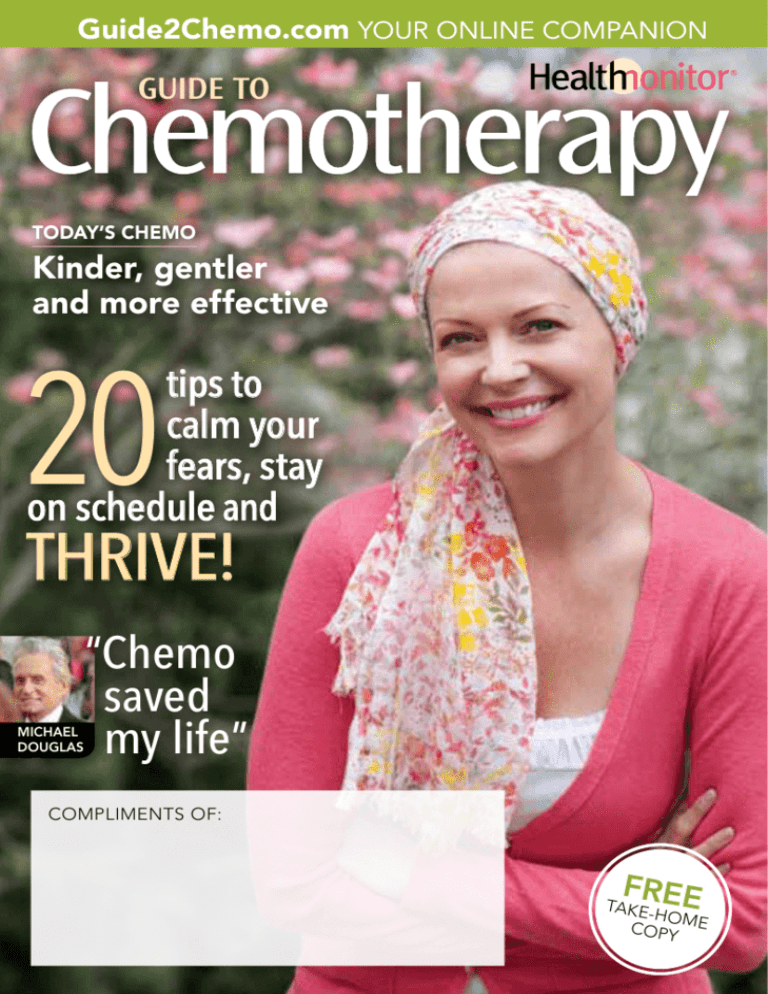
Guide2Chemo.com YOUR ONLINE COMPANION
GUIDE TO
TODAY’S CHEMO
Kinder, gentler
and more effective
20
tips to
calm your
fears, stay
on schedule and
THRIVE!
MICHAEL
DOUGLAS
“Chemo
saved
my life”
COMPLIMENTS OF:
FREE
TAKEHO M
COPY E
table of contents
letter from the editor
Welcome!
If you’re about to start
chemotherapy, your head may be swimming with
questions and concerns. Will I feel ill? Will I be able
to work? Will I be able to care for my family? The
good news is that today’s chemo is more effective—
and more livable than ever. You may be surprised to
discover, for instance, that the side effects you experience are milder than you anticipated. And your chemo
care team will help you manage any symptoms that do
occur so you can stick to your treatment schedule.
To help you along the way, we asked three cancer
experts for the most up-to-date info to help you on
your journey. Read on to learn everything you need to
know about how chemo works and how to thrive during treatment. Our goal is to instill in you the knowledge and confidence that will help you get the best
benefit from your treatments and get on with your
next chapter.
—From the editors at Health Monitor
4 Get back to the life you love
Chemo is your bridge to the future
6 Top questions about chemo
10 Staying the course
Adhering to your treatment schedule
can get you the best results from chemo
16 Understanding your
blood counts
17 The side effects you
must know about
18 Conquering chemo anxiety
Overcome anxiety and de-stress
before your first session
SPECIAL PULLOUT SECTION
Your chemo calendar, questions to ask
20 Chemo mentors
How a support group can help
Zen inspiration
for your journey
Repeating a gatha (a short
verse) daily can help you
find peace, calm and confidence, says Zen master
Thich Nhat Hanh. One
chemo patient repeats this
one, written by her son:
“I will be healthy.
I will heal.
I will survive.
I will thrive.”
To learn more about Thich Nhat
Hanh and living mindfully, visit
plumvillage.org.
22 Circle of support, chain of love
One woman’s mission to spread hope
24 Get the nutrition you need
28 Thrive during treatment
20 tips for taking care of your
body, mind and spirit
33 Don’t forget about
“date nights”
How to keep the intimacy during chemo
34 Chemo and your job
Tips to make it work
36 Understanding cancerspeak
Words of inspiration
from our medical review board
“Chemo works like an
antibiotic—it kills off
something that you
don’t want in your body
because it’s making you ill.”
—Lillie Shockney, RN, administrative director
of the Johns Hopkins Avon Foundation
Breast Center and the Johns Hopkins Cancer
Survivorship Program
“Rest assured that
what you’ve heard
about chemo is probably
not true!”
—Theodore Tsangaris, MD, chief of breast
surgery at Johns Hopkins
“New advances help
combat chemo side
effects like nausea,
making it easier to stay
on schedule and get the full benefit
of therapy.”
—Marc B. Garnick, MD, clinical professor of
medicine, Harvard Medical School
! Web Extra!
Be sure to visit
Guide2Chemo.com for
more useful tools and
information.
All the terms you need to know
®
This publication is not intended to provide advice on personal medical matters, or to substitute for
consultation with a physician. Health Monitor Network is the nation’s leading patient-education publishing company, with 10 publications
available in doctors’ offices, including Living with Cancer. For more information: Health Monitor Network, 135 Chestnut Ridge Road, Montvale,
NJ 07645; 201-391-1911. ©2011 Data Centrum Communications, Inc.
the journey begins
Getting back to the life you love!
Think of chemo as a strong ally—the healing therapy
that will take you to your new life after cancer.
O
f all the facts you should know
about chemo, here’s the most
important: It may be your single best
chance to rid your body of cancer cells.
But to get the maximum benefit from
your chemo, it’s critical to complete your
treatments on schedule.
Luckily, you don’t have to go it alone.
With this guide, you’ll get input from
people like 75-year-old Zeva, who is now
undergoing chemo. “One minute, you’re
fine; the next, your life has changed. But
you really can’t think negatively…you
have to be upbeat, and remember that
when the chemo goes in, it’s doing what
it’s supposed to do.”
So what will chemo be like? How
will you feel? How will it affect your
daily routine? While everyone reacts
differently, one thing is for sure: Today’s
chemo is gentler and more effective
than ever.
Many people are able to work and take
care of their families throughout their
treatment. And there are plenty of medications that can help ease chemo side
effects—if they occur.
To learn more about chemo—what it
4 Health Monitor Guide to CHEMOTHERAPY
is, how it works and how to feel your best
throughout your treatment—make yourself comfortable and spend some time
reading this guide. Becoming informed
about the process will help you work
effectively with your doctors and stay on
schedule. That’s the key to getting every
bit of restorative power from chemo—and
getting back to the life you love.
