2015 Issue #2
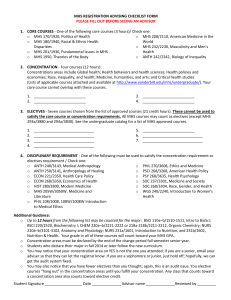
advertisement

Key Stakeholder’s N E W S L E T T E R 2015 Mid-Year Update from Kevin O’Toole With the launch of HIP 2.0 and Hoosier Care Connect this year, Managed Health Services (MHS) has been busy reaching out and connecting with our new membership. Kevin O’Toole MHS President & CEO We have been very pleased to see the notable level of member interaction in the new HIP 2.0 program overall. MHS has seen an increase in member engagement with electronic communications, with gains in online POWER Account contribution payments, as well as in email click through rates to learn more about product, benefit and special programs information. Our new Hoosier Care Connect Care Coordinators are working with members to talk about goals, objectives and interventions to make sure our members have an open line of communication with their providers as well as MHS. And our MHS Community & Member outreach team has already planned and participated in close to 200 events across the state so far this year! As we celebrate our 20-year anniversary this year, we are honored to continue to provide health coverage and personalized services to Hoosiers, and are excited to see what new opportunities lie ahead for MHS in the next 20 years to come. Network Development of MHS Products MHS has been proudly serving Hoosiers for two decades through the Hoosier Healthwise (HHW), Healthy Indiana (HIP) and Hoosier Care Connect Medicaid Programs. MHS has worked to create the largest provider network in our 20 year history, and currently includes an expansive provider network including primary care physicians, specialists and hospitals across the state. If you are a provider who would like to contract with MHS, contact MHS VP of Network Development Bob McDaniel at romcdaniel@mhsindiana.com. N O V E M B E R 2 0 1 5 MHS Partners with MoneyGram to Offer More Ways to Pay for HIP Members MHS is excited to offer another easy way for members to pay their monthly POWER Account Contribution. Members can use MoneyGram to make payments. MoneyGram is fast, convenient and has no fee for HIP POWER Account contributions. To make cash or in person payments, visit any MoneyGram agent location including CVS/pharmacy, Walmart, or Advance America. Find one near you at MoneyGram.com/billpaylocations or call 1-800-926-9400. Learn more about paying bills through MoneyGram at MoneyGram.com/billpayment. To pay your monthly POWER Account Contribution through MoneyGram you will need the following items: • Your POWER Account Invoice • Your Member ID (found on your invoice) • Cash or PIN debit card also accepted at Walmart • MoneyGram Receive Code: 15200 In addition to MoneyGram, MHS gives our members many other easy ways to pay their Fast Track and POWER Account Contributions. • Online using a credit/debit card at mhsindiana.com • By mail with check, money order or credit/debit card to: Managed Health Services Member Mailstop 16253487 PO Box 660160 Dallas, TX 75266-0160 * include payment voucher from bottom of invoice with lockbox payment submission • By phone with credit/debit card at 1-877-647-4848 • Electronic Funds Transfer • Payroll deductions by your employer mhsindiana.com • 1-877-647-4848 Hoosier Care Connect Update Hoosier Care Connect is a new coordinated care/managed care program for Indiana’s Medicaid enrollees with a disability who are not Medicare eligible and do not have an institutional level of care. Through Hoosier Care Connect, FSSA continues to improve the quality of care and health outcomes for members, seeking to achieve the following goals: • Improve quality outcomes and consistency of care across the delivery system • Ensure enrollee choice, protections and access • Coordinate care across the delivery system and care continuum • Provide flexible, person-centered care • Transition planning, contract oversight and implementation issues MHS is one of three managed care entities selected to provide coordinated healthcare services through Hoosier Care Connect. We were assessed on factors such as experience serving complex populations and our approach to care management. Hoosier Care Connect launched on April 1, 2015. The transition and go-live was smooth, and MHS has begun reaching out to members on the phone and electronically, as well as out in the community. Hiring and system changes also occurred. In order to help grow the population cared for by Hoosier Care Connect, MHS is meeting with various nonprofit organizations and Centers for Independent Living (CILs). We are also starting more marketing campaigns about the program, including commercials. Care Coordination and Children with Special Needs Program MHS offers several specialized health programs for our members’ care management needs, including diabetes, COPD and asthma. We also offer a “Children with Special Needs” program for children with developmental disorders or chronic health conditions. Each MHS member is assigned a care coordinator, who is a BSW, LSW or LPN. We have no less than quarterly contact with each member, and we also integrate with our case management team for members with unstable conditions. Our case management RNs and LCSWs are field based and schedule face-to-face meetings with members depending on their condition. We may also accompany members to physician appointments to help our members understand what they are supposed to do and help the physician understand what the member’s needs are. We also work closely with the Department of Child Services’ case managers for children in foster care or adoption assistance to help them work through the system and get the proper healthcare they need. The MHS Children with Special Needs program was developed to improve our members’ and their families’ knowledge of various developmental disorders and to assist them in transitioning to and establishing a medical home. MHS Education Network MHS has partnered with accessABILITY Center for Independent Living to serve Hoosier Care Connect members in Marion County with the MHS Education Network. Hoosier Care Connect members are very engaged in their healthcare and may have questions, so MHS has partnered with accessABILITY to answer those questions. The Network will work to provide in-person specialized education to Hoosier Care Connect members on a variety of topics, such as the scope of health plan benefits, how to access care and our members’ rights and responsibilities. We use methods that are clear, concise and accurate and reflect the cultural, language and other special needs of our specific populations. Components of the MHS Education Network include: • Benefit education • Health Needs Survey completion (if applicable) • Materials include: • PMP selection (if applicable) - 80-slide deck • Member Satisfaction Survey - Member handbook - CentAccount flyer - Portal flyer - Copy of member ID card MHS is working on training for staff. Because cultural competencies are important, our staff needs to be prepared for helping these members. So far, training has been going great! AccessABILITY has been able to connect with some consumers due to connections employees have with the community. There is also a process in place by which MHS call center staff can refer members to accessABILITY for additional information when necessary. mhsindiana.com • 1-877-647-4848 0715.MA.O.NL 07/15