ASHP 2013 Midyear Clinical Meeting Student Poster Abstracts
advertisement
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
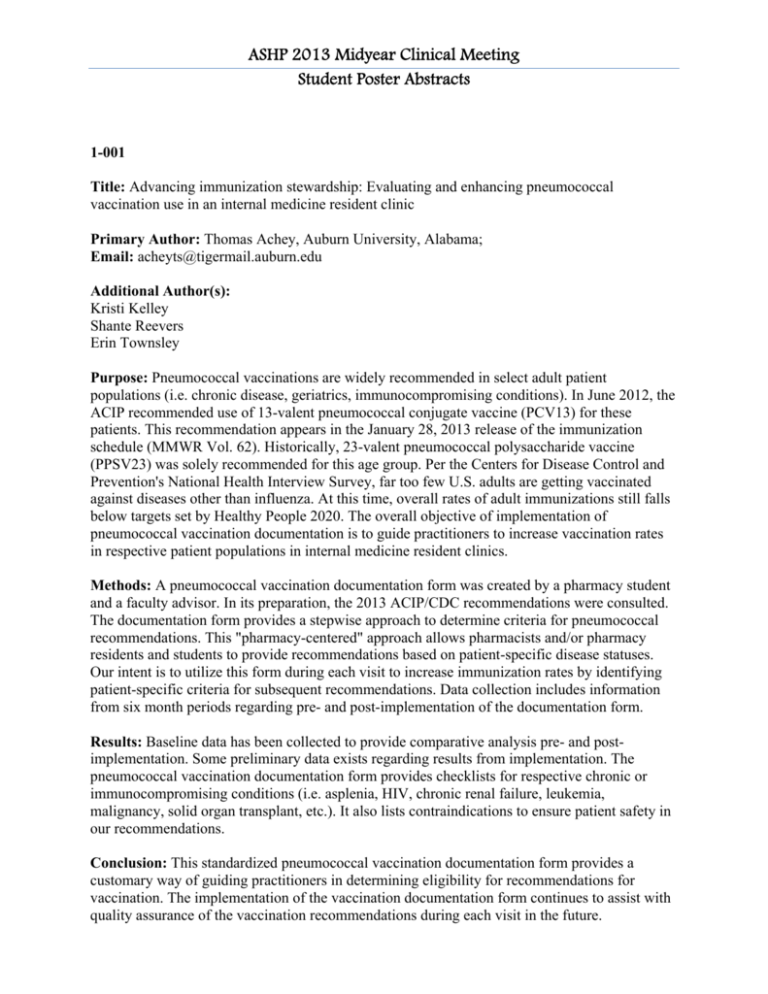
1-001
Title: Advancing immunization stewardship: Evaluating and enhancing pneumococcal
vaccination use in an internal medicine resident clinic
Primary Author: Thomas Achey, Auburn University, Alabama;
Email: acheyts@tigermail.auburn.edu
Additional Author(s):
Kristi Kelley
Shante Reevers
Erin Townsley
Purpose: Pneumococcal vaccinations are widely recommended in select adult patient
populations (i.e. chronic disease, geriatrics, immunocompromising conditions). In June 2012, the
ACIP recommended use of 13-valent pneumococcal conjugate vaccine (PCV13) for these
patients. This recommendation appears in the January 28, 2013 release of the immunization
schedule (MMWR Vol. 62). Historically, 23-valent pneumococcal polysaccharide vaccine
(PPSV23) was solely recommended for this age group. Per the Centers for Disease Control and
Prevention's National Health Interview Survey, far too few U.S. adults are getting vaccinated
against diseases other than influenza. At this time, overall rates of adult immunizations still falls
below targets set by Healthy People 2020. The overall objective of implementation of
pneumococcal vaccination documentation is to guide practitioners to increase vaccination rates
in respective patient populations in internal medicine resident clinics.
Methods: A pneumococcal vaccination documentation form was created by a pharmacy student
and a faculty advisor. In its preparation, the 2013 ACIP/CDC recommendations were consulted.
The documentation form provides a stepwise approach to determine criteria for pneumococcal
recommendations. This "pharmacy-centered" approach allows pharmacists and/or pharmacy
residents and students to provide recommendations based on patient-specific disease statuses.
Our intent is to utilize this form during each visit to increase immunization rates by identifying
patient-specific criteria for subsequent recommendations. Data collection includes information
from six month periods regarding pre- and post-implementation of the documentation form.
Results: Baseline data has been collected to provide comparative analysis pre- and postimplementation. Some preliminary data exists regarding results from implementation. The
pneumococcal vaccination documentation form provides checklists for respective chronic or
immunocompromising conditions (i.e. asplenia, HIV, chronic renal failure, leukemia,
malignancy, solid organ transplant, etc.). It also lists contraindications to ensure patient safety in
our recommendations.
Conclusion: This standardized pneumococcal vaccination documentation form provides a
customary way of guiding practitioners in determining eligibility for recommendations for
vaccination. The implementation of the vaccination documentation form continues to assist with
quality assurance of the vaccination recommendations during each visit in the future.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-002
Title: Impact of a faith-based diabetes support group: a focus on blood pressure in rural Perry
and Sumter Counties
Primary Author: Allana Alexander, McWhorter School of Pharmacy, AL;
Email: aalexan1@samford.edu
Additional Author(s):
Gary Bumgarner
Frances Ford
Eddie Davis
Purpose: The Standards of Medical Care in Diabetes 2013 update reports that cardiovascular
disease (CVD) is the major cause of morbidity and mortality for diabetics. With hypertension as
a CVD risk factor, the update suggests a systolic blood pressure less than 140 mmHg and
diastolic blood pressure less than 80 mmHg to decrease CVD risk and microvascular
complications in diabetes mellitus patients. The objective of this study is to determine if a faithbased support group with a focus on hypertension education including diet, exercise and
medication compliance will improve blood pressure and decrease these risks.
Methods: This study was approved on May17, 2013 by Institutional Review Board. Participants
attend a student facilitated support group meetings on a Saturday of each month. Meetings focus
on the ABCs of diabetes: A1C, blood pressure and cholesterol. Emphasis on blood pressure
focuses on education, management, and medication compliance. In consideration of cultural
competency, a faith-based approach is incorporated with blood pressure management; Perry and
Sumter counties are located in the Bible Belt region of the United States. This attribute enables a
durable connection to be made with participants in an effort to achieve optimal outcomes. Blood
pressure measured will be compared to previously acquired values. A Thanksgiving meal that
exemplifies selection of diabetic-friendly foods and portion control will also be provided for
participants. This not only provides education but enhances the relational aspects that are core to
this project. With Perry county as the 53rd and Sumter county as the 76th poorest counties in the
United States, access to healthcare services, education and support is highly limited. This study
provides a model that derives in one of the most severe diabetes conditions in the US and can
easily be duplicated in other areas.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-003
Title: Evaluating clinical pharmacist impact on diabetes control: outcomes on hemoglobin A1c
Primary Author: Mark Amoo, Auburn University, Alabma;
Email: amoomar@auburn.edu
Additional Author(s):
Dalton Walsh
Kalyani Sonawane
Emily Armstrong
Purpose: Several studies have shown that pharmacist collaboration in the management of
chronic disease states will improve outcomes. In particular, studies have demonstrated
significant improvements in hemoglobin A1c (HbA1c), blood pressure, and lipid levels of
diabetic patients who are routinely seen by a clinical pharmacist. The objective of this study is to
evaluate the impact of a pharmacists management in a collaborative care setting on diabetes
mellitus in an outpatient internal medicine clinic.
Methods: This study was approved by the Institutional Review Board. This study is a
retrospective chart review of diabetic patients followed at an internal medicine outpatient clinic.
Charts were identified based on claims data with associated ICD-9 codes for type 2 diabetes.
Charts are being screened for those patients who received clinical pharmacy services between
January 1, 2010 and December 31, 2012, with data collection including a 12 month follow up
period. The study excludes patients who are pregnant, have renal or hepatic disease, prisoners,
are under age 19, and those with Type 1 Diabetes. All data is de-identified. The primary outcome
for this study is the impact on HbA1c levels for patients managed by collaborative patient care.
Secondary outcomes include the total number of diabetic medications needed, classes of diabetic
medications included, and the number of patients initiated on insulin therapy. Patient
demographics and pertinent laboratory data will also be collected.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-004
Title: Long-term cholesterol management: Analyzing and enhancing documentation in an
internal medicine resident clinic
Primary Author: Haley Andress, Auburn University, Alabama;
Email: Haleyandress@gmail.com
Additional Author(s):
Kristi Kelley
Purpose: Healthy People 2020 recognizes the significance of heart disease among Americans
and has set targets to encourage patients to be adherent with all aspects of managing
cardiovascular diseases, including cholesterol management. The Third Report of the Expert
Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult
Treatment Panel III) [ATP III] from the National Cholesterol Education Program (NCEP)
provides guidelines for the management of cholesterol. The latest estimates from the American
Heart Association (AHA) report that 32 million adults in the U.S. have total cholesterol (TC)
levels ≥240 mg/dL. In addition, the AHA has established National Goals for
Cardiovascular Health for 2020 in which targets TC < 200 mg/dL in patients with ideal
cardiovascular health. In consideration of the recommendations established in ATP III, a
cholesterol-monitoring program involving proper documentation of cholesterol drug therapy
regimens as well as monitoring for efficacy and safety will be implemented. The overall
objective of this monitoring form is to guide practitioners to increase monitoring of lipid therapy
for efficacy and safety in respective patient populations in internal medicine resident clinics.
Methods: A documentation form to assess long-term management of cholesterol lowering
therapy was created by a pharmacy student and a faculty advisor using components that are
typically assessed during cholesterol lowering therapy. The documentation form does offer a
standardized method of tracking and assessing a patients information pertaining to their
cholesterol therapy such as their lipid panels, liver function tests (LFTs), and dose adjustments.
The purpose of this form is to provide an efficient way to recognize safety parameters for
cholesterol lowering therapies and to maximize patient benefit. Data collection includes
information from a one-year pre-implementation period.
Results: The cholesterol documentation form does provide a checklist for patient indication,
low-density lipoprotein (LDL) goal, current dose, dose adjustments, LFTs, creatine kinase (CK),
lipid panel, and lifestyle changes such as smoking, diet, and exercise. In addition, the
standardized documentation form does assist with any necessary follow-up to ensure patient
compliance and safety with the medications and lifestyle changes. Baseline data has been
collected to provide analysis for pre- and post-implementation of the monitoring form.
Conclusion: Implementation of this documentation form will provide healthcare professionals
with a standardized method of following cholesterol lowering therapy. This documentation form
will assist providers in the assessment of a patients care as well as enhance the ability to identify
potential contraindications and barriers to achieving optimal therapy. Implementation of this
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
form will serve as a step towards increased clinic compliance with NCEPs ATP III guidelines
and increase in patient safety and practitioner efficiency during each patient visit.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-005
Title: Determination of the stability of extemporaneously compounded oral viscous budesonide
suspensions
Primary Author: Jordan Burt, McWhorter School of Pharmacy, Samford University, AL;
Email: jburt@samford.edu
Additional Author(s):
John Arnold
Purpose: Recently, the corticosteroid drug budesonide has become increasingly utilized as an
extemporaneously prepared oral suspension for the treatment of eosinophilic esophagitis in
pediatric patients. Typically, patients are instructed to administer the budesonide by mixing
prescribed amounts of Aspartame (Nutrasweet) and budesonide inhalation solution (Pulmicort
respules). However, some compounding pharmacies are beginning to create more elegant
compounded budesonide oral suspensions from bulk powders of the drug. The purpose of this
study is to assess the stability of budesonide over time when compounded by these different
methods.
Methods: Preparations were made from either budesonide inhalation solution (Pulmicort
respules) or bulk budesonide powder. For one formulation, 2 mg of the 0.5mg/ ml budesonide
inhalation solution (Pulmicort respules) was mixed with 2 g of Aspartame (Nutrasweet). For the
other formulation, budesonide powder was added to methylcellulose to achieve a final
budesonide concentration of 0.5 mg/ml by a local compounding pharmacy. The stability of the
budesonide in the two formulations was assessed via high performance liquid chromatography
(HPLC). Initially, a standard curve was prepared from the known amounts of budesonide and
measured at an absorbance of 240 nm. Subsequently, both formulations were added to amber
medicine bottles. Aliquots of each formulation were stored under refrigeration (4 degrees
Celsius) or at room temperature (25 degrees Celsius). Samples (50 mcl) were sampled at various
time-points, mixed with 950 mcl of mobile phase, and injected into the HPLC for determination
of budesonide content.
Results: Budesonide oral suspensions compounded by either method result in viscous
suspensions which retained physical stability over the course of the stability experiment. Initial
concentrations of 0.162 plus/minus 0.02 mg/ml (4 degrees Celsius) and 0.155 plus/minus 0.01
mg/ml (25 degrees Celsius) were measured in the oral suspension compounded from the
budesonide inhalation solution (Pulmicort respules). Initial concentrations of 0.474 plus/minus
0.02 mg/ml (4 degrees Celsius) and 0.460 plus/minus 0.02 mg/ml (25 degrees Celsius) were
measured in the oral suspension compounded from the budesonide powder. After 32 days,
measured budesonide concentrations in the oral suspension compounded from the Pulmicort
respules were 0.177 plus/minus 0.01 mg/ml (4 degrees Celsius) and 0.160 plus/minus 0.07
mg/ml (25 degrees Celsius). Measured concentrations in the oral suspension compounded from
the budesonide powder were 0.494 plus/minus 0.03 mg/ml (4 degrees Celsius) and 0.543
plus/minus 0.07 mg/ml (25 degrees Celsius) after 32 days.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Budesonide, compounded by the two methods reported, is stable for up to 32 days
in suspension whether in the refrigerator or at room temperature. Extemporaneously
compounded budesonide suspension will likely continue to be an important formulation for the
treatment of eosinophilic esophagitis in pediatric patients.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-006
Title: Faith-based diabetic education/support groups facilitated by pharmacy student impacts
hemoglobin A1c: a focus on Perry and Sumter counties in rural Alabama
Primary Author: Kelli Carpenter, McWhorter School of Pharmacy, Alabama;
Email: kcarpent@samford.edu
Additional Author(s):
Gary Bumgarner
Eddie Davis
Frances Ford
Purpose: Diabetes is reaching epidemic proportions in rural Alabama. Hemoglobin A1c is a
marker of glycemic control. In order to lower hemoglobin A1c, and better control diabetes,
patients must be educated, as well as supported and motivated. Implementing support groups to
share diabetes education and awareness, utilizing group dynamics, will help patients better
control their diabetes. The purpose of this study is to determine the effectiveness of a student
facilitated faith based diabetes education and support group on patients hemoglobin A1c levels in
two rural counties in Alabama that are among the 100 poorest counties in the US.
Methods: The study has been approved by the Institutional Review Board and informed consent
forms are signed. The diabetes support and education classes are held the first Saturday of each
month. Each meeting is opened and closed with a prayer, which incorporates cultural
competency in this deeply spiritual population. The meetings are held in rural Alabama in two
counties, Perry and Sumter. The meeting in Perry County is held at the Perry County Health
Department and the meeting in Sumter County is held in a community pharmacy, York Drug.
The participants include African American males and females with type 2 diabetes. Each month
the discussion focuses on a diabetes related topic and the participants are provided handouts to
fill in and follow along. Emphasis is placed on building authentic relationships and the
subsequent effect of this on behavioral and lifestyle changes. We share a Thanksgiving meal,
emphasizing fellowship with proper diet education. Meeting topics include the basics of
hemoglobin A1c, blood pressure and cholesterol (ABCs of diabetes) and the impact of diet,
exercise, and medication adherence. The meetings are interactive and the participants are
encouraged to share ideas with the group. Hemoglobin A1c levels are monitored and compared
to previous levels.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-007
Title: Patient perception of pharmacist involvement in direct care in university-affiliated
outpatient clinics.
Primary Author: Jeanna Coleman, Auburn University Harrison School of Pharmacy, Alabama;
Email: mjc0001@auburn.edu
Additional Author(s):
Bradley M. Wright
Haley Phillippe
Miranda Andrus
Kimberly B. Garza
Purpose: Pharmacists are becoming more involved in direct patient care in the primary care
setting with the goal of ensuring optimal medication therapy outcomes. Studies in this setting
have shown that pharmacist involvement in direct patient care can improve HbA1c, blood
pressure, lipids, and other clinical outcomes; however, few studies have shown pharmacist
impact on humanistic outcomes. The objective of this study is to determine patient perception of
pharmacist involvement in disease state management and the impact of counseling by a
pharmacist on patient confidence and understanding of their medications and disease states
within primary care. This information will help pharmacists and physicians understand the role
and impact of collaboration in the primary care setting from the perception of patients.
Methods: This study will be submitted to the Institutional Review Board for approval. A survey
will be developed in order to determine patient perception of the benefits of pharmacist and
physician collaboration, the pharmacists ability to educate patients, how well the patient can
manage their own health, and the patients perception of pharmacists as a health care provider. In
addition, basic demographic information will be collected. This survey will be administered to
patients at two university-affiliated, family and internal medicine outpatient clinics who are
referred to a pharmacist for education or disease state management. Patients who are unable to
understand the survey will be excluded. The survey will be given to patients to complete after a
visit with the pharmacist. All data collected will be anonymous, maintaining patient
confidentiality.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-008
Title: Attendance barriers to diabetes self-management classes
Primary Author: Julie Craft, Auburn University Harrison School of Pharmacy, Alabama;
Email: jac0041@auburn.edu
Additional Author(s):
Angela Hammond
James Leeper
Dana Carroll
Purpose: Studies have shown there are both provider and patient barriers to attending Diabetes
Self Management Education (DSME) classes. Some focus on barriers perceived or reported by
the providers, while others focus on barriers reported by patients. Previous studies have
identified patient barriers to include: lack of transportation to the site (for education), travel
distance to site (for education), lower health literacy levels and being in lower socioeconomic
brackets, especially those with no insurance. The purpose of this study was to identify barriers to
patients attending newly implemented interdisciplinary DSME classes to try to meet the needs of
our patient population.
Methods: From September 2010 through May 2012, one hundred twenty one adult (&#8805;18
years old) patients were invited to participate in free DSME classes. One hundred and two (84%)
of those invited did not attend. Patients were referred to the classes by their primary care
physicians, a diabetes care coordinator or a diabetes educator. Several months after the
conclusion of the classes, a 28 question survey was developed and administered to those who did
not attend the classes either in person or via phone to assess for barriers that prevented
attendance at DSME classes. Patient contact was attempted by phone on five different occasions
or through the course of a clinic visit in order to administer the survey.
Results: A total of forty-seven (46%) patients responded to the survey with 46 (45%) completing
the entire survey. Seven patients declined to participate, 1 patient was deceased, 1 patient was
terminated from the practice, and the remaining patients (n=46 [45%]) could not be reached
(reasons include invalid number, lack of follow up in clinic, failure to answer phone/respond to
messages). The mean age of study participants was 48.3 years. Thirty-nine (83%) were female.
Forty-two patients (89%) lived <30 minute drive from the clinic, with the majority (n=34) living
within the same city limits of the clinic. Twenty-seven (57%) indicated they thought it was
important to attend DSME classes, while twenty-three (49%) patients stated that they wanted to
attend DSME classes, but could not due to various reasons. Of these patients, nine (43%)
indicated lack of transportation as the main reason. Seven (33%) patients had conflicting events,
one (5%) patient had issues with childcare, and the remainder stated other reasons for lack of
attendance. Of the twenty-four (51%) patients who stated that they did not want to attend DSME
classes, attitude [I dont need to come, I think my diabetes is under control, etc] (n=14, 56%)
proved to be the main barrier.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: This data shows that barriers to attending DSME classes in our clinic for those who
wanted to attend were primarily related to lack of transportation, and inconvenient/conflicting
class schedules. The primary reason for lack of attendance in those who did not want to come
was overall poor patient attitude towards diabetes management. Class attendance at our clinic
may improve by offering classes at a variety of times throughout the day for different lengths of
time. It may also prove useful to deliver diabetes education through telemedicine, website or
social media in order to overcome transportation barriers.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-009
Title: An Assessment for the Presence of Pharmacy Deserts in Jefferson County, AL
Primary Author: Nicholas Daniel, McWhorter School of Pharmacy, Samford University,
Alabama;
Email: ndaniel@samford.edu
Additional Author(s):
Michael Hogue
Purpose: The purpose of this study was to determine if areas with limited or no access to
community pharmacy services in Jefferson County, AL exist.
Methods: The location of community pharmacies in Jefferson County, AL were geo-mapped
and contrasted against census tract population data. Jefferson County is Alabama's most
populous county and includes the city of Birmingham. Census tract population data was obtained
from the U.S. Census, 2010. Pharmacy locations were obtained utilizing pharmacy websites for
all chain, grocery, and mass merchandisers operating pharmacies in the county. Independent
pharmacy locations were obtained from an independent pharmacy buying cooperative. The
number of pharmacies per 10,000 population was calculated for each census tract. A secondary
analysis compared our pharmacy access map to one from the U.S. Department of Agriculture
showing food deserts in Jefferson County to determine if correlations exist between access to
food resources and pharmacy services. The USDAs criteria for determining food deserts are as
follows: "To be designated as a food desert, a census tract must be both: Low-income (poverty
rate &#8805; 20% OR median family income &#8804; 80% of the area's median family income)
AND low-access (&#8805; 500 people OR &#8805; 33% of the population lives >1 mile from a
supermarket or large grocery store)". Similarly, we are defining pharmacy desert as a census
tract with poverty rate >20% and no community pharmacies.
Results: The 2010 Census identifies 163 census tracts in Jefferson County inclusive of a
population of 658,466. 173 community pharmacies operate in the county, for a mean ratio of
2.63 pharmacies per 10,000 population. The 173 community pharmacies were comprised of 46
(26.6%) mass merchants/grocery stores, 59 (34.1%) chain pharmacies, and 68 (39.3%)
independent pharmacies. The number of pharmacies per 10,000 population for each census tract
varied from 0 to 23.4. Of the 163 census tracts, 84 (51.5%) had no community pharmacy. 62 of
the 163 census tracts (38.0%) had no community pharmacy within a 1-mile radius of the
centroid. The secondary analysis showed that of the 40 USDA-identified food desert census
tracts, 28 (70.0%) also had no pharmacy. 33.3% (28/84) of the census tracts with no pharmacy
were also food deserts. In the 12 food deserts with pharmacies, 13.0% (3/23) of the pharmacies
were mass merchant, 26.1% (6/23) were chains, and 60.8% (14/23) were independent. 41 census
tracts met our definition of pharmacy desert. Of the 28 food deserts with no pharmacy, 26
(92.8%) were also pharmacy deserts.
Conclusion: There are areas of limited physical access to a pharmacy in Jefferson County, AL,
the states most populous county, and these areas appear to be highly correlated with USDA-
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
designated food deserts. Pharmacy desert is a novel term coined as a result of this study to
describe these areas.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-010
Title: Prescription medication adherence in PharmD students
Primary Author: Rachael DeWeese, McWhorter School of Pharmacy, Samford University,
Alabama;
Email: rdeweese@samford.edu
Purpose: In accordance with current push in healthcare, specifically pharmacy, to increase
prescription medication adherence, this study is being conducted to discover adherence rates in
PharmD students as both patients and furture pharmacists. This population has pre-set,
appreciatable differences in health literacy. Adherence rates among the classes are to be
compared to gauge the influence of differing levels of health literacy on medication adherence.
Only one survey of healthcare professionals has been published since 2000, and only physicians
and nurses were surveyed. The results of this study may provide further insight into influences
on medication adherence in the general population.
Methods: The Institutional Review Board has approved this study being performed by
anonymous online survey, using the Qualtrics system. The link for the survey will be emailed to
the PharmD classes of 2014-2017 of one school of pharmacy using the schools Google Listserv.
This survey will be open for appoximately three months. Participants will only need to click the
link, complete the survey, and submit it. The survey consists of eleven questions and should take
a maximum of ten minutes to complete. Demographics such as age, gender, and current status
(P1-4) in pharmacy school will be gathered. Number of chronic prescriptions, as well as rates of
adherence to both chronic (>90 days) and acute (90 days or less) prescriptions will be acquired.
Responders will be considered adherent when medication is taken as prescribed 80% or more of
the time because this adherence rate has been associated with improved therapeutic outcomes in
previous studies. Adherence rates will be compared and contrasted between genders, among ages
and pharmacy classes, as well as between chronic and acute medications. Adherence differences
in both chronic and acute medications due to different frequencies of administration will also be
assessed.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-011
Title: Time to guideline based empiric antibiotic therapy in the treatment of pneumonia in a
community hospital: a retrospective review
Primary Author: Beth Erwin, Samford University, McWhorter School of Pharmacy, Alabama;
Email: berwin@samford.edu
Additional Author(s):
Erika Cretton-Scott
Jeffrey A Kyle
Leland N Allen, III
Purpose: The 2005 ATS/IDSA guidelines for hospital acquired pneumonia (HAP), ventilator
associated pneumonia (VAP), and healthcare associated pneumonia (HCAP) stress the
importance of initiating prompt appropriate and adequate empiric antibiotic therapy because
failure to do so is associated with increased mortality. The objective of this study is to determine
the percentage of patients with HAP, VAP, or HCAP who received guideline based empiric
antibiotic therapy as well as the average time from suspected diagnosis to administration of the
first dose of the final antibiotic in the empiric regimen among these patients.
Methods: This study has been approved by the Institutional Review Board. It will take place at a
hospital in suburban Birmingham, Alabama. The hospital's electronic medical record system will
identify patients who were diagnosed with pneumonia over a four month period. The definitions
from the 2005 ATS/IDSA guidelines for the management of adults with HAP, VAP, and HCAP
will be used to classify the type of pneumonia and to define appropriate empiric antibiotic
therapy. Patients who do not meet the definition for HAP, VAP, or HCAP will be excluded. The
following data will be collected from electronic medical records: patient age, antibiotic allergies,
date and time of admission, date and time of pneumonia onset, type of pneumonia, presence of
risk factors for multi drug resistant pathogens, initial empiric antibiotics ordered, date and time
the first dose of each antibiotic was administered, and any subsequent changes made to empiric
antibiotic therapy. The percentage of patients who received guideline based empiric antibiotic
therapy will be calculated. Of the patients who received guideline based therapy, the mean time
from suspected diagnosis of HAP, VAP, or HCAP to initial administration of the final antibiotic
within the empiric regimen will be calculated.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-012
Title: Accuracy of formularies in an electronic health record and Epocrates mobile application
for Blue Cross Blue Shield and Medicaid patients
Primary Author: Kenda Germain, Auburn University, Alabama;
Email: kke0001@auburn.edu
Additional Author(s):
Jeanne Forrester
Miranda Andrus
Lea Eiland
Purpose: Physicians commonly use formulary drug coverage information generated by
electronic health records (EHR) and the Epocrates mobile application for medication selection,
and non-formulary selections could lead to non-adherence with prescribed regimens. However,
the accuracy of these selection tools have not been systematically verified in our population. The
studys purpose is to assess the accuracy of formulary status icons generated by the EHR and
Epocrates mobile application for patients with Medicaid and Blue Cross Blue Shield, the primary
insurance providers in our state.
Methods: Patients of all ages who had a chart review performed by pharmacy students at the
outpatient pediatric and family medicine clinics at our institution from May to November of
2013 will be included in the analysis. Patients who are uninsured or are insured by third party
payers other than Medicaid or Blue Cross Blue Shield will be excluded. Data will be collected
retrospectively from the EHR, and from published online formularies for Medicaid, Blue Cross
Blue Shield, and the Epocrates mobile application. For each patient reviewed, we will collect
prescription medication information, date seen in clinic, third party payer, and coverage status in
the EHR and Epocrates. Coverage status will be defined as covered, prior authorization required,
or not covered. Once data collection is complete, the status provided in the EHR and the
Epocrates mobile application will be compared to the actual Medicaid and Blue Cross Blue
Shield formularies published online, and the accuracy of the two databases will be determined.
This study received Institutional Review Board approval.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-013
Title: Development of an inter-professional practice at an established student-run free clinic in
Birmingham, AL
Primary Author: Natalie Gist, Auburn University Harrison School of Pharmacy, Alabama;
Email: nwg0001@auburn.edu
Additional Author(s):
Erin McCreary
Meredith Ginn
Davis Bradford
Eric Craig
Purpose: To describe the implementation of a collaborative, inter-professional program at an
established, student-run free health clinic. The objective of the collaboration was to integrate the
provision of pharmacy and medical services in order to optimize care of patients without health
insurance.
Methods: Pharmacy and medical students from two different universities volunteered time to
work at the clinic. Patients were triaged and initially interviewed by both medical and pharmacy
students. Students consulted with an attending physician and pharmacist to determine ultimate
diagnosis and plan for therapy. Medical students instructed and engaged pharmacy students in
the diagnostic process while pharmacy students communicated with medical students about
appropriate evidence-based pharmacotherapy, prescribing within a formulary, and appropriate
administration of medications. Additionally, pharmacy students assisted with provision of
medications and patient counseling. Round-table discussions followed clinic to broaden
knowledge base of both disciplines.
Results: The ultimate goal of this collaboration was to provide quality, free healthcare for
uninsured patients and advance the knowledge and skills of students from multiple health
disciplines. Through this interdisciplinary collaboration, the clinic enhanced patient care, student
education, and professional development.
Conclusion: This program allowed pharmacy and medical students to expand and apply their
knowledge of evidence-based medicine, as well as strive for optimization of patient care through
collaborative inter-professional provision of health services.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-014
Title: Implementation of computerized provider order entry (CPOE) in a community hospital:
impact on time to administration of first antibiotic dose
Primary Author: John Hensley, Samford University, Alabama;
Email: jhensley@samford.edu
Additional Author(s):
Amy Clark
Angela Thomason
Purpose: The CPOE program has shown to improve the quality of healthcare provided to
patients and increase efficiency among providers. The objective of this study will consist of a
retrospective chart review to determine the difference in the time to administration of first
antibiotic doses before and after the implementation of CPOE.
Methods: This study was approved by the Institutional Review Board. There will be no
interventions by the investigators and data collection will include non-identifying patient
information. The treatment group will consist of two hundred patients greater than or equal to 19
years of age hospitalized between January 1, 2013 and August 15, 2013 who received antibiotic
therapy. The primary outcome will be the time to administration of the first antibiotic dose (from
the time the order was placed) before and after the implementation of CPOE. Secondary
endpoints will include the hospital length of stay, antibiotics received and rate of death. A
standardized data collection form will be utilized to collect the following information for each
patient: height, weight, age, sex, date of admission, date of discharge, admitting diagnosis,
antibiotic administered, initial antibiotic order date/time, initial antibiotic administration
date/time and death prior to hospital discharge. Data from patients will be accessed by the
investigators to determine if time of administration of first antibiotic was decreased for patients
using the CPOE system. Secondary outcomes will help determine if there was an increase in the
quality of healthcare the patient received and the efficiency among providers.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-015
Title: Oral surgeons evaluation and management of pain control in chronic opioid patients
Primary Author: Jerame Hill, Samford University McWhorter School of Pharmacy, Alabama;
Email: jhill2@samford.edu
Additional Author(s):
Jeffrey Kyle
Pamela J Sims
Purpose: Pain management is a topic that many prescribers find difficult to assess in patients
with underlying chronic pain. The objective of this survey is to better understand the knowledge
base and how comfortable oral surgeons are in combating acute pain in these patients.
Furthermore, the survey will look to evaluate what role pharmacist can play in helping with these
complicated patients. The importance of this study is to further evaluate the knowledge base of
prescribers in regards to pain management, as well as, look for avenues in which a pharmacist
can utilize their skills to improve patient outcomes.
Methods: This study will consist of a survey and will be sent to all oral surgeons in the greater
Birmingham area. Samfords IRB was obtained and will be the only permission needed. The
surveys will be sent out via email to all participates. The emails will contain a recruitment letter
along with a link to assess the survey via survey monkey. This step will be granted two weeks
before each non-responder will be sent a reminder email. This step will be given an additional
two weeks. Once all results are received, statistical test will be conduced using Samford's SSPS
software. Data collected will include: area of practice, length of time in practice, questions
related to opiod dosing, methods used to control pain, and possible methods for pharmacy
intervention. Participates will only have to complete the survey and will not have any follow-ups.
Descriptive data will be collected and thus descriptive statistics will be utilized. The primary
outcome will be a composite measure of oral surgeons knowledge of acute pain control in
chronic pain patients, and evaluate their need for continual education on the topic. Furthermore,
this survey should allow for insight into what types of educational programs pharmacist could
help develop.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-016
Title: Development of a community antibiogram for urinary pathogens in a family medicine
outpatient clinic.
Primary Author: Tim Holton, Auburn University, Alabama;
Email: tjh0015@auburn.edu
Additional Author(s):
Meredith Jernigan
Jason Chapman
Sarah Treadway
Purpose: Resistance patterns for urinary pathogens differ upon regions due to protective
mutations in the bacteria and exposure to antibiotics. As antibiotic resistance among urinary
pathogens has increased, it is imperative that local susceptibility patterns are known in order to
optimize therapy. The purpose of this study is to develop a clinic-specific antibiogram for
urinary pathogens to determine local susceptibility patterns.
Methods: A retrospective chart review will be performed to obtain susceptibility of urinary
pathogens. Approval from the Institutional Review Board has been obtained. Urine cultures
eligible for inclusion will be those with an antimicrobial susceptibility profile obtained from
adult patients (&#8805; 18 years of age) without an indwelling catheter. Cultures will be
considered positive if there is growth of > 10^3 cfu/ml of a single urinary pathogen. Cultures
collected within 14 days of hospital discharge will be excluded. Demographic information for
each patient with a urine culture eligible for inclusion will also be collected. When available, the
MIC values (quantitative) for each antibiotic will be recorded, as well as whether the isolate is
resistant, intermediate, or susceptible (qualitative). For patients with multiple urinary cultures
during the specified time frame, only the first urinary isolate will be included, as is consistent
with the CLSI M39-A2. To develop the antibiogram, only urinary species with at least 30
isolates will be included. Percent of isolates susceptible will be reported for antibiotics for which
susceptibility testing was conducted and which would be used in clinical practice.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-017
Title: Evaluation of an empiric guideline-recommended weight-based vancomycin dosing
protocol in critically ill patients at a tertiary care facility
Primary Author: Seng Huot, Auburn University Harrison School of Pharmacy, Alabama;
Email: szh0029@tigermail.auburn.edu
Additional Author(s):
Robert Helmer
Meredith Jernigan
Sarah Treadway
John Allen
Purpose: Vancomycin is a frequently utilized antibiotic in critically ill patients with serious
gram-positive infections. In order to optimize therapy, current guidelines recommend weightbased dosing (Loading dose: 25-30 mg/kg; Maintenance dose: 15-20 mg/L) with a goal of
achieving target trough concentrations of 15-20 mg/L. The purpose of this study was to assess
the impact of a weight-based vancomycin dosing protocol in critically ill patients on initial
dosing regimens and trough concentrations.
Methods: This was a retrospective chart review comparing vancomycin therapy in patients
located in the Surgical Trauma Intensive Care Unit, Medical Intensive Care Unit, and Burn
Intensive Care Unit who received at least three doses of vancomycin during the pre- or postprotocol implementation periods (Pre:12/1/2012-2/28/2013; Post:4/1/2013-6/30/2013). The
primary outcome was the percentage of patients who achieved an initial trough concentration of
15-20 mg/L. Secondary outcomes included median initial serum trough concentration;
percentage of patients receiving appropriate loading and maintenance dosages based on the
protocol; time to first dose of vancomycin; timing of trough levels; time to achievement of goal
trough concentrations; and percentage of patients with an increase in serum creatinine
concentrations of 0.5 mg/L or 50%. All parameters were compared in pre- and post-protocol
implementation groups.
Results: To date a total of 18 unique episodes of the protocols initial use have been identified
and evaluated in the post-protocol implementation group. Fifty-six percent (10/18) of patients in
which the protocol was utilized attained goal trough concentrations between 15-20 mg/L during
therapy, however, 83% (15/18) attained goal levels with the concentration target was broadened
to 10-25 mg/L. The median initial trough concentration achieved was 12.15 mg/L. The majority
of patients received appropriate weight based dosing based on the protocol with 78% of patients
receiving an appropriate loading dose while 72% of patients received an appropriate maintenance
dose with frequency adjusted based on renal function. Two patients experienced nephrotoxicity
while receiving Vancomycin.
Conclusion: A weight-based Vancomycin dosing protocol was developed and implemented
among critically ill patients at an academic medical center. We predict that utilization of this
protocol will significantly impact the initial trough concentrations and initial dosing regimens
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
based on preliminary data from the post-implementation study group that demonstrated that the
majority of patients received appropriate doses and attained goal trough concentrations after
protocol implementation.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-018
Title: Retrospective evaluation of levetiracetam use for generalized clonic status epilepticus in
pediatric patients admitted to an academic pediatric intensive care unit (PICU)
Primary Author: Fuh Tzer Jong, Auburn University, Harrison School of Pharmacy, Alabama;
Email: fzj0002@auburn.edu
Additional Author(s):
Allison Chung
Rosa Vidal
Sheryl Falkos
Jingjing Qian
Purpose: Levetiracetam use as adjunct to antiepileptic drugs (AEDs) has been correlated with its
efficacy in reducing seizure frequency in critically ill children for refractory status epilepticus,
status epilepticus or acute repetitive seizures. Despite phenytoin being the recommended drug for
generalized clonic status epilepticus (GCSE), levetiracetam has been used widely in the absence
of studies with established effectiveness. The purpose of this study is to evaluate the efficacy of
levetiracetam use in controlling seizure activity, including any adverse effects reported with
levetiracetam use in pediatrics with GCSE.
Methods: The institutional review board approved this retrospective study. A list of patients
names whose medication profile included levetiracetam was generated from the pharmacy
database and chart reviews were then performed on patients. Males and females (0 to 18 years)
admitted to pediatric intensive care unit (PICU) with GCSE while in PICU with or without prior
use of levetiracetam, and with prior or new onset seizure activity were included in the study.
Pediatrics with prior levetiracetam use but did not receive levetiracetam during the PICU stay,
had a medication order for levetiracetam but did not receive the medication, and those with
history of hypersensitivity to levetiracetam were excluded from the study. Data collection on
demographic information, past medical history and home medications, medications received
during PICU stay, subjective and objective data pertaining to levetiracetam use, and length of
PICU stay were obtained. Levetiracetam dose per kilogram body weight per day for each
individual patient was calculated and efficacy outcome was recorded. Any reported adverse
effect was included in the results. In addition, all AEDs prescribed post discharge were also
reported in the results. The primary outcome was seizure control in pediatrics with GCSE on
levetiracetam.
Results: Fifty nine pediatrics received levetiracetam for GCSE during a PICU stay within the
two year observation period, with a median age of 3.43 years. 37 of the 59 patients were males
versus 22 were females. 50.8 percent of 59 patients were Caucasians versus 47.5 percent were
African Americans. 92.5 percent of the 40 patients with seizures history had prior levetiracetam
use. Median body weight of patients was 15 kg (range, 3.2 to 116 kg). Median levetiracetam
dose was 63.6 mg per kg per day (range, 3.1 to 150 mg per kg per day). Median length of
levetiracetam use prior to discharge from PICU was 5 days (range, 2 to 45 days). Fifty two
patients with GCSE responded to levetiracetam, one with controlled GCSE after levetiracetam
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
dose was changed, and one did not respond to levetiracetam. Two patients exhibited extreme
somnolence.
Conclusion: Levetiracetam use in pediatrics with status epilepticus shows promising results not
only in terms of seizure control, but the drug itself also proves to be safe and tolerable. This
study provides support for future prospective studies on levetiracetam use in pediatric status
epilepticus.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-019
Title: Insulin dose requirements in chronic kidney disease
Primary Author: Jennifer Lakanen, Auburn University Harrison School of Pharmacy, Alabama;
Email: jll0018@auburn.edu
Additional Author(s):
Anne Marie Liles
Purpose: It has been observed that patients with chronic kidney disease (CKD) require lower
doses of insulin than patients without kidney impairment. The objective of this study is to
determine appropriate insulin dosing per kilogram of body weight for each stage of CKD in non
dialysis patients diagnosed with CKD stage 3 to 5 and stable diabetes (type 1 or 2).
Methods: This retrospective, chart review study was approved by the institutional review board.
Data will be collected from previous routine visits from patients at a chronic kidney disease
clinic. To be included, patients must be diagnosed with stage 3 to 5 CKD and diabetes (type 1 or
2), currently be taking insulin, and have an A1c less than 8 percent. The following data will be
collected from patients meeting the inclusion criteria: age, race, gender, weight, cause of CKD,
glomerular filtration rate, type of diabetes, total daily dose of insulin, types of insulin the patient
is taking, A1c, iPTH, phosphorus, vitamin D, bicarbonate, hemoglobin, albumin, and urine
protein. Patients will be excluded if taking anti diabetic medication besides insulin, taking
steroids or have a history of kidney and pancreas transplant. The study will determine the total
daily doses of insulin (units per kg) used in patients with CKD and correlate these doses with
level of kidney function (or glomerular filtration rate). It is predicted that the dose of insulin
required in these patients will decrease as kidney function decreases. This project will help
provide guidance for health professionals initiating and adjusting doses on insulin in patients
with CKD.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-020
Title: Bupivacaine liposome use specifically in colorectal surgery at a large community hospital
Primary Author: Grant McGuffey, Auburn University Harrison School of Pharmacy, Alabama;
Email: Gem0002@auburn.edu
Additional Author(s):
April Williams
Edward H. Eiland, III
Purpose: The use of bupivacaine liposome has been associated with a mechanism of action
which may produce a longer duration of pain relief compared to regular bupivacaine and a
subsequent decrease in opioid requirements for post-operative pain control. Therefore,
bupivacaine liposome was brought before our hospitals pharmacy and therapeutics committee for
review and approval as a designated inpatient formulary medication to be stocked and distributed
by the pharmacy department. The objective of this analysis is to evaluate, following formulary
addition, the use and therefore the benefit of bupivacaine liposome in patients undergoing
colorectal surgery within our large community hospital.
Methods: This retrospective analysis was reviewed and approved by the Institutional Review
Committee. Scheduled colorectal surgeries and protocol order sets were developed and used to
identify patients undergoing colorectal surgery who meet our criteria for bupivacaine liposome
utilization. Following formulary review and approval, the use of bupivacaine liposome was
restricted by our hospitals pharmacy and therapeutics committee to selected colorectal surgeons
for specific use in left or right laparoscopic colon surgery, open colectomy, and
hemorrhoidectomy. Patients were stratified into four groups which include TAP block with
regular bupivacaine, TAP block with bupivacaine liposome, use of a spinal narcotic, or standard
PCA alone. Data collected and collated via the electronic medical record will include patient
characteristics, amount of opioid use post-operatively, opioid-related adverse events, and length
of hospitalization.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-021
Title: Evaluation of the prevalence of HIV-infected patients with uncontrolled diabetes in a
southeastern US clinic
Primary Author: Chidiya Ohiagu, Auburn University- Harrison School of Pharmacy, Auburn
University, Alabama;
Email: coo0004@auburn.edu
Additional Author(s):
E. Kelly Hester
Purpose: Modern advances with highly active antiretroviral therapy have led to an increased
lifespan in the treated HIV-infected population. As a result, chronic diseases such as diabetes,
hypertension, and hyperlipidemia are more likely to affect the lives of these patients.
Antiretroviral therapy, hepatitis C co-infection, family history and obesity contribute to the
development of new onset diabetes in this population. Patients treated for HIV infection are at a
higher cardiovascular risk and uncontrolled diabetes could contribute to morbidity and
compound the risk of cardiovascular outcomes. The purpose of this study is to evaluate the
prevalence of HIV-infected patients with uncontrolled diabetes.
Methods: The institutional review board approved this retrospective chart review. The electronic
medical record system was used to identify adult, HIV-infected patients with a hemoglobin A1c
(HbA1c) >7% during the study period (January 1st 2012 to July 31st 2013). In addition to
demographic data, the following data were collected during this period: current HbA1c, BMI,
cardiovascular risk factor measurements (blood pressure, cholesterol panel, past cardiovascular
medical history, smoking status), HIV viral load, CD4 count, current and past antiretroviral
medication use, current diabetes medications, and duration of diabetes and HIV infection. The
primary objective was the percentage of HIV-infected patients with uncontrolled diabetes.
Secondary objectives included evidence of diabetes complications, assessment of control of other
cardiovascular risk factors, and virologic control of HIV infection.
Results: 41 patient charts were reviewed retrospectively. These patients were 54% male, 73%
African-American with an average age of 49. The average BMI was 32. The mean duration of
diabetes was 7.6 years and duration of HIV infection 7.8 years. HbA1c was > 7% in 63% of
patients and the mean HbA1c was 8.2%. Patients with controlled HIV but uncontrolled diabetes
were 52% with a mean HbA1c of 9.4 and 55% of these patients had a HbA1c > 9.0%. Insulin
was used in 56% of this population. A high number of concomitant medications were observed
(mean 11.4). Diabetes complications were evident with 39% having peripheral neuropathy and
29% having renal impairment. The control of other cardiovascular risk factors was reviewed.
Blood pressure was uncontrolled in 49% of patients, LDL was > 100 mg/dL in 44% of patients,
and 37% were smokers. HIV and diabetes was uncontrolled in 34% of patients.
Conclusion: This population had advanced diabetes that was largely uncontrolled with evidence
of complications. While approximately a third were uncontrolled for both HIV and diabetes, it is
concerning that more than half of the patients had controlled HIV and significantly uncontrolled
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
diabetes. While the large number of concomitant medications may contribute to this, the
discordance suggests a disproportionate concern for HIV infection. Pharmacists can assist HIV
providers in cardiovascular risk reduction with HIV infection by working with patients with selfmanagement to control diabetes and other risk factors, and reduce morbidity in this high-risk
population.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-022
Title: Antibiotic selection for the treatment of acute exacerbations of chronic obstructive
pulmonary disease
Primary Author: Ryan Owens, Auburn University Harrison School of Pharmacy, Alabama;
Email: reo0004@auburn.edu
Additional Author(s):
Takova D. Wallace
Kurt A. Wargo
Purpose: Acute exacerbations of chronic obstructive pulmonary disease (COPD) are often
treated with antibiotics when cardinal symptoms are present, a practice that is supported by the
Global Initiative on Obstructive Lung Disease (GOLD) guidelines. The GOLD guidelines are
vague with the recommendation for antibiotic selection, specifically in hospitalized patients;
however it is recommended to administer either an aminopenicillin with or without clavulanate,
macrolide, or a tetracycline. Therefore, the goal of this study is to compare current practice
trends to established GOLD guideline recommendations. Three outcomes were assessed in this
study: 1) determination of patients who are eligible to receive antibiotics based upon cardinal
symptoms; 2) comparison of antibiotic selection to GOLD guideline recommendations; 3)
patients who are at risk for multidrug resistant (MDR) bacteria and antibiotics selected.
Methods: This was an institutional review board approved retrospective analysis of the medical
records of 200 patients with COPD exacerbation admitted between November 2011 and
November 2012 to an 881-bed tertiary care hospital in North Alabama. Patients who received
intensive care treatment, were less than 40 years of age, or had concurrent respiratory disease
were excluded. Upon inclusion into the study, medical history, and specific pharmacotherapy for
COPD prior to admission, in-hospital pharmacotherapy, and therapy upon hospital discharge
were collected for analysis. The cardinal symptoms of a COPD exacerbation (dyspnea, increase
in sputum volume, and purulent sputum production) were collected and analyzed with respect to
appropriateness of antibiotic therapy. Furthermore, risk factors for MDR pathogens were also
collected to determine if empiric therapy was appropriate (antimicrobial therapy within the
previous 90 days, hospitalization for greater than 48 hours in the previous 90 days, nursing home
or long term care facility resident, home infusion therapy, chronic dialysis within 30 days, family
member with documented MDR pathogen, immunosuppressive disease and/or therapy).
Results: A total of 200 patients were included in the data analysis of this study. Out of the 200
total patients, 187 received antibiotics. A total of 153 (82%) did not meet the criteria for
receiving antibiotic therapy; however, 140 of those patients (92%), were treated with antibiotics.
The most common antibiotics administered were levofloxacin (n = 137), azithromycin (n = 54),
ceftriaxone (n=44), and the combination of ceftriaxone with azithromycin (n = 26). Of the other
GOLD recommended antibiotics, 8 patients received doxycycline, three received amoxicillin,
and two received amoxicillin-clavulanate. A total of 24 patients met criteria for antibiotics who
also had risk factors for MDR pathogens. Of those patients, none received vancomycin, and only
3 received piperacillin-tazobactam, and one received cefepime.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: This study demonstrates the need for antimicrobial stewardship and education of
prescribers of patients with acute exacerbation of COPD. The high percentage of patients who
received antibiotics without an indication puts them at risk for the development of resistance and
unnecessary adverse effects. The results of this study will be shared with physicians at our
institution, including those in the Emergency Department, in order to prevent unnecessary use of
antibiotics.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-023
Title: Patient perception of pharmacists as mid-level practitioners
Primary Author: Jacob Parker, McWhorter School of Pharmacy, Samford University, Samford
University; Birmingham, AL;
Email: j1335p@gmail.com
Purpose: The ratification of the Patient Protection and Affordable Care Act and related statutes
has extended health-care coverage to millions of Americans and offered pharmacists an
expanded role in many practice environments. The objective of this study was to evaluate patient
perception of pharmacists, examine patient understanding of the role of a pharmacist, and
identify areas of care that pharmacists need to improve or educate to show the value of
pharmacists in healthcare.
Methods: An anonomyous 24-question survey was developed and approved by the appropriate
Institutional Review Board. The survey consisted of questions relating to pharmacists medical
knowledge, involvement in patient care, and perception as mid-level practitioners. All patients
who visited a local industrial health clinic between July 1, 2013, and October 1, 2013, were
asked to complete this voluntary survey. Data collected included age, highest level of education,
ethnicity, number of health conditions, and number of current medications. The statistical
analyses primarily focused on examining the variation within the sample population and
concentrated on the use of descriptive statistics to highlight knowledge, attitudes, and practices
of pharmacists.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-024
Title: Vancomycin use in adult medicine patients: Validation of a weight-based vancomycin
dosing protocol in a tertiary care facility
Primary Author: Jessica Patanella, Auburn University Harrison School of Pharmacy, Alabama;
Email: jlp0025@tigermail.auburn.edu
Additional Author(s):
John Allen
Robert Helmer
Sarah Treadway
Meredith Jernigan
Purpose: Vancomycin is a frequently utilized antibiotic in the treatment of serious gram-positive
infections. In order to optimize therapy, current guidelines recommend weight-based dosing
(Loading dose: 25-30 mg/kg; Maintenance dose: 15-20 mg/L) with a goal of achieving target
trough concentrations of 15-20 mg/L. The purpose of this study was to assess the impact of a
weight-based vancomycin dosing protocol following guideline recommendations in adult
medicine patients on initial dosing regimens and trough concentrations.
Methods: This was a retrospective chart review comparing vancomycin therapy in adult
medicine patients who received at least three doses of vancomycin during the pre- or postprotocol implementation periods (Pre:12/1/2012-2/28/2013; Post:4/1/2013-6/30/2013). The
primary outcome was the percentage of patients who achieved an initial trough concentration of
15-20 mg/L. Secondary outcomes included median initial serum trough concentration;
percentage of patients receiving appropriate loading and maintenance dosages based on the
protocol; time to first dose of vancomycin; timing of trough levels; time to achievement of goal
trough concentrations; and percentage of patients with an increase in serum creatinine
concentrations of 0.5 mg/L or 50%. All parameters were compared in pre- and post-protocol
implementation groups.
Results: To date a total of 79 unique episodes of the protocols initial use have been identified
and evaluated in the post-protocol implementation group. Thirty-nine percent (31/79) of patients
in which the protocol was utilized attained goal trough concentrations between 15-20 mg/L
during therapy, however, when the goal trough concentration was expanded to 10-25 mg/L, 67%
of patients attained goal levels. The median initial trough concentration achieved in this
population was 12.15 mg/L. The majority of patients received an appropriate weight-based
regimen based on the protocol with 68% (54/79) of patients receiving an appropriate loading
dose while 81% (64/79) of patients received an appropriate maintenance dose with frequency
adjusted based on renal function. Three patients experienced nephrotoxicity while receiving
vancomycin, with only one of these patients being on concurrent nephrotoxic agents.
Conclusion: A weight-based vancomycin dosing protocol was developed and implemented
among adult medicine patients at an academic medical center. We predict that utilization of this
protocol will significantly impact the initial trough concentrations and initial dosing regimens
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
based on preliminary data from the post-implementation study group that demonstrated that the
majority of patients received appropriate doses and attained goal trough concentrations after
protocol implementation.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-025
Title: Evaluation of HPV vaccination rates in HIV-infected patients indicated for the vaccine
Primary Author: Kaitlin Raley, Auburn University Harrison School of Pharmacy, Auburn, AL;
Email: ktrayhsop14@gmail.com
Additional Author(s):
Kelly Hester
Purpose: Recent reports indicate significant underutilization of human papillomavirus (HPV)
vaccine in the general population since its availability. The prevalence of HPV in HIV-positive
patients is high and reported in 75% and 98% in women and men who have sex with men,
respectively. Compared to immunocompetent patients, those with HIV-infection have higher
rates of invasive anal and cervical cancer related to high risk HPV types (16 and 18). The HPV
vaccine has demonstrated excellent immunogenicity in HIV-infected men and women. The
purpose of this study is to evaluate HPV vaccination rates and missed opportunities in HIVinfected patients indicated for the vaccine.
Methods: This study was submitted and approved by the Institutional Review Board. This will
be a retrospective chart review. The electronic medical record system will identify adult, HIVinfected patients 19 to 26 years of age receiving primary care from the HIV clinic between 2007
and July 2013. The following data will be collected: patient age, gender, ethnicity, HPV
vaccinations or contraindications to use, duration of HIV infection, duration of HIV care at the
clinic, HPV risk factors, past medical history related to HPV and family history of cancer.
Information related to HIV infection will also be collected: CD4 count, viral load, and current
treatment with antiretroviral therapy. Records will be reviewed to determine if there was not a
reasonable opportunity for vaccination. All data will be recorded without patient identifiers and
maintained confidentially. The incidence of HPV vaccinations for indicated patients will be
calculated. The following data for this population will be analyzed descriptively: demographics,
HPV risk factors, evidence of cytology abnormalities with screening, clinical status of HIV
infection and medical management. Based on results, recommendations will be provided for
optimizing HPV vaccination rates in the HIV-infected population.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-026
Title: Assessment of Standardized Patient Encounters to Prepare Pharmacy Students for
Smoking Cessation Counseling
Primary Author: Anna Reid, McWhorter School of Pharmacy, Alabama;
Email: areid@samford.edu
Additional Author(s):
Terri M. Wensel
Purpose: This study evaluates how students’ knowledge of smoking cessation correlates to their
perceived confidence and preparedness. It also assesses the ability of third-year pharmacy
students to collect patient histories and provide accurate information to a patient in a simulationbased setting.
Methods: This study was submitted to the Institutional Review Board for approval and informed
consent was obtained from all participants. Third year pharmacy students participated in two
simulated patient encounters in which they counseled patients on a new prescription for a
smoking cessation medication. These encounters took place at the University of Alabama
Birmingham or McWhorter School of Pharmacy. During both encounters standardized patients
were used. The first controlled patient encounter assessed the student’s ability to counsel a
patient on varenicline. The second assessed over-the-counter smoking cessation products. The
design for both encounters was the same. Students had ten minutes to interact with the patient
and provide them with the appropriate information. Standardized patients filled out a rubric
documenting their interaction with the students. After completion of the second encounter,
students were given a survey assessing their smoking cessation knowledge, perceived
preparedness, and their impression of the encounters. Both the evaluation rubrics completed by
the standardized patients and student surveys were used to assess the students. Statistical analysis
will be used to compare the results of the student surveys and the evaluation rubrics. Further
information on the methods used for this study is available from the Samford University IRB
application.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-027
Title: Analysis of a postpartum counseling service at a university hospital
Primary Author: Kristina Schatz, Samford University, McWhorter School of Pharmacy,
Alabama;
Email: kschatz@samford.edu
Additional Author(s):
Jennifer Chapman
Jongwha Chang
Purpose: Choosing a method of contraception is an important decision for a postpartum woman.
During this imperative time, health care providers can evaluate the needs of their patients when it
comes to birth control. The objective of this study is to describe a pharmacists counseling service
pertaining to methods of contraception on the postpartum unit of a university hospital.
Furthermore, it evaluates the number of postpartum patients who desire information on
contraception with the demographics of age, public or private insurance, and whether the patient
was English or Spanish-speaking.
Methods: This is a retrospective cohort data analysis of postpartum women who received the
option of counseling by a pharmacist or pharmacy intern at a university hospital from August 1,
2011, to February 28, 2013. Postpartum patients were approached by a pharmacist or intern to
assess their needs and desire for counseling on contraception. The pharmacist or intern used data
collection forms to document the patients age, insurance type, method of interest (if any), and if
the patient wanted counseling on contraception usage. Pamphlets were also provided to the
women who wanted handouts and were available in English and Spanish. There were 2,048 cases
included for this study. The total number of patients who wanted information as well as
pharmacist preparation time and counseling time were also noted.
Results: Patients who were interested in a hormonal contraception method were 3 times more
likely to desire counseling compared with patients who declined information (p<0.05). Also,
patients who wanted an implantable form of contraception were 8 times more likely to desire
information compared with patients who declined counseling (p<0.05). Patients in the age range
of 18-25, 26-30, and 31-45 years were less likely (56%, 64%, & 65%) to want counseling
compared with the age range of 12-17 years (all p<0.05). Lastly, patients who spoke Spanish
were 3 times more likely to have been counseled compared with non-Spanish speaking patients.
The number of postpartum patients counseled on different contraception methods was 1,546
versus 699 patients who declined counseling. Total pharmacist preparation time totaled 160.95
hours, while total patient counseling time totaled 204.55 hours.
Conclusion: Overall, postpartum women who chose to be counseled by a pharmacist were
considering either a hormonal or implantable method of contraception, were younger than the
age of 17 and were Spanish speaking. Furthermore, the average amount of pharmacist
preparation time spent was 4.3 minutes per patient and actual counseling time on average was
5.5 minutes per patient. These factors may represent a trend that could be noted by pharmacists
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
and applied to other counseling services. Also the counseling service helped provide good
pharmaceutical patient care by meeting postpartum womens need for accurate information about
contraception before leaving the hospital.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-028
Title: Impact of the Joint Commission pneumonia core measures on antibiotic use and selection
Primary Author: Boopathy Sivaraman, Auburn University, Harrison School of Pharmacy, AL;
Email: bzs0021@auburn.edu
Additional Author(s):
Natalie Gist
Jason Parson
Marilyn Bulloch
Purpose: Prior to 2012, the Joint Commission pneumonia core measure (PN-5) required
antibiotic administration for suspected pneumonia within six hours of arrival to the emergency
room. In January 2012, the Joint Commission issued a new core measure (PN-6) requiring initial
antibiotic administration within 24 hours of presentation that was appropriate according to
current guideline recommendations. This study evaluated the impact of the Joint Commission
Pneumonia core measure on appropriate antibiotic use and selection in the emergency
department (ED) for patients with suspected community acquired pneumonia (CAP).
Methods: The institutional review board approved this retrospective chart review study. Medical
records of patients aged 18 years and older that presented to the emergency department with an
initial diagnosis of CAP and were subsequently admitted to our institution during the years 2011
(PN-5) and 2012 (PN-6) were reviewed. Patients were identified using ICD-9 admission codes
480-489.9 (Pneumonia and Influenza). The primary outcome for this study was to determine the
appropriateness of initial antibiotic agent(s) and dose selection for patients admitted with
suspected CAP in the emergency department and primary diagnosis at hospital discharge.
Exclusion criteria included: recent hospitalization for two or more days, residence in a nursing
home, rehabilitation, or other extended care facilities, and antibiotic use, chemotherapy, home
infusion therapy, wound care, or hemodialysis within previous 30 days. Comparisons between
the two groups (patients admitted in 2011 and admitted in 2012) were performed using
descriptive statistics and contingency table analysis with a Chi-square or Fishers Exact test for
categorical variables and t-tests for continuous variables to determine statistically significant
differences. Statistical analyses were performed using Microsoft Excel 2010 and SAS version
9.4.
Results: One hundred eighty-three patients with an initial ED diagnosis of CAP were reviewed.
Of these, 92 patients met the inclusion criteria. The majority of patients admitted to both groups
were female and the mean age was between 57-61 years and similar between groups. There was
a trend that indicated antibiotic use in 2012 (PN-6) was more appropriate than in 2011 (PN-5),
but results were not statistically significant (52 percent vs. 46 percent, P equals 0.353). The
number of patients presenting with an initial diagnosis of CAP in the emergency department
whose final diagnosis at hospital discharge remained CAP showed an increased trend in 2012 but
was not statistically significant between the two groups (91 percent vs. 81 percent, P equals 0.
184). Appropriateness of antibiotic prescribing did not differ between groups for patients
admitted to the intensive care unit (P equals 0.263) nor a general medical unit (P equals 0.721).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: After PN-6 was implemented, a greater percentage of patients admitted to the ED
with suspected CAP had a final diagnosis of pneumonia compared to patients admitted under
PN-5 protocol. Changes in the Joint Commission pneumonia core measure requirements did not
have a significant effect on appropriate antibiotic prescribing.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-029
Title: Near-miss transcription errors: a comparison of reporting rates utilizing an order imaging
software and a formal reporting system
Primary Author: David South, Samford University McWhorter School of Pharmacy, Alabama;
Email: dsouth1202@gmail.com
Additional Author(s):
Jessica Skelley
Mary Dang
Purpose: The medication use process is composed of several steps, each with the potential for
occurrence of medication errors. Such errors have been highly publicized, and hospitals are
constantly improving measures to prevent such errors. Currently, focus is being placed on
identifying near-miss events as a way to prevent errors, and transcription errors identified
through pharmacist review of medication orders are a category of near-miss to analyze. This
study evaluated the number and types of transcription errors identified by pharmacists at a large
community hospital and compared the reporting rates between two reporting mechanisms for
these near-misses.
Methods: Two near-miss transcription error reporting mechanisms were assessed for three
months. The reporting mechanisms assessed included a specific queue within the institution's
order imaging software (OIS) and the institution's formal error reporting system. The order
imaging software queue mentioned above was utilized by pharmacists to identify and comment
on order images associated with transcription errors. Date, patient-care unit, and type of
transcription error were recorded by the investigator for each order image in the queue. For the
formal reporting system, reports containing near-miss transcription errors were identified by the
medication safety pharmacist and reviewed by the investigator. Each error in the two reporting
mechanisms was classified according to a standardized classification scheme developed for this
project. The scheme was continually revised over the first week of data collection to include
several common types of transcription errors and was finalized following this initial collection
period. When an order image did not contain any comments regarding the type of transcription
error committed, the error type was classified as unknown. Following data collection, the
difference in reporting rates between the two systems was determined. Percentages for each type
of transcription error reported were determined and compared between the two reporting
systems.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-030
Title: Evaluation of single, fixed-dose rasburicase for tumor lysis syndrome (TLS) at a
community hospital
Primary Author: Amanda Stanley, Auburn University Harrison School of Pharmacy, Alabama;
Email: afs0006@auburn.edu
Additional Author(s):
Jennifer N Davis
Matthew E Eckley
Brannon Flores
Purpose: Rasburicase, a urate oxidase enzyme, is indicated for the treatment or prophylaxis of
hyperuricemia in patients with cancer that are at high risk for tumor lysis syndrome (TLS). While
rasburicase is currently approved for weight-based dosing, there have been case reports of single,
fixed doses being used effectively for TLS prevention and treatment. The purpose of this study is
to evaluate if a single, fixed dose of 3 mg or 6 mg (based on eligibility criteria) is appropriate and
assess cost-effectiveness compared to traditional dosing methods.
Methods: This institutional review board approved study will evaluate patients that receive
rasburicase at fixed doses of 3 mg or 6 mg as single or repeated doses for tumor lysis syndrome.
A criteria for use and dosing guide has been approved by the hospital's pharmacy and
therapeutics committee that outlines single, fixed-dosing strategies for patients. Patients will
receive rasburicase 3 mg dose via intravenous infusion if they weigh less than 90 kg and have a
baseline uric acid level of less than 18 mg/dL. All other patients will receive rasburicase as a
single 6 mg dose. A second dose of 6 mg may be administered based on follow-up uric acid
levels. All data will be recorded without patient identifiers to maintain confidentiality. The
following data will be collected: patient age; gender; cancer diagnosis; baseline and postrasburicase labwork (uric acid, serum creatinine, WBC, LDH, potassium, phosphorous, albumin,
and calcium); other TLS preventative measures utilized; and complications of TLS (if available).
The authors will determine the effectiveness of the above single, fixed dosing strategy for
rasburicase, based on this data. The authors will also statistically analyze the cost-benefit ratio of
the single dosing method versus traditional weight based dosing.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-031
Title: Impact of pharmacy student facilitated faith-based diabetic educational support on
cholesterol levels: a focus in rural Perry and Sumter counties
Primary Author: Kristin Tribiano, Samford McWhorter School of Pharmacy, Alabama;
Email: ktribian@samford.edu
Additional Author(s):
Gary Bumgarner
Eddie Davis
Frances Ford
Purpose: Despite continual medication advancements, diabetes continues to be an ever growing
metabolic disease that affects people with devastating consequences. Diabetes presents both
short and long term micro and macrovascular complications and in order to prevent and manage
these, individuals need to have knowledge which is obtained through education. Along with the
education component, it is encouraging to feel understood and to relate to others which can be
available through support groups. The objective of this study is to evaluate the impact of faith
based diabetic education and support on participants cholesterol levels in rural Perry and Sumter
Counties of Alabama.
Methods: This study received Institutional Review Board approval and informed consent forms
are signed. Saturday morning and afternoon meetings are held at two facilities, one in the Perry
County Health Department in Marion, Alabama, and the other in Sumter County at an
independent pharmacy, York Drug, in York, Alabama. These counties are among the poorest 100
counties in the US and the Birmingham News recently referred to them as the third world of
Alabama. They have one of the highest diabetic incidences in the nation. For each monthly
meeting we begin and end in prayer and discuss diabetes related topics such as diet, exercise, and
proper medication usage and compliance. Each participant receives a typed handout of the
material to take home, use, and share with others. An emphasis is placed on building
relationships with the patients that could result in positive lifestyle changes. Working at this
deeper level can enhance patient acceptance of the disease. Meeting discussions have included
the importance of getting hemoglobin A1c, blood pressure, and cholesterol (ABCs of diabetes)
levels checked and knowing personal goals. Cholesterol levels are drawn and recorded. The data
will be analyzed and compared to previous data.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-032
Title: Frequency of beta-blocker use following exacerbations of chronic obstructive pulmonary
disease in patients with compelling indications for use
Primary Author: Tara Veasey, Auburn University, Harrison School of Pharmacy, Alabama;
Email: tmv0004@auburn.edu
Additional Author(s):
Wesley D. Oliver
Jessica A. Starr
Nathan A. Pinner
Purpose: Cardiovascular disease is a common and important comorbidity in chronic obstructive
pulmonary disease (COPD). Cardioselective beta-blockers are underutilized in patients with
COPD and concomitant ischemic heart disease and heart failure (HF) despite being
recommended and considered safe. This study determined the proportion of patients discharged
on a beta-blocker with a compelling indication for use following an acute exacerbation of COPD
(AECOPD).
Methods: This was a retrospective study performed at two medical centers with institutional
review board approval at each. Patients admitted over a 2-year period with a diagnosis of
AECOPD and a past medical history of myocardial infarction (MI) or systolic HF (LVEF less
than 40 percent) were included in the analysis. Patients with beta-blocker contraindication, betablocker allergy, asthma, concomitant respiratory disease, age less than 40 years, admission to the
ICU, or need of inotropic therapy were excluded. Patient characteristics obtained from the
medical record included age, gender, race, blood pressure, heart rate, home COPD medications,
and use of home oxygen. Beta-blocker use prior to, during, and after hospitalization was assessed
with the primary objective of determining the proportion of patients discharged on a betablocker. Secondary objectives included the proportion of beta-blockers discontinued following
an AECOPD, the proportion of patients discharged on a cardioselective beta-blocker, and
identifying factors that may have contributed to withholding beta-blockers.
Results: Two hundred and twenty-one patients were included in the analysis with average age of
68.7 years and 63 percent male. Beta-blockers were used in 66 percent of patients prior to
admission and 71 percent of patients at discharge. Of discharge beta-blockers, 42 percent were
cardioselective. A larger proportion of patients with HF (86 percent) compared to MI (63
percent) were discharged on a beta-blocker (p equals 0.0005). Discharge beta-blockers were used
in 64 percent of patients with more severe COPD, defined as being treated with long acting
anticholinergic, long acting beta agonist, and inhaled corticosteroid, compared to use in 72
percent of patients with less severe disease (p equals 0.3264). Mean age was similar in patients
discharged on beta-blockers, 68.7 years, and not receiving beta-blockers, 68.6 years (p equals
0.9467).
Conclusion: Approximately three fourths of the patients admitted for an AECOPD with a
compelling indication for beta-blocker use were discharged on a beta-blocker with less than half
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
being cardioselective. The proportion of patients treated with a beta-blocker did not decrease
from admission and trended toward increase. Rate of beta-blocker use was greater in patients
with heart failure but not significantly different by age or COPD severity.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-033
Title: Corticosteroid usage in the treatment of acute exacerbations of chronic obstructive
pulmonary disease
Primary Author: Takova Wallace, Auburn University Harrison School of Pharmacy, Alabama;
Email: tdw0012@auburn.edu
Additional Author(s):
Ryan E. Owens
Kurt A. Wargo
Purpose: Acute exacerbations of chronic obstructive pulmonary disease (COPD) are often
treated with corticosteroids, a practice that is supported by the Global Initiative on Obstructive
Lung Disease (GOLD) guidelines. The GOLD guidelines offer specific recommendations for
corticosteroid dosing, suggesting the administration of prednisolone 30 to 40 mg daily by mouth
for 10 to 14 days. Clinically in our institution, we have recognized a trend in prescribers not
following these guidelines, with much larger doses of intravenous (IV) corticosteroids being
administered. Therefore, the goal of this study is to compare current practice trends at an 881bed community hospital in North Alabama to established GOLD guideline recommendations.
Three main outcomes will be assessed in this study: 1) comparison of corticosteroid prescribing
practices to GOLD guideline recommendations; 2) evaluate the variable glucose effects of
steroid dosing during COPD exacerbation; 3) determination of any risk factors that may lead to
the development of hyperglycemia in these patients.
Methods: This was an institutional review board approved retrospective analysis of the medical
records of 200 patients with COPD exacerbation admitted between November 2011 and
November 2012 to an 881-bed tertiary care hospital in North Alabama. Patients who received
intensive care treatment, were less than 40 years of age, or had concurrent respiratory disease
were excluded. Upon inclusion into the study, medical history, and specific pharmacotherapy for
COPD prior to admission, in-hospital pharmacotherapy, and therapy upon hospital discharge
were collected for analysis. Corticosteroid dosing was collected upon presentation to the
Emergency Department, throughout the hospital stay, and upon discharge. Additionally, diabetes
status, and elevations of glucose levels greater than 180 mg/dL were recorded.
Results: A total of 200 patients were included in the data analysis of this study. In this study,
191 out of 200 patients received corticosteroids. The most common initial agent and average
starting dose was methylprednisolone 95 mg IV every 8 hours (range: Single dose every 6 hours)
for an average of two days (range 1 to 9 days). The most common dose of methylprednisolone
initiated was 125 mg (n = 101). Out of the 191 patients given corticosteroids, 87 (46%)
developed hyperglycemia (blood glucose greater than 180 mg/dL). Having preexisting diabetes
and being on a beta blocker were two common risk factors for developing hyperglycemia. A total
of 54 patients had preexisting diabetes, of those 47 (87%) developed hyperglycemia (46 were on
concomitant corticosteroids). In addition, a total of 71 patients were on a beta-blocker, of those
40 (56%) developed hyperglycemia (all were on concomitant corticosteroids). Hospital length of
stay (LOS) was not impacted by initial dosing of corticosteroid. Those who received
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
methylprednisolone 125 mg IV had an average LOS of 5.62 days, compared to 80 mg IV with
5.66 days, 60 mg IV with 4.75 days, and 40 mg IV with 5.8 days.
Conclusion: Corticosteroid dosing for the treatment of acute exacerbations of COPD in this
study were inconsistent with GOLD guideline recommendations. Overall, dosing was found to
be substantially higher than recommended dosing and hyperglycemia was great, especially in
patients with diabetes and those on beta-blockers. Furthermore higher doses of corticosteroids
did not shorten the hospital length of stay for patients. The results of this study will be shared
with physicians at our institution, including those in the Emergency Department, in order to
determine the appropriateness of high dose corticosteroids.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-034
Title: Quantitative analysis of medication utilization rates for implementation of an outpatient
pharmacy automated medication storage carousel
Primary Author: Angela Walsh, University of Arizona College of Pharmacy, Arizona;
Email: awalsh@pharmacy.arizona.edu
Additional Author(s):
Shenelle R. Leon
Bryan W. Edwards
Purpose: The primary goal of this project was to determine the top 100 medications with the
highest turnover and assign them to specific carousel locations, and the secondary goal was to
educate pharmacists of the new technology. Workflow is crucial to outpatient pharmacy
productivity, especially in medical centers. Due to space constraints, there was a need to
implement an automated medication storage/shelving carousel system to increase efficiency and
maximize the available floor plan. Medication carousels are more commonly utilized in inpatient
pharmacies, thus the installation of this automation in an outpatient pharmacy setting was
unique.
Methods: Medication reorder point (PAR) levels and fill frequencies from 2012 were used to
determine highest and lowest turnover medications using a Microsoft Excel spreadsheet.
Accuracy of PAR levels was assessed; when dosage form, container type, and corresponding
units of medication were inappropriate, PAR levels were recalculated and rounded to reflect
current procurement trends. The carousel was approximately 98 inches wide, with 30 rows that
each fit up to 11 eight-inch bins, 22 four-inch bins, or a combination. The top 100 medications
with the highest turnover (fast-movers) were assigned to 4-inch or 8-inch wide bins, based on
medication container size, corresponding PAR levels, and estimated physical space requirements
of the maximum (MAX) levels. Some medications were assigned fractions of bins (up to 8
sections per bin) to utilize bin space. Fast movers were grouped together on lowest-numbered
rows to reduce carousel spin time. Heavy items were evenly split among rows to distribute
weight and reduce mechanical stress. Medical supplies, refrigerated medications, controlled
substances, and heavy/bulky items were not assigned a carousel bin, but were assigned barcodes
and entered into the electronic inventory.
Results: The top 100 fast-movers were determined and assigned locations in the medication
carousel. Each location was characterized by a numerical row and bin designation, which filled
approximately the first 8 rows of the carousel. A Microsoft Excel document listing the
medication and carousel location was created and provided to the lead and procurement
technicians for reference in continuing medication assignments. A presentation was created
regarding this project and delivered to interested pharmacy staff. The presentation explained how
the carousel utilizes barcode technology to improve workflow efficiency, maintain patient safety,
and reduce errors; how the medications were selected; and how the carousel was being
incorporated into the pharmacy. The presentation also stated additional benefits of implementing
automation, which included improved inventory monitoring which ultimately reduces costs,
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
enhances productivity, and increases inventory turns. The pharmacists that attended this project
presentation verbally expressed increased confidence and familiarity with medication carousel
implementation in the hospitals outpatient pharmacy.
Conclusion: Some PAR levels did not reflect current pharmacy procurement activity, which was
likely due to drug shortages, medication backorders, and other events that changed the usual
number of prescriptions filled in the pharmacy in 2012. Despite these limitations, the primary
goal was met, which was successful assignment of the top 100 fast-movers to carousel locations.
The secondary goal was also met, indicating that a summary presentation increased familiarity
and successfully educated pharmacists about the timeline, specifications, and calculations
involved with setup of a medication carousel in an innovative practice setting.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-035
Title: 12-Month impact of Countryside Diabetes, a social media diabetes educational tool, by
quantifying membership response rates to post type and topic for enhancing future care of
disease management
Primary Author: Ee Vonn Yong, Auburn University Harrison School of Pharmacy, Auburn
University, Alabama;
Email: evy0001@auburn.edu
Additional Author(s):
Heather Whitley
Rebecca Lee
Purpose: Patients with diabetes mellitus benefit from extensive disease state management,
education, and social support. To enhance and promote this aspect of patient care, the Facebook
page, Countryside Diabetes, was developed by a multidisciplinary healthcare team in May 2012
to serve as a supportive network for those living with and caring for diabetes. Through this
medium, participants have the opportunity to exchange information and share ideas while
receiving daily education and feedback. The purpose of this project is to determine the impact
and reach of Countryside Diabetes from October 2012 through September 2013 to provide
guidance for future social media development.
Methods: Data analysis will utilize Facebook Insights. Member demographics include age,
gender, and location of residence. Posts will be organized by post type (question, statement, or
links to other articles or websites) and topic (diet and nutrition, medication, physical exercise,
social support, and current events). Each post type and topic will be analyzed by rate of Likes
and member comments to determine interest . This will provide insight into what topics and post
types the members respond to most often. Additionally, participants questions and comments to
these posts will be evaluated to identify the areas of greatest interest for future education and
support.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-036
Title: Case series of opioid-related injuries with a focus on pharmacist liability and risk
management
Primary Author: Suvra Adhikari, Harding University College of Pharmacy, Arkansas;
Email: skarki@harding.edu
Additional Author(s):
Sadaf Khan
Shanly Chen
Purpose: Opioids fill legitimate pain treatment needs when prescribed and dispensed
responsibly. However, since 1999 the number of opioid prescriptions dispensed has nearly
tripled while the number of opioid-related deaths has increased more than four-fold. Separate but
related, the number of malpractice claims against pharmacists alleging injuries that arise from
opioid misuse is increasing. The purpose of this study is to identify causes of injury and sources
of error in cases where opioids are the primary contributor to patient injury and pharmacists are
alleged to have made a medication error, and identify implications for pharmacist liability and
risk management.
Methods: This institutional review board-approved retrospective evaluation will derive data
from opioid-related malpractice claims reported to our center during the period of 2001-2012.
Claims in which opioid use did not result in injury will be excluded. Data sources will include
medical/pharmacy records, autopsy/toxicology reports, peer-review/quality improvement
summaries, depositions, and expert opinions. Data collected will include: demographics (age,
race, gender, respiratory status, drug abuse history); opioid data (dose, indication, and whether
the regimen at the time of injury was newly initiated, chronic dosing, or undergoing dosage
escalation); toxicology data; and concomitant CNS depressants. Opioid injuries will be
categorized as: addiction; respiratory depression-related anoxic injury defined as cases where the
cause of injury was opioid intoxication, alone or in combination with other drugs; or other CNS
depression-related injury. Data will be confidentially recorded without patient identifiers.
Pharmacist reviewers with expertise in judging opioids-related errors and their preventability
will independently evaluate the claims. Errors will be categorized as: technical errors; or errors
of clinical judgment which will be subcategorized as early refill, dose too high, duplication of
therapy, wrong indication, wrong frequency, drug-drug interaction, drug-disease interaction, and
allergy. Contribution to error and injury by the patient or healthcare provider(s) will also be
identified.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-038
Title: Retrospective analysis of respiratory cultures of tracheostomy dependent individuals
Primary Author: Rachael McCaleb, University of Arkansas for Medical Sciences, Arkansas;
Email: rmccaleb@uams.edu
Additional Author(s):
Holly Maples
Robert Warren
Denise Willis
Catherine E. O'Brien
Purpose: Pediatric patients requiring tracheostomy become chronically infected with bacteria
that may increase their likelihood of developing respiratory symptoms and requiring an increased
level of support. Little is known about the pathogens that infect or colonize these patients as
opposed to other respiratory compromised patients, such as cystic fibrosis (CF). Likewise, little
is known about the benefit of treating these patients with antibiotics directed against these
pahogens. The primary aim of this study is to describe respiratory cultures of patients followed
by Arkansas Center for Respiratory Technology Dependent Children (ACRTDC). A secondary
aim is to evaluate differences in microbiology by respiratory disease severity.
