a Jaymar dynamometer , there was 14 kg of force on the right and 14 kg of force on the left. Diaanosis: Cervical strain resolved. Lumbosacral strain resolved. Left knee contusion now resolved. Comment: This individual is a 54- year-old female who alleged an injury to the neck , back and left knee. Currently, she shows no signs or symptoms of permanence relative to the musculoskeletal system. She is currently not disabled. She is capable of gainful employment in a demanding capacity as a manager. She is capable of her activities of daily living. Dr. Kelemen states in said physician s report of neurological examination: PHYSICAL EXAMINATION: On examination , the claimant was an alert , cooperative woman in no obvious distress. She is 5' 1" tall and weighs 105 pounds, and she has dark- brown eyes and brown hair. The claimant was able to bend and move without difficulty to remove her footwear and to get up onto and off the examining table. Examination of the head revealed no tenderness or bruits. There was no palpable paracervical , lumbar or occipital tenderness, and there was no spasm. Straight leg raise testing was negative bilaterally. There was no sciatic notch tenderness. MENTAL STATUS: Mental status examination revealed the following: The claimant was alert and oriented x3. Recent memory was intact. Language function was intact without evidence of aphasia. Speech was of normal quality. Higher integrative functions were normal. CRANIAL NERVE EXAMINATION: Olfaction was intact bilaterally. Visual fields were full to confrontation. Funduscopic examination was unremarkable. Pupils were equal , round and reactive to light and accommodation. There was no ptosis and the extraocular muscles were intact. Corneal reflexes , facial sensation and the muscles of mastication were intact. There was not facial paresis. Hearing was grossly normal. There was no nystagmus. Gag reflexes and palatal movements were intact bilaterally. The sternomastoid muscles were intact bilaterally. Tongue movements were full , and there was no atrophy of the tongue. MOTOR EXAMINATION: Motor examination revealed intact strength , tone and mass. Finger-to-nose and heel- to- knee- to-shin testing was intact. Gait , including heel , toe and tandem walking, was normal. Roomberg test was negative. There were no abnormal involuntary movements. Deep tendon reflexes were 2+ in the biceps , brachioradialis , triceps , knees and ankles , with flexor plantar responses. SENSORY EXAMINATION: Sensory examination was intact to primary and cortical modalities. IMPRESSION: Status post cervical and lumbar strain. I find no evidence of a neurological abnormality or disability , from a neurological perspective. If the history is accurate , this claimant's complaints can be related to the event of 7/18/06. Dr. Rothpearl sets forth in his review of his examination of the December 12 , 2006 MRI of the plaintiffs Cervical Spine: MRI OF THE CERVICAL SPINE: Examination is dated 12/12/2006. Multiplanar T1 and T2 weighted acquisitions were obtained. Film quality is adequate. There is degeneration at the C2- , C3- , C4- , C5- , C6- C7 and C7 - levels , characterized by desiccation of disc material. There is a disc bulge at , C4- , C5- C6levels where disc material approximates the ventral thecal sac. The cervical cord and craniocervical junction are unremarkable in appearance. The visualized osseous structures demonstrate normal marrow signal characteristics. There is no evidence of central canal stenosis bony lateral recess stenosis or neural foraminal stenosis. the C3- IMPRESSION : Multilevel disc deneration. Minimal degenerative bulges at C3- , C4- C5 and C5- C6. No evidence of disc herniation. This is not consistent with the original report which notes disc herniations at C3- , C4C5 and C5- C6. The original report does not specifically note the presence or degree of multilevel disc degeneration. COMMENTS ON CAUSAL RELATIONSHIP The presence of disc degeneration indicates a chronic process of longstanding duration. Within a reasonable degree of medical certainty, it is unrelated etiologically to the accident of 07/18/2006. Disc bulges of this nature are often seen in association with disc degeneration of the type depicted on this examination and , consequently, are most likely related to this process. A review of the plaintiffs deposition transcript sets forth subjective complaints of pain which are insufficient to establish a serious injury pursuant to the Insurance Law (see , Scheer v Koubek , 70 NY2d 678 , 518 NYS2d 788 , 512 NE2d 309). The Court finds that the defendants have submitted evidence in admissible form to make a " prima facie showing of entitlement to judgment as a matter of law" (Winegrad v. New York University Medical Center , 64 NY2d 851 , 853; Pagano v. Kingsbury, supra at 694) and is sufficient to establish that the plaintiff did not sustain a serious injury. Accordingly, the burden has shifted to the plaintiff to establish such an injury and a triable issue of fact (see Gaddy v. Eyler, 79 NY2d 955, 582 NYS2d 990, 591 NE2d 1176; Jean- Meku v. Berbec, 215 AD2d 440, 626 NYS2d 274, Second Dept., 1995; Horan v. Mirando, 221 AD2d 506, 633 NYS2d 402 , Second Dept., 1995). In opposition