Cell Pathology Handout
advertisement
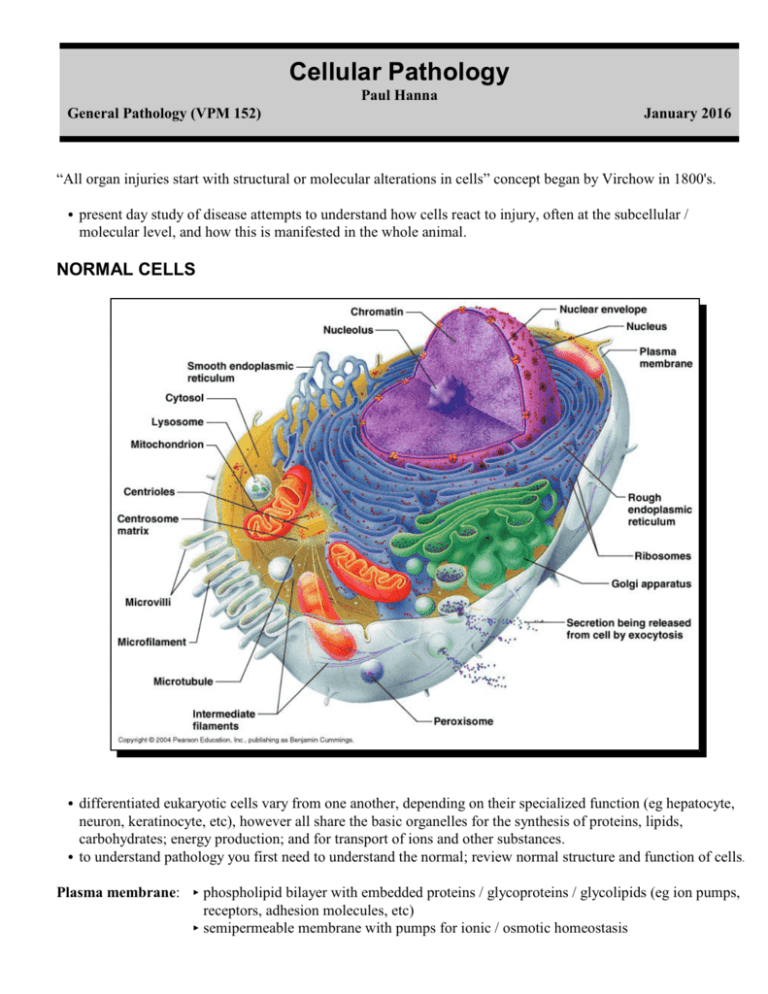
Cellular Pathology Paul Hanna General Pathology (VPM 152) January 2016 “All organ injuries start with structural or molecular alterations in cells” concept began by Virchow in 1800's. C present day study of disease attempts to understand how cells react to injury, often at the subcellular / molecular level, and how this is manifested in the whole animal. NORMAL CELLS C differentiated eukaryotic cells vary from one another, depending on their specialized function (eg hepatocyte, neuron, keratinocyte, etc), however all share the basic organelles for the synthesis of proteins, lipids, carbohydrates; energy production; and for transport of ions and other substances. C to understand pathology you first need to understand the normal; review normal structure and function of cells. Plasma membrane: < phospholipid bilayer with embedded proteins / glycoproteins / glycolipids (eg ion pumps, receptors, adhesion molecules, etc) < semipermeable membrane with pumps for ionic / osmotic homeostasis Gen Path (VPM 152) Cell Pathology Nucleus: < nuclear envelope / nuclear pores < chromatin (euchromatin vs heterochromatin) < nucleolus (synthesis of ribosomal RNA) Mitochondria: < inner & outer membranes, cristae < intermembranous and inner matrix compartments < oxidative phosphorylation (main source of ATP) 2 Endoplasmic reticulum (ER), Ribosomes & Golgi Apparatus: < RER & Golgi - synthesis and packaging of proteins for export, membranes, lysosomes < SER - lipid biosynthesis (eg membranes, steroids) - detoxification of harmful compounds (via P450’s) - sequestration of Ca2+ ions Chaperones & Proteasomes: < chaperones assist proper folding of proteins and transport across organelle membranes. < proteasomes degrade both excess proteins and incorrectly folded (misfolded) proteins. Lysosomes: < enzymatic (acid hydrolases) digestion of materials in the cell < primary vs secondary lysosomes; residual bodies < autophagy vs heterophagy / endocytosis < phagocytosis / phagosome; pinocytosis / pinocytotic vesicle; receptor-mediated endocytosis Cytoskeleton: < structure and movement of cells / organelles / granules / surface molecules / phagocytosis < Microfilaments: actin in various forms ! cell shape & movement < Microtubules: polymers of tubulin ! organelle movement / flagella / cilia / mitotic spindle < Intermediate filaments: cytokeratins, vimentin, desmin, GFAP, neurofilament proteins Peroxisomes: < enzymes (eg catalase, oxidases) ! metabolism of hydrogen peroxide & fatty acids. CELL ADAPTATION, CELL INJURY and CELL DEATH I. DEFINITIONS AND TERMINOLOGY 1) Homeostasis C cells are able to maintain normal structure and function (eg ion balance, pH, energy metabolism) in response to normal physiologic demands. 2) Cellular Adaptation C as cells encounter some stresses (eg excessive physiologic demand or some pathologic stimuli) they may make functional or structural adaptations to maintain viability / homeostasis. C cells may respond to these stimuli by either increasing or decreasing their content of specific organelles. C adaptive processes: atrophy, hypertrophy, hyperplasia and metaplasia are forms of adaptation. 3) Cell Injury C if the limits of adaptive response are exceeded, or in certain instances when adaptation is not possible (eg with severe injurious stimulus), a sequence of events called cell injury occurs. Gen Path (VPM 152) Cell Pathology 3 a) Reversible Cell Injury < removal of stress / injurious stimulus results in complete restoration of structural and functional integrity. b) Irreversible Cell Injury / Cell Death < if stimulus persists (or severe enough from the start) the cell will suffer irreversible cell injury and death. < cell death is one of the most crucial events in pathology and can affect any type of cell. < two principle morphologic patterns that are indicative of cell death: Î Necrosis: type of cell death characterized by severe membrane injury and enzymatic degradation; always a pathologic process. Ï Apoptosis: regulated form of cell death; can be physiologic or pathologic process. II. CELLULAR ADAPTATIONS OF GROWTH AND DIFFERENTATION C major adaptive responses: atrophy, hypertrophy, *hyperplasia, *aplasia,*hypoplasia,*metaplasia,*dysplasia. (*to be discussed in more detail in neoplasia section) 1) Atrophy C definition: decrease in the amount of a tissue or organ after normal growth has been attained. C adaptive response whereby a tissue or organ undergoes a reduction in mass, due to a decrease in either the number of cells and/or the size of the cells (results in decrease in size of the organ / structure). a) Etiology < decreased workload (disuse atrophy), loss of innervation (denervation atrophy), loss of hormonal (trophic) stimulation, reduced blood supply / hypoxia, inadequate nutrition, compression, persistent cell injury, aging (senile atrophy). < atrophic cells are not dead or necessarily badly injured but they have a reduced functional capacity (but may progress to cell injury / death if stimulus persists or worsens). < retain ability to control their internal environment and produce enough energy to survive. < given "enough time" and removing the reason for cellular atrophy, the cells can return to 'normal'. b) Mechanisms and Biochemistry < decreased amount of substance produced within cell, ie catabolic processes exceed anabolic processes. eg: with muscle atrophy (due to denervation atrophy or disuse atrophy) : 9 myofilaments, 9 mitochondria, 9 endoplasmic reticulum, 9 metabolic activity. < organelles removed by autophagocytosis and decreased proteins by ubiquitin-proteosome pathway. < cell shrinks in volume and shuts downs its differentiated functions ÿ decreased it energy requirements. c) Gross Appearance < tissue/organ is decreased in size. d) Microscopic Appearance < cells are smaller than normal C eg’s Î endocrine gland, following decreased trophic stimulation (eg physiologic: uterus / breast following pregnancy / lactation or pathologic: eg pituitary destruction), medical supplementation of the corresponding hormone (eg corticosteroid) or overproduction of hormone by the contralateral gland. Ï starvation, results in atrophy of various tissues (eg muscle, liver) & loss (serous atrophy) of fat. - there is a definite sequence in which body proteins are broken down during starvation in order to preserve the blood glucose level (via glucogenic amino acids): first, digestive enzymes of the gastrointestinal tract and pancreas and various hepatic enzymes that normally process incoming nutrients from the intestine; later, muscle proteins. - there is a sequential use (& loss) of muscle mass as an endogenous sources of protein and energy; postural muscles (eg supraspinatus) are preserved at the expense of other muscles (eg longissimus dorsi) that are used for locomotion. - there is also a sequential mobilization of fat depots; in most terrestrial mammals, subcutaneous fat is used first, visceral fat is used next and bone marrow fat is used last. Gen Path (VPM 152) Cell Pathology 4 2) Hypertrophy C definition: organs are increased in size due to an increase in cell size