STAR TALK
Plus-size model
Emme [Aronson]
Hodgkin’s lymphoma survivor
How it was treated:
surgery and chemotherapy
How she coped: “Cancer isn’t
something anyone should try to go
through alone,” she has said.
“I had 12 chemo buddies. Each
one of them gave
up a day to be
with me.”
Best advice:
“No matter what
life throws at
you, you can
handle it.”
chemotherapy 101
Top 10
chemo questions
–answered
F
2
orget what you may have heard
about chemo. This type of cancer
therapy has come a long way since it was
first introduced more than half a century
ago. Read on for the latest on these
powerful medications.
1
How does chemotherapy
work? It kills cancer cells, reduces
the size of tumors and relieves symptoms
of the disease. In most cases, a cocktail
of two or more medications is used,
although certain cancers can be treated
with a single drug. While chemo also kills
some healthy cells, most of those cells
eventually repair themselves.
! Web Extra!
Thinking of getting a
wig? Find surprising tips
to make your decision
easier at Guide2Chemo.
com/wig
6 Health Monitor Guide to CHEMOTHERAPY
How is it given? In a few
instances, chemo is taken in the
form of a pill, liquid or injection (or, in
the case of some skin cancers, by topical
cream). However, in most cases it’s given
intravenously through a needle inserted
into a vein in your hand or lower arm,
a procedure known as an infusion. Ask
your doctor if you can get a catheter
(a thin tube) with a port, which makes
needle insertion easier. Sometimes the
medication leaks into the surrounding
tissue, causing pain as the drugs flow
through the IV. If that happens to you,
simply alert your infusion nurse.
3
How frequently will I
need it? It depends on the
type and stage of your cancer and the
medications in your regimen, but it can
be once a day, once a week, once every
10 days or even once a month. When
remission or prevention of recurrence
is the goal, chemo usually lasts three to
12 million
Your CHEMO TEAM
During treatment, you’ll be cared for
and supported by a variety of medical
professionals, including your:
!"Medical oncologist, a physician
who determines the drugs you need
and your schedule.
! Oncology nurse, a specialized
nurse who may administer your
chemo.
!"Oncology nutritionist, who
can help you plan menus during
your treatment.
cancer survivors
are living in the U.S.
today—more than ever.
And chemo advances
are part of the
reason.
!"Oncology social
worker, who can
assist you with psychosocial and
financial needs.
! "Phlebotomist, who will draw
blood whenever tests and procedures
are needed.
! Physical therapist, who can help
you find appropriate exercise during
treatment.
Guide2chemo.com
7
chemotherapy 101
six months. If the goal is to shrink your
tumor and ease symptoms, there is no
time frame.
4
Will it make me feel
sick? Many patients say they
feel perfectly fine. Even if you do
experience side effects, they can be
alleviated with medication. “We have
very good antinausea drugs now,”
says Sanjay Goel, MD, an oncologist
at Montefiore Medical Center in New
York City. Other side effects include
fatigue and infection brought on by a
low white blood cell count. Alert your
doctor if you have a fever over 100.5°,
uncontrolled vomiting, diarrhea, or
abnormal bleeding or bruising. (See
page 16 to learn how a CBC blood test
can help your medical team monitor
your progress.)
5
Will I be able to eat? Yes.
Aim for small, frequent meals and
high-protein snacks such as peanut butter
crackers, cheese and milk shakes. Stay
hydrated with plenty of water and juice.
And note when your appetite peaks—you
may be able to sneak in a big breakfast,
say, before symptoms hit later in the day.
6
Will I lose all my hair?
Not necessarily, although many
medications do cause hair to thin or fall
out. That includes eyebrows, body hair
and pubic hair. Take charge by cutting
8 Health Monitor Guide to CHEMOTHERAPY
WHAT ABOUT A
CLINICAL TRIAL?
Clinical trials allow doctors to test the
safety and effectiveness of new drugs
or combinations of drugs. The decision to enroll in a clinical trial is very
personal—one you should consider
carefully after discussing the pros and
cons with your healthcare provider.
The goal of most trials is to yield improvements in survival, side
effects and convenience, with the
hope that outcomes are at least as
good as standard treatments. Log on to
cancer.gov/clinicaltrials to learn more.
your hair short or shaving it off. You
can wear a cap, scarf or wig. When your
treatment is over, your hair will grow
back. It’s often curly at first; it will return
to your normal texture soon.
7
If I get infusions, how
long will each one last,
and what can I do to pass
the time? A session can last
anywhere from a few hours to most of
the day, says Dr. Goel. At many chemo
centers, patients talk to pass the time; it’s a
great way to find support and make new
friends. But you can also watch a movie,
listen to relaxing music or read a book.
8
What if I’m too tired to get
chemo? It’s important to stay on
the schedule your doctor has prescribed,
says Dr. Goel. If you skip a treatment,
cancer cells could regrow, and your chances
of remission will drop, he says. Ask your
doctor what you can do about fatigue and
any other troublesome side effects, and ask
a friend to take you to your appointments.
9
Can I work during chemo?
Yes, most people can. “Many patients
want to maintain as much normalcy as
possible, so they like to continue their
regular work schedule,” says Dr. Goel. If
you’re tired after treatment, talk to your
boss about reducing your hours or taking
off a day or two after a chemo session.
Remember, if you work for a public
agency, a school or a company with more
than 50 employees, you’re protected by
the Family Medical Leave Act, which
guarantees you 12 weeks of unpaid leave
without risking your job.
10
Will I feel better as soon
as my course is over? Yes.
In fact, many of the most frustrating side
effects—nausea, loss of appetite and hair
loss—will vanish a few weeks after your
last session. Although it can take longer to
shake the last remnants of fatigue and pain,
exercise and yoga can help. If you continue
to have muscle pain or tingling in your
fingers and toes, talk to your doctor.
—Marisa Cohen
STAR TALK
Actor
Michael Douglas
Stage IV throat cancer
survivor
How it was treated: chemotherapy and radiation
How he coped: “I took
[my children] down to a
couple of radiation treatments. They thought it
was cool, you know, all
this space-age stuff. It
made up for all those days
when Dad was lying on
the couch.”
Best advice: Michael has
said that he cherishes his
new life since beating
cancer. “I have a much
deeper
appreciation of my
friends
and
family.”
! Web Extra!
Caring for someone
undergoing chemo?
Get expert tips and advice
for helping your loved one
cope at Guide2Chemo.
com/caregiving
Guide2Chemo.com
9
on schedule
Staying the course
You can keep your chemo sessions going smoothly and help ensure the best results with these simple steps.
>
Before
chemo begins
!"Attend a chemo class.
>
Most cancer centers offer a
pre-chemo education program to prepare you.
!"Get regular care and
screenings. Take care of
dental work and get any
exams you’re due for, such
as a Pap or colonoscopy.
!"Consider having a
port implanted. Needles
are inserted more easily
through a port than directly through the skin.