Methods: This was a retrospective analysis of the respiratory cultures of ACRTDC patients with
a tracheostomy in place 1 year. Demographics, length of tracheostomy, respiratory culture
results, and primary diagnoses were collected from patients followed from 1985 to June 2011.
The primary aim was to describe the respiratory microbiology including: 1)overall prevalence of
pathogens, 2) mean time to isolation of specific pathogens after tracheostomy placement, 3)
prevalence of pathogens by length of tracheostomy, and 4) prevalence of pathogens based on
respiratory management score (RMS), a measure of the severity of respiratory disease. All
subjects and culture results were included in the first objective, data after 2006 was used in the
second objective, and culture results from 2010 were used for objectives three and four.
Results: 93 patients (57% male) were included with a mean age of 9.2(5.9) yrs. Mean age at
time of tracheostomy was 3.0(4.3)yrs and mean time with tracheostomy 6.2(4.7) yrs. Primary
diagnoses varied and included both congenital and acquired neurodisabilities. The most common
pathogens were Pseudomonas aeruginosa(PA) (90%), Stenotrophomonasmaltophilia (76%),
Serratia marcescens (66%), methicillin resistant Staphylococcus aureus (56%), and methicillin
sensitive Staphylococcus aureus(MSSA) (45%). Mean first appearance for PA was 14.1(2.2)
months, for S.maltophiliawas 19.0 (2.6) months, for S.marcescens 30.8 (3.0) months, for MRSA
9.0 (2.4) months, and for MSSA was 33.9 (4.0) months. When 2010 culture results were
analyzed, PA was the most prevalent organism for all times after tracheostomy placement.
MSSA and MRSA had a similar prevalence 0-4 yrs after tracheostomy, with MSSA declining
and MRSA increasing thereafter. There was a minimal change in PA prevalence based on RMS
categories (P>0.5). The prevalence of S. marcescens among the RMS categories appeared to
decrease as the severity score increased however there did not appear to be a statistical
significance among RMS categories (P=0.58).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Once a tracheostomy was placed, MSSA was isolated the soonest (mean 5.2 (10.2)
months) and S.marcescens the latest (mean 13.3 (11.7) months) although there was significant
variability. With increased time with tracheostomy in place, MSSA was less likely to be seen on
culture and S.marcescens more likely. However, there does not seem to be a difference in
organism pathogen prevalence based on the level of respiratory care. Further study is needed to
assess the effects on clinical outcomes in our study population. However, understanding the
spectrum of pathogens isolated from respiratory cultures is an important first step.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-039
Title: Treatment of metastatic melanoma with pazopanib: a report of 5 patient cases
Primary Author: Kaitlin Merrell, University of Arkansas for Medical Sciences College of
Pharmacy, Arkansas;
Email: ksmerrell@uams.edu
Additional Author(s):
Lindsey E Dayer
Jill T Johnson
Laura F Hutchins
Purpose: Metastatic melanoma has a median length of survival after diagnosis of 6-9 months
and long-term survival rates for patients with distant metastatic disease of only 10%.
Unfortunately, the National Comprehensive Cancer Network (NCCN) clinical practice
guidelines for treating stage IV, unresectable, metastatic melanoma are limited with regard to
treatment options. These include systemic therapy, clinical trials, and/or palliative resection +/radiation for symptomatic patients. Pazopanib (Votrient) is FDA approved for advanced soft
tissue sarcoma and advanced renal cell carcinoma. Pazopanib has multiple mechanisms of
action; it is a multi-target tyrosine kinase inhibitor against vascular endothelial growth factor
receptor-1, -2, and -3, platelet derived growth factor alpha and beta, and cytokine receptor
inhibitor. To date, three Phase I trials have assessed the use of pazopanib in patients with
advanced solid tumors. The following case series presents 5 patient cases in which pazopanib
was used in combination with paclitaxel +/- carboplatin for treatment of unresectable, metastatic
melanoma.
Methods: This case series involved 5 patients with unresectable, metastatic melanoma. The
UAMS Institutional Review Board (IRB) reviewed and determined this project was not deemed
human subject research and was therefore not included in the IRB review process. Patients had
previously received other systemic therapies indicated for treatment of their disease prior
initiation with pazopanib in combination with paclitaxel +/- carboplatin. The initial dose for
pazopanib was 800 mg daily in either a single 800 mg dose or 400 mg divided doses. The initial
paclitaxel dose varied from 150-175 mg/m2; carboplatin was dosed at 6 area under the curve
(AUC). Each patient received at least one cycle of pazopanib in combination with paclitaxel +/carboplatin. Patients showed mixed results after pazopanib treatment. Dose limiting side effects
included: febrile neutropenia, increased nausea and vomiting, frequent diarrhea, renal
insufficiency, and dysuria.
Results: This case series reviews 5 patients treated with pazopanib for unresectable, metastatic
melanoma. Dose-limiting myelosuppression, as well as other complications, were found to be a
barrier that hindered scheduled therapy in 1 of these patients. This could be due to a possible
interaction of pazopanib with paclitaxel and/or pazopanib with carboplatin, requiring a dose
reduction in the systemic agents. It was also noted that of the 5 patients in this series, 3 of them
had progression in the brain prior to initiation with pazopanib. Of these, 2 stopped therapy within
2 months due to lack of response to therapy, as opposed to patients without brain mets at
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
initiation. In these patients, response rates were considerably longer (<1-2 months versus 10-20
months). At the time of this report, there are currently 2 ongoing clinical trials investigating
pazopanib in patients with metastatic melanoma.
Conclusion: There is limited research available with the specific combination of pazopanib in
combination with paclitaxel with or without carboplatin. An interim analysis of pazopanib for
unresectable or metastatic melanoma offers promising results. There seems to be some benefit in
select patients when offered pazopanib in combination with paclitaxel with or without
carboplatin for unresectable metastatic melanoma, however further research is needed to define
the best uses for this combination.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-040
Title: Pediatric High-Alert Medications Ranked by Pediatric Pharmacists and Pediatric
Prescribers
Primary Author: HyeJin Son, Harding University College of Pharmacy, Arkansas;
Email: hson@harding.edu
Additional Author(s):
Alyssa A Laurich
Katie D Patterson
Kenneth M Yates
Julie C Kissack
Purpose: The objective of this research is three-fold: to ascertain the top-ten most problematic
pediatric medications; to identify the least, moderate, and most problematic medication
categories with respect to overall patient safety; and to compare the responses of pediatric
prescribers to those of pediatric pharmacists. The Institute for Safe Medication Practices (ISMP)
periodically releases an updated list of high-alert medications and encourages clinicians to use
special safeguards to reduce the risk of errors associated with the use of these medications.
Although research shows that pediatric patients may suffer significant harm when treated with
many of the same medications on ISMPs list, due to developmental differences between adults
and pediatrics, the establishment of a pediatric-specific high-alert medication list is warranted.
Methods: Through the review of pediatric literature and the ISMPs list of high-alert
medications, a list of 50 potentially problematic medications and 11 medication categories was
developed. This list was used to generate a Survey Monkey survey, asking participants to rank
these medications and medication categories in terms of patient safety. Surveys invites were
distributed via e-mail between 2011 and 2013 to members of the American College of Clinical
Pharmacy Pediatric Practice & Research Networks, the Pediatric Pharmacotherapy Advocacy
Group, the Academic Pediatric Association, and the Society of Physician Assistants in
Pediatrics. Harding University alumni who have entered the medical field were also given the
opportunity to participate. Approximately 3000 pediatric prescribers and pharmacists were
invited to participate. Participants selected the 10 most problematic medications from a list of 50
choices for three separate categories: dosing complications, adverse effects, and medication
errors. Individual participant choices were compiled to create scores for each individual
medication. Scores for each medication in each of the three categories were summed and ranked
from 1 to 50 to identify the top-ten list. Medication categories were ranked as least, moderately,
or most problematic in regards to overall patient safety.
Results: The survey was completed by 232 pharmacists and 56 prescribers. Primary practice
sites of participants were mainly childrens hospitals (64%) and pediatric units (20%) in 38 states
plus the District of Columbia and 3 Canadian provinces. Regarding overall pediatric patient
safety, pharmacists ranked anticoagulants as most problematic, and opioids and electrolytes
ranked equally as moderately problematic. The most problematic medications, according to
pharmacists, from first to tenth were: 1-insulin, 2-vancomycin, 3-warfarin, 4-heparin, 5-
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
methadone, 6-digoxin, 7-morphine, 8-gentamicin, 9- potassium phosphate and 10-(tied)
amphotericin B & fentanyl. In comparison, prescribers ranked opioids as most problematic and
sedatives as moderately problematic. The most problematic medications, according to
prescribers, from first to tenth were: 1-insulin, 2-heparin, 3-morphine, 4-digoxin, 5-warfarin, 6fentanyl, 7-vancomycin, 8-amphotericin B, 9-potassium chloride, and 10-amiodarone. From
above two top-ten lists, pediatric high-alert medications according to prescribers and pharmacists
are insulin, vancomycin, heparin, warfarin, digoxin, morphine, methadone, potassium chloride,
potassium phosphate, gentamicin, fentanyl, amphotericin B, and amiodarone.
Conclusion: As expected, the top-ten lists generated by responses from pediatric pharmacists
and prescribers differed. However, both lists contained 80% of the same medications, including
six of the medications on Franke et al.s list of top-ten most problematic pediatric medications.
The results of this survey suggest that pediatric pharmacists and prescribers have similar views
regarding the medications with the most potential for dosing complications, adverse effects, and
medication errors when used in pediatric patients.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-041
Title: Using gap analysis and United States Pharmacopoeia (USP) 797 guidelines to improve
outcomes in sterile compounding at a regional academic medical center
Primary Author: Kathryn Alver, University of Arizona College of Pharmacy, Arizona;
Email: alver@pharmacy.arizona.edu
Additional Author(s):
Megan Handley
Amanda Zale
Albert Cortese
Purpose: USP 797 is a regulatory document of policies and procedures that is endorsed by the
Joint Commission of Accreditation of Health Care Organizations and is followed by any
institution that compounds sterile products. Sterile compounding techniques decrease infections
transmitted to patients through pharmaceutical products. The purpose of this study was to
decrease the risk of contamination of compounded medications through identifying problem
areas within USP 797 protocol using a gap analysis to ultimately improve patient outcomes at a
regional academic medical center.
Methods: This was a quality improvement project, therefore it did not meet the federal
definition of research and approval was not required by the institutional review board as per
university guidance. Pharmacy technicians at a regional academic medical center were observed
once a week for 3 hours between January-March 2013 and analyzed using a gap analysis to
determine problems in sterile compounding techniques. Three nurses were also observed in the
emergency department (ED) for compounding techniques by injecting a vial of normal saline
into an intravenous bag of normal saline. A quiz was administered to technicians to determine
understanding of USP 797 guidelines. Technicians were then provided a PowerPoint presentation
to demonstrate correct compounding skills. This presentation highlighted the areas of USP 797
that needed improvement, such as questions answered incorrectly from the quiz, and incorrect
technique observed during January to March 2013. After this intervention, technicians were
given another quiz to assess whether their USP 797 knowledge improved. The independent
variable was time of measurement (pre or post presentation). The dependent variable was staffs
understanding of USP 797 guidelines, gap analysis score, and quiz score. Data were analyzed
using percentages and chi-square analysis, with an a priori value of 0.05.
Results: This project used a purposive sample of pharmacy technicians and nurses from the ED.
Results showed that 13 out of the 22 proper garbing procedures evaluated were followed less
than 100 percent of the time. Pre-intervention data showed that 20 percent of total questions were
answered incorrectly. After administration of the PowerPoint presentation highlighting areas of
USP797 that needed improvement, such as proper garbing technique and post-intervention data
revealed that 0 questions were answered incorrectly. Chi-square analysis showed a significant
difference between the pre- and post- intervention groups evaluating knowledge of USP797 (p
less than 0.001).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Pre-intervention, there were a number of garbing procedures followed less than 100
percent of the time, showing a need for improvement in sterile compounding technique. There
was a statistically significant decrease of incorrect answers in the post-intervention quiz
compared to the pre-intervention quiz. This improvement can be associated to identifying
problem areas within garbing procedure and providing technician staff with correct procedures
tailored to those problems.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-042
Title: Implementation of an interactive approach to educate older adults about polypharmacy
Primary Author: Valmira Asllani, University of Arizona, College of Pharmacy, Arizona;
Email: asllani@pharmacy.arizona.edu
Additional Author(s):
Lena Phung
An Nguyen
Jeannie Lee
Purpose: To create and implement an educational presentation on polypharmacy using
interactive strategies. Secondly, to determine the effectiveness and helpfulness of the
interventional presentation and to increase polypharmacy awareness among older adults residing
in independent senior living facilities as measured by a retrospective pre-post participant survey.
Methods: Residents of six independent senior living facilities in Tucson, AZ were invited to
attend an interactive educational program entitled "What is Polypharmacy?" created and
presented by fourth year pharmacy students. This educational session consisted of a 30-minute
PowerPoint presentation, including various interactive learning approaches, followed by a 10minute question and answer period. An anonymous retrospective pre-post survey was distributed
to the participants to evaluate the effectiveness and helpfulness of the presentation, as determined
by the participants willingness to confidently engage in medication self-management. All
participants provided informed consent, and the study procedures were approved by the
University of Arizona Institutional Review Board (human subjects committee) for each
participating facility.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-043
Title: Evaluation of a womens reproductive health elective course in a pharmacy school
curriculum
Primary Author: Asal Azizoddin, Midwestern University, College of Pharmacy-Glendale,
Arizona;
Email: aazizoddin19@midwestern.edu
Additional Author(s):
Lara Petrossian
Shareen El-Ibiary
Purpose: Reports suggest that womens health education in pharmacy curricula has been lacking.
With the expanded role of pharmacists providing reproductive health services such as emergency
contraception, contraception, vaccines, prenatal and infertility counseling, womens reproductive
health topics are essential in pharmacy curricula. To date, evaluation and description of a
womens health elective focusing solely on various topics related to reproductive health has not
been published. The objective of this study is to evaluate a womens reproductive health elective
in a pharmacy school curriculum and to evaluate its influence on students knowledge and
confidence in counseling on reproductive health issues.
Methods: Second year pharmacy students enrolled in a womens reproductive health elective
focusing on topics such as contraception, infertility, prenatal and postpartum issues will be given
pre- and post-course surveys. The validated survey tool assessed students knowledge and
confidence in counseling on various womens reproductive health products such as combined
hormonal contraceptives, progestin-only contraceptives, emergency contraception, and over-thecounter fertility tests. Knowledge and confidence regarding preconception counseling, use of
drug information resources to answer pregnancy-related questions and confidence in counseling
on medication-use during pregnancy were also assessed. Sociodemographic information was also
collected. This study was submitted to and approved by the Institutional Review Board. The
surveys were voluntary and were not a component of the course. Completion of the surveys
served as consent.
Results: The response rate for the pre-course survey was 100%(n=33) and 94%(n=31) for the
post-course survey. Matched pre- and post-surveys was 73%(n=24). A majority (81%) of
students indicated their reasons for taking the course to be gaining confidence in providing
education on and expanding their knowledge in womens health issues. Students confidence in
counseling on womens health issues significantly increased after the course on a Likert scale
whereby 1= not confident at all and 5=extremely confident (mean scores:2.62 pre-course and
3.75 post-course, p=0.000). Similar results were seen in students perceptions of their overall
knowledge in womens health (mean scores:2.58 pre-course and 3.97 post-course, p=0.000). No
significant differences in improvement were noted between male and female students. Prior to
the course, students were least confident in counseling on the progestin-only implant and most
confident in counseling on emergency contraception (mean scores:1.82 and 3.70,respectively).
After the course, students confidence increased for the mentioned products (mean scores: 3.81
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
and 4.29, respectively). These trends were similar when looking at counseling on side effects,
missed doses, and drug-drug interactions with the various products. Drug-drug interactions
ranked lowest. Knowledge and confidence regarding preconception counseling, medication-use
during pregnancy and knowledge of drug-information resources for pregnancy-related issues also
increased.
Conclusion: Pharmacy students rated a higher level of knowledge and confidence in womens
reproductive health issues and products following the completion of a womens reproductive
health course. Students had perceived low confidence and knowledge in counseling on various
reproductive health products and issues prior to the elective course potentially indicating that
womens reproductive health topics may be lacking in pharmacy curricula. Pharmacy schools
may wish to consider incorporating additional womens reproductive health education into the
core curriculum to help better prepare students for their careers, particularly in light of the
expanding pharmacist roles in womens health.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-044
Title: Health literacy assessment of students at two schools in Tucson, Arizona using the Rapid
Estimate of Adolescent Literacy in Medicine (REALM-Teen): a descriptive study.
Primary Author: Brian Barkow, University of Arizona College of Pharmacy, Arizona;
Email: barkow@pharmacy.arizona.edu
Additional Author(s):
Chelby Helmrich
Jenene Spencer
Purpose: Studies have looked at how health literacy has a correlation to health outcomes.
Research also supports the fact that, in adults, low health literacy tends to lead to poorer health
outcomes and, inversely, high health literacy leads to better health outcomes. However, few
studies look at this correlation in childhood. The purpose of this study is to assess students in the
5th and 6th grades in two schools in Tucson, Arizona using the REALM-Teen, a validated health
literacy assessment, to increase awareness of the need for childhood health literacy.
Methods: This study has been deemed exempt from Institutional Review Board (IRB) since it
will be conducted in common educational settings and uses typical educational practices.
Children in the 5th and 6th grades at two schools in Tucson, Arizona, were sought for assessment
by receiving permission from the school, parents and children themselves. The REALM-Teen
will be utilized to determine if the children are at, above, or below grade level in relation to the
validated grade levels of this assessment. It contains sixty-six words, taken from adolescent
patient education materials of the American Academy of Pediatrics, and will take around five
minutes to complete. The children will be individually asked to read out loud each word. A
correct pronunciation will be scored as correct. A child will be able to say skip to any word,
which will count it as incorrect, but will allow the child to move on. The words will become
progressively more difficult. Upon completing the assessment, the child will be thanked, given
positive encouragement and all students will be given a small thank you gift. Each childs raw
score will be converted into an estimated grade level range as provided by the developers of the
assessment tool.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-045
Title: Frequency of return to stock errors in a community pharmacy running weekly electronic
waiting bin reports: an observational study
Primary Author: Monica Boomer, University of Arizona College of Pharmacy, Arizona;
Email: mboomer@pharmacy.arizona.edu
Additional Author(s):
Sara Andrus
Mahdieh Fazel
Kellie Goodlet
Allan Bates
Purpose: The intent of this project was to explore the frequency at which a community
pharmacy experienced return to stock errors, defined as prescriptions that were left ready on the
shelf after a weekly electronic bin report designates them for removal. Factors associated with
these errors include instances when patients received a change in therapy causing a duplicate fill,
a medication was left on the shelf despite patient requests for removal, and a medication was left
waiting past the return to stock designation date. The prevalence of these errors was noted along
with any patient dissatisfaction resulting from these occurrences.
Methods: This was a quality improvement project; therefore, it does not meet the Federal
definition of research and Institutional Review Board approval was not required. Observational
data were collected within the pharmacy over a three month period during which the electronic
waiting bin report was run weekly, and the number of errors per day that occurred due to return
to stock issues was recorded. Each error was classified as one of the following: duplicate
therapy, patient requested return to stock that remained in the will call bin, and past return date
that remained in the will call bin. It was also recorded whether each specific issue resulted in
patient dissatisfaction. The incidence of return to stock errors was analyzed using descriptive
statistics. The data were utilized to determine the incidence of return to stock errors on each day
of the week (total average calculated per day, sum of every issue type), which type of issue was
most prevalent (total calculated per week of each issue type), and whether these issues resulted in
patient dissatisfaction (total calculated per day).
Results: A total of 143 return to stock errors were recorded over the three month observational
period. Prescriptions that were kept past the pharmacys return to stock date and prescriptions that
had failed to be returned to stock after a patients request made up the majority of errors and
occurred with approximately equal frequency (44 percent and 41 percent, respectively). Double
fills, when a prescription had been filled twice for the same patient, made up only a small
percentage (15 percent) of the total return to stock errors. Errors occurred most frequently on
Mondays (25 percent of all return to stock errors) and Fridays (21 percent). Of the total return to
stock errors, 12 percent resulted in patient dissatisfaction. Patient dissatisfaction occurred most
frequently on Fridays (dissatisfaction was observed with 23 percent of the return to stock errors)
and Tuesdays (23 percent).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Running the weekly electronic bin report failed to prevent all return to stock errors,
and pharmacists should be aware of the potential of these errors to occur. The results of this
project are important for illustrating the frequency at which medications are left on the shelf for
pick up and the potential for patient dissatisfaction resulting from these return to stock errors.
This project can be used to highlight the importance of preventing procedure failures within
healthcare systems in order to avoid patient dissatisfaction and provide a higher quality of patient
care.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-046
Title: Assessing the impact of the transition to an enterprise-wide health information system on
pharmacy performance.
Primary Author: Steven Boyles, University of Arizona College of Pharmacy, Arizona;
Email: boyles@pharmacy.arizona.edu
Additional Author(s):
Kurt Weibel
Purpose: The Health Information Technology for Economic and Clinical Health (HITECH) act,
which is part of the larger American Recover and Reinvestment Act (ARRA) of 2009, mandates
that hospitals implement electronic health records that are used meaningfully. To accomplish
this, many institutions are transitioning from the use of separate software programs in each
department to an enterprise-wide electronic health record (EHR) software solution. The purpose
of this study is to quantitatively analyze the pharmacy departments performance before and after
the transition from a segmented set of systems to an enterprise wide electronic health record.
Methods: This study does not use patient specific data and does not involve human subjects and
therefore was exempt from Institutional Review Board approval. Retrospective data will be
collected from the pre-implementation and post-implementation electronic systems. Dependent
variables that will be analyzed include: medication turnaround time, the rate at which nurses
override automated dispensing cabinets prior to pharmacist review of medication orders, the
number of nursing generated missing medication requests to the pharmacy, and a set of quality
metrics suggested by the vendor of the new EHR. The medication turnaround time is defined as
the time from prescriber order entry to the moment it is available for nursing access in an
automated dispensing cabinet. The purpose of measuring these specific variables is to assess the
impact an enterprise-wide system has on the efficiency (turnaround time) and safety (pharmacist
review prior to medication use) of the order review and dispensing portions of the medication
use process. The enterprise-wide system will be implemented on November 1, 2013. Preimplementation data will be collected for August 2013, and post-implementation data will be
collected for November 2013 and February 2014 which will evaluate the immediate effects of
the transition as well as three months post-implementation.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-047
Title: Medication use evaluation of stress ulcer prophylaxis at a county teaching hospital
Primary Author: Jake Bradshaw, Midwestern University, Arizona;
Email: jbradshaw53@midwestern.edu
Additional Author(s):
Melinda Burnworth
Karen Holmes
Purpose: The development of stress ulcers in hospitalized patients is a medical concern, and
acid suppressive therapy is commonly used in prevention. Deciding which patients are
appropriate candidates for stress ulcer prophylaxis (SUP) can be challenging since many possible
risk factors have been identified. However, inappropriate use of acid suppressive therapy should
be avoided due to unintended adverse events of acid suppressive therapy such as c. difficile
infection and pneumonia. The purpose of this study was to evaluate the appropriateness of stress
ulcer prophylaxis use at a county teaching hospital. The study evaluates the use and duration of
SUP and discharge prescription for a SUP agent at Maricopa Integrated Health System (MIHS).
Methods: The institutional review board and pharmacy and therapeutics committee approved
this randomized retrospective cohort study. Hospitalized adults were included if at least one dose
of famotidine, pantoprazole, or sucralfate was received in June 2012 and excluded if
continuation of home therapy, indication other than SUP, or active gastrointestinal bleeding. A
literature search was performed to identify appropriate indications for SUP. The most
appropriate indications included invasive ventilation and coagulopathy/thrombocytopenia in the
critically ill.
Results: During the 30-day study period 567 unique patients received at least one dose of an
agent for SUP; 167 were randomly screened to obtain 50 patients who met inclusion criteria;
n=31 admitted to Internal Medicine (IM), n=14 to Intensive Care (ICU), n=5 other. Of the 29
patients started on SUP by IM, greater than 60% was inappropriate and via an IM general
admission order set. Of the 17 started on SUP by ICU, greater than 90% was appropriate.
Famotidine was initiated in 62% of patients; pantoprazole in 38%. Including IM and ICU, only
46% of the patients were started on SUP appropriately and the mean duration of SUP was 5 days.
Annual extrapolated medication costs for inappropriate use may exceed $12,000. Continuation of
therapy was prescribed at hospital discharge in 20% of patients.
Conclusion: SUP is overused at MIHS increasing inappropriate medication use and costs.
Healthcare provider education about appropriate SUP, removal of SUP prompters from IM order
sets, and inclusion of famotidine and pantoprazole criteria for use during prescribing will be
implemented.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-048
Title: Effect of a pharmacist led medication education group on acute inpatient adult psychiatric
readmissions
Primary Author: Audrey Bushway, University of Arizona College of Pharmacy, Arizona;
Email: bushway@pharmacy.arizona.edu
Additional Author(s):
Allison Arterbury
Lisa W. Goldstone
Purpose: Pharmacists can significantly impact patient outcomes and it is important to measure
the impact that pharmacists can have on psychiatric patient care. To date, there has been little
research on the impact of pharmacist led group medication education for psychiatric patients.
The purpose of this study is to assess the impact of a pharmacist led medication education group
on acute inpatient adult psychiatric readmission rates.
Methods: The University of Arizona Institutional Review Board (IRB) approved this
retrospective chart review. Informed consent was not required by the IRB for this study. Patients
admitted to the inpatient psychiatric units between September 1, 2011 and July 31, 2012 will be
identified. A random sample of 100 patients who attended the group as well as 100 patients who
did not attend the group will be selected. The following data will be collected: patient age,
gender, ethnicity, insurance benefits, primary diagnosis, substance abuse history, number of
medications at first discharge, length of stay on initial admission, time to first readmission, and
length of stay on first readmission. All data will be recorded without patient identifiers and
stored confidentially. A chi square analysis will be conducted to determine if admission rates are
different between the two groups. An independent t test will be conducted to determine if time to
first readmission or length of stay on first readmission are different between the two groups.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-049
Title: Effects of pharmacist intervention type and potency on therapeutic outcomes
Primary Author: Bach-Truc Chau, University of Arizona, Arizona;
Email: bchau@pharmacy.arizona.edu
Additional Author(s):
Ling Yuan Lee
Trang Vo
Marion Slack
Jeannie Lee
Purpose: Multiple reviews have shown that the interventions of pharmacists in patient care have
a positive impact on health related outcomes. Different types of pharmacist interventions that
have been studied include: technical, behavioral, educational and affective. This case control
study will focus on comparing high impact pharmacists interventions (cases) to low impact
interventions (controls) using published studies.
Methods: This study will not be submitted to the Institutional Review Board for approval since
only data from published research reports will be analyzed. Literature search will be based on
keywords and Mesh terms in databases such as PubMed, Ovid SP/Medline, and Cochrane. The
inclusion criteria were evidence of pharmacist involvement in direct patient care, patient-related
therapeutic outcomes, studies done in the United States, randomized controlled trials, studies
with reported number of subjects in the intervention and control group, and studies that reported
means and standard deviations of therapeutic outcomes. For the study selection and data
extraction, two students will independently review each study and meet to resolve any
discrepancies. In addition, each study will be assigned a potency score based on the amount of
interventions used. Data extraction will include: pharmacists interventions (technical, behavioral,
educational, and affective), patient characteristics, and therapeutic outcomes. The standardized
mean difference (SMD) will be calculated; studies with SMD less than or equal to 0.3 will form
the low impact group (controls) and studies with SMD greater than or equal to 0.8 will form the
high impact group (cases). These two groups will be compared to identify which pharmacists
interventions have the greatest effect on outcomes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-050
Title: Assessment of an intervention to improve hepatitis b vaccination rates in patients with
type 2 diabetes
Primary Author: Amanda Condon, University of Arizona, Arizona;
Email: condon@pharmacy.arizona.edu
Additional Author(s):
Shahene Badie
Junyan He
Alina Kurita
Roxana Lang
Purpose: A new guideline released in early 2012 from the American Diabetes Association
(ADA) and the Advisory Committee on Immunization Practices (ACIP) recommends Hepatitis B
vaccination for diabetic patients between 18 and 60 years of age. The objective of this quality
improvement project is to evaluate a pharmacist-led intervention to increase Hepatitis B
vaccination administration in patients with type 2 diabetes at a federally qualified community
health center.
Methods: This is a quality improvement project and therefore does not meet the federal
definition of research, and Institutional Review Board approval is not required. The electronic
medical record system will identify patients diagnosed with diabetes between 18 and 60 years of
age seen between April and June 2012 for inclusion in the pre-intervention analysis. The
following data will be collected: patient age, gender, ethnicity, vaccine order status, and health
insurance. Patients will be excluded for the following criteria: no immunization history, human
immunodeficiency virus positive, viral hepatitis, chronic liver disease, history of intravenous
drug use, and kidney dialysis patient. All data will be recorded without patient identifiers and
maintained confidentially. An intervention consisting of a presentation will be held to inform
providers of the new recommendation. Data will be collected post-intervention using the same
methods as pre-intervention. The intervention will be assessed for success by determining the
significance of increased vaccine orders using a chi square.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-051
Title: Prevalence of metabolic syndrome in patients treated with atypical antipsychotics in an
outpatient health clinic
Primary Author: Thomas Deeren, The University of Arizona, Arizona;
Email: deeren@pharmacy.arizona.edu
Additional Author(s):
Tanya Kent
Robert Sanzenbacher
Amy Kennedy
Purpose: Metabolic syndrome (MetS), as determined by NCEP ATP III guidelines, is a
combination of factors that demonstrates an increased risk of developing cardiovascular disease,
diabetes and stroke. Second generation antipsychotics (SGAs) are used in the treatment of
various mental health conditions. Treatment with SGAs has been shown to cause increases in
body weight and altered serum lipids, occasionally leading to diabetes or exacerbation of existing
diabetes, dyslipidemia, and ultimately metabolic syndrome. The objective of this study is to
determine if the use of SGAs are associated with an increased prevalence of MetS in patients
treated in an outpatient health clinic.
Methods: This study will be submitted to the Institutional Review Board for approval. Patients
over the age of eighteen who have been diagnosed with a Serious Mental Illness (SMI) will be
identified by utilizing ICD-9 diagnosis codes for psychotic, bipolar, obsessive-compulsive, major
depressive, anxiety, personality, and other mood disorders. The following data will obtained:
age, gender, ethnicity, blood pressure, height, weight, lipid panels, fasting blood glucose, SGAs,
and treatment length. The SGAs include: aripiprazole, asenapine, clozapine, iloperidone,
lurasidone, olanzapine, paliperidone, quetiapine, risperidone, and ziprasidone. All patient data
will be de-identified and remain confidential. Patients having at least one SMI diagnosis will be
separated into two groups. The first group will include patients that are not taking or have not
taken a SGA in the past three months. The second group will include patients taking at least one
SGA for a minimum of three months. Patients will be excluded if inadequate data are available
or if there sole diagnosis is a personality disorder. MetS will be determined using NCEP ATP III
guidelines. The primary outcome measured will be the difference in the prevalence of MetS
between each group using a chi-squared test with an alpha a priori set at 0.05.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-052
Title: Comparison of buprenorphine/naloxone and methadone efficacy in medically assisted
treatment (MAT) of opioid dependence in a parolee population
Primary Author: Shannon DeGrote, University of Arizona, Arizona;
Email: degrote@pharmacy.arizona.edu
Additional Author(s):
Mary Cradick
Spencer Marshall
Terri Warholak
Purpose: Opioid addiction is a growing problem. Research has shown opiate abuse increases
morbidity, mortality and costs to community members and the government. Medically Assisted
Treatment (MAT) has shown to decrease these risks with methadone being the current gold
standard. The objective of this retrospective study is to compare the effectiveness of
buprenorphine/naloxone, methadone and no MAT in the treatment of opioid-dependence in a
criminal justice population. Additionally, this study aims to identify which factors (acquiring
employment, urine toxicology screens and probation violations) are positively associated with
successful treatment.
Methods: This study will involve retrospective records review. Case files will be obtained from
the Pima County Adult Probation Office. Those included must be 18 years of age or older and on
probation for an illicit substance-related offense in Pima County. Pregnant women will be
excluded. The three treatment groups will include buprenorphine/naloxone (n=25), methadone
(n=25) and no MAT (n=25). Buprenorphine/naloxone and methadone groups will be compared
irrespective of medication dose. The primary dependent variables are time to a negative event,
including missed or positive urinalysis, missed court appearance and documented violations of
probation terms. The secondary outcome variables include time to finding employment, time
without negative incident and documented social improvement. Demographic information,
including highest education level attained, drug(s) of choice and substance use/abuse history will
also be collected. Comparison of demographic variables between groups will be performed by
Chi square and t-tests as appropriate. The Kaplan-Meier approach to survival analysis will be
used to analyze time to event. A Cox proportional hazards model will be used to control for
covariates. An alpha of 0.05 has been selected a priori. This study has received Institutional
Review Board approval.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-053
Title: Evaluation of appropriate antibiotic usage in community-acquired pneumonia in
hospitalized pediatric patients: a quality improvement project
Primary Author: Sarah Deitering, University of Arizona College of Pharmacy, Arizona;
Email: sarahjd@email.arizona.edu
Additional Author(s):
Amy Nguyen
Elaine Truong
Emily Kilber
Megan Brandon
Purpose: In 2011, the Infectious Diseases Society of America (IDSA) released clinical practice
guidelines for the treatment of pediatric Community-Acquired Pneumonia (CAP). These
guidelines recommend ampicillin for parenteral therapy and amoxicillin for oral therapy. While
research has shown that adherence to antibiotic guidelines improves outcomes and reduces
bacterial resistance, anecdotal evidence at this hospital suggested that adherence to this set of
guidelines was poor. Therefore, the primary objective of this project was to examine the
prescribing patterns for the treatment of CAP in pediatric patients in comparison to IDSA
treatment guidelines and to local susceptibility patterns.
Methods: This retrospective chart review evaluated pediatric patients admitted to the pediatric
floor of a regional academic medical center. Patients were included in the evaluation if they had
a positive chest x-ray, an inpatient order for antibiotic therapy, and were older than 3 months but
less than 18 years. Patients were excluded if they had a recent history of antibiotic treatment for
pneumonia or were diagnosed with aspiration pneumonia, viral pneumonia, or cystic fibrosis.
Electronic medical records were evaluated and the following information was collected: sex,
allergies, weight, age, antibiotic prescribed (date and dose), chest x-ray results, history of lung
disease, and history of previous admission for pneumonia. Pre-intervention data were collected
over a period of 3 weeks then data were compiled into a brief presentation for pediatric medical
residents. Residents were also provided a reference card containing current antibiotic treatment
guidelines for CAP. Post-intervention data were collected over a period of 4 weeks and the
results were analyzed using a chi-square statistical test. An alpha of 0.05 was selected a-priori.
This was a quality improvement project therefore it did not meet the federal definition of
research and Institutional Review Board (IRB) approval was not required according to
University guidance.
Results: The medical records of 45 pediatric pneumonia patients between the ages of 5 months
and 15 years were analyzed. During the pre-intervention period, ampicillin, ceftriaxone, and
amoxicillin were prescribed 7, 23, and 41 percent of the time, respectively. Post-intervention,
ampicillin, ceftriaxone, and amoxicillin were prescribed 32, 8, and 38 percent of the time,
respectively. A statistically significant difference was found between pre- and post-intervention
ampicillin prescribing (P equals 0.015).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Adherence to the IDSA pediatric CAP guidelines for parental therapy improved
after an educational intervention. A statistically significant 5-fold increase in ampicillin
prescribing was observed. This finding suggests that educational interventions may improve
adherence and outcomes. Future research could aim to examine the relationship between patient
outcomes, such as length of stay or length of infusion therapy, and antibiotic prescribed.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-054
Title: Review of insulin alerts in a smart pump system at a tertiary hospital
Primary Author: Brian Do, University of Arizona College of Pharmacy, Arizona;
Email: briando@pharmacy.arizona.edu
Additional Author(s):
Christopher Edmonds
Sebastian Mak
Cynthia Ling
Jacqueline Brody
Purpose: The purpose of this quality improvement (QI) project is to reduce alert fatigue by
creating more meaningful alerts in the intensive care unit (ICU) setting of a tertiary teaching
hospital. The facility uses smart pump electronic intravenous medication administering devices
with preset settings.
Methods: This prospective, cross sectional project analyzed the difference in outcomes after
implementing a new clinical advisory for insulin in the ICU profile for smart pumps in a tertiary
hospital. This new protocol provided an option for low dose insulin and high dose insulin. Low
dose insulin was defined as doses lower than 30 units per hour and high dose insulin was defined
as any dose higher than 31 units per hour. The measured outcomes were the number of soft and
hard limit alerts triggered and the number of times nurses overrode these alerts. Hard limits are
drug administration limits that cannot be overridden by the nursing staff, whereas soft limits can
be overridden. The difference in the number of times an alert was overridden and absolute
overall number of alerts were compared using descriptive statistics and chi square analysis. An
alpha of 0.05 was selected. This is a QI project therefore it does not meet the Federal definition
of research and Institutional Review Board approval is not required as per University guidance.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-055
Title: Weight based continuous intravenous insulin dose-related hypoglycemia in obese patients
Primary Author: Paul Frey, The University of Arizona College of Pharmacy, Arizona;
Email: frey@pharmacy.arizona.edu
Additional Author(s):
John Radosevich
Holly Paddock
Yong Gu Lee
Brian Erstad
Purpose: There are limited studies regarding dosage adjustments in obesity. The use of high
doses of insulin in obese patients treated in intensive care units (ICU) can lead to increased risk
of hypoglycemia. A better understanding of the relationship between insulin dosing and
hypoglycemia may facilitate more effective dosing, thus reducing the risk of hypoglycemia. The
objective of this study is to evaluate the number of patients that experienced a hypoglycemic
event and the clinical outcomes of those patients.
Methods: This retrospective study was approved by the Institutional Review Board. The study
will involve a comparison of continuous intravenous insulin therapy and rates of hypoglycemia
(blood glucose < 70 mg/dL) based on point-of-care (POC) capillary glucose values. Clinical data
will be obtained through a chart review and will then be divided into two groups, obese and nonobese patients admitted to an ICU. Data collection will focus on age, sex, height, weight, race,
body mass index (BMI), insulin dosing, blood glucose readings, timing of hypoglycemia, total
daily insulin received, pertinent laboratory parameters, and patient outcomes. Data will be
compiled into Microsoft Excel for descriptive and inferential analyses. To analyze the
descriptive and demographic data, we will compare the categorical variables by the Chi-squared
test. The analysis will be performed according to whether subjects are non-obese
(BMI<30kg/m2) or obese (BMI>30kg/m2). Additionally, the data will be analyzed according to
the following BMI subsets: normal 18.5 to 24.9 kg/m2, overweight BMI 25 to 29.9 kg/m2, obese
30 to 39.9 kg/m2, and morbidly obese BMI 40 kg/m2 or greater.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-056
Title: The effect of follow-up phone calls after patient discharge on 30-day hospital readmission
rates
Primary Author: Kristen Fyfe, University of Arizona College of Pharmacy, Arizona;
Email: fyfe@pharmacy.arizona.edu
Additional Author(s):
Tiffany Lee-Chan
Heather Marrow
Terri Warholak
Janet Cooley
Purpose: Medication reconciliation is an important part of comprehensive health care delivery.
It allows both physicians and pharmacists to effectively manage patients medications by
minimizing or eliminating the complications arising from duplicate or inappropriate therapy and
ineffectual communication. The purpose of this study is to examine the effect of a follow-up
phone call upon patient discharge and discharge medication reconciliation on 30-day
readmission rates at an Arizona teaching hospital.
Methods: Men and women aged 18 years and older who provided informed consent participated
in this prospective, pre-post study. Patients under the age of 18 were excluded, as were those
who were discharged to home health services or skilled nursing facilities currently admitted to
the hospital, unable to be contacted, discharged without any medications, or were non-English
speakers. The intervention consisted of a scripted follow-up phone call to each patient after
discharge. At three to seven days post-discharge, a pharmacy student on an advanced pharmacy
practice experience rotation at a teaching hospital called each patient discharged from a
designated ward and collected information regarding prescription filling, understanding of
medication(s), concerns regarding medications, and the community pharmacy he/she used to fill
the discharge medications. The specified community pharmacy was then called to verify that the
patient filled discharge medications at that pharmacy. Patient readmissions were tracked using
medical record numbers. The results were compared to the readmission rate in the same ward
over the same time period one year prior to implementation of the intervention. Chi-square and
descriptive analysis will be used and the alpha a priori is 0.05. The institutional review board
approved this study.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-057
Title: Arizona community pharmacy quality assurance legislation: evaluation of attitude and
knowledge change after attending a continuing education program
Primary Author: Kristina Gerboth, University of Arizona, Arizona;
Email: kgerboth@email.arizona.edu
Additional Author(s):
Patrick Campbell
Terri Warholak
Purpose: On April 18, 2007, the Arizona legislature passed the Pharmacy Quality Assurance
law. The law requires all community pharmacies to have a continuous quality assurance program
in place by January 1, 2014. Pharmacists knowledge and attitudes about quality assurance are
important to evaluate since they are integrally linked with legislation compliance. The purpose of
this program evaluation is to assess pharmacy staff knowledge of the Arizona Pharmacy Quality
Assurance legislation and to identify changes in knowledge and attitudes associated with the
quality assurance process after the continuing education session.
Methods: This cross sectional program evaluation consisted of a paper-based retrospective
preassessment postassessment evaluation that was completed by participants after a two-hour
live continuing pharmacy education symposium. The continuing education session was offered
during the Community Pharmacy Academy Conference hosted by the Arizona Pharmacy
Association on September 22, 2012. When completing the assessment instrument at the end of
the session, participants rated themselves on the level of knowledge, motivation, and awareness
of quality assurance and medication errors they possessed before attending and after attending
the educational session. Descriptive variables including practice setting, job title, length of
pharmacy work experience, type of quality related event reporting system in place at
employment location, and history of quality assurance exposure were collected. A Wilcoxon
Signed-Rank will be utilized to evaluate participant questionnaire results. The analysis will
include a Boniferroni correction value to control for type I errors. Both of these calculations will
be done using SPSS software. Program evaluations are not classified as human subject research
as per federal regulations and University guidance and this evaluation was exempted by the
Institutional Review Board; the results are not generalizable to other populations or settings.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-058
Title: Quality assessment of smart pump intravenous infusion technology at an inpatient
university medical center
Primary Author: Matthew Grimes, University of Arizona College of Pharmacy, Arizona;
Email: grimes@pharmacy.arizona.edu
Additional Author(s):
Parissa Moghimi
Marie Ngan
Hershil Parekh
Charles Marsalla
Purpose: Medications administered by intravenous infusion are a common source of error
contributing to patient morbidity and mortality. Smart pump technology, which utilizes
pharmacy approved dosage limits and patient specific drug libraries, has been developed to help
minimize the risk of infusion error. However, only correctly programmed smart pumps will
provide the additional safety features, so nursing staff programming accuracy is essential. If
nurses become desensitized to alerts and choose to manually program infusions, they negate the
safety technology. The purpose of this project was to determine if audits of programming
compliance would increase proper utilization of smart pump technology.
Methods: Because this quality improvement project was not generalizable, human subject
approval was deemed unnecessary as per Institutional Review Board guidance. Audits were
conducted at three sites: an inpatient hospital, and two satellite cancer clinics. The auditors
surveyed whether programming parameters were input correctly. The parameters included:
patient profile type, unit identification number, medication selection, dosing within limits, and
connection tubing alignment. A baseline audit was performed to determine programming
compliance prior to intervention. Baseline data were analyzed, compiled into reports, and sent to
the charge nurses of each unit or facility. The charge nurses were given four weeks to train their
staff to improve programming compliance. A follow up audit was performed after the
intervention period and the data were compared to the baseline findings. Statistical analysis was
completed using chi squared analysis with an a priori alpha value of 0.05.
Results: Overall programming of intravenous drug channels increased by 8.7 percent (P equals
0.184) between baseline and follow up. Changes in programming compliance for each of the
observed parameters were as follows: patient profile type showed no change (compliance was
100 percent at baseline and 100 percent at follow up), correct unit identification number
decreased by 1.4 percent (P equals 0.648), correct medication selection increased by 4 percent (P
equals 0.231), dosing within predetermined limits increased by 2.5 percent (P equals 0.505), and
proper alignment of connection tubing decreased by 2.5 percent (P equals 0.0503).
Conclusion: The results of this project showed no statistically significant change in
programming compliance of any of the observed parameters. This may have resulted from an
insufficient intervention time between audits, or may suggest that a more aggressive intervention
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
is needed. It is evident that adherence to smart pump technology is an area with need for
improvement. Significant progress could be made through regular and consistent auditing of
smart pump usage. With further data collection it would be possible to elucidate a more accurate
assessment of overall programming compliance, as well as compliance improvement over time.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-059
Title: Therapeutic drug monitoring and dose adjustment of posaconazole in adult patients with
acute myeloid leukemia: a single-center experience
Primary Author: Shelly Hummert, University of Arizona, Arizona;
Email: hummert@pharmacy.arizona.edu
Additional Author(s):
Myke R. Green
Purpose: Posaconazole is an extended-spectrum triazole antifungal indicated for prophylaxis in
adults with acute myeloid leukemia (AML) receiving intensive remission induction
chemotherapy. Due to narrow therapeutic index and poor absorption, therapeutic drug
monitoring may be necessary in order to obtain maximal efficacy. However, a paucity of data
exists evaluating therapeutic drug monitoring and dose adjustment based upon serum
concentrations. The primary objective of this study is to evaluate serum posaconazole
concentrations following dose adjustment in response to subtherapeutic serum concentrations.
Other objectives include determination of optimal dose adjustment schema and toxicity with
doses above 200 mg per os three times daily.
Methods: Following approval by the University of Arizona institutional review board, the
electronic health record was queried for patients age > 18 years with AML who were initially
receiving posaconazole 200 mg per os three times daily as prophylaxis concurrent with intensive
remission induction therapy and required at least 1 dose adjustment secondary to a
subtherapeutic posaconazole serum concentration between October 2008 - December 2012.
Patients were excluded if received < 5 days of posaconazole following the first dose adjustment.
Data collection will include patient demographics, organ function tests, posaconazole dose &
administration schedule, posaconazole serum concentration, and compliance with ancillary
agents employed to maximize absorption. Planned statistical analyses include percentage change
in serum concentration relative to posaconazole dose & schedule, successful achievement of goal
serum concentration and toxicity with higher posaconazole doses. Data will be analyzed using
descriptive statistics.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-060
Title: Comparison of pharmacy intern and nurse impact on home medication list completeness
during medication reconciliation
Primary Author: Michael Ivey, University of Arizona College of Pharmacy, Arizona;
Email: mivey@pharmacy.arizona.edu
Additional Author(s):
Ferena Salek
Linda Calkins
Purpose: Medication reconciliation is an essential process in the hospital setting; it consists of
acquiring a patients current home medication list so that their medications can be continued
during the hospital stay and after discharge. If not performed accurately and completely, the
medication reconciliation process can be a source of future medication errors. In contrast to a
nurse-driven medication reconciliation process, some institutions now utilize pharmacy interns to
perform this duty. The purpose of this evaluation is to compare completeness of home
medication lists obtained by either pharmacy interns or nurses in a hospital.
Methods: This quality improvement project will be a retrospective review of completed home
medication lists obtained by pharmacy interns or nurses in a Southern Arizona community
hospital. Since this project did not meet the federal definition of research, it was considered IRB
exempt. During August and September 2013, medication lists from the previous days admissions
will be collected and de-identified. Medication lists will be included in the evaluation if the
patient was admitted directly to the hospital or through the emergency department, stayed for at
least 24 hours and had at least one home medication upon admission. The primary outcome will
be the number of omissions on home medication lists completed by pharmacy interns or nurses.
An omission will be defined as any missing information in the medication list categories of drug
name, dose, unit, route and frequency. The secondary outcome will be the number of substantive
errors on the completed home medication lists. Substantive errors will be defined as any
therapeutically incorrect or inappropriate errors created by the group performing medication
reconciliation. Fifty medication lists will be collected from each group. The total number of
omissions and substantive errors between groups will be compared using a chi-square test.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-061
Title: Synthesis and evaluation of an ASPH inhibitor
Primary Author: Grace Jang, Midwestern University, College of Pharmacy - Glendale,
Arizona;
Email: gjang91@midwestern.edu
Additional Author(s):
John-Michael Thomas
Arihiro Aihara
Jack R. Wands
Mark J. Olsen
Purpose: Hepatocellular carcinoma (HCC) and pancreatic adenocarcinoma have poor prognosis,
and outcomes have not been impacted by traditional chemotherapeutic agents. Current
therapeutic options include surgery and sorefenib, but neither option has demonstrated a
significant increase in 5-year survival for late stage HCC. There is a need for targeted drug
therapy for these two cancers.
Methods: Previous research has demonstrated that aspartate-ß-hydroxylase (ASPH) is highly
expressed on the surface of these cancer cell types, and this enzyme is directly linked to
proliferation, migration and invasiveness. Recently, we have identified an ASPH inhibitor, MOI-1100, with the ability to suppress HCC proliferation, migration, and invasiveness. MO-I-1100
has also demonstrated activity in a nude mouse model against a subcutaneous injected
dedifferentiated HCC cell line (FOCUS).
Results:
Conclusion: This poster presents the design, synthesis, and activity of MO-I-1100 and analogs
against HCC and pancreatic cancer.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-062
Title: Use of standardized counseling points to improve quality of nursing-lead discharge
counseling
Primary Author: Vanessa Jordan, University of Arizona College of Pharmacy, Arizona;
Email: jordan@pharmacy.arizona.edu
Additional Author(s):
Vanessa Gaerig
Jinjie Huang
Manfei Jiang
Brent Hall
Purpose: Medication counseling for pediatric patients remains a challenging part of the
discharge process in hospitals. Inadequate patient/caregiver education can lead to increased
readmission rates and unexpected hospital or clinic visits, so inpatient nursing staff serves a vital
role in this process. Recent publications suggest that collaboration between nursing and
pharmacy staff can reduce readmission rate after discharge. It was hypothesized that providing
the nursing staff with counseling points that focused on commonly prescribed discharge
medications would enhance the patients and/or their caregivers understanding of medication use;
in turn, this would improve overall clinical outcomes by decreasing readmission rates.
Methods: Itemized counseling pamphlets containing administration techniques, dosing
information and major side effects of five commonly prescribed medications were developed.
This quality improvement intervention aided the nursing staff in delivering comprehensive
medication education to the patients and/or their caregivers upon discharge. In spring 2013,
patients from birth to age 21 years who had been discharged from a regional academic medical
centers pediatric wards on one or more of the five selected medications were contacted for this
study. These patients or their caregivers participated in a telephone questionnaire 12 to 16 days
post-discharge. The questionnaire assessed the patients or caregivers basic understanding of the
discharge medication(s) and how other discharge-related processes were conducted. The preintervention group received standard discharge education by the nursing staff; the postintervention group was counseled with the aid of the intervention. Patient readmission rates were
used to assess the overall clinical outcome of this intervention. A Chi-squared test with an alpha
level of 0.05 was used. This was a quality improvement project; therefore, it did not meet the
federal definition of research, and Institutional Review Board approval was not required.
Results: Sixty-one telephone questionnaires were completed for the pre-intervention group;
thirty-four were completed for the post-intervention group. Between the two groups, the postintervention group showed an increase in the number of positive responders who had been
counseled by a nurse on proper use of their discharge medications (78 percent pre-intervention
versus 91 percent post-intervention, p equals 0.01). All other measures did not reach statistical
significance. The questionnaires showed that nurses at the regional academic medical center
were frequently covering both general and medication-specific counseling points. Rates of
readmission due to the same condition or complications from the original admission were
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
approximately the same in both groups, indicating that the intervention had no significant clinical
outcome.
Conclusion: Pamphlets containing key counseling information were provided by pharmacy and
proved efficacious in improving the frequency of nurse-lead counseling on discharge
medications. No statistically significant differences were identified in the patient's or caregivers
knowledge of discharge medications; there was also no difference in readmission rate. Due to
small sample size, low readmission rate, and language barriers, further investigation may be
needed.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-063
Title: Prevalence and willingness of mothers in a local support group to ask pharmacists for
pediatric dosing of over the counter (OTC) products: a descriptive study
Primary Author: Katrina Kittell, University of Arizona/ PharmD Candidate 2014, University of
Arizona/Arizona;
Email: kittell@pharmacy.arizona.edu
Additional Author(s):
Jacquelyn Adkins
Jenene Spencer
Purpose: Pharmacists are very accessible for the public to ask questions about their prescription
medications or over the counter (OTC) medications. This becomes important for pediatric OTC
medications as the directions for use are not always clear or specific, especially in regards to
dosing. The purpose of this study is to assess the prevalence of mothers asking pharmacists for
pediatric dosing of OTC medications and to assess their baseline knowledge about the
appropriate use of OTC medications in pediatrics.
Methods: An application was approved by the Institutional Review Board. This descriptive
study will obtain data through the use of an online questionnaire. To be eligible for this study,
participants need to be 18 years or older and must be mothers with at least one child under the
age of six and be part of Tucson Moms, a local organization facilitating communication and
camaraderie of mothers and their children. A link to a survey containing 19 questions will be
emailed out weekly over the course of a month through the Tucson Moms listserv and posted to
the groups social media website. The survey will become available after the participants read a
consent statement and agree to continue. The primary dependent variable is utilization of
pharmacists for pediatric OTC medication information. The secondary dependent variable is the
knowledge assessment of pediatric OTC medications. Continuous variables will be ages and
number of children. Categorical variables will include pharmacist utilization, knowledge based
questions, and certain demographic information. The categorical variables will be analyzed using
Chi Squared tests. The continuous variables will be analyzed using t tests. The a priori alpha
level is 0.05.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-064
Title: Direct costs of unnecessary antibiotic prescribing in patients administered imipenem in the
emergency department
Primary Author: Michael Klein, University of Arizona College of Pharmacy, Arizona;
Email: mklein@pharmacy.arizona.edu
Additional Author(s):
Kathryn R Matthias
Purpose: The purpose of this study is to examine the appropriateness of antibiotic use in patients
prescribed imipenem in the emergency department and the direct costs associated with
unnecessary antibiotic prescribing. The central hypothesis is that pharmacists can identify
appropriate prescribing patterns of antibiotics a posteriori and make suggestions to improve
prescribing in case suboptimal prescribing is identified. The rationale of this study is to identify
any discrepancies in antibiotic prescribing in patients given broad-spectrum antibiotics to prevent
future misuse of antibiotics and to minimize institutional costs by avoiding antibiotic waste.
Methods: This study is an IRB approved retrospective chart review with waived subject consent.
Subjects over 18 years old who were administered imipenem within 48 hours of admission to the
emergency room at a tertiary care, academic medical center between January 1, 2013 and March
31, 2013 and spent at least 72 hours in the hospital were included in the study. Eligible subjects
were screened until 50 patients were included in the study to allow for a sufficient sample size
for analysis. All antibiotics received within the first 48 hours of admission were noted.
Demographic characteristics, co-morbid conditions, and immunosuppression state were
characterized. Patients were considered high risk if they had 1) resided in a skilled nursing or
assisted living facility within the last 30 days 2) had antibiotics within 90 days 3) had an
outpatient procedure or been discharged from the hospital within 30 days or 4) were intravenous
drug users. Two pharmacists specializing in antimicrobial therapy will assess the appropriateness
of antibiotics used by collecting differential and final diagnosis and culture and susceptibility
data from each patient. The direct cost of all antibiotics administered to each subject and the cost
of inappropriate or duplicative therapies will be determined.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-065
Title: Efficacy of low dose levetiracetam for seizure prophylaxis in traumatic brain injury
Primary Author: Alina Kurita, University of Arizona College of Pharmacy, Arizona;
Email: kurita@pharmacy.arizona.edu
Additional Author(s):
Elaine Truong
Asad Patanwala
Purpose: Guidelines from the Brain Trauma Foundation recommend that after traumatic brain
injury (TBI) patients should be given seizure prophylaxis for up to seven days. Currently,
phenytoin is the first line therapy for this indication. However, levetiracetam is increasingly
being used as an alternative because it does not require serum concentration monitoring and has
a desirable safety profile. Studies evaluating levetiracetam have used a loading dose, followed by
a maintenance dose of 1000 mg every 12 hours. The primary objective of this study was to
evaluate the efficacy of low-dose (500 mg every 12 hours) levetiracetam for seizure prophylaxis
after TBI.
Methods: This was a retrospective cohort study conducted in a tertiary care, academic institution
that is designated as a level 1 trauma center. Institutional review board approval was obtained
prior to data collection. Consecutive patients with TBI between 2010 and 2012, who received
levetiracetam for seizure prophylaxis, were included. Patients who met at least one of the
following criteria were included: cortical contusion on computerized tomography scan, subdural
hematoma, epidural hematoma, intracerebral hematoma, depressed skull fracture, penetrating
head injury, or Glasgow Coma Scale (GCS) of 10 or less. Patients were excluded if they were
less than 16 years of age, had a previous head injury, previous neurosurgery, history of seizure,
or anti-seizure medication, or were given a loading dose of levetiracetam, or given a maintenance
dose greater than 500 mg every 12 hours. The primary outcome was the occurrence of a seizure
within seven days of TBI. A one-sample test of proportions was used to compare the rate of
seizures while being treated with levetiracetam to a hypothesized value of 3.6 percent (from
previous trials), using an a priori alpha for 0.05.
Results: There were a total of 146 patients included in the study, who were treated with
levetiracetam 500 mg every 12 hours. The median age was 51 years (interquartile range 31 to 65
years), 110 (75 percent) were male, and the median GCS on admission was 11 (interquartile
range 5 to 14). The mechanisms of injury were fall (n equals 49), motor vehicle or motorcycle
collisions (n equals 42), pedestrian or bicyclist (n equals19), assault (n equals16), suicide attempt
(n equals 2), and other (n equals18). The median time to first dose of levetiracetam was 4 hours
after injury (interquartile range 1 to 13 hours). After initiation of levetiracetam, there were 5 (3.4
percent) patients who had a seizure within seven days. This was not significantly different than
the hypothesized population value (p equals 0.910). The median length of stay was 13 days
(interquartile range 9 to 21) and 7 (4.8 percent) patients died during hospitalization.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: A low-dose of levetiracetam 500 mg every 12 hours after TBI was effective for
early seizure prevention. This regimen may be an appropriate alternative to phenytoin or
traditional dose levetiracetam for this indication. Future, prospective studies are needed to
confirm these findings.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-066
Title: Stenotrophamonas maltophilia and time to appropriate antibiotic therapy
Primary Author: Amelia Kwong, University of Arizona, Arizona;
Email: ameliak@email.arizona.edu
Additional Author(s):
Jenny Zhu
Kathryn Matthias
David E. Nix
Purpose: Stenotrophamonas maltophiliais a problematic pathogen due to its intrinsic resistance
to many antibiotics that are used for empiric therapy in acutely ill patients. Since prior or empiric
antibiotic therapy may not always cover Stenotrophamonas maltophilia, the time to identification
of the organism from a patient sample may affect the time to appropriate therapy. The objective
of this study is to determine when appropriate therapy for Stenotrophamonas maltophilia
infections were prescribed and potential factors associated with the delay in initiation of
appropriate therapy before implementation of a laboratory method for earlier species
identification.
Methods: In this IRB-approved retrospective study with waived informed consent, the time to
identification of Stenotrophamonas maltophilia along with time to appropriate antibiotic therapy
and time to streamlined therapy will be evaluated as baseline data before implementation of mass
spectrometry for earlier species identification. Subject selection included all patients with
Stenotrophamonas maltophilia isolated from any source while admitted to a tertiary care,
academic medical center between June 1, 2011 and May 31, 2012. Patients with initial
Stenotrophamonas maltophilia isolate from a post-mortem sample were excluded. Appropriate
antibiotic therapy was based on susceptibility data reported for each isolate of Stenotrophamonas
maltophilia, site of infection, and patient characteristics. Potential appropriate therapy that will
be evaluated includes high-dose sulfamethoxazole-trimethoprim, ticarcillin-clavulanate plus
aztreonam, moxifloxacin or levofloxacin, and ceftazidime. Clinical notes will be reviewed to
evaluate if organism was classified as a colonizer or caused an infection for each subject.
Primary endpoints will be time to isolate identification, time to appropriate antibiotic therapy,
and time to streamlined antibiotic therapy.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-067
Title: Assessing student satisfaction from redesigned review for objective structured clinical
examination (OSCE)
Primary Author: Ibrahim Lala, Midwestern University - College of Pharmacy, Glendale,
Arizona;
Email: ilala43@midwestern.edu
Additional Author(s):
Julie Nguyen
Paul Nguyen
Lara Petrossian
Chiu Tong
Purpose: Peer education is an integral part of a complete and successful curriculum. While there
are multiple instances of peer education at Midwestern University - College of Pharmacy
Glendale, assessing the appropriateness and efficacy of these peer education programs is an area
that is lacking. This project was designed to assess whether a particular program - a seminar
designed to help first year pharmacy students prepare for their objective structured clinical
examination - was beneficial for the students, and in what ways the seminar could improve. This
project is important in informing those who design peer education programs what they should
focus on, and how best to reach their peers.
Methods: After presenting a two-hour review seminar and disseminating an electronic version of
the presentation, a survey was sent out to those who attended the seminar and to those who
received an electronic copy. The survey was distributed after the results of the exam were
received by the students. The survey consisted of a total of 16 Likert-scale rating questions and
free-response questions. Subjects received three total notices of the survey, which remained open
for 17 days. Students then answered the anonymous survey, which assessed whether each
particular portion of the seminar (in this case, a review of the material that would on the
upcoming exam) was beneficial, and how it could be improved. It was not required to complete
the survey in its entirety.
Results: All questions were answered by a minimum of sixty three and a maximum of seventy
students. Overall, 100% of students indicated that they found the seminar to be helpful in
preparation for the exam. For a specific subject portion of the seminar, a minimum of 79% and a
maximum of 100% of students agreed or strongly agreed that it was beneficial in preparation for
the exam. 97% of students indicated that they would encourage future students to attend a similar
review seminar. The open ended questions provided feedback as to what could be improved
during the seminar, such as "provide more examples" or "provide more detail" for a particular
disease state.
Conclusion: The seminar was beneficial in preparing students for their upcoming objective
structured clinical examination. An assessment of each individual portion of the seminar
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
indicated what portions need to be strengthened in future seminars, and what portions worked
well.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-068
Title: Medication error identification rates by pharmacists, physicians, and nurses
Primary Author: Brian Lamhang, University of Arizona, Arizona;
Email: brianlamhang@gmail.com
Purpose: Pharmacists can play an important role as an active member of the patient care team
especially when they are incorporated into the checks and balances of the prescribing process.
Many healthcare professionals can identify prescription errors, but pharmacists education
focuses on medication knowledge and they are therefore uniquely poised to identify possible
prescribing problems that can result in a serious adverse event. The Joint Commission standard
requires that pharmacists review all prescription or medication orders unless a licensed
independent practitioner controls the ordering, preparation, and administration of the medication
or in urgent situations when the resulting delay would harm the patient. When pharmacists are
involved in the prescribing process, the interprofessional team is able to maximize the patients
health care as well as minimize medication errors because the pharmacist's expertise can be
utilized in many ways that can benefit nurses, physicians as well as patients. The purpose of this
study is to determine if pharmacists are able to identify more prescribing errors, or more complex
prescribing errors, compared to other healthcare professionals such as physicians and nurses. In
addition, we will be assessing the validity of a medication error knowledge assessment
instrument in the health professional population.
Methods: This study will use a randomized, cross-sectional design. Pharmacists, physicians, and
nurses from three institutional locations: University of Arizona Medical Center, Tucson Medical
Center, and Northwest Medical Center will be eligible to participate. The questionnaire will
consist of 10 fictitious patient prescriptions and additional patient-related information (name,
date of birth, weight, and diagnosis for the prescription under consideration, drug allergies, and
current medications) that may assist in the decision-making of the healthcare professionals. The
questionnaire was designed using the top 200 medications dispensed in 2011 by total
prescriptions obtained from the pharmacy times. Participants will be given an email invitation
containing a link to the questionnaire powered by Adobe. A cover letter, before the survey,
describing the rationale behind the survey will be included in the email. The researcher will
provide consent to participate in the one-time survey. They will be allowed to finish within 10
minutes. The data collected for this study will include whether the question was answered
correctly, location of work, occupation, years of field experience, and other participant
demographics.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-069
Title: Economic impact of pharmacokinetic monitoring on the use of oral (PO) and intravenous
(IV) busulfan in patients undergoing hematopoietic stem cell transplantation (HSCT)
Primary Author: Marti Larriva, University of Arizona College of Pharmacy, Arizona;
Email: larriva@email.arizona.edu
Additional Author(s):
Stephen Karpen
Ivo Abraham
Christopher Campen
Erin Ballard
Purpose: Intravenous busulfan has been widely adopted as a safer alternative to the less costly
oral formulation based upon studies that found it decreased the rates of hepatic venoocclusive
disease (HVOD). However, HVOD is associated with the busulfan area under the curve (AUC)
and these studies did not conduct therapeutic drug monitoring (TDM) in both IV and PO arms.
The purpose of this project is to evaluate the economic impact of the adverse effect profile of
busulfan in light of TDM of IV and PO busulfan when used as part of a conditioning regimen for
HSCT.
Methods: This observational retrospective project is using data from a cohort of patients
obtained through charts from an academic medical center in Tucson, AZ. Subjects included in
the project are 18 years of age or older and treated with either IV or PO busulfan as part of
conditioning for HSCT from January 2007 to April 2013. The following baseline data is being
collected: age, disease, preexisting lung or liver disease, number of previous transplants,
concurrent GVHD prophylaxis, CD34 dose, and previous chemotherapy agents. The outcome
data to be analyzed include: cost of treatment, busulfan dose and AUC, 100-day mortality,
duration of hospital stay, presence and severity of mucositis, presence of pulmonary toxicity, and
presence and severity of HVOD. All data is being de-identified and maintained confidentially.
Analysis of this data will include separating patients by treatment route and determining
differences in the presence or severity of toxicities. Additionally, a decision tree analysis will be
performed to determine the incremental cost effectiveness ratio for IV vs. PO busulfan. This
project is considered quality improvement for the associated academic medical center and is
recognized as exempt from institutional review board approval.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-070
Title: Educational interventions to increase baseline metabolic monitoring for second-generation
antipsychotics in an acute inpatient psychiatric setting
Primary Author: Yong Gu Lee, University of Arizona, Arizona;
Email: yonglee@pharmacy.arizona.edu
Additional Author(s):
Phalyn Butler
Echo Fallon
Amelia Kwong
Lisa W. Goldstone
Purpose: Second-generation antipsychotics (SGA) can cause a metabolic syndrome, which
increases the risk of cardiovascular disease and ultimately, mortality. Currently, many healthcare
institutions do not follow the American Diabetes Association/American Psychological
Association (ADA/APA) guidelines for obtaining baseline assessments when starting a SGA in
treatment nave patients. By obtaining baseline measures of weight, waist circumference, blood
pressure, fasting blood glucose, and lipids, healthcare practitioners can monitor these values and
prevent patients from developing associated co-morbidities and cardiovascular mortality. The
purpose of this quality improvement project was to measure the rate at which baseline labs were
obtained before and after an educational intervention.
Methods: As this was a quality improvement project, approval from the Institutional Review
Board was not required. However, permission to conduct this project was granted by the Medical
Office at The University of Arizona Medical Center South Campus. An educational intervention
was developed to alert the attending physicians and residents of the inpatient behavioral health
units at a local institution of the importance of getting baseline lab values for patients on a SGA.
Two separate presentations were given to the attending physicians and residents informing them
of the suggested baseline monitoring parameters and frequencies, and pocket cards with these
parameters and frequencies were distributed. A retrospective chart review was conducted both
pre- (n = 198) and post- (n = 212) intervention to assess whether the following monitoring
parameters had been acquired: family history, weight, waist circumference, blood pressure,
plasma glucose, and a lipid panel. Data were analyzed using the Chi-Square test to determine the
effectiveness of the educational presentations, with a priori alpha level set at 0.05.
Results: Post-intervention data indicated that, similar to pre-intervention data, weight and blood
pressure data were obtained nearly 100% in the total patient population. Similarly, waist
circumference remained unchanged (0%). Compared to pre-intervention data, post-intervention
data showed increased documentation of family history (11.6% vs. 15.6%), plasma glucose
(85.9% vs. 93.9%) and lipid panels (4.5% vs. 10.4%). A significant difference in the total sample
of the treatment naive and non-treatment naive patients with respect to plasma glucose readings
and lipid panels (p = 0.007 and 0.026, respectively) was observed. In sub-group analysis between
treatment and non-treatment nave patients, the only significant difference was an increase in
frequency of non-treatment naive patients plasma glucose level monitoring (p = 0.007).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The data showed that significantly more lipid panels were ordered postintervention. Improvements may be attributed to successful intervention and education, and it is
possible that additional instruction or reminder methods would further improve monitoring.
More should be done to ensure proper baseline assessment in patients receiving a SGA to aid in
proper follow-up and long-term monitoring and ultimately, better safety outcomes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-071
Title: Institutional compliance with NCCN guidelines for the use of granulocyte colony
stimulating factors for primary prophylaxis
Primary Author: Shannon Lim, The University of Arizona, Arizona;
Email: lim@pharmacy.arizona.edu
Additional Author(s):
Jacob Frick
Michael Hebert
Purpose: Bone marrow suppression is the most common dose-limiting toxicity of cancer
chemotherapy. Severe or prolonged neutropenia is associated with an increased incidence of
febrile neutropenia (FN), which may result in extended hospitalization, use of broad-spectrum
antibiotics, and significant morbidity and mortality. Dose reductions of chemotherapy agents or
treatment delays are often used in subsequent cycles to abrogate the adverse effect on bone
marrow. Such modifications result in decrease dose intensity which may compromise clinical
outcomes. The prophylactic use of granulocyte colony stimulating factors (G-CSFs) has been
shown to reduce the incidence, severity and duration of chemotherapy-induced neutropenia in
patient receiving myelosuppressive chemotherapy; however its cost has prevented its routine use.
Therefore, the selective use of G-CSFs in patients at increased risk for neuropenic complications
is warranted. Organizations including the National Comprehensive Cancer Network (NCCN)
have published guidelines related to the recommended use of colony stimulating factors. The
objective of this study is to determine the adherence to the NCCN guidelines recommendations
for the use of G-CSF as primary prophylaxis.
Methods: This retrospective medical record review determined the hosptials adherence to the
NCCN Guidelines Myeloid Growth Factors (version 1.2012) recommendations for the use of GCSF as primary prophylaxis. The hospitals electronic medical record system was used to identify
patients who received G-CSFs including filgrastim and pegfilgrastim from October 2011 through
September 2012. The data collected included the G-CSF used (pegfilgrastim or filgrastim);
whether the patient received G-CSF following the first cycle of chemotherapy; the patients
chemotherapy regimen; the neutropenic risk of the chemotherapy regimen per the NCCN
guidelines; and whether or not patient specific risk factors were present. Patient specific risk
factors included age older than 65, previous myelosuppresive chemotherapy or radiotherapy,
Eastern Cooperative Oncology Group (ECOG) performance status of 3 or 4, poor renal (CrCl <
30 mL/min) or hepatic function (total bilirubin > 3x upper limit normal), and pre-existing
conditions such as pre-existing neutropenia, bone marrow involvement, or open infection. Use
was determined to be adherent to guidelines if patient at high risk (>20%) or intermediate risk
(10-20%) of developing FN was given G-CSF as primary prophylaxis. Patients who received GCSF with a low-risk chemotherapy regimen, one additional risk factor was required in order to
be considered adherent.
Results: Between October 2011 and September 2012, a total of ninety-nine patients were
identified as receiving primary prophylaxis with G-CSF. Use of G-CSF as primary prophylaxis
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
was determined to be adherent to guidelines for 100% of patients who were evaluated. It was
also determined that 38 (38.3%) patients were on chemotherapy for curative intent, 56 (56.6%)
patients were on chemotherapy without intention of cure, and 5 (5.0%) patients intent of cure
was unknown. In this evaluation, 10 (10.1%) patients received filgrastim and 89 (89.9%) patients
received pegfilgrastim. In addition, 8 (8.1%) patients were on a chemotherapy regimen
consistent with a low risk of developing FN, 66 (66.7%) patients were on an intermediate
chemotherapy regimen, and 25 (25.3%) patients were on a high risk chemotherapy regimen. All
8 patients on a chemotherapy regimen associated with low risk of developing FN had one
additional risk factor, which therefore considered the use of G-CSF in these patients adherent to
the guidelines.
Conclusion: In this evaluation, all G-CSF use was adherent within guidelines for appropriate
primary prophylactic use, however it is limited by its retrospective nature. However, this data
can be used to provide direction for future evaluation of G-CSF use in the non-curative setting,
as there are a large proportion of patients receiving G-CSF in this circumstance. In addition
future studies could target patients receiving G-CSF for primary prophylaxis with intermediate
and low risk regimens.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-072
Title: Inpatient management of blood pressure and fluid overload in patients with end-stage
renal disease on hemodialysis
Primary Author: Patrick McNeill, University of Arizona College of Pharmacy, Arizona;
Email: mcneill@pharmacy.arizona.edu
Additional Author(s):
Alex Jasensky
Marcella Hoyland
Brian Erstad
Purpose: A common medical emergency of hemodialysis (HD) patients involves fluid overload
and hypertension. Secondarily, hypotension often occurs during acute HD sessions due to the
relatively rapid removal of the excess fluid. The purpose of this study is to describe the
management pattern for end-stage renal disease (ESRD) patients admitted with fluid overload
receiving HD during an inpatient stay at an academic medical center. The main hypothesis is
additions and/or dose increases in anti-hypertensive medications will result in a larger interdialytic weight gain and a greater number of episodes of intra-dialytic hypotension, owing to
inadequate volume removal at baseline.
Methods: The Institutional Review Board has approved this retrospective chart review. The
electronic medical record system will identify patients that received HD between January 1, 2008
and January 1, 2013. The following data will be collected: the admission diagnosis and patient
comorbidities; time on dialysis prior to admission and time since last HD session; the number
and class of anti-hypertensive medications documented on admission, while inpatient, and upon
discharge; the use of midodrine, receipt of erythropoietin stimulating agents, total time on
dialysis while admitted, intra-dialytic hypotensive events, blood pressure readings pre- and postHD, and inter-dialytic weight gain; descriptive and demographic variables will be collected from
the electronic medical record systems. The investigators will use this information to compare the
number of anti-hypertensive medications upon admission versus discharge, determine the
fluctuation of systolic blood pressure (SBP) between each inpatient HD session, determine the
minimum SBP during each inpatient HD session and compare pre-HD weight to post-HD weight
to determine inter-dialytic weight gain and total volume removed per each HD session.
Descriptive statistics will be used to analyze our demographic data. Multiple linear regression
analyses will be completed to evaluate independent predictors of inter-dialytic weight gain and
intra-dialytic hypotension.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-073
Title: Electronic prescribing errors originating from a healthcare facility identified in a retail
pharmacy
Primary Author: Jaci Moench, University of Arizona College of Pharmacy, Arizona;
Email: moench@pharmacy.arizona.edu
Additional Author(s):
Danielle Manley
Herman Johannesmeyer
Jaime von Glahn
Purpose: The purpose of this study was to reduce the number of electronic prescription errors
sent from Marana Health Center (MHC) in Tucson, Arizona, to a nearby Fry's Pharmacy by
educating the prescribers at MHC on the most common discrepancies.
Methods: Data were collected by Fry's Pharmacy staff members. Fifteen health care
professionals were identified as Marana Health Center (MHC) prescribers. Whenever an
electronic prescribing error was made by an MHC prescriber, a Fry's Pharmacy staff member
indicated and recorded the type of error. The categories included product selected/dosage form,
AB rating, SIG codes, specific directions, quantity, days supply, and refills. Data collection
occurred during pharmacy hours for a 4-week period prior to an intervention. The intervention
consisted of a presentation by 3 pharmacy students to MHC prescribers at their monthly meeting
and focused on the 3 most common errors (product selected/dosage form, SIG code, and
quantity). Visual images of erroneous electronic prescriptions and explanations of how the errors
could be avoided in the future were included. Data collection occurred following the intervention
using the same methods as the previous round. Fishers Exact Test was used to determine if any
significant difference existed between the pre- and post-intervention data with respect to the
number and type of errors. The alpha a priori P-value was equal to 0.05. This was a quality
improvement project therefore it does not meet the Federal definition of research and
Institutional Review Board approval is not required.
Results: Fishers Exact Test demonstrated no significant difference between the number of
electronic prescription errors for each category relative to the total number of errors for pre- and
post-intervention data. There was no statistical significance in the category with the largest
numerical reduction (product selected/dosage form)(P equals 0.28). However, non-significant
reduction was noted in four of the seven categories of errors. These categories were product
selected/dosage form, SIG codes, quantity, and specific directions.
Conclusion: Prescriber education on the most common electronic prescribing errors may play a
role in the reduction of errors. While this study failed to show statistical significance, there is a
great need for improved accuracy and efficiency of electronic prescribing. Enhanced
communication between community pharmacies and healthcare facilities is encouraged. Data
collection can be carried out for a longer period of time, allowing pharmacists to compare error
rates over the course of time and stage further interventions as necessary. Collaborative practice
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
agreements between facilities can be discussed to allow for pharmacists to use their judgment for
resolution of certain errors.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-074
Title: Outcomes reporting at a medication therapy management center: a quality improvement
project
Primary Author: Amber Montoya, University of Arizona College of Pharmacy, AZ;
Email: montoya@pharmacy.arizona.edu
Additional Author(s):
Danielle F. Okerblom
Maria A. Tedesco
Angela N. Walsh
Aimee Keller
Purpose: The primary outcome was to determine accuracy of an outcomes report (OR)
generated at a medication therapy management center (MTMC) which was not formally
validated. Accuracy of the report was defined as correct documentation of the addition of a
medication recommended by a pharmacist.
Methods: This was a quality improvement project, therefore it did not meet the federal
definition of research and Institutional Review Board approval was not required. An OR of over
27,000 Add Angiotensin Converting Enzyme Inhibitor/Angiotensin Receptor Blocker (Add
ACE/ARB) alerts from electronic patient records (PR) were provided from 2012 by quality
assurance employees of the MTMC. A random sample of 500 alerts was selected from the total
of 27,000 alerts. Patient population consisted of Medicare Part D and other beneficiaries
considered high risk for medication-related problems that consented to medication therapy
management (MTM) services. An interventional success in the OR included an ACE or ARB
prescription being filled within 120 days following pharmacist recommendation. A non-success
was when these criteria were not met. Prescription fill history was compared to the OR for
accuracy, which determined whether interventions were successful (matched) or unsuccessful
(unmatched).
Results: From the random sample, 460 of 500 Add ACE/ARB alerts were verified using specific
patient identification numbers and compared to the PR. Patient records were irretrievable for 40
alerts. Overall, 460 of 460 OR interventions matched PRs, with Add ACE/ARB outcomes being
100% accurate.
Conclusion: Accuracy of the medication therapy management centers outcomes reports is
important because Centers for Medicare and Medicaid Services (CMS) assigns insurance
companies STAR ratings, based on Pharmacy Quality Alliance quality metrics. The Add
ACE/ARB alert is a heavily weighted component in determining Quality Bonus Payments.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-075
Title: Comparison of length of hospital stay and cost of intravenous and oral n-acetylcysteine in
acute acetaminophen toxicity
Primary Author: Jazmin Moreno, The University of Arizona College of Pharmacy, Arizona;
Email: jmoreno@pharmacy.arizona.edu
Additional Author(s):
Misael Porras
Purpose: The use of n-acetylcysteine in a clinical setting for acute acetaminophen toxicity may
not adhere with the use Food and Drug Administration approved dosing regimen. Changes in a
dosing regimen will affect length of hospital stay and cost of treatment of acute acetaminophen
toxicity with n-acetylcysteine. The objectives of this study are to determine the use of nacetylcysteine in a clinical setting and the cost of treatment of acute acetaminophen toxicity with
n-acetylcysteine using data collected from documented subject cases.