without cellular proliferation. C in organs / tissues which have minimal proliferative capacity (cardiac and skeletal muscle) see only hypertrophy, whereas in tissues / organs with cells capable of division see both hypertrophy and hyperplasia. a) Etiology < a response to increased work load: Î physiologic: eg with exercise see increase in muscle cell size (grossly muscles increase in size). Ï pathologic: eg heart failure ÿ see enlargement of myocardial fibers (grossly heart increases in size). < a response to trophic signals: Î physiologic hypertrophy (& hyperplasia), eg uterus and mammary gland in pregnancy / lactation. Ï pathological hypertrophy, eg myocardial hypertrophy in hyperthyroid cats. < response to certain drugs or toxins: increased SER in liver (organelle hypertrophy) with phenobarbital. b) Mechanisms and Biochemistry < anabolic processes exceed catabolic ones (ie, increased synthesis of cellular constituents). < increase in organelles / total cellular proteins: 8mitochondria, 8endoplasmic reticulum, 8myofibrils. < may not always be advantageous (eg myocardial hypertrophy can exceed the limits of vascular supply). c) Gross Appearance: tissue / organ increased in size / weight. d) Microscopic Appearance < cellular enlargement due to a proportional increase in the number and size of organelles. < must be distinguished from cellular swelling, which is due to an increased intake of fluid by the cell 3) *Hyperplasia C increase in organ size or tissue mass caused by an increase in the number of constituent cells. C hypertrophy and hyperplasia are not mutually exclusive and are often seen together in structures which can undergo division (esp reproductive and endocrine organs). 4) *Hypoplasia C incomplete development or underdevelopment of an organ / tissue (less severe in degree than aplasia). 5) *Aplasia C lack of development of an organ or tissue (may have a rudimentary organ). C can also refer to lack of production of cells from an organ or tissue (eg aplastic anemia). 6) *Metaplasia C reversible change in which one differentiated cell type is replaced by another differentiated cell type. C eg, squamous metaplasia of trachea in chronic smokers; ciliated columnar to stratified squamous epithelium. 7) *Dysplasia C in the context of organ development, it refers to abnormal organization of cells (‘abnormal growth’), eg retinal dysplasia, hip dysplasia, renal dysplasia, etc. C in the context of neoplasia, it refers to disordered growth of cells (loss of uniformity and architectural orientation), eg epithelial cell dysplasia in squamous cell carcinoma. [*to be discussed in more detail in Disturbances of Growth / Neoplasia section of course] Gen Path (VPM 152) Cell Pathology 5 III. CAUSES OF CELL INJURY 1) Hypoxia (Oxygen Deficiency) C one of the most important and common causes of cell injury and cell death. C hypoxia causes impairment of oxidative respiration, ie it interferes with energy production. C occurs with: a) Deficient blood supply < ischemia = deficiency of blood supply from impeded arterial flow or reduced venous drainage = hypoxia + 9 delivery of nutrients and 9 removal of metabolites. < cells may adapt to mild ischemia (eg muscle atrophy) or die with severe ischemia. < infarction = localized area of ischemic necrosis. b) Reduced oxygen-carrying capacity of the blood < due to anemia = reduction in numbers or volume of erythrocytes or quantity of hemoglobin (Hb). < due to Hb dysfunction, eg methaemoglobinemia - nitrate / nitrite poisoning, carboxyhaemoglobinemia - carbon monoxide poisoning. c) Interference with respiratory chain / oxidative phosphorylation < eg, cyanide poisoning inactivates cytochrome oxidase in mitochondria ÿ blocks oxidative phosphorylation. 2) Physical agents C severity of a physical injury may be increased by tissue hypoxia due to associated local vascular injury. a) Direct mechanical trauma - lacerations or crush injuries. b) Temperature extremes - heat (thermal burn), cold (frostbite). c) Radiation - radioactive isotope emissions or electromagnetic radiation (eg UV light, x-rays). d) Electric Shock e) Sudden changes in atmospheric pressure 3) Chemicals, Drugs & Toxins a) Inorganic poisons - eg lead, copper, arsenic, selenium, mercury, etc. b) Organic poisons - eg nitrate/nitrite, oxalate, hydrocyanic acid, etc. c) Manufactured chemicals - eg drugs (overdose / idiosyncratic), pesticides, herbicides, rodenticides, etc. d) Physiologic compounds - eg salt, glucose, oxygen, etc. e) Plant toxins - eg ragwort, sweet clover, braken fern, etc. f) Animal toxins - eg snake or spider venom, tick toxin, etc. g) Bacterial toxins / Mycotoxins - eg botulinum toxin, aflatoxin, ergot, etc. 4) Infectious agents (such important causes of disease, you have individual courses to study them in detail!) a) Viruses b) Bacteria / rickettsiae / chlamydia c) Fungi d) Protozoa e) Metazoan parasites 5) Immunologic Reactions a) Immune response - eg cells damaged as “innocent bystanders” in immune / inflammatory response. b) Hypersensitivity (allergic) reactions - eg anaphylactic reaction to a foreign protein or drug. c) Autoimmune diseases - reactions to self-antigens. Gen Path (VPM 152) Cell Pathology 6 6) Genetic abnormalities a) Cytogenetic disorders / chromosomal aberrations - one cause of congenital anomalies. b) Mendelian disorders (mutant genes) < enzyme defects, eg lysosomal storage disease. < structural / transport protein defects - eg collagen dysplasia, cystic fibrosis, sickle cell anemia, etc. c) Multifactorial inheritance - combined effects of environmental factors and 2 or more mutated genes (eg neoplasia, hypertension, coronary artery disease, etc). 7) Nutritional Imbalances a) Deficiencies - deficiencies of protein-calories (starvation), vitamins (A to E), minerals (eg copper). b) Overnutrition - eg excess lipids / calories ÿ obesity, diabetes, atherosclerosis, etc. 8) Workload Imbalances a) Overworked cells - if stimulus prolonged and/or exceeds ability to adapt. b) Underworked cells - prolonged lack of stimulation (eg disuse, denervation, lack of trophic hormones) will lead to atrophy and eventually the loss of cells. 