!"Stock up on these essentials. Face and body lotion,
lip balm and nasal gel to
combat dryness; products
that fight dry mouth.
Start right!
Infection due to a low
white blood cell count
is the most common
cause of treatment delays, so ask your doctor
how to avoid
infection.
Before
each session
>
!"Drink water. The infusion nurse will be able to
find your veins more easily if there’s fluid in your
system. Drink about 10
8-oz. glasses of water the
day before.
!"Ask about numbing
cream. If you have a port,
ask your infusion nurse to
recommend a cream that
will make infusions more
comfortable and how to
care for your port at home.
During
your session
!"Visualize your chemo
working! Try envision-
ing your chemo drugs
searching and destroying
the cancer cells in your
body. Studies show visualization may help relieve
anxiety, boost your spirits and even rev your immune system temporarily. It just may help you
walk out of your session
feeling more positive and
in control.
>
Before
you leave
!"Get post-infusion
instructions. Are there
medications you’ll need?
Some patients get an injection the day after chemo
of a colony-stimulating
factor (CSF) medication.
This drug helps keep your
white blood cell count at
a healthy level, so you can
avoid infections and stay
on schedule with your
chemotherapy. If you’ll
need this, make sure you
have a prescription.
!"Double-check the date
How does your doctor
plan your treatment?
Which chemo drugs will help rid your body of cancer…in
what doses… how often? The answers are different for
each person. Your doctor will decide what’s right for you
by weighing various factors, including the type of cancer
you have, its stage, and your weight or body surface
area. As your chemo progresses, it’s not unusual for your
doctor to further fine-tune your formula depending on
your body’s response.
>
and time of your next
appointment. Then mark
it on your calendar!
There’s more!
See “What to
bring to your chemo
treatments” in the
tear-out section of this
guide for more
practical
tips.
Before
next
appointment
!"Watch for signs of infection! (See “Infection
alert!”)
!"Keep a log. Throughout
your treatment, record
any symptoms on your
chemo calendar. (See
“Use your calendar
wisely” in the tear-out
section.) It will help you
talk to your doctor about
your progress.
Infection ALERT!
Infection can stall your chemo schedule.
If you develop any of these signs
of an infection, contact your doctor
right away:
" fever above 100.5° orally, sudden chills,
sore throat
" new cough or shortness of breath
" nasal congestion
" pain or burning when you urinate
" diarrhea or uncontrolled vomiting
" new onset of pain, especially in your back
" redness, swelling, pain and warmth at the
site of an injury or an IV site
" abnormal bleeding or bruising
Guide2chemo.com
11
Help boost your
natural defenses
with
®
Neulasta (pegfilgrastim)
Ask your doctor if Neulasta® should be a part
of your overall treatment plan
Chemotherapy can lower
your white blood cell count,
raising the risk of infection.
“Yes, I have cancer. And cancer may mean chemotherapy. My doctor
told me strong chemo could lower my white blood cell count, putting me at risk
for infection.
Neulasta®, injected 1 day after every cycle of my chemotherapy, helped boost
my white blood cell count and helped reduce my risk of infection. Your results
may vary.
Before you start chemotherapy, ask your doctor if Neulasta® should be a part
of your overall treatment plan.”
Visit Neulasta.com for more information.
Neulasta® is a prescription medication used to reduce the risk of infection
(initially marked by fever) in patients with some tumors receiving strong
chemotherapy that decreases the number of infection-fighting white blood cells.
Neulasta® may not prevent all infections.
Please see Important Safety Information on the following page.
The Neulasta FIRST STEP® co-pay coupon program can help eligible commercially
insured patients meet their Neulasta® deductible, co-insurance, and/or co-payment
(out of pocket) requirement. Log on to www.AmgenFIRSTSTEP.com or call
1-888-657-8371 for a complete list of eligibility requirements and restrictions.
Neulasta® can help boost
your white blood cell count—
your body’s natural defenses.
Important Safety Information
Do not take Neulasta® if you have had an allergic reaction to Neulasta® or to
NEUPOGEN® (filgrastim). Tell your doctor if you have sickle cell disorder before
using Neulasta®. Ruptured spleen (including fatal cases), a serious lung problem
called acute respiratory distress syndrome (ARDS), serious allergic reactions,
and sickle cell crises can occur. Call your doctor or seek emergency care right
away if you have: pain in the left upper stomach area or left shoulder tip pain
(symptoms of an enlarged or ruptured spleen); shortness of breath, trouble
breathing, or a fast rate of breathing (symptoms of ARDS); shortness of breath,
wheezing, dizziness, swelling around the mouth or eyes, fast pulse, sweating,
and hives (symptoms of an allergic reaction); or if you have pain or difficulty
breathing (symptoms of sickle cell crises). The most common side effect you may
experience is aching in the bones and muscles.
If you have any questions about this information, be sure to discuss them with
your doctor. You are encouraged to report negative side effects of prescription
drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please see important product information
for patients on the following page.
BRIEF SUMMARY OF PATIENT PACKAGE INSERT
Neulasta®
(pegfilgrastim)
This brief summary of the patient package insert provides information and instructions for people who will be receiving
Neulasta or their caregivers. This brief summary does not tell you everything about Neulasta. You should discuss any
questions you have about treatment with Neulasta with your doctor.
What is Neulasta?
Neulasta is a man-made form of granulocyte colony-stimulating factor (G-CSF), which is made using the bacteria
E coli. G-CSF is a substance produced by the body. It stimulates the growth of neutrophils (nu-tro-fils), a type of
white blood cell important in the body’s fight against infection.
Who should not take Neulasta?
Do not take Neulasta if you have had:
s!SERIOUSALLERGICREACTIONTO.EULASTA® (pegfilgrastim) or to Neupogen® (filgrastim).
What important information do I need to know about receiving Neulasta?
Occasionally pain and redness may occur at the injection site. If there is a lump, swelling, or bruising at the injection site
that does not go away, talk to the doctor.
Neulasta should only be injected on the day the doctor has determined and should not be injected until approximately
24 hours after receiving chemotherapy.
The needle cover on the single-use prefilled syringe contains dry natural rubber (latex), which should not be handled
by persons sensitive to this substance.
What should I tell my healthcare provider before taking Neulasta?
What are the most common side effects of Neulasta?
The most common side effect you may experience is aching in the bones and muscles. If this happens, it can usually be
relieved with a non-aspirin pain reliever, such as acetaminophen.
What about pregnancy or breastfeeding?
Neulasta has not been studied in pregnant women, and its effects on unborn babies are not known. If you take Neulasta
while you are pregnant, it is possible that small amounts of it may get into your baby’s blood. It is not known if Neulasta
can get into human breast milk. If you are pregnant, plan to become pregnant, think you may be pregnant, or are
breastfeeding, you should tell your doctor before using Neulasta. If you become pregnant during Neulasta treatment,
you are encouraged to enroll in Amgen’s Pregnancy Surveillance Program. You should call 1-800-77-AMGEN
(1-800-772-6436) to enroll.
How should Neulasta be stored?