Methods: This study was exempt from review by the Institutional Review Board because the
study will involve existing records and the manner in which information will be recorded will
not allow for subjects to be identified. The electronic medical record will identify patients 18
years of age or older who experienced an acute acetaminophen overdose and received treatment
with oral or intravenous n-acetylcysteine in 2009, 2010, 2011, 2012, and January 2013 to June
2013. The medical records will be reviewed and the following data will be collected: age, sex,
type of treatment, number of doses administered, administration of an antiemetic, length of stay
in the intensive care unit, length of stay in the non-intensive care unit, and length of stay in the
emergency department. The following values will be determined from the data collected: mean
length of stay in the hospital for oral and intravenous n-acetylcysteine and total doses
administered of oral and intravenous n-acetylcysteine. The calculated means will be used along
with values from the primary literature and other sources to determine oral and intravenous nacetylcysteine cost of treatment for acute acetaminophen toxicity and length of hospital stay due
to acetaminophen toxicity.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-076
Title: Comprehension and attendance of prescription warning labels
Primary Author: Thu Nguyen, University of Arizona College of Pharmacy, Arizona;
Email: nguyent@email.arizona.edu
Additional Author(s):
Mina Baghzouz
Sarah Flocks
Marti Lindsey
Purpose: Prescription labels play an important role in patient education to inform patients about
their medications and disease states. While many American adults read at an 8th grade reading
level, warning labels can have higher reading levels, making it difficult for some patients to
understand them. The purpose of this study is to determine if people who take or manage
medications attend to the prescription warning labels and if education levels affect how they
interpret these warnings.
Methods: This study was exempt from review by the institutional review board since it was
classified as category type 2 research that involved survey procedures. A survey was designed to
assess whether or not the general population attends to warning labels and if education levels
affect how they interpret these warnings. The first part of the questionnaire is to find out if
participants attended to warning labels. The second part is a multiple choice quiz to assess
participants understanding of the warning labels. The last part is the participants demographic
information. Surveys will be collected at Joel Valdez Main Library in Tucson, AZ. Inclusion
criteria includes 18 years or older and literate in English. The exclusion criteria includes
participants who have impaired vision or hearing, those with a cognitive impairment, those who
are too ill to participate. Participants will give oral consent before participating. For data
analysis, the percentage of patients who attend to warning labels will be calculated. To compare
the two education groups (high school education/equivalent vs. lower education), mean and
standard deviation will be calculated for the numbers correct on the quiz portion of the survey. A
chi square analysis will be done on the dichotomous data.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-077
Title: Medication adherence education in U.S. schools and colleges of pharmacy
Primary Author: Danielle Nguyen, University of Arizona College of Pharmacy, Arizona;
Email: dnguyen@pharmacy.arizona.edu
Additional Author(s):
Jeannie K. Lee
Purpose: Medication adherence is the extent to which patients take their medications correctly
and consistently as prescribed. It is central to successful pharmacotherapy. If pharmacists can
interact with patients to empower them to adhere to their medications, clinical outcomes and
quality of life can be expected to improve. The purpose of this study is to survey Accreditation
Council for Pharmacy Education (ACPE)-preaccredited and accredited schools and colleges of
pharmacy for adherence course or content in their curricula.
Methods: The study has been submitted to the Institutional Review Board for approval and
informed consent will be obtained from all subjects. The ACPE website identifies all U.S.
preaccredited and accredited schools and colleges of pharmacy. Emails to invite participants to
the study will be sent to the Department of Pharmacy Practice Chair, or equivalent, at each
institution. Data will be collected via an online questionnaire including: establishment of an
elective or required course in medication adherence, number of credit hours of such course,
number of lecture hours in adherence education and course it is incorporated in if no stand-alone
course in place, interest to develop an adherence course, adherence textbook(s) used, clinical
activity of adherence instructor(s), medication adherence topics taught, educational year
adherence is taught, and demographic information about the college or school of pharmacy. All
data will be recorded without personal identifiers and remain confidential. The number of
institutions that require a course on medication adherence versus those offering elective course
or no such course offered will be calculated. The number of hours of adherence education will be
compared between older (in existence twenty years or more) and newer (less than twenty years)
colleges and schools of pharmacy.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-078
Title: Description of the management of alcohol withdrawal in hospitalized patients
Primary Author: Meira Nocella, University of Arizona College of Pharmacy, Arizona;
Email: nocella@pharmacy.arizona.edu
Additional Author(s):
Karen Parades
Regina Wu
Kara Snyder
Purpose: Studies indicate some alcohol withdrawal (AW) patients are diagnosed and treated
inappropriately in hospitals. Many adverse events correlate with the management of AW,
including withdrawal seizures, tremors, delirium, respiratory depression, among others. The
literature indicates wide differences in the management of AW, the incidences of adverse events,
and the role of pharmacotherapy in hospitalized patients. The objective of this pre-intervention
quality improvement (QI) project was to describe the AW management practices in hospitalized
patients diagnosed with AW. Additionally, it was to assess the quality of AW care, and to
identify possible areas in need of improvement.
Methods: This descriptive, retrospective, quality improvement report used hospital charts
(emergency department nursing documents and discharge summaries) of AW patients from a
regional academic medical center. Two queries were performed. The first was a query for all
Clinical Institute Withdrawal Assessment (CIWA) order occurrences between January 2010 and
December 2012. The second query was for the patient population that was at least 18 years of
age and coded with Diagnosis Related Group (DRG)-291.0 (AW) in the same time frame. The
patient population included those who were and those who were not managed using CIWA. A
systematic sampling procedure was used to obtain a sample (10 percent of the population)
wherein every tenth patient was selected and enrolled for further record review. Retrospective
data were collected using the patients health record, which included: CIWA scores,
benzodiazepine (BNZ) use, length of stay (LOS), complications associated with AW, and
readmissions. For each patient visit examined, a readmission was counted if it occurred within
seven days of the discharge date. This was a quality improvement project, therefore it did not
meet the federal definition of research and Institutional Review Board (IRB) approval was not
required according to University and hospital guidance.
Results: Only the patients with a DRG code of 291.0 were included in this project, enabling a
more focused examination of how well AW patients were handled at the medical center (n equals
35). Most patients in DRG 291.0 were managed using CIWA and all those managed with CIWA
had a standing order for lorazepam that included a guideline for lorazepam doses according to
CIWA score. The average time on CIWA was less than two days. Few complications were
found, with the exception of readmission (22.86 percent of the patients were readmitted). Under
the CIWA protocol, 25 out of the 34 patients were administered lorazepam. Seven of these
patients were administered diazepam. Sixteen of the 35 AW patients received non-BNZ sedating
drugs, sometimes in addition to the lorazepam and diazepam doses given according to CIWA
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
protocol. Also, administration of BNZs was not always associated with a documented CIWA
score.
Conclusion: This QI project provided an insight to how AW patients have been managed at a
regional academic medical center. Most of the patients were treated using symptom-triggered
therapy that incorporated CIWA scoring. The majority did not experience adverse outcomes such
as withdrawal tremors or long LOS. Readmission was the most prevalent of the complications
with a rate of about 23 percent. Future investigations should include a closer look at reasons for
AW patient readmissions and ways to prevent them.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-079
Title: Assessing adherence to the tetanus, diphtheria and pertussis vaccination guidelines at a
federally qualified health center before and after a clinical pharmacist intervention
Primary Author: Dawne O''Brien, University of Arizona College of Pharmacy, Arizona;
Email: obrien@pharmacy.arizona.edu
Additional Author(s):
Ashley Santa-Cruz
Amy Kennedy
Purpose: Tetanus, diphtheria, and pertussis are diseases which are preventable through proper
vaccination. Although these vaccines are widely available, there has recently been a surge in the
number of pertussis cases in the United States. The objective of this study is to determine
provider adherence to tetanus, diphtheria and pertussis guidelines set forth by the Advisory
Committee on Immunization Practices in a primary care setting before and after a clinical
pharmacist intervention.
Methods: This study has been submitted to the Institutional Review Board for approval. This
analytic study will use a before and after design. The before design will be a retrospective cohort
of chart reviews to determine provider adherence to tetanus, diphtheria and pertussis
immunization guidelines. A clinical pharmacist-based intervention in the form of a series of
cross-sectional chart reviews will then be initiated for approximately two weeks. The after design
will be another retrospective cohort of chart reviews following the intervention to determine if
vaccination rates with tetanus, diphtheria and pertussis improve. The longitudinal effectiveness
of the intervention will be determined by completing chart reviews one month and three months
following the intervention. Charts will be randomly selected and the data will be de-identified. It
is estimated that 300 charts will be analyzed during each period. The following data will be
collected: demographic information, provider type, and date of last tetanus-containing vaccine.
For each chart, the reviewers will determine if there was a missed vaccination opportunity. The
percentage of patients that received or did not receive the appropriately indicated vaccines will
be calculated during each review period and compared with the baseline data and/or postintervention data using a chi-square test.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-080
Title: Incidence of ICH post-tPA in acute ischemic stroke and validation of the HAT risk scale
for symptomatic ICH in a geriatric hospital cohort.
Primary Author: Sabrina Pennock, Banner Health, Arizona;
Email: Sabrinapennock@gmail.com
Additional Author(s):
Christi Jen
Mark Neufeld
Purpose: Because of the paucity of data on thrombolysis in patients aged greater than 80 years
old, the study aims to determine incidence of intracerebral hemorrhage amongst those 80 years
and older compared to those younger than 80 years old post-thrombolysis for acute ischemic
stroke (AIS). The secondary outcome is to validate the Hemorrhage After Thrombolysis (HAT)
risk scoring system to predict symptomatic intracerebral hemorrhage (sICH) between the two age
groups.
Methods: The inclusion criteria of this retrospective cohort study were patients 18 years old and
older who received intravenous tPA for acute ischemic stroke between 2008 to 2013. Patients
were excluded if CT was not performed prior to tPA treatment or if patient received antiplatelet
or anticoagulants prior to CT or MRI within 24 hours post-thrombolysis. Patients were
dichotomized into two groups: 80 years old and < 80 years old. The primary outcome is the
incidence of sICH as defined by the NINDS trial as hemorrhage not seen on previous CT scan
with either a suspicion of hemorrhage or any decline in neurologic status, while the secondary
outcome will validate the HAT scale in the cohort, which prognosticates the risk of symptomatic
ICH post-thrombolysis in AIS. The HAT scale assigns points to the top four risk factors
associated with the highest odds ratios: history of diabetes mellitus or baseline glucose 200
mg/dL, pretreatment NIHSS score, and presence of easily visible hypodensity on initial
noncontrast head CT scan. Student t and Fischers exact tests will be used for continuous and
categorical variables, while the c-statistic and 95% confidence intervals will be calculated to
predict risk of sICH.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-081
Title: Pharmacy technician behaviors and their impact on patient attendance rates: A quality
improvement project
Primary Author: Bryan Sears, The University of Arizona College of Pharmacy, Arizona;
Email: sears@pharmacy.arizona.edu
Additional Author(s):
Kayla Ward
Brittney Witmer
Lily Howden
Hussam Kutbi
Purpose: A medication therapy management program (MTMP) provides services to eligible
beneficiaries to optimize drug therapy, reduce adverse effects, reduce medication costs and
address patient questions. A comprehensive medication review (CMR) is one component of an
MTMP. The MTMP used in this project utilizes pharmacists to provide telephone based CMRs.
Pharmacy technicians are responsible for scheduling the CMRs that patients request by letter or
phone. The purpose of this quality improvement project was to improve adherence to scheduled
appointments by determining if technician behaviors affected patient attendance.
Methods: A total of 20 CMR scheduling calls were monitored randomly for a convenience
sample of 6 technicians over 5 weeks. During select times, four raters observed the technician
behaviors remotely using headsets connected to monitoring software. Technicians were rated on
6 objective measures (explained MTMP services, updated allergy information, updated
medication list, updated lab values, provided MTMP phone number, asked if patient had
questions) and 5 subjective measures (behaved confidently, pronounced medications correctly,
behaved professionally, spoke clearly, behaved distracted). Subjective behaviors were
normalized by consensus among raters before observations began. In addition, patients were
analyzed on 4 different measures (monitoring their own medications, taking medications for
cognitive impairment, patient called the MTMP, and sex). Raters either marked yes or no for
each behavior, and male/female for sex on a data collection tool. Patient attendance was
measured post hoc using a computer record database of CMRs. An intention to treat analysis was
performed using a chi squared test for each outcome with an a priori alpha level of 0.05. This
was a quality improvement project therefore it does not meet the Federal definition of research
and Institutional Review Board approval was not required.
Results: Twenty CMR scheduling calls were measured resulting in 14 attended CMRs and 6
unattended CMRs. No significant differences were found between objective technician behaviors
or subjective technician behaviors and CMR patient attendance (P was greater than 0.05 in all
areas of measurement). In addition, no significant differences were found between patient
information and CMR patient attendance (P was greater than 0.05 in all areas of measurement).
Conclusion: The measured technician behaviors, as well as patient information, have no impact
on patients CMR attendance. One major limitation to this study was the small sample size. It was
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
determined that future research would be needed to assess the significance of technician
behaviors on patient attendance of CMR appointments.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-082
Title: Impact of implementing a step wise approach to confirm the diagnosis and appropriate use
of treatment for malaria
Primary Author: Clarissa Sema, The University of Arizona, Arizona;
Email: sema@pharmacy.arizona.edu
Additional Author(s):
Simon Appiagyeih
Patrick Yamoah
Michael Katz
Purpose: Malaria is a life threatening disease that is endemic throughout most of the tropics.
Prompt and accurate diagnosis of malaria is critical for implementation of appropriate treatment
to reduce associated morbidity and mortality. The objectives of this study are to evaluate the
effectiveness of rapid diagnostic tests (RDTs) to confirm malaria, increase use of RDTs to
testing to confirm malaria diagnosis, increase number of confirmed malaria cases versus
presumptive cases, decrease over diagnosis and over use of malaria medications, and identify
prevalence of malaria species in Central Region, Ghana.
Methods: This study will be submitted to the Institutional Review Board for approval. Baseline
data to be collected includes: patient age, gender, diagnosis, Giemsa stained blood film result
with parasite density, diagnosis, and treatment. The following outcome data will be collected:
patient age, gender, RDT result, Giemsa stained blood film result with parasite density, malaria
species identified, diagnosis, and treatment. All data will be recorded without patient identifiers
and maintained confidentially. Patients with a chief complaint and positive signs and symptoms
for malaria will be identified in Triage and referred to the Laboratory for a RDT. Positive tests
will be confirmed using microscopy and classified based on the number of malaria parasites
observed and malaria species. Physicians will diagnose and treat confirmed malaria based on
severity of signs and symptoms and lab results. Negative tests will be referred to the physicians
to consider other possible diagnosis, unless physicians have a strong suspicion of malaria.
Descriptive analysis will be used to analyze the data to determine the impact of implementing a
step wise approach to confirm malaria cases in Central Region, Ghana.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-083
Title: Assessment of late refill requests for bulk liquid medications at the El Paso State
Supported Living Center
Primary Author: Aubrey Silvester, University of Arizona College of Pharmacy, AZ;
Email: aubreys@email.arizona.edu
Additional Author(s):
Kalyn Schmidt
Dharti Bhakta
Amista Salcido
Purpose: The El Paso State Supported Living Center is a state-funded, long term care facility
that provides comprehensive behavior treatment and healthcare services to residents with
developmental disabilities. Pharmacy department personnel prepare weekly supplies of unit dose
medications. Bulk liquid medications are sent from the pharmacy and administered by nursing
staff from original containers; this practice created medication administration errors. The purpose
of this quality improvement (QI) project was to identify and decrease inappropriate late refill
requests of bulk liquid medications. Focus was placed on medications ordered the most days late
and that had the largest number of late requests.
Methods: This was a QI project therefore it did not meet the Federal definition of research and
Institutional Review Board approval was not required as per University guidance. The number of
late refill requests from September 1, 2012 to March 31, 2013 were identified by compiling data
from handwritten medication request forms, current patient census, hospitalizations, and
approved absences into an Excel spreadsheet. Pre-intervention data were analyzed for late refill
requests by patient, unit, medication, and average number of days late. After late refill requests
were identified, in-service training was provided to the nursing staff. In-service training included
education on adverse events and other morbidities caused by providing medications late or by
withholding medications as well as the importance of checking medications against the
medication administration record (MAR). Lastly, pharmacy personnel inspected all medication
rooms to ensure all active medications were stored correctly and to return discontinued
medications to the pharmacy. Post-intervention data were then complied using an Excel
spreadsheet. Chi-squared and Students t-test were used for data analysis. Statistical significance
was set at a 5 percent significance level or with a Bonferroni adjustment.
Results: Lactulose, atropine, ergocalciferol, fluticasone nasal spray, budesonide and megestrol
resulted in 80% of the total late requests. Calcitonin, ergocalciferol, fluticasone HFA inhaler,
levetiracetam and fluticasone nasal spray were identified as being requested the most days late
with an average of 83 days late. Total number of late refill requests significantly decreased from
195 in the pre-intervention period (153 days) to 39 in the post-intervention period (55 days) (P
equals 0.012). The number of late requests for lactulose significantly decreased from an average
of 17.6 requests per 30 days in the pre-intervention period to an average of only 2 requests per 30
days in the post-intervention period (P equals 0.001). Only fluticasone nasal spray had a
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
significant decrease in number of days late from an average of 27.1 days to 12.6 days (P equals
0.034).
Conclusion: For this QI project, in-service training significantly decreased total number of late
refill requests. Lactulose, the medication with the highest number of late refill requests, had the
most significant reduction in late requests. Additional data are necessary to determine the
duration of the training effectiveness, how often to retrain the staff, and whether changes to the
training curriculum are necessary. Furthermore, investigation into other interventions to decrease
inappropriate late refill requests could be beneficial to this facility.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-084
Title: Determination of adherence to metformin discontinuation guidelines in type 2 diabetes
mellitus patients in a community health center
Primary Author: Beena Vemulapalli, University of Arizona, Arizona;
Email: vemulapalli@pharmacy.arizona.edu
Additional Author(s):
Yin Lai
Amy Kennedy
Purpose: Metformin is considered first-line therapy in patients with Type 2 Diabetes Mellitus.
Advantages of metformin include a lower risk of hypoglycemia, absence of weight gain, and
neutral to positive effects on lipids and blood pressure. Metformin use is contraindicated when
estimated glomerular filtration rate (eGFR) falls below 30 ml/min/1.73 meters squared. Early
discontinuation in patients with mild to moderate renal insufficiency can impact a patients ability
to achieve optimal blood glucose targets, which may require adding additional agents that have
their own adverse events. The objective is to determine adherence to metformin therapy
prescribing guidelines in a community health center.
Methods: The study was submitted and approved by the Institutional Review Board. The
electronic medical record at a federally qualified health center will identify adult patients
diagnosed with Type 2 Diabetes Mellitus with a history of metformin therapy and renal function
data available and readily accessible. The following data will be collected: metformin history,
reasons for discontinuation of therapy, presence of contraindications, age, gender, weight, height,
race, ethnicity, body surface area, creatinine clearance, and estimated glomerular filtration rate
(eGFR). The frequency of adherence to metformin prescribing guidelines will be determined. All
data will be recorded without patient identifiers and will be confidentially maintained. The
frequencies and percentages for each group will be compared using a Chi Square test. The
possible reasons why metformin was discontinued will be assessed. Prescribing practices for
these patients will be compared to metformin therapy prescribing guidelines and categorized as
adherent or nonadherent.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-087
Title: Impact of automated dispensing technology on medication safety and costs at an inpatient
pharmacy
Primary Author: Eric Wong, The University of Arizona, Arizona;
Email: ewong@pharmacy.arizona.edu
Additional Author(s):
Daniel P. Burgos
Kurt J. Weibel
Purpose: Automated dispensing technology use has increased over recent years in an effort to
increase efficiency, decrease costs, and improve patient care. In addition, the American Society
of Health System Pharmacists Pharmacy Practice Model Initiative encourages the use of
automation and technology throughout the medication use process. The purpose of this project is
to compare two groups of automated dispensing technologies, a pharmacy automatic
replenishment system and an automatic print unit dose system versus an automated medication
storage and retrieval system and a high speed automatic tablet packager, and their impact on
medication safety and costs at an inpatient pharmacy.
Methods: This is a quality improvement project and is not considered human subjects research,
thus it is exempt from the Institutional Review Board. The primary outcome will be the
automated dispensing cabinet refill error rate between the pharmacy automatic replenishment
system and automated medication storage and retrieval system. Data will be collected by
obtaining refill reports for automated dispensing cabinets throughout the hospital. Every other
medication on the refill report will be audited for errors in the corresponding location of the
automated dispensing cabinet. Error categories include wrong drug and strength, wrong drug and
right strength, right drug and wrong strength, right drug and wrong dosage form, filling error or
wrong pocket, expired medication, and miscellaneous error. The rate of reported errors will also
be incorporated into the analysis using data obtained from a self reported error program. The
secondary outcome will be to evaluate costs incurred while using the automated technologies.
This analysis will include automated dispensing cabinet inventory, drug expense per pharmacy
intensity score adjusted discharge, drug costs per patient day, and costs associated with bulk
repackaging. All data associated with costs will be obtained from pharmacy financial records.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-088
Title: Simultaneous determination of the nucleoside analogues clofarabine and fludarabine by
liquid chromatography-tandem mass spectrometry in low volume clinical samples: application to
a pharmacokinetic study in children
Primary Author: Ryan Beechinor, University of California at San Francisco, California;
Email: Ryan.Beechinor@ucsf.edu
Additional Author(s):
Janel Long-Boyle
Purpose: Fludarabine and Clofarabine are nucleoside analogs increasingly utilized in
conditioning regimens for patients undergoing allogeneic hematopoietic cell transplantation
(alloHCT). Currently, the combination of low dose clofarabine added to standard fludarabine and
busulfan is being evaluated for safety and efficacy in a phase II dose-escalation clinical trial.
Characterization of clofarabine and fludarabine pharmacokinetics (PK) will significantly
advance our understanding of the optimum systemic concentrations required to elicit drug
synergism with concomitant administration. This study aims to characterize the PK of both
clofarabine and fludarabine in pediatric patients receiving combination nucleoside analog
therapy prior to alloHCT.
Methods: We have prospectively collected PK data from pediatric patients undergoing alloHCT
at UCSF Benioff Childrens Hospital between June 2012 and March 2013. Patients were eligible
to be included in the analysis if they had undergone a related or unrelated HCT including
combination nucleoside analog therapy with fludarabine and clofarabine, were between 0 to 18
years of age, and had nucleoside analog time-concentration data available for analysis. Drug
levels and potential covariates influencing drug exposure will be analyzed with standard
population PK methodologies using non-linear mixed effects modeling software (NONMEM).
Retrospective PK data available in children receiving monotherapy of fludarabine or clofarabine
will be used in the model-building process.
Results: This study will utilize nucleoside analog time-concentration data available in 11
pediatric HCT recipients (7 males/4 females). Subjects range in age from 3 months to 12 years.
Median weight is 13.2 kg (range, 7.3-50) and includes 4 subjects with an actual body weight less
than 12kg. A total of 134 quantifiable concentrations are available for PK modeling. The range
of observed fludarabine and clofarabine concentrations are 0.313-300.0 and 0.462-137 ng/mL,
respectively.
Conclusion: Data collection is complete. PK analysis is underway and will be completed with
results available at the time of the ASHP Midyear Meeting.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-089
Title: Impact of brief insulin focused teaching within a diabetes education class on perceived
barriers to insulin therapy in type 2 diabetes and prediabetes patients
Primary Author: Jon Benner, Skaggs School of Pharmacy and Pharmaceutical Sciences,
California;
Email: jbenner@ucsd.edu
Additional Author(s):
Stephanie Chauv
Jan Hirsch
Panteha Kelly
Renu Singh
Purpose: Patients with diabetes managed by insulin therapy need to be adherent to their
regimen, comfortable with self administration, and understand proper insulin administration and
glycemic management. However, the fear of injecting insulin remains a barrier to some patients
with diabetes. The purpose of this study was to evaluate diabetes and prediabetes patients
perceptions of insulin use prior to receiving insulin education and compare changes to
perceptions after completion of two education sessions that include a brief insulin focused
discussion.
Methods: The institutional review board approved this prospective cohort study. Eligible
subjects were age 18 or older with type 2 diabetes, or prediabetes who attended a diabetes self
management programs two core group education classes and consented to participate in the
study. The first class was a two hour session addressing various diabetes self management topics.
In addition, the diabetes educators briefly covered insulin devices, formulations, and injection
technique. Patients returned for a second class where they received additional topics. The Insulin
Treatment Appraisal Scale (ITAS) is a validated 20 item survey, using a Likert scale, with
questions related to perceptions of insulin use. The ITAS survey was distributed to subjects as a
pre survey prior to the first education class and as a post survey at the end of the second
education class. The primary outcome measure was a change in ITAS score from the pre and
post survey to reflect a change in patient perception to each question. 29 patients were enrolled
in the study, with 17 patients completing both a pre and post survey. Descriptive statistics were
calculated for all variables. Paired t-tests were used to examine the differences in the pre versus
post survey scores.
Results: Of the patients who completed both a pre and post survey, patient demographics
included 83 percent with type 2 diabetes, 33 percent using insulin at the time of the study, and 52
percent being men. Improvement in perception to insulin therapy was seen in six individual
negative perception questions, the Mean Total Negative Appraisal (pre survey 49.1, post survey
43.5, P-value 0.04) and the Total ITAS score (pre survey 55.6, post survey 48.9, P-value 0.01).
These findings indicate that patients negative perceptions of insulin use significantly improved
after attending the two education classes. Improvement in attitudes was observed toward disease
prognosis, complexity of disease management, and social stigma associated with insulin use.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
There was no significant difference in the positive appraisal of insulin among the pre and post
surveys indicating that patients were aware of the potential benefits of insulin therapy before
entering the core education classes with no change in perception. The majority of subjects agreed
or strongly agreed with the idea that insulin improved prognosis, improved health, and
maintained good control of blood glucose.
Conclusion: A brief insulin focused teaching discussion within a diabetes education class
improved patients negative perceptions of insulin therapy. This study reinforces that diabetes self
management programs should ensure that discussion of insulin use is included in its core classes,
even if the participants are not currently taking insulin. Further studies will be required to better
determine how patients perceive the different aspects of insulin therapy, and what the best
strategy will be in tailoring their education toward a more positive outlook of insulin therapy.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-090
Title: Metformin Decreases Pancreatic Cancer Risk Associated with Dipeptidyl Peptidase IV
Inhibitors: Assessing FDA Adverse Event Reporting System Database
Primary Author: Wendy Chaing, California Northstate University, College of Pharmacy,
California;
Email: wchaing3338@cnsu.edu
Additional Author(s):
Xiaodong Feng
Purpose: Increasing evidence indicates that many antidiabetic drugs increase the risk of cancers
in diabetic patients. Recently, the FDA issued warnings that pioglitazone increases the risk of
bladder cancer for Type 2 Diabetes Mellitus (T2DM) patients. Our group reported that dipeptidyl
peptidase IV (DPP IV) inhibitors, such as sitagliptin, and saxagliptin, increase the risk of
pancreatic cancer in T2DM patients. In addition, T2DM triggers multiple factors, such as
hyperinsulinemia and insulin receptor over expression, which may increase the risk of cancer in
diabetic patients. Furthermore, metformin activates 5 adenosine monophosphate-activated
protein kinase (AMPK). New evidence indicates that the activation of AMPK by metformin
inhibits various cancer cell growth. The FDA Adverse Event Reporting System (FAERS)
provides an excellent platform for post marketing drug safety surveillance to assess the risks of
adverse events associated with drug therapy. The objective of this research is to use FAERS
database to assess the cancer risks associated with antidiabetic drugs, such as pioglitazone and
DPP IV inhibitors with or without metformin. The hypothesis is that the combination with
metformin will decrease the cancer risks associated with pioglitazone and DPP IV inhibitors.
Methods: Using the FAERS public database, the cancer related adverse event reports (AERS)
associated with widely used antidiabetic drugs such as sitagliptin and pioglitazone will be
generated and evaluated. The database has also shown a decrease risk of cancer among the use of
metformin. Standardized pharmacovigilance tools will be applied to detect the signal of cancer
risk from sitagliptin and pioglitazone and metformins ability to decrease cancer prevalence
among those classes of drugs.
Results: Among 12,618 AERS associated with sitagliptin from 2007 to 2011, there were 223
cases of cancer. There was a significant correlation between the cancer reporting ratio and the
time from 2007 to 2011 (R = 0.796, P<0.001). Pancreatic cancers accounted for 22% of all
combined cancer adverse events reported. Pharmacovigilance assessment from 2007 to 2012
indicated that there was a significant risk of pancreatic cancer associated with DPP IV inhibitors
treatment (ROR=5.922). Interestingly, there was a correlation between the AERS of minimal
pancreatic cancer risks and the use of metformin (ROR=1.214). Combination of DPP IV
inhibitor such as sitagliptin with metformin correlates with significantly lower risk of pancreatic
cancer compared to sitagliptin treatment without metformin (OR=0.277, 95%CI: 0.210-0.365).
Conclusion: There was a significant signal of pancreatic cancer risks associated with DPP IV
inhibitor treatment. For the first time, we demonstrated that the combination with metformin may
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
significantly reduce the risk signal of pancreatic cancer associated with DPP IV inhibitors based
on the FAERS evaluated. Considering the limitations of the FAERS such as potential biased
reporting, under reporting, and over reporting, this study implied the potential strategy for cancer
control and prevention in T2DM patients, and providing directions for future clinical studies.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-091
Title: Correlation among stroke occurrence, dementia, and atypical antipsychotic
Primary Author: Kevin Chen, University of California, San Francisco, California;
Email: kevin.chen@ucsf.edu
Additional Author(s):
Bridget LeBlanc
Christin Pansawira
Lawrence Troxell
Purpose: A recent Taiwanese study found a two-fold increased risk of stroke among newlydiagnosed dementia patients on atypical antipsychotic. This is consistent with the addition of the
boxed warning on atypical antipsychotics in 2005, indicating an increase in mortality when used
by patients with dementia. Because these findings revealed an increased risk in, but not the cause
of mortality, the objective of this study is to look at stroke as an outcome of atypical
antipsychotic use. This is a retrospective correlation study, seeking to quantify the prevalence of
stroke in dementia patients who are taking atypical antipsychotic.
Methods: This study is awaiting final approval from the Northern California Institutional
Review Board, after a local facility approval had been granted recently. Electronic Medical
Record for 2400 patients with an ICD-9 code of dementia will be reviewed to determine the rate
of stroke occurrence among patients who have used atypical antipsychotic medications. This
review will look at prescription records from 1990-2013 for atypical antipsychotic prescription
fills as well as the diagnosis codes indicating a stroke or transient ischemic attack. All data was
de-identified and kept confidential for purposes of this analysis. Included patients are men and
women age 50 or greater. This review will also examine co-morbidities in the patient population,
including diabetes, hypertension, and hyperlipidemia for potential contributory factors of stroke
occurrence. Patients with mental health conditions such as schizophrenia and bipolar disorder
were included in this study if they also had a diagnosis of dementia. Upon completion of the
records review, analysis was completed to determine the rate of stroke occurrence in dementia
patients who had received atypical antipsychotic medication therapy as well as those who had
not received such therapy.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-092
Title: The impact of age on the pharmacokinetics of artemether-lumefantrine for treatment of
uncomplicated malaria in Tororo, Uganda
Primary Author: Xixi Cheng, University of California, San Francisco School of Pharmacy,
UCSF, California;
Email: xixi.cheng@ucsf.edu
Additional Author(s):
Norah Mwebaza
Richard Kajubi
Sunil Parikh
Francesca Aweeka
Purpose: Malaria infections, mainly those caused by Plasmodium falciparum, remains high in
sub-Saharan Africa despite preventive programs. It is the leading cause of mortality in Uganda,
particularly in vulnerable populations such as children. Children exhibit increased drug clearance
that may lower antimalarial drug exposure, leading to treatment failure, increased risk for reinfection and drug resistance. Current treatment guidelines have not considered the impact of
developmental changes on drug clearance. This study will address the impact of age on the PK
exposure of artemether-lumefantrine to optimize dosing guidelines and ultimately decrease
mortality rates and risks of re-infection in children with malaria infections.
Methods: A prospective pharmacokinetic study will enroll 48 HIV-negative children between 6
months and 8 years of age and 30 HIV-negative non-pregnant adults aged 16 years or older from
Tororo District Hospital. Eligible participants will receive standard treatment for uncomplicated
malaria which includes 6 weight-based doses of artemether-lumefantrine (AL) administered over
4 days. Intensive PK samples will be collected after the 6th treatment dose and sampling for
artemether, its active metabolite dihydroartemisinin and long-acting partner drug lumefantrine
will be done with 500uL venous plasma samples. Follow-up studies for treatment outcomes will
continue until study day 42. Quantification of drugs will be performed by LC/MS/MS and PK
parameters will be estimated using non-compartmental analysis via the linear up-log down
trapezoidal rule using WinNonlin 5.2.1. Clearance, volume of distribution, and rate of absorption
will also be used to construct a PK model to represent the effects of age on AL exposure. For
these comparisons, 90% power will be used to detect a difference in AUC of 35% or more, given
an overall Type I error of 0.05. All reported PK parameters will be compared between groups
using the Wilcoxon Rank-Sum Test calculated with Stata/SE 12.1.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-093
Title: Characterization of erythropoietin stimulating agents in critically ill patients with renal
dysfunction
Primary Author: Diana Cowell, UCSF School of Pharmacy, California;
Email: diana.cowell@ucsf.edu
Additional Author(s):
Chad Rockwell
Korana Avdagic
Ashley Thompson
Cindy Burg
Purpose: Critically ill patients are often anemic and have a high incidence of renal dysfunction.
Erythropoietin stimulating agents (ESAs) such as epoetin alfa and darbepoetin alfa are often
prescribed in this patient population; however their use is not well characterized. ESAs are highcost, high-risk drugs that are associated with thrombotic risks including stroke, myocardial
infarction, and death. The purpose of this study is to describe the use of ESAs in patients with
renal dysfunction and associated adverse events in the adult intensive care unit (ICU).
Methods: The institution review board approved this retrospective review evaluating patients
receiving ESAs in the adult ICUs between July 1, 2012, and June 30, 2013, at a university
hospital. We included patients 18 years of age and older admitted into the adult medical,
surgical, or cardiac intensive care units for a minimum of 24 hours and who received at least one
dose of epoetin alfa or darbepoetin alfa. Patients receiving ESAs with cancer-associated anemia
or those who received ESA therapy prior to the intensive care unit admission were excluded
from the study. The following data will be included: date, time, type of and dose of ESA, patient
demographics, length of hospital stay, chronic kidney disease/acute kidney injury classification,
need for renal replacement therapy, number of blood transfusions, reason for intensive care unit
admission and diagnoses, pre- and post-ESA administration hemoglobin and iron studies, as well
as thromboembolic events and 28-day mortality.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-094
Title: Lack of life-threatening arrhythmias despite QTc prolongation with concurrent use of
ranolazine and dofetilide: a case study
Primary Author: Daniel Da Costa, University of the Pacific, California;
Email: d_dacosta@u.pacific.edu
Additional Author(s):
Gregory Koyama
Leo Yuan
Sachin Shah
Pei-Chun McGregor
Case Report: Prolongation of the QTc interval above 500 msec, or greater than 30 msecs from
baseline, has been shown to increase the risk of life-threatening arrhythmias such as torsade de
pointes (TdP). The class-III antiarrhythmic medication dofetilide has been found to significantly
prolong the QTc interval and increase the risk of TdP precipitation in a dose-dependent manner
due to blockade of the rapid delayed rectifier potassium current (Ikr). According to the package
insert, dofetilide 250 mcg BID prolongs the QTc by approximately 13 msec. The antianginal
agent ranolazine has shown to modestly prolong the QTc interval by 2-6 msec and is
consequently contraindicated in combination with class-III antiarrhythmic agents. Despite these
effects, preclinical and limited clinical evidence suggests that ranolazine is not associated with a
significant increase in the precipitation of TdP. This may be due to ranolazines proposed
mechanism of actioninhibition of the inward late phase sodium current (INa) during cardiac
repolarization and subsequent reduction in intracellular sodium and calcium overload. While
this mechanism prolongs the QTc interval, another proarrhythmic substratetransmural dispersion
of repolarization (TDR)was reduced in an experimental model involving canine ventricular
wedge preparations. In this model, treatment with ranolazine did not induce TdP, suggesting that
ranolazine may actually suppress proarrhythmic activity and indicating that TDR may actually be
a better predictor for precipitation of TdP compared to QTc. We report a case of a 67-year-old
male maintained over the past 18 months on concomitant dofetilide and ranolazine therapy for
paroxysmal atrial fibrillation (AF) and ischemic cardiomyopathy, respectively.
In 2006, upon diagnosis of paroxysmal AF, the patient received an implantable cardioverterdefibrillator (ICD). Past medical history includes ischemic cardiomyopathy, congestive heart
failure, coronary artery disease requiring multiple bypass grafts, diabetes mellitus, hypertension
and multiple transient ischemic attacks. Current relevant medications include ranolazine 1000
mg twice daily, dofetlide 250 mcg twice daily, digoxin 125 mcg daily, aspirin 81 mg daily,
carvedilol 12.5 mg daily, warfarin 5 mg daily, rosuvastatin 40 mg daily, niacin 1000 mg ER
twice daily, fosinopril sodium 10 mg daily, furosemide 40 mg daily, and glucagon and regular
insulin as needed.
Eight months prior to the initiation of dofetilide, the patient was started on amiodarone 200 mg
twice daily in response to multiple hospitalizations for congestive heart failure with onset of AF.
Due to an episode of amiodarone-associated thyrotoxicosis, the medication was discontinued.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
The patient was subsequently initiated on dofetilide while continuing ranolazine therapy. QT
interval and TDR were manually measured using standard practices by two independent
investigators. ECG data analyzed included both pre- and post-dofetilide therapy initiation, in
addition to 2- and 14-month follow-up.
Overall a significant increase in both automatic and manually measured averages of QT interval
following the initiation of dofetilide was observed. In contrast, the patients average TDR was
maintained over the same time period. The patients QTc interval was measured at 437, 473, 464
and 468 msec prior to dofetilide initiation, during initial administration, and two and four months
post-initiation, respectively. The measured TDR was 60, 62, 66 and 56 msec at the same
respective points in time. Finally, analysis of the patients medical records following initiation of
dofetilide with concomitant ranolazine therapy did not reveal any significant arrhythmic events.
This case of concurrent ranolazine and dofetilide therapy supports the implication that ranolazine
may be a safe addition to dofetilide due to its ability to attenuate TDR despite QTc prolongation.
Future studies are warranted for the addition of ranolazine with other potent IKr blocking agents
and further exploration of TDR as a predictive tool for life-threatening arrhythmias such as TdP.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-095
Title: A COMPARATIVE ASSESSMENT OF FENTANYL PATCH PRESCRIBING
PRACTICE IN A COMMUNITY Hospital
Primary Author: Bin Deng, California Northstate Unveristy College of Pharmacy, Santa
Barbara Cottage Hospital, California;
Email: bdeng8654@cnsu.edu
Additional Author(s):
Purpose: Fentanyl transdermal patch is a potent opioid narcotic indicated for chronic pain
control. Therapy should only initiate when a patient demonstrates opioid tolerance, which is
equivalent to 60mg of oral morphine for a minimum of 7 days. The objective of this study is to
evaluate effectiveness of pharmacists driven fentanyl patch order set by assessing physician
compliance with fentanyl prescribing guideline published by California Department of Public
Health (CDPH) in a community hospital setting.
Methods: A comparative retrospective chart review of 266 patients was conducted between
March 2011 and May 2012 at Santa Barbara Cottage Hospital. Of these patients, 113 patients
from 2012 were on pharmacists directed fentanyl patch order set. All patients who were on
fentanyl patch prior to or after admission were included. The criteria used to evaluate fentanyl
patch prescribing compliance were: (1) patient on fentanyl patch when ordered/admitted (2)
patient on opiates prior to admission or during hospitalization for 7 days with a minimum daily
dose of 60 mg oral morphine equivalents, (3) fentanyl patch use to manage chronic pain. Primary
end point was compliance in individual patch strength after fentanyl order set implementation.
Secondary end point was adverse outcome, measured by naloxone usage. Mcnamars test was
used for statistical analysis.
Results: Implementation of pharmacist driven fentanyl patch order set in 2012 resulted in a 27%
increase in compliance with fentanyl patch prescribing criteria (83% in 2012 vs. 54% in 2011, P
< 0.0001, OR 5.048, 95% CI 3.139-8.491). All patches were correctly prescribed for chronic
pain management. The primary point end was significant in variation of compliance between
different strength of fentanyl patch. In particular, 12mcg and 25mcg have lowest compliance rate
(59%) compared to higher patch strength (50mcg, 75mcg, 100 mcg), which have a compliance
rate between 74% and 100%. The variation in compliance rate between lower strength and
higher strength was most likely due to physicians clinical judgment to start patients on fentanyl
patch due to therapy failure on multiple opioid analgesics, even though patients do not meet
guideline criteria. All individual patch strength increased compliance from 2011, range from
19% to 31%.The secondary end point was insignificant between both groups, as naloxone was
only administered to 2 patients in 2011 and 1 patient in 2012. No death resulted in all patients.
Conclusion: Implementation of pharmacists driven fentanyl patch order set greatly increased
physician compliance with fentanyl patch prescribing guideline. Pharmacist should continue to
educate physicians and provide alternative treatment options for patients who do not meet the
criteria of fentanyl patch prescribing guideline.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-096
Title: Evaluation of the multiple mini-interview across stakeholders in a pharmacy schools
admissions process
Primary Author: Gary Fong, University of California, San Francisco, California;
Email: Gary.Fong@ucsf.edu
Additional Author(s):
Ryan Beechinor
Michael Creason
Karen Hudmon
Robin Corelli
Purpose: In 2013, a four-station Multiple Mini-Interview (MMI) was implemented to replace a
standard student and faculty member team interview for admission to the PharmD program. This
change occurred with a goal of enhancing the admissions committees ability to standardize and
improve the quality of information obtained during on-site interviews for PharmD candidates.
The purpose of this study was to (1) evaluate the perceptions of the MMI process across three
major stakeholders (candidates, interviewers, and admissions committee members) and (2)
estimate the comparative human and facility resource costs required for the MMI and standard
interview formats.
Methods: Using an email recruitment approach, candidates (n=285), interviewers (faculty, n=15;
students, n=44; standardized professionals, n=8), and admissions committee members (n=39)
received a hyperlink to an anonymous web-based survey. Each survey contained approximately
7-10 items assessing perceptions of the process (response options: strongly agree, agree, neither
agree nor disagree, disagree, strongly disagree) and demographic data to characterize the
populations. Candidates were surveyed approximately 1 week after their on-site interview, but
prior to receiving notification of their final admission status. Interviewers and admissions
committee members were surveyed approximately 4 weeks after completion of the candidate
interviews and the final admissions committee meeting, respectively. Costs of resource
requirements were estimated using actual training and staffing schedules from the 2012 cycle
(standard format) and the 2013 cycle (MMI format).
Results: Survey response rates were: candidates (85%), interviewers (83%), and admissions
committee members (87%). Three percent of applicants had participated in an MMI interview in
past 6 months, and 34% agreed that the compared to a standard interview, the MMI is less
stressful. Among interviewers, 69% believed that they were able to formulate an accurate
assessment of the candidates abilities using the MMI format, and among admissions committee
members, 48% perceived that the information obtained when using the MMI approach was more
useful than the information obtained when using the standard interview evaluation form (in prior
years). The proportion of candidates, interviewers, and admissions committee members that
perceived the MMI format as an effective method for evaluating applicants nonacademic
qualities for the profession was 65%, 86%, and 79%, respectively, and most agreed that the
school of pharmacy should continue to use the MMI format instead of the standard interview
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
(candidates, 59%; interviewers, 84%; admissions committee members, 77%). A comparative cost
analysis estimated a 45% cost reduction per applicant interviewed when MMI ($75.30 per
applicant) is used compared to the standard interview approach ($136.34 per applicant).
Conclusion: The overall perception of the MMI process was favorable across all stakeholders.
Furthermore, the MMI process is less costly, per applicant interviewed, to implement. These
results support the continued use of the MMI format as part of the admissions process for
PharmD candidates.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-097
Title: Effects of erotic visual stimulus on analgesia: a meta-analysis
Primary Author: Alexander Fung, University of the Pacific, California;
Email: a_fung2@u.pacific.edu
Additional Author(s):
Timothy Tang
Jesse Chea
Robert Gapuz
Sachin A. Shah
Purpose: Sexual arousal stimulates the release of dopamine in the human body, which has an
analgesic effect through descending inhibition of pain. Pain is a prevalent problem that is often
inadequately managed and the need for novel pharmacologic and non-pharmacologic
interventions exists. Several studies have been conducted assessing the impact of erotic visual
stimulus and its effect on lowering pain levels. Current evidence suggests conflicting results
indicating the need for more data. The primary objective was to conduct a meta-analysis
assessing the impact of visual erotic stimuli and corresponding pain levels.
Methods: PubMed, CINAHL, and the Cochrane database were searched using the following key
terms: erotic, pain, emotion, modulation along with hand searching of relevant references. Search
results were limited to humans, clinical trials, and English language. The primary endpoint was
pain levels before and after exposure to visual erotic stimulus. The following data were extracted
from all clinical trials: author, year of publication, study design, duration of study, intervention
type, patient population, and pain levels. A weighted mean difference from baseline using the
DerSimonian-Laird random effects model was calculated with a corresponding 95% confidence
interval. Subgroup analyses were performed to assess for clinical heterogeneity. Statistical
heterogeneity was assessed using the Cochrans Q statistic while publication bias was assessed
using funnel plots. In cases of data reported only in figure form, the data was extracted manually
under magnification. JADAD scores were utilized to assess the quality of publications.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-098
Title: Assessing student ability to apply evidence-based medicine to clinical practice decisions
Primary Author: Vanessa Guzman, University of California, San Francisco, California;
Email: vanessa.guzman@ucsf.edu
Additional Author(s):
Nicola Clayton
Purpose: The objective of this study is to assess the ability of pharmacy students to apply
evidence-based medicine (EBM) to clinical decisions. Our hypothesis is that although students
learn how to assess literature during their second year didactic curriculum, these skills regress
during the third year due to underutilization. This study will assess student ability to find,
interpret and communicate evidence-based medicine at various points in the curriculum. It will
also propose mechanisms for integrating EBM practices consistently into therapeutics.
Methods: This study will be submitted to the Institutional Review Board for approval. Data will
be collected from first and third year pharmacy students via the national Pharmacy Curriculum
Outcomes Assessment. We will compare mean correct scores for all first year pharmacy students
when compared to mean national percent correct in the following categories: Biostatistics and
Research Design, Literature Evaluation and Practice Guidelines and Clinical Trials and Drug
Information. The data from first year students will provide an understanding of the baseline
knowledge of the school of pharmacy population and the data from third year students will be
used to assess growth in their evidence-based medicine skills. Data will be collected from first
through fourth year students in a self-reported survey asking them to self-assess their ability,
efficiency and confidence finding evidence based information, integrating that evidence into
clinical decisions and communicating those decisions to other healthcare professionals. Finally,
data will be collected from clinical clerkship preceptors via a survey assessing preceptor
perception of fourth year pharmacy students ability to find and interpret evidence-based
medicine while on rotations. In this survey, we will also assess the skills they believe are
necessary for student pharmacists to be successful on clinical clerkships.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-099
Title: Clozapine induced myocarditis
Primary Author: Nghi Ha, University of Callifornia, San Francisco - School of Pharmacy,
California;
Email: nghi.ha@ucsf.edu
Additional Author(s):
Abraham Chang
Kelly Matsuda
Purpose:
Methods:
Results:
Conclusion:
Case Report: Myocarditis induced by the antipsychotic drug clozapine is rare, but frequently
fatal. This case demonstrates the identification and management of clozapine induced
myocarditis in a young patient with no prior history of cardiac disease. A 22 year old male
patient with severe bipolar disorder with paranoia was transferred to medicine from inpatient
psychiatry for workup due to worsening sinus tachycardia, mild white blood cell (WBC) count
elevation, mild troponin elevation, and C-reactive protein (CPR) elevation after clozapine
loading. On exam, patient was asymptomatic with no chest pain, cough, shortness of breath,
palpitation, fevers, chills, or URI prodrome. Baseline laboratory results showed WBC at 11.7
K/uL with normal diff, troponin at 0.3 ng/mL, CRP at 16.7 mg/dL, and D-dimer of 3,725 ng/mL
FEU. EKG showed atrial tachyarrhythmia [Heart Rate (HR) = 130 beats per minute (bpm)] with
ST elevation. A transesophageal echocardiogram (ECHO) was done showing a normal size left
ventricle with a mildly-moderately reduced left ventricular ejection fraction (LVEF) of 43%.
Due to the elevated D-dimer, a computed tomography angiography was done which showed no
evidence of pulmonary embolism. Given test results and patient’s medical history, the
medicine team suspected myocarditis and discontinued clozapine. Acute coronary syndrome was
ruled out by the medicine team due to patient’s age, lack of risk factors, and the lack of
increase of troponin during monitoring period. The elevated D dimer was attributed to
inflammation. Elevated CRP was noted, non-specific but supports inflammatory process like
pericarditis. Patient was started on aspirin 325 mg PO daily. Lamotrigine 100 mg PO QPM and
ibuprofen 400 mg PO Q6hr PRN was continued from before. On medicine service day 1,
patient’s troponin peaked at 1.6, HR improved to around 110 bpm, and WBC continued to
rise. On medicine service day 2, his troponin returned to 0.3, improved HR at 80-110 bpm, and
WBC peaked at 14.3. On medicine service day 3, patient WBC normalized to 8. Patient
tachycardia has resolved HR at 70-80 beats per minutes. Patient was transferred back to
psychiatry on the 4th day of medicine service. Patient was discharged from the hospital with
carvedilol 3.125 mg PO BID, lamotrigine 100 mg PO QPM, and ibuprofen 400 mg PO Q6hr
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
PRN for management of his psychiatric problem and myocarditis. Patient was given instruction
to follow up with an outpatient cardiologist and to have a repeat ECHO in 2-4 weeks. This case
demonstrates the importance of close monitoring during clozapine titration. Rechallenging with
clozapine is not recommended in patients with clozapine induced myocarditis.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-100
Title: Mormordica charantia (Bitter Melon) does not show any significant hypoglycemic effect
on Type 2 diabetic patient.
Primary Author: Hemant Hirpara, Western University of Health Sciences, California;
Email: hhirpara@westernu.edu
Additional Author(s):
Nancy C. Lee
Raynold V. Yin
Olivia J. Phung
Purpose: Mormordica charantia (bitter gourd or bitter melon) has been investigated for use in
lowering plasma glucose in patients with diabetes mellitus (DM). However, the evidence is
currently inconsistent to determine the magnitude or statistical significance of this effect. Our
current project aims to synthesize the available evidence on this topic to determine whether bitter
melon has a favorable effect in lowering plasma glucose in patients with DM.
Methods: We searched PubMed, EMBASE and Cochrane Central Register of Controlled Trials
from database start to July 2013 without any language restrictions for randomized controlled
trials (RCT) which compared bitter melon to no treatment in patients with type 1 or type 2
diabetes. Studies were selected, data was extracted, and the validity of each article was
independently assessed by two investigators. Each RCT was appraised for proper random
sequence generation, allocation concealment, blinding, selective reporting and completeness of
outcomes reporting to help assess the risk for any biases. Information collected from each trial
included study characteristics, inclusion and exclusion criteria, and results on the outcomes of
glycosylated hemoglobin (A1c) and fasting plasma glucose (FPG). The glycemic results of each
RCT were analyzed to yield the weighted mean differences (WMD) and 95% confidence
intervals (CIs).
Results: After identifying and screening for eligibility, four RCTs, each with 40 to 66
participants, followed between 4 to 12 weeks were used in this meta-analysis. Overall risk of
bias for each of the included RCTs was determined to be unclear. A total of 208 participants with
type 2 diabetes mellitus (T2DM) with a mean age of 56.5 years were evaluated. Compared with
no treatment, bitter melon supplementation did not significantly lower the A1c (WMD -0.13%,
95%CI -0.41 to 0.16) nor FPG (WMD 2.23 mg/dl, 95%CI -14.91 to 19.37).
Conclusion: Bitter melon supplementation compared with no treatment did not show significant
glycemic improvements on either A1c or FPG.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-101
Title: Barriers to sunscreen use among high school teens
Primary Author: Joon Hwang, Skin Cancer Awareness Committee, Western University of
Health Sciences School of Pharmacy/California;
Email: jkhwang@westernu.edu
Additional Author(s):
Daisy Park
Jennifer Ito
Rachel Chung
Doreen Pon
Purpose: Childhood sun exposure and use of tanning beds are associated with an increased risk
of developing skin cancer later in life. A 2002 study found that 75% of US high school students
had a preference for tanned skin. Modifying childhood sun safety behaviors may decrease the
risk for skin cancer. The purpose of our study was to determine barriers to sunscreen use in teens
and if teens with a preference for tanned skin were less likely to report use of sunscreen before
and after a skin cancer awareness educational program than teens without a preference for tanned
skin.
Methods: An hour-long interactive skin cancer awareness educational program was presented to
approximately 800 high school students during scheduled class hours. Institutional review board
approved written surveys were administered to students before (baseline) and immediately after
(post-intervention) the educational program. The surveys were designed to evaluate skin cancer
and sun safety knowledge, self-reported sun safety behaviors, and perceived barriers to sunscreen
use. Parental consent and student assent were obtained to participate in the study.
Results: 433 students completed their consents and baseline and post-intervention surveys and
were included in the study. The majority of the students were female (60.9%), between the ages
of 15-18 years old (87.9%), and either Hispanic/Latino (51.2%) or White/Caucasian (28.7%).
Major barriers to sunscreen use were lazy/busy/forget (47%), not necessary (30.9%), and
oily/smelly/uncomfortable (9.1%). Cost was identified as the major barrier by only 1.1% of
students. Although only 5.4% of students reported not using sunscreen because they wanted to
tan, 61.5% of students overall reported that tanned skin was attractive, and 62.6% of those
students reported intentionally tanning, compared to 19.2% of students who did not agree that
tanned skin was attractive (Fishers exact p<0.0001, odds ratio 7.0, 95% CI 4.4-11.1). In the
baseline and post-intervention surveys, self-reported or intended daily sunscreen use improved
from 8.3% to 55.7% (Fishers exact p<0.0001), and skin cancer prevention as the major
motivation for sunscreen use changed from 9.3% to 70.6% (Fishers exact p<0.0001). There was
no statistically significant difference in daily sunscreen use nor motivation for sunscreen use in
the baseline and post-intervention survey responses for students with and without preferences for
tanned skin.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Daily sunscreen use is uncommon among teens, with the major reason for non-use
related to inconvenience. Education can improve teens intention and motivation for sunscreen
use, even among those teens with a preference for tanned skin.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-102
Title: Scholarly contributions of required senior research projects within a Doctor of Pharmacy
curriculum
Primary Author: Francisco Ibarra, University of California San Francisco, California;
Email: francisco.ibarra@ucsf.edu
Additional Author(s):
Mitra Assemi
Purpose: Student participation in a curriculum integrating research-related opportunities
promotes the development of clinicians who think critically, discover alternative health
solutions, and implement best practices. This study investigates faculty perceptions of and
dissemination outcomes related to required senior research projects completed by PharmD
students enrolled in the least research intensive pathway [Pharmaceutical Care] at a School of
Pharmacy from 2008-2011. A secondary aim compares these results to outcomes of 1)
Pharmaceutical Care projects completed between 2002-2007 and 2) projects completed by
students in the two more research intensive pathways [Health Services and Policy Research,
Pharmaceutical Sciences] from 2002-2011.
Methods: This study received exempt approval by the Institutional Review Board. From 20082011, 132 projects were precepted by 64 research preceptors. Of these, 131 projects were linked
to 63 preceptors with an email address. A Qualtrics survey, designed based on instruments used
in two previous studies, determines preceptors perceptions regarding the value of each research
project and outcomes related to dissemination of study findings. Following a pilot with 22
projects (4 preceptors), the survey was administered in September 2013. Data collection ends
October 2013. Preliminary data on 77 projects (31 preceptors) found 68% of projects were
retrospective clinical studies. Twenty-four of 35 (69%) projects submitted for publication were
accepted and published in various journals (e.g., American Journal of Addiction, American
Journal of Pharmaceutical Education, Annals of Pharmacotherapy, Journal of Emergency
Medicine). Faculty agreed involvement with student projects was valuable to themselves (88%)
and their institution (85%), and were largely willing to work with future students (93%). Deidentified data will be analyzed in SPSS and combined with/compared to that for Pharmaceutical
Care projects completed from 2002-2007 and collectively compared to that for Health Services
and Policy Research and Pharmaceutical Sciences projects completed from 2002-2011.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-103
Title: Assessing the effectiveness of a pharmacist-managed transition of care service at reducing
30-day readmission rates in a community hospital
Primary Author: Mary Margaret Kwong, University of California, San Francisco, California;
Email: MM.Kwong@ucsf.edu
Additional Author(s):
Sarah Liu
Askar Nadjafov
Nancy Nkansah
Purpose: Nearly one in five Medicare patients are readmitted within 30 days of hospital
discharge, and approximately two-thirds are medication-related. Drug-related issues are common
after hospitalization when medication changes frequently occur. Different transition of care
models have been used in an effort to reduce readmission rates, and it appears that pharmacistled models may have a significant impact in preventing unnecessary medication-related adverse
events and subsequent re-hospitalization. The objective of this study is to assess the effectiveness
of a pharmacist-managed transition of care service at reducing 30-day readmission rates in a
community hospital in Fresno, California.
Methods: The University of California, San Francisco Institutional Review Board has approved
this study. This retrospective study will compare the proportion of patients who were readmitted
to the Telemetry unit from January to June 2012, in the absence of pharmacist-led interventions
(control group), to patients readmitted from January to June 2013, when pharmacist joined the
care team (intervention group). Pharmacist-directed interventions included: inpatient counseling,
discharge counseling, and/or telephone follow-up. All patients with local indigent insurance
program, as well as Medicare patients admitted for a high-risk diagnosis (e.g. heart failure,
chronic obstructive pulmonary disease, asthma, pneumonia, diabetes mellitus, or acute coronary
syndrome) will be assessed. The electronic medical record system, hospital readmission reports,
and Redcap database will be used to identify patients who meet at least one pre-specified, highrisk criteria for readmission: patients 65 years and older and taking more than six medications,
patients taking more than nine medications, patients taking at least one high-risk medication (e.g.
anticoagulants, injectables, brand/non-formulary medications), or patients with an unplanned
readmission within six months. The proportion of subjects that were readmitted during each
period will be calculated and efficacy and cost-effectiveness will be determined.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-104
Title: Adrenal suppression with topical corticosteroid use in psoriasis patients
Primary Author: Lisa Lam, University of California, San Francisco, CA;
Email: lisa.lam@ucsf.edu
Additional Author(s):
Jeffrey Sugarman
Purpose: Topical corticosteroids (TCS) are used for a variety of skin conditions, including
psoriasis. Because of potential systemic absorption, chronic TCS use may have side effects
similar to those of systemic corticosteroids. Long term effects include immunosuppression and
adrenal suppression. However, patients using TCS are not routinely screened for adrenal
suppression, and it is not a factor that many physicians consider when prescribing TCS. The
degree of suppression and the resulting health effects are unknown. There are no signs or
symptoms of adrenal suppression until clinical signs of Cushings syndrome occur. These patients
may be unaware of their risk in the case of serious trauma during which their atrophied adrenal
glands may not be able to produce physiological concentrations of cortisol, and thus cannot
respond to shock. In this study, the degree of adrenal suppression, assessed in chronic psoriasis
patients by measuring average post-cosyntropin stimulation cortisol levels, was greater in
patients with severe psoriasis involving larger body surface area (BSA) than those with moderate
psoriasis involving a smaller BSA (averages of 18.83 and 23.22mcg/dL, respectively; P=0.03).
Both groups had significantly lower post-cosyntropin cortisol levels in comparison to normal,
healthy individuals (average=32.5, P<0.001 for both).
Methods: Data from this retrospective study is provided from screening visits from a separate,
but related clinical trial evaluating the efficacy of a potent TCS combination for patients with
moderate to severe psoriasis. All patients had a clinical diagnosis for psoriasis and were assumed
to have a history of TCS use, although it may not have been captured in every case at the
screening visit during which medication use history from only the past year was recorded.
Patients with psoriasis affecting 10 to 15% of total body surface area (BSA) were assumed to
have moderate psoriasis and therefore using lower potency TCS or non-steroidal treatment for
management (n=9). Patients with psoriasis affecting 16 to 20% of total BSA were assumed to
have severe psoriasis and therefore using higher potency TCS for management (n=6). Therefore,
these two sets of patients were compared for differences in degree of adrenal suppression using a
t-test, as well as compared to normal, healthy individuals (n=45). Adrenal suppression was
assessed by measuring patients cortisol level 30 minutes following adrenal stimulation with
Cosyntropin, a synthetic adrenocorticotropic hormone (ACTH).
Results: Patients with moderate psoriasis involving 10 to 15% of total BSA and using lower
potency TCS or non-steroidal medications had an average post-cosyntropin cortisol level of
23.22 mcg/dL. Those with severe psoriasis affecting 15 to 20% of total BSA and using highpotency TCS had an average post-cosyntropin cortisol level of 18.83 mcg/dL, which was
significantly less than that of those with severe psoriasis (P=0.03). Both severe and moderate
psoriasis patient groups had significantly lower post-cosyntropin cortisol levels in comparison to
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
normal, healthy individuals (average=32.5, P<0.001 for both). Secondary adrenal insufficiency,
such as secondary to medication use, is defined as a post-cosyntropin level < 25mcg/dL. Patients
in the high-potency TCS group were significantly below this threshold for diagnosis of adrenal
suppression (P=0.049).
Conclusion: Prescribers should be aware that chronic TCS use may have potential adverse
effects which may not be recognized until significant morbidity has occurred. These results
demonstrate that chronic TCS use, as is often practiced in real clinical settings, rather than for
two to four week intervals as is directed in the package insert, is associated with adrenal
insufficiency and suppression. Chronic TCS use may put patients at risk for Addisonian crisis
following trauma, orthostasis, hypoglycemia, and mood disorders. Larger studies are warranted
to further assess the degree of adrenal suppression and the incidence of systemic effects
associated with TCS use.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-105
Title: Increased Risk for Atypical Fractures Associated with Bisphosphonate Use
Primary Author: Nancy Lee, Western University of Health Sciences, California;
Email: nlee@westernu.edu
Additional Author(s):
Hemant Hirpara
Raynold V. Yin
Samantha Llanos
Olivia J. Phung
Purpose: Studies suggest an increasing occurrence of atypical femoral fractures with the use of
bisphosphonates. The purpose of this systematic review is to examine whether the use of
bisphosphonates increases the risk for atypical fractures.
Methods: We conducted a literature search of MEDLINE, Embase, and Cochrane CENTRAL
(1948-to-June 2013). Studies were included in this systematic review if:1) it was either a
randomized controlled trial (RCT) or an observational study which adjusted for confounders, 2)
evaluated bisphosphonate therapy versus no treatment, and 3) reported an incidence of
subtrochanteric or diaphyseal fracture individually, or a composite of subtrochanteric fracture
and diaphyseal fracture. The estimated effects and associated variances were pooled using a
random-effects model, and results reported as adjusted odds ratios (AOR) with accompanying
95% confidence intervals (CI). Heterogeneity was evaluated with I2 statistic. Publication bias
was assessed using the Eggers p-value
Results: Six studies (n = 658,497) were included in the meta-analysis which demonstrated a
statistically significant increased risk of subtrochanteric or diaphyseal fracture with
bisphosphonate use (AOR=1.99, 95%CI: 1.28 to 3.10). A high heterogeneity was detected
(I2=84.3%) and publication bias was detected Egger P=0.01). Subtrochanteric fractures showed
an AOR=2.71 (95%CI = 1.86 to 3.95) with I2=83.6% and Eggers P=2.29. Diaphyseal fractures
had an AOR=2.06 (95%CI = 1.70 to 2.50), I2=29.7% and Eggers P=1.22.
Conclusion: The results from this systematic review suggest that there is an increased risk for
atypical fractures associated with the use of bisphosphonates and also helps to raise awareness to
the potential complications related with bisphosphonate therapy. These findings warrant the
comprehensive evaluation of each patient before initiating bisphosphonate therapy to determine
if the benefits will outweigh the associated risks.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-106
Title: Prevalence and compliance of dietary supplement advertisements with United States
regulations in popular Spanish, Chinese, and Korean media outlets
Primary Author: Anthony Lee, University of California, San Francisco, California;
Email: tony.lee@ucsf.edu
Additional Author(s):
Wingchi Wong
Lesley Vasquez
Jaekyu Shin
Purpose: Little is known about the prevalence of dietary supplement advertisements in Spanish,
Chinese, and Korean media outlets despite growing populations speaking these languages in the
United States. In addition, it is unknown how well these advertisements comply with the
regulations of the Federal Trade Commission (FTC) and the Food and Drug Administration
(FDA). The objective of this study is to compare the prevalence and compliance of dietary
supplement advertisements with the FTC and FDA regulations among popular English, Spanish,
Chinese, and Korean media outlets in the San Francisco and Los Angeles areas.
Methods: This is a cross sectional study examining dietary supplement advertisements in
popular English, Spanish, Chinese, and Korean media outlets (i.e., daily periodicals, weekly
periodicals, and television) in San Francisco Bay Area and Los Angeles areas from September
30, 2013 to January 12, 2014. In each language, two daily and two weekly periodicals as well as
one popular TV station will be selected based on circulation volume and TV rating data. Study
outcomes are percent of dietary supplement advertisements, percent of dietary supplement
advertisements violating health claim regulations, and number of dietary supplement
advertisements containing unsubstantiated health claims. FDA authorized health claims will be
used to determine violation of health claim regulations. The number of quality studies identified
in MedlinePlus will be used to determine substantiation of health claims. Data collection will be
performed on a rotating schedule to include one weekday and one weekend day each week. Each
study day will be considered as an observation unit. Depending on the data distribution, analysis
of variance or Friedman test will be used to compare each study outcome across the 4 different
languages by media outlet. When appropriate, pair wise comparisons will be conducted with the
Bonferoni test.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-107
Title: Peripheral and central hemodynamic parameter changes post-exercise, high-fat meal
intake, or energy drink consumption
Primary Author: Shawlien Lie, University of the Pacific, Thomas J. Long School of Pharmacy
and Health Sciences, California;
Email: s_lie@u.pacific.edu
Additional Author(s):
Shu Lu
Keira A. Simmons Domer
Cynthia Song
Sachin A. Shah
Purpose: Multiple studies have shown that central (aortic) blood pressure (CBP) is a stronger
predictor of cardiovascular incidents compared to peripheral blood pressure (PBP). Health care
professionals are increasingly using central hemodynamic parameters to further evaluate
cardiovascular risks. Recommendations for CBP assessment require fasting overnight, abstaining
from caffeinated drinks, and avoiding exercise 24 hours prior to measurements, among other
stringent recommendations. To better understand the magnitude of impact if the above
recommendations are not followed, we evaluated the change in hemodynamic parameters after
high-intensity exercise, high-fat meal intake, or energy drink consumption.
Methods: This was a pilot evaluation using a cross-over methodology in a healthy, male
volunteer. The primary endpoint was the maximum change in augmentation index (AIx)
corrected at a heart rate of 75 beats per minutes (bpm) seen in each arm. Secondary endpoints
were peripheral systolic blood pressure (PSBP), diastolic blood pressure (PDBP), and pulse
pressure (PPP), and central systolic blood pressure (CSBP), diastolic blood pressure (CDBP),
pulse pressure (CPP), subendocardial viability ratio (SEVR). The intervention arms comprised of
high-intensity exercise, high-fat meal intake, energy drink consumption, and a per
recommendation control arm. All endpoints were evaluated at baseline, 30, 90, 210, and 330
minutes for each arm. PBP was measured using a standard calibrated automated blood pressure
machine, and central hemodynamic parameters were measured using the validated SphygmaCor
system. The subject avoided exercise during the preceding 24 hours, fasted overnight (8 hours),
refrained from taking any medications or dietary supplements, avoided caffeine consumption,
and fasted during all PBP and CBP measurements. Each intervention was performed over 15
minutes, after which 12 ounces of water was consumed. All data will be reported using
descriptive statistics.
Results: The maximum change in AIx from baseline for high-intensity exercise, high-fat meal
intake, energy drink consumption, and a per recommendation control arm, were 4mmHg,
1mmHg, 19mmHg, and 9mmHg, respectively. A consistent increase of AIx was observed in the
energy drink arm, starting at 90 minutes, with an over 300% increase observed at 330 minutes.
There were no significant adverse effects experienced in any of the arms.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Monster Energy drink consumption increased the AIx, while high-fat meal intake
and vigorous exercise had no impact on AIx. Future large scale, longer duration studies are
warranted on the impact of energy drinks and central hemodynamic parameters for validation of
our pilot results.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-108
Title: Discordance in Nucleic acid amplification tests (NAATs) among Urinary Gonorrhea (G)
and Chlamydia (C) Screening versus G/C Screening via Throat and Rectal Swap
Primary Author: Jian-ya Lin, University of California, San Francisco - School of Pharmacy,
California;
Email: Jian-ya.Lin@ucsf.edu
Additional Author(s):
Nghi Ha
Joshua Smith
Wilson Ly
Purpose: The CDC currently recommends site-specific G/C screening based on sexual risk
factors, especially among men who have sex with men (MSM). However, urine based screening
is still the main method even in high risk patients. G/C screening using only urine NAATs test in
MSM has been shown to have high proportion of unidentified G/C infections which poses
increased risk of complication for the patient, as well as public transmission. Thus, the purpose
of this study is to identify the discordance in G/C screening in MSM in a community-based HIV
clinic.
Methods: Retrospective chart review of new and returning patients from July 1, 2012 through
July, 13, 2013 at Santa Clara Valley Medical PACE (Partners in AIDS Care and Education)
clinic. All MSM patients with urine and throat and/or rectal G/C results will be included in the
analysis. Major exclusion criteria were patients who were not screened for G/C, patients who do
not engage in MSM, or those who refused G/C screening. Primary endpoint is percent
discordance between urine G/C results versus throat and/or rectal results. Secondary endpoint is
to report percent of MSM patients with risk factors who were not screened with throat and/or
rectal swap. A positive result is determined by nucleic acid amplification tests (NAATs) of oral,
anal, and/ or urine sample from the patient. Risk factors will be assessed using chart review. Data
analysis will be done via STATA 11.0.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-109
Title: Evaluation of time to first-dose intravenous antibiotic administration in hospitalized
patients
Primary Author: Amy Lo, Western University of Health Sciences, California;
Email: loa@westernu.edu
Additional Author(s):
Juanqi Zhu
Mark Richman
Julianne Joo
Patrick Chan
Purpose: Delay in appropriate antibiotic administration is associated with increased mortality
and length of stay (LOS) in patients with severe sepsis and septic shock. In an effort to improve
timeliness of first dose antibiotic in all patients, frequently used intravenous (IV) antibiotics,
previously only available via delivery from the inpatient pharmacy, were placed in Pyxis
machines in all units of the hospital in August 2012. The purpose of the study is to examine the
effect on time to first dose antibiotic before and after implementation (PRE versus POST) of
floor stock antibiotics.
Methods: The institutional review board approved this retrospective chart review of adult
patients hospitalized between January to March 2012 and February to March 2013. Hospitalized
patients who received piperacillin/tazobactam 3.375 grams IV were included. Those who
received the first dose in the emergency department were excluded. Medical charts and
pharmacy database were used to collect demographic, clinical and medication information.
Primary endpoint was the total time elapsed from the time of physician order to the documented
time of antibiotic administration (order-to-administration). In addition to time of physician order
(order) and medication administration (administration), we identified time of order scanned to
pharmacy (queue) and medication order entry by pharmacist (release) to assess which steps of
the drug distribution process were affected by the implementation of Pyxis antibiotic floor stock.
Moreover, we evaluated indication of antibiotic, discharge diagnosis, in-hospital mortality and
LOS.
Results: A total of 121 subjects were included (PRE: n equals 65; POST: n equals 56). There
was a significant reduction in total mean time to antibiotic administration from 4.5 plus/minus
4.1 to 2.9 plus/minus 2.5 hours (p equals 0.009), a 1.7 hour reduction, with implementation of
floor stock antibiotics. Analysis of additional time points showed a significant reduction in time
of queue-to-administration time (3.3 plus/minus 3.4 versus 1.7 plus/minus 1.5 hours, p equals
0.001) and release-to-administration (2.4 plus/minus 2.4 versus 1.4 plus/minus1.5 hours, p equals
0.034). However, the time from order to queue did not change significantly between the groups
(1.7 plus/minus 1.9 versus 1.2 plus/minus 2.0 hours, p equals 0.817). Piperacillin/tazobactam
was indicated for pneumonia in half of all patients (50 percent, 61/121) followed by intraabdominal infection (26 percent), skin/soft tissue infection (12 percent) and urinary tract
infection (8 percent). Majority had an infection requiring antibiotic therapy. However, a
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
proportion in each group had a final diagnosis that was not infection-related (28 percent versus
36 percent, p equals 0.34). There was no difference in mortality (8 percent versus 4 percent, p
equals 0.33) and LOS (10 plus/minus 12 versus 12 plus/minus 13 days, p equals 0.39).
Conclusion: There was a significant reduction in time to first dose piperacillin/tazobactam
administration after the implementation of floor stock antibiotics. While the LOS increased
slightly post-implementation of the floor-stock antibiotics, mortality was reduced. Continued
effort to further decrease the mean time to first dose antibiotics is warranted. Future studies may
include timeliness of antibiotic and its effect on clinical outcome in those with severe sepsis and
septic shock.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-110
Title: Evaluation of meropenem use and its correlation to carbapenem resistant
enterobacteriaceae in a 455 bed acute care facility.
Primary Author: Shari McClendon, Loma Linda University School of Pharmacy, California;
Email: smcclendon@llu.edu
Additional Author(s):
Travis Lawler
Marcus Baker
Purpose: Carbapenem resistant enterobacteriaceae is a growing problem and healthcare
professionals are struggling to understand the best way to prevent the resistant strand. Evaluating
meropenem use will help the antimicrobial stewardship committee understand the best way to
restrict the use of carbapenems. By investigating the prevalence of meropenem for empiric
therapy, de-escalation, and susceptibilities we can ultimately, educate other healthcare
professionals to make better choices using meropenem to prevent carbapenem resistant
enterobacteraiaceae.
Methods: The patient population base were adult patients treated with meropenem during this
last June. Patient baseline characteristics were compared and averaged across the patient
population. To verify appropriateness of indication, criteria for an actual diagnosis of a disease
state was determined by looking at a combination of the patients chief complaint, initial
diagnosis, imaging and positive laboratory results. Evaluation of empiric therapy compared
patients receiving mono or dual therapy, with or without meropenem. De-escalation was
determined generally by the discontinuation of meropenem before discharge. The comparison
was made of patients initiated on meropenem empirically verses delayed, with the number of
patients discharged with active meropenem orders. Meropenem therapy duration was assessed to
the patients length of stay to determine the percent of stay on meropenem. The prominence of
cultures and susceptibilities were compared to how many cultures were positive, and how many
of those had susceptibilities. Susceptibilities were compared to treatment changes to determine
acceptance of de-escalation and appropriateness of medication changes.
Results: One hundred six patients met the inclusion criteria but one was removed due to an
incomplete medication list, leaving a total population of one hundred five. The patient population
included were 54% female, their average age was 66 years, average BMI was 30.2 kg/m2, and
their average length of stay was 8.3 days. The criterion placed forth for actual diagnosis was
compared to initial diagnosis and there was a decrease in infections by 16%. In general, 80% of
patients were started on meropenem for empiric treatment the their infection, 30% of those were
on meropenem only, while the other 70% also had an additional agent. The percentage of
patients de-escalated from meropenem prior to discharge was 40%. Out of those empirically
started on meropenem, 40% were de-escalated before discharge. At the time of discharge, 63%
of all patients had active meropenem orders. On average, patients were taking meropenem 65%
of their length of stay or an average of five days. Out of the 95% of patients to had cultures
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
ordered, 51% of patients had positive cultures with 46% of those having susceptibilities, and
72% had appropriate de-escalation based off of those susceptibilities.
Conclusion: Physicians are using meropenem as empiric therapy for suspected infections; this is
a concern when trying to use the narrowest spectrum for antibiotic therapy. The rate of deescalation is good, but needs to improve, becoming an event greater priority. By using cultures
and susceptibilities and de-escalation, pharmacists and physicians together can make greater
strides in preventing carbapenem resistant enterobacteriaceae.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-111
Title: Assessment of patient risk factors for extended spectrum beta lactamase producing
Escherichia coli
Primary Author: Janine Ng, Western University of Health Sciences, California;
Email: Janine.Ng@va.gov
Additional Author(s):
Arthur Jeng
Patrick Chan
Purpose: The bacteria Escherichia coli is the most common cause of urinary tract infections
(UTIs). Extended spectrum beta lactamase (ESBL) E. coli exhibits resistance to many antibiotics
which can result in higher mortality rates and longer hospital stays. ESBL UTIs force hospitals to
increase usage of carbapenems, the treatment of choice for ESBL infections. Identification of
risk factors to screen patients can improve empirical treatment, reserving carbapenem use for
when it is truly needed. The objective of this study was to determine the presence and
significance of literature reported risk factors for ESBL E. coli UTIs at a large county hospital.
Methods: This retrospective, observational, case control study included patients who were 18
years or older that were admitted to the hospital between September and December 2012 with a
urinary tract isolate of E. coli. Pediatric and neonatal patients were excluded. There were 28
patients in the ESBL E. coli group and 30 in the case control (non ESBL) E. coli group. Twelve
literature identified risk factors were assessed: recent hospitalization, recent antibiotic use, use of
a foley catheter, residence in long term care (LTC), recent travel history, pets, diabetes mellitus
(DM), hemodialysis (HD), history of a UTI, use of immunosuppressive therapy, malignancy, and
history of a prior ESBL E. coli infection. Recent was defined as within 3 months of admission.
Patient demographics, history, comorbidities, the twelve literature identified risk factors,
diagnosis, course of hospital stay, and outcomes were gathered from computerized medical
charts. Outcomes included the mean length of hospital stay, whether the pt was admitted to the
Intensive Care Unit and whether the patient expired. Two analyses were performed: comparison
by isolate and comparison by gender. Statistical analyses, including a paired t test, Fishers exact
test, and odds ratio, were performed using Microsoft Excel and GraphPad Prism.
Results: ESBL E. coli patients more frequently had history of UTI (61 percent versus 27
percent, odds ratio equals 4.25, P less than 0.001), history of ESBL infections (46 percent versus
0 percent, odds ratio equals 53.13, P less than 0.001), recent hospitalization (64 percent versus 8
percent, odds ratio equals 4.95, P equals 0.003), recent antibiotic use (82 percent versus 27
percent, odds ratio equals 12.65, P less than 0.001) and residence in LTC (21 percent versus 0
percent, odds ratio equals 17.62, P equals 0.01). Use of a foley catheter, recent travel, pets, DM,
HD, immunosuppressive therapy, and malignancy were not significant between the two groups.
The mean total number of risk factors between the ESBL E. coli and non ESBL E. coli patients
were 4.5 plus or minus 1.5 and 1.8 plus or minus 1.6, respectively, (P less than 0.001). A few
ESBL patients (4 percent) and non ESBL patients (20 percent) had zero risk factors upon
admission for UTI (P equals 0.10). A sub group analysis was performed which showed all
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
literature reported risk factors for ESBL E. coli between males and females, including male sex,
age and history of UTI, were not significant in this study.
Conclusion: While patients with a non ESBL E. coli UTI have many choices for antimicrobial
treatment, those with ESBL E. coli UTIs are less likely to receive appropriate, empirical
antimicrobial therapy (i.e., with a carbapenem). However, increasing usage of carbapenems
escalates the risk of its resistance. In our county hospital, a decision for empirical treatment of
UTIs should weigh risk factors associated with ESBL E. coli UTIs, including a history of UTI,
history of ESBL infections, recent hospitalization, recent antibiotic use, and residence in LTC.