9) Cell Aging C the cumulative effects of a life time of cell damage (chemical, infectious, nutrition, etc) leads to a diminished capacity of aged cells / tissues to maintain homeostasis and adapt to harmful stimuli. Mnemonic acronym for agents of disease = “double MINT” Malformation (genetics, teratogens, etc) Miscellaneous (metabolic, aging, hypoxia, etc) Infectious (viruses, bacteria, fungi, etc) Immune (immune mediated, hypersensitivity, autoimmune, etc) Nutritional (protein-caloric intake, vitamins, minerals, etc) Neoplastic (genetic, viral, chemical, radiation, etc) Trauma (mechanical, temperature, radiation, etc) Toxicity (inorangic, chemicals / drugs, plant toxins, etc) Gen Path (VPM 152) 7 Cell Pathology IV. MECHANISMS OF CELL INJURY 1) General Considerations a) the cellular response to injurious stimuli is dependant on the type of injury, its duration and its severity. < eg, low doses of toxins or brief durations of ischemia may lead to reversible cell injury, whereas larger toxin doses or longer ischemic intervals may result in irreversible injury / cell death. b) consequences of an injurious stimulus are dependent on the type of cell injured and its current status, ie nutritional, hormonal, metabolic, oxygen requirement, etc. Tissue sensitivity to hypoxia - dependant upon energy dem ands of the cell and/or its ability to utilize anaerobic glycolysis as a source of energy SUSCEPTIBILITY CELL TYPE TIM E (to irreversible cell injury) HIGH Neurons ~ 3 to 5 m inutes INTERMEDIATE Cardiac m yocytes Hepatocytes Renal epithelium ~ 30 m inutes to 1 hour " " LOW Fibroblasts Keratinocytes Skeletal m yocytes m any hours " " c) 4 intracellular systems are particularly vulnerable to injury. Î cell membranes - especially ionic / osmotic homeostasis. Ï mitochondria - oxidative phosphorylation / ATP production. Ð protein synthesis and packaging - structural and functional proteins. Ñ genetic apparatus - DNA / RNA. d) interrelationship of structural and biochemical elements means that damage at one focus leads to wideranging secondary effects. eg, impairment of aerobic respiration (eg 9O2 or mitochondrial damage) ÿ disruption of the energydependent membrane sodium pump ÿ ionic and fluid imbalance ÿ cell swelling. 2) Biochemical Mechanisms C several molecular / biochemical sites are commonly damaged by a variety of inciting causes. a) ATP depletion < ATP depletion and 9ATP synthesis are common consequences of both ischemic and toxic injury. < 8 AMP activates phosphofructokinase & phosphorylase ÿ 8 anaerobic glycolysis ÿ depletion of glycogen stores ÿ 8 lactic acid & [Pi] ÿ 9 intracellular pH ÿ impaired cell enzyme activity. < ATP required for membrane transport (Na+/K+ & Ca2+ pumps) / osmotic balance, protein synthesis, protein stability (proper folding), lipogenesis, etc. < cells with greater glycolytic capacity (eg liver cells) have an advantage over cells which are more reliant on oxidative phosphorylation (eg neurons). Gen Path (VPM 152) Cell Pathology 8 b) Free radical induced injury (Oxidative Stress) < free radicals are chemical species with a single unpaired electron in outer orbit (donate or steal electrons, extremely unstable); readily react with organic or inorganic chemicals, avidly attack/degrade membranes, proteins & nuclei acids < free radical-induced injury, particularly that induced by activated oxygen species, is an important mechanism of cell damage in many disease processes (chemical, radiation, O2 toxicity, inflammation, reperfusion, etc). < cell injury occurs when the free radical generation overwhelms antioxidant defense mechanisms. Generation of free radicals Î Cellular metabolism - small amounts produced from cell redox reactions, eg normal oxidative phosphorylation (leakage from mitochondria), other intracellular oxidases (eg peroxisomes), PMN’s in inflammation, excess O2, altered metabolism in cell stress (eg reperfusion injury) Ï Enzymatic metabolism of exogenous chemicals - some intermediary metabolites of chemical / drugs are highly reactive free radicals. Ð Ionizing radiation - hydrolyzes water into hydroxyl (•OH) and hydrogen (H•) free radicals. Ñ Divalent metals - the transition metals (copper and iron), accept or donate free electrons during certain intracellular reactions, ie catalyze free radical formation. Important reactants Î superoxide anion (O2.-), hydroxyl radical (•OH), hydrogen peroxide (H2O2) and peroxynitrite (ONOO•). Ï H2O2 (not a free radical) is a frequent by-product of oxidative metabolism that can generate hydroxyl radicals from reactions with copper or ferrous ions (eg Fenton reation = Fe2+ + H2O2 ÿ •OH + OH- + Fe3+). Ð most intracellular stored iron is in the ferric (Fe3+) state and must be reduced to the ferrous (Fe2+) state to act in the Fenton reaction (often reduced by O2-. ); iron & O2.- required for maximal cell damage. Main sites of damage Î Damage of Membranes (lipid peroxidation) < free radicals (esp •OH) are highly reactive & unstable (don’t last long or travel far) ÿ “steal” single electrons from the hydrogen next to a double bond in unsaturated fatty acids in cell membranes ÿ form lipid peroxides (which themselves are reactive & unstable) ÿ autocatalytic chain reaction (selfpropagating) ÿ can cause rapid widespread membrane / organelle damage. Ï Damage of Proteins < free radicals cause fragmentation and cross-linkage between proteins ÿ damaged structural proteins / loss of enzymatic activity ÿ increased degradation by proteosomes. Ð Damage to DNA < free radicals damage nuclear & mitochondrial DNA, producing strand breaks & DNA-protein adducts (short-term ÿ apoptosis; long-term ÿ low level damage implicated in cell aging & neoplasia). Protective Mechanisms of the Cell Î Storage and transport proteins: < iron & copper can catalyze formation of reactive oxygen forms; they are minimized by being bound to storage and transport proteins (eg ceruloplasmin, transferrin, lactoferrin, apoferritin/ferritin) and kept in an oxidized state. Ï Antioxidants - either block the formation of free radicals or inactivate (scavenge) them: < Vitamins A&E (lipid soluble, found in cell membranes), Vitamin C (aqueous-phase antioxidant) and glutathione - in reduced form (GSH) reacts with H2O2 or •OH ÿ oxidised glutathione (GSSG) + H2O. Ð Enzymes which are involved in neutralizing free radicals: < Glutathione peroxidase - a selenium-containing enzyme which catalyzes GSH to GSSG. - this enzyme also catalyses the reduction of lipid peroxides by glutathione, preventing propagation of lipid peroxidation reactions. < Superoxide dismutase (SOD) - catalyze the conversion of O2.- to H2O2. < Catalase - breaks down H2O2 to O2 + H2O. Gen Path (VPM 152) Cell Pathology 9 c) Intracellular calcium and loss of calcium homeostasis < cytosolic free Ca2+ is at low concentration compared to extracellular Ca2+ (1:104) due to energy-dependant pumps and sequestration within mitochondria and ER. < membrane damage / ischemia or certain toxins cause 8 cytosolic [Ca2+] due to influx from ECF / ER / mitochondria. < 8 cytosolic [Ca2+] ÿ activation of numerous enzymes that have deleterious effects, ie ATPases (ATP depletion), phospholipases (membrane damage), proteases (breakdown of membrane & cytoskeletal proteins) and endonucleases (DNA / chromatin damage). d) Mitochondrial damage < all cells are depend on oxidative metabolism for long term survival, regardless of glycolytic ability. < irreparable damage to mitochondria, directly or indirectly, will ultimately kill cells. < directly by certain toxins (eg cyanide) or indirectly (8cytosolic Ca2+, free radicals, lipid peroxidation, etc). < indirect damage ÿ large channels in mitochondrial membrane (nonselective pore called mitochondrial permeability transition = MPT); if persists becomes irreversible and is a death blow to the cell, ie no oxidative phosphorylation and/or leakage of cytochrome c into cytosol (ie trigger for apoptosis). e) Defects in membrane permeability < membranes are integral to virtually all organelles, eg plasma membrane, lysosomes, mitochondria, ER, etc. - indirect damage by ATP depletion & Ca2+ activation of phospholipases / proteases / etc. - direct damage by free radicals, physical / chemical agents, bacterial toxins, viruses, lytic complement components, cytotoxic lymphocyte perforins, etc. < with lysosomal membrane damage see leakage of enzymes which will digest most cell components. Gen Path (VPM 152) Cell Pathology 10 V. ISCHEMIC AND HYPOXIC CELL INJURY C a common type of cell injury in clinical veterinary medicine. C hypoxia just blocks aerobic respiration, while ischemia results in hypoxia + 9 nutrients + 8 metabolites (impairs anaerobic glycolysis as well); ie ischemia injures tissues faster than hypoxia alone. 