Neulasta should be stored in the refrigerator at 2° to 8°C (36° to 46°F), but not in the freezer. Neulasta should be
protected from light, so you should keep it in its carton until you are ready to use it. Avoid shaking Neulasta. If Neulasta
is accidentally frozen, allow it to thaw in the refrigerator before injecting. However, if it is frozen a second time, do not
use. Neulasta can be left out at room temperature for up to 48 hours. Do not leave Neulasta in direct sunlight. For all
questions about storage, contact your doctor, nurse, or pharmacist.
What are the ingredients in Neulasta?
Each syringe contains pegfilgrastim in a sterile, clear, colorless, preservative-free solution containing acetate, sorbitol,
polysorbate 20, and sodium.
If you have a sickle cell disorder, make sure that your doctor knows about it before using Neulasta. If you have a sickle
cell crisis after getting Neulasta, tell your doctor right away.
If you have any questions, talk to your doctor.
What are possible serious side effects of Neulasta?
sSpleen Rupture. Your spleen may become enlarged and can rupture while taking Neulasta. A ruptured spleen can cause
death. The spleen is located in the upper left section of your stomach area. Call your doctor right away if you have pain in
the left upper stomach area or left shoulder tip area. This pain could mean your spleen is enlarged or ruptured.
sA serious lung problem called Acute Respiratory Distress Syndrome (ARDS). Call your doctor or seek emergency
care right away if you have shortness of breath, trouble breathing, or a fast rate of breathing.
sSerious Allergic Reactions. Neulasta can cause serious allergic reactions. These reactions can cause shortness of
breath, wheezing, dizziness, swelling around the mouth or eyes, fast pulse, sweating, and hives. If you start to have
any of these symptoms, call your doctor or seek emergency care right away. If you have an allergic reaction during
the injection of Neulasta, stop the injection. Call your doctor right away.
sSickle Cell Crises. You may have a serious sickle cell crisis if you have a sickle cell disorder and take Neulasta.
Serious and sometimes fatal sickle cell crises can occur in patients with sickle cell disorders receiving filgrastim,
a medicine similar to Neulasta (pegfilgrastim). Call your doctor right away if you have symptoms of sickle cell crisis
such as pain or difficulty breathing.
Neulasta® (pegfilgrastim)
Manufactured by:
Amgen Inc.
One Amgen Center Drive
Thousand Oaks, California 91320-1799
This product, its production, and/or its use may be
covered by one or more US Patents, including US
Patent Nos. 5,824,784; 5,582,823; 5,580,755,
as well as other patents or patents pending.
© 2010 Amgen Inc. All rights reserved.
www.neulasta.com
1-800-77-AMGEN (1-800-772-6436)
v 8.0
65494-R1-V5
MC38484-E-1
on schedule
The BLOOD TEST that
helps keep your chemo on track
>>
When you’re on chemo,
getting a blood test called
a CBC (complete blood
count) becomes part of the
routine. It’s usually done
right before you get your
chemo and then about two
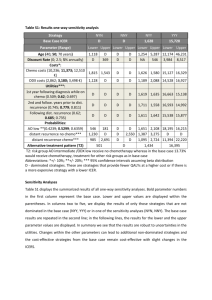
Type of cell
Red
blood
cells
White
blood
cells
Platelets
weeks later. The reason?
The same drugs that help
rid your body of cancer
can also cause levels of
your blood cells to dip. A
CBC gives your doctor a
comprehensive look at the
type and number of cells in
your blood—particularly,
your red blood cells, white
blood cells and platelets. He
can prescribe medication to
boost low blood counts and
help you stay on course.
Function
Normal range
Transport
oxygen-rich
hemoglobin
through your
body.
4.7 to 6.1
million cells/
mcL (male);
4.2 to 5.4 million cells/mcL
(female)
A low red blood cell count means
you are anemic and that your
body has to work much harder
to supply oxygen to your tissues.
This can leave you feeling tired
and short of breath.
Help protect
your body
against
infection.
4,500 to
10,000 cells/
mcL
If levels of neutrophils, a type of
white blood cell, are too low, you
have neutropenia, a condition that
makes you vulnerable to infection.
Cause your
blood to clot.
150,000 to
400,000
platelets/mcL
If your count is out of range
If your platelet count is too low, you
may not be able to stop bleeding.
Alert!
Be sure to have your
blood tested per your doctor’s orders during your
treatment—and report
symptoms such as extreme
fatigue or dizziness, chills
or sudden onset of new
pain ASAP.
Source: National Institutes of Health
! Web Extra!
Undergoing chemo? Keep track of your
sessions, test results and more with our chemo
calendar at Guide2Chemo.com/calendar
THE OTHER
SIDE EFFECTS of chemo
Outsmarting
While you may be gearing
up for nausea and hair loss,
you may be unprepared for
these chemo side effects.
Here’s what to know to stay
well—and stay on track.
Neutropenia
Chemo can cause white
blood cells to plummet to
abnormally low levels, a
condition called neutropenia.
Since white blood cells fight
off infections, it’s vital that
they remain in the normal
range so you can remain on
your chemo schedule.
REPORT: Any signs of
infection, including fever,
chills and aches.
WHAT YOUR DOCTOR
CAN DO: Prescribe medi-
cation that elevates white
blood cell levels.
WHAT YOU CAN DO:
Wash your hands often,
stay away from sick people
and avoid procedures, dental work or vaccinations, all
of which can increase your
infection risk.
Anemia
Some chemo drugs can
lower your red blood cell
count, causing anemia.
REPORT: Fatigue, weakness, dizziness, shortness
of breath.
WHAT YOUR DOCTOR
CAN DO: If your anemia
is severe, he may recommend a drug or a blood
transfusion to boost your
red blood cell count.
WHAT YOU CAN DO: Rest
when you need to, eat well
and exercise when you feel
up to it.
Peripheral
neuropathy
Some chemo drugs can
damage nerves in your
hands and feet, known as
peripheral neuropathy.
REPORT: Numbness, tingling or a “pins and needles”
sensation in your hands and
feet; loss of balance.
WHAT YOUR DOCTOR
CAN DO: Prescribe a pain
reliever; adjust your chemo.
WHAT YOU CAN DO:
Avoid extreme temperatures, protect hands and feet
and check daily for wounds.
WHAT’S CHEMO BRAIN?
Some chemo patients say they feel like they’re
in a fog, forgetting things, misplacing objects or
having trouble expressing themselves. But chemo
drugs aren’t always the sole culprit—low blood
counts, stress, hormonal changes and nutritional
deficiencies may play a role. Since medication
can help, mention the problem to your
healthcare team. And scan this guide
for tips that help you relax—they can
help ease chemo brain, too.
Guide2Chemo.com
17
support strategy
Conquering
chemo anxiety
W
hen you’re preparing for treatment, it’s natural
to feel anxious. But remember, millions have
gone through chemo and are doing great. They may even
include your neighbors, friends and co-workers. Here, a
few chemo veterans share the strategies that kept their
stress low and their spirits high throughout treatment.