Such data can be used to construct an empirical treatment algorithm that more judiciously
utilizes carbapenems.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-112
Title: Evaluation of pharmacist-managed outpatient warfarin therapy for post total knee
arthroplasty
Primary Author: Rachel Pavelko, South Dakota State University - College of Pharmacy, South
Dakota;
Email: rachel.pavelko@jacks.sdstate.edu
Additional Author(s):
Krista Sarvis
William Hayes
Purpose: The American College of Chest Physicians recommends venous thromboembolism
(VTE) prophylaxis with an anticoagulant following total knee arthroplasty (TKA) for at least 1014 days. The estimated incidence of VTE after TKA without anticoagulation is 40-88 percent.
The institution under evaluation started performing TKAs in January 2013. The surgeon prefers
warfarin after surgery with INR goal 1.7-2.3 for 21 days which is consistent with other facilities
in our region. At this institution, warfarin is managed centrally through a pharmacist-run
anticoagulation clinic. This quality improvement projects purpose is to assess the efficacy and
safety of warfarin management by pharmacists after TKA.
Methods: In this quality improvement project, a retrospective chart review, by a pharmacy
student, reviewed all patients from January 1, 2013 to June 30, 2013 who underwent a TKA with
outpatient warfarin managed by a pharmacist through outpatient anticoagulation clinic for a total
of 21 days. Management of inpatient warfarin therapy was not evaluated. Data points collected to
evaluate safety and efficacy included: international normalized ratio (INR), warfarin dosage
adjustments, frequency of follow-up appointments, incidence of VTE and incidence of bleeding
or bruising.
Results: Surgery was performed on a Monday with discharge from the hospital the following
Thursday or Friday after surgery. The evaluation period was divided into days 7-13 and days 1421. During the assessment period, 15 patients received outpatient warfarin managed by a
pharmacist for VTE prophylaxis following TKA. A total of 51 INR checks were completed
between days 7 and 21, and of these, 15 (29 percent) were therapeutic (INR 1.7-2.3), 31 (61
percent) were subtherapeutic (INR less than 1.7), and 5 (10 percent) were supratherapeutic (INR
greater than 2.3). At the first INR check after discharge (days 7-13 post TKA), 1 (7 percent) was
therapeutic, 12 (80 percent) were subtherapeutic, and 2 (13 percent) were supratherapeutic.
During days 14-21, 7 (47 percent) INR results were therapeutic, 7 (47 percent) were
subtherapeutic, and 1 (6 percent) was supratherapeutic. Three (20 percent) patients never had a
therapeutic INR during the entire duration of outpatient warfarin therapy. The highest INR
recorded was 3.4. There was no incidence of VTE or bleeding/bruising during the assessment
period.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The findings in this quality improvement project show inconsistencies in dose
adjustments when the INR is out of goal range and follow-up time. With the high incidence of
subtherapeutic INR levels, anticoagulation clinic standardization will be considered. A reference
sheet may benefit patients and pharmacists by providing guidance on the initial dosage, dosage
adjustments, and follow-up frequency for outpatient warfarin treatment post-TKA. No incidence
of bleeding or thromboembolism was identified during the review period, and ongoing
monitoring will be conducted by anticoagulation clinic.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-113
Title: Predictors and outcomes of nopal use in Mexican-American adults with type 2 diabetes
Primary Author: Maria Rivas, University of California, San Francisco School of Pharmacy,
California;
Email: Maria.Rivas@ucsf.edu
Additional Author(s):
Jenna Kruger
Lisa Kroon
Judy Quan
Alicia Fernandez
Purpose: In the United States the use of complementary and alternative medication (CAM) has
become common among the diverse population. Clinicians increasingly need to ask patients
about their use in order to gather a complete list of medications they are taking. Prickly pear
cactus, nopal, is frequently used as a dietary supplement among Mexican immigrants/MexicanAmericans to help treat diabetes. Nopal has been shown in studies to decrease blood glucose
levels. Among Mexican-Americans, it is unclear what factors predict nopal use, which can be
useful information for the treating clinician to consider. The objective is to determine the
predictors, clinical correlates, and diabetes behaviors and beliefs associated with nopal use
among Mexican-American adults with type 2 diabetes.
Methods: This study was approved by the Institutional Review Boards at the University of
California, San Francisco, the Cook County Health and Hospital System, and the participating
institutions in Chicago and the San Francisco Bay Area. The study design is a secondary dataanalysis of the Immigration, Culture, and Health Care (ICHC) survey and chart review study,
conducted in 2008-2009. The subjects are 404 English and Spanish-speaking Mexican-American
adults with type 2 diabetes obtaining care in safety-net clinics in San Francisco and Chicago.
Nopal users were those who reported using nopal daily, weekly or monthly. Non-users were
those who reported ingesting nopal rarely or never. Multivariate logistic regression was used to
determine the independent predictors of nopal use, and if nopal use predicted glycemic control or
was associated with differences in the illness experience.
Results: Nopal users were 154 (38%) and non-users were 250 (62%) of respondents. On
bivariate analysis, nopal use was reported more by Spanish-speakers than English-speakers (66%
vs 34%, p<0.0001) and by patients without a degree than those with a high school degree (66%
vs 14%, p=0.004). After adjusting for demographics (age, gender, language, education, income,
acculturation score), health services (health insurance, PCP) and clinical confounders (diabetes
duration, comorbidity count, insulin use, other dietary supplement use), the only predictor of
nopal use was acculturation, with more acculturated respondents less likely to report use
(OR=0.53; CI:0.40-0.70). Nopal use was not associated with differences in mean or poor
glycemic control (defined as A1C >8.5%) or in reports of occasional hypoglycemia (89.5% vs.
90.7%; P=0.70). Nopal users and non-users scored similarly on the Diabetes Self-Efficacy Scale
(Mean (SD) 7.75 (1.50) vs. 7.43 (1.63); P=0.07), Diabetes Distress Scale (3.70 (1.53) vs. 3.59
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
(1.61); P=0.53) and had similar rates of depression on the PHQ-9 Depression Scale (27.9% vs.
36.4%; P=0.08).
Conclusion: Nopal use was widespread among these low-income Mexican-American patients.
Remarkably, only low acculturation predicted its routine use. Use of nopal was not associated
with greater or lesser diabetes self-efficacy, diabetes distress, or depression scores. We found no
evidence to suggest that using nopal was associated with better or worse glycemic control. While
only a randomized trial can determine the impact of nopal on glycemic control, clinicians can be
somewhat reassured that patients who report nopal use are not more likely to have worse illness
experiences or outcomes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-114
Title: Effect of Demographic and Clinical Factors on Clinical Outcomes in PTSD-Associated
Nightmares Treated with Prazosin
Primary Author: Dimitrae Rynsburger, University of the Pacific, California;
Email: d_rynsburger@u.pacific.edu
Additional Author(s):
Jonathon Lacro
Rene Endow-Eyer
Purpose: Prazosin is commonly prescribed to manage nightmares associated with Post
Traumatic Stress Disorder (PTSD). Prazosin affects norephinephrine, which has been implicated
in producing PTSD hyperarousal symptoms. Whereas the majority of published studies have
demonstrated prazosin's benefit, the reports have methodological limitations such as small
sample sizes and short observation periods. Additionally, little is known about potential
demographic and clinical factors associated with positive or negative outcomes. Hence, our study
aims to calculate the percentage of Veterans with PTSD nightmares who positively respond to
treatment with prazosin and to explore the relationship of a priori demographic and clinical
characteristics with outcomes.
Methods: We are conducting a retrospective chart review of Veterans receiving PTSD care at a
VA Medical Center. Each subject has PTSD defined by DSM-IV-TR criteria and received at
least one prescription of prazosin for recurrent distressing dreams or nightmares. Subjects will be
observed for a maximum of 12 months. Demographic factors such as age, gender, type of trauma
(combat, sexual or other) and conflict (Vietnam, Afghanistan/Iraq or other) along with clinical
characteristics such as duration of PTSD illness, concurrent psychiatric illness, adherence status
as measured by medication possession ratios, frequency of dose escalation during prazosin
initiation and maximum daily dose will be reviewed and contributions to outcomes will be
examined. Planned outcome assessments include a global assessment of change, frequency and
intensity of nightmares, and sleep quality. Appropriate statistical analyses are planned.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-115
Title: Vacuolar Protein Sorting 35 (Vps35) rescues Locomotor Deficits and shortened Lifespan
in Drosophila expressing a Parkinson's Disease Mutant of Leucine-Rich Repeat Kinase 2
(LRRK2)
Primary Author: Shannon Shea, Thomas J. Long School of Pharmacy and Health Sciences,
University of the Pacific, California;
Email: s_shea@u.pacific.edu
Additional Author(s):
Jieyun Cao
Sarah Anne Wong
Radek Linhart
Katerina Venderova
Purpose: Current Parkinsons Disease (PD) pharmacotherapy options do not slow the detrimental
progression of neurodegeneration. In order to find disease modifying treatment for PD patients,
the lab generated mutant PD expressing Drosophila model that overexpresses the second most
common causative gene of PD, LRRK2. Then a genetic modifier screen identified a core unit of
the retromer encoding gene. We present evidence that overexpression of the Vps35 retromer
subunit ameliorates the pathogenic mutant LRRK2 eye phenotype. Furthermore, Vps35
overexpression protects from the locomotor deficits and rescues their shortened lifespan, as
assessed by the negative geotaxis assay. Over expressing Vps35 alone protects from rotenone as
well.
Methods: Drosophila Genetics: UAS&#8208;LRRK2(I2020T) characterized previously
(Venderova et al., 2009)P{EPgy2}Vps35EY14200/CyO (line#20913) was obtained with the
empty UAS element upstream of Drosophila Vps35, allowing for a Gal4&#8208;dependent cell
tissue over expression (Bellen et al., 2004; Korolchuk et al., 2007). To increase transgene
expression under temperature&#8208;sensitive UASGal4 expression system (Venderova et al.,
2009), flies were cultured on cornmeal medium at 29C (12&#8208;hrs dark/light cycle), except
for the rotenone&#8208;treated flies. Assessing the eye phenotype, GMR&#8208;Gal4 drove the
expression of LRRK2(I2020T) and/or Vps35 in the eye. After 10 days, 156 flies from 3 crosses
were analyzed under stereomicroscope. LRRK2(I2020T) and/or Vps35, was overexpressed in
DA neurons of progeny for geotaxis climbing assays: 5, 10 and 20 days. We recorded flies that
crossed a line after being tapped down 8 cm above the tube base: 5, 10 and 30 seconds. The flies
used in the climbing assay were daily analyzed for survival. Flies were placed in vials containing
fly-food (Carolina Biological Supplies) + rotenone (1mM; Enzo, Farmingdale, NY). Survival
and locomotor activity assessed daily. Rotenone is light&#8208; and
temperature&#8208;sensitive, the flies were reared at RT and in the dark. All data analyzed with
One&#8208;Way ANOVA with a Tukeys post&#8208;hoc test, or by Two&#8208;way
ANOVA then Bonferonis post&#8208;hoc test.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Results: Vps35 partially rescues the eye phenotype of flies expressing pathogenic mutant
LRRK2: Expression of one of the PD-causing kinase mutants LRRK2(I2020T), under GMR
promoter causes a rough eye + pigmentation(7.56% of eyes, +/&#8208; 3.92%). A genetic
modifier screen was used to identify Vacuolar protein sorting 26 as a LRRK2 interacting gene
Vps26. Vps26 along with Vps35 and Vps29, makeup the cargo&#8208;recognition unit of the
retromer. VPS35, has been recently identified as a new candidate PD gene
(Vilarino&#8208;Guell et al., 2011). Increased Vps35 expression completely rescued the black
lesion phenotype of LRRK2 mutants: none of the analyzed eyes displayed any black lesions
(P<0.0001; F (2, 6) = 102.3) (F1). Vps35 genetically interacts with LRRK2 in the Drosophila
eye. VPS35 rescues the locomotor and lifespan deficits of flies expressing pathogenic mutant
LRRK2: Overexpressing hLRRK2(I2020T) in DA neurons causes significant locomotor deficitswas reduced by 61.45% +/&#8208; 7.49% on day 5. LRRK2 phenotype can be rescued by
overexpressing Vps35 in DA neurons. 70.00% +/&#8208; 6.36% flies overexpressing Vps35 +
mutant LRRK2 crossed the line within 5 seconds) (P < 0.0001; F (4, 77) = 8.20) (Figure 3A).
Similar to day 5, Vps35 overexpression rescued the LRRK2(I2020T) phenotype on day 10.
MORE RESULTS ON POSTER.
Conclusion: The data provide evidence in support that LRRK2 plays a role in the endolysosomal
pathway and that the pathology caused by mutant LRRK2 may be at least partly linked to a
disruption of this important protein sorting and recycling cellular process. However, how exactly
this pathway contributes to PD pathology is at present entirely unknown. Elucidation of new
molecular pathways involved in the pathogenesis of PD may bring forward novel
pharmacological targets for better treatments. Therefore, deciphering the precise role of LRRK2
in the retromer&#8208;dependent pathway and the role of this pathway in PD pathogenesis
deserves further investigations.-K. Venderova
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-116
Title: Prevalence and Risk Factors for Sexually Transmitted Diseases (STD) among HIVpositive Patients
Primary Author: Joshua Smith, University of California, San Francisco - School of Pharmacy,
California;
Email: Joshua.Smith@ucsf.edu
Additional Author(s):
Nghi Ha
Jian-ya Lin
Wilson Ly
Purpose: The risk of HIV transmission is greater in those co-infected with another STD due to
increase likelihood HIV shedding in genital secretions. Thus, identifying and treating STD
infection has major public health implication in this population. The purpose of this study is to
assess the prevalence and risk factors of STD infection in a population of HIV-positive patients
being followed by a HIV specialist pharmacist.
Methods: Retrospective chart review of new and returning patients from July 1, 2012 through
July, 13, 2013 at Santa Clara Valley Medical PACE (Partners in AIDS Care and Education)
clinic. All patients encountered are included in the analysis. Primary endpoint is the prevalence
of STD(s) in HIV-positive patients. Secondary endpoint is to identify risk factors associated with
STD infection. STD screening include: hepatitis B (HBV), hepatitis C (HCV), syphilis, herpes
simplex virus (HSV), and gonorrhea (G) and Chlamydia (C) infection. HBV infection is
determined by HBV surface antigen and antibody blood test. HCV infection is determined by
HCV antibody blood test. Syphilis infection is determined by syphilis antibody with reflex to
RPR quant. Herpes infection is determined by HSV 2 type-specific serologic test or symptoms
associated with herpes infection as determined by providers. G/C infection is determined by
nucleic acid amplification tests (NAATs) of oral, anal, and/ or urine sample from the patient.
Patients risk factors were assessed using chart review. Data analysis will be done via STATA
11.0.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-117
Title: Comparison of Medication Therapy Management (MTM) in the United States with
Medication Use Review (MUR) and New Medicine Service (NMS) in the United Kingdom
Primary Author: Nicha Tantipinichwong, University of California, San Francisco, University
of California, San Francisco / California;
Email: nicha.tantipinichwong@ucsf.edu
Additional Author(s):
Graham Davies
Tina Brock
Purpose: As medication experts, pharmacists in the United States and in the United Kingdom
are considered to be underutilized healthcare professionals despite extensive education and
accessibility as front-line medical advisors. Both countries have implemented programs to
enhance pharmacists' contributions to patient care by providing services to optimize drug
therapy. MTM in the United States and MUR/NMS in the United Kingdom are counseling
services developed to provide proper medication use and drug education to help patients
pharmacologically manage chronic medical conditions. The goal of this project is to compare the
infrastructure, goals and objectives, and key outcomes of these programs.
Methods: The project included two phases: review of the literature and structured interviews
with pharmacists. A literature review provided valuable insight into background differences in
the two countries health system, background of MTM and MUR/NMS and their implementation
logistics. MTM and MUR/NMS were evaluated in the contexts of self-care, non-acute care, acute
care, and public health. Objective data on effectiveness outcome in these programs were
expected to be limited and therefore, structured interviews were conducted with three
pharmacists in the United States and eight pharmacists in the United Kingdom providing these
services. Findings from the structured interviews were summarized and key points were
extracted and reported in aggregate.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-118
Title: Interprofessional learning experience: a pharmacy student-led introductory pharmacology
course for physical therapy students
Primary Author: Dan Tran, University of California, San Francisco, School of Pharmacy,
University of California, San Francisco, School of Pharmacy / California;
Email: tina.tran@ucsf.edu
Additional Author(s):
Ryan Beechinor
Marissa Trester
Tina Brock
Purpose: In 2012, the school of pharmacy responded to a need for pharmacology instruction in
the doctor of physical therapy program by creating a course combining traditional lectures
delivered by faculty with case-based discussions led by pharmacy students. Building on this, in
2013, this course was transitioned to a "flipped" model in which fifty percent of the sessions
required students to review a pre-recorded lecture and complete a formative assessment prior to
class, reserving class time for interactive case-based learning. The purpose of this project was to
design, implement, and evaluate a pharmacy student-led "flipped" pharmacology course for
physical therapy students.
Methods: The physical therapy (PT) pharmacology course was sub-divided into twelve sessions
including: four in-class lecture sessions and eight case-based problem-solving sessions. Of the
eight case-based sessions, two followed a traditional lecture format and six used pre-recorded
mini lectures. Each pre-recorded lecture was less than twenty minutes and was created by senior
pharmacy student teaching assistants (TAs). For each, the TAs created lecture objectives,
content, and recorded commentary using the Articulate software. Additionally, the TAs
identified supplemental reading materials and created a five-item formative assessment. Prior to
each in-class case-based session, PT students were asked to watch the mini lecture, complete the
quiz, and read supplemental materials. Course content was delivered via the Moodle-based
learning management system. Technical content was validated by a therapeutic expert and
pedagogy was reviewed by an educator. The pharmacy student TAs were also tasked with
writing the cases and leading the in-class discussions, where students worked collaboratively in
groups of five to six. At the end of the course, an in-class case-based final exam was
administered. Students were allowed to complete the exam with members of their assigned
groups and with open access to drug databases and course content.
Results: A standard post-course evaluation and a supplemental survey were distributed after the
completion of the course. Of the forty one students in the 2013 cohort, ten responded to the postcourse evaluation (24% response rate), and sixteen students responded to the supplemental
survey (39% response rate). In the post-course evaluation which included standardized questions
related to overall course organization and content, 90% strongly agreed that the course discussed
the relationship between pharmacology and physical therapy practice and that small group
discussion activities provided the opportunity for knowledge integration to clinical problems. In
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
the supplemental survey which included specific questions related to the non-traditional
"flipped" classroom, 75% students reported that reviewing basic materials by completing the
mini lecture videos prior to the in-class sessions contributed to their learning experience.
Students unanimously indicated that focusing on actively solving case-based clinical problems,
as opposed to passively listening to lectures, contributed to their learning. All students also
agreed that the peer-to-peer teaching model was a positive experience. With the online formative
assessment, although 69% of students felt that completing the quizzes prior to the in-class
sessions helped them gauge their knowledge on the topics, 31% of students felt undecided or
disagreed.
Conclusion: Evaluation responses validated the initial success of the pharmacy student-led
"flipped" pharmacology course for physical therapy students. The student feedback on the
"flipped" classroom structure warrants further efforts to continue improving the course. The
peer-to-peer teaching model led by pharmacy student TAs was well received by fellow PT
students. Additionally, interactive case-based learning puts an emphasis on the application of
relevant pharmacology knowledge to physical therapy treatments. Most importantly, having
pharmacy students as an integral part of the course increases PT students' awareness of the role
of pharmacists and builds a foundation for future collaborative and interprofessional practice.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-119
Title: Show me the money: tracing the flow of funds in pharmaceutical markets
Primary Author: Tadeh Vartanian, University of Southern California, California;
Email: tadehvar@usc.edu
Additional Author(s):
Neeraj Sood
Purpose: Prescription drug spending has risen rapidly over the last two decades, with
policymakers eager to find ways of lowering spending without jeopardizing patient outcomes. To
do so, an understanding of the flow of prescription drugs, as well as payments, is crucial. Some
players within the distribution channel include manufacturers, wholesalers, retail pharmacies
(which includes community and mail order distribution centers), pharmacy benefit managers,
and ultimately payers (which in itself includes consumers, insurance plans, and the government).
This report seeks to discern the flow of $100 consumer spending to the aforementioned players,
how much does each sector take as profits, and give commentary on their contributions to the
overall system.
Methods: To understand the flow of funds, the author pulls data from 2012 Annual Reports
(AR) under 10K or 20F formats. Companies include 10 manufacturers (Novartis, Merck, Pfizer,
AstraZeneca, Teva, Roche, GlaxoSmithKline, Eli Lilly, Amgen, Abbott), 3 wholesalers
(McKesson, Cardinal Health, AmerisourceBergen), 6 retail pharmacies (CVS Caremark,
Walgreens, Walmart, Rite Aid, Express Scripts, UnitedHealth), and 4 PBMs (Express Scripts,
CVS Caremark, UnitedHealth, Catamaran). Using these reports, the revenue, costs of goods sold
(COGS), and gross profit are calculated for prescription drugs only, while leaving out over-thecounter, health and beauty, animal care, and other items the firm may sell. If a 2012 AR does not
end its reporting on 12/31/2012, then adjustments are made using 2013 AR as well. Next, each
sample is scaled up in accordance to their market share of 49.6% for manufacturers, 85% for
wholesalers, 64.4% for retail pharmacies, and 65% for PBMs, and funds are allocated using the
Congressional Budget Office resource of drug distribution. The consumer spending information
is obtained from the National Health Expenditure Accounts.
Results: All values reported are in millions. Using 2012 AR and proper scaling, manufacturers
have $209,395 revenue, $57,165 COGS, $152,230 gross profit, and 72.7% profit margin.
Wholesalers have $128,295 revenue, $123,402 COGS, $4,893 gross profit, and 3.80% profit
margin. Next, retail pharmacies have $272,219 revenue, $214,288 COGS, $57,931 gross profit,
and 21.3% profit margin. PBMs have $222,109 revenue, $208,640 COGS, $13,468 gross profit,
and 6.10% profit margin. Then, insurers earn $252,397 revenue, $222,109 COGS, $30,288 gross
profit, and 12.0% profit margin. Consumer out-of-pocket (OOP) spending was $49,239, while
other spending equates to $14,340. Ultimately, for every $100 spent by a consumer in the form
of OOP, taxes, and premiums, $9.59 goes to insurance companies, $4.26 to PBMs, $18.34 to
retail pharmacies, $1.54 to wholesalers, and $48.18 to manufactuers. This leaves $18.09 as the
cost of raw pharmaceutical material, with $81.91 going to different healthcare firms.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Manufacturers obtain the largest share, in accordance to their higher gross profit
margins. The retail industry comes next, though it should be noted that mail order pharmacies
only get $0.90 while retailers $17.44. Next, insurers get a larger portion of the funds than PBMs,
presumably due to the former bearing the risk of increased drug spending and patient outliers.
Finally, wholesalers operate efficiently and get only $1.54. The challenges ahead should prompt
policymakers to consider all options when attempting to reduce prescription drug costs and to
use these findings in various reimbursement and taxation legislation.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-120
Title: Survey of current attitudes, prescribing practices, and knowledge of clozapine among
psychiatrists in training
Primary Author: Rosalie Virata, University of Southern California, California;
Email: rvirata@usc.edu
Additional Author(s):
Susie Park
Purpose: Only one in four patients with treatment-resistant schizophrenia are given a clozapine
trial. Despite sound literature supporting the effectiveness of clozapine, this atypical
antipsychotic medication continues to remain an under-prescribed agent. This study aims to
characterize patterns and attitudes of clozapine prescribing among resident psychiatrists and how
prescribing can be encouraged with further education and training. The purpose is to determine
which aspects of the drug are misunderstood or unknown. The results will assist in promoting
increased prescribing of clozapine by psychiatrists so they may become more comfortable and
capable of using clozapine when indicated.
Methods: The institutional review board approved the 33-item questionnaire survey study. A
hard copy was administered to residents in each of the four class levels training at a clinical
county teaching facility. Data was collected between March and August 2013. Each question
reflected one of three major categories: current attitudes, prescribing patterns and knowledge of
clozapine. The survey incorporated topics such as clozapine benefits versus risk, application of
clinical treatment algorithms to actual practice, circumstances for considering a clozapine trial,
beliefs about recommended monitoring parameters, required registration and its impact on
prescribing, number of patients who were prescribed clozapine during residency training,
rationale for remote and recent clozapine prescribing and specific circumstances that may have
prevented a clozapine trial or resulted in clozapine discontinuation for patients, considerations
for re-challenge with clozapine, and familiarity with significant, related clinical studies (i.e.,
CUtLASS 2 and InterSePT). Finally, residents were asked how many hours of supplemental
education are sufficient to improve prescribing comfort, with options of one to six hours, or
more. Data analysis compared survey responses of the residents in the first half of psychiatry
training (first- and second-year residents) to residents who were in their second half of training
(third- and fourth-year residents).
Results: The response rate was 85% (29 completed surveys from a total of 34 psychiatry
residents who were given a survey in person). Sixteen were in their first half of training (Group
1) and 13 in their second half (Group 2). At the time the survey was administered, 31.2 percent
of Group 1 and 84.6 percent of Group 2 (p equals 0.0034) had at least one patient on clozapine.
There are 6.2 percent and 100 percent (p less than 0.001) of Group 1 and 2 residents,
respectively, who are registered with the Clozapine Patient Registry. All respondents believed
that clozapine was an underutilized antipsychotic compared to other available agents. Knowledge
of significant clinical studies was comparable in both groups. Only 37.5 percent of Group 1 and
23.1 percent of Group 2 identified themselves as being familiar with the CUtLass 2 study. Only
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
two of the total sample population were familiar with the InterSePT study; both of these
residents belonged to Group 1. Furthermore, 93.3 percent and 61.5 percent of Group 1 and 2,
respectively, would feel more comfortable prescribing clozapine with at least one additional hour
of supplemental education.
Conclusion: One salient deterrent of clozapine utilization in this study population is the limited
knowledge of resources and major evidence-based literature regarding clozapine and its
usefulness. Despite unanimous beliefs that clozapine is grossly underutilized, very few residents
have prescribed or even recommended it to their treatment-resistant patients with schizophrenia
or schizoaffective disorder. Greater exposure to evidence-based knowledge would allow
residents to recognize benefits despite the hazards and inconveniences of factors like blood
dyscrasias and patient monitoring, respectively. Supplemental education should be considered
early in residency training to better prepare trainees earlier and to further increase the utilization
of this effective treatment.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-121
Title: Screening and educating older adults in the community for medication related problems: a
pilot study
Primary Author: Kanizeh Visram, University of California San Francisco, California;
Email: kanizehfatema.visram@ucsf.edu
Additional Author(s):
Tina Dinh
Shikha Sanjiv
Kamelia Ghazi
Kirby Lee
Purpose: Older adults frequently take multiple medications, including prescription, over-thecounter and dietary supplements, placing them at increased risk for medication-related problems
(MRPs). MRPs include adverse drug events, drug interactions, over/under dose, duplicate or
unnecessary therapy, and issues with adherence. MRPs are common in the geriatric population
resulting in decreased quality of life, hospitalizations, readmissions and death, costing an
estimated $200 billion per year. The purpose of this study was to develop and pilot test a
medication outreach program for older adults living in the community at risk for MRPs.
Methods: The institutional review board approved this cross sectional study. We created a
medication outreach program for men and women aged 65 or older living in the community that
conducted free screenings for MRPs and provided education and tools for medication selfmanagement from Nov 2011 to Nov 2012. Staffed by a volunteer clinical pharmacist and 4
pharmacy students, the program involved partnering and coordinating outreach events with
senior homes, community centers and clinics in the bay area (n=7 sites). A pharmacist conducted
medication reviews and counseling was provided in semi-private, mobile work stations with
laptops, printers and wi-fi to access online drug information resources. Medication histories were
obtained and an updated medication list was created for participants along with a report
describing potential drug interaction risks using a free, online medication monitoring service
available at www.mediguard.org. All participants provided informed consent. Descriptive
statistics were used to evaluate demographics, medication use, MRPs and satisfaction with the
program. Risk factors associated with MRPs were identified using multivariate regression
analysis.
Results: One hundred fourteen older adults participated in the program with an average age of
78 years, mostly female (67%), white (61%), insured (99%), and took on average 9 total
medications. Participants self-reported problems with medication non-adherence (45%) and side
effects (41%). A total of 1,245 drug interactions were identified, averaging 10 per participant.
The top drug classes associated with moderate to severe drug interactions included NSAIDs, beta
blockers, statins, SSRIs, calcium channel blockers and acetaminophen/hydrocodone. Factors
independently associated with high risk drug interactions on adjusted multivariate analyses
included whites compared to ethnic minorities (3.1 drug interactions; 95% CI 0.8-5.4; p=0.009)
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
and taking 9 or more total medications (3.3 drug interactions; 95% CI 1.5-5.0; p=0.001).
Satisfaction with the program was very high.
Conclusion: Our medication outreach program identified a number of MRPs among older adults
living in the community. Participants reported high satisfaction and enthusiasm for the program.
Further research is needed to evaluate the cost-effectiveness of this program.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-122
Title: Standardization of drug shortage management in an oncology hospital
Primary Author: Cedona Watts, University of Southern California, California;
Email: cedonawa@usc.edu
Additional Author(s):
Wyndie Tse
Purpose: A retrospective review of drug shortages was conducted to determine the current
hospital drug shortage practices and to identify opportunities for streamlining drug shortage
management. The goal of the study is to improve the drug shortage process through the
development of a checklist to guide the decision making process.
Methods: Eighty drug shortage email communications to pharmacy staff were analyzed from the
period of June 2012 to August 2013. During the time period 41 different drug shortages were
addressed which were further subdivided into the following 6 categories: parenteral
nutrition/electrolytes, antimicrobials, analgesics, antineoplastic agents, cardiology, and
other/miscellaneous. The cause of the drug shortage was sub-classified by whether it was due to
a concentration change, discontinuation of agent, manufacturer delay, or other reason. Drug
shortage management steps were reviewed (i.e., updating of pre-printed order sets, changing of
pharmacy system entries, re-entering orders for patients, removing stock from automated
dispensing cabinets, etc.). A checklist will be developed to manage drug shortages taking into
consideration the drug shortage management steps identified through review of the shortage
email communications. An algorithm illustrating these steps was developed specifically for
parenteral nutrition, due to the frequent reoccurrence of this shortage within the institution. The
algorithm assessed the origin of the drug shortage, steps involved in finding clinical alternatives,
and effectively communicating with the interdisciplinary health care team.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-123
Title: Effect of enhanced external counterpulsation on exercise performance in a healthy adult
Primary Author: Athena Xides, University of the Pacific, California;
Email: a_xides@u.pacific.edu
Additional Author(s):
Hoan Ngo
Danielle Castillo
Eva Berro
Sachin A. Shah
Purpose: Enhanced external counterpulsation (EECP) is a non-invasive therapeutic intervention
that is Food and Drug Administration (FDA) approved for the treatment of chronic stable and
unstable angina, congestive heart failure, and acute myocardial infarction. EECP exerts its
therapeutic benefits by increasing cardiac output, improving circulation, and stimulating
angiogenesis. Several studies have reported EECPs beneficial effects on exercise tolerance in
patients with coronary artery disease, but its impact on normal, healthy patients has not been well
examined. The purpose of this pilot case is to determine whether EECP therapy can improve
exercise performance in a healthy adult.
Methods: This is a pilot case for the purposes of designing future clinical studies and did not
necessitate IRB approval. This is a before and after evaluation assessing the impact of EECP on
exercise performance. A total of 35 one-hour EECP treatments will be administered over a seven
week period using the FDA approved Vasomedical EECP device. One healthy male volunteer
will perform a standard cardiopulmonary stress test and a 1.5 mile timed run at baseline, at the
fourth week, and at the end of the 35 treatment sessions. The primary endpoints of interest are
VO2 max and the time to complete a 1.5 mile run. Additional endpoints include heart rate, blood
pressure, cardiac output, stroke volume, VCO2, work, anaerobic threshold, VEmax, tidal
volume, respiratory rate, and lipid profile. Baseline exercise, dietary, and sleep patterns will be
monitored to ensure consistency throughout the treatment period. Data will be reported using
descriptive statistics.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-124
Title: Evaluating antimicrobial stewardship principles following implementation of an indication
field in the electronic health record
Primary Author: Nkau Xue Yang, University of California, San Francisco, California;
Email: xuevee.yang@ucsf.edu
Additional Author(s):
Brittney K. Biegel
Michelle L. Yee
Marisa N. Mendez
Purpose: In an effort to minimize antimicrobial resistance and related health care costs, the
California Department of Public Health requires all acute care hospitals to develop practices
aimed at improving the appropriate use of antimicrobials. The purpose of this study is to evaluate
the effect of the electronic health record on length of therapy when providers are required to
select from 14 general indications during antimicrobial order entry. In addition, this study aims
to evaluate how often providers document an indication for use in patients progress notes and
appropriateness of antimicrobial therapy.
Methods: This study will be submitted to the Institutional Review Board for approval. A
retrospective electronic medical record review of antimicrobial orders for all non-pregnant
patients, greater than 18 years of age, receiving systemic antimicrobial therapy will be performed
during two time periods. The pre-implementation period, October 16 November 14, 2012, and
the post-implemetation period, October 16 November 14, 2013, represent a 30-day timeframe
before and after the antimicrobial indication field was introduced into the elecronic health record.
The following data will be collected: patient age, encounter number, medical record number,
pregnancy status, antimicrobial indication(s), antimicrobial(s) ordered, microbiology reports, and
length of therapy. Length of therapy will be compared between the study period before and after
implementing the indication field to the electronic health record. Provider progress notes within
the first 48 hours of antimicrobial order entry will be reviewed to determine if the indication(s)
for antimicrobial therapy were documented. Finally, appropriateness of therapy will be evaluated
based on the indication documented in the progress note, if available, or by the indication
selected upon ordering the antimicrobial.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-125
Title: Evaluation of an intravenous drip reorder process for adult intensive care unit patients at
an academic medical center
Primary Author: Kristen Alspaugh, Georgia Regents Medical Center, GA;
Email: alspaugh@alumni.unc.edu
Additional Author(s):
Trisha Nguyen Branan
Jacquelyn Bryant
Kelley Norris
Purpose: In February 2013, the medical center implemented adult intensive care unit (ICU)
pharmacy drip reorder process guidelines. The purpose of the guideline is to provide guidance
and standardization, to improve nurse satisfaction, to provide a more predictable pharmacy
response, to anticipate patient needs, and to more efficiently utilize pharmacy personnel. This
study will evaluate pharmacy and nursing's adherence to the guideline.
Methods: A retrospective chart review will be conducted on a random sample of 100 adult ICU
orders to assess the use of the institution's adult ICU drip reorder process guidelines. Patients
will include those who were on vasoactive (norepinephrine, epinephrine, phenylephrine,
vasopressin or milrinone) or sedative (dexmedetomidine, or lorazepam) infusions during June
2013. Data to be collected include the medication, volumes dispensed, and order processing
information for the medication. Patient information will be accessed using the hospital's
electronic medical record system. All patient identifiers will be removed and data will be kept
confidential to protect patient privacy. This project is part of the health system Medication Use
Evaluation (MUE) and Improvement program, which has been approved by the institutional
review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-126
Title: Pharmacy practice model initiative: case studies in health-system pharmacy
Primary Author: Quyen Bach, Mercer University School of Pharmacy, Georgia;
Email: quyennbach@gmail.com
Additional Author(s):
Annesha Lovett
Teresa Pounds
Pamela Moye
Purpose: In 2008, the American Society of Health-System Pharmacists and the Research and
Education Foundation introduced the Pharmacy Practice Model Initiative (PPMI). The goal of
this model is to promote pharmacy leaders to better manage their resources to increase focus on
patient-centered and team-based care to improve patient satisfaction and integration across health
care settings. Few studies have been done to assess the implementation of the PPMI across the
United States highlighting the need to provide a comprehensive overview of the implementation
of the PPMI within the United States.
Methods: PubMed and CINAHL were searched for articles from 2008 to 2013. This timeframe
was selected because the PPMI became officially recognized in 2008. The studies that were
chosen also focused on roles other than the pharmacists role (the role of pharmacy technicians).
Keywords used in the search strategy were "pharmacy practice model," "models,"
"organizational," then narrowed down by using the MeSH term, "organizational, model." The
reference list of each entry was then searched for additional articles. Each entry was evaluated
against the following exclusion criteria using a step-wise approach; 1) the entry did not assess
the implementation of the PPMI, 2) the entry was conducted outside the United States, 3) the
entry was not a case study. It was necessary to highlight case studies as other items (interviews,
newsletters, summit highlights, and letters) were not comprehensive with regard to a description
of the implementation process. The outcomes from each included study were tabulated and
categorized by location/design, resources, intervention, and findings/implications.
Results: Of the fifty-nine findings from the literature search (case studies, articles, summit
highlights, special features, notes of reflection), two case studies met the inclusion criteria. The
first case study involved University of Minnesota Medical Center, a multi-campus academic
medical center with 300 patients. This facility used technology such as pagers for decentralized
technicians, computerized provider order entry, and wireless computers on wheels for
decentralized pharmacists. Key personnel included pharmacy technicians, clinical specialists,
decentralized pharmacists, staff pharmacists, buyers, and managers. A new role was created for
the technicians to round the floors for drug distribution issues. The implementation teams
worked together on clinical and distributive functions which allowed for consistency in patient
care, expanding pharmacy hours and services, and improved employee satisfaction. The second
case study involved Providence Health & Services, a multihospital system with locations in
Washington State and Montana. These facilities used technology such as automated dispensing
cabinets, order-image scanners, and automated telephone trees to route calls to technicians. The
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
pharmacy directors and hospital administrators over pharmacy introduced the initiative to staff.
Training in therapeutic monitoring and documentation was an ongoing process. The outcome
was a positive clinical and economic impact with a return on investment of $709,321.
Conclusion: Although the goal was to provide a comprehensive overview of the implementation
of PPMI in the United States, only three states were found to have published a formal case study.
Nevertheless, these two case studies provided useful insights and have highlighted significant
benefits from the transition. An important finding from this review is the lack of research
assessing the implementation of the PPMI. Based on the positive findings of these two case
studies, it is evident that further research is warranted.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-127
Title: Evaluation of vancomycin use and the incidence of red man syndrome in a childrens
hospital
Primary Author: Brittany Bennett, University of Georgia College of Pharmacy, Georgia;
Email: brittj@uga.edu
Additional Author(s):
Meredith A Beker
Cady Ploessl
Purpose: Vancomycin is an antibiotic known for its use against methicillin-resistant
staphylococcus aureus. Vancomycin is also known to cause the hypersensitivity reaction red man
syndrome (RMS). Current recommendations state that a maximum infusion rate of 10mg/minute
or one gram over one hour should be used in adult patients. Currently, there is a lack of data for
the prevalence or management of RMS in pediatric patients. The goal is to evaluate the
relationship between vancomycin dose, infusion time, and the incidence of RMS with the hope
of preventing future incidences of RMS in the pediatric population and therefore improving
patient outcomes.
Methods: This project is part of the health system Medication Use Evaluation (MUE) and
Improvement program, which has been approved by the institutional review board. A
retrospective chart review of 168 patients will be conducted to evaluate the use of vancomycin in
a pediatric setting, the incidence of RMS, and to document preventative action taken for RMS.
Data to be collected includes incidence of RMS in a six month period, initial vancomycin dose,
initial infusion time ordered, changes in infusion time after RMS occurrence, presence of
treatment with diphenhydramine, previous documented history of RMS, and patient
demographics (age, gender, race).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-128
Title: Glucose disturbances and atypical antipsychotic use in the intensive care unit
Primary Author: Amy Bishara, University of Georgia College of Pharmacy, Georgia;
Email: acbishara@gmail.com
Additional Author(s):
Saranya Venkatachalam
Stephanie V. Phan
Tze-Chun V. Liao
Purpose: In the intensive care unit (ICU), atypical antipsychotics are initiated in the treatment of
delirium due to a lower incidence of extrapyramidal symptoms and potentially fewer adverse
effects compared to haloperidol. Hyperglycemia from any cause is associated with increased
mortality and morbidity, and case reports have shown that glucose dysregulation can occur
within days of atypical antipsychotic initiation. The objective of this study is to identify the
incidence of hyperglycemia (defined as a glucose level of greater than 180mg/dL) in patients
taking an atypical antipsychotic medication in the ICU.
Methods: The institutional review board approved this case-controlled, retrospective,
observational chart review. Patients at least 18 years of age prescribed an antipsychotic in the
ICU will be identified. Exclusion criteria include patients initiated on conventional
antipsychotics, patients receiving antipsychotics as needed, and patients receiving antipsychotics
prior to ICU admission. Demographic data will include: patient age, gender, ethnicity, ICU type,
ICU admission indication, APACHE II score, steroid use, use of total parenteral or enteral
nutrition, and the presence of baseline disease states involving glucose abnormalities. All data
will be recorded without patient identifiers and maintained confidentially. The primary outcome
measure will be the incidence of at least one hyperglycemic episode during a patient's stay in the
ICU after initiation of the atypical antipsychotic. Descriptive statistics will be used to identify the
prevalence of hyperglycemia, and to compare patients who experienced multiple episodes of
hyperglycemia with patients who experienced one episode or less. Additional outcome measures
include number of patients discharged from the ICU on an atypical antipsychotic, types of
atypical antipsychotics used, number of patients receiving a benzodiazepine during ICU
admission, and the average daily dose of benzodiazepines used. A regression model will be used
to identify the impact of potential confounders.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-129
Title: Assessing community-associated extended-spectrum beta-lactamase infections in a tertiary
care facility
Primary Author: Whitney Blan, Mercer University College of Pharmacy, Georgia;
Email: wlblan@valdosta.edu
Additional Author(s):
Deanne Tabb
Purpose: Since the mid-2000s, a new trend of community-associated extended-spectrum betalactamase (ESBL) infections have emerged. These types of infections can cause a challenge to
the management of community-associated infections as the empiric drug selection typically does
not include coverage for ESBLs. The primary objective of this study is to review cases of ESBL
infections to determine if community-associated ESBL infections are a concern in the local area.
Methods: This study will be submitted to the Institutional Review Board for approval. A 12
month retrospective report of ESBL organisms will be generated from the institutions MicroScan
WalkAway system registered by Seimens Healthcare Diagnostics. Patient data to be collected
includes age, gender, allergies, reason for admission, and healthcare-associated risk factors.
Antibiotic specific data to be generated includes microbiology in vitro susceptibilities, type of
infection, diagnosis, empiric antimicrobial therapy, target antimicrobial therapy, duration of
therapy, clinical outcomes, and length of stay. All data will be recorded without patient
identifiers and maintained confidentially. If present, healthcare-associated risk factors will be
recorded and reviewed to determine the percentage of healthcare-associated EBSLs present over
the past 12 months.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-130
Title: Evaluation of corticosteroid use in the intensive care unit for chronic obstructive
pulmonary disease (COPD) exacerbations
Primary Author: Kimberly Boyle, Mercer University, Georgia;
Email: kimberly.boyle@live.mercer.edu
Additional Author(s):
Stacey Folse
Micah Fisher
Purpose: The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines
recommend the use of corticosteroids in COPD exacerbations in addition to inhaled beta-2
agonist therapy. This recommendation of 30-40mg of oral prednisolone per day for 10-14 days is
weak due to lack of consistent data on the optimal route, dose, and duration of therapy. Even less
data exists for critically ill patients. This creates wide variability in prescribing patterns, which
are not fully supported by evidence-based practice. The objective of this study is to characterize
systemic corticosteroid use during acute COPD exacerbations in intensive care unit (ICU)
patients.
Methods: This is a single-center, retrospective cohort study which has been submitted to the
Emory institutional review board for approval. The electronic medical record will be used to
collect data for patients over 40 years old admitted to ICUs at Emory University Hospital and
Emory University Hospital Midtown from January 1, 2008 to December 31, 2012 with a
diagnosis of acute COPD exacerbation. Other inclusion criteria include history of cigarette
smoking and administration of scheduled inhaled short acting beta-2 agonist therapy. Patients
excluded include those who have a prior history of asthma, evidence of pneumonia, or allergy to
corticosteroids. The primary objective of this study is to characterize corticosteroid use during
acute COPD exacerbations in ICU patients in terms of formulation, dose, and agent used.
Secondary outcomes include identifying adverse events associated with corticosteroid use,
describing the duration of corticosteroid therapy, and characterizing the length of ICU stay,
duration of mechanical ventilation, and all-cause in-hospital mortality. Data will be collected on
age, sex, race, past medical history, recent corticosteroid use, FEV1 and FEV1/FVC. The
medication administration record will be reviewed to determine type of corticosteroid agent
used, route of administration, daily dose given, and duration of therapy.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-131
Title: Rapid response team access to intravenous push medications and outcomes at an academic
medical center
Primary Author: Lauren Buchbinder, University of Georgia College of Pharmacy, Georgia;
Email: buchbinderl@mail.rx.uga.edu
Additional Author(s):
Heather R. Harrell
Timothy R. Robinson
Purpose: The Joint Commission National Patient Safety Goal 16 recommended having a system
in place to proactively assess a patient and quickly provide assistance if imminent decline was
expected. However, recent studies question efficacy of rapid response systems. By evaluating
intravenous (IV) push medication (hydralazine, labetalol, and metoprolol) availability in
different locations during rapid response team (RRT) calls and subsequent timeliness of
administration, association to patient rescue without transfer to an increased level of care will be
assessed.
Methods: A retrospective evaluation will be conducted for all 121 RRT calls that involved use
of an IV push medication (hydralazine, labetalol, and metoprolol) during a 12-month period from
August 1, 2012 to July 31, 2013. Adult patients in locations where IV push medications were
available in the dispensing cabinet will be compared to patients where IV push medications had
to be obtained from the main pharmacy. Data collected will include demographics, reason for
admission, patient location and medical service, IV medication used and dispensing location,
vital signs relative to the specified medication during the RRT call, initiator of the RRT call, and
comparisons of the time intervals between when the RRT call was placed and arrival time, RRT
call and medication order, RRT call and medication administration, as well as the medication
order and administration time noted. Finally, additional actions other than medication
administration will be noted. The patient outcome to be assessed is whether the patient was
stabilized and remained on the floor verses transferred for escalation of care. This project is part
of the health system Medication Use Evaluation (MUE) and Improvement program, which has
been approved by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-132
Title: Evaluation of the adverse effects of codeine postoperatively in pediatric patients
Primary Author: Samantha Burke, University of Georgia College of Pharmacy, Georgia;
Email: burkes@rx.uga.edu
Additional Author(s):
Kelley Norris
Purpose: Serious adverse effects including unusual sleepiness, confusion, difficult or noisy
breathing and death have been associated with codeine use postoperatively to
tonsillectomy/adenoidectomy in pediatric patients. In February of 2013, the Food and Drug
Administration published a safety review update highlighting a new, boxed warning and
contraindication for this population. The purpose of this study is to evaluate the adverse effects
of codeine in all postoperative pediatric patients at this institution.
Methods: A retrospective chart review will be conducted on all patients less than 18 years of age
who received codeine or an acetaminophen/codeine combination product postoperatively from
February 2012 to February 2013. Data collection will include demographics (age, weight,
gender, race), prescribing service, diagnosis, allergies, procedure type, medication used (dose,
total daily dose, frequency and number of doses required), duration of therapy and additional
pain medications. Adverse effects will be evaluated by collecting the pre and post codeine use
vital signs, and adverse reaction documentation. Additionally, we will confirm that codeine or
acetaminophen/codeine combination products have not been ordered or administered to pediatric
patients since the publication of the latest FDA Drug Safety Communication in February 2013.
All patient identifiers will be removed and no protected health information will be transmitted
electronically in order to protect patient privacy. This project is part of the health system
Medication Use Evaluation (MUE) and Improvement program, which has been approved by the
institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-133
Title: Implementation of a pharmacist/physician collaborative practice pilot program to improve
care for patients with community-acquired pneumonia and chronic obstructive pulmonary
disease acute exacerbations
Primary Author: Mary Carpenter, South University School of Pharmacy, Georgia;
Email: mhannahcarpenter@gmail.com
Additional Author(s):
Bruce M. Jones
David Cretella
Gifford Lorenz
Joseph Crosby
Purpose: Community-acquired pneumonia (CAP) and chronic obstructive pulmonary disease
(COPD) acute exacerbations are common diagnoses that require hospital admission as well as
utilize a considerable amount of healthcare resources. Multiple efforts have been implemented to
reduce length of stay and cost per admission for patients with these diagnoses; however, this
institution lacks formal meetings between physicians and pharmacists to discuss medication
therapy plans. Pharmacists are familiar with up to date evidence based medicine, which makes
them an important resource for physicians making medication therapy decisions for patients. We
hypothesize that implementation of a pharmacist/physician collaborative practice program will
improve patient outcomes.
Methods: This is a prospective study that will be conducted with an open enrollment between
October 2013 and March 2014 until significant power is achieved. The pharmacist/physician
collaborative practice program will pilot with a pulmonologist, and patients under his care. A
retrospective chart review from October 2012 to March 2013 for the same pulmonologist will
serve as the control. Male and female patients greater than eighteen years of age admitted on a
medical/surgical floor with an admission for COPD or CAP will be included in the study.
Patients identified as having hospital-acquired or healthcare associated pneumonia and patients
with initial admissions to an intensive care unit or non-medical/surgical floor will be excluded.
The study pharmacist will review patients meeting inclusion criteria daily and discuss the
patients therapeutic plan (treatment length, antimicrobial selection, IV to PO conversion,
coordination of care, barriers to discharge) and therapeutic recommendations to implement in a
way that is consistent with current clinical pharmacy practice. Coordination with other healthcare
professionals will be done as needed. Length of stay is the primary outcome. Secondary
outcomes include cost data, days of antimicrobial therapy (IV/PO), and 30-day readmission rate.
This study will begin after the submitted IRB approval has been granted.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-134
Title: Evaluation of organism directed treatment of osteomyelitis within an urban safety net
hospital
Primary Author: Lindsey Carter, Mercer University College of Pharmacy, Georgia;
Email: lindsey.l.carter@live.mercer.edu
Additional Author(s):
Michael D. Knauss
Jordan Wong
Purpose: Management of osteomyelitis varies due to the lack of consensus treatment guidelines.
Principles of antimicrobial stewardship promote the need for pathogen directed therapy to avoid
unnecessary use of broad-spectrum antimicrobials. A bone biopsy is the ideal culture to identify
the causative organism(s), while deep exudate or tissue cultures may offer some guidance for
antimicrobial therapy. The objective of this study is to quantify the number of patients that
received organism directed therapy for osteomyelitis based on results of a bone biopsy and/or
deep exudate/wound culture.
Methods: This study was approved by the Institutional Review Board. Patients with a diagnosis
of osteomyelitis will be identified using ICD-9 codes. The first 100 unique patients will be
selected for review. Patients are included only for their first encounter between January 1, 2012
and April 1, 2013. Patients are excluded if they are less than 18 years of age, pregnant, or
incarcerated. The electronic medical record will be reviewed to collect the following data:
method of diagnosis, cause and location of osteomyelitis, identified microorganism(s), choice of
antibiotic, length of treatment, non-pharmacologic treatments, and readmission within 60 days of
treatment. The primary outcome is the percentage of patients receiving organism directed
therapy. Secondary outcomes include the percentage of patients diagnosed with radiologic and/or
clinical methods, the percentage of patients treated with MRSA, pseudomonas, or anaerobe
therapy (alone or in combination), the percentage of patients readmitted for osteomyelitis within
60 days, and the percentage of patients that received treatment for a minimum of four weeks.
Descriptive statistics will be used to analyze the data.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-135
Title: Drug utilization evaluation of doripenem use within a health system
Primary Author: Jessica Chen, University of Georgia, University of Georgia/Georgia;
Email: chenchen5121@gmail.com
Additional Author(s):
Charles Durham
NaaDede Badger-Plange
Todd Parker
Purpose: Carbapenems are antibiotics that cover gram positive, gram negative, as well as
anaerobic bacteria. Doripenem, the newest carbapenem, is recommended by the Infectious
Disease Society of America (IDSA), for use in hospital acquired intra-abdominal and
complicated urinary tract infections. In 2012 a trial involving doripenem was halted after
preliminary results demonstrated increased mortality in doripenem patients compared to
imipenem. In addition, doripenem has non-inferiority parallel indications and higher cost than
meropenem and imipenem. The purpose of this study is to assess doripenem use and substantiate
conversion from doripenem to meropenem as the preferred carbapenem within the health system.
Methods: This study is a retrospective medication use evaluation of all patients who received
doripenem between Feburary 2013 and August 2013. It was approved by the Pharmacy &
Therapeutics (P&T) committee of the health system. A computer-generated list was used to
capture the patient population. Data to be analyzed include patient demographics, indication of
use, culture and sensitivity, doses, concurrent antibiotics, duration of therapy, and major adverse
events. All data will be collected and recorded without patient identifiers to ensure
confidentiality. The primary outcome is to measure appropriateness of use, based on indication
and duration of treatment as defined by standard guidelines. Secondary outcomes include length
of stay, clinical cure, in hospital mortality and adverse drug reactions. Clinical cure is defined as
complete resolution of signs and symptoms of infection.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-136
Title: Prevention of Cisplatin-induced Nephrotoxicity with Hydration Plus Mannitol vs.
Hydration Alone
Primary Author: Linda Cheng, Mercer University, Georgia;
Email: linda.cheng@live.mercer.edu
Additional Author(s):
Trevor McKibbin
Amy Grimsley
Purpose: Cisplatin is a platinum-based alkylating agent used in chemotherapy regimens to treat
many types of solid tumors and lymphomas. Nephrotoxicity is the dose-limiting side effect of
cisplatin occuring in approximately 28-36% of patients. If nephrotoxicity is experienced it is
recommended to hold cisplatin therapy until normal renal function is regained. Delaying
cisplatin therapy may lead to suboptimal outcomes for patients. Hydration with IV fluids alone
or with a diuretic such as mannitol is often used to prevent nephrotoxicity, however based on
current literature, it is unclear whether the addition of mannitol with IV hydration provides
optimal renal protective effects.
Methods: This is a single-center retrospective cohort study which will analyze and compare the
renal protective effects of IV hydration with mannitol to IV hydration alone in patients receiving
cisplatin 100 mg/m2 combined with radiation for squamous cell cancer of the head and neck.
Inclusion criteria include patients who were treated at the Winship Cancer Institute of Emory
University who were treated with cisplatin therapy between 1/1/2008 and 3/1/2013, baseline
calculated creatinine clearance &#8805; 70 ml/min and age &#8805;18 years. Patients were
identified from Emory University Hospital's medical records database. Sample size is estimated
to be 140. The primary outcome is to determine if the use of mannitol with hydration is
associated with less nephrotoxicity than hydration alone. Secondary outcomes include comparing
the number of patients who failed to complete all planned cycles of cisplatin due to
nephrotoxicity, comparing the rate of decline of creatinine clearance, and comparing the total
number of patients whose serum creatinine returned to baseline after completion of therapy.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-137
Title: Contribution of Atypical Psychotics to Hepatic Steatosis & Choledocholithiasis
Primary Author: Shahrouz Dehgahi, Philadelphia College of Osteopathic Medicine School of
Pharmacy, Georgia;
Email: shahrouzde@pcom.edu
Additional Author(s):
Shari N. Allen
Case Report: A 60 year old female (height, 160 cm; weight, 78.8kg) was admitted to the
emergency room with a chief complaint of epigastric pain radiating to the right upper quadrant,
nausea, and vomiting that has been occurring for approximately one week. Previous to this
current ER visit the patient has been trying to alleviate her pain by taking approximately 35
Lortab (7.5mg/500mg) (hydrocodone/acetaminophen) and Percocet (5mg/325mg)
(oxycodone/acetaminophen) tablets over a four day span. The patients nausea has not been
alleviated by Phenergan (promethazine) 25 mg suppositories. The patients past medical and
social history revealed a history of depression, anxiety, type 2 diabetes mellitus, hyperlipidemia,
hysterectomy, appendectomy, cholecystectomy, shoulder surgery, arthritis, and a urinary tract
infection. She had no reported history of alcohol, or illicit drug use which was confirmed by a
negative urine toxicology screen. The patient smokes 1 pack of cigarettes per day. Her complete
metabolic panel and complete blood count revealed elevated liver enzymes; AST 262 U/L
(Reference Range 0-48) and ALT 362 U/L (Reference Range 12-78), elevated total bilirubin 2.6
mg/DL (Reference Range 0-1), elevated blood glucose 185 mg/DL (Reference Range 65-99).
The patient is also obese 78.8kg (BMI 30.7) and has high blood pressure 167/82 mmHg
(Reference range 140/80). The patients current home medications include metformin 1000 mg
twice a day, clonazepam 1 mg twice a day as needed, hydrocodone-acetaminophen 10-325mg
every 6 hours as needed, pravastatin 20 mg once a day at bedtime, omeprazole OTC 20 mg once
a day, nitrofurantoin 100 mg two times a day for 5 days, promethazine 25 mg every 4 hours as
needed, and quetiapine 200 mg twice a day. The patient underwent an endoscopic retrograde
cholangiopancreatography (ERCP), which showed choledocholithiasis with extraction of a large
pigmented bile duct stone. The charge nurse inquired a drug information question in regards of
the patients medication, quetiapine; whether quetiapine could cause hepatic steatosis. Published
literature suggests that atypical antipsychotics, such as Seroquel (Quetiapine), are associated
with various metabolic side effects. Dyslipidemia, hyperglycemia, diabetic ketoacidosis, and
weight gain have all been reported in patients taking quetiapine regularly. Published literature
also strongly suggests a close correlation between metabolic syndrome with gallstone formation
and hepatic steatosis. The quetiapine 200 mg twice daily was continued in this patient secondary
to stability of her psychiatric disorders, however it was noted that this may secondarily be
contributing to her chief complaint of epigastric pain. Although many factors particular to this
patient may play a role in the cause of hepatic steatosis and choledocholithiasis ,we could
correlate the long term use of quetiapine as one of those factors. This case report highlights
additional factors that may contribute to metabolic disturbances (i.e. hepatic steatosis) such as
medications, but particularly medications that may be overlooked in medical practice such as a
the atypical antipsychotics.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-138
Title: Assessment of warfarin education documentation in an academic medical center
Primary Author: To-My Dinh, University of Georgia College of Pharmacy, Georgia Regents
Medical Center;
Email: tdinh1990@gmail.com
Additional Author(s):
Thomas Flynt
Purpose: Anticoagulants, such as warfarin, are considered to be high-risk medications due to the
complexity of proper dosing, monitoring, adverse drug events, and patient compliance. National
core measures have been implemented to ensure that patients are adequately educated on proper
use of such medications upon discharge from the medical facility. The objective of this
medication use evaluation is to assess the completeness, quality, and core measure compliance of
warfarin counseling documentation in patients' electronic health records. We also want to
identify gaps in care that can be improved upon.
Methods: A retrospective analysis was conducted of patients discharged from the hospital on
warfarin therapy from August 2013-September 2013. A total of 172 patients were found to be on
warfarin therapy during this time period in which at least 50 patients were randomly chosen for
the study. Assessment of whether warfarin education was documented will be done through
information obtained from the hospital's electronic health records. An evaluation of these records
will be completed to ensure four main points were addressed during the patient education,
including compliance issues, dietary advice, follow-up monitoring, and potential for adverse
drug reactions and interactions. We will also gather data related to how many patients declined
consultation, a reason for decline and whether alternative education was offered. Documentation
that warfarin and dietary discharge instructions were given to the patient or their family member
will also be assessed. This project is part of the health system Medication Use Evaluation (MUE)
and Improvement program, which has been approved by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-139
Title: Pharmacoeconomic impact of tirofiban versus eptifibatide in percutaneous coronary
intervention with novel dosing modality.
Primary Author: Charles Durham, Univeristy of Georgia College of Pharmacy, Georgia;
Email: cwdurha@uga.edu
Additional Author(s):
Jessica Chen
Sarah Murphy
Purpose: For several years, the American Heart Association and American College of Chest
Physicians assigned eptifibatide a level IIa recommendation for use in ST elevation myocardial
infarction patients and a Class I for use in unstable angina/non-ST elevation myocardial
infarction patients. Recently these guidelines have been updated to give tirofiban an equal level
of evidence supporting its use, though with a new dosing modality. Additionally, tirofiban offers
other benefits including single package size and expanded use in patients with renal impairment.
Considering these factors, a financial comparison was performed on actual use of eptifibatide
versus theoretical use of tirofiban.
Methods: The Pharmacy & Therapeutics committee approved this retrospective study of all
patients who received eptifibatide for percutaneous coronary intervention between January and
April 2013. A computer-generated list was used to identify patients receiving the target drug
during the study period. Data obtained includes: patient weight, sex, age, creatinine level, bolus
dose, infusion dose, infusion time, and the number of vials used. All data was recorded and
analyzed without patient identifiers to ensure confidentiality. This information was used to
generate an equivalent regimen of tirofiban based on the AHA/ACCP recommendations. If a
patient received an eptifibatide bolus, a 25 mcg/kg tirofiban bolus dose was calculated. If a
patient received an eptifibatide infusion, a 0.15 mcg/kg/min tirofiban infusion dose was
calculated for the same dosing interval. Adjustments were made for patients with creatinine
clearance less than 50 mL/min. This theoretical tirofiban regimen was then converted to a
discrete number of 500 mL vials. These virtual costs were aggregated and compared to the cost
of actual eptifibatide vials used. The primary outcome is to determine the cost difference
between a tirofiban and eptifibatide regimen in patients undergoing PCI. A secondary outcome is
inventory impact expressed as number of vials used.
Results: Twenty-eight patients were included in the analysis. Potential cost savings over the
four-month period would have been $7164.58, or 24%. Twenty-five patients had to receive both
bolus and infusion doses of eptifibatide; all of these patients would be eligible for conversion to a
single dosage form of tirofiban. Twenty-five procedures would have required a reduced number
of tirofiban vials. Three would have needed additional medication compared to eptifibatide. One
hundred six vials of eptifibatide were used during the study period, while only 47 would be used
if the patients were on a tirofiban regimen, a reduction of 55.7%.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The cost of a typical regimen of tirofiban is lower than that of eptifibatide.
Considering both drugs have equal standing in evidence supporting their use, tirofiban may be
considered as a cost-effective alternative to eptifibatide in patients undergoing percutaneous
coronary intervention. The small sample size does limit the applicability of these results.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-140
Title: Does pharmacist monitoring of anti-Xa levels in high-risk patients receiving enoxaparin
improve therapeutic goals?
Primary Author: Susanne Emerich, Mercer University College of Pharmacy, Georgia;
Email: susanne.pribeagu@live.mercer.edu
Additional Author(s):
Christopher Paciullo
Kathy Yaughn
Annie Winkler
Purpose: Despite extensive usage, anticoagulants result in high rates of adverse events.
Pharmacist monitoring of anticoagulation has been shown to improve patient outcomes when
compared to usual medical care. Strong evidence showing the benefit of pharmacist-managed
anticoagulation therapy with LMWHs is lacking. More recently, enoxaparin has been shown to
be just as unsafe and unpredictable in therapeutic response as unfractionated heparin with many
patients falling out of therapeutic range after initial dosing. The purpose of this study is to
determine the effect of pharmacist monitoring of anti-Xa levels and management of enoxaparin
therapy in high-risk inpatients.
Methods: The Emory and Mercer University investigational review boards approved this
retrospective chart review study of medical, non-critically ill adult patients admitted to Emory
University Hospital. Inclusion criteria are as follows: treatment with enoxaparin and high risk
status (age &#8805; 70, weight &#8805; 100 kg, or creatinine clearance &#8804; 50 ml/min).
Patients will be identified from enoxaparin monitoring forms used by pharmacists to monitor
anti-Xa levels in high-risk patients. Any pregnant, critically ill, s/p device implant, left
ventricular assist device (LVAD), and patients with a change in serum creatinine (SCr) of 50%
or greater from baseline will be excluded. The sample size will be approximately 200 patients.
The following data will be collected: age, gender, weight, SCr, indication for enoxaparin,
enoxaparin doses administered, anti-Xa levels, dosing changes made by pharmacists including
number of changes made to meet therapeutic goals, concurrent pertinent medications, comorbid
conditions, and adverse events (bleeding, recurrent thrombosis, thrombocytopenia, length of
hospital stay, and hospital mortality). The primary outcome is to determine whether there is a
significant difference in the number of high-risk patients initially therapeutic with a standard
dose of enoxaparin as compared to those brought to therapeutic range after pharmacist
monitoring and dose adjustment.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-141
Title: Assessment of appropriate parameters and instructions for inpatients receiving an as
needed blood pressure medication at an academic medical center
Primary Author: Michelle Eun, Georgia Regents Medical Center, Georgia;
Email: eunm@rx.uga.edu
Additional Author(s):
Christina E. DeRemer
Purpose: The Joint Commission requires institutions to have clear instructions or parameters for
the interpretation of administration, especially when multiple as needed medications are used for
the same indication.The JNC-7 guidelines do not establish a consensus for treating high blood
pressure while inpatient unless it is a hypertensive emergency or urgency. The purpose of this
study is to evaluate current practice for the use of as needed blood pressure medications and
assess the instructions and parameters provided.
Methods: A retrospective chart review will be conducted on all inpatients at the academic
medical center who received an as needed blood pressure medication (hydralazine, clonidine,
and labetalol) for the treatment of high blood pressure from April 2013 to June 2013. Data
collection will include the name and quantity of intravenous or oral as needed blood pressure
medication(s), quantity of scheduled blood pressure medication(s), frequency of as needed blood
pressure medication use, presence of instructions and blood pressure parameters, and the location
of the patient. The presence of clear instructions and parameters for nurses will also be assessed.
Efficacy parameters will be determined by collecting average systolic and diastolic blood
pressures. All patient identifiers will be removed and data will be kept confidential to protect
patient privacy. This project is part of the health system Medication Use Evaluation (MUE) and
Improvement program, which has been approved by the institutional review board.
Results: Preliminary results: There were approximately 309 patients received an as needed order
for one of the above listed blood pressure medications. Approximately 73 percent was as needed
hydralazine with the majority being oral for as needed blood pressure management.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-142
Title: Evaluation of glycemic control in patients with type 2 diabetes transitioned from basal
insulin therapy to premixed insulin therapy in an uninsured, indigent outpatient clinic
Primary Author: Victoria Finch, Mercer University College of Pharmacy, Georgia;
Email: victoria.finch@live.mercer.edu
Additional Author(s):
Ryan Crossman
Purpose: The American Diabetes Association recommends initiation of insulin with basal
insulin followed by basal-bolus insulin if glycemic control is not achieved, as opposed to adding
premixed insulin. Clinical trials comparing basal-bolus to premixed insulin have shown basalbolus therapy has a greater reduction in A1c level. Despite this potential benefit, issues such as
numerous daily doses and carrying and storing insulin equipment can lead to poor adherence,
and thus compromise treatment. The objective of this study is to determine if patients with Type
2 diabetes can achieve better glycemic control with premixed insulin versus basal/bolus insulin
in an indigent, outpatient clinic.
Methods: This study will be submitted to the Institutional Review Board for approval. A
retrospective review of the electronic medical record system will identify patients with Type 2
diabetes transitioned from basal/bolus insulin to premixed insulin. The following data will be
collected: patient age, gender, race, prescription fill dates, and A1c levels at baseline and at three,
six, nine, and twelve months prior to review. Upon data collection, patient identifiers will be
replaced with a random study identifier. The participant code list linking the patients identifying
data with the random study identifier will be stored on a password protected electronic file
accessible only by the investigators involved in data collection. Patients A1c levels will be
reviewed by a clinical pharmacist to determine if there was a decrease from baseline, and if the
A1c level prior to review is at goal. Fill dates of the premixed insulin will also be reviewed to
help determine patient compliance. Data from all patients transitioned from basal/bolus insulin to
premixed insulin will be included in the results. If a patients A1c level is only available three
months post transition, this data will be included in the results. A1c reduction will be stratified
by months post transition.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-143
Title: Pharmacists play a vital role while serving on interdisciplinary medical mission team in
Honduras.
Primary Author: Kayla Flowers, Mercer University College of Pharmacy, Georgia;
Email: kayla.hayes@live.mercer.edu
Additional Author(s):
Purpose: Honduras is one of the poorest countries in the western hemisphere. As a result, many
Hondurans do not have reliable access to health care due to decreased stock, medication outages,
lack of health care professionals, road conditions and many other issues. The Honduran
government relies heavily on non-governmental organizations to provide health care to its rural
inhabitants. This trip was developed to provide health care to underserved villages in the
Department of Olancho located in the Agalta Valley of Central Honduras as well as allow
students from different medical backgrounds to work together in an interdisciplinary team.
Methods: The medical team consisted of 2 pharmacy students, 4 medical students, 1 nurse
practitioner student, 2 nursing students, 2 undergraduate students, 1 clinic administrative staff
member, and 4 faculty members from the listed disciplines; all team members were affiliated
with Mercer University. The team provided 8 days of primary care clinics during the mission
trip. Primary care clinics were set up in small nurse clinics, open air schoolrooms, and outdoor
pavilions. Prior to departure, the pharmacy team reviewed the formulary, ensured appropriate
medications had been ordered in country, and participated in a packing day to ensure all over the
counter medications were properly packed for transport. In country, the pharmacy team
conducted an overall inventory and kept a perpetual inventory throughout the time in country.
The pharmacy team organized, supervised and aided in the counting and daily packaging of
medications. In addition, a pharmacy student ran the pharmacy, with supervision from the
pharmacy faculty, providing direction and assistance to other students rotating through the
pharmacy. The pharmacy team was involved throughout the entire process providing an integral
role in patient intake, triage at provider stations, patient counseling, dispensing medications, and
assessing patients for reading glasses.
Results: During the 8 clinic days a total of 1132 hours of service were provided; 220 of the
service hours were provided by the pharmacy team. A total of 764 patients were seen and 2,227
prescriptions were dispensed. The pharmacy team assisted in providing blood pressure
screenings, glucose screenings, and taking weight and temperatures. Pharmacy students also
worked alongside medical students to provide triage, aid in choosing the correct medication,
providing drug information, and teaching medical, nursing, and undergraduate students how to
dose medications by weight and indication. Recommendations were made to medical students
and physicians about wrong drug, wrong dose, or drug substitutions. Keeping a perpetual
inventory allowed the pharmacy team to keep everyone informed of medication shortages and
outages.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The pharmacy team contributed to the interdisciplinary team by informing
members of the medication inventory to allow for proper substitutions, providing drug consults,
dispensing medication, and teaching other students about the practice of pharmacy. Clinical and
patient assessment skill training allowed the pharmacy team to add value in areas outside of the
pharmacy. Utilization of the pharmacy team allowed patients to receive well-rounded health
care.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-144
Title: Evaluating the use of intravenous magnesium sulfate in electrolyte imbalance in an
academic medical center
Primary Author: Sheryle Gillette, University of Georgia College of Pharmacy, Georgia;
Email: gillettes@rx.uga.edu
Additional Author(s):
Tana Bagby
Purpose: Magnesium disorders can be multifactorial and can be related to renal function, disease
state and medication therapy. Magnesium in parenteral administration is typically provided as
magnesium sulfate. One gram of magnesium sulfate is equal to 8.12 mEq of elemental
magnesium. Hypomagnesaemia requiring treatment is when magnesium levels fall below 1.5
mg/dL (1.25 mEq/L). The objective of this retrospective medication use evaluation is to assess
the adherence of prescribers to medical staff-approved, evidence-based intravenous magnesium
sulfate guidelines in electrolyte imbalance.
Methods: A retrospective review of the electronic medical records of patients receiving
intravenous magnesium sulfate for treatment of electrolyte imbalance between July–August 2013
will be conducted to evaluate indication, duration of therapy, monitoring parameters and safety.
Data collection will include patient demographics (age, sex, race). Efficacy parameters will
include magnesium level, pre and post administration and time associated with these levels.
Additionally, safety will be based on the respiration rate at time of administration and
appropriate urine output preceding each dose. All patient identifiers will be removed and data
will be kept confidential to protect patient privacy. This project is part of the health system
Medication Use Evaluation (MUE) and Improvement program, which has been approved by the
institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-145
Title: Assessment of prohibited abbreviations in the electronic medical record
Primary Author: Erin Gurley, University of Georgia College of Pharmacy, Georgia;
Email: ErinUGA@UGA.EDU
Additional Author(s):
Richard Burrell
Purpose: According to the Institute of Medicine, over 3 billion dollars goes towards treating the
consequences of medication errors. In 2002, The Joint Commission approved a National Patient
Safety Goal requiring accredited organizations to implement a list of prohibited abbreviations.
The introduction of computerized prescriber order entry eliminates many of the opportunities for
unsafe abbreviations in medication orders; however, other parts of the chart use free text entry
and have received less scrutiny. The objective of this study is to evaluate the compliance of an
academic medical center with Joint Commission recommendations for avoiding prohibited
abbreviations in the electronic medical record.
Methods: A retrospective analysis will be conducted for all electronic medication related
documentation entered in the medical records during a 24 hour period on a single adult medicine
nursing unit. Data collected for analysis will include the type of documentation, date and time of
entry, author of the documentation (e.g., resident, attending, nurse practitioner, physician
assistant, pharmacist), and if an unsafe abbreviation was included within the documentation. All
patient identifiers will be removed and data will be kept confidential to protect patient privacy.
The information collected will be analyzed to determine the extent to which the electronic
medical record was free of unsafe and prohibited abbreviations. This project is part of the health
system Medication Use Evaluation (MUE) and Improvement program, which has been approved
by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-146
Title: Electronic prescribing: an evaluation on cost effectiveness, clinician adoption and
limitations
Primary Author: Annie Hahn, Mercer University College of Pharmacy, Georgia;
Email: annie.hahn@live.mercer.edu
Additional Author(s):
Annesha Lovett
Purpose: The enactment of the Medicare Modernization Act of 2003 has resulted in greater
utilization of electronic prescribing. E-prescribing has flourished due to the promise of
improving efficiency and decreasing prescription errors caused by its handwritten counterpart,
yet only 44% of doctors offices use paperless prescriptions. Many studies have assessed the
value of e-prescribing in the clinical setting, yet there is no all-inclusive summation of these
findings. The aim of this study was to review the literature within the last decade pertaining to
the cost effectiveness, clinician adoption and limitations of e-prescribing.
Methods: Journal articles were compiled through use of the search engines: PubMed,
International Pharmaceutical Abstracts (IPA), and Google Scholar. The key terms utilized were:
future and e-prescribing, future and pharmacy informatics, e-prescribing and limitations, clinical
pharmacist and e-prescribing, HITECH act and electronic prescribing and computerized provider
order entry (CPOE). Articles selected for review were published from January 1, 2003 through
May 1, 2013. The articles required information on e-prescribing; particularly, articles pertaining
to limitations, cost-effectiveness, clinician perceptions and future needs. To explore efforts
toward the future of e-prescribing a list of quality management systems developed to improve the
e-prescribing experience were also derived from the literature. Articles pertaining to pharmacy or
the use of pharmacy informatics were also utilized as a secondary search and mainly focused on
U.S. data. However, international studies were utilized to characterize crucial points or opinions
about e-prescribing. Subsequent related U.S. articles were then searched to support those claims.
Once articles were retrieved, they were summarized in a table which was organized by noting the
year published, author(s), title, study design, intervention, findings, and source for each study.
The articles were assessed for quality by a second author to ensure that all articles met the
inclusion criteria.
Results: A total of fifty-seven peer-reviewed articles were included in this review. Trends show
that most clinicians view e-prescribing positively despite some limitations. Limitations of eprescribing include cost of implementation and maintenance, insufficient training, and lack of
standardization. As more legal regulations come into effect promoting standardization, there is
greater incentive to invest in integrated e-prescribing systems as well as promote clinician
adoption. The cost to implement an integrated system with alerts and decision support is $29,000
per physician for the first year and $4,000 every year thereafter. Furthermore, clinicians may use
e-prescribing to facilitate disease state management with the use of an integrated system with
formulary support. These systems may provide information on medication copayments,
coinsurance, and tiers. For every $10 increase in copayment for a patients initial hyperlipidemia
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
medication, the patients likelihood to be at goal decreases by 5%. Additionally, for every dollar
invested to increase medication adherence, there is a potential to save $3-$10 in medical costs
estimated as $14 billion per year. Decreases in prescription error resulted in a 12.5% reduction in
medical errors or 17 million errors in over 4,700 hospitals. Finally, e-prescribing has little
disruption to workflow and no statistically significant increase in processing time.
Conclusion: Although limitations exist, an expansion of e-prescribing is expected in the future.
An initial investment is required but studies reveal cost savings, reduction in prescription errors
and improvement in prescription quality. Efforts should be increased to promote clinicians
adopting e-prescribing. This study has pointed to the main drivers and benefits of
standardization. Key interest groups advocating for standardization need to meet the demands
required to make e-prescribing systems user-friendly and valuable. Clinical pharmacists can
promote e-prescribing advocacy by highlighting potential use to effectively maintain patients
disease states and create better integration between pharmacists, physicians and patients.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-147
Title: Retrospective evaluation of inpatients with suspected Clostridium difficile infection (CDI)
at a community hospital
Primary Author: Leslie Harris, Mercer University College of Pharmacy, Georgia;
Email: leslie.k.harris@live.mercer.edu
Additional Author(s):
Bobby Jacob
Adam Bressler
Rodna Larson
Martin Kelvas
Purpose: Clostridium difficile is a toxin producing anaerobe that leads to nosocomial infectious
diarrhea. Studies suggest that Clostridium difficile infection (CDI) may be replacing methicillin
resistant Staphylococcus aureus (MRSA) as the most common etiology of hospital acquired
infection in community hospital settings. The incidence of CDI in the United States has been
steadily increasing over the past decade and significant economic burdens have been
demonstrated. Recently, clinical guidelines have been published regarding the appropriate
diagnosis and management of patients with suspected CDI. The purpose of this study is to
evaluate the management of patients with suspected CDI in a community hospital.
Methods: This is a retrospective case-control study involving electronic inpatient medical chart
review. There is no planned patient intervention and, as such, patient informed consent will not
be obtained. Patients will be identified using a record of all samples sent to the laboratory for
testing of CDI from August 2012 to July 2013. Cases are defined as those patients having a
positive test for CDI. Cases will be matched to controls that tested negative for CDI. Data
collection forms will be used to collect: patient baseline demographics, admission diagnosis, past
medical history, date of CDI symptom onset, laboratory test results, number of stools, presence
of risk factors for infection, treatment selected, response to therapy, and recurrence of CDI
within 30 and 90 days post-discharge. Patient data will be reviewed for trends in patient risk
factors, treatments selected, and recurrence rates of infection. Approval has been obtained from
the Institutional Review Board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-148
Title: Ponatinib induced adverse effects: acute pancreatitis, hepatotoxicity and thrombocytopenia
Primary Author: Saba Hasan, Philadelphia College of Osteopathic Medicine School of
Pharmacy, Georgia;
Email: sabaha@pcom.edu
Additional Author(s):
Crystal Fedorkiv
Naba Rahman
Jennifer Andres
Case Report: Chronic myeloid leukemia (CML) is a myeloproliferative disease that generates
from malignant transformation of pluripotent hematopoietic stem cells. First line treatment for
CML is the tyrosine kinase inhibitor (TKI), imatinib. For patients resistant or intolerant to
imatinib, other TKIs, dasatinib, nilotinib, and ponatinib, are approved treatments. Patients who
are resistant or intolerant to other agents are started on ponatinib as a last line option. Common
adverse events of ponatinib are hypertension, dry skin, rash, abdominal pain, constipation, and
nausea. More serious adverse effects include cardiovascular effects, fluid retention, pancreatitis,
severe myelosuppression, and hepatotoxicity. Treatment for these adverse effects can include
interrupting ponatinib therapy and providing symptomatic and supportive care. Reintroduction of
agent can be considered when the serious event has resolved or the potential benefit of resuming
therapy is judged to outweigh the risk. The patient is a 65 year old Caucasian male with a history
of imatinib-resistant CML. The patient was started on ponatinib 45mg approximately 3 months
prior to presentation after failure of previous regimens. He requires platelet transfusions for
ponatinib associated thrombocytopenia. He presents with 4 days of new right flank pain with
radiation to his right groin. Evidence of pancreatitis was found on endoscopic retrograde
cholangiopancreatography (ERCP). LFTs were elevated on admission. The patient had no
history of alcohol or steroid use. Ponatinib was discontinued on admission and within three days
the patients symptoms of thrombocytopenia, pancreatitis and hepatotoxicity began to resolve.