1) Reversible Ischemic Injury C affected cells can recover if blood flow restored. a) Reduced activity of ATP-dependant Na+ pump (and Ca2+ pump) < 8 intracellular Na+ (8H20) / 9intracellular K+, 8Ca2+ ÿ ionic / osmotic imbalance ÿ acute cell swelling. b) Altered cellular energy metabolism < 9oxidative phosphorylation ÿ 8anaerobic glycolysis ÿ 9glycogen stores ÿ 8lactic acid & [Pi] ÿ 9pH. c) Detachment of ribosomes from RER and polysomes < reduction in protein synthesis. d) Morphologic changes < plasma membrane: loss of microvilli, blebbing, myelin figures, loosening of intercellular attachments. < endoplasmic reticulum: dilation of cisternae (fluid accumulation) detachment / disintegration of polysomes < mitochondria: swelling, appearance of small densities. < nucleus: clumping of chromatin. e) Functional impairment < eg heart muscle stops contracting in 60 sec. of coronary occlusion; however myocardial cell not dead. 2) Irreversible Ischemic Injury C irreversible injury occurs if ischemia persists (eg heart muscle within 20 - 60 min after coronary occlusion). C the critical transition point to irreversible injury is not known. C two features consistently characterize irreversibility (ie “point of no return” or “lethal hit”): Î inability to reverse mitochondrial dysfunction. Ï profound disturbances of membrane function. C morphologic / functional changes: < severe swelling of mitochondria with large densities within the matrix. < extensive damage to plasma & organelle membranes (loss of proteins, essential coenzymes & RNA from leaky membranes ÿ unable to restore ATP production; marked influx of Ca2+). < swelling of lysosomes (further injury to lysosomal membranes results in leakage of enzymes into cytoplasm ÿ acid hydrolases are activated in 9pH ÿ degradation of cytoplasm and nuclear material). C after cell death: < cell parts continue to be digested by lysosomal acid hydrolases. < widespread leakage of cellular enzymes into ECF (eg CK from muscle, ALT from liver). < influx of macromolecules from the ECF. < cell debris either removed by phagocytosis or broken down into fatty acid residues (± calcification). 3) Reperfusion Injury [for information only] C a transient period of ischemia causes the death of some cells and injury to others. C these injured cells are "at risk" due to metabolic changes, but are not yet dead and may be able to survive. C reperfusion can induce new damaging processes that cause death in cells that might otherwise recover. a) mechanisms of reperfusion injury Î new O2 free radicals from reoxygenation of injured parenchymal / endothelial cells (from damaged mitochondria, altered oxides, damaged antioxidants) and from leukocytes (“spill over”). Ï marked influx of new Ca2+ due to membrane / ion pump damage. Ð initial ischemic injury leads to 2o inflammation following reperfusion ÿ additional injury. Gen Path (VPM 152) Cell Pathology 11 VI. CHEMICAL INJURY 1) Mechanisms of Chemical Injury C chemicals and certain drugs and toxins produce damage in one of two general ways. a) Direct interaction < some chemicals act directly by damaging particular organelles or critical cell molecules. - eg cyanide ÿ damages mitochondrial cytochrome oxidase ÿ blocks oxidative phosphorylation. - eg fluoroacetate ÿ converted to fluorocitrate ÿ prevents citrate from being used in the citric acid cycle. b) Conversion to reactive toxic metabolites < toxic metabolites usually produced by cytochrome P-450 mixed function oxidase (MFO) in the SER of liver < toxic metabolites can be in the form of reactive free radicals or can form strong covalent bonds with cell molecules (thus damaging them). < since liver is a major site of chemical modification of drugs and toxins, it is therefore particularly susceptible to drug / toxin-induced injury. Acetaminophen (Tylenol) Toxicity < in humans & dogs most acetaminophen is detoxified in liver to glucuronide and sulfate conjugates which are then excreted in the urine; only small amounts converted to highly reactive metabolite NAPQI by P450 MFO. < cats are relatively deficient in glucuronyl transferase and a large portion of acetaminophen is metabolized to NAPQI, which is electrophilic ÿ binds to molecules in hepatocytes (ie adduct formation) and causes necrosis. < additionally cats (and dogs) appear to produce relatively more of the metabolite para-aminophenol, which is released from the liver cells and results in oxidative damage to hemoglobin (ie methemoglobinemia). Gen Path (VPM 152) Cell Pathology 12 Carbon Tetrachloride (CCl4) Toxicity < CCl4 metabolized by P450 MFO enzyme system on the SER of the hepatocyte (CCl4 + e ÿ CCl3• + Cl- ). < CCl3• is highly reactive and causes lipid peroxidation (autocatyzing) ÿ see severe and rapid membrane destruction ÿ 9protein synthesis (30 min); ER swelling & ribosomal dissociation (2 hrs). MORPHOLOGY OF CELL INJURY AND NECROSIS C gross morphologic changes usually require hours to develop, ie no sign of myocardial necrosis if an animal dies immediately from a myocardial infarct (however a thrombus would be evident in a coronary artery!) C in general: i) cell swelling (reversible injury) - can start within minutes of the initial insult. - note, loss of function is also rapid, eg heart muscle stops contracting with 60 sec of coronary occlusion. ii) cell death (irreversible injury) - eg can occur in the myocardium within 20 to 60 min of coronary artery occlusion. - biochemical changes (eg creatine kinase, troponins) within minutes & EM changes within few hrs. - LM changes in 4 to 12 hrs and gross changes not apparent for 12 to 24 hrs after initial insult. I. REVERSIBLE CELL INJURY C two main types recognized by LM ÿ cellular swelling and fatty change. 1) Cellular Swelling a) Etiology / Pathogenesis of Cellular Swelling (see prior discussion) < early and almost universal manifestation of cell injury. < due to loss of ion and fluid homeostasis (esp Na+ pump) ÿ net 8 [intracellular H2O]. b) Gross Appearance of Cellular Swelling < organ swollen with rounded edges, tissue may show slight palor. < cut surface: tissue bulges and can not be easily put in correct apposition, heavy. c) Histologic Appearance of Cellular Swelling < affected cells appear enlarged, with pale cytoplasm, nucleus in normal position. < staining characteristics are altered: - if mild, may have cloudy appearance = "cloudy swelling". - as the process continues many vacuoles of variable size appear in the cytoplasm; called “hydropic (vacuolar) degeneration” or when severe “ballooning degeneration” (esp viral infected cells). d) Ultrastructural Changes of Cellular Swelling < see reversible ischemic injury pg 10. e) Prognosis of Cellular Swelling < cell swelling is reversible, ie if stimulus / stress is removed the cell returns to its normal state. 