Talk it out. “After surgery and chemo, I
started seeing a therapist and stuck with
her for a year and a half. It helped that
she was not ‘family.’ I could share
anything with this person,” says
Jacki, who underwent treatment for
breast cancer several years ago.
WHY IT WORKS: “Therapy can offer
you a safe place to express feelings
you may not be comfortable sharing
with loved ones,” says Erin M. Rafter,
PhD, a psychologist at The Gathering
Place in Westlake, OH. “A professional can help you learn
coping strategies and different perspectives to help
you through the process
of treatment.”
TO TRY IT: Contact CancerCare (800-813-4673,
cancercare.org) for free phone counseling or
referrals to resources in your community.
Take a stroll, walk the dog, go to a put-
ting green. “I didn’t want to go out and see my
friends or do anything,” says Sally, a colon cancer survivor. “Then my neighbor friend took
me for a walk. Wow! There’s no question that it
helped my mood.”
WHY IT WORKS: The latest guidelines from the
American Council on Sports Medicine urge
people undergoing chemo to exercise as much
as those not going through the treatment—
about two and a half hours a week. Studies show
getting in some physical activity can reduce
anxiety, preserve strength and counter fatigue.
TO TRY IT: It’s as easy as taking a walk, but if
you prefer more structured activity, try an exercise program designed especially for cancer
patients (check with your hospital). And clear
any program with your oncologist.
Say yes to help. “People will come out
of the woodwork to help,” says Irene, a one-year
cancer survivor. “Do not be too proud to take
them up on their offers.”
WHY IT WORKS: “Accepting help is not a sign
of weakness; it is a sign of friendship,” says Lillie
Shockney, RN, MAS, a two-time breast cancer
survivor and the administrative director of the
Johns Hopkins Clinical Breast Programs and
Cancer Survivorship Programs. “Make a list of
the errands you will need help with. Ask people
to fix casseroles you can freeze.” Leaning on others to handle small daily hassles relieves stress
and enhances the healing process.
Reassurance
from folks who’ve
been there
We found these encouraging words on cancer blogs
and forums.
“They give you meds that
control the nausea. Other
than being tired the first
week after treatment, I
have done pretty well.”
– Jane S.
“Life will be good again—
not quite the same, but
you will appreciate things
that you didn’t before.
Before you know it, you’ll
have your life back.”
– Pat D,
“The chemo suite is a
very calm place with caring and experienced staff.
There are usually other
patients around to talk to
and after a while, it feels
very familiar and safe.”
– Susan F.
! Web Extra!
Get moving to reduce
stress with these
gentle treatmentfriendly exercises at
Guide2Chemo.com/yoga
Guide2Chemo.com
19
support strategy
Chemo mentors
Get the inside scoop on everything from hair loss
to early menopause from Haralee and Crystal,
survivors who spread help and encouragement.
“My support group
helped me anticipate
side effects and told me
about clinical trials.”
H
—Haralee Weintraub, 58,
Portland, OR
aralee Weintraub, who was
diagnosed with breast
cancer at 48, joined a support
group just before her second chemo
treatment began. “The women helped
me to anticipate side
effects, such as joint
stiffness,” she recalls.
“When I heard what
other women were
experiencing, I wasn’t as
scared.” She also found
their words comforting,
since some of the
women were 15 or more
years out of treatment.
Through her support group, Haralee also
20 Health Monitor Guide to CHEMOTHERAPY
learned about clinical trials that were
recruiting breast cancer patients. “I
participated in six of them,” she says.
One was for a new chemo medication,
and the others involved exercise, bone
density, falls and vision. “My oncologist
could have told me about the trials, but
I didn’t see him as often as I saw the
women in my support group,” she says.
The group played another key role
for Haralee—as an unofficial focus
group for her new business venture.
When chemo threw her into menopause with drenching night sweats, she
sewed a nightie out of wicking fabric
meant for athletic wear. “I brought a
couple of prototypes to my support
group, and the women went wild
with enthusiasm,” says the owner of
the company she named after herself,
Haralee (“Cool Garments for Hot
Women”). Two members modeled the
sleepwear for a photo shoot. “They
helped me so much,” she says. “Now I
want to help other patients.”
“Survivors reassured
me that my hair would
go back to normal.”
W
—Crystal Brown-Tatum, 43,
Shreveport, LA
hen Crystal Brown-Tatum
learned she had breast
cancer in 2007, she dreaded the
thought of chemotherapy. “Everything
I knew about it came from TV and
movies,” says the owner of a public
relations firm. So when her doctor
told her that she’d need chemo, she
was devastated.
Luckily, Crystal heard about the
Sisters Network (sistersnetworkinc.org),
a national support group for African
American women with breast cancer.
Women in her local chapter comforted
her, reassuring Crystal that the side
effects wouldn’t be as bad as she feared.
“The morning before my first chemo, I
called one of the women in the group,”
she says. “Her reassurance was the
motivation I needed.”
Group members also shared tips,
such as to ask her doctor for a prescription mouth rinse if she developed
mouth sores and to wear cotton gloves
to bed if her hands got cold (a symptom of peripheral nerve damage).
“Their support meant the world
to me,” she says. “Everyone needs a
chemo mentor.”
—Beth Howard
Guide2Chemo.com
21
support strategy
Circle of support,
chain
of love
B
efore starting chemo seven years
ago, Jacki Donaldson had a
special wig made up—cotton on top,
human hair on the sides, designed to
be worn with hats or scarves: “I loved
the thought of a baseball cap on top
of hair that looked real.” The wig was
so well made, in fact, that a neighbor
commented on how great it was that
Jacki had not lost her hair.
Little did she know her “underhair”
would eventually travel the U.S.,
bringing hope and happiness to other
women going through chemo.
The blog begins
The journey started back in 2004, when
Jacki, then 34, found a lump in her breast.
As she got her diagnosis and embarked on
treatment, concerned friends and family
22 Health Monitor Guide to CHEMOTHERAPY
Breast cancer survivor
Jacki Donaldson started a
blog to keep loved ones in the
loop. Now it’s leading others
on the path from cancer and
chemo to good health.
kept checking in on her. That’s when her
husband prompted her to start a blog—
something she knew nothing about—to
keep her loved ones up to date. It wasn’t
long before Jacki was posting like a pro
on “my Breast Cancer blog” (cancerspot.
org) and reaping an unexpected benefit: “I
was able to process everything I was going
through and feel better,” she says.
Things like finding her cancer while
showering: “I knew it was not normal.
It was hard and felt like a small green
pea.” Things like getting her first chemo
treatment: “The chemo is done for today.
I’ve had fluids, antinausea medication
and the chemo drugs, and now I’m
home. The whole process took about
four and a half hours.” Things like losing
her hair: “I think my morning routine
is going to be much quicker now. I just
have to put my hair on—instead of
drying it, curling it, styling it.”
Seeing the silver lining
Quite unexpectedly, blogging gave
Jacki a purpose: “[Through my blog]
other people are finding me—like other
survivors and loved ones of cancer
patients…the disease begins looking more
like a gift than a curse.” It even launched
a writing career and widened her circle
of support: “I hear from someone every
day—it might be a comment on this site
or a personal email. Something might
arrive in the mail or someone might call
to check on me. It keeps me going. It
lifts my spirits in moments of weakness.