After complete resolution of the pancreatitis, the patient was restarted on ponatanib 15mg as an
outpatient. Patients started on ponatinib should have their serum lipase, amylase, liver enzymes,
and platelets checked every 2 weeks for the first 2 months and then monthly. By checking levels
regularly it may allow the physicians to decrease the dose before complications arise that may
require hospitalization. Signs and symptoms of pancreatitis should also be monitored. Patients
should be started on a low dose to avoid complications and then titrated up as tolerated.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-149
Title: Effectiveness of a comprehensive medication reconciliation program in reducing
medication discrepancies in heart failure and stroke patients at a community hospital
Primary Author: Rebecka Hazelwood, Mercer University College of Pharmacy, Georgia;
Email: rebecka.hazelwood@live.mercer.edu
Additional Author(s):
Angela Shogbon
Bobby Jacob
Chika Ugwuoke
Martin Kelvas
Purpose: The Joint Commission (TJC) has set forth measures to improve patient safety and
quality of care, including medication reconciliation and core measures. Medication reconciliation
is the process of comparing a patients medication orders to all of the medications the patient has
been taking. Core measures are a performance measurement system that includes standards for
heart failure and stroke patients. The objective of this study is to evaluate the effect of a
pharmacy-driven comprehensive medication reconciliation program in detecting and eliminating
medication discrepancies in heart failure and stroke patients and in ensuring compliance with
medication specific core measure sets.
Methods: This prospective, controlled study with a historical control group was approved by the
institutional review board. The study group will consist of patients 18 years admitted with a
primary diagnosis of heart failure, stroke, or transient ischemic attack. The control group will
consist of patients 18 years admitted with matching primary diagnoses during the same time
period but in the previous year. A home medication interview will be conducted with patients in
the study group within 24-48 hours of admission. The interview medication list will be compared
with the current medication list in the patients electronic medical record, and any noted
discrepancies (omission, addition, duplication, interaction, others) and subsequent action taken
will be documented. Discharge orders will be compared to medication specific core measure sets
for heart failure and stroke, as well as the home medication history list compiled previously and
the most recent active inpatient medications list. A medication discharge counseling session will
be conducted. All data will be recorded without patient identifiers and maintained confidentially.
The effectiveness of this pharmacy-driven program in reducing medication discrepancies at
admission and discharge, in ensuring compliance with TJC medication specific core measure
sets, and in reducing readmission rates will be examined.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-150
Title: Revised range order policy for the improvement of patient safety
Primary Author: Kendal Hembree, University of Georgia College of Pharmacy and Northside
Hospital, Georgia;
Email: kendal.hembree@gmail.com
Purpose: Consistent interpretation and application of range order policies in hospital settings is
important not only to promote patient safety but also to comply with accreditation standards. The
release of The Joint Commission Sentinel Event Alert last year promoted the review and revision
of the current range order policy. This project was designed to revaluate the hospitals range order
policy to comply with The Joint Commission standards and improve patient safety.
Methods: The Joint Commission Sentinel Event Alert on the safe use of opioids in hospitals was
released in August 2012. The alert examined the use of opioids and provided actions hospitals
could implement to avoid adverse events with opioid use. The alert prompted the hospitals
review of opioid prescribing, administration and monitoring. Since most opioid prescriptions in
the hospital are written as range orders, the current range order policy was revised. The policy
was revised to better define uniform guidelines for interpreting dosing and frequency range
orders. Educational resources were created to help inform all hospital staff on the new policy
changes. Education was presented to nurses and pharmacists at staff meetings and fliers were
placed in break rooms to reinforce the changes. Memos were sent to all medical staff announcing
the changes and education was presented at medical staff meetings prior to implementing the
revised policy. All education, fliers and memos contained examples of the changes and practice
problems were available to help ease the transition.
Results: The revised range order policy was created based on The Joint Commission Sentinel
Event Alert however it was also in compliance with The Joint Commission accreditation
standards. The policy limited all frequency ranges to the lowest frequency and all frequency
orders be stated as no more often than. The policy also limited the maximum dosing range to
four times the minimum dose. All changes to the frequency and dosing ranges were designed to
be automatically implemented by pharmacy. The policy also revised administration guidelines to
make sure the patient is always receiving the most effective and safe dose. The revised
guidelines help decrease the chance for adverse events in the hospital and create a standardized
method for handling range orders.
Conclusion: The evaluation of opioid safety and range orders in hospital pharmacy is essential
to improving patient safety. In compliance with The Joint Commission recommendations the
current range order policy was revised. This policy helped to create a uniform method for
handling all range orders through the hospital and help to enforce The Joint Commissions
mission to continually improve health care for the public.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-151
Title: Antimicrobial stewardship: empowering student involvement in an intravenous (IV) to
oral (PO) conversion project focused on direct patient care
Primary Author: Amanda Herrin, University of Georgia College of Pharmacy, Georgia;
Email: ahyoung@uga.edu
Additional Author(s):
Bruce Jones
Purpose: When patients in clinical settings are treated for infectious diseases, intravenous
formulations of antimicrobials are typically used. Switching the patient from intravenous (IV) to
oral (PO) therapy once clinically stable can reduce the length of hospitalization and lower
associated costs to both the patient and institution. Due to these benefits, IV to PO conversion
protocols have already been implemented at many sites; however, clinical pharmacists now have
many responsibilities that are considered more pressing. Student pharmacists practicing at these
sites are available to step into this role. This study will assess the impact of student directed
interventions on patient care.
Methods: This study was approved by the Institutional Review Board. This will be a
retrospective study to assess IV to PO interventions made between June 11, 2013 and November
11, 2013 at one clinical site. Interventions made during the same period in 2012 will serve as
controls. Clinical pharmacists at the site make these conversions as part of normal practice. A
new system is in place in which these conversions are also made by student pharmacists and their
preceptors as part of the Infectious Disease Advanced Pharmacy Practice Experience (APPE).
Students use the electronic medical records system to identify patients who are receiving
intravenous antimicrobials. The IV to PO conversion protocol of the institution is then used to
evaluate the patients eligibility for oral therapy based on set inclusion and exclusion criteria. The
student then presents the proposed interventions to the preceptor for implementation.
Antimicrobials involved are predetermined by the conversion protocol and include
fluoroquinolones, macrolides, metronidazole, doxycycline, fluconazole, clindamycin, and
linezolid. The costs of both intravenous and oral formulations of each antimicrobial will be
evaluated by acquisition costs. The total cost of the antimicrobials, including administration costs
and associated underlying expenses, will then be evaluated to determine the monetary savings.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-152
Title: Identifying predictors of inappropriate aminoglycoside dosing: using the Hartford
Nomogram in the critically ill
Primary Author: Sarah Hinton, University of Georgia College of Pharmacy, Georgia;
Email: hintons@rx.uga.edu
Additional Author(s):
Dallas Schepers
Carolyn Maness
Hal Richards
Purpose: Aminoglycoside extended interval dosing (once daily dosing) is utilized to provide
efficacious treatment while reducing the incidence of toxicity; however, limited data is available
specifically validating the efficacy of extended interval dosing in critically ill patients. Therefore,
the purpose of this study is to determine if extended interval aminoglycoside dosing is
appropriate to use in the critically ill, and if not, to identify possible factors that complicate
aminoglycoside dosing in this class of patients.
Methods: A prospective, observational cohort study evaluating patients who received a
clinically appropriate dose of an aminoglycoside based on actual or adjusted body weight (7
mg/kg of gentamicin/tobramycin or 15 mg/kg of amikacin) from October 2013 to January 2014
at one institution's ED or ICU. For inclusion in the study, all patients must have a 10-hour
random aminoglycoside level plotted on the Hartford nomogram to determine the predicted
dosing interval. Based on this predicted dosing interval a second random level will be obtained to
confirm that the dosing interval is appropriate. Using those levels inappropriate dosing will be
confirmed based on subtherapeutic or supratherapeutic results. Patients will then be separated
into two groups: those that had appropriate dosing intervals predicted by the Hartford nomogram
and those that did not. Analysis of patient specific factors (i.e. height, weight, age, gender, etc.)
to identify potential predictors of inaccurate dosing will be performed using chi square for
categorical or ordinal predictors and logistic regression for numerical predictors. This study has
been submitted to the Institutional Review Board for approval.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-153
Title: Assessment of a fixed-dose rasburicase protocol at an academic medical center
Primary Author: Stephanie Hoge, University of Georgia College of Pharmacy, Georgia;
Email: shoge@uga.edu
Additional Author(s):
Stephen M. Clark
Amber B. Clemmons
Purpose: Primary literature indicates that fixed-dose rasburicase is safe, clinically effective and
cost effective for the management of hyperuricemia associated with tumor lysis syndrome (TLS).
Current guidelines at this academic medical center recommend the use of rasburicase as a 6 mg
fixed-dose in adult patients with laboratory or clinical TLS and in those individuals who meet
criteria as high risk for TLS. The primary objective of this study is to determine if the fixed-dose
rasburicase protocol is effective and being appropriately utilized per protocol at this institution.
Methods: A retrospective chart review will be conducted of all patients at this academic medical
center who received rasburicase since implementation of the protocol (August 2012 through
August 2013). Data collection will include: patient demographics (age, gender, race, weight,
cancer diagnosis), appropriateness of rasburicase use per protocol, pre-rasburicase blood values
(white blood cell count, serum creatinine, lactate dehydrogenase, uric acid), dose(s) of
rasburicase, need for additional doses of rasburicase, and post-rasburicase uric acid levels. For
safety analysis, we will also collect data on methemoglobinemia occurrence and glucose-6phosphate dehydrogenase (G6PD) deficiency. Patient information will be accessed using the
hospital's electronic medical record system. To protect patient privacy, all patient identifiers will
be removed, and data will be kept confidential. This project is part of the health system
Medication Use Evaluation (MUE) and Improvement program, which has been approved by the
institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-154
Title: Incidence of acute kidney injury in pediatric patients receiving ketorolac alone versus
ketorolac and concomitant vancomycin
Primary Author: Katelyn Hood, Univeristy of Georgia College of Pharmacy, Georgia;
Email: khood@uga.edu
Additional Author(s):
Kelley Norris
Purpose: This evaluation was prompted by two recent reports of acute kidney injury (AKI) in
patients receiving ketorolac at the children's medical center. The primary objective is to assess
the incidence of AKI in pediatric patients receiving ketorolac with and without concomitant
vancomycin. Since both of these agents have the potential to cause AKI, proper monitoring,
appropriate dosing, and early recognition of drug-induced AKI can help improve patient
outcomes and decrease the risk of long-term complications.
Methods: This project is part of the health system Medication Use Evaluation (MUE) and
Improvement program, which has been approved by the institutional review board. A
retrospective chart review will be conducted on a random sample of pediatric patients who
received ketorolac alone and ketorolac with concomitant vancomycin from July 2012 to June
2013. Data collection will include: patient demographics (i.e., age, gender, race, weight,
allergies), medical service/location, baseline serum creatinine (SCr), blood urea nitrogen (BUN)
and urine output, dose of ketorolac and vancomycin (mg/kg/dose and mg/kg/day), vancomycin
trough, total length of ketorolac and vancomycin therapy, and use of other potentially
nephrotoxic agents (i.e., aminoglycosides, other NSAIDs). Data will also be collected regarding
the timeline of ketorolac and vancomycin therapy initiation and the monitoring parameters that
were used to assess for AKI (i.e. vancomycin trough after initiation of ketorolac, routine SCr and
BUN levels, and routine monitoring of urine output).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-155
Title: Assessing the impact of implementing a pharmacy benefit manager (PBM) querying
software into the medication reconciliation process at an inpatient psychiatric facility
Primary Author: Eun Pyung Im, University of Georgia College of Pharmacy, Georgia;
Email: imph@rx.uga.edu
Additional Author(s):
Thomas Wesley Wilkerson
Jennifer Marlowe
Purpose: Medication reconciliation at inpatient facilities is critical in preventing medication
errors. Medication reconciliation typically involves the patients primary nurse consulting the
patient and various sources to compile a current list of medications for a practitioner. This can
turn out to be a frustrating process, and in the end the nurse can still be left with an inaccurate
list. The purpose of this study is to assess the impact that implementation of a PBM querying
software has on medication reconciliation at an 85 bed inpatient psychiatric facility, in terms of
documentation additions, deletions, and modifications.
Methods: This study has been submitted to an Institutional Review Board and is pending
approval and waiver of consent. Data collection will proceed as follows: Initial medication
reconciliation will be performed via patient or caregiver interview, transcription from
prescription bottles, or calls to pharmacies used by the patient. Information gathered will then be
entered into the Hospital Information Systems Home Med application. The medication
reconciliation form will be printed from Home Med for use as a baseline form. The PBM
querying software will then be queried for the patients outpatient prescription list within the past
year. The query results will be compared to baseline and any discrepancies will be edited in
Home Med. Discrepancies include medications absent in the baseline (additions), medications in
the baseline discontinued by the patient (deletions), and medication details (e.g. dose) that differ
between the baseline and query report (modifications). The edited, final medication
reconciliation form will lastly be printed for comparison to the baseline. Data collection will take
place for two weeks on 100 patients. Statistical analysis of the data will be conducted by
performing a one way ANOVA between the forms. Results will be reported as a whole and as
per unit within the facility.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-156
Title: The evolving landscape of health care: The clinical pharmacist's emerging role in
accountable care organizations
Primary Author: Simone Jiandani, Mercer University College of Pharmacy, Atlanta, Georgia;
Email: simone.austin@live.mercer.edu
Additional Author(s):
Annesha Lovett
Purpose: A major focus in health care reform supports the development of accountable care
organizations (ACOs). An ACO is a group of health care providers and suppliers of services that
work together to coordinate care for their patients with a goal to improve quality and decrease
cost. The ACO model provides financial incentives to clinical care coordinators that meet
specific health quality measures. Hospital pharmacists have the skill set to provide clinical care
coordination services. The purpose of this study was to review the literature published within the
last three years related to the role of the pharmacist in ACOs.
Methods: PubMed, pharmacy association websites, the Center for Medicare and Medicaid
Services website, the Kaiser Family Foundation website, and Google Scholar were searched for
articles from 2010 to 2013 in an attempt to identify the various roles and responsibilities of
clinical pharmacists within ACOs. As the implementation of the ACO model began with the
passing of the Affordable Care Act in 2010, the search was limited to articles written from 2010
to 2013. Search terms utilized were ACO, pharmacist and health care reform, Medicare, and care
coordination. The abstract and/or full text of each article was reviewed and studies cited in the
bibliographies produced by these searches were also included in the review. Relevant articles
discussing the functions of current clinical pharmacists and their roles on the health care team, as
well as articles discussing recent health care policy changes were included. Articles were
excluded if they failed to address these two topics.
Results: Results of the literature search yielded 25 articles. Findings revealed three major
themes. Pharmacists were shown to achieve positive clinical outcomes, provide patient centered
care coordination, and achieve valuable economic outcomes within accountable care
organizations. Evidence showed that pharmacists performed a number of functions including
discovering cost-effective methods of medication use, analyzing patient refill requests and care
gaps, tracking physician prescribing practices, and assisting in assessing and managing patient
risk. A growing need was often highlighted with regard to medication therapy management
services such as lipid management, anti-coagulation clinics, and brown bag reviews. One
example, Group Health Cooperative, a Washington state-based ACO that employs more than 200
pharmacists noted that a third of their pharmacists played supportive roles in health plan and
integrated delivery system platforms. Pharmacist duties were broad and ranged from developing
strategies to reducing costs while increasing effective medication use. Other pharmacists focused
on tracking physician performance and prescribing practices. On the other hand, pharmacists
working with HealthCare Partners, a California-based group, were actively involved in clinical
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
administration such as managing patient refill requests and care gaps while pharmacists at the
Houston-area Kelsey-Seybold Clinic also monitored patients and detected care gaps.
Conclusion: Pharmacists are increasingly being recognized as essential members of the health
care team. Their clinical expertise will be necessary to ensure the delivery of optimal streamlined
care within the healthcare system. Access to patient health records will allow the pharmacist to
identify improvement opportunities in treatment plans and make suggestions for modifications.
Medication therapy management services will be needed within ACOs as the U.S. population
ages. Pharmacists will be sought to help patients manage chronic illnesses, perform educational
outreach, and monitor patient progress. Pharmacists can play key roles in ensuring medication
adherence and drug safety to reduce health care costs.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-157
Title: Efficacy of an insulin infusion protocol at a community hospital
Primary Author: Spencer Lei Jones, University of Georgia College of Pharmacy, Georgia;
Email: spencerl@uga.edu
Additional Author(s):
Virginia Fleming
Beth Melvin
Robin Southwood
Purpose: Hyperglycemic crisis is a common admission diagnosis. Insulin dosing algorithms
have been shown in clinical trials to be efficacious at safely and rapidly achieving glycemic
control and expediting transitioning to basal bolus insulin therapy. Many real world factors
(protocol deviations) can influence the efficacy of these algorithms; however, the impact of these
protocol deviations upon patient outcomes is poorly documented. The aim of this study is to
evaluate the efficacy of an insulin drip protocol at a community hospital. This study has been
submitted to the Institutional Review Board for approval.
Methods: Patients admitted with hyperglycemic crisis to the intensive care unit of a 200 bed
community hospital and treated with intravenous insulin drip have been reviewed for inclusion.
Patients less than 18 years, with creatinine clearance less than 30 mL/min, or with a history of
gastroparesis will be excluded. Patients will be categorized as diabetic ketoacidosis (DKA) or
hyperosmolar syndrome (HOS) based upon physician diagnosis and initial venous carbon
dioxide value. Medical records will be reviewed to evaluate demographic information, protocol
process compliance, hypoglycemia risk factors, and markers of successful conversion to basal
bolus therapy. Process compliance evaluation will encompass initiation of dextrose containing
intravenous fluid, electrolyte correction, evidence of 4 hours of glucose control prior to
conversion, predicted total daily insulin (TDI) requirements, TDI administered at conversion,
and TDI at discharge. Data for hypoglycemic risk factor evaluation will include initiation of
dextrose containing fluid when blood glucose values fall below 250 mg/dL, administration of
pre-drip bolus insulin doses, and number of patients converted to basal bolus therapy prior to
target blood glucose range. Successful conversion will be defined as at least fifty percent of
blood glucose values less than 180 mg/dL during the initial 24 hours after conversion without
hypoglycemia.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-158
Title: Formation of a new student organization to promote interest in clinical pharmacy
Primary Author: Julianne Jones, University of Georgia College of Pharmacy, GA;
Email: julianne816@gmail.com
Additional Author(s):
Kristen Alspaugh
Beth Bryles Phillips
Purpose: A student clinical pharmacy organization was formed to educate pharmacy students
about careers in clinical pharmacy and pathways to pursue this goal. The mission of the
organization is to educate student pharmacists about opportunities to further their careers both
during and after pharmacy school. This includes providing information about pharmacy
residency programs and the application process to students. The organization also strives to
develop student members' clinical skills by reviewing and discussing a number of clinical topics,
encouraging students to participate in an annual student competition, and connecting students to
mentors for patient care and research opportunities.
Methods: A proposal was developed outlining the purpose, mission, goals, budget and plan of
implementation. Specific goals were set which included producing a bi-annual, student-written
newsletter, coordinating research opportunities between students and clinical pharmacists,
learning from experts in the field of residency, gaining national recognition as a student chapter,
and conducting chapter meetings connecting the main campus with two regional campus sites. A
faculty advisor was appointed and a constitution was drafted according to the bylaws of the
university's student affairs center. The resources utilized were the faculty advisor, faculty with
expertise in the field of residency training, and the Assistant Dean for Student Affairs at the
College of Pharmacy.
Results: The organization has held four meetings since it was established in the fall of 2012.
There are currently 50 members with a majority of P1 and P2 students represented (P1 n=16, P2
n=24, P3 n=5, P4 n=5). At these meetings, pharmacy students have discussed new medications,
clinical trials and current clinical topics. The organization has also utilized distance-learning
technology to include student members at our regional campuses. A newsletter, written and
edited by pharmacy students has been published. The organization has coordinated student
research opportunities with clinical pharmacy faculty. Preparation for national recognition as a
student chapter has begun.
Conclusion: The formation of a student clinical pharmacy organization was designed to increase
student awareness and interest in clinical pharmacy. The organization has successfully increased
pharmacy student involvement through implementation of a newsletter, identification of research
opportunities, and establishing networking opportunities with clinical pharmacists.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-159
Title: Assessing appropriateness of antibiotics prescribed for treatment of pyelonephritis in the
emergency department of a tertiary care facility
Primary Author: Lopa Joshi, UGA College of Pharmacy, Georgia;
Email: joshil@rx.uga.edu
Purpose: In 2010, the Infectious Diseases Society of America (IDSA) released an update to the
1999 clinical practice guideline for the treatment of women with acute uncomplicated cystitis
and pyelonephritis. This update addresses the increasing resistance of uropathogens to commonly
prescribed antibiotics, and recognizes that appropriate empiric therapy is paramount in a real-life
setting where initial treatment is often determined prior to urine culture and susceptibility tests
being performed or their results known. The objective of this study is to assess the
appropriateness of antibiotics prescribed to female patients who present to the emergency
department and have a diagnosis of pyelonephritis.
Methods: This study will be submitted to the Institutional Review Board for approval. A twelve
month retrospective report of patients with a pyelonephritis diagnosis will be extracted from the
electronic medical record system. Patient data to be collected includes age, sex, drug allergies,
specific diagnosis and code, pregnancy state, site of admission, reason for admission, whether
hospitalization was required, and length of stay. Antibiotic specific data to be generated includes
urine culture and susceptibility results, empiric antimicrobial therapy, target antimicrobial
therapy, duration of therapy, and clinical outcomes. All data will be recorded without patient
identifiers and maintained confidentially. If available, the number of cases in which antibiotic
therapy was revised based on susceptibility results received post-discharge will be noted. The
IDSA guideline for pyelonephritis treatment in women is limited to nonpregnant, premenopausal
women. However, this study includes pregnant and postmenopausal women. Therefore,
appropriateness of antibiotic therapy will be determined based on both the clinical guideline and
susceptibility results.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-160
Title: Evaluation of the use of intravenous acetaminophen post-operatively in patients at an
academic medical center
Primary Author: Ah Hyun Jun, Georgia Regents Medical Center, Georgia;
Email: ajun1@uga.edu
Additional Author(s):
Marjorie S Phillips
Purpose: Since its addition to the hospital formulary in May 2011, use of intravenous
acetaminophen resulted in increased hospital costs while failing to show significant benefit over
less expensive analgesic alternatives. Appropriate use of intravenous acetaminophen has the
potential to improve patient outcome and reduce hospital cost in the immediate post-operative
period. The purpose of this retrospective evaluation is to assess compliance with institutional
guidelines for intravenous acetaminophen, which were updated in May 2013 to further limit use
to patients unable to take any oral medications. The study also assesses the roles of pharmacists
in overseeing adherence to the guidelines.
Methods: This project is part of the health system Medication Use Evaluation (MUE) and
Improvement program, which has been approved by the institutional review board. A
retrospective review was performed on a random sample of fifty-six patients who received
intravenous acetaminophen post-operatively during August 2013. Evaluation parameters include
indication, stop date, duration of therapy, pharmacy intervention, and safety.
Results: A formulary indication for intravenous acetaminophen was documented in 84 percent
(47/56) of patients. The other nine patients included three with sickle cell crisis, one with fever,
one with discomfort and four lacking a clear indication. All 47 post-operative intravenous
acetaminophen orders had an initial automatic 24-hour stop date. Intravenous acetaminophen
was discontinued once the patient was able to take medications orally in 83 percent (39/47) of
patients. After the 24-hour post-operative stop date, the intravenous medication was not
reordered in 87 percent (41/47) of patients. Of the six patients who received reorders, 50 percent
(3/6) were not able to take oral medications post-operatively. For the other three patients, there
were no pharmacist interventions to discontinue or interchange intravenous acetaminophen to the
oral or rectal form. Ninety-one percent of patients (51/56) received no greater than 4 grams of
acetaminophen (all routes) in a 24 hour period. Of the five patients whose daily dose exceeded 4
grams, three were receiving an oral acetaminophen-containing combination product along with
intravenous acetaminophen.
Conclusion: Many steps were taken at this institution to limit the use of intravenous
acetaminophen and reduce the hospital cost, including updating the guidelines for use and
promoting pharmacist involvement. Continued improvement is needed in adherence to the
guidelines as well as pharmacist involvement in making appropriate interventions when the
guidelines are not followed. There is also a concern for patient safety as some patients received
more than the recommended daily dose of acetaminophen in a 24-hour period. The Pharmacy
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
and Therapeutics Committee will meet and discuss the next steps regarding the optimal and safe
use of intravenous acetaminophen.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-161
Title: Acute pancreatitis induced by an over-the-counter (OTC) antacid
Primary Author: Emily Kraus, University of Georgia, Georgia;
Email: ejkraus2817@gmail.com
Additional Author(s):
Diane Nykamp
Purpose:
Methods:
Results:
Conclusion:
Case Report: A case of acute pancreatitis associated with the administration of high doses of
over-the-counter (OTC) antacid containing calcium carbonate is reported. A 68-year-old male
presented to the emergency department with a four-day history of nausea, vomiting, and
abdominal pain. Patient reported taking 15-20 Tums EX Strength tablets for four to five days
prior to admission for stomach discomfort. The current recommendation from the Institute of
Medicine for calcium intake is 1,000mg to 1,200mg daily for most adults. A single Tums EX
Strength tablet contains 750mg of calcium carbonate (300mg of elemental calcium). This patient
ingested 4.5-6.0g of elemental calcium per day, two to three times the upper limit of calcium in
patients with normal renal function. The calcium level upon admission was 18.5 mg/dL (normal
calcium level ranges from 8.4-10.3 mg/dL). An abdominal computed tomography confirmed
acute pancreatitis. Laboratory values of amylase and lipase peaked at 2,768 U/L (normal amylase
ranges from 20-110 U/L) and 7,091 U/L (normal lipase ranges from 0-160 U/L). For a period of
45 days, the patient was treated in the intensive care unit for acute pancreatitis and later
progressing to necrotizing pancreatitis. There are several proposed mechanisms by which
hypercalcemia causes pancreatitis, though still unclear. One mechanism is that calciumdependent activation of trypsinogen to trypsin within the pancreas leads to activation of other
digestive enzymes, which results in damage and necrosis to the pancreas and other organs.
Another mechanism involves the acinar cells, where pancreatitis is thought to originate.
Hypercalcemia is one trigger that causes excessive release of acinar cytosolic free ionized
calcium and precipitates acute pancreatitis. This case study supports an association between
hypercalcemia and pancreatitis in a patient who ingested greater than recommended dosages of
calcium-containing antacids. This case study reports organ damage secondary to elevated
calcium, which was the result of excessive self-care dosages of an antacid containing calcium
carbonate.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-162
Title: Evaluation of allergy documentation at an academic medical center
Primary Author: Jennifer Lee, University of Georgia College of Pharmacy, Georgia;
Email: leeje@rx.uga.edu
Additional Author(s):
Kamika Felder
Marjorie S. Phillips
Purpose: To evaluate allergy documentation for accuracy and completeness in the clinical
information system of an academic medical center.
Methods: A retrospective chart review will be conducted on allergy documentation in the
electronic medical record for one week of discharged patients in August 2013 (roughly 2 percent
of annual discharges). Data collected will include age of the patient, hospital unit, and whether
an allergy or no known allergy (NKA) is listed. For those with a listed allergy, the description
and severity of the reaction will be recorded to differentiate between a true allergic reaction
(hives, anaphylaxis) and an adverse reaction that is not classified as life-threatening (nausea,
drowsiness, etc.). In cases where inaccurate or exemplary allergy documentation is noted, the
personnel type of the responsible individual (resident or attending physician, nurse, pharmacist,
patient care assistant) will be recorded. This project is part of the health system Medication Use
Evaluation (MUE) and Improvement program, which has been approved by the institutional
review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-163
Title: Review of the use of bevacizumab in glioblastoma multiforme (GBM)
Primary Author: Mei Li, Philadelphia College of Osteopathic Medicine School of Pharmacy,
Georgia;
Email: heyitsmei@yahoo.com
Additional Author(s):
Sonia Patel
Purpose: Glioblastoma multiforme (GBM) is an aggressive glioma which has a median survival
of about 18 months. Standard first-line treatment for newly diagnosed GBM is surgery followed
by concurrent chemoradiation with temozolomide followed by temozolomide for maintenance
treatment for one year. After bevacizumab received FDA approval for recurrent GBM,
physicians have been using bevacizumab as first-line treatment without any data to support the
decision. The purpose of this poster is to provide a summary of safety and efficacy data of
bevacizumab from some of the larger clinical trials for the use of bevacizumab in GBM.
Methods: The package insert for bevacizumab, a PubMed search and recent updates from the
2013 American Society of Clinical Oncology (ASCO) meeting were used to find major clinical
trials for the use of bevacizumab as first-line therapy for GBM and second-line therapy for
recurrent GBM. Results from four studies were used to determine the safety and efficacy of
bevacizumab in GBM.
Results: The AVF3708g (BRAIN) was an open-label, multi-center phase II trial randomized to
either bevacizumab alone or bevacizumab and irinotecan. Overall survival was higher in the
bevacizumab alone arm at 9.3 months compared to 8.8 months in the bevacizumab plus
irinotecan group. NCI06-C-0064E (NCI) was a single-arm, single-site study including previously
treated GBM patients with temozolomide and radiation who then received bevacizumab. The
objective response rate was 19.6% with a 95% confidence interval and a median response
duration of 3.9 months. BO21990 (AVAGLIO) is a large, randomized, double-blind, placebo
controlled phase III trial in Europe currently still recruiting and planning to have 920 patients at
about 140 centers worldwide. NCT00884741 (RTOG) was a randomized double-blind, placebo
controlled phase III international study conducted in the United States at MD Anderson Cancer
Center with 637 patients with newly diagnosed glioblastoma. Patients underwent standard of
care with surgery and temozolomide with radiation and then were randomized to receive either
placebo or bevacizumab. The researchers found no difference in overall survival between the
bevacizumab and placebo arms with 15.7 months in the bevacizumab arm and 16.1 months in the
placebo arm. The study also found that the bevacizumab arm had significantly more toxicities.
Conclusion: It can be concluded from a review of the BRAIN and NCI studies, which are the
two studies that earned bevacizumab its FDA indication for use in recurrent glioblastoma, that
bevacizumab is safe and effective to use as second-line therapy for relapsed glioblastoma.
However, the same cannot be said for use of bevacizumab in newly diagnosed glioblastoma as
first-line therapy based on the RTOG study which showed no difference in overall survival and
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
more adverse events in the bevacizumab groups. Further studies need to be done to evaluate the
use of bevacizumab as first-line treatment option for GBM.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-164
Title: Appropriate discontinuation of surgical prophylactic antibiotics before and after
implementation of automatic stop orders in physician computerized order entry
Primary Author: Xiaofeng Li, University of Georgia College of Pharmacy, Georgia;
Email: lip@rx.uga.edu
Additional Author(s):
Ansley S. Barnett
Purpose: National guidelines for antimicrobial prophylaxis in surgery recommend that
prophylactic antibiotics be discontinued by 24 hours after surgery end time for most procedures
and by 48 hours for cardiac procedures. Not only does the use of antibiotics beyond
recommended durations offer no additional benefit to the patient, it also increases the risk for
Clostridium difficile infections and the development of microbial resistance. The objective of
this study is to determine whether the implementation of automatic stop orders for prophylactic
antibiotics improved institutional adherence to guidelines.
Methods: This project is part of the health system Medication Use Evaluation and Improvement
program, which has been approved by the Institutional Review Board. A retrospective review
will be conducted of the electronic medical records of patients receiving antibiotics for surgical
site prophylaxis sixty days before the implementation of automatic antibiotic stop orders in
computerized physician order entry. An identical review of patients receiving prophylactic
antibiotics during the same time frame one year later will be conducted and compared. The data
that will be collected for both groups include: date of surgery, procedure type, prophylactic
antibiotic used, anesthesia end time, and antibiotic discontinuation time. Presence of a computergenerated versus physician-entered stop date/time and whether the prescriber extended the order
beyond the initial stop will be noted. Inclusion and exclusion criteria and evaluation of adherence
to guidelines will follow methods outlined by the Surgical Care Improvement Project Quality
Measure Set 3 for the timely discontinuation of surgical prophylactic antibiotics.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-165
Title: Assessment of bleeding associated with the use of oral anticoagulants at an academic
medical center
Primary Author: Wen Liu, University of Georgia College of Pharmacy, Georgia;
Email: liuw@rx.uga.edu
Additional Author(s):
David Killough
Hazem Elewa
Purpose: A large number of serious bleeding events associated with the use of the new oral
anticoagulants (NOACs) are reported while warfarin-related bleeding events are likely
underreported in the U.S. Food and Drug Administration's (FDA) Adverse Events Reporting
System (AERS) database. The objective of this study is 1) to review the types of bleeding, 2) to
evaluate the confounding factors contributing to the bleeding, 3) to assess the clinical outcomes
and admission costs due to bleeding associated with the use of apixaban, dabigatran,
rivaroxaban, and warfarin.
Methods: A retrospective analysis will be conducted on patients admitted due to hemorrhage
from September 2012 to August 2013 and with a medication reconciliation record of an oral
anticoagulant (apixaban, dabigatran, rivaroxaban, or warfarin) prior to admission. Appropriate
International Classification of Disease Ninth Revision (ICD-9) codes and target discharge
medications will be used to select the patient population for the project. Data collection will
include demographics, hemorrhagic characteristics, pertinent laboratory values (hemoglobin,
serum creatinine), drug-specific information on previous admission, concomitant high-risk
medications or antiplatelet medications, patients outcomes (discharged or deceased), lengths of
stay, time to readmission, and the cost per admission or readmission. Patient information will be
accessed using the electronic medical record system. All protected health information will be
kept confidential and destroyed upon the completion of research. This project is part of the health
system Medication Use Evaluation (MUE) and Improvement program, which has been approved
by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-166
Title: Medication use evaluation of tigecycline in a regional health system hospital
Primary Author: Tessa Lowachee, South University, Georgia;
Email: tlowachee@gmail.com
Additional Author(s):
Anne Thiong'o
Jaymin Patel
Paul Newman
Kimberly L. Tackett
Purpose: Tigecycline is a glycylcycline intravenous antibiotic indicated for use in multidrug
resistant infections such as community acquired pneumonia, complicated skin and skin structure
infections, and intra abdominal infections. The Medication Use Evaluation (MUE) was designed
to evaluate the prescribed indication, efficacy and safety of tigecycline in a regional community
hospital.
Methods: This MUE was submitted to St. Joseph/Candler IRB Committee for approval. A
retrospective systematic chart review was conducted on patients admitted to St. Joseph/Chandler
who received tigecycline as part of a pharmacotherapy treatment regimen. A data collection form
was developed to assess justification for use, safety, efficacy and adverse events to tigecycline.
Data being assessed included any changes from baseline vital signs, serum BUN, serum
creatinine, liver enzymes, dose, drug interactions, blood glucose and clinical outcomes. Patient
characteristics (height, weight, age, admission diagnosis, comorbidities) will be described using
descriptive statistics. A paired t-test will estimate the significance of the safety and efficacy of
tigecycline based upon pre and post-treatment data.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-167
Title: Intra-articular versus Intravenous Administration of Vancomycin or Aminoglycosides for
Infected Joint Prosthesis
Primary Author: Jordan Mangum, University of Georgia College of Pharmacy, Georgia;
Email: mangumj@rx.uga.edu
Additional Author(s):
Chelsie Sanders
Purpose: To evaluate the efficacy of intra-articular infusions versus intravenous administration
of vancomycin or aminoglycosides for infected joint prostheses.
Methods: The study was completed as a multi-center, retrospective, observational investigation.
The population included adult patients with documented infection of joint prosthesis at St.
Josephs/Candler from January 1, 2008 to December 31, 2013 that received vancomycin or an
aminoglycoside intra-articular or intravenous infusions. Inclusion criteria included: males and
non-pregnant females of at least 18 years of age, documented infection of joint prosthesis,
received intra-articular or intravenous infusion of vancomycin or an aminoglycoside, admitted to
St. Josephs/Candler from January 1, 2008 to December 31, 2013. Exclusion criteria included
patients receiving empiric therapy for suspected joint prosthesis infection. Data collection was
based on: patient demographics, patient WBC, temperature, SCr, CRP and ESR, serum
vancomycin and aminoglycoside levels, vancomycin and aminoglycoside dose/concentration,
cultures and sensitivities, other antibiotics initiated, hospital length of stay, days of therapy of
each antibiotic, antibiotic exposure or history, number of revisions, number of previous
infections, physicians consulted. Primary outcomes included: escalation of antibiotics, addition
of IV to IA antibiotics, readmission within 1 year for infected prostheses. Secondary outcome
variables included: hospital length of stay in days, greater than 50% increase in SCr during the
time on antibiotics. Data analysis was performed using Chi-squared test, fisher's exact, and
Student's T test.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-168
Title: Apixaban versus warfarin for stroke prophylaxis in patients with non-valvular atrial
fibrillation: a cost-benefit analysis
Primary Author: Francisco Marrero, University of Georgia College of Pharmacy, Georgia;
Email: francisco.marrero.pharmd@gmail.com
Purpose: Apixaban offers monitoring-free, fixed-dose treatment for patients with non-valvular
atrial fibrillation. When compared to warfarin in the ARISTOTLE (Apixaban for Reduction in
Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial, apixaban demonstrated
superior efficacy over warfarin in stroke/systemic embolism, major bleed, and all-cause
mortality. Despite advantages in event outcomes, apixaban therapy costs significantly more than
warfarin with INR monitoring. A Markov chain model was created to simulate a patient
population and evaluate the true lifetime cost of apixaban and warfarin therapies from a
Medicare perspective.
Methods: A Markov chain model was developed using the Python programming language to
compare the cost-effectiveness of warfarin and apixaban. Simulated patients transitioned
between 5 potential health states (e.g. ischemic stroke, major bleed), each state possessing its
own quality adjusted life year (QALY) and cost. The rates at which patients transitioned to other
health states varied with age, current health state, any previous health state(s), and therapy
chosen. Initial rates for transition were based on the ARISTOTLE trial. Appreciating rates as a
result of age, current health state, and any previous health states were based on seven long term
trials. Costs for drug acquisition were based on the July 2013 average wholesale price from
micromedex. Medical expenses for health states were based on Medicare A and B payments for
acute treatment as well as post-event treatment. QALY values were based on patient surveys.
QALY was discounted at a rate of 3% per year assessed at an instantaneous rate of change. The
accuracy of this model was assessed by comparing generated results to the ARISTOTLE trial.
Results: Outcomes were assessed for 40,000 simulated patients, randomly assigned to either
warfarin or apixaban therapies. The apixaban cohort yielded $994,017,487 total cost, 4,815
major bleeds, 2,387 strokes, 774 hemorrhagic strokes, and 20,000 deaths. Per patient, apixaban
averaged $49,701 total cost, $37,202 for drug acquisition, $12,499 for event cost, 8.09 QALYs,
and 9.78 years lived. Warfarin produced $570,370,957 total cost, 5,563 major bleeds, 2,375
strokes, 1,190 hemorrhagic strokes, and 20,000 deaths. Per patient, warfarin averaged $27,817
total cost, $13,821 for drug acquisition, $14,698 for event cost, 7.77 QALYs, and 9.43 years
lived. The incremental cost effectiveness ratio (ICER) for apixaban compared to warfarin was
$68,388 per additional QALY and $63,431 per additional year lived.
Conclusion: Based on the simulation data, warfarin with INR monitoring is substantially
cheaper than apixaban with an average savings of $21,884. Although event costs were lower in
the apixaban group, their savings did not match the increased cost of drug acquisition. An ICER
of $50,000/QALY is often used as a threshold for cost-benefit. Apixaban exceeds this figure by
$18,388, and so may not be suited for coverage. As of September 29, 2013, mini-sentinel, the
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
FDAs drug surveillance system, has not published post-marketing data for apixaban. This data
will be essential in assessing the real-world cost-effectiveness of apixaban.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-169
Title: Statistical analysis of A1c scores, medication adherence, and health literacy in type 2
diabetic patients
Primary Author: Jacquelyn McRae, Mercer University College of Pharmacy/Student, Mercer
University College of Pharmacy/Georgia;
Email: Jacquelyn.m.mcrae@live.mercer.edu
Additional Author(s):
Maria M. Thurston
Gina J. Ryan
Purpose: The lack of adherence to pharmacologic interventions is often a major barrier to
meeting patient-specific clinical goals, such as A1c target reduction, in chronic disease states.
Diabetic patients are particularly at risk for the development of secondary complications due to
lack of proper disease management with pharmacologic therapies. Previous research studying the
impact of health literacy on medication adherence has been inconclusive. The purpose of this
research is determine if the level of health literacy in patients produces a statistical difference on
hemoglobin A1c scores and medication adherence in Type 2 diabetic patients.
Methods: The Institutional Review Board approved this study. Inclusion criteria included:
patients at Grady Health System; type 2 diabetic patients taking at least one diabetic medication
for at least six months; and minimum of one A1c measurement. Exclusion criteria included: less
than 18 years old, unable to consent, non-English speakers/readers, or a disability/acute
condition that decreased one's mental/physical stability. Eligible, consented subjects were
administered the short-form Test of Functional Health Literacy in Adults (s-TOFHLA) and
Morisky 8-Item Medication Adherence Scale (MMAS-8). Demographics collected: age, gender,
race, highest level of education completed, fluent language, use of injectable or oral medications,
diabetic medication refill history, and most recent A1c value. SSPS was utilized to perform a ttest and one-way ANOVA. Patients were dichotomized into two groups depending on s-TOFLA
scores greater than or equal to 23(adequate) and less than 23(limited). The A1c scores were
averaged for the two groups; a t-test was performed. Patients were grouped into three levels of
adherence based on MMAS score; less than 6(low), 6-7 (moderate), and greater than or equal to
8 (high). The s-TOFLA score was run as a continuous variable against the three nominal groups
of adherence in an ANOVA test.
Results: A total of 145 patients were included in this study; 94.5 percent were African American
and 43 percent were women. The patients' education levels varied, with no majority of patients
with one particular level of education. Of the 145 patients, 7.6 percent finished 8th grade or less;
23.4 percent finished some of high school; 9.7 percent received a GED; 36.6 percent finished all
of high school; 22.8 percent finished college or higher. For the entire sample of patients (N
equals 145), the average s-TOFLA score was 23.5 (SD equals 10.48); the average MMAS score
was 5.5 (SD equals 1.9); the average A1c score was 7.9 (SD equals 1.9). The average A1c score
of subjects with limited literacy (n equals 62) was 7.7 (SD equals 2.0) compared to an average of
8.1 (SD equals 1.9) for patients with adequate literacy (n equals 83) (p equals 0.56). Comparison
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
of s-TOFLA scores as a continuous variable for patients with low adherence (n equals 82),
moderate adherence (n equals 38), and high adherence (n equals 25) provided an ANOVA
analysis (p equals 0.47).
Conclusion: There does not appear to be any statistical differences among patients' A1c value or
level of adherence respective to their level of health literacy. However, A1c is a variable on a
small scale, and the sample size might not have been large enough to detect a difference. These
results show that the level of one's health literacy is not a differential factor in comparing
diabetic patients A1c value. There was also no apparent difference between the three groups of
adherence and their respective s-TOFLA scores. Further study is warranted.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-170
Title: Characterization of 30-day readmission risk for patients with heart failure and stroke at an
urban community hospital
Primary Author: Tabitha McWhorter, Mercer University College of Pharmacy, Georgia;
Email: tabitha.jane.mcwhorter@live.mercer.edu
Additional Author(s):
Pamela Moye
Teresa Pounds
Purpose: Due to increased concerns of diminished reimbursements to hospitals with excess
readmissions for various conditions, institutions are exploring ways to minimize readmissions
while maximizing outcomes. Although many studies have investigated precipitating factors of
heart failure exacerbations and risk assessments to identify stroke readmissions, there have been
no consistent or remarkable findings. Determining the risk of readmission for patients is difficult,
and risk may vary among institutions. The purpose of this study is to identify patient that may
predict readmission for heart failure or stroke within 30 days of discharge from an urban
community teaching hospital.
Methods: The investigational review board of the institution approved this retrospective, chart
review of 573 patients admitted for heart failure exacerbation and/or stroke. Inclusion criteria are
as follows: admission from January 1, 2012 to June 30, 2012 for heart failure and/or stroke as
identified by the daily Evidenced Based Medicine Report. Exclusion criteria includes: patients
who regularly live outside the area of influence of the hospital, nursing home residents, patients
discharged to a social-health center or other centers for acute patients, those suffering any type of
dementia or disabling psychiatric disease, or readmission for a reason other than heart failure or
stroke. The following data will be collected: age, gender, ethnicity, weight, height, length of
hospital stay, reason for readmission if applicable, lifestyle factors, past medical history,
medications prescribed, as well as interventions and services performed at discharge. Factors
contributing to readmission risk will be assessed and documented using the patient electronic
medical record. Characteristics that differ between groups of those readmitted within 30 days and
those not admitted will be determined. By identifying characteristics that may result in premature
readmission, better ways of managing and discharging those patients can be established.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-171
Title: Assessing coagulase negative staphylococcus positive blood cultures and risk factors for
true bacteremia verses contamination in a tertiary care hospital
Primary Author: Sarah Miller, Mercer University College of Pharmacy, Atlanta Georgia;
Email: sarah.martin.miller@live.mercer.edu
Additional Author(s):
Deanne Tabb
Purpose: Coagulase negative staphylococcus (CoNS) can be the causative organism in true
bacteremia but also a common reason for bottle contamination. Treating patients that have
positive blood cultures due to contamination, and not infection, can lead to inappropriate
antibiotic use, increased hospital stay, and increased morbidity and mortality. Risk factors for
true bacteremia due to CoNS include intravascular devices, prosthetic devices, IV drug users,
recent surgery and neonates. The primary objective of this study is to determine the difference in
true CoNS bacteremia versus CoNS contamination. The secondary objective is to determine risk
factors for true CoNS bacteremia in this area.
Methods: This study has been approved by the Mercer University Institutional Review Board
(IRB). A three month retrospective report of all positive CoNS blood cultures was generated
from the TREK blood culture recovery system. Patient data collection includes age, gender, vital
signs (blood pressure, temperature, respiratory rate), labs (WBC, ANC), and culture/sensitivity.
Patient outcomes will include length of hospital stay, duration of therapy, and targeted therapy
following sensitivity. The patients will also be evaluated based on primary reason for
hospitalization: infectious versus non-infectious etiology. All data collection will be reviewed to
determine the percentage of true CoNS bacteremia verses the percentage of contamination in this
hospital. If present, risk factors for true CoNS bacteremia will be evaluated.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-172
Title: Thioredoxin interacting protein is required for high fat diet induced endothelial
inflammasome activation & microvascular degeneration.
Primary Author: Islam Mohamed, Clinical and Experimental Therapeutics program, College of
Pharmacy, University of Georgia;
Email: imohamed@gru.edu
Additional Author(s):
Modesto Rojas
Ruth Caldwell
Adviye Ergul
Azza El-Remessy
Purpose: Obesity, an established risk factor for vascular diseases is characterized with
endothelial dysfunction. Thioredoxin interacting protein (TXNIP) is recognized as an activator of
NOD like receptor protein (NLRP3) inflammasome. Nevertheless, there is a gap in knowledge
whether obesity induced TXNIP expression results in endothelial inflammasome activation.
Methods: 4 to 8 week old Wistar rats were fed with high fat diet (HFD, 45 percent fat) for 8 to
10 weeks. 6 weeks old wild type (WT) and TXNIP knock out (TKO) mice were fed with HFD
(60 percent fat) for 7 to 8 weeks. Human retinal endothelial cells (HREC) were incubated with
sodium palmitate coupled to bovine serum albumin (Pal-BSA) with or without 100 micro molar
peroxynitrite (PN).
Results: In Wistar rats, HFD significantly increased retinal TXNIP expression and its
association with NLRP3. This coincided with increased oxidative and nitrative stress, expression
of cleaved caspase 1, cleaved interleukin 1 beta and acellular capillary formation; the hallmark of
retinal ischemia. Colocalization studies identified retinal vasculature as prominent tissue for
TXNIP expression. TKO mice were protected against HFD induced retinal inflammasome
activation and leukostasis compared to WT mice. In vitro, 400 micro molar Pal-BSA triggered
TXNIP, cleaved caspase-1 and cleaved interleukin 1 beta expression in HRECs with parallel
increases in adhesion molecules (ICAM 1 & PECAM 1) and the proapoptotic cleaved caspase 3
expression. Silencing TXNIP abolished such responses and Pal-BSA mediated mature
interleukin 1 beta release but not PN mediated release in HRECs.
Conclusion: These findings show that TXNIP is required for HFD induced activation of NLRP3
inflammasome and release of interleukin 1 beta in endothelial cells. This will help identifying
innovative therapeutic targets for early vascular protection for nearly 79 Million obese
prediabetic Americans.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-173
Title: Evaluation of as needed pain medication prescribing at an academic medical center
Primary Author: Sarah Myrna, University of Georgia College of Pharmacy, Georgia;
Email: sjmyrna@gmail.com
Additional Author(s):
Christina E DeRemer
Purpose: The Joint Commission standard on as needed order prescribing requires clear
instructions or parameters for interpretation for administration. The purpose of this project is to
evaluate current as needed prescribing practices for opioid pain medication and determine the
use of instructions/parameters for nurse elucidation of administration plan.
Methods: This study will be a retrospective chart review of any patient with as needed opioid
pain medication orders. It will include a convenience sample of all inpatients for the month of
August 2013 with a random selection of patients for a representation of approximately ten
percent overall use to assess as needed pain medications used in the adult and pediatric
populations. Data collection will include: demographics (age, race, gender), history of chronic
pain or drug abuse, location/service, attending physician, number of as needed and/or scheduled
pain medications prescribed, incidence of as needed pain medication changed to scheduled pain
medication, number of as needed pain medications are oral or intravenous, instructions or
parameters provided with as needed order, frequency of as needed pain medication use, and
average pain scale. All data collected will be de-identified during the recording to minimize risk
to patients. Descriptive statistics will be used for interpretation of the information collected. The
project is part of the health system medication use evaluation and improvement program, which
has been reviewed and approved by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-174
Title: Nurses' perceptions and satisfaction with the use of insulin pen devices versus insulin vial
and syringes in an inpatient setting
Primary Author: Dao Ngo, Mercer University College of Pharmacy, Georgia;
Email: Dao.Q.Ngo@live.mercer.edu
Additional Author(s):
Angela Shogbon
Bobby Jacob
Laura Kimble
Gina Ryan
Purpose: Insulin vial and syringes have been utilized for many years as the primary method of
insulin delivery. Insulin pen devices were developed to overcome barriers to insulin selfadministration by patients using vial and syringes, and to improve the convenience, ease of use,
and accuracy of dosing for patients. A limited number of published studies have evaluated nurses
satisfaction with utilizing both methods of insulin delivery in an inpatient setting. The purpose of
this study was to evaluate nurses' perceptions and satisfaction with the use of insulin pen devices
versus vial and syringes for insulin delivery in an inpatient setting.
Methods: The institutional review board approved this survey-based study. All nurses who
practiced at the study institution and voluntarily provided written informed consent were
enrolled. The study institution had been utilizing the insulin pen device for over 6.5 years at the
time of this study, in addition to the insulin vial and syringe. A 23-item survey on the insulin pen
device and a 19-item survey on the insulin vial and syringe were distributed to enrolled nurses.
The surveys included questions on number of years practiced as a nurse, experience
administering insulin to patients using each device, perceptions of each of the two insulin
delivery devices in the areas of ease of use, ease to teach patients, confidence and comfort in use,
and overall satisfaction and preference with use of each delivery device. Safety questions in
relation to perceptions on risk of needle sticks and risk of giving the wrong insulin dose or type
with each insulin device were also assessed. Nurses perceptions were rated on a 4-point Likert
scale with 1 = strongly disagree and 4 = strongly agree. Collected data was analyzed using
descriptive statistics, chi-square analysis and paired t-tests.
Results: A total of 139 (95%) nurses from 9 nursing units provided informed consent and
participated in this study. The study participants had an average SD of 9.8 9 years of experience
as a nurse, and 4.4 3.4 years of experience with the insulin pen device versus 8.7 7.7 years of
experience with the insulin vial and syringe (p<0.001). A greater proportion of nurses agreed and
strongly agreed that the insulin pen device saves on time to prepare and administer insulin, is
easy to measure insulin dose, easy to administer insulin to small patients and easy to teach
patients how to use the devices compared with the vial and syringe (p<0.001). In addition, most
nurses perceived that the use of insulin pens decrease risk of needle sticks and the risk of giving
the wrong dose or wrong type of insulin to patients, compared with the insulin vial and syringe
(p<0.001). Overall, the majority of nurses preferred the use of insulin pen devices to vial and
syringes in an inpatient setting (83% vs. 15%, respectively).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: A greater proportion of nurses felt more comfortable and confident with the use of
the insulin pen devices and perceived insulin pen devices to be safer to use compared with the
insulin vial and syringe. Further exploration of nurses perceptions on the safety questions with
each device is needed to determine if there are measures to be taken to improve the safe use of
insulin delivery devices.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-175
Title: Heparin monitoring using anti-factor Xa assay versus activated partial thromboplastin
time: a retrospective trial
Primary Author: Giang Nguyen, University of Georgia College of Pharmacy, University of
Georgia College of Pharmacy, Athens, GA;
Email: gtonguyen@gmail.com
Additional Author(s):
Melody Sheffield
Maura Hall
Purpose: This research will objectively compare anti-factor Xa heparin assay (anti-Xa) to
activated partial thromboplastin time (aPTT) testing to determine which test is more
advantageous for patients on the heparin drip.
Methods: Data will be collected on two cohort groups receiving continuous IV infusion of
unfractionated heparin. Each group will be separated based on the heparin monitoring tests they
received: aPTT test or anti-Xa test. Each group will contain 25 different patients undergoing
heparin infusion for the treatment of a deep venous thromboembolism or a pulmonary embolism.
Data will be collected from the hospitals electronic medical record. All patient data will be deidentified. Researchers will assess the time to reach therapeutic anticoagulation. Therapeutic
anticoagulation is defined as two consecutive laboratory values within the goal range. Research
will assess the following: number of times laboratory values were within goal range, below goal
range, above goal range, and the patients length of hospital stay. The research will compare the
total cost of anti-Xa tests versus total cost of aPTT tests. This study represents retrospective,
observational research conducted as part of a health system medication use evaluation in a
community hospital. The facility Investigational Review Board gave this research exempt status
because data to be reviewed already exists and the information will be recorded in a manner that
subjects cannot be identified, directly or through identifiers linked to the subjects.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-176
Title: Implementation of a pharmacy managed epoetin protocol for renal patients: conversion
from intravenous to subcutaneous route and weight based dosing
Primary Author: Joanne Nguyen, Mercer University College of Pharmacy, Georgia;
Email: j.nguyen289@gmail.com
Additional Author(s):
Jennafer Pennell
Frank Moulis
Kimathi Blackwood
Purpose: Recent guidelines and studies recommend subcutaneous (SC) administration of epoetin
to be more clinically efficacious than intravenous (IV) administration by maintaining target
hemoglobin at a reduced dose. Economic implications of SC over IV administration, however,
have not been extensively studied. In this study, pharmacists collected data on epoetin doses and
administration routes in 284 renal patients to determine need for performance improvement and
expenditure reduction. The purpose of this study was to assess the economic impact of
implementing a pharmacy managed protocol that converted epoetin administration from IV to
SC route in renal patients being treated for anemia.
Methods: Nephrologist and pharmacists with advance clinical training drafted and prepared an
epoetin dosing protocol for all renal patients admitted to the hospital and receiving treatment for
anemia. The written protocol is based on recent 2000 National Kidney Foundation Kidney
Disease Outcome Quality Initiative guidelines for anemia treatment. Key characteristics of
implemented protocol include: SQ administration for all epoetin doses, weight based dosing,
pharmacy monitoring and dosing of all epoetin doses, doses are administered on a standardized
schedule, and epoetin administration is on the floor and not in the dialysis unit. Pharmacy student
also prepared an epoetin monitoring plan. Key information documented on plan included:
hemoglobin and hematocrit values, initial and current dose, administration route, and iron panels.
The total amount of epoetin used in terms of units for October 2013 will be compared with
amount used in October 2012. Cost-savings for the hospital in terms of US dollars will be
calculated based on the difference in epoetin usage.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-177
Title: Managing the dextrose 50 percent shortage: evaluation of the efficacy and safety of
dextrose 10 percent versus dextrose 50 percent in hypoglycemia management
Primary Author: Anh Nguyen, University of Georgia College of Pharmacy, Georgia;
Email: yanhnguyen611@yahoo.com
Additional Author(s):
Jennifer Maddux
Purpose: Dextrose 50% prefilled syringes are commonly used for hypoglycemia management
based on their ease of administration and efficacy. However, due to recent dextrose 50%
shortage, dextrose 10% premixed bags were utilized to treat hypoglycemia. The purpose of this
study is to evaluate the efficacy and safety of dextrose 10% given at equivalent doses of dextrose
50% in hypoglycemia management. Efficacy endpoints include the ability to reach blood glucose
goal (BG: 70 - 180 mg/dl) and average time to treatment. Safety endpoints include the incidence
of hyperglycemia (BG > 180 mg/dl) or resistant hypoglycemia (BG < 70 mg/dl) post treatment
Methods: This study will be submitted to the Institutional Review Board for exemption as data
will be confidentially collected without patient identifiers. This retrospective chart review will be
conducted comparing the three month time period during which dextrose 10% IV bags were used
with the prior three month time period during which dextrose 50% prefilled syringes were
utilized for hypoglycemia management. This study will include non-pregnant patients older than
18 having hypoglycemic events (BG < 70 mg/dl) that were treated with dextrose. Patients will be
excluded if they received glucose gel or glucagon within 1 hour prior to dextrose treatment.
Collected data will include patient age, gender, history of diabetes, hypoglycemic agents, pretreatment BG, dextrose treatment dose, post-treatment BG, time to treatment, and time to reach
post-treatment BG. Based on hospital protocol, alert patients with BG between 50 and 69 mg/dl
would receive dextrose 50% 20 ml (IV push) or dextrose 10% 100ml (10 minute infusion); alert
patients with BG < 50 mg/dl or unconscious patients with BG < 70 mg/dl would receive dextrose
50% 50ml (IV push) or dextrose 10% 250ml (15 minute infusion). Statistical analysis will be
performed to determine if any of the primary measurements achieve statistical significance.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-178
Title: Perceptions of podcast use among first, second and third year student pharmacists in
clinical and research methods courses
Primary Author: Tuyen Nguyen, Mercer University College of Pharmacy, Georgia;
Email: tuyen.l.nguyen@live.mercer.edu
Additional Author(s):
Annesha W Lovett
Carla L Bonner
Lisa M Lundquist
Purpose: Studies show that students can benefit from podcasts because they can listen to the
lectures more than one time at their own pace and review the parts of the lectures that they
missed. Although studies have been conducted with regard to medical student use of video
recorded lectures, currently, there is limited available literature on pharmacy student perceptions
of podcast use. The purpose of this study was to describe the perceptions of podcast use of first,
second and third year pharmacy students and to explore student confidence in clinical topics
covered in the selected courses.
Methods: All pharmacy students of first, second, and third professional year (approximate class
size for each year was 155) were invited to participate in pre-course and post-course surveys.
First year students were enrolled in a Research Methods course in Fall 2012, second year
students were enrolled in a Cardiovascular Diseases I course, and third year students were
enrolled in an Infectious Diseases I course, both in Spring 2013. Podcasts were provided as a
supplement to lectures and covered all topics of each course. The surveys included a section to
collect demographic information and utilized 4-point Likert Scales (1=strongly disagree,
2=disagree, 3=agree, and 4=strongly agree as well as 1=not confident, 2=limited confidence,
3=confident, and 4=very confident). The data was entered into SPSS 21.0 and descriptive
statistics were utilized to analyze the data. The study was approved by the university's
Institutional Review Board.
Results: Pre-course surveys were completed by 114, 134, and 85 first, second, and third year
students, respectively. Post-course surveys were completed by 120, 74, and 44 participants,
respectively. The pre-surveys, which explored student perceptions on podcast usefulness,
showed that the majority of students across three pharmacy profesional years agreed or strongly
agreed that podcasts were a useful learning tool (91.2%, 92.3%, and 90% for the first, second,
and third year, respectively), podcasts promoted understanding of course material (89.3%,
93.9%, and 90%), podcasts helped with missed concepts (96.4%, 95.4%, and 93%), and podcasts
helped prepare for exams (92.9%, 92.3%, and 85%). Post-course surveys revealed that the
majority of students across three classes felt confident or strongly confident on most topics at the
end of the courses. First year students had mean scores of 3.23, 3.02, and 3.01 in Observational
Studies/Randomized Controlled Trials, Literature Evaluation, and Research Related Skills.
Second year students had mean scores of 3.41, 3.27, 3.23, and 3.43 in Physiology of the Heart,
the Peripheral Circulation, Kidney Anatomy/Function, and Anatomy/Physiology of the Blood.
Among third year students, mean scores were 3.25, 3.27, 3.22, and 3.15 in Bacterial
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Pathogenesis, Medicinal Chemistry and Pharmacology of Cell Wall Inhibitors,
Quinolones/Sulfonamides, and Antiretrovirals, respectively.
Conclusion: Trends show that podcasts are beneficial for students as a supplement to lecture in
various pharmacy courses, despite students professional year in the pharmacy program. The
majority of students agreed or strongly agreed with the usefulness of podcasts and the level of
confidence in course topics, both clinical and non-clinical, increased with the use of podcasts.
Podcasts have the potential to be a valuable learning tool for student pharmacists when integrated
into the pharmacy curriculum. Future research should focus on an empirical comparison of
podcast perceptions between the three pharmacy classes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-179
Title: Prolonged unneeded use of liposomal amphotericin B
Primary Author: Megan Patch, University of Georgia/Georgia Regents Medical Center,
Georgia;
Email: patchm@rx.uga.edu
Additional Author(s):
J. Russell May
Purpose: Liposomal amphotericin B is a costly, broad-spectrum antimicrobial agent. Overuse of
this antimicrobial can lead to increased institutional cost and fungal resistance. Liposomal
amphotericin B carries a higher adverse drug reaction (ADR) profile than other antifungals.
Empiric therapy for antifungal and antimold coverage for patients can be unnecessarily
prolonged, which is very costly to both the patient and the institution. This review aims to
analyze the current use of liposomal amphotericin B, appropriate and timely targeting of therapy
or discontinuation when indicated, and adverse reactions related to liposomal amphotericin B
that may have been avoided with an appropriate alternative agent.
Methods: This project is part of the health system Medication Use Evaluation (MUE) and
Improvement program, which has been approved by the institutional review board. A
retrospective chart review will be performed on all inpatients that received treatment with
liposomal amphotericin B to collect data for the time period of one year (July 2012 through June
2013). Data to be collected will include patient demographics (age, race, gender), indication for
use (empiric or specific therapy), duration of use, time to susceptibility results and possible
change of therapy, adverse reactions, and other antimicrobial agents used.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-180
Title: Role of the clinical pharmacist practitioner in the prevention of hepatitis B virus infection
in patients with diabetes mellitus at a family medicine practice
Primary Author: Ami Patel, Campbell University College of Pharmacy and Health Sciences,
North Carolina;
Email: adpatel0213@email.campbell.edu
Additional Author(s):
Matthew B. Harrell
C. Brock Woodis
Purpose: Patients with diabetes mellitus (type 1 or 2) are at increased risk for contracting
hepatitis B virus (HBV) due to contact with supplies exposed to blood. The Advisory Committee
on Immunization Practices (ACIP) and the American Diabetes Association (ADA) Standards of
Medical Care in Diabetes- 2013 recognize that unvaccinated patients with diabetes aged 19-59
years should receive HBV vaccination, with vaccination to be considered in patients &#8805; 60
years of age. The objective of this study is to show how the clinical pharmacist practitioner
(CPP) can aid in the prevention of acute and chronic liver infection in these patients.
Methods: Institutional Review Board approval will be obtained prior to data collection. The
electronic medical record system will retrospectively identify patients with diabetes mellitus that
have not received the HBV vaccination that visit the CPP-managed Pharmacotherapy Clinic. The
following data will be collected: patients' diagnosis of diabetes mellitus either type 1 or type 2,
patients' age, and a record indicating that HBV vaccination is indicated. All recorded data will be
de-identified. Patients referred to the Pharmacotherapy Clinic by the patient's primary care
provider for more intensive diabetes management will be evaluated and educated on the risks and
complications of contracting HBV, as well as educated about the benefits of receiving the
vaccination. The CPP will schedule a nursing appointment for the patients interested in starting
their three-dose HBV vaccination series, to be given over a 6 month period. Descriptive statistics
will be used to analyze the data. Results will include the number of patients receiving the HBV
vaccine due to the CPP interventions and referrals.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-181
Title: Evaluation of opiate use in opioid naive and tolerant patients receiving patient controlled
analgesia at an academic medical center
Primary Author: Kartik Patel, University of georgia college of pharmacy, Georgia;
Email: patelk@rx.uga.edu
Additional Author(s):
Christy Norman
Purpose: The Food and Drug Administration sentinel alert and statistical reports highlight the
risk of respiratory depression associated with opioid use in inpatient settings. The objective of
this study is to determine if patients who receive Patient Controlled Analgesia (PCA) to manage
their pain are screened for their opioid history of use and initiated on appropriate doses of opiates
based on patient specific results.
Methods: A retrospective review will be conducted on adult patients at our institution who
received PCA with opiates to manage pain during the month of August 2013. Data collected will
include age, gender, patient opioid history, PCA opioid selection and dosing parameters, adverse
events, and rate of dose titration. The appropriateness of opiate treatment will be based on the
initial starting dose relative to opiate history, consideration of high risk conditions for opioid
induced respiratory depression during screening, and if agents were converted appropriately
when necessary. Patient information will be accessed using the hospital’s electronic medical
record. All patient identifiers will be removed, and data will be kept confidential to protect
patient privacy. This project is part of the health system Medication Use Evaluation (MUE) and
Improvement program, which has been approved by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-182
Title: Evaluation of patients receiving oral anticoagulation therapy admitted to the hospital
secondary to a bleeding event
Primary Author: Emily Peedin, UNC Eshelman School of Pharmacy/Mission Health System,
North Carolina;
Email: emily.peedin@msj.org
Additional Author(s):
Krista K. Luck
Henry M. Dunnenberger
James E. Usedom
Purpose: One of The Joint Commissions (TJC) National Patient Safety Goals is to "reduce the
likelihood of patient harm associated with the use of anticoagulant therapy" (NPSG.03.05.01).
To achieve this goal, TJC recommends evaluating the anticoagulation safety practices at each
institution. The objective of this study is to determine the percentage of patients who were
receiving inappropriate anticoagulation management out of all the patients who experienced
hospitalization secondary to a bleeding event associated with the use of oral anticoagulants.
Methods: This retrospective observational study was approved by the Institutional Review
Board and Research Institute. A query of the electronic medical record system will identify
patients who meet the following inclusion criteria: discharge from the hospital between February
1, 2012 and August 31, 2013 with an ICD-9 code for a bleeding event, 18 years of age or older
and taking warfarin, rivaroxaban, or dabigatran at admission. The following data will be
collected: age, gender, race, health insurance, total body weight, height, anticoagulant used and
dose, concurrent medications, initial serum creatinine, INR, PT, aPTT, reversal agent or blood
transfusion given, order sets, and outpatient anticoagulant records. The study population will be
divided into two groups by a clinical evaluation of the appropriateness of each patient's
anticoagulation management. Descriptive and inferential statistics will be used to compare these
groups. Percentages of the following potential sources of error will be assessed: dosing, drug
interactions, monitoring, holding before procedures, and high bleeding risk scores. A subanalysis of patients greater than 75 years of age will be performed. A comparison of patients
followed at the outpatient anticoagulation service and non-clinic patients as well as potential
errors between warfarin and oral target-specific anticoagulants will be completed.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-183
Title: Evaluation of a pharmaceutical calculations workshop on the skill set of third year
pharmacy students
Primary Author: Naba Rahman, Philadelphia College of Osteopathic Medicine-School of
Pharmacy, Georgia - US;
Email: nabara@pcom.edu
Additional Author(s):
Samuel John
Mandana Ghodrat
Hongjun Yin
Purpose: The role of the pharmacist is crucial in successfully reviewing medication orders and
therapies while ensuring a safe and efficacious process. Pharmaceutical calculations is a course
offered in the first professional year of pharmacy school which focuses on basic mathematical
concepts and reviews of measurement systems specific to the profession of pharmacy. The
purpose of this course is to emphasize the importance of calculations for students and the value
placed on pharmacists' competency in patient care. Our primary outcome measure was to assess
the mathematical and critical skill set of students based on objective pre- and post-workshop
examinations.
Methods: An optional two-day calculations workshop was offered to seventy-five pharmacy
students in their third professional year. The workshop was announced via email to students in
the summer of 2012 to recruit students for the course. Enrolled students were given a preworkshop examination to assess their baseline understanding of pharmaceutical calculations,
concepts and skills. This tutorial was designed to allow students to review fundamental concepts
such as ratio strength, percentage strength, dilutions, contemporary compounding, electrolyte
formulations, aliquots, alligations, intravenous infusion rates and selected clinical calculations
such as heparin dosing, aminoglycoside and vancomycin dosing. Core concepts were reviewed
while incorporating active learning strategies such as in-class case problems with discussion and
use of the document camera to enhance student learning. Upon completion of the two-day
workshop, students were given a post-course examination to assess their mathematical and
problem solving skills. This study was exempt by the university's institutional review board. All
third year professional students who participated in the workshop and completed both the preand post-course examination were enrolled in the study.
Results: The workshop was made available to all seventy-five incoming third year pharmacy
students. Twenty-nine students participated in the two day workshop; however, only twentyseven students completed both the pre- and post-workshop examination for assessment and were
included in the final data analysis. The pre-workshop examination consisted of nine short answer
questions encompassing topics such as calculation of creatinine clearance, nutrition, clinical
dosing of antimicrobial agents, dilution of liquids, pediatric formulations and alligations. The
post-workshop examination consisted of eighteen questions similar in rigor and was also short
answer in design requiring full work to be shown. The average scores for the pre- and postworkshop examinations were 39.4% and 80.7%, respectively. The students' pre-workshop scores
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
had a wider distribution (SD=17.2) than the post-workshop scores (SD=9.5). The raw change in
average score was 41.3 (95% CI 33.49, 44.70). A paired t-test was performed to analyze the data
and a statistically significant difference was found between the pre- and post-workshop scores
(p<0.01).
Conclusion: The results showed a statistically significant improvement for all twenty-seven
students who completed both the pre- and post- examinations. The increase in post-test scores
ranged from 15- to 73-points, with an average improvement of 41.3 points (p<0.01). Our study
confirms the significant impact of additional training in pharmaceutical calculations on the
performance of pharmacy students. Based on the results of this study, future workshops designed
to be delivered at the midpoint of our curriculum is being considered to improve student
mathematical skills and reinforce mastery of core concepts critical to student success in
pharmacy school and in practice.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-184
Title: Pediatric Obesity Class: Teaching Kids How to Live Healthy Lifestyle
Primary Author: Sara Reece, Philadelphia College of Osteopathic Medicine School of
Pharmacy, Georgia Campus, Georgia;
Email: sararee@pcom.edu
Additional Author(s):
Mary Ann Clever
Nicole Phipps
Purpose: The purpose of this program is to empower entire families to develop healthy lifestyle
and eating habits.
Methods: The referral process requires a pediatrician referral. The clinical criteria for class
enrollment is to be clinically obese or > 20% higher than the ideal weight. Some areas reviewed
in class are issues of excess weight, definition of calories, problems of excess calorie
consumption, what are empty calorie foods, problems with sugary drinks and what are healthier
alternatives, what do fast foods really offer, portion control, benefits of plate portioning, reading
labels to make more nutritious food calories, cut down on screen time, what does whole grain
really mean, and super snack ideas. The roles of child and parent during class are to take the
ideas given in the class and go home making it a family affair, understand that changes the
family can make will take time, and learn to keep communication open. Examples of teaching
methods are spooning out what they think are number of teaspoons of sugar found in a 20 oz
Coke, etc. and then show them the actual amount, show them the actual fat in test tubes, and
showing actual jump ropes/soft sponge balls before class for the kids to play with as they wait
for the class to start.
Results: The total number of children that have attended classes thus far are 121. There have
been 9 English speaking classes and 9 Spanish speaking classes with interpreter alternating every
other month. For every English class, the average pre-class weight was lower than the average
post-class weight while there were 3 Spanish classes that the average post-class weight was
lower than prior to the class. On an individual level, when a child was followed more closely, the
patient would lose or maintain weight while when a child was left to their own responsibility,
then the child tended to gain weight.
Conclusion: After conducting analysis on the 18 total classes provided by The Longstreet Clinic,
it appears that for instances when the child and his/her family did follow-up with the RD for 6
consecutive months, the better the outcome of weight loss for the child would be. In conclusion,
it is imperative that once a child goes to a pediatric obesity class, to follow-up consistently with
the child and his/her parents to ensure that the lessons have been retained and efforts are being
made for healthier living.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-185
Title: Evaluation of significant factors that influence pharmacy students decisions regarding
residency training
Primary Author: Christina Robbins, Univeristy of Georgia, Georgia;
Email: robbinsc@rx.uga.edu
Additional Author(s):
Lindsey Welch
Lori Duke
Michael Fulford
Purpose: Colleges of Pharmacy recognize that a Pharm.D. students perceived barriers or
motivators regarding residency training can influence their individual decision to pursue or not
pursue residency. The objective of this study is to examine that interest and to evaluate changes
in significant factors over time which may influence that decision.
Methods: This study was approved by the University of Georgias Institutional Review Board.
This study examines current 4th year students individual perceptions of residency training
compared to perceptions during their 3rd year. To accomplish this, the study utilizes information
obtained from reflective essays which were completed by students during the third year after an
Introductory Pharmacy Practice Experience focused on residency training as a baseline for
student interest in residency training. Each students interest in residency training will be
categorized as highly interested, somewhat interested, and not interested. This will be directly
compared to a survey questionnaire which the same students complete during their 4th year. The
survey will collect data which examines intent to pursue residency training and perceived
barriers or motivators associated with residencies. Common perceived barriers and motivators
were obtained from primary literature. Results of the essay and the questionnaire will be
compared for each individual student to determine any changes which may have occurred in
intent to pursue a residency and perceived barriers or motivators. Students will be given unique
identifiers to allow for anonymity, and the student investigator will not have access to the key.
The method of data collection will be the online survey questionnaire.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-186
Title: Evaluation of cost effectiveness differences between ziprasidone and aripiprazole
Primary Author: Afeez Salako, Philadelphia College of Osteopathic Medicine (PCOM) School
of Pharmacy, Georgia;
Email: afeezsa@pcom.edu
Additional Author(s):
Mebanga Ojong
Shari Allen
Eddie Williams
Hongjun Yin
Purpose: According to The National Institute of Mental Healths Clinical Antipsychotic Trials of
Intervention Effectiveness (CATIE) study, the drug classes used for the treatment of
schizophrenia, first and second generation antipsychotics, are equal in efficacy (with the
exception of clozapine) but differ in regards to their side effect profile and tolerability. In the
literature, no pharmacoeconomic study has compared the two types of antipsychotics. The
objective of this study is to analyze cost effectiveness differences between Geodon (ziprasidone)
and Abilify (aripiprazole) in patience experiencing acute psychotic episodes.
Methods: This study has been approved by the Institutional Review Board. A drug report
inquiry, using Meds Manager, will be ran to identify inpatients treated between (January, 2013)
and (August 2013) who were prescribed ziprasidone or aripiprazole. Time horizon of the analysis
will be the inpatient stay of each patient. Given there is no similar data reported before, we
couldnt do a power analysis. A total of 100 patient charts will be evaluated for inclusion in the
study; 50 charts of inpatients treated with aripiprazole and 50 charts of inpatients treated with
ziprasidone. The following data will be collected: patient demographics (age, gender, mental
health history), cost of treatment of psychiatric episodes (cost of drug, cost of hospital stay, net
social benefit of evaluated products, acceptable willingness to pay) time of initiation of drug
therapy and discharge from psychiatric unit, and length of psychiatric unit stay. All data will be
recorded without patient identifiers and maintained confidentially Data will be presented as mean
+/- standard deviation. The primary end point of this study will be average and median time to
resolution of psychotic episode defined as: Length of psychiatric stay and patients tolerating
medication for both aripiprazole and ziprasidone.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-187
Title: Evaluation of the use of intravenous nicardipine in the neuro-intensive care unit
(neuroICU) in an academic medical center
Primary Author: Lindsay Schaack, University of Georgia College of Pharmacy, Georgia;
Email: lschaack@uga.edu
Additional Author(s):
Jody C. Rocker
Purpose: Successfully getting blood pressure under control and transitioning to oral agents
quickly is an opportunity to reduce cost and improve care, especially when the patient is
medically stable to transfer to floor status, but still has a nicardipine drip running. The objective
of this evaluation is to find any barriers, such as inconsistency with blood pressure parameters
being documented in orders or oral agents not being started in a timely manner delaying
transition of the patient from neuroICU status to floor status or discharge. The cost of using
premixed bags versus mixing in the pharmacy will also be determined.
Methods: A retrospective chart review will be conducted to collect data on the use of
nicardipine in the neuroICU before and after the clinical pharmacist educated medical residents
about the importance of including parameters in nicardipine orders and prn IV orders for
hydralazine and labetalol. Data to be collected includes patient demographics (age, gender, race),
indication for nicardipine (i.e. intracranial hemorrhage, ischemic stroke, etc), duration of
infusion, documentation of blood pressure parameters in orders, and start of oral blood pressure
medications. The number of bags used for each patient will also be collected. Patient information
will be accessed using the hospitals electronic medical record system. All patient identifiers will
be removed and data will be kept confidential to protect patient privacy. This project is part of
the health system Medication Use Evaluation (MUE) and Improvement program, which has been
approved by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-188
Title: Factors influencing 30 day readmission to an inpatient psychiatric service at a 600 bed
tertiary care teaching hospital
Primary Author: Marjorie Sen, Mercer University, GA;
Email: marjorie.sen@live.mercer.edu
Additional Author(s):
Peterson Worrell
Klugh Kennedy
Purpose: Psychiatric patients are frequently readmitted to inpatient facilities shortly after
discharge. One goal of many for hospital stays is to reduce early readmission rates (within 30
days), both to improve quality of care and because of financial concerns. The purposes of this
study are to examine patient demographics and other factors that may be contributing to early
readmission.
Methods: This study is a retrospective medical records review. Patients will be evaluated for
discharge from and subsequent readmission to the psychiatric service within 30 days, starting
May 2012 and ending in April 2013. Data collected will include age, gender, diagnosis, disease
severity as defined by Global Assessment of Functioning score, substance abuse, social support,
homelessness, history of previous admissions, length of stay (LOS), payor status, location of post
discharge care, outpatient treatment, and night/weekend admissions. We will also evaluate
medications and compliance. De-identified patient data will be securely stored in order to protect
patient confidentiality. Descriptive statistics will be used. This study was submitted to the local
Institutional Review Board for approval.