2) Fatty Change a) Etiology / Pathogenesis of Fatty Change < occurs in various forms of injury (esp hypoxic, toxic, metabolic). < see abnormal accumulation of lipids within the cell (ie: intracellular). < mainly found in cells dependant on fat metabolism, esp liver, + renal tubular epithelium & myocardium. < seen in abnormalities of uptake, utilization (metabolism) and/or mobilization (export) of fat. < may be an expression of cell injury or a stage of injury in cells that are destined to die. < may be preceded or accompanied by cell swelling. Gen Path (VPM 152) Cell Pathology 13 < eg lipid metabolism and storage in the liver: Î lipids enter hepatocytes as free fatty acids (FFA); - fatty acids can also be synthesized from acetate. Ï lipids are metabolized by hepatocytes - mostly are esterified to form triglycerides (TG). - some synthesized to cholesterol esters or phospholipids. - some oxidized for energy & produce ketone bodies. Ð lipids are exported from hepatocyte - TG’s must be complexed with a lipid-acceptor protein (apoprotein) to form lipoproteins to be exported. - accumulation of hepatocellular intracellular lipid can occur due to abnormalities in any of these steps; esp important is the synthesis of lipid-acceptor protein (apoprotein) to form lipoproteins; - eg’s: excess dietary fat (eg foie gras); starvation/prolonged fasting & diabetes (8FA mobilization & 9protein synthesis); hypoxia (inhibits fatty acid oxidation & 9protein synthesis); some toxins (9apoprotein synthesis). b) Gross Appearance of Fatty Change < in liver: - diffusely yellow if all cells affected or reticular pattern if zones of hepatocytes are affected. - edges rounded and will bulge on cut section, cuts easily and has a greasy texture. - if severe liver may float in fixative / water. c) Histologic Appearance of Fatty Change < presence of well delineated, lipid-filled vacuoles in the cytoplasm. < may be single, large vacuoles or multiple, small vacuoles. < confirm with special stain (since not all clear vacuoles are lipid, ie could be water or glycogen); use frozen sections with oil-soluble dye, eg "oil red O". II. IRREVERSIBLE CELL INJURY 1) Necrosis C term used to describe the range of morphologic changes that occur following cell death in living tissue. C the morphologic appearance is due to 2 concurrent processes: Î denaturation of proteins (ie nonproteolytic structural alteration in 2o or 3o structure). Ï enzymatic digestion of the cell: - endogenous enzymes derived from the lysosomes of the dying cells = autolysis (self digestion). - lysosomes of immigrant leukocytes = heterolysis. C note: autolysis is also often used to describe the changes that occur in all of the cells after an animal has died (the proper term is postmortem autolysis or postmortem decomposition). C a mass of necrotic tissue may exhibit distinctive morphologic patterns depending on whether enzyme catabolism or protein denaturation predominate. a) Coagulation (coagulative) Necrosis < most common manifestation of cell death. < is characteristic of hypoxic / ischemic death of cells in all tissues (except brain). < basic outline of coagulated cell persists at least for a few days; protein denaturation predominates over enzymatic digestion Gen Path (VPM 152) Cell Pathology 14 Gross appearance < architecture of necrotic tissue resembles normal tissue, but color and texture may be visibly different. < lighter in color (pale); due to coagulation of cytoplasmic proteins and decreased blood flow, eg infarcts < usually firm texture. < may be swollen (due to swelling of individual cells) or shrunken (due to cell loss). < may see a local reaction to necrotic tissue (surrounding red zone of hyperemia or white layer of inflammatory cells). Microscopic appearance < original cell shape and tissue architecture preserved, ie dead cells resemble an eosinophilic "shadow" of the original cells. < cytoplasm: - increased eosinophilia (on H&E stain) due to binding of eosin to altered proteins & loss of ribosomes. - cytoplasm is usually hyalinized (homogeneous glassy appearance) due to the loss of glycogen particles. - dead cells may also be mineralized (“calcified”). - eventually necrotic cells are removed by white blood cell proteolysis and phagocytosis. - 3 patterns of nuclear changes: < karyolysis - see dissolution / fading of the nucleus (fading of chromatin 2N to DNAases). < pyknosis - shrunken and densely basophilic nuclei (also seen in apoptosis). < karyorrhexis - nuclear fragmentation. < even with these latter two types, after 1-2 days following the death of the cells, the nuclei disappear. b) Liquefactive Necrosis < occurs when enzymatic digestion of necrotic cells predominates over protein denaturation. < seen in many bacterial infections, due to attraction of neutrophils which contain potent hydrolases which are capable of digesting dead cells. < also, for unknown reasons, hypoxic damage of the brain/spinal cord, can cause liquefactive necrosis. Gross appearance < affected tissue is liquefied; becomes a soft to viscous fluid. < if process was initiated by inflammation, then the liquid is often mostly dead WBC’s (ie pus). Microscopic appearance < may see degenerate neutrophils and amorphous material (or nothing if necrotic tissue has flowed out). c) Caseous Necrosis < typical lesion seen with specific bacterial diseases, eg tuberculosis, caseous lymphadenitis. < common in birds since heterophils don’t have the potent hydrodrolytic enzymes to liquefy cells. Gross appearance < grey-white and dry with friable (crumbly) to pasty (caseous = cheese like) texture. Microscopic appearance < necrotic areas consist of dead cells persisting as amorphous, coarsely, granular debris; often mineralized. < necrotic cells do not retain cellular outline as seen with coagulation necrosis. < necrotic cells do not undergo complete dissolution as seen in liquefactive necrosis. d) Gangrenous Necrosis [= Gangrene] < definition: necrosis (usually ischemic) of extremities, eg distal limbs / digits or tips of ears. < dry gangrene = coagulation necrosis of an extremity. < wet gangrene = when the coagulative necrosis of dry gangrene is modified by the liquefactive action of saprophytic / putrefactive bacteria. < gas gangrene = production of gas bubbles in the necrotic tissue by infecting bacteria (esp Clostridia). Gen Path (VPM 152) Cell Pathology 15 e) Fat Necrosis < type of necrosis distinguished by its location within body fat stores, esp abdominal or subcutaneous fat. < etiology: inflammation (esp pancreatitis), Vit E deficiency, trauma, unknown causes (idiopathic). eg, in pancreatitis digestive enzymes are activated extracellularly ÿ adipose and pancreatic tissues are digested ÿ fatty acids combine with Ca2+ ÿ precipitated as insoluble Ca2+ soaps ("saponification of fat"). Gross appearance < firm to hard, white / chalky, ± gritty areas (often adjacent to normal fat). Microscopic appearance < areas of coagulative necrosis of fat tissue often with cholesterol clefts, with basophilic calcium deposits and often surrounded by inflammatory cells. 