to the defendants ' application the plaintiff submits , amongst other things , an affidavit of the plaintiff an affidavit of Suzanne J. Howard , DC, a treating chiropractor of the plaintiff and an affirmation of Richard J. Rizzuti , MD , a radiologist who performed an MRI examination of the plaintiff' cervical spine on December 12 , 2006. Amongst other things , Dr. Howard states in the affidavit as to treatment of the plaintiff: 2. On July 20 , 2006 Maria Sabalis presented herself to my office for treatment regarding a motor vehicle accident on July 18 , 2006. At the initial visit she presented with complaints of severe neck pain radiating to left trap with occasional left arm shooting pain , headaches and constant low back pain. The patient also complained of left knee pain and left leg weakness with intermittent numbness and tingling of her face and the middle finger on her left hand. The patient also informed me that she was having difficulty turning and moving her neck as well as she was experiencing spasms in her neck and lower back. The patient further related that after the accident she was taken to Mid Island Hospital where she was treated and released. 3. Examination of the cervical spine revealed tenderness upon palpation of C5- T1 spinous processes. Further , palpation of the cervical spine musculature revealed cervical muscle spasm bilaterally left more than right. The following tests were performed and the results were as follows: Foraminal compression test was positive; Extension Compression test was positive; Rotation- Extension Compression test was positive; Jackson Compression test was positive; Maximum Cervical Compression test was positive; and Shoulder Depression test was positive. 4. A cervical spine range of motion study was performed and the results were as follows: flexion was limited to 40 degrees with the norm being 60 degrees with pain; extension was limited to 10 degrees with the norm being 60 degrees with pain; left and right rotation were limited to 60 degrees with the norm being 80 degrees with pain; and left and right lateral flexion were limited to 20 degrees with the norm being 40 degrees with pain. 5. Examination of the thoracic spine revealed tenderness upon palpation of T1-T2 and upon palpation there was tenderness and muscle spasm of the paravertebral musculature on the left. the lumbar spine revealed tenderness upon palpation of L4- S2 spinous processes as well as bilateral lumbar muscle spasm. The following tests were performed and the results were as follows: Bechterew Sitting test was positive bilateral; Kemps test was positive bilaterally; Milgram s test was positive; Laseque s test was positive bilaterally; Braggard' test was positive bilaterally; Ely s test was positive bilaterally; and Yeoman test was positive on the right. 6. Examination of 7. A lumbar spine range of motion study was performed and the results were as follows: flexion was limited to 70 degrees with the norm being 90 degrees with pain; extension was limited to 10 degrees with the norm being 30 degrees with pain; left and right rotation were limited to 20 degrees with the norm being 30 degrees with pain; and left and right lateral flexion were limited to 10 degrees with the norm being 20 degrees with pain. 8. My initial diagnosis of the patient was as follows: cervical subluxation multiple levels; cervical radiculitis; cervical myfibrositis/myofascitis; cervical hypolordosis; cervical hyperflexion/hyperextension; cephalgia; lumbar subluxation; lumbar muscle spasm; and sacroiliac joint dysfunction. 9. Thereafter the patient was placed on a course of chiropractic therapy consisting of chiropractic manipulations , ultrasound and electric muscle stimulation at a rate of three times per week. The patient utilized the services of my office on a regular basis from July 20 , 2008 (sic) through March 20, 2007 when she stopped treating as her no fault benefits had expired and she had reached maximum improvement from chiropractic care as her condition was permanent. 10. It was my expert chiropractic opinion that the results were as follows: Sitting test was positive bilateral; Kemps test was positive Bechterew bilaterally; Milgram s test was positive; Lasegue s test was positive bilaterally; Braggard' s test was positive bilaterally; Ely s test was positive bilaterally; and Yeoman s test was positive on the right. 7. A lumbar spine range of motion study was performed and the results were as follows: flexion was limited to 70 degrees with the norm being 90 degrees with pain; extension was limited to 10 degrees with the norm being 30 degrees with pain; left and right rotation were limited to 20 degrees with the norm being 30 degrees with pain; and left and right lateral flexion were limited to 10 degrees with the norm being 20 degrees with pain. 8. My initial diagnosis of the patient was as follows: cervical subluxation multiple levels; cervical radiculitis; cervical myofibrositis.lmyofascitis; cervical hypolordosis; cervical hyperflexion/hyperextension; cephalgia; lumbar subluxation; lumbar muscle spasm , and sacroiliac joint dysfunctioin. 