It reminds me of the power of love and
friendship. It’s the best medicine—and
the best side effect—so far.”
Paying it forward
Now that she’s cancer-free, “my Breast
Cancer Blog” has become a vehicle for
spreading her optimism: “My goal is to
share the hope with people early in their
journey.” She also shares her underhair,
sending it to some of her blog readers
as they prepare for their own treatment.
It’s traveled to Florida, Ohio and now to
TIP!
To find out how
to start a blog
like Jacki’s, visit
Guide2Chemo.
com
Michelle in Vienna,
VA. “This wig brought
me peace when my
world was crumbling. I
think it will do the same for
whoever is in line next.”
No blog?
PEN AND PAPER
WILL DO!
No matter how you choose to
express your thoughts and feelings—online or in a diary—you
stand to benefit: Cancer patients
who journaled before chemo responded better emotionally and
physically, according to a study
in the journal Oncologist. What’s
more, writing about your personal experiences helps improve
memory and sleep and boosts the
immune system.
Guide2chemo.com
23
feel your best
Get the nutrition
you need!
O
ne way to feel your best during chemo? Eat a wholesome
diet. “You have to eat well in order to heal well,” says
Sharlene Bidini, RD, CSO, a certified specialist in oncology nutrition
in Dearborn, MI. Of course, that’s easier said than done when
challenges like nausea and appetite loss make it hard to eat. Luckily,
there’s a solution to those and other dietary dilemmas...
(American Cancer Society, 2010). Not a
fan of the curds? Consider milkshakes,
puddings, custards and eggs. On the go?
Tote snacks like granola or energy bars,
crackers with cheese or peanut butter, or
small boxes of raisins.
!Avoid
mouth dryness with moist
foods. “Wet” foods, like casseroles,
!"Boost
your appetite with
cottage cheese. Solo, or flavored
with fruit, it boosts calories and protein
intake so you maintain lean muscle and
keep up your strength, says Cynthia A.
Thomson, PhD, RD, CSO, co-author of
the American Cancer Society’s Complete
Guide to Nutrition for Cancer Survivors
24 Health Monitor Guide to CHEMOTHERAPY
scrambled eggs, soup, yogurt and pudding can help, says Bidini, who also
recommends rinsing often with this
homemade mouthwash. Unlike commercial products, it is gentle on soft
mouth tissues:
To one quart of water add a teaspoon
each of salt and baking soda; mix thoroughly. (Store in a cool, dry place—no
need for refrigeration. Discard unused
solution after 24 hours.)
!"Outsmart
constipation with
fiber-rich nuts, seeds and fruits
!"Relieve
diarrhea with banana
baby food. “It works well,” says
Thomson. Also try oatmeal, she suggests—its soluble fiber can help bulk
your stool. On the other hand, you’ll
want to avoid insoluble fiber, so stick
with refined white breads and grains for
now. Skip spicy, greasy or fatty foods,
and avoid coffee, tea or hot soups, which
can stimulate the bowels.
!"Dodge
“bad” food smells with
dishes that are cool or room temperature—they lack aromas that can
make you queasy. Amp up your meals’
flavor with marinades and gravies. If
chemo drugs leave a metallic taste in
your mouth, Bidini recommends rinsing with your homemade mouthwash
before eating.
! Web Extra!
Need mealtime
inspiration? Find
recipes and nutrition
tips for people
undergoing chemo at
Guide2Chemo.com/
recipes
(with the peel on), vegetables and beans.
And stay hydrated, counsels Thomson.
Adequate fluid intake keeps stool moving through your digestive
tract and helps flush the
chemo drugs
through your
system.
STAR TALK
Olympic gold-medal-winning skater,
TV commentator
Scott Hamilton
Testicular cancer
How it was treated: Laparoscopic
surgery and chemotherapy
How he coped: “At first, I was
petrified. I was in shock. I couldn’t
believe it,” Scott writes on his site,
chemocare.com. “But then, I made
up my mind that I would fight and
that I could do it.”
Best advice: The experience wasn’t
as bad as what I
feared,” he says
on his site. “The
fear was worse.
If people can get
information, they
can overcome
their fear and
make it through.”
Guide2chemo.com
25
feel your best
!" Avoid
aggravating mouth
sores with cool, creamy foods.
Steer clear of acidic and spicy foods.
Swap apple or grape juice for orange
juice, and creamy Alfredo sauce for
tomato sauce, says Bidini. “Try cool,
creamy soft foods rather than dry
foods. No toast or chips.”
!" Quell
nausea with small, frequent meals. And choose bland, easy-
to-digest foods. “Have someone else do
the cooking and stay out of the kitchen
to avoid the aromas,”
Bidini suggests. Ask
your doctor about
antinausea medication. And try ginger to
settle a queasy stomach: Brew it as tea or
grate some into
soup.
Gearing up for chemo?
GET YOUR EATING
HABITS ON TRACK
If you haven’t paid much attention
to your diet lately, this is the perfect
time. Meet with a registered dietitian, preferably a certified specialist
in oncology nutrition, says Bidini.
In the meantime, take these easy
steps to healthier eating:
!"Add green tea to your
morning routine.
!"Add strawberries,
blueberries or
raspberries to a meal.
!"Drink grape juice or eat
red grapes.
IMPORTANT: Do not take any
supplements without getting your
oncologist’s approval. Some may
interfere with your chemotherapy.
Low white blood cells? You’re prone to infection, so …
Say YES to
Fully cooked meat,
fish and eggs.
Pasteurized dairy
products and juices.
Municipal or
commercially
bottled water.
Say NO to
Raw eggs or foods containing raw eggs, such as eggnog
or Caesar salad. Sushi, sashimi and other raw fish. Raw
honey, raw nuts and nut butters.
Any unpasteurized products.
Well water that is not tested at least once a year or water
that comes directly from springs, lakes or rivers.
26 Health Monitor Guide to CHEMOTHERAPY
YO U R P E R S O N A L
CHEMO TOOL KIT
Download our free iPhone app to record your info wherever
you are. Track your blood cell counts, chart your progress,
schedule events, share info with your doctor and more.
For the app and more useful tools and info,
visit Guide2Chemo.com
A sampling of what you’ll find:
YOUR CHEMO CALENDAR
For printable record-keeping,
appointment reminders and more
NUTRITION BOOSTERS
Delicious recipes and expert
tips to get critical nutrients
while going through chemo
YOUR PERSONAL ORGANIZER
A comprehensive checklist to keep
those piles of paperwork organized
ALTERNATIVE METHODS OF RELIEF
Complementary therapies to
help ease the side effects of treatment
20 from
thriving tips
people who’ve been there
feel your best
We turned to folks who have gone through chemo or are going through
treatment right now for their best tips and tools—chances are, they can
also help you de-stress, stay upbeat and just plain feel your best while
chemo goes to work ridding your body of cancer.
SUCCESS
STORY
Zeva’s tumors
have shrunk
50% after
just three
treatments.