2) Apoptosis a) Definition (derived from the Greek = “falling off”) < death of single cells as a result of activation of a genetically programmed "suicide" pathway. < differentiating apoptosis from necrosis is important, in that necrosis indicates widespread tissue injury due to severe pathologic stimuli, while apoptosis indicates selective elimination of cells, due to either physiologic or specific pathologic stimuli. < apoptosis involves death of single cells (or small clusters) with intact cell membranes and rapid removal by phagocytosis with little inflammation while necrosis often involves locally extensive areas with loss of cell membrane integrity, enzymatic digestion and an inflammatory response < note, intermediate / hybrid forms of cell death exist that share aspects of necrosis & apoptosis (necroptosis). Gen Path (VPM 152) Cell Pathology 16 b) Causes < seen in many physiologic / adaptive situations or pathologic events (when cells have irreparable damage). Physiologic Î Cells undergoing programmed cell death during embryologic development (eg sculpting of the digits). Ï Cells undergoing normal turnover - hormone-dependent involution (eg endometrium, mammary, prostate). - cell depletion in proliferating population (eg unused neutrophils). Ð Immune System - depletion of autoreactive T cells in thymus. - immune regulation (eg lymphocytes at the end of an immune response). Pathologic stimuli Î DNA damage - when DNA is damaged beyond repair, eg radiation, toxins, Ï Misfolded proteins - excess accumulation in ER, beyond ability to adapt, leads to apoptosis. Ð Specific infectious agents - esp viruses; induced by either direct viral damage or by T-cell response. Ñ Specific immune response - apoptosis of altered cells by cytotoxic T cells (eg viral infected cells, mutated tumor cells, rejection of transplant cells). Ò Pathologic atrophy of organs after duct obstruction (eg pancreas, kidney, salivary gland). c) Biochemical Mechanisms Î Signaling Pathways that Initiate Apoptosis - stimulate targets on surface (eg TNF / TNFR) or in the cell. Ï Control & Integration - balance of pro- & anti-apoptotic molecules determines outcome of affected cell. Ð Common Execution Phase - actual death program accomplished by proteases (esp caspase family). Ñ Removal of Dead Cells - apoptotic cells have ligands for phagocyte receptors; efficient, no inflammation. d) Morphologic Features < because the events are rapid, considerable apoptosis may occur in tissues before it evident on histology. Î Cell shrinkage - cytoplasm has packed organelles Ï Chromatin condensation - dense aggregates of chromatin ± fragmentation Ð Formation of cytoplasmic blebs then apoptotic bodies with intact membranes (± contain nuclear fragments) Ñ Phagocytosis of apoptotic cells / cell bodies - usually by macrophages with no inflammatory response e) Consequence of “too much” or “too little” Apoptosis Î Disorders associated with defective apoptosis (increased cell survival) - increased survival of abnormal cells with neoplasia (eg p53 mutation) or increased survival of autoreactive lymphocytes causing autoimmune disorder. Ï Disorders associated with increased apoptosis (excessive cell death) - increased loss of cells in neurodegenerative diseases, ischemic injured cells or viral infected cells. Gen Path (VPM 152) Cell Pathology 17 PIGMENTS AND OTHER TISSUE DEPOSITS C many pathologic processes are accompanied by accumulations of material either within the cell (intracellular) or within the extracellular space. 1) Lipid Accumulation a) Intracellular < types of lipids which can accumulate: Î Triglycerides - (see previous discussion of fatty change in reversible cell injury) Ï Inherited Storage Diseases (Lipid storage disorders) Ð Cholesterol accumulations < eg inflammation and necrosis: foamy macrophages at sites of cell injury and inflammation, ie phagocytosis of lipid material from dead cells. < eg atherosclerosis: accumulation of lipids in smooth muscle cells and macrophages in walls of arteries / arterioles (in vet med, in some dogs with hypothyroidism / hypercholesterolemia). < eg xanthomas: tumor like masses in skin formed by clusters of foamy macrophages. b) Adipose (Fatty) Tissue Infiltration < occasionally seen in skeletal muscle and myocardium (sometimes called muscle steatosis). < microscopically see normal fat tissue, which has replaced lost (congenital or acquired) muscle fibers. < usually not associated with functional disturbance. 2) Glycogen Accumulation C excessive intracellular deposits of glycogen, ie seen with abnormalities of glucose or glycogen metabolism. C eg’s, in renal tubular epithelium with diabetes mellitus, in hepatocytes of dogs with excess corticosteroids (“steroid hepatopathy”), in various cells with glycogen storage diseases. C microscopically, see poorly delineated vacuoles within cell; to confirm use PAS stain (ie rule-out fat or H20). 3) Protein Accumulation C terminology: Î hyaline is the name given to any substance, intracellular or extracellular, which has a homogeneous, glassy, eosinophilic appearance; the substance is often protein in nature (eg’s amyloid; Ag-Ab complexes causing thickened BM’s; protein droplets in renal tubular epithelium). Ï fibrinoid is a nonspecific term for hyaline material within an arterial wall. < the presence of plasma proteins / Ag-Ab / complement within a damaged vascular wall causes intense eosinophilic staining (often called “fibrinoid necrosis”). C eg’s Î reabsorption droplets in renal tubular epithelium: often with glomerular damage protein is lost in the urine, some of this protein can be reabsorbed by proximal tubular cells; see eosinophilic droplets in the cytoplasm. Ï "Russell bodies" of plasma cells (Mott cells): when Ig’s accumulate within the cisternae of the RER. Ð defects in protein folding can cause intracellular or extracellular accumulations of protein: a) ER stress / “unfolded protein response” is induced by accumulation of unfolded & misfolded proteins. b) aggregates of misfolded proteins (genetic / acquired) - eg amyloid, prions in TSE’s, Alzheimer’s, etc. Gen Path (VPM 152) Cell Pathology 18 4) Amyloid and Amyloidosis Î amyloid: a pathologic proteinaceous substance (95% amyloid fibrils) which is resistant to proteolysis. - amyloid fibrils are insoluble aggregates that result from the self-assembly of abnormally folded proteins (typically the abnormal folded protein has excess â sheet conformational change). - almost all types of misfolded proteins are degraded intracellularly (proteosomes) or extracellularly (macrophages); however a few types of protein which misfold with excessive and/or externalized â sheet structures can form amyloid. - ultrastructurally see masses of linear, nonbranching fibrils 7.5-10 nm in diameter. Ï amyloidosis: a disorder of protein folding in which normally soluble proteins are deposited as abnormal, insoluble fibrils that disrupt tissue structure and function. C amyloid can be formed in a variety of pathologic conditions (eg neoplasia, inflammation, genetic) from a variety of proteins (derived from about 20 unrelated proteins in humans). C