Sentinel Event Policy - Johns Hopkins University
advertisement
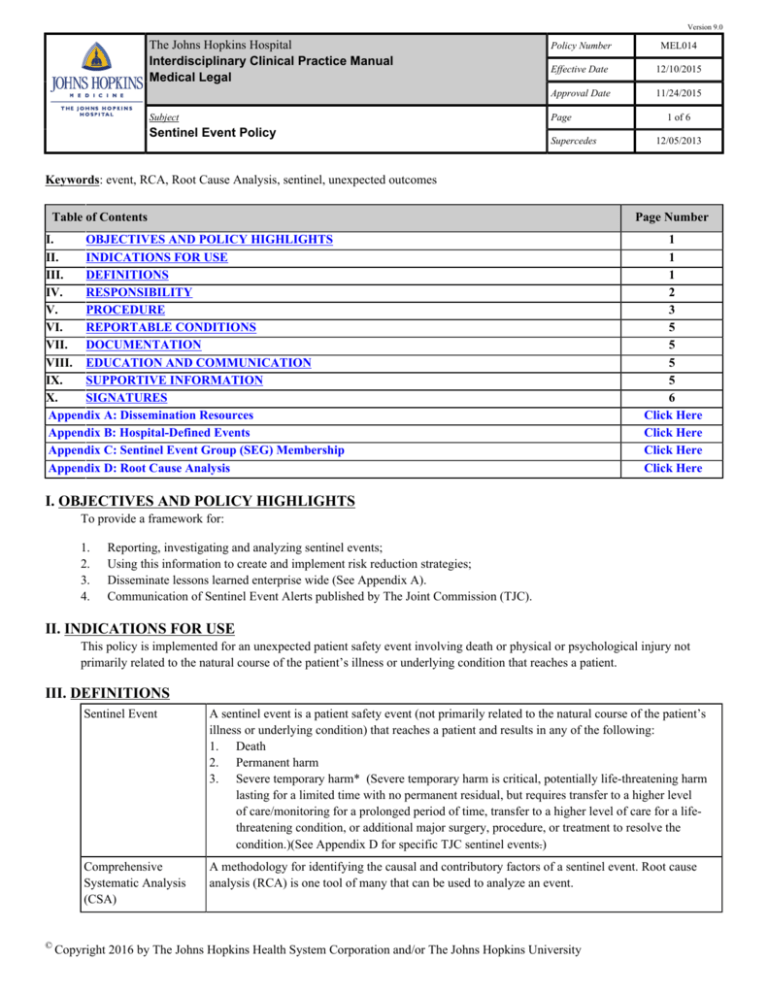
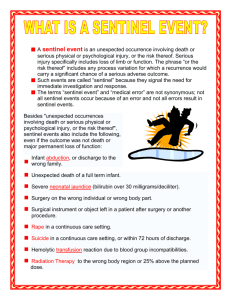
Version 9.0 The Johns Hopkins Hospital Interdisciplinary Clinical Practice Manual Medical Legal Subject Policy Number MEL014 Effective Date 12/10/2015 Approval Date 11/24/2015 Page Sentinel Event Policy Supercedes 1 of 6 12/05/2013 Keywords: event, RCA, Root Cause Analysis, sentinel, unexpected outcomes Table of Contents Page Number I. OBJECTIVES AND POLICY HIGHLIGHTS II. INDICATIONS FOR USE III. DEFINITIONS IV. RESPONSIBILITY V. PROCEDURE VI. REPORTABLE CONDITIONS VII. DOCUMENTATION VIII. EDUCATION AND COMMUNICATION IX. SUPPORTIVE INFORMATION X. SIGNATURES Appendix A: Dissemination Resources Appendix B: Hospital-Defined Events Appendix C: Sentinel Event Group (SEG) Membership Appendix D: Root Cause Analysis 1 1 1 2 3 5 5 5 5 6 Click Here Click Here Click Here Click Here I. OBJECTIVES AND POLICY HIGHLIGHTS To provide a framework for: 1. 2. 3. 4. Reporting, investigating and analyzing sentinel events; Using this information to create and implement risk reduction strategies; Disseminate lessons learned enterprise wide (See Appendix A). Communication of Sentinel Event Alerts published by The Joint Commission (TJC). II. INDICATIONS FOR USE This policy is implemented for an unexpected patient safety event involving death or physical or psychological injury not primarily related to the natural course of the patient’s illness or underlying condition that reaches a patient. III. DEFINITIONS © Sentinel Event A sentinel event is a patient safety event (not primarily related to the natural course of the patient’s illness or underlying condition) that reaches a patient and results in any of the following: 1. Death 2. Permanent harm 3. Severe temporary harm* (Severe temporary harm is critical, potentially life-threatening harm lasting for a limited time with no permanent residual, but requires transfer to a higher level of care/monitoring for a prolonged period of time, transfer to a higher level of care for a lifethreatening condition, or additional major surgery, procedure, or treatment to resolve the condition.)(See Appendix D for specific TJC sentinel events.) Comprehensive Systematic Analysis (CSA) A methodology for identifying the causal and contributory factors of a sentinel event. Root cause analysis (RCA) is one tool of many that can be used to analyze an event. Copyright 2016 by The Johns Hopkins Health System Corporation and/or The Johns Hopkins University Version 9.0 The Johns Hopkins Hospital Interdisciplinary Clinical Practice Manual Medical Legal Subject Policy Number MEL014 Effective Date 12/10/2015 Approval Date 11/24/2015 Page Sentinel Event Policy Supercedes 2 of 6 12/05/2013 Root Cause Analysis (RCA) Root cause analysis is a process for identifying the causal factors that underlie variation in performance, including the occurrence or possible occurrence of a Level I adverse/ sentinel event. The RCA focuses primarily on systems and processes, not individual performance. (See Appendix B) Action Plan Risk Reduction Strategy A plan developed during the CSA which identifies the strategies the Hospital intends to implement to reduce the risk of a reoccurrence of a similar event. This plan addresses responsibility for implementation, oversight, time line and strategies for measuring the effectiveness of process and system improvements to reduce risk. Level 1 Adverse Event The State of Maryland defines a Level 1 adverse event as “an event resulting in death or serious disability”. Serious disability is defined as “a physical or mental impairment that substantially limits one or more of the major life activities of an individual lasting more than seven days or is still present at the time of discharge." Sexual abuse/assault (including rape) The Joint Commission defines sexual abuse/assault (including rape) as a sentinel event as nonconsensual sexual contact involving a patient and another patient, staff member, or other perpetrator while being treated or on the premises of the hospital, including oral, vaginal, or anal penetration or fondling of the patient's sex organ(s) by another individual's hand, sex organ, or object. One or more of the following must be present to determine that it is a sentinel event: • • • Sentinel Event Alerts Any staff-witnessed sexual contact as described above Admission by the perpetrator that