Results: During this timeframe, there were 111 readmissions within 30 days to the inpatient
psychiatric service. The median community tenure (time between discharge and readmission)
was 12 days. Half of the study population was Caucasian and half was African American, 52%
was male. Patient ages ranged from 20-61, with a mean age of 43 years. The mean LOS was 9
days. 55% of patients were diagnosed as schizophrenia spectrum, 43% as mood disorder, and 2%
as other, including PTSD and mood disorder secondary to substance use. On readmission 68%
presented as psychotic, 58% reported suicidality, and 7% were manic. Antipsychotic medications
were used in 98% of schizophrenia spectrum and 60% of mood disorders. 46% of readmissions
had substance use disorder. Substance use was not related to community tenure or LOS but was
related to mood disorder. 26% were homeless, and of those 72% reported suicidality. 78% were
on Medicaid. Among those with documented prior inpatient history, 92% were previously
admitted to the regional state psychiatric facility. 15% were documented to be compliant with
medication therapy. 55% were known to be noncompliant; however for a significant proportion
(30%), there was no documentation in the medical records regarding compliance during
community tenure.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: We attempt to identify characteristics that result in early readmission. Our plan is to
follow up this study with a covariate analysis and then a retrospective comparison to a propensity
score matched group with community tenure greater than 30 days.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-189
Title: Gap analysis of a large community hospital's sterile preparation compounding practices
compared to new guidelines
Primary Author: Blake Shay, Mercer University College of Pharmacy and Northside Hospital,
Georgia;
Email: blakeshay2014@gmail.com
Additional Author(s):
Sarah Murphy
Purpose: Sterile compounding has become a critically important topic in hospital pharmacy
today. The objective of this quality improvement study is to develop a gap analysis between
current sterile compounding processes and practices at a large community hospital and new
guidelines for safe preparation of sterile compounds set forth by the Institute for Safe Medication
Practices (ISMP). An in depth comparison and evaluation will be completed to see if the hospital
is fulfilling the 14 core processes stated in the guidelines.
Methods: The Institutional Review Board determined this project to be exempt prior to data
collection. A gap analysis will be performed comparing the current sterile preparation processes
at a large community hospital to the 14 core processes found in the new ISMP guidelines. The
analysis will look at the hospital's written policies and procedures as well as current practices by
staff to see if they meet the new ISMP guidelines. The 14 core processes being analyzed will
include policies and procedures, order entry and verification, drug storage, assembling products
and supplies, compounding, drug conservation, preparation of source or bulk containers,
technology and automation used, IV workflow software, automated IV compounding devices,
quality control and final verification, product labeling, record keeping, and staff management.
Data assessment will evaluate whether the hospital meets each core process and to what extent
based on the guidelines. A review of policies and procedures will be conducted for each core
process to analyze whether the hospital has a written guideline or if the core process is met due
to an agreed upon standard of practice by staff. An action plan and corrective measures will be
formulated for every core process that is not fully met.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-190
Title: Comparison of dispensed medications and healthcare costs between the United States and
Honduras
Primary Author: Indu Shekar, Mercer University College of Pharmacy, Georgia;
Email: indu.shekar@live.mercer.edu
Additional Author(s):
Purpose: To evaluate the disparity in healthcare costs between Honduras and the United States
based on the data that was collected from Mercer on Missions time in country.
Methods: To keep track of our inventory of drugs at the end of every clinic day, we collectively
decided to make a tally of drugs as they were being dispensed. A count was taken each day
regarding the number of disease states to determine the kinds of conditions to which they were
routinely being exposed.
Results: The total amount of prescriptions that we filled during our 8 clinic days in Honduras
totaled 2,227 and we saw 764 patients. On average, this calculates to approximately 278
prescriptions a day. About 25% of the prescriptions were for pain whether it be for joint pain,
headaches or muscle pain. The most common analgesic that was dispensed was Tylenol followed
closely by Ibuprofen. The next most common class of drugs that were dispensed was the
antimicrobials which encompassed approximately 13% of the prescriptions that that were
dispensed. It is also important to note that because of our limited formulary, not all disease states
could be addressed. Out of all the medications that we had in stock, the number of analgesics far
outweighed the rest of the drugs, therefore, pain was primarily treated for in our patients.
Conclusion: The affluence of the United States perhaps creates an environment when too many
medications are available for the public that Americans are being questioned whether certain
health privileges are even necessary. Whereas, since the Hondurans had to ration their funds for
care, their costs for healthcare were naturally lower. From studying the way Hondurans treat
healthcare, they seemed to be very simple people who had very basic problem states such as
pain.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-191
Title: Pharmacists' role in improving health through implementation of an employee wellness
and disease management program
Primary Author: Emily Smith, University of Georgia College of Pharmacy, Georgia;
Email: emilysmith137@gmail.com
Purpose: The wellness program was created in an effort to reduce health care costs, prevent
disease progression, and increase employee health awareness. Disease management and
medication reconciliation both play a major role in accomplishing these goals. Pharmacists
possess a wealth of knowledge in these areas, and were a key asset in implementing and
sustaining the program. Pharmacists had the opportunity to provide medication education,
optimize dosages, help identify and avoid side effects, and prevent drug interactions to name a
few. This study was constructed to gauge the benefit that pharmacists had on the participants
health.
Methods: Any hospital employee or dependent diagnosed with diabetes, hypertension, or
hyperlipidemia had the option of making an appointment with a care manager, which was either
a pharmacist, physician, or fourth year pharmacy student. At each appointment with a care
manager, laboratory values and vital signs such as total cholesterol, LDL cholesterol, HDL
cholesterol, triglycerides, blood glucose, hemoglobin A1c, blood pressure, heart rate, and weight
were assessed. In addition, employees were screened for drug interactions, medication
compliance, vaccinations, and coronary heart disease risk factors. Disease state education was
given, and information regarding lifestyle modifications was included. At the end of each
appointment, employees came up with a personal goal to achieve. If lab results from these visits
were within normal limits, or they were not currently taking medications for their disease state,
the patient would be seen on an annual basis. Patients were seen every six months if their lab
values were not at goal. If a patient presented with values that were elevated to a point where
intervention was necessary, they were referred to their primary care physician. If employees did
not have a primary care physician, they were referred to the physician care manager.
Results: Two hundred and forty five employees and dependents were enrolled in the wellness
program. The following results were collected over a period of five months. Thirty-seven were
diagnosed with diabetes and the average hemoglobin A1c level was 8.33 percent during the first
month, which fell to 7.73 percent in the last month (goal is less than 7 percent). One hundred and
twelve were identified to have hypertension. The average blood pressure increased from
132.92/78.81 mmHg at baseline to 133.18/80.73 mmHg, however, it remained at goal (goal is
less than 140/90 mmHg). Ninety-six participants had hyperlipidemia. The average total
cholesterol decreased from 209.65 to 205.55 mg/dL (goal is less than 200 mg/dL), LDL
cholesterol decreased from 128.26 to 125.27 mg/dL (goal is less than 130 mg/dL), HDL
cholesterol decreased from 50.33 to 49.4 mg/dL (goal is greater than 40 mg/dL), and the
triglyceride level decreased from 138.4 to 136.54 mg/dL (goal is less than 150 mg/dL). There
were eighteen interventions made by the pharmacist and pharmacy student including but not
limited to dose changes, primary care physician referrals, and medication refills. The program
also identified the absence of health awareness in these individuals.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Disease management can be a slow process. Reversing what have often been many
years of poor health habits is not easy and in order to make a greater impact, the wellness
program should be continued. Not only was the need for disease management revealed at this
site, but the potential value of the pharmacist and pharmacy students participation was also
demonstrated. Programs similar to the wellness program could be potential career paths for
pharmacists and open new avenues to the pharmacy profession.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-192
Title: Cisplatin hypersensitivity reaction: a case report
Primary Author: Kirbie St. James, Philadelphia College of Osteopathic Medicine, Georgia
Campus;
Email: kirbiegu@pcom.edu
Additional Author(s):
Allison Corlew
Soo Kim
Chad Weinhold
Jennifer Andres
Case Report: The following case describes an adverse drug reaction of fever, rash, hypotension,
and tachycardia resulting from a cisplatin infusion. TP is a 54 year old male who presented to
the emergency department with a temperature of 102.8 degrees Fahrenheit, non-pruritic rash on
his left arm which spread to his chest, back and legs, blood pressure of 95/58 mmHg, and pulse
of 118 beats/min, following an infusion of cisplatin. His chemotherapy consisted of cisplatin at
70 mg/m2 every 21 days for 3 cycles and a total of 33 radiation treatments to treat his squamous
cell carcinoma of the head and neck. There was no report of adverse events following the initial
cisplatin infusion (day 1). Before presenting to the ER, TP had received his second dose (day
22) of cisplatin along with a premedication regimen consisting of fluids, dexamethasone,
ondansetron, and aprepitant.
TP reported a fever starting around 4 pm that afternoon that peaked at 103.3 degrees Fahrenheit
around 3 am the next morning, following the second dose of cisplatin. He also reported a rash
developing a few hours after the fever. He stated the rash originated in his left arm before
spreading all over his body. He denied any soreness, pain, or itching associated with the rash.
After arriving to the ER, he remained febrile with a temperature of 102.8 degrees Fahrenheit as
well as hypotensive and tachycardic. He was promptly treated with fluids, acetaminophen,
ketorolac, diphenhydramine, levofloxacin, vancomycin, and was admitted to internal medicine.
Over the next few days his symptoms resolved, but he remained hospitalized for other
complications.
The presented case is likely due to cisplatin therapy. The platinum-containing chemotherapeutic
agents, including cisplatin, are considered high-risk drugs for the development of
hypersensitivity reactions, which can range from mild itching and flushing to anaphylaxis.
Although rare, reactions are unpredictable and may cause serious symptoms and illness in
patients.
Several treatment strategies may be employed to decrease the possibility of both mild and severe
adverse events including pre-medicating with corticosteroids and antihistamines, slowing the
infusion rate, implementing desensitization protocols, administering skin tests, and selecting an
alternate agent. Although these strategies have shown some success, they are not proven to
eliminate the potential dangers associated with cisplatin. Due to these findings, it is advisable
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
that physicians use caution when administering cisplatin and other platinum agents and be aware
that a reaction may occur.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-193
Title: Assessment of time to first dose administration of antibiotics with an urgent priority order
status
Primary Author: Christopher Stiles, The University of Georgia - College of Pharmacy,
Georgia;
Email: stilesc@rx.uga.edu
Additional Author(s):
Tim Robinson
Purpose: Timely administration of antibiotics to patients with severe infections can significantly
improve overall outcome. There are a number of factors which may delay the processes of
preparing and distributing urgent first doses. The purpose of this Medication Use Evaluation
(MUE) is to assess the time from order to administration of the first dose for urgent antibiotic
orders in the adult hospital of an academic medical center and to subsequently consider major
contributing factors that delay the process.
Methods: A retrospective electronic medical record review will be conducted for 100 adult
inpatients who were ordered an urgent first-dose antibiotic in August 2013. Data collected will
include patient location, infection, presence of sepsis notifications generated by the clinical
information system, time of order, time of pharmacist verification and time of first dose
administration. Mean time to administration and standard deviation will be calculated for each
location and by medication. This project is part of the health system MUE and Improvement
program, which has been approved by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-194
Title: Best Practices in Tapering Methods in Patients Undergoing Opioid Therapy
Primary Author: John Suttner, Mercer University, GA;
Email: johnhsuttner@gmail.com
Additional Author(s):
Annesha Lovett
Kimberly Vernachio
Purpose: The prescribing of opioids for chronic non-cancer pain has escalated over recent years.
This pattern has led to a larger number of patients who inevitably require de-escalation or
discontinuation of opioid therapy. The purpose of this review was to provide an overview of best
practices for tapering opioid therapy in patients.
Methods: A systematic review of the current literature concerning tapering of opioid therapy
was performed from 2000-2013 utilizing PubMed, Ovid, Google Scholar, and Cochrane Library.
The search terms were opioid, opioids, taper, tapering, detoxification, detox, dependence,
withdrawal, and weaning. Studies cited in the bibliographies produced by these searches were
also included in the review. Articles were selected based upon relevance and quality and
included narrative and systematic reviews, prospective and retrospective studies, and clinical
guidelines from US government agencies and expert panels. Articles were summarized in a table
based upon year of publication, author, title, study design, methods, findings, and source.
Results: After the exclusion criteria were applied to the search results, 24 studies were selected
for review. Considerable variation was found with regard to taper rate and duration. Taper rate
ranged from an initial 20-50% daily reduction in opioid dose to a 5% reduction in dose every one
to four weeks. The most common titration rate was a 10% reduction in the daily dose each day.
Duration in the reduction of doses ranged from to two weeks to three to four months. General
themes were to individualize taper parameters to ensure patient compliance and presentation of
withdrawal symptoms, to slow the rate of the taper at 1/3 or 20% of the original dose, to be able
to slow the tapering if necessary, and to switch patients from short-acting to long-acting
medications. Studies were also consistent in advising a referral of addicted and complex patients
to appropriate specialists for treatment.
Conclusion: The majority of available information on tapering opioid therapy consists of clinical
guidelines that have been created based on practice experience. There is a need for additional
experimental research to develop a more standardized taper protocol.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-195
Title: Evaluation of supplemental insulin use in pediatric patients at a children's medical center
Primary Author: LeeAnn Thompson, University of Georgia College of Pharmacy, Georgia;
Email: leeannt89@gmail.com
Additional Author(s):
Kalen Manasco
Purpose: Our children's hospital does not currently have a computerized physician order entry
hyperglycemia order set in place for dosing supplemental insulin in the pediatric population.
Doses are ordered on an as needed basis according to the point-of-care glucose readings and
patient-specific correction factors. Because timely administration of insulin and control of
hyperglycemia can affect patient outcomes, an evaluation will be conducted of supplemental
insulin use and the timeliness of insulin administration in comparison to the blood glucose
reading.
Methods: A retrospective analysis will be conducted on a random sample of pediatric inpatients
that received insulin therapy during August 2012 - July 2013. Data collected will include
demographics (age, gender, race), location of admission, length of hospital stay, underlying
disease states, home medications, supplemental insulin use (time of blood glucose drawn, time of
order sent, time of insulin given), and documentation of endocrinology consult. This project is
part of the health system Medication Use Evaluation (MUE) and Improvement program, which
has been approved by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-196
Title: Evaluation of intravenous phosphorus supplementation use in the intensive care units at an
academic medical center
Primary Author: Caroline Traylor, University of Georgia College of Pharmacy, Georgia;
Email: traylorc@mail.rx.uga.edu
Additional Author(s):
Kevin Corbin
Purpose: Hypophosphatemia is a serious condition often seen in patients receiving treatment in
intensive care units (ICU). The use of intravenous (IV) phosphorus supplementation in these
patients plays an important role in patient care. Due to recent shortages of this electrolyte, it is
more important than ever to ensure those who need the supplement the most receive it.
Conducting this evaluation will ultimately show if the institution is providing treatment to those
who need it most based on this center’s current guidelines.
Methods: A retrospective chart review will be conducted on the use of IV phosphorus
supplementation in ICU patients during August 2013. Data to be collected will include patient
demographics, indication, dose given and duration of use. Whether or not phosphorus levels
were monitored 12-24 hours post administration will also be evaluated. The appropriate use of
the drug will be judged using the lab values for serum phosphorus prior to administration and
current institutional guidelines. All patient identifiers will be removed, and data will be kept
confidential to protect patient privacy. This project is part of the health system Medication Use
Evaluation (MUE) and Improvement program, which has been approved by the institutional
review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-197
Title: Evaluation of treatment outcomes for Clostridium difficile at a large academic institution
Primary Author: Liana Tyson-Haynes, Mercer University College of Pharmacy, Georgia;
Email: liana.tyson-haynes@live.mercer.edu
Additional Author(s):
Saira Rab
Marina Rabinovich
Purpose: Clostridium difficile is the most common cause of hospital-associated infectious
diarrhea. Studies have associated Clostridium difficile infection (CDI) with increased costs and
length of hospital stay. In 2010, SHEA and IDSA published the Clinical Practice Guidelines
Update on the management of CDI based on severity of the disease. The purpose of this study is
to evaluate current practices and compliance with protocol for the treatment of CDI at a large
academic institution and to identify opportunities to improve patient outcomes and potentially
decrease costs associated with CDI.
Methods: An investigational review board approved this retrospective, quality improvement
project. A clinical surveillance software system, Theradoc, will identify patients with a positive
C. difficile test from January 1 through May 31, 2013. Patients will be included if they have a
stool test positive for C. difficile or its toxins and the presence of diarrhea. The primary objective
is to evaluate the response to treatment of CDI (success, failure, or relapse). The secondary
objectives include evaluation of: compliance with guidelines for treatment of CDI based on
disease severity, readmission rates for CDI recurrence, length of hospital stay, mortality at 28
days or at time of discharge, and discontinuation of empiric concurrent antibiotics after initiation
of treatment for CDI. Additional data that will be collected includes: demographics, presence of
CDI on admission, initial or recurrent CDI, place of residency prior to admission, disease
severity, antibiotic exposure within 28 days of CDI, concurrent use of antibiotics for other
disease states, concurrent use of proton pump inhibitors, laboratory data, vitals, and readmission
rates. All patient information will be de-identified and each patient will be assigned a unique
identifier. The anticipated sample size is 200 patients.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-198
Title: Subtherapeutic INR levels associated with concomitant phenytoin and warfarin therapy
Primary Author: Saranya Venkatachalam, University of Georgia College of Pharmacy,
University of Georgia College of Pharmacy (Athens, GA);
Email: vsaranya710@gmail.com
Additional Author(s):
Amy Bishara
Stephanie Phan
Carolyn Hunter
Purpose:
Methods:
Results:
Conclusion:
Case Report: Phenytoin and warfarin demonstrate a complex and unpredictable drug interaction
that result in alterations of the international normalized ratio (INR). Patients initiated on both
drugs may have an increased risk of bleeding because phenytoin can displace warfarin from
protein binding sites. However, these patients may ultimately require increased warfarin doses
due to increased warfarin metabolism from long-term phenytoin therapy. Most case reports
document that concomitant phenytoin and warfarin therapy typically presents with
supratherapeutic INR levels, an increase in the hypoprothrombinemic response, and hemorrhagic
adverse effects. A 47-year-old female was admitted for suicidal ideation with laceration on her
wrists and complaints of leg swelling. Her past medical history included recurrent deep vein
thromboembolism (DVT), seizure disorder, cocaine dependence, bipolar disorder, and a history
of small bowel resection. Upon hospitalization, she was initiated on enoxaparin 60 mg twice a
day for confirmed DVT. She received a one-time dose of warfarin 10 mg and was continued on
warfarin 5 mg daily. Several home medications, including phenytoin 400 mg orally at bedtime,
were restarted. Her medication adherence prior to admission was questionable as she had an
active prescription for warfarin 5mg daily, yet the INR was normal at 1.02. By day 3, the INR
slowly trended upwards to 1.21 and the warfarin dose was increased to 10 mg daily. At day 4,
the INR decreased to 1.01 despite a dosage increase. The patient reported consistency with diet,
denied any vomiting or diarrhea, and medication adherence was documented. Her INR continued
to fluctuate slightly from 0.97 to 1.1 for four more days and she was subsequently given warfarin
15 mg. The next day, her INR increased significantly to 1.49 and the warfarin dose was adjusted
to 12.5 mg daily. A therapeutic phenytoin level of 15.3 mcg/mL (albumin 3.6 g/dL) was reported
on day 9. Other known causes of persistently subtherapeutic INR could not be identified, though
impaired absorption due to the patients history of small bowel resection was considered.
Additional relevant medications received throughout hospitalization included ciprofloxacin,
metronidazole, atenolol, esomeprazole, mirtazapine, sertraline, fluoxetine, duloxetine, trazodone,
tramadol, and acetaminophen, which have been theorized to potentiate effects of warfarin. On
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
day 13, the patient complained of numbness, tingling, and difficulty closing her hands. Nurses
noted a blue discoloration from the palms to the sides of the hand. These symptoms suggested
possible purple glove syndrome, a rare cutaneous adverse effect that usually results from
intravenous phenytoin, though one case report has documented the occurrence with oral
overdose. Alternatively, warfarin has been associated with purple toe syndrome which is
characterized by a painful purple, mottled coloring that waxes and wanes, is cool to touch, and
thought to be due to cholesterol microemboli or warfarin toxicity on capillaries. The syndrome
may also occur in the upper extremities, however, usually appears after several weeks of
warfarin therapy. The patient also had increased liver transaminase levels and gamma-glutamyl
transpeptidase, which may be associated with phenytoin use. Phenytoin was switched to
levetiracetam, and following discontinuation, the patient noted the symptoms related to her hand
to be better. Thus, warfarin induced purple toe syndrome is less likely, though caution should be
exercised with associating the adverse effect to phenytoin alone. The day after phenytoin was
discontinued, the INR increased from 2.40 to 3.37 and warfarin was reduced to 10 mg daily. On
the last in-patient day, INR was 2.32 and patient was discharged on warfarin 10 mg daily to an
outpatient pharmacist-managed warfarin clinic. Eight days after discharge, the INR was stable at
1.9. This case demonstrates that persistently subtherapeutic INR may occur despite dosage
increases with concomitant warfarin and phenytoin therapy.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-199
Title: Pharmacy student perceptions regarding understanding of and confidence in literature
evaluation following a student chapter journal club
Primary Author: Matthew Wallace, Mercer University College of Pharmacy, Georgia;
Email: matthew.david.wallace@live.mercer.edu
Additional Author(s):
Katherine Brumfield
Kimbria Brown
Maria Miller Thurston
Melissa M. Chesson
Purpose: Journal club and literature evaluation are key components of Advanced Pharmacy
Practice Experiences (APPEs), residencies, and clinical practice as a whole. The purpose of this
study is to determine whether students had perceived benefits, such as enhanced confidence in
discussing and analyzing primary literature, as a result of participation in a student chapter
facilitated journal club activity.
Methods: This study has been approved by the Institutional Review Board. Student members
will be asked to volunteer for the study and complete a pre- and post-survey regarding their
confidence in and understanding of primary literature. Informed consent will be obtained through
an online pre-survey. A Likert scale will be used to collect data on topics such as identifying
pertinent background information, understanding statistics, and assessing clinical significance of
a study. Students will be asked to evaluate a selected article using guidelines and a provided
template. Subsequently, students will engage in a discussion about the article with a pharmacist
facilitator prior to completing a post-survey. The results of the two surveys will be compared to
see if participation in the journal club changed perception of confidence and/or understanding
regarding evaluation of primary literature. Participant responses will be recorded without
identifiers to maintain confidentiality, but the results will be paired based on unique
identification numbers. The proportion of responses in each Likert scale category will be
compared between the pre- and post-surveys to assess if students perceived a change in their
understanding and confidence in literature evaluation from participation in the journal club.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-200
Title: Characterization of thirty-day readmission risk for patients with acute myocardial
infarction and pneumonia at an urban community hospital
Primary Author: Marina Ward, Mercer University COP, Georgia;
Email: Marina.Ward@live.mercer.edu
Additional Author(s):
Pamela Moye
Teresa Pounds
Purpose: Hospital readmissions are perceived as an indicator of poor hospital care and missed
opportunities for clinical interventions. They also impact hospitals financially since federal
programs started to modify hospital reimbursements based on their performance. Measuring and
improving hospital quality of care, outcomes of care in particular, is essential in order to
maximize quality of care during initial admissions and to prevent subsequent readmissions. The
purpose of this study is to identify patients who are at highest risk for readmission after initial
hospitalization to the Atlanta Medical Center (AMC) with a primary diagnosis of acute
myocardial infarction (AMI) or pneumonia.
Methods: This study is a retrospective chart review of patients admitted to AMC over a time
period of 6 months with a primary diagnosis of AMI or pneumonia. Both AMC and Mercer
University Investigational Review Boards approved this project. All emergency room and
hospital admissions were screened for the targeted disease states as well as inclusion and
exclusion criteria. Inclusion criteria are as follows: admission from January 1, 2012 to June 30,
2012 for pneumonia and/or AMI as identified by the daily Evidenced Based Medicine report.
The study sample consists of 33 AMI patients and 215 pneumonia patients. Data collection is
related to basic patient population demographics, primary diagnosis, length of hospital stay,
comorbidities, baseline laboratory values, smoking and alcohol history, medications prescribed,
and other interventions. SPSS 12.0 software will be used to conduct statistical analysis.
Demographical data will be analyzed using descriptive statistics. Categorical and continuous data
will be analyzed using Chi- Square and Student t-tests, respectively. At its completion, the study
will determine what percentage of the patients were readmitted to AMC within 30 days, identify
reasons for readmission, and evaluate readmitted patients for similarities in demographic
characteristics, comorbid conditions, and discharge medications.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-201
Title: Effect of factor eight inhibitory bypassing activity (FEIBA) on international normalized
ratio (INR) in patients actively bleeding while on concomitant warfarin therapy: a retrospective
study
Primary Author: Misty Warthen, South University School of Pharmacy, Georgia;
Email: mlh0131@gmail.com
Additional Author(s):
Christina A. Smith
Lilia Z Macas-Moriarity
Lauren Garton
Jack Dean
Purpose: Patients on warfarin are at an increased risk for bleeds that can become life-threaten if
the INR is not reversed. Currently, vitamin K and fresh frozen plasma (FFP) are the
recommended agents to reverse an INR. FEIBA is an anti-inhibitor coagulant complex that
consist of mainly non-activated factors II, IX, X and mainly activated factor VII. FEIBA has
been reported to be effective in correcting an international normalized ratio (INR) while
overcoming limitations that exist with FFP. This retrospective study is designed to report the
experience of FEIBA use within a four hospital tertiary health care system.
Methods: A retrospective chart review was conducted for all patients with an active bleed who
received FEIBA between October 2008 and April 2013 following institutional review board
(IRB) approval. Inclusion criteria were to have a diagnosed active bleed, warfarin therapy for 3
or more days prior to the bleed, and administration of FEIBA. The primary outcome is to identify
time taken to change INR from baseline to a target INR of </= 1.5. The sample is stratified into
two groups, those whose INR baseline was < 3 and those whom baseline INR was >/= 3. The
INR to first reach 1.5 or less post FEIBA administration was recorded along with time of INR
from FEIBA administration. The two groups were further stratified into two time intervals of <1
hour or 1-24 hours. For each group, a Wilcoxon signed rank test will be utilized to identify
statistically significant differences between baseline INR and first to target INR, with an alpha
level set at 0.05. Secondary outcomes include percent survival at discharge and median length of
stay in hospital.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-202
Title: Cost avoidance of using an automatic therapeutic interchange of racemic albuterol in place
of levalbuterol
Primary Author: Chad Weinhold, Philadelphia College of Osteopathic Medicine, Georgia;
Email: chadwe@pcom.edu
Additional Author(s):
Christopher Holaway
Purpose: To determine if any cost avoidance would occur by utilizing an automatic therapeutic
interchange of racemic albuterol for levalbuterol in a health system.
Methods: An annual drug usage evaluation for levalbuterol 0.625mg and 1.25mg was completed
for the time period of January 1, 2012 through January 31, 2013 across all patient populations.
The annual cost avoidance of automatically substituting racemic albuterol in place of
levalbuterol was determined by comparing the purchase costs and usage of levalbuterol 0.625mg
and levalbuterol 1.25mg against the purchase costs of racemic albuterol 1.25mg and racemic
albuterol 2.5mg. Racemic albuterol is a 50:50 mix of R- and S-enantiomers, whereas levalbuterol
includes only the R-enantiomer. The consensus standard of substitution of racemic albuterol for
levalbuterol occurs with a 2:1 ratio (e.g. albuterol 2.5 mg for levalbuterol 1.25 mg and albuterol
1.25mg for levalbuterol 0.625mg). Cost avoidance in this study was calculated using this ratio
for substitution. Additionally, the cost avoidance at conversion rates between 70% through 100%
was calculated, as obtaining full conversion of levalbuterol to racemic albuterol may be
unrealistic.
Results: There was a total of 15096 units of levalbuterol 0.625mg and 17214 units of
levalbuterol 1.25mg used in the specified time period at an annual spending of $49816 and
$68823, respectively. At a conversion rate of 70% up to the full conversion rate of 100%, total
cost avoidance was in the range of $71186 to $101695.
Conclusion: The automatic therapeutic interchange of racemic albuterol in place of levalbuterol
in a health system yields an annual cost avoidance from $71186 to $101695, depending on the
annual rate of conversion. A protocol for automatic therapeutic interchange of racemic albuterol
for levalbuterol can offer substantial savings, even at conversion rates of less than 100%.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-203
Title: Inappropriate use of proton pump inhibitors in a psychiatric clinic and its cost implications
Primary Author: Eddie Williams, Philadelphia College of Osteopathic Medicine, Georgia;
Email: eddiewi@pcom.edu
Additional Author(s):
Mebanga Ojong
Shari Allen
Hongjun Yin
Purpose: Inappropriate use of medications causes harm to patients and is an economic loss to
society. There are four objectives to this study: the first is to find out the prevalence of
inappropriate use of proton pump inhibitors (PPIs) in psychiatric patients; the second objective is
to examine factors that are associated with the inappropriate use of PPIs in psychiatric patients;
the third objective is to develop protocol for appropriate use of PPIs in psychiatric patients; and
the final objective is to estimate cost saved if inappropriate use is avoided.
Methods: The study has been approved by the Institutional Review Board. A cross-sectional
study will be conducted. Psychiatric patients 18 years or older will be included. Patients medical
records as well as a patient survey will be used to collect the data. Patients age, sex, types of
psychiatric condition, comorbidities, and medications prescribed will be collected. Based on a
power analysis, a sample size of 72 patients will be needed. Patients will be interviewed with a
standard set of questions. Then the prevalence rates will be examined: prevalence of PPI,
prevalence of PPI for an appropriately documented upper gastrointestinal tract diagnosis,
prevalence of PPI for symptomatic treatment based on extraesophageal symptoms, prevalence of
PPI for gastroprotection, prevalence of PPIs for no documented appropriate indication for PPI
therapy. An analysis will be conducted that will illustrate the amount of money saved from
avoiding the inappropriate use of PPIs. Statistical tests of correlation and regression will be
applied to examine the potential associations between age, sex, types of psychiatric conditions,
comorbidities, and the chance of inappropriate PPI use.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-204
Title: Outcomes evaluation of Clostridium difficile infections among patients treated with
fidaxomicin vs. standard treatment
Primary Author: Kara Williams, Mercer University, Georgia;
Email: karwill@gmail.com
Additional Author(s):
Vanthida Huang
Angelina Davis
Lisa Oakley
Purpose: Clostridium difficile, an anaerobic, Gram-positive bacillus, is one of the most
widespread causes of healthcare-related infection in the United States. The Society for
Healthcare Epidemiology of America and the Infectious Diseases Society of America published
practice guidelines for C. difficile infection (CDI) in 2010 with first-line treatment options being
metronidazole 500 mg PO q8h or vancomycin 125 mg PO q6h for 10-14 days. Fidaxomicin, a
bactericidal macrolide, was approved by the FDA in 2011 for treatment of CDI. The objective of
this study is to evaluate the outcomes of CDI among patients treated with fidaxomicin vs.
standard treatment.
Methods: This will be a retrospective cohort study of all patients with confirmed CDI infection
presenting in an acute setting. The study will take place in a not-for-profit organization
comprised of five community-based hospitals in metro Atlanta, Georgia. We will enroll 377
patients from January 2013 through December 2013. Electronic medical charts will be reviewed
and information collected for each patient from the time of presentation until discharge for all
initial and recurrent CDI. Patient demographics, antibiotics, and laboratory information will be
collected. Clostridium difficile-related factors and microbiologic results will also be reviewed
and collected. The primary endpoint will be the clinical cure as defined by clinical improvement,
with maintenance of clinical improvement for the duration of therapy and lack of persistent
infection with the requirement for additional therapy or modification in current therapy at the end
of treatment in each treatment arm. Secondary endpoints will be recurrence rates of CDI, time to
recurrence, length of stay, and severity of CDI. Categorical endpoints will be evaluated with the
chi-squared test. Student-t tests will be utilized for analysis of all continuous data. Statistical tests
will be 2-tailed and a P value of < 0.05 will be considered as statistically significant.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-205
Title: Antibiotic overuse in the transition of care from inpatient to outpatient
Primary Author: Lauren Willis, UGA College of Pharmacy, Georgia;
Email: willisl@uga.edu
Additional Author(s):
Chris Stiles
Lydia Im
J. Russell May
Purpose: Pharmacists have become vigilant stewards of antibiotic therapy in order to stay one
step ahead of evolving bacteria that continue to develop resistance to previously effective
antibiotics. Contributing factors to the development of antibiotic resistance include unsuitable
antibiotic choice and inappropriate treatment duration either in the form of reduced or prolonged
antibiotic administration. The purpose of this study is to investigate the duration of prescribed
antibiotic therapy following hospital discharge as compared to evidence based recommendations
in the duration of antibiotic therapy for specific infections.
Methods: Subjects included patients diagnosed with pneumonia, urinary tract infection,
diverticulitis, or cellulitis on general medicine units at Georgia Regents Medical Center from
June 6, 2013 to July 10, 2013. Patients had received antibiotics qualifying for pharmacy directed
intravenous to oral conversion while inpatient and were subsequently prescribed additional
antibiotic therapy upon discharge. Patients were excluded if they were positive for concomitant
immunosuppression, HIV infection, sepsis, or had received antibiotics simply for pre or post
surgical prophylaxis. Antibiotic duration in days and doses was calculated for each qualifying
inpatient and total duration was determined by combining inpatient duration with the number of
days and doses prescribed upon discharge from the hospital. These durations were compared to
published guidelines specific to the management of each disease. Preliminary data indicate that
total duration of antibiotic therapy exceeded published guidelines in the majority of cases
investigated. This project is part of the health system Medication Use Evaluation (MUE) and
Improvement program, which has been approved by the institutional review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-206
Title: Lung cancer after heart transplantation
Primary Author: Russell Wise, Mercer University, GA;
Email: russell.wise@live.mercer.edu
Additional Author(s):
Meredith Herndon
Diane Nykamp
Purpose:
Methods:
Results:
Conclusion:
Case Report: This case report describes the probable cause of squamous cell lung cancer
associated with immunosuppressant therapy following heart transplantation. Development of
cancer after long-term immunosuppressive therapy is a leading cause of morbidity and mortality
in heart transplant recipients. Lung cancer is one of the three most common types of cancers to
develop in this patient population. Lung cancer in heart transplant patients occurs with greater
frequency than in the general population, and malignancy is thought to be associated to the
greatest extent with calcineurin inhibitor (CNI) therapy.
A 64 year-old Caucasian male was diagnosed with squamous cell carcinoma of the right lung
after receiving 21 years of immunosuppressive therapy for his orthotopic heart transplant. The
patient presented to the emergency department with symptoms of right-sided chest pain,
productive cough, shortness of breath, and fever. The patient was admitted to the hospital for a
lower respiratory tract infection. Computed tomography (CT) angiogram showed a suspicious
right lower lobe 4-5 centimeter mass-like consolidation in the lung and bronchoscopy confirmed
squamous cell carcinoma. The Naranjo Scale indicated the likelihood of the immunosuppressant
therapy causing this adverse drug reaction (ADR) was probable.
In this patient, chronic immunosuppression along with other risk factors, such as male gender,
age greater than 60 years, and a history of pre-transplant smoking, may explain the development
of cancer. Prevention with cancer screenings is an important component of patient care after
heart transplant, especially in patients with a history of tobacco use. Cancer screening
recommendations for lung cancer range from regular chest x-rays to CT scans in high-risk
patients. Squamous cell cancer of the lung has a poor prognosis since detection is commonly
incidental and at an advanced stage when diagnosed. Long-term care of transplant patients
should include regular cancer prevention screening.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-207
Title: Evaluation of the use of liposomal bupivacaine for the management of pain in patients
undergoing video-assisted thoracoscopic surgery and spinal surgery in a community hospital
Primary Author: Ayberk Yenilmez, University of Georgia College of Pharmacy, Georgia;
Email: ayberkyenilmez@gmail.com
Additional Author(s):
NaaDede Badger-Plange
Leah Cochran
Purpose: The management of postsurgical pain is an essential part of the patients recovery
process. Adequate pain control has been shown to lead to better outcomes and faster recovery.
Although opioids are the mainstay of pain management, they continue to be associated with
unwanted and potentially severe adverse events. During the last decade the use of multimodal
pain management, especially in the peri-operative setting, has been utilized to minimize opioid
use in surgical patients. The purpose of this study was to determine the effectiveness of
liposomal bupivacaine in patients undergoing spinal and video-assisted thoracoscopic surgery as
compared with current practice.
Methods: This medication use evaluation was approved by the hospital's pharmacy and
therapeutics (P&T) committee. This was a single-center, retrospective and prospective
descriptive investigation, evaluating the use of liposomal bupivacaine in the two target
procedures performed by two specific surgeons, between March and July 2013. All patients who
received liposomal bupivacaine during this study period were included in the study. An equal
number of patients matched by surgical procedure were identified as a control group by the
electronic medical record system. The following data was collected: patient age; gender; length
of stay; pain scores (using Wong-Baker FACES pain scale) in post-anesthesia care unit and on
the nursing unit; pain medications received before, during, and after surgery; and any opioid pain
medications patient was taking prior to admission. All data was recorded in a data collection
form without patient identifiers to maintain patient confidentiality. The primary outcome was to
assess the need for post-operative opioid analgesia expressed in morphine equivalents. The
secondary outcomes were median pain score; difference in the length of stay; use of non-opioid
analgesia; readmission within 30 days due to surgical complications; and total hospital and drug
cost between the two groups.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-208
Title: Legionella pneumophilia on Kauai: a case report of an emerging pathogen or under
diagnosed condition?
Primary Author: Andrea Brauer, University of Hawai'i at Hilo Daniel K. Inouye College of
Pharmacy, HI;
Email: abrauer@hawaii.edu
Additional Author(s):
Michelle Kim
Jeremy Daube
Roy Goo
Sheri Tokumaru
Case Report: In March 2013, a 68 year old man reported to the emergency department
complaining of fatigue, myalgia, headache, hypoxia, nausea, diarrhea, and cough. Patient stated
he was a retired visitor from Colorado, vacationing on Kauai over the past two weeks. Upon
admission, preliminary chest x-ray readings showed scattered bilateral infiltrates. Subsequently a
urine antigen test for Legionella pneumophilia was taken. The patient was started on empiric
azithromycin with a single administration of ceftriaxone. On day 2, a chest x-ray was retaken
showing leukocytosis with a left shift and bilateral interstitial infiltrates. Patient was started on
meropenem, as well as solumedrol and levalbuterol, for his continued hypoxemia. On day 3,
results from the urine antigen assay returned positive for Legionella pneumophilia serotype 1.
Patients regimen was changed to levofloxacin and both azithromycin and meropenem were
discontinued. On day 6, patient was transferred to another hospital, and the Department of Health
was notified of the confirmed Legionella case; the first reported incidence of Legionella to
originate in Kauai. The incidence of Legionnaires' disease, in the United States, increased 192
percent from 2000 to 2009. No incidences were reported from Kauai prior to 2011, and only two
cases of Legionnaires' disease have been reported since; one in 2011 and 2012 respectively. The
latter two infections were contracted off island as deduced by the timing of onset of symptoms,
patient arrival date to Kauai, and Legionella's incubation period before onset of symptoms. Due
to Legionella's preference for colonizing man-made water systems, approximately 20 percent of
Legionnaires' disease is travel-associated; involving air conditioners and hot tubs found in hotels
and cruise ships. Despite the prevalence of hotels and high rates of visitation; in 2012, 8,028,744
and 1,084,681 people visited Hawaii and Kauai respectively, reported cases of Legionella in
Hawaii are some of the lowest in the nation. Hawaii's tropical climate was previously thought to
be a limiting factor; however, a 2011 study found the epidemiological features of Legionella in
Singapore, a tropical city-state, comparable to those in temperate climates. The possibility of
under diagnosis of Legionnaires' disease should be considered. Further research is required to
determine if routine testing for Legionella pneumophilia should be implemented on Kauai.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-209
Title: Identifying the rising risk of Staphylococcus aureus resistance posed to a community
hospital in Hawaii and the importance of compliance to national vancomycin guidelines
Primary Author: Sharon Lum, University of Hawaii at Hilo Daniel K. Inouye College of
Pharmacy, Hawaii;
Email: sdlum@hawaii.edu
Additional Author(s):
Laura Ota
Roy Goo
Eryn Kishimoto
Purpose: Methicillin-resistant Staphylococcus aureus (MRSA) is the most commonly isolated
antibiotic-resistant pathogen in US hospitals and poses a major therapeutic challenge for
clinicians. Vancomycin is the treatment of choice for MRSA infections, but requires frequent
therapeutic drug monitoring to ensure its safety and efficacy. In order to address the increasing
rates of Staphylococcal resistance, national guidelines were published to ensure appropriate
dosing and monitoring procedures for vancomycin. This study was designed to identify trends of
MRSA infections in a community hospital in Hawaii in order to provide insight on the
importance of compliance to national vancomycin therapeutic monitoring guidelines.
Methods: A PubMed database search of literature in English-language was performed using the
terms vancomycin, pharmacokinetics, Hawaii, methicillin resistant, vancomycin resistant, and
Staphylococcus aureus. Additional searches were also performed in the following peer-reviewed
journals: Pharmacotherapy, Journal of American Medical Association, New England Journal of
Medicine, and Clinical Infectious Diseases using the same search terms. These searches were
completed between September 8 and September 19, 2013. A total of six primary literature
articles, three secondary literature articles, and five tertiary literature articles were reviewed.
Hospital laboratory data from 2010 to 2012 was also reviewed.
Results: According to articles reviewed from the literature search, it was found that there are
growing cases of MRSA resistance to vancomycin in the United States. In 2010, the national
prevalence of MRSA infection in hospitalized patients was 66.4 per 1,000 inpatients. In Hawaii,
prevalence of MRSA infection is 65.5 per 1,000 inpatients. One case report from 2011
documented the first vancomycin-intermediate Staphylococcus aureus infection in Hawaii. No
case reports were found identifying vancomycin-resistant Staphylococcus aureus in Hawaii.
Laboratory data from 2010 to 2012 of a community hospital in Hawaii, found that of all
staphylococcal isolates, 40.2% (626), 36.5% (588), and 34.7% (589) were MRSA from 2010 to
2012, respectively. Out of a total 580 MRSA isolates identified from June 2012 to May 2013,
1.6% (9) exhibited a MIC &#8805;2 mg/L and 54.3% (315) exhibited a MIC &#8805;1 mg/L6.
Of the 315 isolates with a MIC &#8805;1 mg/L, 23 were cultured from the lungs.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Staphylococcus aureus resistance is on the rise in the United States. Such trends are
also prevalent in laboratory surveillance data from Hawaii hospitals. The evolving nature of
Staphylococcal resistance and the lack of available alternative therapies necessitate the need for
compliance to national guidelines.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-210
Title: Medication use evaluation of enoxaparin dosing in a rural hospital
Primary Author: Amanda Nicolas, Daniel K. Inouye College of Pharmacy, HI;
Email: amandarn@hawaii.edu
Additional Author(s):
Shanele Shimabuku
Melissa Yoneda
Audrey Kumasaka
Roy Goo
Purpose: The appropriate dose of enoxaparin in deep vein thrombosis prophylaxis is
controversial since the doses are fixed while enoxaparin dosing for the treatment of deep vein
thrombosis or acute coronary syndrome is weight-based. This review is to determine if deviation
from the manufacturers recommended dose of enoxaparin exists in a rural setting, and whether or
not it is associated with an increased incidence of either clots or bleeds.
Methods: Data was collected from April 1, 2013 to June 30, 2013 on patients given enoxaparin
for venous thromboembolism prophylaxis or treatment during hospitalization. Doses
administered in the emergency department and duplicate orders for a single patient were
excluded. From 322 patients, a random number generator was used to select 110 patients. Using
EPIC, the patients medical record number, gender, age, weight, date of administration with
corresponding serum creatinine, calculated creatinine clearance using the Cockcroft-Gault
equation, dose, frequency, and indication were recorded. The patients age and gender were
retrieved from the patient profile. Enoxaparin regimen was found in the medications tab, under
medication history. If the patient had multiple doses, reviewers randomly selected a day to
collect the correlating data. The date of administration and relative weight were gathered from
the medication history. Serum creatinine for that day was found under results review. Creatinine
clearance was calculated based on the data collected. Indication for enoxaparin was determined
with physician notes. The appropriateness of enoxaparin dosing was evaluated using the CHEST
guidelines and reported as "Y" for yes or "N" for no. If the dose was not appropriate, a chart
review was done to determine if any adverse events occurred.
Results: Of the 110 patients randomly reviewed, 15 patients (~14%) were given regimens that
deviated from manufactured recommending dosing. All 15 patients received enoxaparin for
venous thromboembolism prophylaxis. Fourteen patients were administered 30mg subcutaneous
daily, but could have been dosed with enoxaparin 40mg subcutaneous daily based on their
creatinine clearance. One patient was administered 40mg subcutaneous daily, but could have
been dosed with enoxaparin 30mg subcutaneous daily based on their creatinine clearance. Patient
profiles were reviewed for adverse events due to potentially inappropriate dosing of enoxaparin,
and it was found that there were no reported venous thromboembolic events or major bleeds due
to the under or over dosing of enoxaparin.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Enoxaparin dosing data from April through June of 2013 indicated that ~14% of
patients in a rural hospital received doses that were not consistent with current manufacturer
recommendations. This deviation from recommended dosing did not lead to an increase in
adverse events. Manufacturer recommended dose, patients weight, comorbidities, and overall
clotting/bleeding risk should be taken into account when using enoxaparin prophylactically. Our
review demonstrates that lower doses of enoxaparin may be appropriate for patients of advanced
age or low body mass index.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-211
Title: Novel pathogens in skin and soft tissue infections secondary to skin popping: a case report
Primary Author: KristiAnne Nishek, University of Hawaii at Hilo Daniel K. Inouye College of
Pharmacy, Hawaii;
Email: nishek@hawaii.edu
Additional Author(s):
Stephanie L. Sumner
Jenny Lee Ramos
Roy Goo
Jack Goldsberry
Case Report: Skin popping is a term that refers to the subcutaneous and/or intradermal injection
of illicit drugs. Some of the most popular drugs used in skin popping include opiates (heroin) and
stimulants (cocaine and amphetamine). A common practice in skin popping is to lick the
injection needle prior to injecting drugs into the skin, which introduces the potential for skin and
soft tissue infections (SSTI) caused by pathogens not normally associated with this type of
infection.
VM, a 62 year old male, reported to the emergency department with extreme pain (patient rated
10/10) on the left side of the body (left arm and chest area), cough, fever, and difficulty
breathing. The left and right arms had large and very painful, warm lumps. The patient had a
height of 68 inches, weight of 53.6 kilograms, and body mass index of 17.97 kilograms/meter
squared upon admission. Patients social history includes: smoking 0.25 packs of cigarettes/day
with a 3 pack year history, drinks 4.5 ounces of alcohol per week, and has ongoing substance
abuse issues including subcutaneous injection of crushed oxycodone for many years (referred to
as skin popping). Patients past medical history includes penicillin allergy that results in a rash,
diabetes mellitus type II, hypertension, chronic pain, and hepatitis C. Upon admission the patient
physically appeared to be thin with temporal wasting, looked chronically ill, and had multiple
skin abscesses likely related to the history of drug abuse. Chest examination revealed rhonchi
throughout with no wheezing; the abdomen was soft with some tenderness, but no rebound
guarding or rigidity; the patients extremities were thin without edema; during the neurological
exam the patient moved easily in bed without focal motor weakness. Blood cultures, CT of the
chest with IV contrast, ECHO, gram stain and cultures were ordered upon admission. Chest xray imaging showed evidence of bilateral lung base alveolar infiltrates with noted haziness and
left lung base effusion. Broad spectrum antibiotics ceftriaxone, vancomycin, and levaquin were
administered. Metronidazole was later added due to the presence of gas in the patients wounds
on the fourth day of treatment as wound and sputum cultures were positive of Klebsiella
pneumoniae. Although Klebsiella is a common pathogen in respiratory and urinary tract
infections, it does not commonly cause skin and soft tissue infections. Due to presence of lung
infiltrates along with sputum and wound cultures being positive for the presence of Klebsiella
pneumoniae, and in the absence of any other bacteria, it was concluded that this patients current
illness could be due to the patients skin popping practices of licking the needle prior to injection
which resulted in the introduction of Klebsiella pneumoniae into his wounds. Subsequently the
patients ceftriaxone, vancomycin and metronidazole were discontinued; however meropenem
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
was added out of concern for a sudden rise in white blood cells: 20.7. A thorcentesis was
performed due to suspected bilateral pneumonia. A right chest tube thoracostomy was performed
and a right subclavian triple lumen central line was placed on the tenth day of treatment due to
dyspnea, cough, hypoxia, and increasing pleural effusion. Patients symptoms improved after a
course of antibiotics (levaquin and meropenem). Pleural effusions decreased from day 11-16
(chest tube removed on day 16) and remained unchanged for the remainder of treatment. On day
25, the patients lungs were clear, had a pulse oximeter oxygen of 90 and denied dyspnea.
Patients skin abscesses caused by recent drug use healed to small scabs and no dressings were
necessary by day 26. The patient was discharged from the hospital after 27 days of treatment on
the basis of promising to attend a drug rehabilitation program.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-212
Title: Evaluation of controversial interactions with warfarin encountered in a pharmacist-driven
anticoagulation clinic in Hawaii
Primary Author: Jennifer Ota, University of Hawaii Hilo Daniel K. Inouye College of
Pharmacy, Hawaii;
Email: jeota@hawaii.edu
Additional Author(s):
Eryn Kishimoto
Sheri Tokumaru
Stacie Sakauye
Purpose: Warfarin is a common oral anticoagulant used in the United States for the treatment
and prevention of thromboembolisms. Warfarin has many interactions, which are well studied
and documented. However, a handful of interactions are poorly understood. This two-part
literature review and case report study evaluates three controversial warfarin interactions with
cranberry, mango, and non-steroidal anti-inflammatory drugs (NSAIDs), encountered at a
pharmacist-driven anticoagulation clinic in Hawaii. We review three clinic case reports that
provoke further research into these potential interactions. The purpose of this study is to provide
clinicians with possible explanations for INR fluctuations in otherwise stable warfarin patients.
Methods: A PUBMED search of literature in the English-language, between July 1-Aug 9 2013,
was preformed using terms including: warfarin, Coumadin, interaction, NSAIDs, ibuprofen,
mango, cranberry, mechanism, and acenocoumarol. 18 articles were reviewed; 5 case reports, 4
systematic reviews, and 9 study trials. Case reports of current clinic patients are included to
further illustrate the potential interactions between warfarin and NSAIDs. All warfarin vs.
NSAID case reports are first-hand documentations at a pharmacist-driven anticoagulation clinic
in Hawaii.
Results: Various hypotheses attempt to explain the interaction between warfarin and cranberry,
however a precise mechanism of interaction was not concluded. Many case reports show that
ingestion of copious amounts of cranberry may result in serious and sometimes fatal adverse
effects. One warfarin patient in a published case report passed from a fatal hemorrhage after
cranberry consumption. However, two evidence-based trials showed no significant change in
INR when warfarin was challenged with cranberry consumption. With regards to the warfarin
interaction with mango, one case report demonstrated an average INR increase of 38% in
patients who ingested mango fruit over a varied amount of time. There are no randomized trials
documented for this interaction. It is well known that NSAIDs cause an increased risk in
bleeding. However, it is less understood if NSAIDs also increase INR in stable warfarin patients.
In this case report, we evaluate an 89-year-old male, stable on warfarin, who presented with
increasing INR after starting naproxen therapy. Upon discontinuation of naproxen, his INR
normalized. Two case reports and one RCT, showed an increase in bleeding events and INR.
However, a second RCT showed no difference in INR.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: This literature review and case report study demonstrates cranberry, mango and
NSAIDs to be possible explanations for INR fluctuations in otherwise stable warfarin patients.
However, there is currently no direct evidence for a causal relationship between elevated INR on
warfarin and cranberry, mango, and NSAIDs. Additional studies, accounting for potential causes
of INR fluctuations, are necessary to demonstrate a definitive interaction between these
substances. We recommend monitoring patients cranberry, mango, and NSAID intake and
discontinuing ingestion if there is an unexplained fluctuation in INR.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-213
Title: Assessing treatment options and cost effective strategies for acute migraine headaches
Primary Author: Keri Oyadomari, University of Hawaii at Hilo Daniel K. Inouye College of
Pharmacy, Hawaii;
Email: kerio@hawaii.edu
Additional Author(s):
Denise Kobashikawa
Sheri Tokumaru
Eryn Kishimoto
Michelle Zacchetti
Purpose: Migraine headaches are a painful and often debilitating neurovascular disorder that can
significantly affect the quality of life of a patient. Approximately 30 million Americans suffer
from this chronic condition. Migraine headaches commonly present as a pulsating and disabling
pain often accompanied by nausea and vomiting causing many patients to warrant immediate
care. The goals of acute therapy include aborting pain and restoring the patients ability to
function. Our aim of this literature review is to compare treatment strategies and cost analysis for
acute management of migraines.
Methods: Extensive background research was conducted to find evidence that supports the
rationale and treatment strategies for acute treatment of migraines. A PubMed search was
conducted from 1990-2013 in the English language using MeSH terms migraine disorders,
therapeutics, adult, and pharmacology. We evaluated medications for abortive therapy and
addressed efficacy, safety and cost to aid in selection of an appropriate agent. Furthermore, we
performed a class analysis using primary literature of the serotonin-5HT1B/1D receptor-agonists,
prescription strength nonsteroidal anti-inflammatory drugs (NSAIDs) and a combination of
acetaminophen/aspirin/caffeine (Excedrin) to provide patient-specific guidance in agent
selection. In addition, we reviewed other supportive care measures and medications such as
antiemetics, dexamethasone, ergotamines, isometheptene compounds and intranasal lidocaine
that may be considered in acute treatment.
Results: Migraine headaches can be divided into mild to moderate and severe based on the
presentation of symptoms. Various literature supports the use of prescription strength
nonsteroidal anti-inflammatory drugs (NSAIDs) or a combination of
acetaminophen/aspirin/caffeine (Excedrin) as abortive therapy for an acute migraine. Given the
patients history of prior use, a serotonin-5HT1B/1D receptor agonist (triptan) may be considered
if initial abortive therapy fails to relieve pain. In the case of a severe acute episode, a migrainespecific medication such as a triptan may be considered as initial abortive treatment, taking into
consideration the patients comorbid conditions and history. In the case of both mild to moderate
and severe intensity migraines, if nausea and vomiting occurs an antiemetic such as
metoclopramide, promethazine, or prochlorperazine may be administered in the appropriate
dosage form. In an emergency, intravenous administration of antiemetics should be used as
warranted. In certain patient populations that cannot tolerate the suggested initial abortive
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
therapy, other agents such as dexamethasone, ergotamines, isometheptene compounds or
intranasal lidocaine may be considered for relief.
Conclusion: Migraine headaches prove to be a burden to society. They not only affect the
patient but also the families and caregivers of those involved. Evidence shows that initial
treatment in an acute migraine episode may necessitate immediate abortive therapy for maximum
benefits. Various studies demonstrate that optimal treatment can maintain a cost effective profile
without compromising the quality of care. Patients should be encouraged to get involved in their
migraine management to prevent future episodes and not only improve their overall quality of
life, but also decreases the incidence of readmission to the emergency department.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-214
Title: Developing the role of student pharmacists in palliative care teams
Primary Author: LaTasha Riddick, University of Hawaii at Hilo, The Daniel K. Inouye College
of Pharmacy, HI;
Email: riddick@hawaii.edu
Additional Author(s):
Samantha Hanabaga
Jack Goldsberry
Roy Goo
Lara Gomez
Purpose: Palliative Care refers to the comprehensive care and management of the physical,
psychological, emotional and spiritual needs of patients (of all ages) and their families with
serious and/or life-threatening illness. Medication therapy often plays an integral role in the
symptom management of these patients. The goal of this project was to develop the role of
pharmacy students in a multidisciplinary palliative care team at a small rural hospital. This role
would not only help decrease pharmacy workload, but would also provide students with valuable
training opportunities in this emerging field.
Methods: In May 2013, a multidisciplinary palliative care team was formed at a community
hospital on the rural island of Kauai, Hawaii (est. population 68,000). The team was comprised
of a palliative care physician, a hospice nurse, a pharmacy faculty member (pharmacist), a case
manager and a social worker, along with other ancillary members being involved as needed (i.e.
dietitian, wound care RN, etc.). Primary focus was on promoting a system of care that fosters
timely access to palliative care services. This includes: 1) optimizing symptom control and when
appropriate, functional status, 2) educating patients and family members to promote
understanding of the underlying disease process and expected course of illness, 3) educating and
mentoring staff, and 4) coordinating discharge planning to appropriate level of care in a timely
manner. In addition, student pharmacists were integrated into the team by assisting in literature
collection and review, as well as preparing draft medication use protocols, which were then
reviewed by the pharmacist for appropriateness and accuracy.
Results: Since the inception of the palliative care service, student pharmacists have helped draft
two new prescribing policies and an intravenous (IV) opioid titration protocol to optimize
symptom management. The new opioid prescribing guidelines and IV opioid titration protocol
discourages the use of vague, non-specific titration orders by providing specific guidance on rate
and intensity of titration while providing appropriate symptom management. The IV opioid
protocol allows for frequent breakthrough bolus doses, which increase in a manner proportional
to a patient's specific basal rate. Another policy pertaining to the off-label use of haloperidol IV
allows patients, who are on comfort care measures, to receive haloperidol to alleviate terminal
restlessness without the need for deep intramuscular injections. Student pharmacists assisted
physicians in calculating equipotent opioid doses and reviewed current literature pertaining to the
selection of opioids in patients with impaired renal or hepatic function. Additionally, students
helped identify and recommend novel routes of delivery and secure unusual formulations of
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
discharge medications to ensure optimal comfort for patients and a smooth transition out of the
hospital.
Conclusion: Integration of student pharmacists on a multidisciplinary palliative care team
provides valuable experiences for students to manage complex symptoms in severe and lifethreatening diseases. These experiences also provide exposure to unique patient care services
(i.e. spiritual, ethical, psychological and physical). Students contribute an essential element to
workforce productivity. In this emerging field, it is important to maximize pharmacist impact
and also prepare future pharmacists for these roles.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-215
Title: Developing student rotations in an innovative care transition model on Kauai
Primary Author: Michael Taylor, The Daniel K. Inouye College of Pharmacy - University of
Hawaii at Hilo, Hawaii;
Email: taylorme@hawaii.edu
Additional Author(s):
Roy Goo
Lara Gomez
Karen Pellegrin
Purpose: Regardless of the field students ultimately pursue, student pharmacists are expected to
be proficient in core competencies such as interpersonal communication skills, collaboration
with other healthcare providers, critical evaluation of medication therapy, familiarity with
medical charts, and understanding of the overall medical care for patients encompassing both
inpatient and outpatient experiences. The purpose of this project was to utilize the innovative
Pharm2Pharm model as a comprehensive experiential rotation that would develop all of these
universally required competencies.
Methods: To improve medication management, the University of Hawaii at Hilo College of
pharmacy Center for Rural Health Science received a CMS Health Care Innovation Award to
launch a new service model called Pharm2Pharm. The Pharm2Pharm program team consists of a
hospital-based consulting pharmacist collaborating with community-based pharmacists, to
identify drug therapy problems for patients most at risk when making the transition from the
hospital to home. Through pharmacist collaboration with physicians and their patients, this
service seeks to improve outcomes for those at risk of medication-related readmissions. Students
are trained in the standard operating procedures of the Pharm2Pharm enrollment process and
allowed to develop hands-on skills as they assist in the screening and interviewing of selected
patients. Under the strict guidance of a Pharm2Pharm site supervisor, the student interacts with
the patient, performing comprehensive medication reconciliation, communicating any
inconsistencies back to the medical team. The student is also responsible for following the
patient during the hospitalization and assisting in any clinical decisions that arise. Upon the
patients discharge, the supervised student performs extensive medication education for the
patient. The final step includes sending all relevant information to a community pharmacist who
will promptly follow up with the patient upon discharge.
Results: Since the Pharm2Pharm project in Kauai began enrolling patients on 04/01/13, there
have been fifteen students participating in the rotation that were fulfilling their required APPE
hours (fourth year of pharmacy school) and nine students participating in this rotation that were
fulfilling their required IPPE hours (second/third year of pharmacy school). These students
received the extensive training in the Pharm2Pharm standard operating procedures and have
successfully completed a rotation through the Pharm2Pharm model. Based upon student
evaluations, the students report gaining confidence in interpersonal communication skills,
collaboration with other healthcare providers, critical evaluation of medication therapy,
familiarity with medical charts, and understanding of the overall medical care for patients
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
encompassing both inpatient and outpatient experiences, which can be directly related to the
activities performed while operating in the Pharm2Pharm model.
Conclusion: In the rural county of Kauai in the State of Hawaii, where physician shortages are
having a large impact on the health-care of the residents, Pharm2Pharm is providing an
innovative, pharmacist-led care transition model. Pharmacy students are being trained in this
model and through the course of the rotation, the students are developing their core competency
skills that will allow them to be successful not only in the Pharm2Pharm model, but in any
setting of pharmacy they chose to practice.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-216
Title: Impact of student pharmacists on vancomycin dosing and compliance to national
guidelines for vancomycin therapeutic monitoring in a community hospital
Primary Author: Koon Ting, The Daniel K. Inouye College of Pharmacy, University of
Hawai`i at Hilo, HI;
Email: kting@hawaii.edu
Additional Author(s):
Sharon Lum
Christopher Tsue
Sheri Tokumaru
Eryn Kishimoto
Purpose: Vancomycin is one of the most widely used antibiotics in the U.S. and the treatment of
choice for Methicillin-resistant Staphylococcus aureus (MRSA) infections. In order to address
the increasing rates of Staphylococcal resistance, the ASHP, IDSA, and SIDP Task Force
established the 2009 Consensus Guidelines for Vancomycin Therapeutic Monitoring. Much
variation still exists in clinical practice because these guidelines are not necessarily universally
applied throughout the nation. The purpose of this study is to determine the impact of student
pharmacists on vancomycin dosing and compliance to national guidelines in a community
hospital.
Methods: This study will be submitted to the Institutional Review Board for approval. The
electronic medical record system will identify patients who have had at least one vancomycin
level drawn. The following data will be collected: patient age, gender, ethnicity, height, weight,
site of infection, baseline serum creatinine, peak serum creatinine throughout the duration of the
vancomycin therapy, vancomycin regimen (dose and frequency), date and time of vancomycin
administrations, vancomycin level, date and time of vancomycin level, reason for discontinuation
of therapy, microbial cultures and sensitivities, concomitant medications, review of systems,
physical exam, medical, title of clinician performing initial vancomycin dosing, title of clinician
ordering initial vancomycin level. All data will be reviewed by a team of pharmacists and student
pharmacists to determine the rate of compliance to the 16 consensus recommendations put forth
by the 2009 Consensus Guidelines for Vancomycin Therapeutic Monitoring from the ASHP,
IDSA and SIDP Task Force. The reviewers will compare the rates of compliance to the
guidelines between student pharmacists, pharmacists, and non-pharmacy clinicians.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-218
Title: Nontraditional pharmacy residency programs: exploring residency training opportunities
for rural and small hospital pharmacists
Primary Author: Matt Bilhimer, University of Kansas School of Pharmacy, Kansas;
Email: mbilhimer@ku.edu
Additional Author(s):
Amber Lucas
Purpose: The Kansas Council of Health-System Pharmacists (KCHP) has included residency
program expansion across the state in their strategic plan. Initial steps of this initiative include
the investigation of non-traditional pharmacy residency programs, none of which exist in Kansas,
as a means of achieving residency training, especially for pharmacists in small hospitals and
rural areas. KCHP intends to pursue viable opportunities for non-traditional residency training by
first identifying characteristics of established successful non-traditional ASHP-accredited
pharmacy residency programs in other states.
Methods: Non-traditional pharmacy residency programs were identified from the American
Society of Health-System Pharmacists (ASHP) online residency directory. Through a
professional network, additional programs not listed in the ASHP directory were discovered.
Residency Program Directors (RPDs) were contacted by email with a brief questionnaire with
open-ended questions to determine operational components of their non-traditional programs.
Information was requested regarding number of non-traditional residents, length of program,
whether or not the program was accredited by ASHP, how staffing and rotations were set up,
reimbursement through outside sources and awareness of other non-traditional programs in their
state. Some RPDs provided additional contact information for their current and past nontraditional program residents. Those individuals were also contacted with a separate
questionnaire.
Results: Thirteen Residency Program Directors across the nation were contacted, eleven of
which completed the questionnaire. Three programs forwarded contact information for their
residents and six residents responded to the supplemental questionnaire. Eleven of the 13
programs had a hospital size over 200 beds. All but one of the programs has a concurrent ASHPaccredited traditional Post Graduate Year 1 (PGY1) residency program. Many hospitals consider
only current employees of their respective health system for their non-traditional program and
some require an employment commitment post residency. None of the programs accept grant
money from the Center for Medicare and Medicaid Services or other federal or state government
organization. Ten of the programs are two years in length and three programs are three years. All
programs require a set ratio of staffing months to residency months. Time spent in each capacity
varied between institutions but most commonly involved the resident staffing for one to three
months for every month of residency training. All six residents that responded felt their
residency was worth while. Upon completion of their respective programs, they all stayed with
their hospital post-residency stating they felt more confident and capable as a result of their extra
training.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Efforts to make non-traditional programs a reality in small hospitals and rural areas
must include an evaluation of each institutions needs and budget to allow an employee to take
time off from regular employment responsibilities to complete the necessary training. The
potential challenges faced by small hospitals to have adequate staffing and financial resources
for programs similar to those already established creates an opportunity for an alternative nontraditional model. KCHP will explore a collaborative non-traditional pharmacy residency model
that incorporates multiple, smaller hospitals to achieve the additional training necessary to meet
ASHP accreditation criteria of a residency trained pharmacist.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-219
Title: Tigecycline combination therapy for the treatment of Clostridium difficile infection
Primary Author: Nicholas Britt, University of Kansas School of Pharmacy, KS;
Email: nbritt@kumc.edu
Additional Author(s):
Molly Steed
Lisa Clough
Purpose: The incidence of C. difficile infection (CDI) is increasing in recent years.
Metronidazole and vancomycin have been mainstays of CDI treatment for several decades, but
increasing rates of treatment failure have prompted the need for alternative therapies.
Tigecycline is a broad spectrum antibiotic that has shown favorable in vitro activity against C.
difficile, including resistant strains. However, there is a paucity of clinical data investigating the
use of tigecycline in this setting. The objective of this study is to describe the safety and
effectiveness of tigecycline combination therapy for the treatment of severe, refractory CDI.
Methods: This is a single center, retrospective case series of patients with CDI treated with
tigecycline combination therapy. The primary outcome is clinical cure. Secondary outcomes are
clinical failure, sustained response, hospital length of stay (LOS), and hospital all-cause
mortality. Additionally, associations between clinical cure and disease severity scores will be
evaluated. Data to be collected include patient demographics and characteristics, microbiological
and laboratory data, medications, and comorbidities. This study will be submitted to the
institutional review board for approval.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-220
Title: Evaluation of antibiotic use in respiratory syncytial virus (RSV) positive pediatric patients
at a community hospital
Primary Author: Alyssa Kaspar, Stormont-Vail HealthCare, Kansas;
Email: akaspar03@gmail.com
Additional Author(s):
Amber Howard
Jo Ann Harris
Katie Burenheide
Purpose: Respiratory syncytial virus (RSV) is a common viral illness, infecting nearly 100% of
children by two years of age. It can present with symptoms of otitis media and/or lower
respiratory tract infections. Concurrent bacterial infection in children with RSV is uncommon,
however viral symptoms can be concerning for possible bacterial infection. For this reason,
antibiotics are often prescribed unnecessarily. The purpose of this study was to determine the
appropriateness of antibiotic therapy prescribed for RSV positive inpatient children during the
2012 2013 season.
Methods: This study is pending Institutional Review Board approval. A single center,
retrospective chart review of all RSV positive patients under the age of 19 years old, who were
admitted to the hospital between November 2012 and May 2013, was performed. The following
data was collected: date of RSV positive test, patient age, temperature at presentation, antibiotic
prescribed, indication of antibiotic, and length of antibiotic treatment. Data was recorded without
patient identifiers in order to maintain confidentiality. Appropriateness of antibiotic therapy was
evaluated for each patient. Antibiotics were deemed appropriate if the patient: was admitted to
the pediatric intensive care unit (PICU), displayed signs and symptoms of severe sepsis, was
completing an antibiotic course started prior to admission, or was less than or equal to four
weeks of age at the onset of illness. Descriptive statistics were utilized to determine results.
Results: Seventy-four patients admitted were positive for RSV, of whom twenty-five (32%)
received antibiotics. One patient was excluded from the results because his antibiotic was a onetime pre-surgical dose. There were six different indications for antibiotics, which include the
following: otitis media (n=14, 56%), possible sepsis (n=5, 20%), pneumonia (n=4, 16%), febrile
neutropenia (n=1, 4%), and bacterial superinfection (n=1, 4%). Eight different single-agent or
multi-agent antibiotic regimens were utilized, with ceftriaxone (n=9, 36%) being the most
common antibiotic prescribed. Of the twenty-five patients given antibiotics, eleven (44%) were
considered appropriate, and fourteen (56%) were considered inappropriate.
Conclusion: More than half of the antibiotics prescribed were deemed inappropriate per the
parameters previously set. Physician education regarding appropriate indications for prescribing
antibiotics to RSV positive children may help decrease overuse of antibiotics.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-221
Title: Clinical outcomes and safety of vancomycin and daptomycin outpatient parenteral
antibiotic therapy (OPAT) for Gram-positive osteomyelitis
Primary Author: Rachel Louis, University of Kansas School of Pharmacy, Kansas;
Email: rclouis@gmail.com
Additional Author(s):
Ngoc Yen Vo
Molly Steed
Daniel Hinthorn
Purpose: Osteomyelitis remains a difficult infection to treat effectively and is complicated by
adverse events associated with long-term use of vancomycin (nephrotoxicity and
thrombocytopenia) and daptomycin (CPK elevation and myopathy). The purpose of this study
was to evaluate the efficacy and safety of a full course of vancomycin (VAN) alone versus
vancomycin followed by daptomycin (VAN/DAP) in the treatment of osteomyelitis.
Methods: An institutional review board approved, single center retrospective cohort study of
adult patients with osteomyelitis, who received at least four weeks VAN or VAN/DAP including
outpatient parenteral antibiotic therapy (OPAT) from 2010-2013. Medical records were reviewed
for patient characteristics, comorbidities, surgical interventions, microbiological cultures,
antimicrobial therapy, clinical outcomes, pertinent laboratory values, and adverse events. The
primary outcome measure was clinical response at the end of treatment and follow-up within 12
months. Secondary outcome measures were incidence of adverse events for VAN
(nephrotoxicity, thrombocytopenia) and DAP (myopathy, elevated CPK).
Results: Of 37 patients, clinical cure rates were 95.8% (VAN, 23/24) and 84.6% (VAN/DAP,
11/13) (P=0.3). Recurrence at follow-up occurred in 20.8% (5/24) and 30.8% (4/13) of VAN and
VAN/DAP patients, respectively (P=0.1). Nephrotoxicity occurred in 32.4% of patients on VAN
leading to discontinuation in 13.5%. Thrombocytopenia occurred in 1 patient on VAN and led to
discontinuation. Of 13 patients switched to DAP, 1 experienced elevated CPK level (> 2000
units/L).
Conclusion: Both VAN and VAN/DAP groups experienced high rates of recurrence.
Daptomycin was well tolerated while many patients on vancomycin developed nephrotoxicity,
leading to the discontinuation of the drug. Additional research in the area is warranted.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-222
Title: Review of ceftaroline applications in the clinical setting
Primary Author: Ashley Martin, School of Pharmacy, University of Kansas;
Email: ashl1990@ku.edu
Additional Author(s):
Amber Sawyer
Molly Steed
Daniel Hinthorn
Purpose: Ceftaroline (CPT), a novel methicillin-resistant Staphylococcus aureus (MRSA)
cephalosporin, is approved by the Food and Drug Administration for complicated skin and skin
structure infections (including MRSA) and community acquired bacterial pneumonia
(methicillin-sensitive Staphylococcus aureus only). Clinicians have been treating other MRSA
infections with CPT despite limited data in its efficacy. The purpose of this study is to conduct a
drug utilization review to evaluate the rationale behind CPT use and its efficacy in non-approved
MRSA infections.
Methods: This study will be submitted to the Institutional Review Board for approval. The study
design is a single center retrospective cohort study of adults who have received CPT inpatient for
greater than 72 hours from May 2011 to July 2013. Of those that received CPT therapy, medical
charts will be reviewed for the following information: patient demographics, such as age and sex,
comorbidities, including diabetes mellitus and hepatic and renal disease, microbiological data
including cultures and sensitivities, infection(s) as diagnosed at the discretion of the provider,
rationale of initiation and discontinuation of CPT therapy when documented, clinical outcomes,
and adverse side effects. Concurrent, prior, and post CPT antibiotic therapy will also be
recorded. The primary outcome measure is the patient status at the conclusion of inpatient CPT
treatment.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-223
Title: Perceived value of a clinical intern program: a ten year experience
Primary Author: Raksha Patel, Lawrence Memorial Hospital, Kansas;
Email: raksha08@ku.edu
Additional Author(s):
Breaer Miller
Laura Prohaska
Patrick Parker
Purpose: The expressed initiatives for beginning a clinical intern program at an institution are to
provide a valuable, developmental resource for students as they progress through their academics
and beyond, increase time to allow pharmacists opportunities for additional direct patient care
functions, and to enhance patient care in collaboration with other healthcare professionals.
Clinical interns can be trained to assist pharmacists with medication reconciliations, dosing
consults, patient education, and more. The purpose of this study was to subjectively asses how
well a clinical intern program is meeting the first stated initiative and if the overall program
influenced post-graduate job selections.
Methods: A 17-question online survey was developed to assess the value and impact of a
clinical intern program. The survey was delivered via email to the 26 graduates that participated
in the first ten years of a clinical intern program at one institution. Survey responses were
anonymous to reduce potential bias. Post-graduate job selections among the graduates and their
peers were compared. The data was analyzed using the Fisher's Exact Test with a statistical
significance set at p equals 0.05. This study was approved by the institutional review board.
Results: Responses were obtained from 21 of the 26 graduates that were surveyed. For their first
role in pharmacy after graduation, 11 of the graduates went into a residency, 6 went into hospital,
and 4 went into retail. Twenty of the 21 graduates indicated that the clinical intern program
substantially helped them throughout their Advanced Pharmacy Practice Experiences (APPE)
and had a key influence on their early career path. Sixteen of the 21 graduates indicated that the
program substantially benefited their clinical knowledge base in the pharmacy profession. For
post-graduate job selections, 11 of the graduates of the clinical intern program went into a
residency (52%) and 10 went into another pharmacy career (48%). In comparison to their peers,
135 of them went into a residency (19%) and 560 of them went into another pharmacy career
(81%). Analysis of the data determined a statistically significant p value of 0.001, rejecting the
null hypothesis that stated there is no difference in initial job selection between the graduates
who participated in a clinical intern program and their peers.
Conclusion: The implementation of a clinical intern program for students at an institution is
beneficial and influential on their academics and career paths after graduation. Students who
participate in a clinical intern program are more likely to pursue a residency. Similar programs
should be developed at other institutions to provide the opportunity to more students to increase
their exposure to the pharmacy profession before graduation.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-224
Title: Colistin dosing and outcomes for multi-drug resistant gram-negative infections
Primary Author: Kaydee Tran, The University of Kansas School of Pharmacy, Kansas;
Email: ktran89@ku.edu
Additional Author(s):
Kody Koester
Kaili Melton
Molly Steed
Purpose: The rapid increase of multi-drug resistant (MDR) Gram-negative infections in recent
years has lead to a resurgence of colistin use, a polymyxin antibiotic from the 1950s.
Unfortunately, improper dosing of colistin can lead to suboptimal bacterial killing, the
emergence of resistance, and an increased risk of nephrotoxicity/neurotoxicity. The purpose of
this study is to determine if pharmacist and physician education on the new colistin dosing
guidelines will lead to improved treatment outcomes, decreased resistance, and decreased
toxicities.
Methods: A quasi-experimental study of adult patients who received colistin for 72 hours from
2010-2015. Phase 1 (2010-2013): pre-intervention observation. Intervention: dosing guideline
education. Phase 2 (2013-2015): post-intervention observation. Medical records were reviewed
for demographics, co-morbidities, APACHE II and Charlson scores, cultures and susceptibilities,
predictive factors of AKI, colistin dose, combination Gram-negative therapy and concurrent
nephrotoxic drugs. The primary outcome measure was infection related death. Secondary
outcome measures were appropriate colistin use (dose and combination therapy), microbiological
eradication, rate of neurotoxicity, and rate of nephrotoxicity.
Results: During phase 1 (n=13), patients received colistin monotherapy (n=1), single
combination (n=7), double combination (n=4), and triple combination (n=1). On average a
patient was underdosed or overdosed by 42% and 58% respectively. Zero patients suffered
infection related death and 30.8% (n=4) had microbiological eradication. Nephrotoxicity
occurred in 53.8% (n=7) of patients on colistin according to RIFLE criteria: risk category (n=3),
injury category (n=2), and failure category (n=2). No cases of neurotoxicity were seen.
Conclusion: In our cohort, colistin is only being dosed correctly according to Garonzik
guidelines <8% of the time and nephrotoxicity rates were concerning at over 50% leaving much
room for improvement in dosing and outcomes in phase 2.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-225
Title: Retrospective cohort study of privately insured type 2 diabetes patients to evaluate betablocker exposure after myocardial infarction
Primary Author: Ryan Hickson, University of Kentucky College of Pharmacy, Kentucky;
Email: hickson.ryan@uky.edu
Additional Author(s):
Emily Brouwer
Candace Brancato
Daniela Moga
Purpose: Beta-blockers remain an important therapeutic tool for secondary prevention of a
myocardial infarction (MI). However, there is still disagreement regarding their utilization in
patients with diabetes despite recommendations for their use in numerous clinical guidelines.
Several studies in diabetic patients have shown that beta-blockers may worsen glycemic control;
clinicians may also worry about beta-blockers masking the warning signs of a hypoglycemic
event. Some beta-blockers exhibit unique pharmacologic differences though, and little research
has evaluated their relative safety and efficacy in this population. This study aims to identify
patterns in beta-blocker utilization among type 2 diabetes (T2DM) patients after an MI.
Methods: This project has received Institutional Review Board approval. We will construct a
retrospective cohort of employed, commercially insured individuals with dependents using deidentified data from 2007-2009. Patient enrollment files, medical claims, and pharmacy claims
will be utilized. Inclusion criteria will be: (1) T2DM, (based on ICD-9 diagnosis codes [249 and
250] and/or prescriptions for oral anti-diabetes drugs) (2) 18 years and older, (3) three years
continuous eligibility, (4) MI (ICD-9 code [410.xx]). Exclusion criteria will be: (1) females
prescribed metformin exclusively in the absence of T2DM diagnosis codes, (2) less than 6
months eligibility pre-MI, (3) MI before first T2DM date, (4) beta-blocker use pre-MI. Patients
with a new beta-blocker prescription fill after MI will be identified using NDCs mapped to
American Hospital Formulary Service (AHFS) Pharmacologic-Therapeutic Classifications and
then compared to non-users. Beta-blockers will be categorized by presence of cardioselectivity,
intrinsic sympathomimetic activity, and alpha-antagonism. Descriptive statistics (chi-square
analysis and t-tests) will be employed to compare the distribution of demographic and
cardiovascular comorbidities between new beta-blocker users and non-users. Logistic regression
with odds ratios and 95% confidence intervals will be used to evaluate the impact of age and
cardiovascular comorbidities as predictors of beta-blocker exposure post-MI in T2DM patients.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-226
Title: Does cigarette smoking contribute to the progression of breast cancer?
Primary Author: Lindsay Barr, Sullivan University College of Pharmacy, KY;
Email: LBARR2192@my.sullivan.edu
Additional Author(s):
Myranda Tran
Taralein Beckmann
Wasana Sumanasekera
Purpose: Breast cancer is a devastating disease that leads to fatality if not detected and treated
during early stages. Several factors including hereditary / genetic mutations contribute to the
etiology of breast cancer. Some studies indicate that exposure to cigarette smoke (CS)
contributes to the development of breast cancer and cancer related deaths. However, few studies
show negative correlation between CS and breast cancer progression. The purpose of this review
is to summarize and present the excising literature about the link between cigarette smoking and
the progression of breast cancer.
Methods: An extensive literature search has been conducted using search engines such as
Pubmed. The most up to date original research based literature as well as cohort studies on the
contribution of cigarette smoking in development of breast cancer were gathered, analyzed, and
presented under different major sub headings. Sub headings include, harmful components
present in cigarette smoke & the contribution of those to the development of cancer; original
research based In-vitro and in-vivo studies; Population based / Cohort studies; and involvement
of receptor mediated signaling in breast cancer progression. Many aspects were discussed under
each sub heading.