in vet medicine, mostly see as reactive systemic amyloidosis secondary to chronic inflammatory disease. C in humans most commonly associated with plasma cell neoplasia (less common in vet med). C chemical composition: Î Protein AA - derived from an acute phase protein called serum amyloid A (SAA) in chronic inflammation Ï Protein AL - derived from immunoglobulin light chains with plasma cell neoplasia. Ð Familial amyloid - in humans, Shar pei dogs, Abyssinian cats. Ñ Endocrine amyloid - derived from polypeptide hormones or prohormones in neoplastic or degenerative conditions, eg islet amyloidosis in cats with type 2 diabetes mellitus. Ò Other amyloids - eg’s, misfolded prion protein (PrPsc) in TSE’s; amyloid plaques in Alzheimer disease. C it can be deposited locally or systemically; once deposited is difficult to digest / remove. C grossly: < organ involved may be normal or enlarged, and often firm. < amyloid stains black when Lugol's iodine is applied to fresh tissue. C microscopically: < on H&E staining see lightly eosinophilic, amorphous, hyaline material that is deposited extracelluarly. < on congo red staining amyloid is orange-red & under polarized light shows apple green birefringence. C sites and significance: Î renal < amyloid in glomerular BM ÿ impairs glomerular filtration, causing protein losing glomerulopathy. < amyloid in medullary interstitium ÿ impairs medullary function. Ï other organs (eg liver, pancreas, spleen, vessel walls, skin) < can enlarge, distort and/or compress organ. < can interfere with function (eg blocking space of Disse in liver, obliterating pancreatic islets). Gen Path (VPM 152) Cell Pathology 19 5) Endogenous Pigments C endogenous pigments (colored substances) are those that originate in the animal. a) Lipofuscin < also known as "wear-and-tear" or “aging” pigment. < origin: breakdown products of lipids, usually derived from cell membranes (esp lipid peroxidation). < sites: aged cells, eg myocardial cells and neurons of old animals, or in chronically injured cells. < grossly: when severe can give yellow-brown discoloration to tissue. < microscopically: golden brown, finely granular, intracellular pigment. < significance: does not injure cell, but is a sign of aging or excess free radical damage. Lipofuscinosis - disorders characterized by the excess storage of lipofuscin. eg “brown gut syndrome” of dogs - vitamin E/selenium deficiency ÿ increased free radical damage. grossly the intestine has a distinct yellow-brown discoloration (intestinal lipofuscinosis); microscopically see increased amount of lipofuscin in smooth muscle cells. b) Ceroid < variant of lipofuscin which is acid-fast positive and autofluorescent. c) Melanin < insoluble, intracellular, brown-black pigment derived from tyrosine. < origin: normal pigment found in epidermis & some cells of the eye. - in the skin, melanocytes (derived from neural crest cells) produce melanin granules which they inject into keratinocytes for skin / hair coloration & protection from UV light. < sites: melanin can also occur incidentally at other sites and when in excess called melanosis, eg leptomeninges (esp ruminants), intestine, kidney, lung, base of aorta, etc. < grossly: melanosis will appear as a dark (pigmented) area of otherwise normal tissue. < microscopically: see finely granular, brown, intracellular pigment. d) Copper < less commonly stored in tissues (primarily in hepatocytes). < occurrence: sheep with chronic copper poisoning. - some dog breeds with inherited copper storage disorder (Wilson's disease), eg Bedlington terriers. < significance: storage of large amounts of copper is toxic to the hepatocyte and may produce a sudden onset of acute hepatocellular degeneration (via catalyzing lipid peroxidation). e) Hemosiderin < origin: represents stored iron (ferric form = Fe3+), recovered from the hemoglobin of destroyed rbc’s. - in cells, Fe3+ bound to apoferritin forming ferritin; excess ferritin forms hemosiderin granules. < sites: normal in macrophages of spleen and bone marrow. - anywhere excessive breakdown of erythrocytes or excessive accumulations of iron. eg’s: in macrophages at sites of congestion / hemorrhage (eg bruise), splenic macrophages and Kupffer cells in hemolytic anemia, alveolar macrophages in congestive heart failure (“heart failure cells”). < grossly: may give a light brown color to the tissues. < microscopically: yellow-brown, granular, intracellular pigment (stains positive with Prussian blue). < significance: a mild or even moderate accumulation, usually causes no damage, called hemosiderosis. - called hemochromatosis when a massive accumulation causes cell damage (eg idiopathic hemochromatosis of mynahs and some other birds). Gen Path (VPM 152) Cell Pathology 20 f) Bilirubin < bilirubin is end product of heme degradation (no iron); mostly from senescent rbc’s via macrophages. < origin: heme ÿ biliverdin (by heme oxygenase) ÿ uncongugated bilirubin (by biliverdin reductase) ÿ binds albumin & transported to the liver ÿ conjugated to its glucuronide (water soluble) ÿ excreted in bile. < occurrence: Î prehepatic jaundice ÿ primarily with increased breakdown of erythrocytes, eg hemolytic disease. Ï hepatic jaundice ÿ with failure of conjugation or excretion. Ð post hepatic jaundice ÿ obstruction of bile duct flow. < sites: in hepatocytes (intracytoplasmic or in canaliculi); in renal tubular epithelium (can be toxic). < grossly: in blood and tissues produces a yellow discoloration, called jaundice or icterus. < microscopically: green-brown to yellow-brown granular pigment in cytoplasm of hepatocytes or distending bile canaliculi. g) Hematoidin < bright yellow-brown homogenous pigment occasionally seen at sites of previous hemorrhage. < believed to be locally precipitated bilirubin (stains negative for iron). h) Acid-Hematin < blood + acid = acid hematin (black color). < imparts black color to blood in stomach (eg gastric ulcers), ie blood + stomach HCl = melena. < is also an artifact in histologic tissue, ie black precipitate on slide, due to improperly buffered (acidic) formalin reacting with blood from tissues (called “formalin pigment”). 