sexual contact, as described above, occurred on the premises Sufficient clinical evidence obtained by the hospital to support allegations of unconsented sexual contact "Sentinel Event Alerts" are published periodically by The Joint Commission. The alerts describe common underlying causes of sentinel and adverse events and recommend steps to reduce risk and prevent future occurrences. IV. RESPONSIBILITY A. B. C. D. © Sentinel Event Group (SEG) 1. The SEG shall evaluate events to determine if they are sentinel events and oversee the conduct of comprehensive systematic analyses and the organization and implementation of an action plan. 2. Each member of the SEG shall identify a designee to evaluate events during his or her absence. 3. Refer to Appendix C for members of the SEG. The CSA Facilitator shall: 1. With the advice of the SEG, appoint the Team Leader. 2. Work with the root cause analysis team in the development of the root cause analysis. 3. Provide preliminary investigation of the event and training to analysis team members who may not have participated in a root cause analysis. 4. Complete the documentation for the analysis. 5. Create tools (e.g., flow diagrams) helpful in discerning root causes. CSA Team 1. Membership is determined by the facilitator with advice from SEG. Team Leader shall: 1. Chair the analysis team. 2. Have expertise in the clinical area of the event. Copyright 2016 by The Johns Hopkins Health System Corporation and/or The Johns Hopkins University Version 9.0 The Johns Hopkins Hospital Interdisciplinary Clinical Practice Manual Medical Legal Subject Sentinel Event Policy Policy Number MEL014 Effective Date 12/10/2015 Approval Date 11/24/2015 Page Supercedes 3 of 6 12/05/2013 3. E. F. G. H. Guide the team to help understand the issues, and assist with the identification of root causes and contributing factors. 4. Participate in Leadership meeting. Quality Improvement Monitor 1. The QI monitor is the Quality Improvement Department Team Leader supporting the functional unit involved in the Sentinel Event. 2. The QI monitor shall be a member of the analysis team, assists with the development of the action items, supervises the completion of action items, systematically keeps track of and communicates the status of each action item monthly to the Director of the Quality Improvement Department. Champion 1. The Champion of the sentinel event shall hold a significant leadership position in the Hospital or the functional unit that is involved in the Sentinel Event and shall be chosen at the completion of the Leadership meeting. The Champion shall work with the QI Monitor to follow the activities and completion of the action plans. When necessary, the Champion shall support the staff responsible for action items and work to eliminate barriers to completion of the action items. Action Item Holder 1. The Action Item Holder is the individual(s) identified and responsible for completion of action items. Leadership Review 1. Vice-Chairs and/or Physician Advisors shall be responsible for reviewing, revising and finalizing an analysis tool in collaboration with departmental Chairpersons prior to implementation of action items. Once the Chairperson/s of involved departments approve of a CSA including action items, the analysis will be presented to the SEG for final recordation through Risk Management of the accepted action plan. V. PROCEDURE A. B. C. © Medical Health Care Workers 1. Health care workers shall report unexpected patient safety events that may be sentinel events to unit leadership and to the Risk Management Department. A report of the event shall be placed in event reporting system.This report shall not be used to evaluate performance and competence of the individual reporting. Individuals may be held accountable for their actions if after thorough review of an event such actions are determined to be non-compliant with hospital policies and procedures. Senior Counsel for Patient Care, Risk Management, and Ethics 1. The Senior Counsel, when notified of an unexpected patient safety event, shall decide whether to convene the Sentinel Event Group (SEG) on the basis of an evaluation of available information. If the unexpected patient safety event may be a sentinel event, the SEG shall meet within one business day. Sentinel Event Group 1. When meeting to determine if a sentinel event has occurred, the SEG shall make, by the end of the business