“I will be
healthy.
I will heal.
I will survive.
I will thrive”
1 Create a calming
ritual. “At home, I listen to a tape that guides
me with deep breathing
and relaxing. I take a
deep breath in and say
to myself, I am, then
breathe out and say,
Relaxing. Then another
deep breath in, I am.
Then breathe out and say,
Letting go,” says Zeva.
2 Think positive
thoughts. Says Zeva,
“There are four lines my
son wrote for me, inspired
by Zen master Thich Nhat
Hanh, to repeat over and
28 Health Monitor Guide to CHEMOTHERAPY
over: ‘I will be healthy.
I will heal. I will
survive. I will thrive.’
I say them when I’m
walking or anytime.”
3 Sneak in some Zzzs.
“Chemo was on Friday,
then Friday and Saturday
and even Sunday I felt
pretty good,” says Terri.
“But by Monday, I was
dead-tired. I’d go to work,
but at 2 PM I’d go to my
car and take a nap!
4 Get a handle on hair
loss. “I bought two wigs,
one short and one long,”
says Rebecca. “Then I
braided my real hair, cut
it off and donated it to
Locks of Love, which
makes wigs for children
with cancer. These choices
comforted me.”
5 Outsmart night
sweats. “I wear a cotton
T-shirt to bed and keep
a couple more nearby,”
says Zeva. “So when I
wake up drenched during the night, I can easily change. And I tuck
a soft washcloth under
my shirt; it absorbs the
moisture so my shirt
doesn’t get soaked.”
6 Keep your routine—
as much as possible.
“I still clean the house,”
says Zeva. “And I love to
cook—it’s like therapy. I
get out when I have the
OUR PANEL OF CANCER SURVIVORS
TERRI,
REBECCA,
DEB,
colon cancer survivor
“Don’t anticipate problems that
might not
happen!”
breast cancer survivor
“Make
choices
that bring
you comfort.”
breast cancer survivor
“Don’t be
meek. Ask
questions,
demand
answers.”
Guide2chemo.com
29
feel your best
energy—to the supermarket and to meetings
at the senior citizen
center. It’s good to keep
busy, but you have to
pace yourself.
7 Go wireless. “Most
chemo centers have
free Internet
access (you
may have to ask for the
code), so it’s great to
bring your laptop, if that
relaxes you,” says Deb.
“They usually have TVs
and DVD players, too, so
you can bring the movies
you love to watch.”
8 Pick your perfect
distraction. “I have an
IV in my hand during
chemo, so I can’t knit
as I’d hoped,” says Zeva.
“Instead I read, do crossword puzzles, browse my
new iPad and listen to
tapes of soothing music.”
9 Avoid infection.
“The seventh through
the tenth days after my
infusion is when my
immune system is at its
lowest, so I have to be
careful about germs,” says
Zeva. “I keep hand sanitizer in my pocketbook,
wash my hands often and
stay away from people
with colds. I also use
the sanitizer gel to wipe
down the shopping carts
in the supermarket.”
10 Avoid “what-if?”
anxiety. “You might not
get the same side effects
after each session, so
don’t waste time dreading something that may
never happen,” says Terri.
11
Write it down.
“Take a journal or a day
calendar to each treatment/checkup/visit. Write
what you feel, when you
feel it, what meds do what
30 Health Monitor Guide to CHEMOTHERAPY
and what day procedures
are done,” says Deb. “This
keeps you focused on you
and your health, reminds
you to go to appointments and treatments,
and down the road it will
help you understand the
things you went through.”
12 Take backup.
“The first time you go
to chemo, it can help to
bring your significant
other or a very good
friend,” says Deb. “In
addition to offering comfort, your companion can
act as your second set of
ears, and if you would
like antianxiety meds, he
can drive you home.”
13 Keep your head
cozy. “When you lose
your hair, your head gets
cold more easily,” says
Zeva. “On cool nights, I
wear a knit hat or a scarf
to bed. I even bought
some funny hats in the
children’s
department—one
has eyes
and ears on it—but
they’re soft and they keep
my head warm.”
14 Lean on your
healthcare provider. “I
call my doctor’s office and
talk to the nurses whenever I have a question,”
says Zeva. “I was reading
outside and my daughter
asked, ‘Should you be in
the sun during chemo?’ I
called and they said it was
okay if I wear a hat and
use sunscreen.”
15 Tote a “goodie
bag.” “Keep hard candy,
like lemon drops or Jolly
Ranchers, and water with
you at all times—when
CONFUSED? GET HELP!
Ask to speak to a nurse navigator, social worker
or financial advocate. Every hospital has at least
one of these pros available, and they can help
you resolve a multitude of frustrating issues.
Some of their good deeds: They can explain
consent forms, describe how to get assistance
with high co-pays or the cost of expensive drugs,
locate interpreters and even show you the layout
of the hospital so you’re less likely to get lost!
your mouth is
dry and nothing tastes good,
you’ll be glad to have them
on hand,” says Deb.
16
Speak up for yourself! “My oncologist told
my husband that it would
have been risky to follow
my first doctor’s advice,
which was to wait and see.
Which is why I cannot
stress enough to be your
own advocate. It’s your
body—no one knows it
better than you,” says Deb.
“Don’t be meek. Ask questions, demand answers
and seek second or third
opinions...it saved my life.”
17 Chill your mouth!
“Drink
something
cold during
your chemo
appointment,” says Deb.
“This helps to shrink the
blood vessels in the
inside of your mouth,
which keeps the chemo
from burning you there
and can prevent painful
mouth sores.”
Guide2chemo.com
31
feel your best
18 Rinse well…and
banish mouth sores.
“If you develop mouth
sores, tell your
oncology team.
I used something I called my
‘miracle mouthwash,’ which was
prescribed for me
by my chemo oncologist,”
says Deb.
19 Eat what you can,
when you can. “Your
taste buds will most likely
change. Some foods will
have no taste and others
become a huge unchewable
lump,” says Deb. “Learn to
try malts, shakes, ice cream,
baked potatoes, scrambled
eggs—whatever it takes!”
20 Get all the care you
need. “Don’t be afraid of
whatever medications you
are told you need postchemo. I had an injection
24 hours after each chemo
session to keep my white
blood cells up. It helped
prevent any infections,
which made it possible for
me to stick to my chemo
schedule,” says Deb.
FREE PAMPERING PERKS!
holding hands–they’re a big
part of intimacy.
Take precautions!
If you want to be intimate
the evening after a session,
ask your oncologist if oral
sex is okay. Some drugs appear in semen or vaginal secretions, and you wouldn’t
Along with the treatments and procedures that come
with having cancer are a few surprising perks. Read
on for the info that can help you score a steal—and
feel better!
! Angie’s Spa. This service provides free massages for people undergoing chemo at hospitals in four
states: MD Anderson Cancer Center in Texas, Northridge Hospital Medical Center in California, Hartford
Hospital in Connecticut and Southampton Hospital
in New York. For information, go to angiesspa.org.
Or, ask a local spa if it offers discounted services for
cancer patients.