6) Pathologic Calcification (Mineralization) a) Dystrophic Calcification < calcification of injured cells (no hypercalcemia or other disturbances of calcium homeostasis). < occurrence: - in areas of necrosis (either coagulative, liquefactive or caseous), small membrane fragments produced during cell necrosis act as a nidus for Ca2+/PO4 precipitation. - in cells injured by many mechanisms, eg vascular, toxic, metabolic, inflammation. - most prominent when there is a good blood supply in the injured tissue. < grossly: white, irregular areas, sometimes dry and gritty, (may not be visible). < microscopically: - intracellular or extracellular, amorphous, basophilic granular deposits. - stains black with a Von Kossa special stain. eg’s “white muscle disease” (nutritional myopathy) associated with Vit E / selenium deficiency in farm animals, tuberculosis nodules, abdominal fat necrosis, etc. b) Metastatic Calcification < when apparently normal tissue undergoes calcification; with hypercalcemia / altered Ca2+ metabolism. < occurrence: - primary hyperparathyroidism - renal failure / secondary hyperparathyroidism - vitamin D toxicosis (iatrogenic or plant analogues in cattle; rodenticides in dogs & cats) - paraneoplastic syndrome (with certain neoplastic diseases); eg, canine lymphosarcoma. < sites: many sites can be affected, especially gastric and intestinal mucosa, interstitium of blood vessel walls, basement membranes of many tissues (esp lung and kidney). < grossly: if visible, often as white plaques or streaks. < histo: basophilia (with H&E stain), may be clumped or in linear deposits; usually associated with BM’s and elastic fibers, deposits may be smooth or irregular, stains black with Von Kossa stain. Gen Path (VPM 152) Cell Pathology 21 7) Crystals a) Calcium Oxalate < origin: plants with high levels of oxalic acid, eg halogeton, rhubarb, greasewood. - antifreeze contains ethylene glycol (via hepatic alcohol dehydrogenase) ÿ glycoaldehyde ÿ glycolic acid ÿ glyoxcylic acid ÿ oxalic acid ÿ calcium oxalate (precipitated in lumina of renal tubules). - many of the chemical intermediates of ethylene glycol metabolism are toxic to renal tubular epithelium and/or nervous tissue. < occurrence: - in sheep due to ingestion of poisonous plants. - in cats and dogs due to ingestion of antifreeze. < grossly: kidneys may be slightly swollen, usually none. < microscopically: degeneration & necrosis of tubular epithelium and often see refractile, translucent, yellow crystals (calcium oxalate) in renal tubular lumina / interstitium. < significance: severe renal dysfunction & electrolyte imbalances (eg hyperkalemia, acidosis) ÿ death. b) Urates and Uric Acid < gout: humans: disorder of purine metabolism where there is hyperuricemia and deposition of urates in tissues. birds / reptiles: uric acid is the end product of nitrogen metabolism, so any significant renal dysfunction (including dehydration) can lead to abnormal accumulations / deposits of urates. < occurrence: birds, reptiles and humans. < sites: - in and around the joints, called articular gout. - on serosal surfaces or in tissues, called visceral gout. < grossly: chalky white masses in tissues (called "tophi") or frosting of crystals on serosal membranes. < microscopically: variably sized clear crystals, frequently associated with macrophages. c) Cholesterol Clefts < occurrence: any tissue following severe necrosis or hemorrhage (from cell membranes), esp fat necrosis; also see in metabolic disorders of cholesterol accumulation (eg atherosclerosis, xanthomas). < microscopically: see elongate, needle-like crystals, often in picket fence-type arrangement. 8) Exogenous Pigments C exogenous pigments are those that originate outside the body, ie from external environment. C eg, carbon, soot, dusts, silica, asbestos, tattoo pigments, etc. a) Anthracosis < deposition of carbon particles (esp from air pollution), into lungs / lymph nodes. < gives tissue a black discoloration to tissue; see in macrophages in lungs and draining lymph nodes. < relatively harmless unless present in large quantities (eg chronic lung injury in coal miners). b) Silicosis < deposition of silica dust in the lungs, is a special problem for miners; causes granulomatous pneumonia. c) Asbestosis < deposition of asbestos into lung, associated with mesotheliomas, and chronic lung injury. 9) Parasite Pigments C several parasites are commonly associated with pigmented material, eg’s, < Pneumonyssus simicola - brown to black pigment in the airways of monkeys with lung mites. < Plasmodia - malarial pigment from excretion of catabolized haemoglobin (large deposits in macrophages of spleen and liver). < Fascioloides magna - liver fluke of ruminants; see black discoloration of tissue around bile ducts due to regurgitated iron-porphyrin pigment (“fluke puke”). Gen Path (VPM 152) Cell Pathology 22 POST MORTEM ARTIFACTS [for information only - see also PM artifacts slideshow on website] “Once you know the normal and the artifacts, all the rest is pathology!!” Dr. T Van Winkle 1) Postmortem Scavenging vs Predation C postmortem scavenging = removal of organs (esp eyes, tongue, rectum) of carcass by carrion eating animals (eg dogs, coyotes, ravens, vultures, etc). 2) Rigor Mortis C contraction of muscles after death. C usually within 1-6 hrs after death (depending on glycogen stores, ambient temperature, etc) & lasts 1-2 days C after death, circulation of blood ceases ÿ muscle cells resort to anaerobic glycolysis ÿ when glycogen stores run out & ATP becomes depleted (needed for muscle relaxation) ÿ Ca2+ floods into muscle cells causing myofilaments to contract (note: all muscles affected, flexors / extensors, causing rigidity of joints) ÿ rigor mortis gradually dissipates with autolysis of structural and functional muscle proteins. 3) Algor Mortis C gradual cooling of the cadaver to ambient temperature (in humans 1.5oF per hr). 4) Livor Mortis (hypostatic congestion) C gravitational pooling of blood to the dependant regions ("down side") of the body. 5) Postmortem Clotting C occurs in heart and vessels. C rbc’s may separate from plasma (esp in animals with high fibrinogen levels, eg horses) = “chicken fat clot” 6) Hemoglobin Imbibition C HgB released by rbc breakdown (after death) ÿ staining tissues. C especially lining of heart and blood vessels; also common in tissues of aborted fetuses and frozen tissues. 7) Bile Imbibition C leakage of bile from gall bladder and major bile ducts which stains adjacent tissues green to yellow. 8) Pseudomelanosis C term used to describe an artifactual black discoloration of tissues (similar in an appearance to melanosis). C due to saprophytic/putrefactive bacterial production of hydrogen sulfide (H2S) + iron ÿ iron sulfide (FeS). 9) Postmortem autolysis / decomposition C after death, decomposition of tissues begins by progressive release of endogenous enzymes (autolyis) and more gradually by the action of saprophytic bacteria (especially from gut). C rate of progression dependent upon several factors, eg body temperature at time of death; ambient temperature; size of body; amount of fat/hair/wool; cause of death (eg bacterial infection, hyperthermia, etc). C grossly the tissues become progressively more pale (often mottled) and soft. 10) Putrefaction and Postmortem Emphysema (bloating) C putrefaction (rotting), refers to the enzymatic decomposition of organic material (tissue) with production of foul-smelling compounds (eg H2S, NH3, mercaptans), especially by saprophytic / putrefactive bacteria. C postmortem emphysema occurs when saprophytic bacteria produce gas, causing gaseous distention of G-I tract, organs and body cavities. 11) Postmortem Ruptures and Organ Displacements C with swelling of viscera (due to postmortem emphysema) ÿ rectal prolapse, visceral dislocation, gastric rupture (horses), diaphragmatic hernia. 12) Other Abnormalities C rib indentations on pulmonary pleura. C pale discolored compressions on capsular surface of liver from distended intestine loops and/or rib imprints. C euthanasia with barbiturate ÿ splenomegaly, accumulation of fluid and blood in lung, froth in trachea. C lens opacity in frozen carcasses.