day, one of the following determinations: a. The unexpected patient safety event constitutes a sentinel event requiring the following immediate actions: i. Appointment by the SEG of a root cause analysis team; ii. Notification of the Dean and CEO of Johns Hopkins Medicine, the President of the Hospital, the Chairman of the Quality Improvement Committee of the Board of Trustees, the Chairman of the Medical Board, the COO of the Hospital, the Vice President and General Counsel, the Chairman, Physician Advisor, Director of Nursing, and Administrator of the affected department(s), and the Director of Quality Improvement. b. The unexpected patient safety event does not constitute a Level I adverse/sentinel event, and established risk management and performance improvement procedures are indicated. Only an RCA may be required. Copyright 2016 by The Johns Hopkins Health System Corporation and/or The Johns Hopkins University Version 9.0 The Johns Hopkins Hospital Interdisciplinary Clinical Practice Manual Medical Legal Subject Sentinel Event Policy Policy Number MEL014 Effective Date 12/10/2015 Approval Date 11/24/2015 Page Supercedes c. D. E. F. G. © 4 of 6 12/05/2013 There is insufficient information to determine whether the unexpected patient safety event constitutes a sentinel event and the SEG shall assign a fact-finding team to gather additional information and report to the SEG as soon as possible. 2. The SEG shall require the completion of the comprehensive system analysis and report documents within 45 business days from the date the SEG determines an CSA is required. Upon receipt of the CSA report, the SEG shall review the recommended action plan, and shall meet with the leaders of each Department to review and develop final action plans in a “leadership meeting”. The SEG and relevant departmental leadership shall identify a Champion and the individuals responsible for action plan follow-up. The documents setting out the CSA analysis and the action plan shall be submitted to the leadership of the Hospital. The completed CSA shall be presented to the Risk Management Committee and the Medical Board. A follow up and status report for each event shall be provided to the SEG and shared with Hospital leadership. (See Appendix “B”) 3. The SEG shall consider reporting requirements of TJC, and shall consult with the leadership of the Hospital prior to reporting to TJC. 4. The SEG shall consider reporting requirements of the State of Maryland, Department of Health and Mental Hygiene Office of Health Care Quality requirements for reporting of Level 1 adverse events and shall consult with the leadership of the Hospital prior to reporting to the State. 5. The Senior Counsel for Patient Care and Risk Management (or designee) shall notify the Johns Hopkins Medicine Institutional Review Board if an unexpected patient safety event under review is related to a research study. Sentinel Event Monitoring 1. Within 1 week of the Sentinel Event Leadership meeting, the Champion and the QI monitor shall meet to review all the action items, responsible parties and time frames for completion of actions. 2. A letter written under the signature of the Champion shall be written to each action item holder outlining the responsibilities for each action item. The letter shall contain the following: a. An explanation of the roles of the Champion and QI Monitor (identified by name). b. A statement that the QI Monitor shall communicate with the action item holder at least monthly to follow progress on each item, and to keep the Champion informed of progress. c. Information regarding names, dates and meeting times of pertinent committees (including Chair of the committees) to facilitate policy approval. d. Names of newsletter editors through whom information can be shared with the Hopkins community. e. A copy of the comprehensive systematic analysis with action items. 3. Difficulties with completion of action items are discussed with the Champion and Surveillance Officer to evaluate issues and removal of barriers preventing change. Sentinel Event Status Reporting 1. The QI Monitor shall meet with and/or communicate regularly with the Champion and the Assistant Director of Quality Improvement to discuss action item progress. 2. The Assistant Director of QI shall update the Sentinel Event database and forward reports regularly to the Director of Quality Improvement, Surveillance Officer and the Sentinel Event Group. 