10. It was my expert chiropractic opinion that the injuries sustained by the plaintiff were causally related to the motor vehicle accident of July 18 , 2006 and that said injuries were consistent with the clinical presentation in my office. It was my expert chiropractic opinion that the limitations in the ranges of motion in the lumbar spine and cervical spine were permanent and significant and would inhibit the patient's ability to carry out her normal activities of daily living such as sitting, standing, bending, walking and lifting. 14. Ms. Babalis returned to my office for a re-evaluation on February 5 2008 and presented with the following complaints: neck pain , headaches and low back pain. The patient further related that she has been unable to perform normal daily living activities without pain. 15. Examination of the cervical spine revealed tenderness upon palpation of C5- T1 spinous processes. Further , palpation of the cervical spine musculature revealed cervical muscle spasm bilaterally left more than right. The following tests were performed and the results were as follows: Foraminal Compression test was positive; Extension Compression test was positive; Rotation- Extension Compression test was positive; Jackson Compression test was positive; Maximum Cervical Compression test was positive; and Shoulder Depression test was positive. 16. A cervical spine range of motion study was performed and the results were as follows: flexion was limited to 50 degrees with the norm being 60 degrees with pain; extension was limited to 30 degrees with the norm being 60 degrees with pain; left and right rotation were limited to 70 degrees with the norm being 80 degrees; left lateral flexion was limited to 35 degrees with the norm being 40 degrees; and right lateral flexion was limited to 30 degrees with the norm being 40 degrees with pain. 17. Examination of the thoracic spine revealed tenderness upon palpation of T1- T2 and upon palpation there was tenderness and muscle spasm of the paravertebral musculature on the left. 18. Examination of the lumbar spine revealed tenderness upon palpation of L40S1 spinous processes as well as bilateral lumbar muscle spasm. The following tests were performed and the results were as follows: Milgram s test was positive; Ely s test was positive on the right; and Yeoman s test was positive on the right. 19. A lumbar spine range of motion study was performed and the results were as follows: flexion was limited to 80 degrees with the norm being 90 degrees; and extension was limited to 20 degrees with the norm being 30 degrees with pain. 20. My current diagnosis of the patient is as follows: cervical subluxation multiple levels; cervical radiculitis; cervical myofibrositis/myofascitis; cervical hypolordosis; cervical hyperflexion/hyperextension; cephalgia; lumbar subluxation; lumbar muscle spasm; sacroiliac joint dysfunction; and subligamentous posterior disc herniations at C304 , C4- 5 and at C5impinging on the anterior aspect of the spinal canal. 21. It is my expert chiropractic opinion that the injuries as diagnosed are causally related to the motor vehicle accident on July 18 , 2006. It is expert chiropractic opinion that as the patient is stil exhibiting limitations of motion in the lumbar and cervical spine said limitations and injuries can only be considered permanent and significant at those limitations and the injuries as diagnosed wil continue to inhibit the patient' s ability to carry out her normal activities of daily living consistent with sitting, standing, bending, walking, lifting, recreational activities and household duties. As such , it is my expert chiropractic opinion that the injuries as diagnosed are permanent in nature. Dr. Rizzute sets forth in said physician s affirmation as to the December 12 , 2006 MIR of the plaintiffs cervical spine: 2. On December 12 , 2006 Ms. Maria Elena Babalis presented herself at my office for an MRI examination of the cervical spine. 3. The examination demonstrates subligametnouos posterior disc herniations at C4- 3, C4- 5 and at C5- 6 which impinge on the anterior aspect of the spinal canal. The remaining discs are unremarkable. No abnormality is demonstrated in the lower spinal cord. There is no abnormality of alignment. No acute bony abnormality is demonstrated. There is no evidence of spinal stenosis. 4. My impression of the cervical spine was subligamentous posterior disc herniations at C3- , C4- 5 and at C5- 6 impinging on the anterior aspect of the spinal canal. .".. ............. 5. It is my expert medical opinion that the disc pathology is trauma related and did not pre-exist the accident of July 18, 2006. Based upon the foregoing, there is an issue of fact as to whether the plaintiff suffered a serious injury pursuant to 95102 of the Insurance Law in the accident in issue of July 18 , 2006. As such. the defendants application for an Order pursuant to Rule 3212 of the CPLR granting summary judgment in favor of the defendants, dismissing the plaintiffs complaint on the ground that there are no question of fact herein , the plaintiffs cause of action is without merit , and that the defendant is entitled to summary judgment as a matter of law , is denied. SO ORDERED. DATED: t,fi 4.6. jSC." ENTERED JUN 2 0 2008 6-. .'iAMAU COUNTY -vNr 10- ClEfK' S OFFiCe