Results: Tobacco smoke is an aerosol which contains numerous carbonaceous polymeric
materials with adsorbed heavy metals, polycyclic aromatic hydrocarbons, aromatic amines, and
many other organic compounds. Reactive oxygen species (ROS) present in the gas phase of CS
can cause endogenous antioxidant destruction, including vitamins and enzymatic antioxidants.
Several studies have shown CS induced attenuation of antioxidant vitamins, causing systemic
oxidative stress. ROS present in CS such as hydrogen peroxide and hydroxyl radicals are
destructive and can cause damage to DNA. This damage can lead to mutations that are capable
of initiating cell proliferation leading to metastatic cancer. Antioxidants such as vitamin C can
attenuate free radical induced damage. In addition to oxidative stress, CS component induced
activation of growth factor receptors and nicotinic acetyl choline receptors were also presented
as candidate mechanism for CS induced progression of breast cancer. Many hormones
(especially estrogen), proteins, and genes that are affiliated with breast cancer development can
be induced by CS exposure. Much more research needs to be conducted to fully understand the
effects of cigarette smoke and the effects it has on normal and cancerous breast cells.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Numerous harmful components are present in a cigarette. The carcinogens present
in cigarette smoke are capable of causing DNA damage and mutations that can cause detrimental
effects. People exposed to tobacco smoke before breast cell development have been found to
have the highest risk of breast cancer development later in life. Exposure in adolescents or young
adults has an intermediate risk and adult exposure has the lowest risk. Cigarette smoke itself may
not cause cancer, but it can promote cancer via enhancing breast cell proliferation drastically
once DNA gets mutated.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-227
Title: Effect of cigarette smoke exposure on ovarian cancer cell proliferation
Primary Author: Taralein Beckmann, Sullivan University College of Pharmacy, KY;
Email: TBECKM9491@my.sullivan.edu
Additional Author(s):
Lindsey Barr
Wasana Sumanasekera
Purpose: Ovarian cancer is a silent killer, asymptomatic during the early stages of the disease. In
most cases symptoms beginning to appear when the cancer has metastasize to the other parts of
the body. Because of the silent nature of this disease, investigating the risk factors for ovarian
cancer is at utmost importance. Currently, cigarette smoking is not considered a risk factor for
the development of ovarian cancer. However, detrimental effects of smoking after an ovarian
cancer diagnosis have been established. Our study investigates the possibility of cigarette smoke
exposure as a contributing factor for the progression of ovarian cancer
Methods: Ovarian cancer cells were cultured using RPMI 1640 growth medium with Lglutamine, 10% fetal bovine serum (FBS), insulin, and 1% penicillin/streptomycin. For proper
cell propagation the cells were transferred to larger dishes every 2-3 days using 0.25% Trypsin
EDTA and fresh growth media. Cigarette smoke extracts (CSE) were made using Camel filter
free cigarettes. To prepare CSE, a cigarette was attached to an adaptor, connected to a 60 mL
syringe filled with 10 ml of RPMI medium. Pulling the plunger of the syringe while the cigarette
is lit allowed smoke to enter the syringe. Defined amounts of aqueous CSE was created by
mixing the puff with the serum free RPMI media. Following overnight serum starvation
designated ovarian cancer cells were exposed to CSE for 24 hours. Three different CSE
exposures, which are 0% (no smoke control), 5% and 10%, were utilized. In order to detect CSE
induced modulation of ovarian cancer cell proliferation, BrdU cell proliferation assay was
conducted according to the manufacturers instruction (Millipore). BrdU is an analogue of
thymidine that gets incorporated to cells DNA during DNA synthesis. The incorporation of
BrdU, which is indicative of new DNA synthesis in viable cells, was detected using
spectrophotometric plate reader.
Results: CSE caused a significant increase in ovarian cancer cell proliferation at 5% CSE
concentration. Estrogen increases CSE induced ovarian cancer cell proliferation about 10 fold.
Conclusion: CSE contributes to the development / progression of ovarian cancer due to its
ability to increase ovarian cancer cell proliferation.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-228
Title: Medication use evaluation (MUE) of acetaminophen at a multicenter academic medical
facility
Primary Author: William Black, University of Kentucky, Kentucky;
Email: williamblack@uky.edu
Additional Author(s):
Kimberly Hite
Purpose: Acetaminophen has long been associated with liver failure following both chronic as
well as acute overdose. At this academic medical center, two actions have been taken to prevent
acetaminophen overdoses. First, a warning note was programmed to display on the electronic
medication administration report (eMAR) for acetaminophen containing drug items. Second, all
500 mg acetaminophen containing combination drugs on formulary were converted to 325 mg
acetaminophen combination products, per the 2011 FDA mandate. The objective of this
proposed MUE is to evaluate whether actions to date have been sufficient to prevent
acetaminophen overdoses or if additional interventions are needed.
Methods: Following IRB approval, data will be obtained through querying the electronic
medical record for all doses of acetaminophen containing medications administered during a two
month time period in each of the years: 2010, 2011, 2012, and 2013. The data will be converted
to Microsoft Excel format and evaluated for the amount of acetaminophen that was administered
to each patient during a 24 hour time period. Each overdose, defined as total daily
acetaminophen administration greater than 4 grams, will be evaluated based on the severity as
well as the factors that lead to the overdose. These factors will include: the administration of a
medication at the high end of an available dosing range, use of multiple acetaminophen
containing products, and the administration of doses before they were due to be given. Last, data
that includes the use of 500 mg acetaminophen products will be compared to data that contains
only 325 mg acetaminophen products to determine what impact the conversion of the
acetaminophen strength of the drug combination products had on the degree and number of
overdoses.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-229
Title: Trends in the utilization of procalcitonin for patients admitted with possible sepsis or acute
respiratory tract infections at an academic medical center
Primary Author: Matthew Blum, University of Kentucky, Kentucky;
Email: matt.blum@uky.edu
Additional Author(s):
Mark R Cox
Jennifer A Wiedmar
Lynn C Wardlow
Purpose: Procalcitonin is considered a biomarker for acute bacterial infections and may be
helpful when deciding to initiate or discontinue antibacterial therapy. Currently, at this
institution, there is no procalcitonin-driven protocol utilized for antimicrobial therapy and it is
unclear how providers are utilizing this lab value in clinical decision-making. This study will
investigate the attainment and utilization of procalcitonin for specific infections at one institution
and how antimicrobial treatment decisions correlate with these values.
Methods: This is a retrospective, observational study that will be submitted to the IRB for
approval prior to commencement. Patients with procalcitonin levels obtained between the time
periods of January 1, 2012 and June 30, 2012 will be assessed. Individuals presenting with
suspected acute respiratory infections or sepsis will be included in the evaluation. Exclusion
criteria include patients less than 18 years of age and individuals not directly admitted to this
institution. White blood cell count, C reactive protein and erythrocyte sedimentation rate will be
collected to establish cursory information on usefulness in guiding therapy and if further
provider education and/or a procalcitonin-driven treatment pathway should be considered at this
institution. Additionally, the use of ventilation and/or oxygen, as well as changes in these
requirements, will be documented to assess for clinical improvement. Antibiotic prescribing
patterns relative to procalcitonin levels will be documented to assess for trends and correlation.
Microbiologic and serologic data which may indicate a bacterial, fungal, or viral infection from
the current admission will aid in evaluating the need for antimicrobial therapy and/or optimal
treatment course. Descriptive statistics will be utilized for application of collected data.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-230
Title: Sullivan University College of Pharmacy Student Society of Health System Pharmacists:
Mattingly Center Outreach
Primary Author: Mary Bystrek, Sullivan University College of Pharmacy, Kentucky;
Email: mbystr3467@my.sullivan.edu
Additional Author(s):
Amy Cowan
Purpose: The Sullivan University College of Pharmacy Student Society of Health System
Pharmacists (SUCOP-SSHP) was fortunate to elect a president-elect in 2012 who is involved
with the Mattingly Center for Cerebral Palsy in Louisville. Through Rachel's involvement, the
main outreach for SUCOP-SSHP became bi-monthly presentations to the participants at the
Mattingly Center. The purpose of this project is to describe the monthly presentation and
discussions and the methods of one in particular.
Methods: As part of the SUCOP annual health fair, SSHP has always had a booth for poison
prevention featuring a student-made game called "Medicine or Candy." At this booth, members
play the game, geared toward children, with passers-by. We use the game as an opportunity to
teach about the risks of eating things that look like candy, which could actually be medications.
For instance, some antacids also look like some hard tart candies. As a way to reach out to a
different community, we took this game to the Mattingly Center and played it with participants
who have cerebral palsy. In addition to teaching about the risks of confusing medication for
candy, SSHP members also taught about the Poison Control hotline and what to do in
emergencies.
Results: This was the first of many monthly presentations and it was well-received. Participants
at the Mattingly Center as well as members of SSHP all enjoyed themselves and there was ample
opportunity for learning. The presentation involved about 30 participants and employees of the
Mattingly Center as well as four SSHP members and one faculty representative. The presentation
not only taught participants about the dangers of mistaking medication for candy, but also gave
new students an opportunity for community outreach and a chance to practice their presentation
and public speaking skills.
Conclusion: This project has been so well-received that the Mattingly Center has continued to
ask for SSHP's involvement, not only for the bi-monthly presentations, but also for their annual
fundraising gala. Involvement with the Mattingly Center has given students the opportunity to
reach out to an otherwise forgotten community. Unfortunately, a lot of pharmacists don't know
how to be involved with a community of people with disabilities, but our organization is teaching
those skills to young future pharmacists.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-231
Title: Transitioning from a service based to an indication based antimicrobial restriction strategy
at a large community hospital
Primary Author: Thomas Carroll, University of Kentucky College of Pharmacy, Kentucky;
Email: tjcarroll@uky.edu
Additional Author(s):
Theresa E. Link
Kathryn M. Ruf
Ashley L. Ross
Purpose: Our facility recently switched from a service based to an indication based restricted
antimicrobial prescribing strategy. Restricted antimicrobials no longer require infectious diseases
(ID) physician approval prior to use; but instead, require that certain criteria defined by our
institution's Antimicrobial Stewardship Program are met. This evaluation outlines advantages
and challenges of implementing an indication based prescribing strategy in a community
hospital, explains the crucial steps necessary to successfully implement indication based
antimicrobial restrictions, and identifies how to assess the success of these strategies after
implementation so that similar facilities can make this transition.
Methods: Current antimicrobial stewardship practices were assessed and evaluated through
literature searches and a review of the current guidelines from the Infectious Diseases Society of
America (IDSA), Society of Healthcare Epidemiology of America (SHEA), and American
Society of Health System Pharmacists (ASHP). Previous and current hospital policies at our
facility regarding antimicrobial stewardship were reviewed and compared to current practice
recommendations, focusing on changing from a service based to an indication based restricted
antimicrobial strategy. Success of the indication based restricted antimicrobial strategy
implementation was evaluated through previously analyzed medication utilization evaluation
(MUE) data, analysis of defined daily dose data, and internal hospital cost data of the restricted
antimicrobial medications. This evaluation was approved by the Advanced Medicine Committee
and was found exempt by the Institutional Review Board since no specific patient information
was utilized.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-232
Title: Characterization of stress ulcer prophylaxis prescribing patterns in patients with chronic
liver disease induced coagulopathies at a Veterans Affairs Medical Center
Primary Author: Rachel Clark, University of Kentucky College of Pharmacy, Kentucky;
Email: rachelclark@uky.edu
Additional Author(s):
Kelly W. Davis
Purpose: Due to complications associated with the disease, patients with chronic liver disease
(CLD) are often coagulopathic. While the American Society of Health-Systems Pharmacists
(ASHP) guidelines recommend stress ulcer prophylaxis (SUP) for patients with coagulopathies,
it is unclear whether patients with CLD benefit from SUP, and prescribing practices for this
indication vary. The objective of this study is to characterize SUP prescribing practices for
patients with CLD at a single Veterans Affairs Medical Center (VAMC) in order to assess
adherence to guideline recommendations, and to determine if SUP is being appropriately
prescribed to patients with CLD induced coagulopathies.
Methods: After International Review Board (IRB) approval is obtained, a retrospective study
will be performed at a single VAMC. The electronic medical record system will be used to
identify all patients admitted to the VAMC for at least 24 hours from 1/1/2008 to 6/30/2013 with
CLD and coagulopathies, defined as either an international normalized ratio (INR) greater than
1.5 or a platelet count of less than 50,000/mm3. Patients greater than 89 years old, or with an
upper GI bleed within 48 hours before or 24 hours after admission will be excluded. The primary
objective will be to characterize SUP prescribing patterns for this population and evaluate
guideline adherence. A secondary objective of this investigation is to evaluate the efficacy of
SUP in patients with CLD by examining the relationship between SUP and the incidence of
stress ulcers in this population. Other secondary objectives include an assessment of the
relationship between SUP use and the development of nosocomial infections such as Clostridium
difficile, pneumonia, and spontaneous bacterial peritonitis.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-233
Title: Characterization of stress ulcer prophylaxis use on a pediatric surgery service
Primary Author: Amy Cowan, Sullivan University College of Pharmacy, Kentucky;
Email: abaile6190@my.sullivan.edu
Additional Author(s):
Dennis Harrod
Jason Humphress
Purpose: Medications are often prescribed off-label for pediatric patients due to lack of
pharmacokinetic data. This paucity of data forces practitioners to use professional judgement to
develop dosing regimens for pediatrics from adult data. In turn, greater monitoring of outcomes
and adverse effects is required. It is widely known that the use of histamine blockers in children
causes adverse effects such as necrotizing colitis and abdominal abscess, yet ranitidine continues
to be prescribed off-label for pediatrics. The goal of this study is to characterize the use of
histamine receptor antagonists in a peditriac surgery service in order to avoid adverse outcomes.
Methods: This study has been approved by the Sullivan University Institutional Review Board
under an expedited application. Restrospective data from 2006-2008 of patients aged 2-17 years
old is being reviewed to include patients who underwent surgery during that time and who had
not received a proton pump inhibitor or histamine receptor antagonist prior to surgery. This will
enable us to complete a case series and observational study. Data collected will include: age,
height, weight, temperature, white blood cell count, reason for admission, procedure,
medications, length of stay, complications, and outcome. Data will then be reviewed to
determine if a correlation exists between use of a histamine receptor antagonist and incidence of
negative outcomes. Additionally, to minimize threats to validity, a logistic regression analysis
will be conducted to predict the probability of a pediatric patient developing an adverse effect
after receiving a histamine receptor antagonist on pediatric surgery service. This will be
compared to our results to ensure that no bias was present.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-234
Title: Screening of type II diabetes in pediatric population while in surgical unit
Primary Author: Shaina Doyen, Sullivan University College of Pharmacy, KY;
Email: sesser2467@my.sullivan.edu
Additional Author(s):
Danielle Shoemaker
Harshad Patel
Purpose: Obesity is associated with many comorbidities such as hypertension, dyslipidemia,
metabolic syndrome, hernias, stress urinary incontinence, osteoarthritis, respiratory problems,
and thromboembolism. Because of this correlation, obesity is also a risk factor for complications
that need surgical intervention, such as a cholecystectomy. Obesity has been established as a risk
factor for gallbladder disease. Therefore, the increase in pediatric cholecystectomies without comorbid complications has corresponded to the increase in pediatric obesity. The American
Diabetes Association (ADA) currently has guidelines for screening patients with high risk factors
for type II diabetes mellitus. However, when a patient is admitted for another complication this
tool may not be utilized as frequently as needed. With obesity having such a notable correlation
with comorbidities such as diabetes and surgeries such as a cholecystectomy, health care
providers could use the opportunity to intervene in the obese pediatric population. Routine
laboratory blood tests are frequently conducted prior to surgery. This would be an opportunity to
efficiently evaluate blood glucose to screen for type II diabetes in the pediatric population to
establish early diagnosis and prevent future diabetic complications.
Methods: All patients between the ages 2 and 18 in the surgical unit will undergo the ADA
screening criteria to determine who will be tested for type II diabetes. This study is a prospective,
case series conducted at Kosair Childrens Hospital in Louisville, KY. The data will be collected
by Sullivan University College of Pharmacy Advanced Pharmacy Practice Experience students
from August 2013 to April 2014. The patient data to be collected includes: patients considered
overweight (BMI >85th percentile for age and sex, weight for height >85th percentile, or weight
>120% of ideal for height); Presence of any of the following risk factors such as family history
of type II diabetes in a first or second-degree relative, race/ethnicity (Native American, African
American, Latino, Asian American, Pacific Islander), signs of insulin resistance or conditions
associated with insulin resistance (acanthosis nigricans, hypertension, dyslipidemia, polycystic
ovary syndrome, or small-for-gestational-age birth weight), maternal history of diabetes or
gestational diabetes mellitus during the childs gestation. Patient confidentiality will be
maintained throughout with removal of key patient identifiers. Upon data retrieval, patients
considered at-risk post screening will be tested via blood glucose. Final evaluation will be made
following ADA guidelines criteria for the diagnosis of diabetes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-235
Title: Assessing differences in medication-taking behavior for commonly prescribed oral
atypical antipsychotics in patients with schizophrenia
Primary Author: Ekim Ekinci, University of Kentucky College of Pharmacy, Kentucky;
Email: ekim.ekinci@uky.edu
Additional Author(s):
Emily S. Brouwer
Jeffery Talbert
Purpose: Non-adherence and non-persistence of medication use are predictors of relapse in
patients with schizophrenia. This study aims to determine the effects of commonly prescribed
oral atypical antipsychotic agents on these two aspects of medication-taking behavior. Findings
may be used in developing therapeutic regimens that help minimize relapse and improve patient
outcomes.
Methods: This study has Institutional Review Board approval. This retrospective study uses deidentified health claims information from a commercially insured population representing 15
million patients annually across the US for the period of January 1, 2007 to December 31, 2009.
Among recipients aged 18-64 (inclusive) with a primary or secondary diagnosis of schizophrenia
(defined using ICD-9-CM codes), National Drug Codes were used to identify patients with at
least two prescription claims for one of the following medications: aripiprazole, olanzapine,
quetiapine, risperidone, or ziprasidone. Recipients were limited to those with 18 months of
continuous eligibility to allow for a 6-month run-in, and a 12-month follow-up after first-fill
date. Patients were excluded if first-fill date showed claims for multiple study medications or
primary diagnosis codes for any mental disorder besides schizophrenia. Primary study outcomes
are medication adherence and persistence of medication use. Medication possession ratio
(number of doses dispensed in relation to dispensing period) is used to operationalize adherence.
Persistence of medication use is the duration of time from initiation to discontinuation (over 30days between refills) of therapy. Analysis will include descriptive statistics of population
baseline characteristics, chi-square and one-way ANOVA for categorical and continuous
variables, and multivariate models using logistic and Cox-regression.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-236
Title: Effect of medication dispensing site and patient location on time to antiepileptic drug
administration to patients in status epilepticus
Primary Author: Emilee Feldpausch, University of Kentucky, Kentucky;
Email: emilee.feldpausch@uky.edu
Additional Author(s):
Aaron Cook
Ahmed Mahmoud
Purpose: In 2012 the Neurocritical Care Society (NCS) redefined status epilepticus (SE) as
patients presenting with continuous clinical and/or electrographic seizure activity or recurrent
seizure activity without recovery to baseline between seizures for 5 minutes or more.
Furthermore, the guidelines emphasized the importance of administering emergent, urgent, and
refractory anti-epileptic drugs (AEDs) within a specified time frame. The purpose of this study is
to determine if patient location and/or the medication dispensing site (i.e. Automated Dispensing
Cabinet (ADC), admixture in pharmacy, etc.) impacts time to administration from the time of
order.
Methods: A retrospective chart review was completed for all patients 18 years or older with a
SE diagnosis within the time frame of October 2009 to January 2013. Patients were excluded
from the analysis if they were pregnant, managed on the hypothermia protocol, incarcerated, or
otherwise deemed a vulnerable subject by our institutional review board. Baseline demographics
were collected including age, gender, height and weight. The timing of AED order entry and
administration were collected as well as the drug name, dose and route. One hundred and sixtyeight patients were included in the study. Male patients comprised 56% of the patients treated,
the mean age was 54 years old and the mean weight was 84 kilograms. The emergency
department managed most of patients presenting with SE, followed by the intensive care unit.
The dispensing site of the medication (i.e. ADC, central pharmacy) as well as the patient location
during their hospital stay will be collected and correlated with the existing data. Time to
administration will be reviewed and analyzed based on the differences in medication and patient
location with respect to the updated NCS SE/RSE guidelines.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-237
Title: Effect of severity of subarachnoid hemorrhage on pharmacokinetic parameters of
aminoglycosides and vancomycin
Primary Author: Megan Goetz, University of Kentucky, Kentucky;
Email: megan.goetz@uky.edu
Additional Author(s):
Shaily Arora
Aaron Cook
Sara Parli
Purpose: Critically ill patients, including those post subarachnoid hemorrhages, demonstrate
hyperdynamic responses including increased creatinine and drug clearance. These instances of
elevated response to illness are termed augmented renal clearance. We hypothesize patients with
severe SAH (Fisher Grades 3 and 4 or Hunt and Hess Scores 4 and 5) exhibit a greater
hyperdynamic response that alters the pharmacokinetic (PK) parameters of renally cleared
antibiotics like aminoglycosides (AGs) and vancomycin compared to patients with less severe
SAH. The study purpose is to determine PK parameters of AGs and vancomycin in SAH and
identify the impact of severity of SAH on creatinine clearance.
Methods: This study is an IRB approved, retrospective, electronic chart review of patients
admitted to our facility with SAH between July 2008-July 2012 who received aminoglycosides
and/or vancomycin therapy. Fisher grades and Hunt and Hess scores were analyzed. PK
parameters such as volume of distribution, half-life, elimination rate constant, and creatinine
clearance were estimated by utilizing plasma drug concentrations obtained via therapeutic drug
monitoring and routine monitoring.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-238
Title: Facilitating student learning of business principles in academia: creating a business plan
for a pharmacy pipeline program
Primary Author: Danielle Griggs, University of Kentucky College of Pharmacy, Kentucky;
Email: danielle.antis@uky.edu
Additional Author(s):
Stephanie Wurth
Kelly M. Smith
Purpose: A college of pharmacy sought to initiate a pipeline program to enhance student
recruitment efforts. Program development necessitated a systematic approach, yet there were no
resources available to guide the process. The utility of a business plan model to guide the
development of the program proposal, while simultaneously enhancing an Advanced Pharmacy
Practice Experience (APPE) in Academic Pharmacy for a PharmD/MBA dual degree student,
therefore was assessed.
Methods: A business plan was piloted as a tool to guide program development, given such a
process provides a structure for program description, financial justification, marketing strategy,
operational processes, and implementation timeline. Initial composition of the business plan was
tasked to an APPE student with experience in undergraduate and professional program
recruitment, knowledge of the importance of recruitment platforms as a student member of the
Admissions Committee, and skills in conception and construction of a business plan from dual
enrollment in an MBA program. Development of the business plan began with a market analysis
of benchmark institutions and characteristics of their recruitment programs. Essential
components of the proposed pipeline program were then selected by the student under the
guidance of the Director of Student Admissions to achieve the mission of the program and
identify operational feasibility. This development process was repeated for each component of
the business plan document. Plan success was measured through review by the Academic and
Student Affairs Dean, with a focus on sufficient program justification, feasibility, structured
outcome measures, and plan cohesiveness. Additionally, the student was asked to reflect to
identify lessons learned throughout the APPE project.
Results: Creation of the business plan was deemed effective in program planning, following
administrative review. The format guided the program authors in comprehensive planning,
financial justification and preparation of a timeline for implementation. Primary literature was
evaluated to determine variety of structure and content of existing pipeline programs.
Additionally, key decision points of pipeline program development were identified including age
of target participants, duration of program, content and activities, and financial justification. The
College recognized that development of the business plan required careful analysis of the
multiple variables to ensure the mission and vision of the program were met. For the student, the
activity provided an opportunity to apply skills gleaned from an MBA program to a project likely
to result in program implementation, rather than participating in a simulation or academic
exercise. Upon reflection, the student identified the enhancement of multiple skills through the
experience such as project management, critical thinking, and formal written communication.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Additionally, business management skills developed include assessing needs to develop a
mission, market analysis and strategy development, providing financial justification utilizing
projected revenues and expenses, and identification of operational process necessities. The plan
will be presented to the college leadership for endorsement and subsequent implementation.
Conclusion: The development of a business plan was beneficial to a college in its creation of a
new recruitment program, and to a student who applied lessons learned in the classroom to meet
operational needs. The plan development process prompted a cohesive approach to program
conception while affording a student the opportunity to engage in APPE activities customized to
her interests. Such an approach should be explored for similar programmatic development
activities.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-239
Title: Analysis of Kentucky Medicaid managed care versus fee-for-service systems: medication
adherence in patients with essential hypertension
Primary Author: Catherine Herren, University of Kentucky College of Pharmacy, Kentucky;
Email: katie.herren@uky.edu
Additional Author(s):
Emily Brouwer
Jeffrey Talbert
Purpose: A key goal for managed care organizations is to improve patient health outcomes and
reduce costs. One strategy involves increasing medication adherence among patients with
chronic diseases. The Kentucky Department for Medicaid Services contracted with three
managed care organizations in November 2011 to transition the states traditional fee for service
Medicaid patients into capitated managed care. The purpose of this study is to determine
differences in medication adherence before and after the switch from fee-for-service to managed
care for Medicaid patients in Kentucky with essential hypertension between 2010 and 2012.
Methods: The retrospective cohort study sample is drawn from a database of Kentucky
Medicaid patient medical and prescription claims between 2010 and 2012. The University of
Kentucky Internal Review Board approved the study. Eligibility requirements are (1) to have a
diagnosis of malignant, benign, or unspecified essential hypertension (ICD-9 codes 401.0, 401.1,
or 401.9 respectively) prior to September 2010, and (2) to have at least 1 claim for medication
indicated for essential hypertension between September 2010 and August 2011, and between
January 2012 and December 2012. Claims during September 2011 through December 2011 are
excluded to control for confounders associated with the transition. Medication adherence is a
continuous variable determined using the medication possession ratio (MPR), or the days supply
of medication divided by the days of treatment. The study includes descriptive statistics of MPR
and control variables including patient demographics, type of antihypertensive, and
comorbidities. Bivariate analyses using paired t-tests, one-way ANOVA, and simple linear
regression measure the effect of each variable on MPR before and after the switch. Multivariate
analysis is a difference-in-difference regression analysis of covariance, which determines the
average change in MPR due to the switch to managed care, controlling for other inherent
changes in MPR.
Results: Descriptive statistics and bivariate analysis indicate that there is an insignificant
decrease in MPR after the implementation of managed care in Kentucky Medicaid. Both before
and after the switch, male patients are more likely to have a higher MPR. Before the switch,
white patients tend to have a higher MPR, but the increase in days of possession is not large for a
therapeutic effect to be noticeable. Age is a strong predictor of MPR, in that younger patients
tend to have a lower MPR, and older patients tend to have a higher MPR, regardless of the
implementation of managed care. Comorbidities do not have a significant effect on MPR either
before or after the switch. At this time, the model does not indicate a significant increase in the
MPR as determined in the first full year after implementation of Medicaid managed care in
Kentucky. Instead, the model predicts a slight decrease in MPR, though insignificant. There are
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
likely omitted variables affecting MPR after the switch that should be determined in future
studies.
Conclusion: Kentucky Medicaid made a fundamental switch from fee-for-service to a managed
care model, which sets up an inherent study for examining the effects of the change. This study
provides Kentucky policy makers with the outcomes measures needed to observe the
effectiveness of the change, and whether further policy decisions need to be made. Results from
the first year after implementation indicate a lack of significant evidence of positive outcomes
for patients in managed care. Lag time due to implementation may still be a contributing factor,
however Kentucky policy makers should evaluate the progress of managed care in Kentucky
Medicaid.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-240
Title: Prospective, randomized, cohort study on blood pressure outcomes following a health fair
Primary Author: Christine Hoffman, Sullivan University College of Pharmacy, Kentucky;
Email: choffm9415@my.sullivan.edu
Additional Author(s):
Katie Martin
Bryana Swearingen
Amanda Jett
Stacy Rowe
Purpose: In an effort to increase hypertension awareness, pharmacy organizations have used
health fairs among the community to promote awareness, offer screenings, and counsel patients
on life style modifications. As pharmacy schools around the nation continue to expand the
service learning component of their curriculum, there will likely be an increase in the number of
student run health fairs. Studies examining how follow-up methods influence outcomes after a
health fair are lacking. We hypothesize that increased communication between student
pharmacists and physicians will improve outcomes. Therefore, the purpose of this study is to
determine whether or not faxing patients blood pressure results to their primary care physician
following a health fair will improve outcomes.
Methods: This prospective, randomized, cohort study is currently being carried out by
pharmacists and student pharmacists from Sullivan University College of Pharmacy. Approval
for this study was obtained from the Sullivan University College of Pharmacy Institutional
Review Board. Blood pressure screenings are being conducted at health fairs throughout the
Louisville, KY area from September 2012- April 2014, with follow-up continuing through May
2014. Written consent will be obtained from each participant. To be included in the study,
patients aged 18 or older must present in a hypertensive state (average of two readings showing
systolic blood pressure to be >140 mmHg or diastolic >90 mmHg). In addition, patients must
have a primary care physician and be capable of providing a follow-up blood pressure
measurement. Patients who present with a systolic blood pressure >180 mmHg or diastolic >110
mmHg will be excluded. Patients will be randomized to have their blood pressure results either
faxed or not faxed to their primary care physician. All patients will receive 2- and 6-week
follow-up phone calls. Interventions made since the health fair, as well as SBP and DBP readings
will be documented at each follow-up interval.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-241
Title: Evaluation of glycemic management in parenteral nutrition patients in an inpatient setting
to support educational interventions
Primary Author: Celeste Hollensead, University of Kentucky College of Pharmacy, Kentucky;
Email: c.hollensead@uky.edu
Additional Author(s):
Christopher Miller
Purpose: Parenteral nutrition (PN) provides nutrition to patients who have appropriate
indications and cannot be fed by other routes. One of the major metabolic complications
associated with this therapy is hyperglycemia. Patients at risk for poor glycemic management
include those with a history of diabetes, critically ill, obese, etc. An added challenge has been the
shortage of intravenous lipids. This shortage has resulted in attempting to achieve caloric
requirements primarily through protein and dextrose calories. This study is a retrospective, single
center evaluation, assessing glycemic management of PN patients deemed to be at a high risk for
this metabolic complication.
Methods: This study is being submitted to the institutional review board for exemption approval.
High risk patients, specifically those with a history of diabetes, who received PN from April 1,
2012 to November 1, 2013, will represent the study sample to be evaluated. Key study data will
be obtained using the institutions electronic medical record. The following information on each
subject will be investigated and documented over the first seven days of PN therapy: age, weight,
height, BMI of the patient, admission to critical care versus a non critical care unit, number of
blood glucose levels exceeding 180 mg/dl, amount of dextrose calories in the PN formula and
assessment in mg/kg/min, order initiated for sliding scale insulin (SSI), order initiated for point
of care blood glucose checks, amount of SSI used, and amount of insulin placed in PN bag. All
patients greater than 18 years of age and assessed to be at high risk based on patient history will
be included in this study. All data will be recorded without patient identifiers in order to maintain
confidentiality. This study data will be analyzed, summarized, and reported to guide our
educational focus in attempting to minimize this metabolic complication.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-242
Title: Use of aspirin and newer antiplatelet medications following acute myocardial infarction in
Scotland
Primary Author: Alexandra Hurst, University of Kentucky College of Pharmacy, Kentucky;
Email: alex.hurst@uky.edu
Additional Author(s):
Stuart McTaggart
Purpose: The use of aspirin (ASA) and newer antiplatelet medications (NAM) following AMI is
well established. However it is not known whether these are used in clinical practice according to
current guidelines. We used routinely collected health information to examine the use of ASA
and NAM following AMI and the effects treatment has on mortality by gender and age-specific
populations.
Methods: The national database of acute hospital admission was used to identify patients
admitted with AMI between January and December 2010. Patients were excluded if coded as
subsequent MI or prior admission of MI in the preceding 5 years. The national prescribing
information system (PIS) holds information on all National Health Service prescriptions
dispensed in the community and includes a patient identifier that provides demographic
information and enables linking of prescription event and linking to other data sets. A
prescribing history was extracted from PIS for those patients in the identified cohort receiving
any prescription for ASA or a NAM in the 3 months prior to their AMI through December 2012.
Patients were categorized by treatment; either ASA alone, NAM alone, ASA + NAM, or neither;
in 3 month intervals for the study duration. Additionally, patients were stratified by gender and
age <70 and 70+ years. Patients who died during a time period and for whom no prescription
data was found were categorized using last treatment carryover.
Results: We analyzed data for 9,778 patients. At 3 months post-AMI, 91.2% of patients were
receiving either ASA, a NAM or both: the majority both (58.7%). Younger patients were more
likely to be on the combination than older patients (68.8% vs 48.1%) at 3 months and males
more likely than females (62.7% vs. 52.5%) to be receiving the combination. All cause mortality
at 3 months in females was 23.0% compared with 13.8% in males (RR=1.67; 95%CI: 1.53-1.82)
and this increased relative risk persisted throughout the study period. Risk was greatest for
younger females compared with younger males: 10.1% vs. 4.9% mortality; RR=2.06; 95%CI:
1.65-2.56. Based on treatment at 3 months, ASA + NAM had the lowest overall mortality in all
gender and age groups. However females did less well with mortality of 17.7% vs. 11.6% for
males (RR=1.52; 95%CI: 1.33-1.75). Higher mortality rates were observed for females compared
with males of a similar age across all treatments analyzed, with the exception of ASA + NAM
and neither ASA or NAM: 26.8% vs. 28.4% mortality respectively for older females and males
receiving ASA + NAM and 72.2% vs. 73.5% mortality respectively for those receiving neither
ASA or NAM.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Mortality in patients discharged from hospital following AMI is higher in females
than males and the difference is greatest in younger patients. ASA and NAM are generally used
according to guidelines and the ASA + NAM combination produced the best survival rate in all
gender and age groups studied. However, females were less likely to be prescribed this treatment
than males of an equivalent age. Whether this, or other factors, contributes to the differences in
mortality warrants further investigation.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-243
Title: Cost analysis of a pharmacy intern program at a tertiary academic medical center
Primary Author: Bridgette Kanz, University of Kentucky College of Pharmacy, Kentucky;
Email: bakanz2@uky.edu
Additional Author(s):
Craig Martin
Casey May
Kathleen Faulkenberg
Purpose: With the introduction of the Pharmacy Practice Model Initiative in 2010, the role of
the pharmacy intern has expanded. This study evaluates pharmacy interns employed as pharmacy
extenders in a tertiary academic medical center setting. Pharmacy interns complete clinical as
well as technical tasks, with the bulk of their workload revolving around admission medication
reconciliations. The purpose of this study is to quantify the value of completing an admission
medication reconciliation and to determine the cost effectiveness of utilizing pharmacy interns to
complete this task versus a pharmacist.
Methods: This study is pending Institutional Review Board approval. The electronic medical
record database will be utilized to identify admission medication reconciliations completed by
pharmacy interns between May 2012 and May 2013 and those completed by pharmacists prior to
the initiation of the pharmacy intern program between January 2011 and December 2011. Three
outcomes will be measured including the number of reconciliations completed, the complexity of
the reconciliations, and the average cost of the reconciliations. Each document will be evaluated
for the number of home medications reported as well as the source of the information and
assigned a corresponding complexity factor. The variance of complexity across groups will be
compared using the Wilcoxon Rank Sum test. Each complexity factor will also correspond to an
average time to completion. The cost of each admission medication reconciliation will then be
calculated using average pharmacist and pharmacy intern hourly salaries. The average cost per
complexity factor for each group will be compared to determine what levels of medication
reconciliations each group more efficiently completes. Finally, Students t-test will be used to
detect significant differences in the number of medication reconciliations completed by each
group.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-244
Title: Prescribing error point prevalence study at a National Health Service tertiary academic
medical center
Primary Author: Ashley Lanham, University of Kentucky College of Pharmacy, Kentucky;
Email: ashley.lanham@uky.edu
Additional Author(s):
Bridgette Kanz
Melody Ryan
Steve Williams
Douglas Steinke
Purpose: After participating in the EQUIP Prescribing Error study, medication safety became an
integral part of yearly competencies for this pharmacy. Seven different types of practitioners
have prescribing powers within the English hospital structure including pharmacists, consultants,
nurses, foundation year 1 physicians, foundation year 2 physicians, specialist trainee/trust grade
physicians, and staff grade physicians. The purpose of this audit was to identify the number,
severity, and origin of some prescribing errors with a particular interest in high-risk category
drug prescribing errors.
Methods: A prescription chart review was completed on thirty-four different wards and the
pharmacy dispensary on one randomly chosen day in July 2013. Each newly prescribed item was
recorded by the pharmacist in that area and assessed for accuracy. A prescribing error was
defined as an unintentional, significant reduction in the probability of treatment being timely and
effective or an increase in the risk of harm when compared to generally accepted practice as
written by Dean et al in What is a prescribing error? published in Quality Health Care in 2000.
Each identified error was categorized into error types including indication, drug selection, dosage
regimen, administration information and missing product details. An error severity scale
identified errors as minor, significant, serious or potentially lethal. The data was initially
analyzed by two fourth year American pharmacy students and then errors where validated by a
consultant physician and pharmacist. Prescribing errors were analyzed by grade of doctor, stages
of prescribing, severity of error, and British National Formulary category of drug.
Results: A total of 1,892 prescriptions were documented and analyzed; A total of 212 errors
were identified or 11.21% of prescriptions that day. Foundation Year 1 Physicians had the
highest prescription error rate at 21.3% of prescriptions written while pharmacist prescribers did
not have any identified errors. The majority of errors (73.11%) were significant errors, with the
next largest category being minor errors at 22.17%. Only two potentially lethal errors were
identified or 0.94% of errors. The most common types of errors reported were omission on
admission of a home medication, an overdose, an underdose or omission on discharge. By far the
most common type of drug with a prescription error was analgesics, including both opioid and
non-opioid at 16.04% of errors, followed next by bronchodilators and antibiotics both at 5.66%
of errors. Errors on high risk medication prescriptions accounted for 17.92% of all errors;
10.85% being opioids, followed by 5.66% of anticoagulant prescriptions.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Overall, the error rate recorded this year was higher than those recorded in the past
(9.6% in 2011 and 10.2% in 2010) but the majority of errors were still committed on admission
or discharge, parallel with previous point prevalence audits. The introduction of further efforts to
improve medication safety are necessary and warranted such as the addition of electronic
prescribing systems, further education and supervision for young doctors, and expanded use of
pharmacist prescribers especially on admission and discharge.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-245
Title: Questions regarding the pediatric population while on-call for a pharmacy residency
program
Primary Author: Rachael Lewis, University of Kentucky College of Pharmacy, Kentucky;
Email: rachael.lewis@uky.edu
Additional Author(s):
Aaron M Cook
George A Davis
Robert Z Thompson
Purpose: Pharmacy residents are often exposed to a variety of patient age groups. One group
that might be foreign or intimidating is the pediatric population. While working an on-call shift
in our 24-hour, in-house, on-call program the questions and tasks that are required are
unpredictable and issues with pediatric patients are likely to occur. This study aims to analyze
the responsibilities relating to pediatrics that are expected of residents while working an on-call
shift at the University of Kentucky Chandler Hospital during a one year period.
Methods: This was a retrospective review of patient hand-off reports from the pharmacy
resident on-call service at the University of Kentucky Chandler Hospital. Reports from June
2011 thru June 2012 were reviewed and categorized by the nature, time, origin, and topic of the
call. Data from each report was entered into the data collection program (REDCap) and validated
for patient service and call type. Missing data for each call was determined by medical record
review whenever feasible. Planned statistical analysis primarily consists of descriptive statistics
and tests for comparison such as student t-test or Chi squared analysis.
Results: Results to be presented at the ASHP Midyear Meeting.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-246
Title: Penicillin skin testing: potential cost impact on aztreonam utilization in patients with
reported penicillin allergies
Primary Author: Timothy Marr, University of Kentucky College of Pharmacy, Kentucky;
Email: david.marr@uky.edu
Additional Author(s):
Regan A. Baum
George A. Davis
Purpose: Aztreonam, a synthetic monobactam antibiotic, is commonly utilized in penicillin
allergic patients. The academic medical center is ranked within the top 15 percent of aztreonam
utilization among University HealthSystem Consortium (UHC) hospitals. Our institution does
not utilize penicillin skin testing (PST) to identify patients with reported allergies who could
safely receive penicillin antibiotics. Allergic reactions to beta lactams are reported by 10 percent
of patients, 80 percent of which will have a negative skin test and could receive a penicillin. This
study will determine potential cost savings of PST by evaluating aztreonam utilization and
potential conversion to less costly antimicrobials.
Methods: Retrospective study designed to evaluate the utilization of aztreonam in a subset of
patients reportedly allergic to penicillin antibiotics conducted at an academic medical center.
Following IRB approval, aztreonam utilization from January 1, 2012 to December 31, 2012 was
obtained through the UHC database and electronic medical record. The data were randomized
with the first 100 eligible patients included. Patients 18 years of age and older with a reported or
unknown allergy to penicillin were considered for inclusion. Pregnant patients were excluded.
The primary objective is to determine the potential cost impact of changing antimicrobial
regimens in penicillin skin test negative patients from aztreonam to a beta lactam antibiotic.
Secondary objectives include characterizing the type of allergic reaction, type of care provider
who documented the allergy, and the infection being treated. This study will be utilized to
develop a penicillin skin testing program within the antimicrobial management team and an
accompanying protocol.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-247
Title: Effect of oral examinations on written cumulative final exam scores
Primary Author: Lance Murphy, Sullivan University College of Pharmacy, Kentucky;
Email: lmurph8942@my.sullivan.edu
Additional Author(s):
Ryan Timmons
Drew Cates
Purpose: Pharmaceutical care has evolved into a more patient-centered environment where it is
necessary for students to be able to communicate verbally with patients, caregivers and other
health care providers. The purpose of this study was to assess the impact of oral examinations on
student learning in an advanced self-care pharmacy elective course. The study aims to detect a
final exam score difference amongst students who undergo oral versus written examinations
prior to the final exam. The goal of implementing oral examinations is to enhance students
knowledge and verbal communication skills as it pertains to self-care.
Methods: The Sullivan University College of Pharmacy Institutional Review Board (IRB)
approved this study on July 18, 2013. The methods for this study consisted of changing the
written style of examinations within the academic quarter to oral examinations for the study
group. The final examination of this study group would be a written, cumulative final, as similar
as possible to the previous two academic classes, who took the same Advanced SelfCare/Durable Medical Equipment elective. Other than the oral examinations before the final
examination, the study group was taught and covered the same topics as the control groups of
students from 2011 and 2012. Upon IRB approval, the de-identified final examination scores
from the previous two years were recovered from archive. These scores were used to compare to
the study groups scores as they completed the course in September 2013. The scores were
analyzed using a two-tailed t-test with 95 percent confidence intervals, looking for any
significant changes that could be attributed to the implementation of oral examinations. Other
differences between the two groups were ignored, under the advisement of the IRB, to keep all
student/subject personal information eliminated.
Results: The mean final examination score of students who received written examinations
throughout the academic quarter (control) was calculated at 86.61 percent (N equals 52). The
mean score of those who received oral examinations was 91.78 percent (N equals 27). When
analyzed via two-tailed t-test with a power of 80%, there was a significant increase (P less than
0.05) in score for those who were assessed with oral examinations (5.16 percent; 95 percent CI:
0.95 percent to 9.38 percent). The control group was also separated by academic year. Students
taking the class in 2011 (N equals 24) took written examinations, and had a significantly lower
final exam average (Mean equals 82.83 percent). Those with oral examinations had a mean
increase of 7.02 percent (95 percent CI: 1.61 percent to 12.44 percent, P less than 0.01). Those
students taking the class in 2012 (N equals 28) also took written examinations, and did not have
a significant difference in final scores (Mean equals 89.86; difference equals 1.92; 95 percent CI:
negative 1.92 percent to 5.31 percent, P greater than 0.05).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Oral examinations as the knowledge assessment of choice for an academic quarter
(prior to a written final exam) resulted in an increased cumulative final examination, averaging
5.16 percentage points. With this, it can be assumed that such oral examinations had a positive
effect on student knowledge retention for their cumulative final. Due to the lack of increase
between one subgroup and the study group, along with the relatively small and unequal group
distribution, it is suggested that there be more research on oral examinations and their effect on
student learning.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-248
Title: Prospective, randomized, cohort study on HbA1c outcomes following a student led
diabetes education program.
Primary Author: Jason Newton, Sullivan College of Pharmacy, Kentucky;
Email: jnewto1799@my.sullivan.edu
Additional Author(s):
Rachel Damaske
Harrold Barrantes
Purpose: Historically, diabetes education classes have shown to improve long-term diabetes
management and HbA1c outcomes. In this student led, community based diabetes education
program patients will attend quarterly meetings at a physicians clinic. At each meeting the
patient will hear talks on how to properly control their blood glucose. Also the patients weight
and latest HbA1c results will be acquired for longitudinal assessment. Ideally, the program will
show improved HbA1c outcomes in the year of education.
Methods: Patients will attend quarterly student led meetings at the community physicians clinic.
All patients will receive call and email reminders for upcoming meetings from physicians nurse
and/or student pharmacists. At each meeting patients weight and latest HbA1c results will be
collected and tracked for the duration of the study. Data is currently being collected by student
pharmacists.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-249
Title: Role of the pharmacy residency on-call program in management of direct thrombin
inhibitor (DTI) use for heparin-induced thrombocytopenia (HIT)
Primary Author: Zachary Noel, University of Kentucky College of Pharmacy, Kentucky;
Email: zrnoel2@uky.edu
Additional Author(s):
George Davis
Purpose: Direct thrombin inhibitors (DTI) are the drug of choice for patients with suspected or
confirmed heparin-induced thrombocytopenia (HIT). DTIs require close monitoring and frequent
dosage adjustments to stay within a narrow therapeutic range, and studies have shown that
pharmacist-managed DTI programs can increase safety and efficacy. Pharmacy residents are
trained to help manage DTIs as part of the 24-hour on-call pharmacy service at an academic
medical center. The purpose of this study is to provide a descriptive evaluation of the role of an
on-call pharmacy residency program for the management of DTI use.
Methods: METHODS : This was a retrospective review of patient hand-off reports from the
pharmacy resident on-call service at an academic medical center. Reports from June 2011 thru
June 2012 were reviewed and categorized by the purpose, time, origin, and topic of the call. Data
from each report were entered using Research Electronic Data Capture (REDCap) software and
validated using medical record review. Planned statistical analysis will include descriptive
statistics and Students t-test or Chi squared analysis for comparative analysis.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-250
Title: Utilization of the AIDS Drug Assistance Program versus Medicaid using medication
possession ratio
Primary Author: Jenna Parrett, University of Kentucky, Kentucky;
Email: jenna.parrett@uky.edu
Purpose: Given the uncertainty regarding how the Patient Protection and Affordable Care Act
(ACA) will affect AIDS Drug Assistance Programs (ADAP) nationally as well as the uncertainty
regarding whether ADAPs foster positive patient behaviors and outcomes, such as increased
medication adherence, a study comparing the adherence of patients in an AIDS Drug Assistance
Program and Medicaid as well as the utilization of these programs could provide insight into
how the ACA may affect patients with HIV/AIDS who utilize ADAP to attain their medications
but are newly eligible for Medicaid.
Methods: This research is pending approval by the Institutional Review Board. Data will be
collected retrospectively from records compiled between January 1, 2012 and December 31,
2012 from the infectious diseases clinic at a tertiary academic medical center as well as
prescription records from the associated outpatient pharmacy. Only records from patients
actively enrolled in ADAP or Medicaid during these dates will be used. The medication
possession ratio (the percentage of days a patient is in possession of a prescription) will be
calculated for each highly active antiretroviral therapy (HAART) medication for each patient in
order to extrapolate each patient's adherence. Multivariable ordinal logistic regression will be
used to assess whether the compliance variables (sociodemographic information, medical
history, laboratory data, and pill burden) are either positively or negatively associated with
ADAP or Medicaid utilization. The average medication possession ratio for ADAP patients will
be compared to Medicaid patients to determine if one program fosters adherence more so than
the other. Stata v13.0 statistical software will be used to analyze the data.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-251
Title: Analysis of antimicrobial consultation in the pharmacy residency on-call program
Primary Author: Micah Pepper, University of Kentucky, Kentucky;
Email: micah.pepper@uky.edu
Additional Author(s):
Aaron Cook
George Davis
Purpose: Antimicrobial agents are utilized extensively in the inpatient setting. Many of these
agents require monitoring and discretion during implementation. This is an area where
pharmacists can play a vital role in improving the safety, efficacy and appropriate use of these
agents. At an academic medical center, pharmacy residents participate in a 24-hour on-call
service in which they are available for consultation concerning medications such as
antimicrobials. The purpose of this study is to evaluate the incidence and nature of antimicrobial
consultation provided during the on-call service, with regard to appropriate dosing and time of
consultation.
Methods: This was a retrospective review of patient hand-off reports from the pharmacy
resident on-call service at an academic medical center. Reports from June 2011 thru June 2012
were reviewed and categorized by the purpose, time, origin, and topic of the call. Data from each
report were entered using Research Electronic Data Capture (REDCap) software and validated
using medical record review. Planned statistical analysis will include descriptive statistics and
Students t-test or Chi squared analysis for comparative analysis.
Results: Data and results are currently being analyzed and will be presented at the 2013 ASHP
Midyear Clinical Meeting.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-252
Title: Determining undergraduate factors that predict academic success in pharmacy school
Primary Author: Stephen Polley, University of Kentucky College of Pharmacy, Kentucky;
Email: stephen.polley@uky.edu
Additional Author(s):
Joe Fink
Helen Garces
Purpose: Various papers have been published in an effort to ascertain what factors make a
pharmacy student successful. A variety of factors and endpoints have been considered in these
studies. With the opening of a multitude of new pharmacy schools, both the supply and demand
sides of the market for pharmacists have changed greatly. This leads one to wonder if this market
change has caused a difference in the factors that predict academic success. The objectives of
this study are to determine which factors are significant for predicting academic success and to
create a multivariate regression of these significant factors.
Methods: This study has been submitted for approval by the UK Institutional Review Board.
Information was collected and blinded from the UK College of Pharmacy Class of 2013. Factors
such as GPA (Overall, Math, and Science), type of undergraduate institution (public vs. private
vs. community), PCAT scores (Overall, Chemistry, Biology, Math, and Reading), extracurricular
activities, pharmacy work experience, and technician certification were collected from data
submitted through PharmCAS applications. Interview scores (individual, group, and total) were
collected from admissions data. The last set of data was collected from pre and post pharmacy
school Health Sciences Reasoning Test data. Academic success is being measured by cumulative
pharmacy GPA and a sub-analysis being conducted defines the endpoint of academic success as
first-year GPA. Appropriate statistical tests will be performed to identify a positive, negative, or
neutral correlation between the factors listed above and the endpoint. The significance of each
factor will then be determined and from the list of significant factors a multivariate regression
will be formulated to predict pharmacy school GPA.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-253
Title: Development of a guideline regarding the reversal of anticoagulation
Primary Author: Josh Pruitt, University of Kentucky College of Pharmacy, KY;
Email: josh.pruitt@uky.edu
Additional Author(s):
Shannon Allcron
Michael Berger
Purpose: There have been several new anticoagulants that have come to the market in recent
years. Unfortunately, many of these new anticoagulants have no reliable antidote or reversal
agent. In an urgent setting where a patient is experiencing a life threatening bleed or at risk for
one, and is currently taking one of these new anticoagulants, there are currently no clear
treatment options for these patients. While there have been a few studies completed to address
this issue, lack of agreement on a first-line approach and limited sample size has not provided a
clear guideline on treatment options.
Methods: A PubMed primary literature search was conducted. Literature was reviewed to find
the most concrete and universally supported results. A comparison was made of the available
hospital formulary products, with those mentioned in the studies. Next, a document was
constructed that contained a flow chart for a step wise approach in reversing oral anticoagulants
in patients with a life threatening bleed or if they were in need of emergency surgery. The flow
chart was created to aid a pharmacist or physician to determine the appropriate first line therapy
for each agent in an efficient manner. An urgent reversal guideline containing ten anticoagulants
including oral agents was developed as well. The guideline provides each of the ten drugs class,
elimination half life, if the drug is removed by hemodialysis and to what extent, a reversal
strategy, and how to appropriately monitor the drug.
Results: The reversal flowchart and guideline were presented before the P&T committee for
review and were approved. Following approval, the tools were presented to the Medical
Executive Committee, where they were reviewed and accepted. The guideline and flowchart are
now implemented into the computer system where they are viewable under the hospitals training
materials section.
Conclusion: There is still no 100% effective reversal for many of these new agents, and until
there is one we must constantly stay updated with the evolving research and case studies to stay
informed of the best therapeutic options for these patients. Early feedback from pharmacists
includes positive remarks about the utility of having this information quickly available;
especially, because it is a difficult topic, and in a life-threatening situation, being able to make a
quick recommendation is a necessity.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-254
Title: Effect of pharmacy involvement on medication discrepancies during the admission
medication reconciliation process at a community hospital
Primary Author: Nana- Ama Quansah, University of Kentucky, Kentucky;
Email: nana-ama.quansah@uky.edu
Additional Author(s):
Josh O'Bryan
Purpose: Medication reconciliation discrepancies are emerging as contributing factors to
readmission rates in most health care institutions. One study showed that 14.3% of patients that
experienced medication discrepancies during a hospital admission were re-admitted within 30
days compared to 6.1% of patients without medication discrepancies. The objective of this study
was to determine the effect of pharmacy involvement in reducing medication reconciliation
discrepancies with hospital admissions and eventually decreasing readmissions in the institution.
Methods: Prospective and retrospective medication reconciliations were conducted at a rural
community hospital. Pharmacists and pharmacy students were utilized to reconcile patient
medication lists prospectively upon admissions and retrospectively after the medication
reconciliation had already been completed by a nurse. The assessment focused on patients'
reported medications in comparison with their outpatient pharmacy and the medication list
documented by the nurse. The primary outcome of this study was the number of discrepancies
found by pharmacy involvement in the medication reconciliation process.
Results: Forty-five patients had their medications reviewed by either a pharmacist or a pharmacy
student upon admission, 25 prospective and 20 retrospective. The total number of medications
reviewed was 517 (average of 12 per patient). The average amount of time spent per patient was
20 minutes and the total number of discrepancies detected was 146 (28%). The total number of
discrepancies from retrospective medication reconciliations that were already completed by
nursing was 91, approximately 5 additional errors per patient. There were 55 discrepancies when
comparing the patient medication lists to the outpatient pharmacy medication lists.
Conclusion: The results of this assessment showed that involvement by pharmacy in the
medication reconciliation process reduced the risk of medication discrepancies. Further studies
would be needed to see how these results affected the readmissions of the patient population in
the institution, however current literature suggests that decreased medication discrepancies
would indeed decrease the readmission rates.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-255
Title: Developing a spheroid culture system in non-small cell lung cancer cell lines for assessing
response to therapeutic entities
Primary Author: Ashley Repholz, University of Kentucky College of Pharmacy, University of
Kentucky;
Email: amre225@uky.edu
Additional Author(s):
Ryan Hughes
E.P. Black
Purpose: Despite rigorous research, cancer is still the second leading cause of death in the
United States with lung adenocarcinoma marking the highest mortality rate. Because of latestage disease diagnosis and relative insensitivity to therapy, a need exists for new therapeutic
entities and strategies for use. New compounds are screened for activity using two-dimensional
(2-D) models in-vitro. However, recent studies have provided evidence that 2-D models may not
be physiologically representative of in-vivo conditions and therefore therapeutic outcomes. The
lack of accurate, high-throughput, and cost-efficient methods to screen new pharmacological
agents increases the cost and time to clinical use for most new compounds. We propose that the
development of a three-dimensional (3-D) cell culture model will provide a high-throughput,
efficient, and effective model for response of tumors to new entities.
Methods: Non-small cell lung cancer cell (NSCLC) lines were trypsinized from 2-D culture and
seeded in very-low adherence plates. Following 72 h growth digital images of the cells were
captured. Next, 72h spheroids were collected and evenly redistributed into new very-low
adherence plates. After 24 h, the spheroids were treated with a therapeutic agent and evaluated
for cell cycle state, apoptotic state, and pharmacodynamic response to treatment.
Results: The structure of cells grown in very-low adherence dishes varied among cell lines,
ranging from sheets of loosely aggregated cells to compact, spherical masses of cells. Results of
the cell cycle analysis indicate changes in susceptibility to the therapeutic agent in 3-D cell
cultures in comparison to 2-D cell culture models. Further experiments demonstrated that proapoptotic proteins were expectedly induced in some spheroid cultures and not others.
Conclusion: NSCLC cells grown in 3-D differed in sensitivity to some agents relative to 2-D
counterparts. Future directions of this project include gene expression predictors of response to
select agents in cells grown in 3-D and developing a high-throughput platform for treatment and
assay.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-256
Title: Uptake and patterns of use of dabigatran and rivaroxaban in primary care in Scotland
Primary Author: Christie Scott, University of Kentucky College of Pharmacy, University of
Kentucky College of Pharmacy;
Email: clscott325@uky.edu
Additional Author(s):
Stuart McTaggart
Purpose: Dabigatran and rivaroxaban are new anticoagulant drugs that offer advantages over
warfarin in terms of fixed daily dosing and no requirement for INR monitoring. However, they
are considerably more expensive and there are concerns over the inability to monitor therapeutic
effect and the lack of a reversal agent. This study investigates the uptake and patterns of use of
these newer anticoagulants in primary care in Scotland using routinely collected health
information.
Methods: The national prescribing information system (PIS) holds information on all National
Health Service (NHS) prescriptions dispensed within the community in Scotland. This includes a
unique patient identifier giving access to demographic information and allowing events for an
individual to be linked together. Information was extracted from PIS on the numbers of people
dispensed a prescription for dabigatran, rivaroxaban or warfarin in each month of 2011 and 2012
in each NHS administrative area. Areas were then categorized as rural or urban and the data
aggregated. Rates of use were calculated against National Records of Scotland population
estimates. Age and gender was collected for those people dispensed each drug during 2012 in
order to characterize the treated populations. Data from Q3 and Q4 2012 was used to identify
those who had a prescription dispensed for dabigatran or rivaroxaban in Q4 and had no such
prescription in Q3, i.e. were initiated on therapy during Q4, and whether they had previously
received warfarin. Data was stratified by drug, location, gender and age
Results: Warfarin continues to be the most widely used oral anticoagulant but uptake of
dabigatran and rivaroxaban has been rapid and began soon after acceptance for use. Uptake was
more rapid and greater in rural areas for both drugs. Although rivaroxaban became available
after dabigatran it quickly overtook dabigatran in both rural and urban settings. By the end of
2012 the numbers of people per 100,000 people aged over 50 years being dispensed dabigatran,
rivaroxaban or warfarin each month were 43, 50 and 2106 respectively in rural areas and 9, 24
and 1693 respectively in urban areas. The median age of people treated with both dabigatran and
rivaroxaban was 72 years and was lower than the 74 years for those treated with warfarin. For
patients initiated on dabigatran or rivaroxaban during Q4 2012, 21.7% in rural areas had
previously been treated with warfarin against 32.1% in urban areas.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Uptake of the newer anticoagulants has been rapid and this occurred faster and to a
greater extent in rural compared with urban areas. This could be a reflection of relative ease of
access to INR clinics influencing the choice between warfarin and these drugs. However there
are concerns in terms of the ability to monitor therapeutic effect and the management of bleeding
events. The PIS data could be used to identify unexpected medication discontinuation and/or
linked with other routinely collected mortality and morbidity data to further define the efficacy
of these potential substitutes for warfarin.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-257
Title: Antibiotic prescribing patterns upon inpatient or emergency department discharge in the
state of Kentucky
Primary Author: Benjamin Scott, University of Kentucky College of Pharmacy, Kentucky;
Email: bjscot3@uky.edu
Additional Author(s):
David J. Feola
Craig A. Martin
Purpose: Antibacterial drug use is a major risk factor for bacterial resistance. Most studies
examining the use of antimicrobials are focused upon inpatient prescribing, and most
antimicrobial stewardship published data is in the hospital setting. Currently, there are no studies
that compare hospital prescribing patterns upon discharge in the state of Kentucky. The goal of
this study is to identify the prescribing patterns of outpatient antibiotics after a hospital stay or
ED visit in the state of Kentucky. Secondary goals are to determine differences in prescribing
patterns using hospital demographic and geographic information.
Methods: The Kentucky Medicaid Database was utilized to collect data over a span one year.
Antibiotic prescriptions that were filled within 72 hours after a patient discharge were linked to a
specific hospital stay or ED visit. Each antibiotic prescribed was also linked to patient
demographic information as well as diagnosis codes. All data was recorded without patient
identifiers and confidentiality was maintained. The occurrence rates of different antibiotic
prescriptions were identified. The resulting antibiotic data was then analyzed based on the
hospital demographic information from which they were prescribed and geographic location.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-258
Title: Pharmacodynamics of intravenous levofloxacin 750 mg in morbidly obese individuals
Primary Author: Andrew Stacy, University of Kentucky, Kentucky;
Email: atstac01@gmail.com
Additional Author(s):
Aaron Cook
Craig Martin
Purpose: Many antimicrobials display altered pharmacokinetics in obese patients. A recent
study demonstrated more rapid clearance of levofloxacin in the morbidly obese. Several studies
have shown that fluoroquinolone success correlates with the ratio of area under the
concentration-time curve to the minimum inhibitory concentration of the organism (AUC:MIC).
Different AUC:MIC thresholds are necessary to achieve success in Gram positive (>30) and
Gram negative (>125) organisms.
Methods: The institutional review board approved this study. A Monte Carlo simulation using
pharmacokinetic parameters from 15 morbidly obese individuals who had received a onetime
dose of IV levofloxacin 750 mg were used to evaluate AUC:MIC ratios for hypothetical MICs.
For each MIC 10,000 hypothetical patients were generated and used to evaluate probability of
target attainment (PTA). AUC:MIC thresholds of 30 and 125 were designated to evaluate
success against Gram positive and Gram negative organisms respectively. Subsequently, PTA
for target organisms was determined using MIC distributions from a large database.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-259
Title: Professional Development Experience: Residency Alumni Perceived Benefits
Primary Author: Robert Thompson, University of Kentucky College of Pharmacy, Kentucky;
Email: rzthom2@uky.edu
Additional Author(s):
Craig Martin
Aaron Cook
Daniel Johnson
Purpose: The Professional Development Experience (PDE) was first described in 2006 and has
been a key element to the pharmacy residency programs at this institution for over 20 years. The
PDEs main goal is to give pharmacy residents the opportunity for development of pharmacy
practice and management skills and to build a professional network. A secondary goal is to gain
knowledge of other practice settings and gives residents the chance to implement clinical
services from other institutions into their practice. The experience has been a long-standing
aspect of the pharmacy residency programs and the purpose of this report is to assess the
perception of benefits from the alumni who have participated.
Methods: Pharmacy residency alumni from the year 2000 to 2013 were surveyed to gain
knowledge and determine the benefit of the PDE. Alumni were asked to complete a 17-question
survey and to comment on the knowledge gained from the PDE distributed via REDCap.
Questions included institutions visited, personal cost of trip, activities on site, mode of
transportation and perceived goal of the experience.
Results: The survey had a response rate of 56% (75/133) to our survey. Each residency class
was represented in the data, as well as, every subspecialty. Overall alumni agreed that the PDE
was a beneficial experience for them on both a professional and resident bonding level.
Responders believed that the PDE was a positive 95% (71/75) and beneficial aspect of their
residency training. Alumni agreed 89% (67/75) that the PDE gave them an opportunity to
network with other practitioners and residents. More data will be presented at ASHP Midyear
Clinical Meeting.
Conclusion: The Professional Development Experience has provided residents at this pharmacy
residency program the opportunity to grow both professionally and strengthens the personal bond
of residency classes. Residency alumni agreed that this was a beneficial experience and it
provided them with the chance to network with other practitioners and residents.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-260
Title: Structured self-awareness and career exploration programming for first-year student
pharmacists
Primary Author: Molly Trent, University of Kentucky College of Pharmacy, Kentucky;
Email: mjtren2@uky.edu
Additional Author(s):
Kelly Smith
Helen Garces
Purpose: Entering pharmacy students may lack sufficient self-management skills to quickly
adjust to the rigors of a Doctor of Pharmacy program. Students complete standardized
assessments regarding their learning styles and strengths, but often fail to integrate such results
into a customized plan for success. The 2013 Center for Advancement of Pharmacy Education
(CAPE) Educational Outcomes' emphasis on the affective domain reflects a growing need within
academia to enhance these skillsets. Thus, programming for first-year student pharmacists was
developed to facilitate early self-reflection and career exploration in a College of Pharmacy. The
process to frame, implement and evaluate such programming was evaluated.
Methods: A fourth-year academic administration rotation student was charged with the creation
and implementation of programming to inspire first-year students to utilize self-reflection, grow
in emotional intelligence and assume responsibility for their own professional success.
Orientation was chosen as the ideal time to deliver this content, due to limited distractions that
would hinder reflection time and the need to reinforce such behaviors early in the curriculum to
aid in the transition process to professional school. The Golden Circle concept, popularized
through a TED Talk by Simon Sinek, was used to frame the project. Sequential activities
consisted of large group presentations, with corresponding assignments submitted via a learning
management system. In Phase I, students developed a why statement to define their professional
purpose and passion. Phase II focused on strengths and weaknesses informed by the results of
required programmatic assessments (Health Sciences Reasoning Test and Motivated Strategies
for Learning Questionnaire), as well as discussing personalized approaches to time and stress
management. Career exploration and entrepreneurial thinking followed in Phase III. Major areas
for personal improvement were identified through thematic analysis. Participant impressions
about the value of the program were measured according to a four-point Likert scale.
Results: Each participant (n=114) completed the post survey, of which 105 students rated the
program as either good or excellent on a four point Likert scale. Students were actively engaged
during the large-group presentations and were especially receptive to the delivery of such
programming by a senior pharmacy student. A commonly reported area for self-improvement
was time management skills. Previously, no formal time management tool or systematic
guidance had been provided to assist students with these vital skills. Instead, students with
demonstrated or perceived academic difficulty were targeted for time management skill
enhancement. In response to these findings, the fourth-year student developed a comprehensive
time management plan with templates and manuals. The plan will be piloted in the spring of
2014, with the intent to subsequently engage all entering students in the program. The prevalence
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
of this self-perceived deficiency emphasized the need to integrate student development tools into
the formal curriculum, which will be explored in the Colleges ongoing curriculum revision
efforts. The American Pharmacists Association Career Pathway program was reinstituted as an
activity in an introduction to the profession course based upon student request for career
guidance.
Conclusion: A structured approach to guide entering pharmacy students in their self-awareness,
career considerations and self-improvement identified a number of areas that require large-scale
student development. Time management, which was anticipated to be an area of need, was most
commonly selected by participants for subsequent enhancement. Program delivery by a student
peer was well received. Expanded programming in and support of student development will be
critical as the Colleges ongoing curricular revision is predicated upon student self-empowerment
and motivation to accomplish educational outcomes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-261
Title: Does cigarette smoke cause interleukin production in cardiac stem cells?
Primary Author: Brunhilda Waingeh, Sullivan University College of Pharmacy, Kentucky;
Email: kuobrun@yahoo.com
Additional Author(s):
Houston K Acha
Wasana K Sumanasekera
Purpose: Cigarette smoke is a major cardiovascular risk factor and leading cause of death
around the world. This study investigates whether cardiac stem cells (CSC) produce interleukins
in response to exposure to cigarette smoke (CS), with the view of understanding the role of
inflammatory cytokines (including interleukins) as causative agents in CS-induced modulation of
cardiac stem cell signaling and functions. Although there are reports on modulation of
interleukin secretion due to CS exposure using different models, to date CS induced secretion of
interleukins has not been studied in CSC. The role of these interleukins in cigarette smokeinduced cardiovascular disease remains elusive.
Methods: Cigarette smoke extracts (CSE) were created by combusting cigarettes and dissolving
the puff in cell culture media. Cultured rat CSC were exposed to varying concentrations of CSE
(0%, 2%, 5% and 10%) for different exposure times (15 min, 1hr and 24hours). Whole cell
extracts were made, proteins were quantified, and equal amounts of protein from different
treatments were subjected to IL- 1 beta ELISA assay, which detects IL-1 beta secretion from
CSC due to CSE exposure.
Results: The results show that for all CSE exposure levels and exposure times studied, there was
significant increase in the secretion of IL-1 beta over the control (p 0.05 in all cases). Over short
exposure times (15 min, 1hr), CSE induces IL-1 beta secretion in a dose dependent manner, with
10% CSE inducing the highest production of IL-1 beta. However, over an extended period of
time (24 hours) 5% CSE exposure has resulted in an optimum IL-1 beta production.
Conclusion: These results clearly indicate that cigarette smoke promotes secretion of IL-1 beta,
which is a potent pro-inflammatory cytokine.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-263
Title: Outcomes of piperacillin-tazobactam monotherapy versus combination therapy for low
minimum inhibitory concentration (MIC) Pseudomonas aeruginosa bacteremia
Primary Author: Bethany Wattles, University of Kentucky College of Pharmacy, Kentucky;
Email: bethany.benyo@uky.edu
Additional Author(s):
Jeffrey M. Rybak
Craig A. Martin
Purpose: Bacteremia caused by Pseudomonas aeruginosa is a serious nosocomial infection
associated with poor outcomes and high mortality. Piperacillin-tazobactam is an agent commonly
used to treat these infections but there is controversy as to whether monotherapy or combination
therapy is more effective. Lack of clinical data along with suggestions to change the
susceptibility breakpoint from less than or equal to 64 mcg/mL to less than or equal to 16
mcg/mL for piperacillin-tazobactam has led to a need for further investigation.
Methods: The institutional review board approved this retrospective, cohort study. Our study
includes patients from January 2007 to May 2013 with a positive Pseudomonas aeruginosa blood
culture with an MIC of less than or equal to 16 mcg/mL. Patients who received at least 48 hours
of piperacillin-tazobactam treatment were sorted into the monotherapy group or combination
therapy group. The primary outcome studied was 30-day mortality attributable to infection with
secondary outcomes being duration of therapy and time to a negative blood culture. Monte Carlo
Simulations (n equals 10,000 simulations) were performed using culture results and published
population pharmacokinetic data for piperacillin-tazobactam. Probability of target attainment
(PTA) was calculated for intermittent infusion regimens of 3.375g and 4.5g every 6 hours.
Results: A total of 93 patients were identified for this study. Of these patients 24 received
piperacillin-tazobactam monotherapy while 69 patients received combination therapy. The
primary outcome of 30-day mortality attributable to infection was found to be 4.2 percent for the
monotherapy arm and 14.5 percent in the combination therapy arm (P equals 0.278). Average
duration of therapy was found to be 14 days in patients who received monotherapy versus 13
days in patients who received combination therapy (P equals 0.337). Average time to negative
blood cultures was determined to be the same for both groups at 3 days (P equals 0.136). The
Monte Carlo simulations determined the PTA for 50 percent time greater than MIC of
piperacillin-tazobactam for 3.375g and 4.5g every 6 hours to be 75 percent and 89 percent,
respectively.
Conclusion: Use of combination therapy in bacteremia caused by Pseudomonas aeruginosa was
not proven to decrease mortality in patients with a piperacillin-tazobactam MIC of less than or
equal to 16 mcg/mL.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-264
Title: Assessment of confidence and learning retention from oral examinations one academic
quarter after an ambulatory care elective
Primary Author: Kelsie Whitworth, Sullivan University College of Pharmacy, Kentucky;
Email: kwhitw7012@my.sullivan.edu
Additional Author(s):
Michaela Richardson
Jaclyn Robinson
Purpose: In the medical field, confidence is a key attribute that one must possess. It is essential
to answer questions with conviction to avoid instilling doubt in peers and patients minds. The
growing number of graduate schools has prompted a need to assess the best method of
examination to promote confidence whilst supporting knowledge retention after an elapsed
period of time. One method of assessing knowledge is oral examinations. Requiring critical
thinking by using a strategy such as oral examination will enhance retention of important
knowledge and cultivate confidence in providing life-saving information to patients and healthcare team members.
Methods: To test that oral examinations are best for building confidence, we gave students a
survey in an advanced ambulatory care class at a college of pharmacy assessing their confidence
level pre- and post- completion of the class. Secondly, we assessed students knowledge retention
ten weeks post course completion of the advanced ambulatory care class. The students were
given an oral midterm at week five and an oral final at week ten during course. At the end of
each lecture throughout the ten week course, the professor provided three sets of questions:
competency questions, category B questions, and category A questions. The student was required
to articulate the correct answers to all of the competency questions during the oral examinations,
taking no more than two minutes per question, to be considered a competent pharmacy student.
If the competency questions were answered correctly, the proctor proceeded to randomly select
one category B question for the student to answer. If the category B question was answered
correctly, the proctor proceeded to randomly select one category A question for the student to
answer. The content of the category B questions represented proficient skill/knowledge. The
content of the category A questions represented a distinguished skill/knowledge.
Results: The primary endpoint was to assess the confidence gained from oral examinations.
Students were given a survey pre and post completion of the course to assess the confidence lost
or gained. The survey had four questions asking how the student felt answering questions before
the course, how the student felt after the completion of the course, and if the student felt a
decrease/neutral/increase in confidence. Ninety-five percent of students gained confidence in
answering questions verbally. The secondary endpoint was to assess learning retention one
quarter after completion of the course using oral examinations. Ten weeks after the advanced
ambulatory care elective, students who had participated in the course were reexamined in the
same manner as the midterm and final. Each student was asked the same questions that he had
been asked during the course midterm and final ten weeks prior. Ninety-five percent of students
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
claimed that oral examinations helped them retain more knowledge compared to a multiple
choice test. Ninety-five percent of students passed the midterm and 100% of students passed the
final exam during the course. One quarter post completion, 45% of students passed the midterm
exam and 50% of students passed the final exam.
Conclusion: This study will allow researchers to evaluate the significance and importance of
oral examinations. It has been revealed that confidence significantly increases when a student
answers questions verbally.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-265
Title: Effectiveness of pharmacist-guided nicotine replacement therapy on smoking cessation
outcomes
Primary Author: Lisa Willinger, Sullivan University College of Pharmacy, Kentucky;
Email: lwilli0055@my.sullivan.edu
Additional Author(s):
Corey Willinger
Robert Napper
Sarah Raake
Purpose: This retrospective study will look at the quit rates of patients who are attempting to
stop smoking by using different forms of nicotine replacement therapy (NRT) under the
guidance of pharmacist-led Cooper Clayton Smoking Cessation Program. Results obtained from
this study will be used to determine the most successful smoking intervention strategies currently
utilized. The data obtained may guide how the current courses of the smoking cessation program
are led as well as to further research in the area of smoking cessation with an overall goal of
improving quit rates.
Methods: This study was submitted and accepted by the Institutional Review Board at Sullivan
University in Louisville, KY. All participants were made aware of the research and informed
consent was obtained from all study subjects. The data will come from retrospective chart
reviews of patients voluntarily entering into the Cooper Clayton Method to Stop Smoking
program. The smoking cessation classes take place in an outpatient setting of the InterNational
Center for Advanced Pharmacy Services (INCAPS) at Sullivan University College of Pharmacy
(SUCOP). The data to be collected and reviewed will include the NRT products that the patients
choose, the dose used, and the resulting quit rate. The study population will include patients from
a variety of backgrounds who are attempting to stop smoking with the aid of licensed
pharmacists trained in smoking cessation techniques using a 13-week program. Data will be
collected and stored in-house, in a secure, locked room within INCAPS. All data will be
analyzed on site using descriptive statistics, and additional evaluations of nominal data may be
done using the Chi-squared test as well as the Fishers exact test. All participants will be deidentified, and confidentiality will be maintained when presenting the data.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-266
Title: Incidence of hypoglycemia and sulfonylurea use in an inpatient population
Primary Author: Lindsay Wilson, Sullivan University College of Pharmacy, Kentucky;
Email: lwilso8991@my.sullivan.edu
Additional Author(s):
Kimberly Elder
Crystal Owens
Steve Kain
Sean Boyle
Purpose: Guidelines currently recommend against the use of sulfonylureas for most inpatients
and suggest using insulin as monotherapy instead. There is evidence that links inpatient
sulfonylurea use to hypoglycemia episodes, and inpatient hypoglycemia can increase morbidity
and mortality. The primary objective of this study is to determine if the use of inpatient glipizide
is associated with hypoglycemia episodes. The secondary objective is to assess risk factors
present in patients who experience hypoglycemia during hospitalization. Investigating the
incidence of hypoglycemia related to the use of glipizide could potentially improve medication
therapy decisions in inpatients with hyperglycemia within this institution.
Methods: This retrospective chart review was approved by the appropriate Institutional Review
Boards. The inpatient electronic medical record will be used to collect data for the study. To be
included in the study, patients must have a diagnosis of type 2 diabetes mellitus (T2DM), be at
least 18 years old, and have an inpatient stay on an internal medicine service. Patients who
received at least one dose of glipizide will be compared to those who did not receive glipizide.
Exclusion criteria include patients that experienced a hypoglycemic episode on the day of
admission. An equal number of charts of T2DM patients with and without glipizide treatment
will be examined. Data collection will include age, sex, race, comorbidities, concomitant
inpatient medication use, baseline labs, first occurrence of blood glucose less than 70 milligrams
per deciliter, most recent glycated hemoglobin level prior to admission, inpatient nutritional
status, and length of hospital stay. All patient information will be de-identified to maintain
patient confidentiality. Descriptive statistics will be used to analyze the data collected. Chisquared and Fishers Exact tests will be used to analyze the primary and secondary objectives.
Length of stay will be analyzed using either the Students T test or Mann-Whitney U test.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-267
Title: Medication use evaluation of intravenous acetaminophen use during April 2013 at Maine
Medical Center
Primary Author: Jacob Barker, University of New England, Maine;
Email: jbarker5@une.edu
Additional Author(s):
Stacy Miller
Don Watson
Purpose: The use of IV acetaminophen at Maine Medical Center has increased ever since its
addition to formulary in June 2011. With the increase in use there has also been an increase in
the cost of IV acetaminophen. This has led to an increase in spending of 300,000 dollars per
year. This Medication Use Evaluation (MUE) was aimed at classifying all doses of IV
acetaminophen given during the month of April 2013 into two categories: IV only and enteral
eligible. The overall endpoint was to determine the cost savings if all enteral eligible doses were
given as PO.
Methods: A report was run using electronic health record (EHR) to capture orders charted on the
medication administration record (MAR) as Given during the month of April. EHR autopopulated many fields of data, including: location, service, ordering provider, order date and
time, and dose and frequency. Data that was manually collecting included: enteral eligible doses,
number of doses given, indication, diagnosis, and presence of PO acetaminophen order. To
determine enteral eligibility, we looked at other enteral medications that were charted as Given
on the patients MAR. When we were unsure about a patients status, we assumed the IV route
was the most appropriate at the time. Thus, our results may underestimate the number of IV
doses that could have been given enterally. Data collected was organized by service line and the
number of doses which were IV only and enteral eligible. Costs for both IV and PO
acetaminophen were calculated using the cost to Maine Medical Center.
Results: The report gathered 585 orders for IV acetaminophen that had at least one dose reported
as Given on the MAR. From those 585 orders there were a total of 1944 doses. From the 1944
doses established, 969 (50%) doses were found to be enteral eligible. When the doses were
organized by service it was found that the majority of IV acetaminophen use was limited to the
appropriate locations, such as: anesthesia, CT surgery, internal medicine, and general surgery.