3. The Surveillance Officer shall work with the Champion and the QI Monitor to facilitate the completion of the CSA action items. 4. A presentation on the sentinel event follow up shall be made to the Hospital leadership by the Champion of the sentinel event at regular intervals. Sentinel Event Shared Learning 1. The Chairman of the SEG (or designee) shall report each Sentinel Event and agreed upon action plans at the Quality Improvement Council and the Medical Board. (See QI Plan). 2. The agreed upon action items shall be shared with the individuals involved in the event. Sentinel Event Alerts Copyright 2016 by The Johns Hopkins Health System Corporation and/or The Johns Hopkins University Version 9.0 The Johns Hopkins Hospital Interdisciplinary Clinical Practice Manual Medical Legal Subject Sentinel Event Policy Policy Number MEL014 Effective Date 12/10/2015 Approval Date 11/24/2015 Page Supercedes 5 of 6 12/05/2013 1. H. Regulatory Compliance Committee, Patient Safety Committee and Risk Management Committee distribute copies of each "Sentinel Event Alert" to their committee members. 2. Regulatory Affairs convenes an adhoc group of content experts to review the alert and perform a gap analysis related to current hospital practice and the recommendations in the alert. The gap analysis is presented to Regulatory Affairs Committee and to Risk Management Committee and suggestions for change as a result of the analysis are assigned to applicable workgroups, as pertinent to the alert. Health Care Workers Support 1. The Hospital recognizes that health care workers who are involved in sentinel events are themselves impacted by the event and may require support. For those individuals, the Hospital provides support through the Faculty and Staff Assistance Program (FASAP) (www.Fasap.org.) and the Occupational Health Office. The Hospital also provides support to staff through the "Resiliency in Stressful Events" (RISE) program. The RISE program offers immediate peer support by contacting 410-283-3953. The RISE program is not intended to replace FASAP, but to support staff who are in immediate need of non-judgmental, confidential, peer-to-peer support. VI. REPORTABLE CONDITIONS Health care workers shall report unexpected patient safety events that may be sentinel events to unit leadership and to the Risk Management Department. A report of the event shall be placed in the hospital's event reporting system. VII. DOCUMENTATION The SEG shall require the completion of the comprehensive system analysis and report document within 45 business days from the date the SEG determines a CSA is required. VIII. EDUCATION AND COMMUNICATION This policy will be communicated to the appropriate JHHS personnel via the following channels: 1. 2. 3. 4. Discussion at Risk Management seminars. Nurse Managers, Physician Advisors, Residency Coordinators, Department Chiefs and Department Management will be responsible to train new employees regarding the policy as appropriate, and to communicate updates to the policy. Updates and revisions will be communicated via Medical Staff and Nursing publications. This policy will be placed in the Interdisciplinary Clinical Practice Manual on the JHH Policy website. In the event of web access difficulty, this policy can be found on downtime computers in the clinical areas. IX. SUPPORTIVE INFORMATION See Also: The Johns Hopkins Hospital, Interdisciplinary Clinical Practice Manual • PAT026 Medical Error or Adverse Events Disclosure to Patients and Patients' Surrogates References: The Joint Commission : Sentinel Events Sponsor: • Risk Management Committee Developer: © Copyright 2016 by The Johns Hopkins Health System Corporation and/or The Johns Hopkins University Version 9.0 The Johns Hopkins Hospital Interdisciplinary Clinical Practice Manual Medical Legal Subject MEL014 Effective Date 12/10/2015 Approval Date 11/24/2015 Page Sentinel Event Policy • Policy Number Supercedes 12/05/2013 Risk Management Committee Review Cycle - Three (3) years Medical Board - Approval Date: 11/10/2015 Effective Date: 12/10/2015 X. SIGNATURES Electronic Signature(s) © 6 of 6 Date Redonda Miller Vice President of Medical Affairs, The Johns Hopkins Hospital 03/02/2016 Deborah Baker Acting Vice President of Nursing and Patient Care Services, The Johns Hopkins Hospital 03/02/2016 Copyright 2016 by The Johns Hopkins Health System Corporation and/or The Johns Hopkins University