! Crickett’s Answer for Cancer. Founded
in honor of a 39-year-old woman who had cancer,
CAFC offers free massages, as well as facials, mastectomy supplies and wigs. Go to crickettsanswer.
startlogic.com.
!
Yoga Bear. This San Francisco-based nonprofit
group offers free yoga classes at more than 200
studios in 25 states. Boost your energy during chemo:
Go to yogabear.org to sign up.
Don’t forget about
“DATE NIGHTS”
There’s nothing sexy about
chemo. But there’s nothing
wrong with having sex
while receiving treatment,
either. In fact, if you’re
feeling up to it, it can be a
great idea!
Make time for bonding
While you may not always
good. Expect side effects,
if they occur at all, 24 to 72
hours after a session.
Appearance anxiety?
Hair loss, weight
gain and the aftermath of surgery
can take their toll.
Talk through your
be “in the mood,” there will
be days when you feel quite
well—and will want to be
intimate with your partner.
In time, you’ll be able to figure out when you’re likely to
feel ill and when you’ll feel
feelings with your
partner. You’ll most
likely learn that these issues
loom much larger in your
mind than in your partner’s.
Closeness counts!
Don’t rule out cuddling or
want your partner getting a
chemo dose.
Combat side effects
Vaginal dryness can be an
issue. To prevent painful
intercourse, use a vaginal
lubricant. For men, getting
erections can be difficult.
Drugs are an option—and
insurance will generally
cover them if your oncologist goes to bat for you.
One warning: Sex while
you have low white blood
cell counts is generally not
recommended.
Ask your doctor
about your count
and if sex is safe.
Finally, be
sure to talk.
Sharing dreams
for the future is one of the
most intimate things you
can do.
—Lillie Shockney,
RN, BS, MAS
Cuddling
and hand
holding
count, too!
Guide2chemo.com
33
in the know
On the job with chemo?
How to make it work
Judy. Roughly 60% of cancer patients
who work full-time continue working
through chemo, according to a study
of 1,433 subjects in the journal Cancer.
And that can be a good thing: Changes
in your routine (like watching morning
TV instead of dressing for work) can
stress you out—something that does
not enhance the healing process—and
“sitting home thinking can cause you
to become deconditioned physically,”
says Lillie Shockney, RN, MAS,
administrative director of the
Know your
Johns Hopkins Clinical
rights
Breast Programs and
Visit eeoc.gov/facts/
Cancer Survivorship
cancer.html for details
Programs.
of the Americans with
For Elizabeth, a
Disabilities Act and
breast
cancer survivor,
the Family and Medistaying on the job was
cal Leave Act.
a lifeline: “Work is very
important because it gives you
a reason to get up in the morning
hen breast cancer survivor
and somewhere to go, and it keeps your
Judy learned she’d need
mind off your diagnosis.”
chemo, “My first thought was, I can’t
Of course, if your work is physically
take time off right now!” If you’re
or mentally demanding, doing your
the type who’s wondering if you can
job while undergoing chemo may pose
charge your laptop during your chemo
challenges. So ask your doctor if you
infusion, you probably feel just like
W
34 Health Monitor Guide to CHEMOTHERAPY
can stay on the job. If he says it’s okay,
remember these tips. They can help
smooth your days with bosses, clients
and co-workers and keep you on task:
!"How to tell, if you tell. You’re
not obligated to tell your boss or coworkers about your cancer. But opening
up does have a few advantages: You’ll
be able to ask for flexibility in your
schedule, plan for absences and prepare colleagues for a possible change in
your appearance. You will also be able
to benefit from the Americans with
Disabilities Act and the Family and
Medical Leave Act.
!"Stay
focused by setting limits.
Chemo can leave you foggy and
fatigued, but knowing how long your
attention span is can keep you on track.
If you start to feel fuzzy after two hours,
take a 10-minute break at the end of
that span instead of pushing yourself.
!"Steer the conversation with “yes,
and…” Colleagues will show their con-
cern by asking how you are doing, but
that can leave you feeling like the token
“cancer co-worker.” Next time someone
asks, say something like, “Yes, I feel terrific, and I’m really excited about the
new software we’re getting.” The technique shifts attention from your cancer.
!"Find a way to remember. Now’s not
the time to count on your memory! Use
sticky notes, keep a calendar, record
messages on your smart phone—whatever it takes to help you keep track of
appointments, meetings, deadlines and
to-do’s. Tip: Carry a memo pad around
with you in case of an impromptu
meeting.
IF YOUR INSURER
SAYS NO…
!"Resubmit the claim.
!"Make copies of any paperwork
you send.
!"Record conversations you have
with your insurance company in a
notebook.
!"Enlist the help of your doctor’s
billing office.
!"Call a social worker or nurse on
your healthcare team to discuss unresolved problems. Ask them to contact
your insurer.
!"Ask your doctor to provide
studies to your insurer to show the
effectiveness of your treatments.
!"Contact your Medicaid office
before treatment to find out if you
are eligible for reimbursement. Find
out about pharmaceutical company
reimbursement programs.
Guide2chemo.com
35
glossary
Understanding
cancerspeak
ALOPECIA: Hair loss,
a common side effect.
INTRAVENOUS: Given
through a vein.
ANEMIA: A shortage
of red blood cells.
LEUKEMIAS: Cancers
that originate in the
blood or any bloodforming organs.
ANTIEMETIC: A drug that
controls (or even prevents)
nausea and vomiting.
BLOOD CELL COUNT:
A test that checks the number of red and white blood
cells and platelets
in your blood.
BONE MARROW: The inner
tissue of bones, where blood
cells are made.
CARCINOMAS: The majority of solid tumors that start
on surfaces of the body and
in the lining of glands, such
as the breast, lung and ovary.
Often, the term adenocarcinoma is used.
COLONY-STIMULATING
FACTORS: White blood
cell boosters.
LYMPHOMAS: Cancers
in the lymphatic system.
MALIGNANT: Cancerous.
METASTASIS: The spread
of cancer from one part
of the body to another.
MYELOMAS: Cancers
that start in the immune cells
in bone marrow.
NEUTROPENIA: A
dangerous decrease
in the body’s levels
of infection-fighting
white blood cells.
ONCOLOGIST: A doctor
who specializes in
treating cancer.
INFUSION: Intravenous
delivery of meds or fluids.
36 Health Monitor Guide to CHEMOTHERAPY
PERIPHERAL
NEUROPATHY: Nerve
damage in the hands and/or
feet, which can cause pain or
numbness.
PORT: An implanted device
that allows drugs to be given
intravenously.
PROGNOSIS: The chance of
recovery versus recurrence.
RADIATION THERAPY:
The use of high-energy radiation from X-rays, gamma rays
and other sources to kill cancer cells and shrink tumors.
REMISSION: The partial
or complete disappearance
of a disease.
SARCOMAS: Solid tumors
that start in connective
tissue such as bone, fat
and muscle.
THROMBOCYTOPENIA:
A shortage of platelets
(cells that help blood clot).
Symptoms include easy
bruising, nosebleeds, bleeding gums and/or small dots
on the skin.