CT surgery used close to 500 doses within the month of April. Of those 500 doses, nearly 66%
were deemed enteral eligible. If 100% of the enteral eligible doses were given as oral then the
hospital would have saved approximately $12,000 per month. If only 50% or 25% doses were
given as oral than $6000 and $3000 dollars would have been saved respectively.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: 585 orders with 1944 associated doses of IV acetaminophen were established
during April 2013. From those 1944 doses, 969 were deemed enteral eligible and cost $12000
more than if they were given as PO doses. The data gathered from this MUE show definite
opportunities for cost savings. One of the limitations in this study was that the cost savings do
not take into account any extra opioid use as well as the costs of any anti-nausea/vomiting
medications from using the opioids if change had occurred earlier from IV to PO. It also doesnt
account for any decreased hospital stay duration.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-268
Title: Methicillin-resistant Staphylococcus aureus (MRSA) screening upon inpatient hospital
admission: is there concordance between nasal swab results and samples taken elsewhere from
the body
Primary Author: Kari Fischer, University of New England College of Pharmacy, Maine;
Email: kfischer2@une.edu
Additional Author(s):
Tze Shien Lo
Kimberly D.P. Hammer
Ashley Carver
Purpose: Methicillin-resistant Staphylococcus aureus (MRSA) infections are associated with
increased morbidity, mortality and increased healthcare costs. Patients infected with MRSA need
special hospital protocols which include isolation and contact precautions. The use of many
conventional antibiotics is null and newer medications with alternate mechanisms of action must
be used to fight MRSA infections. Resistance has become widespread throughout hospitals,
however not all carriers of MRSA show positive colonization results from nasal screening, the
gold standard for its indication. The objective is to determine if nares screening matches
secondary-site testing for colonization of MRSA for inpatients at a Veterans Affairs Medical
Center.
Methods: The medical charts of Veterans who had a nares screening plus testing for suspected
infection at an additional site upon hospital admission are included in this study. The VA Health
Care System implemented MRSA nasal screening in 2007. Data collection begins with a
compiled list of all inpatient admissions to the Fargo VA Medical Center from 2007 through
June 2013. Statistical analysis to determine if there is a concordant relationship will begin using
the McNemars test. To detect an absolute difference between nares screenings versus other sites
tested for colonization of MRSA an 80 percent or greater power will be used. The McNemars
test will analyze concordance of primary site, nares screening and secondary sites which include
sputum, urine, blood, wound and tissue. Demographic data for groups with positive concordance
are being collected from the Veterans and include age, sex, ethnicity, geographical residency,
immunocompromised disease state, smoker or chronic obstructive pulmonary disorder, length of
stay, previous hospital admission within 30 days, and prior history of MRSA infection. This
study was approved by the VA IRB of record and is currently active.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-269
Title: Dronedarone use in a large academic hospital: adapting to new guidelines in the aftermath
of the PALLAS trial
Primary Author: Lauren Gray, University of New England, Maine;
Email: lgray2@une.edu
Additional Author(s):
Dorothy Wang
Anne Andrle
Purpose: The PALLAS trial investigated the use of dronedarone in older patients with
permanent atrial fibrillation (AF). The trial was terminated prematurely due to an increase in
cardiovascular events in patients treated with dronedarone. This resulted in additional warnings
restricting its use. The objective of this study is to determine if dronedarone is prescribed
appropriately within a hospital setting, given the new warnings governing its use.
Methods: The study fulfilled criteria as a Quality Improvement Project (QIP) by the hospital
Institutional Review Board (IRB). The electronic medical record system will identify all orders
for dronedarone from January 2013-September 2013. The following information will be
collected for each patient that received dronedarone: date of admission, age, sex, comorbidities,
dronedarone indication, dose, frequency, number of doses received, reason for hospital
admission, admitting service, unit, ordering physician, presence of contraindications, EKG
monitoring, hepatic monitoring during admission, liver function tests within the past six months,
and whether or not patients were discharged on dronedarone. If there is an existing
contraindication, patient charts will be reviewed for presence or absence of documentation of the
rationale for choosing dronedarone. All patient information will be de-identified to preserve
patient confidentiality. Patients will be categorized as either appropriately or inappropriately
prescribed dronedarone according to the revised labeling. Patients categorized as inappropriately
receiving dronedarone will have their specific contraindication recorded. The results will be
communicated back to the hospital pharmacy and therapeutics committee for consideration.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-270
Title: Assessment of the Maine All-Payer Claims Database - Data Quality and Descriptive
Analysis of the Cancer Cohort
Primary Author: Erin Maggie Jones, University of New England, Maine;
Email: ejones4@une.edu
Additional Author(s):
Erin Maggie Jones
Edward Li
Purpose: Recently, comparative effectiveness research has emerged as a method to improve
quality of care decrease overall healthcare costs, specifically through the use of existing data and
large data warehouses. The Maine All-Payer Claims Database (MEAPCD) contains HIPAA
compliant, linked data regarding paid medical, dental, and pharmacy claims for 95% of
publicly/privately insured Maine residents. However, MEAPCD data quality and ability to
identify a cancer cohort is currently unknown. Such evaluations are necessary for future studies
to characterize practice trends and health outcomes to determine future healthcare optimization
strategies in Maine. The purpose of this study is to conduct a macro-level assessment of the
MEAPCD data quality within the MEAPCD. Further, a descriptive analysis of a cohort of
individuals with a cancer diagnosis will be provided.
Methods: For our data quality analysis, we will inspect the MEAPCD for evidence of potential
problems with incomplete tumor diagnosis data and incomplete medical and prescription claims.
This will be done by examining the following on a monthly basis (in all available years) for
apparent gaps in: 1) the number of medical claims; 2) the number of prescriptions claims; and 3)
the number of enrollees with a claim in that month. Data will be stratified by: place of service,
insurance product type (i.e., public vs. private), and claims associated with a tumor diagnosis.
The descriptive analysis of the cancer cohort will be characterized by: prevalence/incidence of
specific tumor types, patient demographic characteristics (e.g., age, gender, etc.), comorbidities,
and antineoplastic use. Descriptive statistics will be used for both these analyses. The UNE IRB
has reviewed this project and determined that it is exempt from IRB review and oversight as
defined by 45 CFR 46.101(b)(4).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-271
Title: The Maine Predicament of Prescription Drug Overdose
Primary Author: Elenna Kuhn, University of New England, Maine;
Email: ekuhn@une.edu
Additional Author(s):
Kenneth McCall
Christina Holt
Gary Cattabriga
Christian Teter
Purpose: Evaluate controlled substance prescribing trends and physician and pharmacy
utilization patterns among persons who died of prescription drug overdose compared to the
general population in Maine.
Methods: Retrospective data analysis of the Maine Prescription Monitoring Program (PMP)
from fiscal years 2005-2010 linked to medical examiner cases of all prescription drug deaths.
The PMP collects data for all Schedule II, III and IV prescriptions dispensed by pharmacies
licensed in Maine. Individuals who received one or more controlled substance prescriptions from
a licensed pharmacy during state fiscal years 2006 to 2010 (1 July 2005 to 30 June 2010; herein
referred to by year only) are included in the study population and compared to decedents of
prescription drug overdose.
Results: A total of 11,542,850 controlled prescriptions were dispensed for 1,024,649 unique
patients from 2006 to 2010, which included 31,736 prescriptions for 690 decedents of drug
overdose. Five or more prescribers were utilized by 4.3% of the entire population compared to
25.5% of decedents (P < 0.001). Five or more pharmacies were utilized by 0.9% of the entire
population compared to 11.5% of decedents (P<0.001). The majority of decedents (52%) were
prescribed a controlled substance within 15 days of overdose. Furthermore, the proportion of
individuals who were prescribed an opioid at a morphine milligram equivalent (MME) dose that
exceeded 100 mg in one or more days was 13.4% of the general population versus 31.4% of
decedents (P<0.001). Among decedents, the mean MME doses prescribed per day over the three
days immediately before overdose was 112.3 mg per day compared to 96.9 mg per day over the
prior 87 days. This suggests an increase in prescribed MME doses immediately prior to death.
The majority of drug overdose decedents had a prescription that matched the cause of death as
identified in the toxicology screen.
Conclusion: This analysis of a data linkage between PMP records and medical examiner cases
of prescription overdose death has revealed a significantly higher utilization of five or more
prescribers and/or pharmacies by decedents. The prescribed MME doses escalated in the final
three days prior to death and the majority of decedents had a prescription in the PMP that
matched the cause of death. The findings from this study support the need for efficient point-ofcare access to the PMP by both prescribers and dispensers to identify patients at risk of substance
misuse and overdose.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-272
Title: Enhancing pharmacy educational outcomes with a team-based, interprofessional case
competition modeled on the Clarion initiative
Primary Author: Justin Levesque, University of New England, Maine;
Email: justin.c.levesque@gmail.com
Additional Author(s):
Lisa Pagnucco
Shelley Cohen Konrad
Purpose: Healthcare costs in the United States increase every year, reaching upwards of $2.7
trillion dollars annually. What is the solution to stop the upward trend in healthcare spending? As
part of the overall clinical care team, pharmacists must work with other providers to find
solutions through increased patient safety and process improvement initiatives. Collaborative
patient care, with a culture of safety and improvement, will be important for future practitioners
when curtailing healthcare spending. This project created an interprofessional case competition
at a health professions university to foster team-based clinical care and process improvement
principles.
Methods: The competition was modeled on the Clarion Competition hosted by the University of
Minnesota. Students from health professions represented at the university, including: pharmacy,
medicine, nursing, occupational therapy, physical therapy, dental hygiene, physician assistant,
social work, and public health were invited to participate as an extracurricular activity.
Participants were randomized into teams of three or four. Each team had no more than two of the
same profession. The case analyzed was a health system re-admission scenario focusing on
chronic-obstructive pulmonary disease written by the University of Minnesota's Clarion
organizers. Students worked in their respective teams over seven weeks addressing the problems
posed by the case. Process improvement tool use was actively encouraged via the Institute for
Healthcare Improvement's Open School website. Each team had 20 minutes to present their
findings during three days of competition in March 2013. Teams were ranked with a rubric by a
panel of healthcare professionals. The winning team was awarded a $3,000 scholarship and paid
travel to the 2013 national Clarion Competition at the University of Minnesota.
Results: Fifty-six students participated. Medicine had 14 students; occupational therapy and
pharmacy each had 13 students. The remaining participants were a mix of nursing, physical
therapy, physician assistant, social work, and dental hygiene students. Fourteen teams were
formed in January 2013; three teams withdrew before final presentations. A winning team of
four students representing pharmacy, medicine, occupational therapy, and physical therapy was
selected. This team then placed second at the 2013 Clarion Competition out of nine teams
representing other universities.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: This project was an interprofessional case competition giving students experience
working within healthcare teams. Team-based care, with clinical pharmacists serving an integral
part, will be crucial when solving issues of rising healthcare cost, patient safety, and care quality.
The success of the project reflects a second place finish in the national Clarion Competition in
the first year the university fielded a team. Students informally polled remarked the competition
was worthwhile in giving a broader view of other healthcare professions. Additionally, exposure
to process improvement tools often neglected in the healthcare classroom was a plus to overall
student development.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-273
Title: An Evaluation of the Exposure of Recent Pharmacy School Graduates to Non-Traditional
Career Opportunities in the Pharmaceutical and Biotech Industry
Primary Author: Alexandra Malinowski, University of New England, ME;
Email: amalinowski@une.edu
Additional Author(s):
Patrick Sorgen
Steven M Richards
Andrew Walfield
Dana Martin
Purpose: Herein, we report on the responses of a random sampling of pharmacy school
graduates representative of varying career pathways including fellowships, residencies,
community and hospital practice. We seek to evaluate the exposure of this cohort to nontraditional career opportunities, specifically opportunities in pharmaceutical and biotech
industry, during the time of their education.
Methods: In August 2013, a nineteen-question electronic survey was emailed to 497 recent
pharmacy school graduates spanning geographical and professional careers across academic
institutions and hospitals, pharmaceutical and biotech industries, and community pharmacies.
Institutional Review Board (IRB) completed review of the study, and therein, the study met the
criteria for IRB exemption. A recent graduate was defined as an individual that graduated from
an accredited pharmacy program in the United States within the past 10 years (2003-2013). The
survey was administered through an online survey tool, Google Forms, and distributed to
potential participants via email. Additionally, the study sought to compile the experience and
exposures of the aforementioned cohort of pharmacists, including highest degree earned (in
addition to the BS Pharm or PharmD), exposure to fellowship training programs, number of
industry rotations or internships completed while working towards attainment of a pharmacy
degree, prior research experience, and membership in professional associations and honor
societies. Survey submissions were anonymous and responses were entered into a central
database, utilizing Microsoft Office Excel. A retrospective analysis was performed to identify
any commonalities in experience and exposures, prior to graduation, of those who decided to
pursue careers in the pharmaceutical and biotech industry.
Results: Sixty-eight of the four hundred ninety seven surveys distributed were completed,
yielding a response rate of 13.7%. Thirty of the total respondents (44%) report exposure, prior to
graduation, to opportunities in the pharmaceutical and biotech industries within their curriculum.
Of the total respondents, 38 (55.8%) report < 1 pharmaceutical or biotech industry lecture or
speaker during their pharmacy education. Fifty-one (75%) of respondents report no experiential
education in the pharmaceutical or biotech industry, yet 47 (70%) of respondents report having
the opportunity to take an industry rotation. Fourteen (20.5%) report to hold a current position in
the pharmaceutical or biotech industry. Of those, 13 of 14 (92.8%) industry pharmacists report to
have completed an industry rotation during their pharmacy education.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Pharmacy graduates report little to no exposure to the pharmaceutical and biotech
industry during their pharmacy education. The majority of respondents report exposure to ~ 1
industry lecturer. Interestingly, the majority indicated that they had the opportunity to complete
an industry rotation. There appears to exist an association between those who completed
experiential industry rotations and those who went on to pursue a non-traditional industry career.
Therefore, more emphasis on industry career opportunities may be necessary across pharmacy
schools. However, larger studies and further data analyses are warranted to validate pharmacy
students exposure to non-traditional career opportunities.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-274
Title: Antidepressant prescribing patterns in solid tumors
Primary Author: Kimberly Mulcahy, University of New England, College of Pharmacy, Maine;
Email: kmulcahy1@une.edu
Additional Author(s):
Devon Sherwood
Edward Li
Gary Cattabriga
Purpose: It has been estimated that between 13 to 40% of cancer patients are suffering from
clinical depression and reports suggest 40-90% of these patients are under-treated. Comorbidities
with depressive disorders have been shown to cause a decrease in chemotherapy adherence and
increase in mortality compared to patients without depression. The primary objective of this
study is to identify solid-tumor cancer patients and their relation to comorbid psychiatric
diagnosis with any corresponding trends in antidepressant prescribing.
Methods: This study was approved by the Institutional Review Board (IRB) at the University of
New England for exempt status. This is a descriptive cohort study of Maine subjects from
inpatient and outpatient services with a solid tumor diagnosis. Using the Maine All-Payer Claims
Database (MeAPCD), subjects were identified by an ICD-9 code for breast, colorectal, non-small
cell lung, prostate or pancreatic cancer from January 1, 2007 December 31, 2009. Demographic
information included age, sex, cancer diagnosis, any psychiatric diagnosis, type of insurance
claim, chemotherapy received, and antidepressant class and drug received. Patients were
excluded if enrolled for less than 90 days from their first claim, under 18 years of age, or
identified as a female with a prostate cancer diagnosis. Descriptive statistics will analyze
demographics, diagnostic trends and any prescribing patterns for both chemotherapy agents and
antidepressants. Results of this hypothesis-generating study may be used to both aid prescribers
in preventing negative outcomes from comorbid psychiatric effects on cancer morbidity and
mortality, and identify future areas of research.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-275
Title: Psychotropic prescribing trends among pediatric patients in an acute psychiatric hospital
Primary Author: Andrea Nakamura, University of New England, Maine;
Email: anakamura@une.edu
Additional Author(s):
Devon A. Sherwood
Gary Roy
Purpose: The National Comorbidity Survey of 2011 found that the lifetime prevalence for a
DSM-IV psychiatric disorder was up to 49.5%. Pediatric patients are commonly treated with offlabel and unlicensed medications that have been approved for adult use but lack pediatric
guidelines, and up to 78% of hospitalized children are treated with medications that without agespecific approval. The objective of this study is to identify psychotropic prescription patterns for
pediatric patients in an acute psychiatric hospital setting and to compare these findings to current
guidelines and evidence-based recommendations.
Methods: This study was approved by the Ethics Committee at Spring Harbor Hospital and is
under review by the Institutional Review Board at the University of New England for exempt
status. Data is available through a drug-utilization-review on all psychotropic medications
administered to pediatric patients between January 1 to June 30, 2013. The population includes
patients age of 4 to 18 years old admitted to a child and adolescent unit at Spring Harbor
Hospital between January 1 and June 30, 2013. Psychotropic medications recorded were noted at
the time of discharge. Patients were excluded if they were 19 years of age or older, or if their
length of stay was 24 hours or less. Data obtained included patients age, physician, hospital unit
(child 4-11 years vs. adolescent 12-18 years), length of stay, and psychotropic medications
prescribed as broken down by class and specific drug (dose, drug, route, and frequency). All data
is maintained confidentially and recorded without patient identifiers. Utilizing current evidencebased recommendations from pediatric psychiatry guidelines and studies, reviewers will track
prescribing trends to compare compliance with best practices.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-276
Title: In vitro activity of colistin, polymyxin B, and tigecycline, alone and in combination with
various antimicrobials, against NDM-1-producing Klebsiella pneumoniae
Primary Author: Alison Paplaskas, University of New England, Maine;
Email: apaplaskas@une.edu
Additional Author(s):
Alexandra Malinowski
George P. Allen
Purpose: Carbapenem-resistant Enterobacteriaceae, such as New Delhi metallo-beta-lactamase1 (NDM-1)-producing Klebsiella pneumoniae, are resistant to most antimicrobials, and
antimicrobial combinations are required against such bacteria. The mutant prevention
concentration (MPC) is a novel measure of resistance induction. The MPC is the MIC of the
most resistant mutant in a population; the mutant selection window (MSW) encompasses the
concentrations between the MIC and MPC. Concentrations within and below the MSW select
mutants. We evaluated resistance selection and bacterial killing by colistin (CST), polymyxin B
(PMB), and tigecycline (TGC), alone and in combination with aztreonam (ATM), doxycycline
(DOX), fosfomycin (FOF), gentamicin (GEN), meropenem (MEM), rifampin (RIF), and
vancomycin (VAN) against NDM-1-producing Klebsiella pneumoniae.
Methods: K. pneumoniae strain ATCC BAA-2146 was tested. MIC testing was performed with
an inoculum of 10^5 colony-forming units (CFU)/mL. MPCs were determined by plating 10^10
CFU of BAA-2146 on agar medium containing increasing supra-MIC antimicrobial
concentrations. Published pharmacokinetic parameters attained by therapeutic regimens of each
antimicrobial were used to analyze the relationship between antimicrobial concentrations and the
MSW. A time-kill assay was used to assess bacterial killing and resistance induction by free
(unbound) peak (Cmax) concentrations of each antimicrobial, alone and in combination, over 24
hours; combination regimens consisted of high or low concentrations of CST, PMB, or TGC, in
combination with ATM, DOX, FOF, GEN, MEM, RIF, or VAN. Tested Cmax were: CST 0.29
mg/L or 1.46 mg/L, PMB 0.33 mg/L or 1.65 mg/L, and TGC 0.64 mg/L or 3.2 mg/L, each in
combination with ATM 34 mg/L, DOX 1.3 mg/L, FOF 26.1 mg/L or 81.8 mg/L, GEN 20 mg/L,
MEM 38.4 mg/L, RIF 3.48 mg/L, and VAN 63 mg/L.
Results: MIC/MPC values were: CST 1/>32, PMB 0.5/>16, FOF 16/>64, TGC 16/>64, ATM
>256/>512, DOX 128/>512, GEN >64/>256, MEM >32/>128, RIF >32/>128, VAN >256/>512.
All agents fail to exceed the MIC and thus do not enter the MSW, except CST 1.46 (time in the
MSW (TMSW) 40.3% of the dosage interval), PMB 1.65 (TMSW 100%), and FOF 26.1
(TMSW 8.4%). FOF 81.8 achieves concentrations above the MPC for 25.2% of the dosage
interval (TMSW 74.8%). In time-kill assays, CST 0.29, PMB 0.33, TGC 0.64, TGC 3.2, ATM,
DOX, FOF 26.1, FOF 81.8, GEN, MEM, RIF, and VAN failed to achieve sustained killing of
NDM-1. CST 1.46 and PMB 1.65 were bactericidal (> 3 log10 CFU/mL kill). Combinations of
CST 0.29 + FOF 81.8, and PMB 0.33 + FOF 26.1, FOF 81.8, GEN, or MEM achieved synergy
(> 2 log10 CFU/mL additional kill by the combination). Combinations containing TGC failed to
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
kill NDM-1. CST 1.46 and PMB 1.65 prevented mutant growth, while TGC 3.2 did not. No
antimicrobial combinations showed antagonism (decreased killing by the combination).
Conclusion: CST, PMB, and FOF, alone and in combination, display variable concentrationdependent killing of NDM-1-producing Klebsiella pneumoniae. TGC fails to kill NDM-1producing Klebsiella pneumoniae and is predicted to select mutants. Antimicrobial combinations
that include CST, PMB, and/or FOF warrant further study against NDM-1-producing K.
pneumoniae.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-277
Title: Evaluation of in vitro antimicrobial resistance selection in Salmonella enterica serovar
Typhi
Primary Author: Donna Park, University of New England, Maine;
Email: dpark@une.edu
Additional Author(s):
Jessica Dizon
Lindsey McIver
George Allen
Purpose: The increasing prevalence of infections caused by Salmonella enterica serovar Typhi
(Salmonella Typhi) has resulted in resistance to many antimicrobial therapies. The worldwide
dissemination of mutant antimicrobial-resistant strains of Salmonella Typhi has led to
replacement of former first-line antimicrobials, such as chloramphenicol, by antimicrobials such
as azithromycin and ceftriaxone. However, the comparative antibacterial activities of
antimicrobials used to treat Salmonella Typhi is unknown. Moreover, the abilities of these
antimicrobials to prevent further resistance development is unclear. We analyzed the
antibacterial activity of azithromycin, ceftriaxone, and chloramphenicol using a time-kill assay.
We also used determination of the mutant prevention concentration (MPC), a novel susceptibility
parameter, to establish the likelihood of induced resistance in Salmonella Typhi.
Methods: Salmonella Typhi strain ATCC 6539 was tested. Minimum inhibitory concentration
(MIC) testing was performed with an inoculum of 10^5 colony-forming units (CFU)/mL. The
MPC was determined by plating a bacterial inoculum of 10^10 CFU on agar medium that
contained each antimicrobial in increasing two-fold dilutions starting from the MIC. The
inoculated plates were incubated for 72 hours and then observed for growth of mutants; the
lowest dilution that contained no growth was determined to be the MPC. The range of
antimicrobial concentrations between the MIC and MPC was deemed to be the mutant selection
window (MSW), the range of concentrations where selective amplification of mutants occurs.
Published pharmacokinetic parameters attained by usual therapeutic regimens of each
antimicrobial were used to analyze the relationship between antimicrobial concentrations and the
MSW. A time-kill assay was used to test the antibacterial activity of the free (unbound)
intracellular Cmax of each antimicrobial against a bacterial inoculum of 10^6 CFU. Bactericidal
and bacteriostatic activity was analyzed by plotting bacterial colony counts (log10 CFU/mL)
versus time.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Results: MIC/MPC (mg/L) values of azithromycin, ceftriaxone, and chloramphenicol were
16/64, 0.125/4, and 2/32, respectively. Concentrations of chloramphenicol fall within the MSW
for 100% of the 6-hour dosing interval, suggesting that resistance to chloramphenicol will result.
Concentrations of azithromycin fall above the MPC and MSW for 100% of the 24-hour dosing
interval, suggesting that azithromycin will not select resistant mutants. Ceftriaxone
concentrations fall above the MSW for 27.1% of the 24-hour dosing interval, but within the
MSW for the remaining 72.9% of the dosing interval, suggesting that selection of mutants will
occur. In time-kill assays, ceftriaxone was bactericidal (3 log10 CFU/mL reduction from the
initial inoculum), while azithromycin and chloramphenicol achieved bacteriostatic activity only
(<3 log10 CFU/mL reduction from the initial inoculum).
Conclusion: At standard doses, resistance to azithromycin may not develop because
concentrations of azithromycin exceed the MSW for 100% of the dosing interval. Resistance to
ceftriaxone and chloramphenicol in Salmonella Typhi will likely develop due to the long interval
that serum antimicrobial concentrations fall within the MSW. However, ceftriaxone achieves
superior bactericidal activity, while azithromycin and chloramphenicol achieve bacteriostatic
activity. Further analysis of these antimicrobials as treatment options for infections caused by
Salmonella Typhi is warranted.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-278
Title: Evaluation of the in vitro activity of ciprofloxacin, levofloxacin, and moxifloxacin against
Neisseria gonorrhoeae
Primary Author: Emily Prescott, University of New England College of Pharmacy, Maine;
Email: eprescott@une.edu
Additional Author(s):
George Allen
Purpose: Antimicrobial resistance in Neisseria gonorrhoeae continues to be an emergent
problem, and few antibiotics are effective against infections caused by Neisseria gonorrhoeae.
Fluoroquinolones are no longer recommended by the Centers for Disease Control for treatment
of gonococcal infections due to resistance concerns, but in vitro data suggests that newer
fluoroquinolones such as moxifloxacin have activity against resistant Neisseria gonorrhoeae. To
minimize selection of resistant microorganisms, a novel susceptibility parameter, the mutant
prevention concentration (MPC) may be used. The MPC is the minimum inhibitory
concentration (MIC) of the most resistant first-step mutant in a large bacterial inoculum.
Resistance is promoted when antimicrobial concentrations fall between the MIC and MPC; this
range of concentrations is called the mutant selection window (MSW). We determined MPC and
MSW values of ciprofloxacin, levofloxacin, and moxifloxacin against a mutant strain of
Neisseria gonorrhoeae, and used a time-kill assay to compare the antibacterial activity of these
agents.
Methods: A fluoroquinolone-resistant gyrA mutant strain of Neisseria gonorrhoeae, m-49226,
was studied. MICs were determined using a bacterial inoculum of 10^5 colony-forming units
(CFU). MPCs were determined by culturing 10^10 CFU of m-49226 on supplemented
gonoccocal agar with known supra-MIC concentrations of each antimicrobial, and then
measuring the lowest concentration to inhibit mutant bacterial growth. Extracellular
pharmacokinetic parameters obtained by therapeutic oral doses of ciprofloxacin 500 mg x1
(Cmax 1.68 mg/L, t1/2 4 hours), ciprofloxacin 500 mg every 12 hours (Cmax 2.08 mg/L, t1/2 4
hours), levofloxacin 250 mg x1 (Cmax 1.93 mg/L, t1/2 7 hours), levofloxacin 250 mg every 24
hours (Cmax 2.21 mg/L, t1/2 7 hours), moxifloxacin 400 mg x1 (Cmax 1.86 mg/L, t1/2 12
hours), and moxifloxacin 400 mg every 24 hours (Cmax 2.70 mg/L, t1/2 12 hours) were used to
determine the relationship between antimicrobial concentrations and the MIC, MPC, and MSW.
The antibacterial activities of each antimicrobial were tested for 24 hours using a time-kill assay,
with bacterial quantification performed at 0, 4, 8, and 24 hours
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Results: The MIC/MPC (mg/L) of ciprofloxacin, levofloxacin, and moxifloxacin were
0.0625/0.25, 0.0625/0.25, and 0.125/0.5, respectively. Concentrations of all of the antimicrobials
studied are predicted to fall above the MSW. Concentrations of ciprofloxacin and moxifloxacin
fall above the MPC for the entire dosage interval. Concentrations of levofloxacin fall above the
MPC for 91.7% of the dosage interval and fall within the MSW for 8.3% of the dosage interval.
In time-kill assays, all of the tested fluoroquinolone regimens achieved bactericidal activity (> 3
log-10 CFU/mL colony-count reduction) by 24 hours, with moxifloxacin achieving the greatest
activity at the 4-hour and 8-hour time points.
Conclusion: Against mutant Neisseria gonorrhoeae, all of the tested fluoroquinolones are
predicted to prevent mutant selection and showed bactericidal activity. However, moxifloxacin
exhibited an increased bactericidal activity compared to the other agents tested. As antimicrobial
resistance in Neisseria gonorrhoeae continues to be an emergent problem, new antimicrobial
therapies are needed. Although fluoroquinolones are no longer routinely recommended for the
treatment of gonococcal infections, few alternative antimicrobials with activity against Neisseria
gonorrhoeae are available. Further studies of fluoroquinolones, particularly newer agents such as
moxifloxacin, are warranted.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-279
Title: Concomitant initiation of vancomycin and metformin is the likely cause of acute kidney
injury (AKI) in a woman diagnosed with cellulitis
Primary Author: Mallory Sherwood, University of New England College of Pharmacy, Maine;
Email: msherwood@une.edu
Additional Author(s):
Matthew Lacroix
Case Report: This case report demonstrates the potential risk of acute kidney injury (AKI)
associated with the concomitant initiation of the medications vancomycin and metformin. Patient
A, a 47 year old female, presented to the emergency room with increasing right leg swelling,
pain, and redness. This began 1.5 days prior and was accompanied by symptoms of reduced
appetite and fatigue. Patient A reported no known trauma to the skin in that area. She was
diagnosed with cellulitis and admitted for IV antibiotic therapy. Upon hospital admission, patient
A weighed 224.7 kg and was classified by her BMI as morbidly obese. Bloodwork showed a
baseline serum creatinine of 0.8, elevated white blood cell count at 14.4, and a slightly elevated
hemoglobin A1c at 6.2, and negative blood cultures. On day 1 of admission, patient A began a
regimen of vancomycin 2 grams IV loading dose followed by vancomycin 1.5 grams IV every 8
hours with trough levels to be monitored by the pharmacy, and piperacillin/tazobactam 3.375
grams IV every 8 hours. On day 2, patient A was started on metformin 850 mg twice a day for
diabetes mellitus type 2 due to the combination of morbid obesity and a slightly elevated
hemoglobin A1c, despite the fact that the hemoglobin A1c was not high enough to classify her as
diabetic. On day 5, patient A had a slightly elevated serum creatinine of 1.0 and by day 6 her
serum creatinine had more than doubled from baseline to 1.8. The vancomycin trough on day 6
was 25.6. Metformin was discontinued, and vancomycin was still used with dosing based on
random vancomycin levels. On day 12, patient As serum creatinine reached 3.6 before it began
to trend down. The patient was discharged on day 16 with a serum creatinine of 3.2. Throughout
her stay in the hospital, the only major changes in laboratory values were in the serum creatinine.
Her blood pressure and heart rate also remained normal. Patient A was treated with a few
different antibiotics throughout her stay, but the vancomycin was used the entire time. She was
eventually discharged on IV vancomycin. There were no obvious reasons as to why patient A
would have experienced AKI other than the initiation of multiple drugs that are renally
eliminated and nephrotoxic. There is limited evidence to confirm that the concomitant initiation
of vancomycin and metformin does cause AKI. However, in this specific case it is the only
reasonable explanation for patient As acute kidney injury.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-280
Title: Assessing the Attitudes and Beliefs of Pharmacists Regarding Prescription Opioids Using
a Modified Version of the Clinician Attitudes about Opioids Scale (CAOS)
Primary Author: Robin Spielmann, University of New England, Maine;
Email: rspielmann@une.edu
Additional Author(s):
Elenna Kuhn
Edward Tchernaia
Chunhao Tu
Christian Teter
Purpose: There is strong evidence that patients receiving high daily doses of opioids for chronic
pain are at a greater risk of overdose and death, particularly as the dose exceeds 100 morphine
equivalent doses (Bohnert et al, 2011; Dunn et al, 2010). Using the results from this study, we
aim to target the specific concerns (e.g. lack of education regarding long-term opioid efficacy
and patient-pressures for pain medication) of pharmacists about opioid prescribing and
dispensing. Ultimately, we will use this information to design tailored interventions for health
care providers to help lessen the overuse, and possibly even misuse and nonmedical use, of
prescription opioids.
Methods: Given these alarming and intertwining issues, we are going to assess the attitudes and
beliefs of pharmacists regarding prescription opioids using a psychometrically sound instrument:
the Clinician Attitudes about Opioids Scale (CAOS; Wilson et al, 2013). Each of the 40 items on
the scale is rated from 0 (strongly disagree) to 10 (strongly agree), covering various specific
aspects of prescription opioid use. Descriptive data will be derived for each item and used to
identify themes in the attitudes and beliefs regarding opioids among our large convenience
sample of pharmacists practicing in the state of Maine. For example, literature suggests there is
no strong evidence supporting the efficacy of opioids for long-term pain management (Von
Korff et al, 2011). Hence, we aim to analyze items from the CAOS that target this issue and
assess whether pharmacist attitudes and beliefs are consistent with the literature.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-281
Title: Pharmacy assisted communication of FDA MedWatch Alerts across a health system
Primary Author: Hubert Tse, Husson University School of Pharmacy, Maine;
Email: tseh@my.husson.edu
Additional Author(s):
Joshua Pruitt
Matthew Marston
Frank Bragg
Purpose: The FDA regularly releases medication alerts that can be directly related to patient
therapy. Keeping patients informed is very important for achieving clinical goals and desired
outcomes. Streamlining and defining important notifications can help healthcare providers
disseminate this information to their patients. Computerized systems provide a great opportunity
to facilitate this process and at Eastern Maine Medical Center (EMMC) we sought to expand on
this. The importance of this project is to utilize pharmacists as a resource with FDA alerts, in
order to protect providers from alert fatigue while providing concise and pertinent information to
assist in treating their patients.
Methods: A computerized system was implemented with notifications to alert physicians. This
alert system was developed with the support of Cardinal Health through funding provided by a
grant. The pharmacy resident on staff reviews the FDA medication alerts that contain new drug
information such as contraindications and drug interactions. The resident then consolidates this
information into a drug monograph that organizes these FDA alerts into one of four categories.
These categories rank from Green, Yellow, Red, and Black, with Black having a very high
likelihood of causing direct harm to the patient and prompting immediate action. At our
institution, physicians are notified via an electronic medical record (Centricity EMR, GE
Healthcare) by a designated physician, who then determines patient risk based on this
information. A computerized notification is entered and the primary care physician is notified
about the patient via an electronic notification linked to the patients medical record. Recent
modifications have incorporated collection of patient outcomes and physician compliance data,
and will allow for a full evaluation of the process.
Results: A recent audit of the EMR system identified 154 of 31,800 patients (about 1 in 200)
who were at risk for adverse events given their current medication status in relation to an FDA
alert. By streamlining FDA alerts and notifying providers when their patients are at risk, we can
potentially decrease the number of adverse drug events in our patient population. Anecdotal
feedback indicates that the process has been effective in delivering targeted notifications to
providers based on the medications their patients are taking. Providers have expressed
appreciation for the system as a useful approach to sifting through FDA notifications, and
ensuring that they see the information that is most relevant to them. Future modifications to
Centricity will require provider documentation, including their action and how they contacted the
patient. This will allow us in the future to further evaluate the benefits of pharmacist FDA alert
review and a computerized physician notification system in order to improve clinical outcomes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Categorizing and consolidating pertinent medication alerts allows our pharmacy to
improve the quality of patient directed health information, safety, and outcomes while ensuring
providers are not overwhelmed with medication alerts. This new system not only helps to keep
providers informed but also may improve patients attitudes and responses to medication
information as it relates to their own personal conditions. The computerized alert system will be
expanded to notify more primary care providers employed by EMMC and these alerts will
eventually reach all providers within the Eastern Maine Healthcare System.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-282
Title: The use of virtual laboratories and other web-based tools in a drug assay course.
Primary Author: Haya Abu-Seir, University of Michigan - Pharm.D. student, University of
Michigan - Ann Arbor, Michigan;
Email: h.abuseir@gmail.com
Additional Author(s):
Mustapha Beleh
Purpose: As part of a longitudinal study, web-based modules are assessed as alternative
instructional tools in a medicinal chemistry course. Virtual laboratories and accompanying webbased tools are used in place of the traditional method of didactic instruction in the laboratory
portion of the course. Students are required to use these tools prior to running the experiments. In
the didactic portion, students are required to watch instructional videos to prepare for each class.
In-class lectures focus on application of information and addresses gaps in knowledge as
identified by pre-class assessments.
Methods: Virtual laboratories are web-based modules that include an interactive step-by-step
simulation of the experimental protocol, with intermittent assessments. This is preceded by an
introductory video that provides background information and explains the significance of the
experiment. Students are required to use both sections and then take an ungraded quiz. The
scores of these quizzes and of the final practical exam are compared to previous classes,
including those who used different instructional methods. Technique videos are optional
resources that demonstrate how to use various analytical instruments. Their benefit is assessed by
administering mini-quizzes prior to each experiment and comparing scores of students who
viewed these videos to those who chose not to use them. For the didactic component of the
course, students completed required pre-lecture instructional videos prior to each lecture that
covered the basic concepts related to the topic. An ungraded online quiz followed each video,
and quiz and final exam scores were compared between different classes.
Results: For the laboratory portion, students who scored above average on the practical final
exam had significantly better average scores on virtual lab quizzes than students who scored
below average (p=0.00165). Better performance on virtual lab quizzes was correlated with
improved test scores (b=0.1661, R^2=0.1295). Additionally, most students rated this tool as
having some or great educational value (87%). Technique videos were used by a small sample
for each video and did not significantly influence mini-quiz scores. However, most students felt
they had some or great educational value (75%). For the didactic component, students who
scored above average on the midterm and final had significantly better average scores on prelecture quizzes than students who scored below average (midterm: p=0.00186, final:
p=0.0000003). Higher average quiz scores were associated with improved grades on both exams
(b=0.3682, R^2=0.175. b=0.2522, R^2=0.326). Most students thought the videos had some or
great educational value (69%). In general, most students expectations for the course were
partially or fully met (84%). Most students felt they gained a good understanding of concepts and
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
familiarity with lab techniques introduced in the course and that the workload was appropriate
but struggled with recognizing relevance of the course to their profession as pharmacists.
Conclusion: With a growing need for non-traditional teaching methods, this novel teaching
model based on web-based modules could provide an alternative method of teaching in
laboratory-based courses. For both the laboratory and didactic components, these web-based
tools, including virtual labs and pre-lecture videos showed promising results as learning tools
and are valued by students.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-283
Title: Analysis of medications from mail order versus local/retail pharmacies returned to a drug
take back event
Primary Author: Elliot Anderson, Ferris State University, Michigan;
Email: andere12@ferris.edu
Purpose: Pharmaceutical waste is believed to be a growing problem. There has also been some
question as to how much of this waste is produced by mail-order pharmacies. The objective of
this study is to compare amounts, types, and trends of pharmaceutical waste produced by mailorder pharmacies versus a local or retail pharmacy.
Methods: This study will be submitted to the Institutional Review Board for approval. Data was
collected from a drug take-back event and all patient identifiers were removed. The data
collected consisted of drug name, strength, and amount. It was also noted whether the
medications were originally dispensed from a mail order or local/retail pharmacy. Participants
were also asked if they would like to complete a brief online survey in order to determine their
demographics. Components included in the survey were age group, gender, reason(s) for
returning medications, where medications are filled, and what type of practitioner prescribes
them. The data was then condensed down into drug classification groups. The types, amounts,
and trends of medications returned from mail order and local/retail pharmacies will then be
compared.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-284
Title: Effect of clinical and attitudinal characteristics on obtaining comprehensive medication
reviews
Primary Author: Nadia Aneese, University of Michigan College of Pharmacy, Michigan;
Email: naneese09@gmail.com
Additional Author(s):
William Doucette
Karen Farris
Purpose: Data elucidating the driving forces behind why patients seek a comprehensive
medication review (CMR) are sparse. By improving this understanding, pharmacists may be able
to target these characteristics in potential patients, thereby increasing the viability of CMRs. The
objective of this study was to quantify the association between attitudinal and clinical factors
with obtaining a CMR among eligible patients with Medicare D.
Methods: A case control design was used for this secondary analysis, and the data were obtained
from an ongoing AHRQ-funded quality improvement project to promote medication therapy
management (MTM) to eligible individuals. Cases were defined as those who obtained a CMR
and the controls were those who did not obtain a CMR. Controls by definition did not obtain a
CMR and were all patients included in the sample that obtained their prescriptions from the same
pharmacy as those who obtained a CMR. Exposure was categorized through a set of survey
questions, obtained by telephone, which assessed attitudinal characteristics, clinical
characteristics, and intention to obtain a CMR. The MUSE (Medication Use Self Evaluation)
survey specifically determined medication use history, general healthcare, medication adherence,
understanding of CMR benefits and finally their likelihood in obtaining a CMR. Upon
completion of all questions, a risk score was computed to evaluate the estimated benefit of a
pharmacist-led medication review and was relayed to the patient. Six of fifteen questions were
used as variables in this study. Data were analyzed using chi-square and logistic regression to
quantify the association between each variable and whether or not patients obtained a CMR.
Results: Among 148 participants, cases represented 28.4% of the study participants who
received a CMR. The demographics across all participants showed an average age of 76.6 + 6.97
years, an average of 5.82 + 5.32 medications and 73% were female. In terms of predictors of
having a CMR, 43.9% of participants had >6 medications, 19.6% experienced side effects,
14.2% worried if medications did more harm than good, 51.4% felt medications were a financial
burden, 16.9% reported poor health status and 35.1% were likely to have a CMR in the next 30
days. In the logistic regression, poor health status was associated with having a CMR, (adjusted
odds ratio of 3.65, 95% CI 1.33, 10.05). No other variables including number of medications or
intention to have a CMR were statistically significant. Three variables trended in the correct
direction with adjusted odds ratios of 1.88 (0.71, 5.02) for experienced side effects, 1.11 (0.36,
3.38) for worry if medications do more harm than good and 1.75 (0.77, 3.97) for likely to have a
CMR in the next 30 days although the sample size was not large enough to show significance.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Participants who reported poorer health status compared to those who reported
good health status were more likely to have a CMR with a community pharmacist. Health status
can be used to promote CMRs as well as bring awareness of its possible benefits to individuals
who rate their health poorly. We can also encourage the use of CMRs for patients who
previously did not realize the potential benefit by assessing their perceptions about their health.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-285
Title: Assessment of propofol for procedural sedation in the emergency department: medication
use evaluation
Primary Author: Jennifer Baric, Wayne State University and Henry Ford Hospital, Michigan;
Email: jbaric1@hfhs.org
Additional Author(s):
Nancy C. MacDonald
Martin Lulek
Nadia Haque
Purpose: Propofol's ultrashort half-life makes it an ideal medication for procedural sedation in
the emergency department (ED). However, serious adverse events, such as hypotension and
respiratory depression can occur, especially when it is used concurrently with opiate
medications. Propofol was recently included in the hospital ED procedural sedation guidelines.
The purpose of this evaluation is to assess compliance to the ED specific guidelines when
propofol is used for procedural sedation in the ED. The data will be used to identify
opportunities for improving compliance with the hospital ED guidelines.
Methods: This study was approved by the hospital's Institutional Review Board. Fifty
consecutive patients, aged 18 and older, who received propofol for procedural sedation in the ED
were included in this retrospective medication use evaluation. Each chart was reviewed by one
investigator to collect the following: patient demographics, American Society of
Anesthesiologists classification, comorbidities, specific procedure performed, length of the
procedure, required elements for patient safety monitoring, medications administered prior to
and during the procedure, adverse events, and the treatment and/or interventions of adverse
events. Descriptive analysis will be used to analyze data collected. Data will be used to
determine compliance with the ED guideline and determine adverse events during the procedural
sedation. It will then be used to improve the safe use of propofol for procedural sedation in the
ED.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-286
Title: Using Lean Thinking to Reduce Waste in Continuous Renal Replacement Therapy in a
Large Academic Medical Center
Primary Author: C. Brett Benfield, University of Michigan College of Pharmacy, Michigan;
Email: cbbenf@umich.edu
Additional Author(s):
Phil Brummond
Purpose: The large academic medical center in which this was studied provides Continuous
Renal Replacement Therapy (CRRT) on a number of patients annually. It has been identified that
the process used by this large academic medical center to procure, prepare, and administer CRRT
has significant opportunities for improvement related to the standardization of processes and
reduction of waste. The use of Lean Thinking will help to identify the waste created in the
current processes while fostering an environment of continuous improvement for the future.
Lean Thinking will additionally promote strategies for waste reduction while maintaining high
standards of patient care.
Methods: Through the utilization of Lean Thinking, an interdisciplinary team, led by the project
investigator, has developed a Value Stream Map to identify the areas of waste associated with
the current CRRT medication use process. With the areas of waste identified, an A3 was created
to aide in devising strategies for improving the process. These strategies were prioritized based
on feasibility, sustainability, and impact on the waste in the process. Preliminary data has been
collected surrounding the doses dispensed, doses wasted, and estimated time associated with
ordering, distribution, and administration of therapy. Surveys have been developed to assess staff
satisfaction for distribution pre- and post-intervention to ensure that the new future state process
has not resulted in unforeseen consequences or waste associated with the implementation of
interventions. Prior to commencement of the study, it was submitted to the Institutional Review
Board and approved.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-287
Title: Characterization of antimicrobial exposure in patients with a history of Clostridium
difficile infection
Primary Author: Shawn Bockelman, Wayne State University, Michigan;
Email: ec8387@wayne.edu
Additional Author(s):
Hana Alawy
Corey Tschannen
Celeste Hirsch
Jamie L Wagner
Purpose: Clostridium difficile infection (CDI) is a growing concern associated with significant
morbidity and mortality. Exposure to broad spectrum antimicrobials is commonly associated
with CDI. The purpose of this medication use evaluation was to identify opportunities for
improving antibiotic use among patients who have a history of CDI.
Methods: This was an IRB-approved retrospective cohort study of patients (July 2012-June
2013) who experienced a CDI episode and readmission within 30 days. Data collected: patient
characteristics, reason for readmission, comorbid conditions, antimicrobial therapy during
readmission and discharge disposition. Antimicrobial therapy was characterized as completely
appropriate if: initially according to guidelines and streamlined within 72 hours when possible;
partially appropriate if: initially according to guideline and delayed/no streamlining OR initially
not according to guideline but streamlined within 72 hours; and inappropriate if: initially not
according to guideline with delayed/no streamlining. A poor disposition was defined as death
during hospitalization, discharge to hospice, or discharge to a skilled nursing facility if admitted
from home. Patient characteristics were compared using standard bivariate tests with a p<0.05
considered significant.
Results: 283 patients were screened for inclusion; 59 (21%) were readmitted within 30 days. Of
the 54 meeting inclusion criteria, 18 (33%) were readmitted for non-CDI infection, 8 (15%) for
CDI and 28 (52%) for non-infection. 49 (91%) patients were treated with antibiotics during
readmission; 14 (26%) only for CDI, 15 (28%) only for non-CDI and 20 (37%) for both.
Indication for therapy was documented in 25/35 (71%) pts receiving any non-CDI antimicrobial.
The most common sites of suspected infection were respiratory, urinary and sepsis not otherwise
specified. Appropriate cultures were obtained in 24/35 (68%). The most common non-CDI
antibiotics were: cefepime (43%), vancomycin (41%), other beta lactams (28%), and linezolid
(13%). The median days of therapy (DOT) of total non-CDI antimicrobials was 7 days (IQR 3,
17). Non-CDI antimicrobials could have been streamlined based on cultures in 30 patients and
was completed within 72hrs in 19/30 (63%). Antimicrobial therapy was completely appropriate
in 19/35 (54%), partially in 10 (29%) and inappropriate in 6 (17%). Treatment with linezolid was
statistically associated with receipt of inappropriate therapy (p=0.032). Poor disposition was
identified in 12/54 (22%) and was more common when readmitted for non-infectious causes.
Receipt of antimicrobials wasnt associated with discharge disposition.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: In this cohort of patients readmitted following an episode of CDI, readmission was
most commonly for non-infectious causes. However, nearly all patients received antimicrobial
therapy during readmission. Improvements in obtaining diagnostic cultures, adhering to
guidelines and de-escalating when appropriate could reduce exposure to unnecessary
antimicrobials in this high risk population.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-288
Title: Descriptive analysis of methadone use in pediatrics
Primary Author: Julia Brown, University of Michigan College of Pharmacy, MI;
Email: jlcrpntr@umich.edu
Additional Author(s):
Erika Howle
Purpose: There is a paucity of available evidence-based literature to guide decisions regarding
methadone utilization in pediatric patients, and in particular a lack of defined dosing regimens
for indications other than abstinence avoidance. This presents challenges for pediatric
practitioners faced with managing chronic pain, oncology pain, and palliative care. The purpose
of this study is to describe the changing trends and patterns in methadone utilization and
prescribing practices over a ten-plus year period at a tertiary care childrens hospital.
Methods: This study will be conducted as a descriptive analysis of inpatient methadone use in a
retrospective longitudinal cohort. The electronic medical records will be searched to identify
pediatric inpatients that were prescribed methadone between January 2001 and June 2012. The
following will be included in the data extraction: patient demographics, methadone dosing
regimen (first, last, and peak prescribed dose), ordering service, and whether the patient was
discharged on methadone. Average daily methadone doses will be calculated, and data will be
analyzed to determine if doses increased or decreased over time. This information will be used to
detail longitudinal prescribing changes in the use of methadone from more traditional indications
such as for abstinence avoidance, which primarily occurs in the hospital, to more frequent
prescribing for treatment of oncology and palliative care pain, which can occur both in the
hospital and at home. This project has received Institutional Review Board approval and patient
privacy will be maintained by entering data in de-identified spreadsheets.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-289
Title: Mentoring the next generation of health-system pharmacy leaders
Primary Author: Lauren Brown, University of Michigan College of Pharmacy, Michigan;
Email: lmbrownn@umich.edu
Additional Author(s):
James G Stevenson
Purpose: The ASHP Statement on Leadership as a Professional Obligation attests that all
pharmacists share the responsibility to mentor pharmacy students, residents, other pharmacists,
and technicians1. A 2011 ASHP survey revealed that 43% of pharmacy students do not currently
have a mentor2. A striking 61% of these students indicated lacking mentorship because they did
not know how to find a mentor2. This percentage has increased since the survey was
administered in 2004, suggesting that more students are struggling to build relationships with
practicing pharmacists3. The purpose of this project is to develop an effective strategy to assist
students in finding mentors.
Methods: In order to promote the personal and professional development of pharmacy students,
a networking night will be implemented that incorporates elements of both speed and flash
mentoring4. The program structure will consist of a social hour with appetizers followed by a
series of three consecutive one-on-one mentoring sessions between health-system pharmacists
and students interested in pursuing a career in health-system pharmacy. Each mentoring session
will last twenty minutes. Health-system pharmacists and pharmacy students will both be
recruited to participate in the event through email. Prior to the event, students will be matched as
closely as possible with their three prospective mentors based on pharmacy practice interest. An
online survey will be administered to participating pharmacists and pharmacy students at one
month post-intervention. The questionnaire will address participant satisfaction with the
mentoring event and attempt to quantify the amount of continued communication between
mentor-mentee pairs afterwards. The results from the survey will be used to determine the
effectiveness of this mentoring strategy in helping students build rapport and establish mentoring
relationships with health-system pharmacists.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-290
Title: Analysis of controlled substances and other prescriptions of returned medications from a
drug take back event
Primary Author: Emily Burley, Ferris State University, Michigan;
Email: burleye@ferris.edu
Purpose: As the pharmaceutical industry has expanded, it has led to an enormous amount of
medicinal waste and disposal. Because of this increase in pharmaceutical waste, more and more
drug take-back programs are being developed. The objective of this study is to analyze the
significance and variation of the quantity, type, treatment condition, and schedule classification
of the collected medications at a drug take back event.
Methods: This study will be submitted to the Institutional Review Board for approval. The
information was collected from prescription labels on medication bottles voluntarily returned to
the drug take back event. All data was recorded without patient identifiers. The following was
collected at the event: drug name (generic or brand), strength, unit of strength (mg, mL, mcg,
mEq, etc.), estimated amount, and amount originally prescribed, and if it was filled by a local
pharmacy, mail order, or sample medication. All those who returned medications were asked to
complete an online survey including the following information: age, gender, if an employee of
the state, city or local government, reasons for returning the medication, where they usually fill
prescription medications, how they normally dispose medications, type of prescription insurance,
and percentage of medications filled by the following types of providers: primary care physician,
specialist, nurse practitioner/physicians assistant, or other health care professionals. Data will
then be condensed into therapeutic drug classes and controlled substance schedules for better
analysis.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-291
Title: Effects of the peer mentorship program on first year pharmacy students
Primary Author: Ashley Caron, Ferris State University College of Pharmacy, Michigan;
Email: carona1@ferris.edu
Additional Author(s):
Gregory Wellman
Margaret Lyons
Purpose: Students reported that upon entering pharmacy school there is an increased level of
perceived stress compared to undergraduate work, an improvement in time management is
needed, and the GPA during the first semester of pharmacy school is lower than undergraduate
GPA. Additionally, students note that time spent on outside activities decreases upon admission
into the pharmacy program. The purpose of this study was to examine the outcomes of the peer
mentor program, specifically if there are positive outcomes for mentees when matched with an
upper classman mentor as compared to students who did not participate in the peer mentorship
program.
Methods: The University Institutional Review Board approved this survey of first professional
year 1 students intended to examine the use and impact of upper class pharmacy student mentors.
First professional year students completed an online survey administered during the end of the
Spring semester in their practice skills lab. Students were asked about their hours/week in
employment, exercise, social/recreational, sleep and student organizations. Students were also
asked to rate their stress during certain periods; time spent in class, studying and sleeping;
frequency of meeting with faculty and study groups; frequency of missed classes; and utilization
of different individuals (e.g. advisor, mentors, fellow students, family, staff) to support exam
preparation, assignments, note taking, time management, confidence boosting and expressing
concerns.
Results: There were 124 valid responses from the first professional year class for a response rate
of 83%. There was no statistically significant difference between respondents and nonrespondents with respect to admission GPA, PCAT, and first professional year semester GPAs
(p-values 0.349 0.923). Approximately two-thirds of mentees responded they were employed 0-3
hours per week during the Fall and Spring semesters; one-half reported exercising 0-3 hours per
week during the Fall and Spring semesters; and one-half reported engaging in social/recreational
activities 4-6 hours per week. There was a significant increase in the amount of time/week spent
involved in student organization from Fall to Spring for mentees (p = 0.017). Mentees reported
significantly more meetings with course faculty (p = 0.04) and with study groups (p = 0.018).
Mentees also obtained a significant increase (p= 0.016) in GPA (Fall to Spring). The greatest
utilization of mentors by mentees was for assisting with expectations for exams, followed by (in
decreasing order) managing time, boosting confidence, advising on taking notes, expressing
concerns and assisting with assignments. In a regression model, hours/week in social/recreational
activities, hours/week of sleep, stress level and missed classes were significant related to Spring
semester GPA (p < 0.001).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The peer mentorship program showed positive outcomes for mentees as compared
with non-mentees in GPA increase from fall to spring semesters. Additionally, mentees also slept
more, had a lower level of perceived stress, and attended class more often than the non-mentee
students.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-292
Title: Efficacy and safety of cephalexin for the outpatient treatment of acute uncomplicated
cystitis
Primary Author: Dustin Carr, Ferris State University, Michigan;
Email: carrd5@ferris.edu
Additional Author(s):
Purpose: Minimal data has evaluated the use of first-generation cephalosporins, such as
cephalexin, for the treatment of acute uncomplicated cystitis. This study aims to evaluate the
efficacy and safety of cephalexin for female patients with acute uncomplicated cystitis that are
empirically treated in an emergency department setting.
Methods: This study will be submitted to the Institutional Review Board for approval. This
study will be a retrospective chart review and patient survey assessing subjective outcomes. The
electronic medical record system will be used to identify female patients 18 years of age or older
that were diagnosed with acute uncomplicated cystitis between September 1, 2013 and
November 30, 2013. Survey data will include: age, allergies, adverse drug reactions, clinical
resolution of infection, overall satisfaction of cephalexin treatment, and side effects attributable
to cephalexin. If available, information regarding uropathogen susceptibilities and co-morbid
disease states will be evaluated. All information will be stripped of patient identifiers and
maintained confidentially in a secure location.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-293
Title: Treating acidosis comparing sodium acetate with sodium bicarbonate
Primary Author: Ellen Chackunkal, Wayne State University, Michigan;
Email: bb8687@wayne.edu
Additional Author(s):
Raymond Cha
Krassimir Denchev
Jessica Jones
Purpose: Sodium bicarbonate is the current exogenous alkali drug of choice to treat metabolic
acidosis in intensive care units (ICU). A recent sodium bicarbonate shortage prompted usage of
sodium acetate as an alternate, but data supporting the use of sodium acetate is sparse. The
purpose of this study is to compare intravenous sodium acetate to intravenous sodium
bicarbonate for the treatment of acidosis in critically ill patients.
Methods: This study will be submitted to the Institutional Review Board for approval. A
retrospective chart review will be performed of patients greater than 18 years, admitted to critical
care or step-down units who were treated for acidosis with sodium acetate infusion from October
2012 through January 2013. We will match these patients with a control group of patients who
received intravenous sodium bicarbonate for metabolic acidosis from August 2012 through June
2013. Approximately 50 patients received sodium acetate during this time. Specific variables that
will be collected include: age, gender, blood pressure, heart rate, BUN, serum creatinine, GFR,
ALT, AST, alkaline phosphate, bilirubin, albumin, ventilator status, pH, CO2, HCO3, oxygen
saturation, lactate, anion gap and alternative sources of alkali therapy received. The cause of
acidosis and any contributing factors including respiratory, renal, liver, and gastrointestinal
function will be evaluated. The primary outcome is the time to resolution of acidosis. Secondary
outcomes are ICU length of stay and mortality rate in both groups. Patient variables will be
compared between groups with Students t-test or Chi Square. Outcome variables will be
compared using multi-variable regression. Preliminary data will be presented at the 48th
American Society of Health-System Pharmacists Midyear Clinical Meeting.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-294
Title: Selenium deficiency in infants dependent on long-term parenteral nutrition: impact of the
nationwide intravenous selenium product shortage
Primary Author: Connie Chen, University of Michigan College of Pharmacy, Michigan;
Email: conniehc@umich.edu
Additional Author(s):
Mary Beth Harris
Maria Luisa Partipilo
Daniel Teitelbaum
Allison Blackmer
Purpose: Selenium, an essential trace element, plays critical roles in glutathione peroxidases,
thyroid function, growth, and development. Typically, selenium requirements are met enterally.
Parenteral nutrition (PN)-dependent patients unable to achieve adequate enteral intake rely on
intravenous supplementation. Selenium deficiency has been reported in adult PN-dependent
patients, including those receiving recommended supplementation. However, data regarding
selenium deficiency in PN-dependent infants is currently lacking; these patients may be at
increased risk for deficiency due to the ongoing nationwide intravenous selenium shortage. This
study aims to examine the impact of the selenium product shortage on the development of
selenium deficiency in PN-dependent infants.
Methods: This retrospective study was approved by the Institutional Review Board at The
University of Michigan. Patients who weighed &#8804;30 kg, received PN for &#8805;1 month,
received intravenous selenium, had &#8805;1 serum selenium measurement, and were &#8804;1
year of age at the time of the study were included. Patients were excluded if they exclusively
received enteral supplementation. No exclusions were made on the basis of gender or race. The
pre-shortage group included patients receiving PN between August 1st 2010 and July 31st 2011,
and the shortage group included patients receiving PN between August 1st 2011 and July 31st
2012. Data retrospectively collected from patient charts included demographics, intravenous
selenium dosing, serum selenium concentrations, pertinent laboratory parameters (e.g., complete
blood counts, thyroid function tests, iron studies, and C-reactive protein), growth parameters, and
clinical indicators of selenium deficiency (e.g., echocardiogram results). The primary outcome of
this study was the incidence of biochemical selenium deficiency, as defined by serum selenium
concentrations below age-adjusted norms, during the pre-shortage and shortage periods.
Secondary outcome measures included evaluations of the severity of biochemical deficiency,
time to development of deficiency, optimal selenium dosing for the prevention of deficiency, as
well as the financial impact of the shortage.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-295
Title: Impact of the change in community-acquired pneumonia guidelines on clinical outcomes
in pediatric patients
Primary Author: Shelby Chopp, Ferris State University, Michigan;
Email: Chopps@ferris.edu
Additional Author(s):
Jennifer Schultz
Purpose: Prior to the 2011 publication of the community-acquired pneumonia (CAP) guidelines
for infants and children older than 3 months of age, hospitalized children almost exclusively
received intravenous ceftriaxone with transition to oral cefdinir at discharge to complete
antibiotic treatment. The standard of care is to treat with intravenous ampicillin followed by
discharge on oral amoxicillin in fully immunized children. The purpose of this study is to
determine whether the change in antibiotic management has altered the clinical outcomes of fully
immunized children hospitalized with uncomplicated CAP.
Methods: This study will be submitted to the Institutional Review Board for approval. It will be
a retrospective cohort study examining patients charts from January 1, 2011 through January 1,
2013. Patients will be eligible based on diagnosis of pneumonia using ICD 9 codes 480-486 and
selection based on inclusion and exclusion criteria to meet a goal study size of 100 patients.
Pertinent patient information will include: patient age, sex, length of hospitalization, reported
immunization status, co-morbid conditions, allergies, respiratory rate, temperature, presence of
respiratory distress, use of supplemental oxygen, bacterial and viral studies, antibiotic usage
(drug and duration) while in hospital and outpatient antibiotic plan, presence of complications
(pleural effusion, empyema, acute respiratory failure, metastatic infection, SIRS), and
readmission for pneumonia within 14 days of hospital discharge. Once collected, all patient
information will be de-identified and further analyzed. Upon completion of the study, all patient
information collected will be appropriately destroyed by being placed in HIPAA bins and all
computer files will be deleted.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-296
Title: Impact of student pharmacist intervention on hospital consumer assessment of healthcare
providers and systems (HCAHP) communication about medication scores
Primary Author: Ryan D'Angelo, Ferrist State University, Michigan;
Email: dangelr@ferris.edu
Additional Author(s):
Lisa Meny
Purpose: To analyze the effect of student pharmacist provided medication education on the
hospital consumer assessment of healthcare providers and systems domain of communication
about medications for patients on the medical/surgical unit at a rural community hospital.
Methods: The institutional review board determined this project to be exempt from review as it
was viewed as a quality improvement initiative. Student pharmacists at a small community
hospital under the supervision of the staff pharmacists identified patients whose length of stay
reached a duration of 1 day by 0700 the following morning. Students reviewed patient charts and
identified new medications not previously prescribed in the outpatient setting. Patients with highrisk medications and/or high-risk disease states were identified as needing medication education.
Counseling points for medications/disease states were developed under guidance of the staff
pharmacist. Student pharmacists then met each patient, communicated indication for new
medication(s), side effects, monitoring parameters and beneficial lifestyle modifications.
Students documented questions from the patient and reviewed them with a pharmacist to develop
answers and reported back to the patient with answers. Each month the institution released data
gathered by a third-party group whom administered and collected HCAHP surveys. Reports were
collected during January-April 2013 to establish a baseline score for communication about
medication domain. Reports were then collected during May-July 2013. The difference from the
pre-intervention period and the interventional period will be measured to analyze the effect
student pharmacists had on those scores.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-297
Title: Pharmacist-led patient education as part of a multidisciplinary team and effect on 30-day
readmission rates for heart failure
Primary Author: Devin DeCator, Ferris State University, Michigan;
Email: decatod@ferris.edu
Additional Author(s):
Margaret de Voest
Michael Schirmer
Purpose: Previous studies have shown that multidisciplinary teams with pharmacist
interventions and discharge counseling have shown improvements in patients knowledge, selfmonitoring and medication adherence. The objective of this study is to evaluate if pharmacist
review of medications and counseling at discharge decreases 30-day readmission rates for heart
failure patients. The secondary outcomes for this study are ensuring patients are discharged on an
ACEI/ARB and on a beta blocker, as well as target doses of heart failure therapies.
Methods: This study was approved by the Institutional Review Board. A multidisciplinary, heart
failure rounding team recently added a pharmacist to their group where previously, pharmacy
independently addressed medication concerns. Pharmacists participating in rounding were
provided with education on the current heart failure guidelines. In addition to rounding with the
team daily, pharmacists provide discharge counseling focusing on the importance of adherence
and indications for each of their medications. Eligible patients with the primary diagnosis related
group (DRG) code of heart failure that were seen or consulted by the heart failure service prior to
adding a pharmacist and those seen after the addition of a pharmacist will be compared to see the
effects of the intervention on 30 day readmission rates. One hundred subjects will be recruited
for the control group and one hundred subjects for the study group. The following data will be
collected: age, gender, weight upon admission and discharge, blood pressure, BNP, ejection
fraction, heart failure stage, functional class of heart failure and medications upon admission and
discharge. Additionally, secondary outcomes will be measured by assessing target doses of
medications were met upon admission and discharge according to the 2013 ACCF/AHA
Guideline for the Management of Heart Failure.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-298
Title: Improvement of drug name pronunciation proficiency through the use of a computerassisted learning tool
Primary Author: Jennifer Dela-Pena, University of Michigan, Michigan;
Email: jendel@umich.edu
Additional Author(s):
Mustapha Beleh
Purpose: Medication errors are the leading cause of negative patient outcomes. Sound-alike
medications have been implicated as one important reason for such errors. Correct pronunciation
promotes patient safety by improving communication with the patients as well as within the
interprofessional health care team of physicians, nurses, pharmacists and other health care
providers. This study explored improvements of student pharmacists' drug pronunciation
proficiency in order to establish the efficacy of active-based learning environment facilitated by
the use of Drug List, an online interactive tool available at the University of Michigan, College
of Pharmacy.
Methods: The project was a double-blinded, randomized, longitudinal prospective cohort study
conducted at the University of Michigan, College of Pharmacy. Approval from the Institutional
Review Board (IRB) was obtained prior to study enrollment. Incoming first year Doctor of
Pharmacy students signed informed consent forms and were asked to record their pronunciation
of ten randomly assigned drugs during three phases, each with a three-week wash out period: the
first phase, there was no use of computer-assisted learning tool, the second phase allowed access
to phonetics breakdown, and the final phase included complete access to the Drug List consisting
of both phonetics breakdown and audio recorded clips of drug pronunciations. Students' ability
to correctly pronounce individual drugs was assessed based on their score using a pre-determined
Likert scale ranging from 1 to 3, with 1 indicative of poor pronunciation and 3 considered as
good pronunciation. Improvement in scores of students' drug pronunciation proficiency as the
phases progressed was considered to be the primary outcome of the study. The secondary
endpoint was improvement of drug pronunciation scores between students in the lower 25th
percentile compared to students in the upper 25th percentile for each phase of the study.
Results: A total of 149 students were enrolled in the study over a three year period and
continued to participate throughout the duration of the study. Students in phase one had a median
score of 25, with an increase in median score during phase two to 27 and the final phase to 29.
Overall improvement in scores from phase one to phase three was statistically significant with P
less than 0.05. During phase one, the top quartile of students scored a 28 or higher while the
bottom quartile scored 22 or lower. Students in the bottom quartile at the beginning of study
showed a significant increase in their scores from phase one to phase three (P less than 0.05),
while those already in the top quartile at the beginning of the study showed no statistical
improvement in their scores as they advanced to phase three (P equals 0.16).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Active-based learning through the use of an online tool resulted in a significant
overall improvement in student pharmacists' pronunciation proficiency of drug names. The effect
of the using the interactive technological resource was more pronounced among students in the
bottom quartile as there was significant improvement in scores as they advanced to the final
phase, while students in the top quartile did not show significant improvement.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-299
Title: Community pharmacist identification and intervention of patients at-risk for developing
acute heart failure: The One Minute Clinic for Heart Failure (TOM-C HF)
Primary Author: Nicholas Dillman, University of Michigan College of Pharmacy, Michigan;
Email: ndillman@med.umich.edu
Additional Author(s):
Dorothy Hoang
Richard Walls
Lindsey Westerhof
Barry Bleske
Purpose: The prevention of acute heart failure is heavily reliant on early identification. Many
patients exhibit signs and symptoms indicative of worsening heart failure on a regular basis;
however many dismiss these signs as an aging process or a comorbid condition. Because the
community pharmacist is often the primary point of health care for many patients, this study
seeks to assess the feasibility of a pharmacist-run intervention program to identify heart failure
patients at-risk for acute decompensation.
Methods: Participating pharmacists were required to review clinical management of heart failure
via an online tutorial that included three simulated scenarios of interactions, as well as sign an
affidavit verifying that they had completed these steps. The pharmacy identified patients with
existing heart failure through medication profile reviews or patient self-identification. The
pharmacist utilized a heart failure intervention questionnaire (the TOM-C HF tool) assessing
common signs and symptoms of worsening heart failure including: edema, shortness of breath
(SOB), paroxysmal nocturnal dyspnea (PND), and orthopnea. The pharmacist then followed a
structured protocol to perform an intervention, if applicable.
Results: A total of 121 patients were enrolled from ten different community pharmacies
throughout southeast Michigan and Ohio. Seventy-five patients (62% of subjects) experienced at
least one trigger symptom, making them eligible for an intervention. Common trigger symptoms
included edema (39%), SOB (29%), PND (19%), and orthopnea (6%). Although interventions
were indicated for 62% of patients, they were only sought in 41% of cases. The most common
intervention documented was for patients to schedule an office visit with their physicians.
Eighty-three percent of the interactions took between one and five minutes to complete, while
96% of the interactions took ten minutes or less. While 98% of pharmacists felt the tool was
somewhat valuable to highly valuable to the patient, 100% of pharmacists felt the tool was
somewhat valuable to highly valuable to their profession.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The TOM-C HF pilot study demonstrates the ability of community pharmacists to
identify and elicit interventions in patients at-risk for developing acute heart failure. A large
portion of heart failure patients in the community setting experienced at least one symptom
indicative of worsening heart failure. The tool required a relatively low time commitment and
was a valuable service to both pharmacists and patients. Early identification of patients at-risk
may help decrease future hospitalizations and may become a novel model for reimbursement for
clinical services.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-300
Title: Preliminary results of the incidence of bronchopulmonary dysplasia (BPD) following
administration of prophylactic surfactant for neonatal respiratory distress syndrome (RDS)
Primary Author: Rashmi Dungarani, University of Michigan College of Pharmacy, Michigan;
Email: rashmid@umich.edu
Additional Author(s):
Krystal Sing
Tracy Hsu
Varsha Bhatt-Mehta
Purpose: Surfactant replacement therapy for respiratory distress syndrome (RDS) is considered
to be mainstay in neonates. Both prophylactic and rescue treatment have been shown to reduce
mortality and the incidence of bronchopulmonary dysplasia (BPD). The incidence of BPD
following a single prophylactic dose of surfactant in neonates less than or equal to 28 weeks
gestation is not well described in the literature. The purpose of this study is to determine the
incidence of BPD following administration of prophylactic beractant (Survanta), a pulmonary
surfactant, in neonates less than or equal to 28 weeks gestation.
Methods: This study was a retrospective study evaluating data in the Vermont Oxford Network
(VON) database to determine the incidence of BPD in neonates born between March 2010 and
December 2011. A total of 67 patients were included in the study. Patients who were born less
than or equal to 28 weeks gestation or weighed less than 1001 grams, if gestational age was
unknown, were intubated at birth and were given beractant prophylactically at a dose of 4 ml/kg
every 12 hours. The primary outcome was the incidence of BPD, defined as requiring oxygen
supplementation, high flow nasal cannula use, or continuous positive airway pressure (CPAP)
use at 36 weeks gestation.
Results: Despite receiving prophylactic surfactant, 47.8% (32 of 67 patients) developed BPD.
Moreover, of the 32 patients, 20 patients (29.9%) required oxygen supplementation, 9 patients
(13.4%) required high flow nasal cannula, and 3 patients (4.5%) required the use of a Continuous
Positive Airway Pressure (CPAP) machine at 36 weeks of gestation.
Conclusion: The administration of prophylactic surfactant did not appear to decrease the
incidence of BPD, as reported in the literature.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-301
Title: Use and interpretation of quasi-experimental studies in pharmacy
Primary Author: Matthew Duprey, Wayne State University Eugene Applebaum College of
Pharmacy and Health Sciences, Michigan;
Email: mduprey@wayne.edu
Additional Author(s):
Jamie L. Wagner
Shawn M. Bockelman
Susan L. Davis
Purpose: Quasi-experimental studies are commonly used to test hypotheses in which
randomization and blinding are neither feasible nor ethical. Identification of quasi-experimental
design in publications is important because these designs have different inherent limitations
when compared with traditional observational or experimental studies. While some disciplines
have evaluated the quality of the reporting of quasi-experiments, no such analysis has been
performed in pharmacy literature. This review aims to evaluate the prevalence and quality of
quasi-experimental studies in pharmacy literature and determine the characteristics associated
with properly reported studies.
Methods: Articles in Pharmacotherapy, Annals of Pharmacotherapy, and American Journal of
Health-System Pharmacy published from 1 January 2010 to 31 December 2012 will be
evaluated. A study will be classified as quasi-experimental or not quasi-experimental by one of
two researchers on the basis of its title and abstract using standardized criteria. Experiments with
designs that cannot easily be evaluated will be read in entirety and adjudicated by a third
investigator. Data collected on each study will include: journal, year of publication, region of the
corresponding author (CA), degrees earned by the CA, single center versus multicenter, and
subject area. The quality of the research will be evaluated based on type of quasi-experimental
study, justification of the study design, correct identification of the study design, and notation of
inherent limitations (high quality indicators). A proportion will be calculated to determine the
presence of high quality indicators in quasi-experimental studies within the evaluated literature.
Secondary data will be analyzed to determine characteristics which may predict high quality.
This study will be exempt from review as it does not deal with any individual human subjects.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-302
Title: Overview of corticosteroid use for septic shock patients: a retrospective cohort study
comparing the duration of steroid treatment
Primary Author: Anna Escamilla, Ferris State University, Michigan;
Email: escamia@ferris.edu
Additional Author(s):
Tara Holt
Purpose: The sepsis guidelines for 2012 recommend that IV hydrocortisone only be used for
patients with septic shock when fluid resuscitation and vasopressor therapy cannot achieve
hemodynamic stability. The use of corticosteroids in septic shock patients is still controversial
and there are not specific recommendations on the duration of steroid therapy. The objective of
this study is to compare clinical outcomes in septic shock patients depending on the duration of
steroid treatment.
Methods: This study will be submitted to the Institutional Review Board for approval. The
electronic medical system EPIC will be used to identify patients who had septic shock and
required corticosteroids in order to achieve hemodynamic stability. The following data will be
collected: age, gender, name of steroid, dose and duration of steroid, fluid requirements, and
antibiotic administration. All data will be recorded without patient identifiers and maintained
confidentially. Descriptive statistics will be used to assess clinical outcomes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-303
Title: Developing an opioid assessment tool to reduce unintentional overdoses in the inpatient
hospital setting
Primary Author: Rebecca Finder, Ferris State University - College of Pharmacy, Michigan;
Email: finderr@ferris.edu
Purpose: Respiratory depression is the most serious adverse drug reaction associated with opioid
analgesics. Literature suggests this reaction occurs most frequently with high doses or erratic
dosing of opioid analgesics, while further research indicates certain comorbidities, age, and
social habits of patients play a role in increasing the risk for unintentional overdoses in the
inpatient setting. The objective is to develop an opioid assessment tool to identify patients in
jeopardy of an unintentional opioid overdose requiring the need for an opioid antagonist.
Methods: Electronic medical records for adult patients admitted to the medical center between
January 1, 2013 and December 31, 2013 requiring opioid antagonist administration will be
retrospectively reviewed for similarities and differences in patient characteristics, opioid
analgesic administration, and provider prescribing practices. Patients will be identified from the
EPIC and Portal systems. All adults not requiring opioid antagonist administration will be
excluded. The following will be collected without personal identifiers and maintained
confidentially: opioid antagonist administration, opioid dose prescribed and administered, timing
of opioid administrations, modifications to opioid prescription(s), total daily morphine
equivalents, department of occurrence, patient age, sex, weight, pain scores, sedation scores,
comorbidities, smoking habits, opioid exposure history, and opioid polypharmacy with
additional sedating medications such as benzodiazepines, antihistamines, sedatives, and central
nervous system depressants. This data will then be developed into an opioid assessment tool with
the goal of reducing unintentional overdoses requiring opioid antagonist administration in the
inpatient hospital setting. This study will be submitted to the Institutional Review Board for
approval.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-304
Title: Evaluation of the keys to a successful mentorship, a student-led mentorship program at a
college of pharmacy
Primary Author: Anna Fiorvento, Wayne State University Eugene Applebaum College of
Pharmacy and Health Sciences, Michigan;
Email: dw4904@wayne.edu
Additional Author(s):
Joshua N. Raub
Taylor M. Thurston
Purpose: Mentorship has been an essential part of training in many professions, including
pharmacy. Studies have shown that those who were mentored are more likely to be promoted,
are more productive and publish more often. In 2008, the "Keys to Successful Mentorship" was
created which was the first student-led mentorship program at a college of pharmacy. First year
student pharmacists (mentees) are paired with third year student pharmacists (mentors). The
objective of this study is to assess the influences and outcomes of initiating a student-led
mentorship program in a college of pharmacy.
Methods: This evaluative survey study has been submitted to the Institutional Review Board for
approval. This study will evaluate the perspectives of both the mentor and mentee, identifying
strengths and areas of improvement within the program. Second and fourth year student
pharmacists enrolled at this college of pharmacy will be provided a survey from the primary
investigator via email from an existing master class email list at the college. The second year
students will receive a mentee survey and the fourth year students will receive a mentor survey.
Participants will be asked to complete the online survey and submit their comments.
Participation in the study is voluntary and participants may opt out at any time. All participants
responses will remain anonymous to the study investigators and will be kept in a secure location
on the computer of the primary investigator. Results of this one time survey will be collected and
analyzed with descriptive statistics.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-305
Title: Heart failure treatment and readmission rates: a comparative retrospective study
Primary Author: Ryan Freye, Ferris State University, Michigan;
Email: rfreye@hotmail.com
Additional Author(s):
Mark Wilson
Purpose: The current heart failure guidelines promote the use of several medications to reduce
patient readmission rates and improve patient outcomes. The objective of this study is to
compare patient outcomes following admission and treatment under the current standard of care
and a new multidisciplinary heart failure treatment camp program.
Methods: This study will be submitted to the Institutional Review Board for approval. The
electronic medical record will be utilized to identify patients who have been admitted with a
diagnosis of heart failure during two set periods of time. Patients will be divided into the two
treatment groups based on their date of admission. The first group will receive treatment based
on the current standard of care while the second group will take part in a planned
multidisciplinary heart failure treatment camp. The following data will be collected: patient age,
gender, height, weight, heart rate, blood pressure, past admission dates, incidence and location of
edema, current medication list, past medical history, serum creatinine, creatinine clearance,
ejection fraction, and attending physician. Provider documentation will be examined to
determine reasons for non-compliance with current heart failure guidelines. All data will be
recorded, de-identified, and maintained in a confidential manner. Data will be reviewed using
appropriate statistical methods to determine possible associations. The main outcome will focus
on overall patient readmission rates at 30 and 90 days following their initial admission.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-306
Title: Effect of azole antifungals on the bioavailability of oral budesonide in patients with acute
gastrointestinal graft-versus-host disease
Primary Author: Katherine Gharibian, University of Michigan College of Pharmacy,
University of Michigan, Ann Arbor, MI;
Email: katghari@umich.edu
Additional Author(s):
David G. Frame
Purpose: Acute gastrointestinal (GI) graft-versus-host disease (GVHD) may be treated with
topically active oral corticosteroids, such as budesonide, to provide targeted therapy with limited
toxicities. Budesonide has low bioavailability due to high first-pass metabolism by the CYP3A4
isoenzyme. However, azole antifungals commonly used in this patient population may alter the
bioavailability of budesonide due to strong CYP3A4 inhibition. This study investigated the
bioavailability of budesonide in patients with GI GVHD to determine whether concurrent
administration of budesonide and azole antifungals would increase the plasma concentration of
budesonide compared to patients receiving budesonide and micafungin, an antifungal with
limited CYP3A4 activity.
Methods: The subjects in this retrospective cohort study were identified from a bone marrow
transplant list of long-term follow-up consented patients. Seventy patients who received an
allogeneic hematopoietic stem cell transplant between April 2008 and February 2013 and
developed acute GI GVHD were evaluated. Twenty-seven patients received oral budesonide for
the treatment of GI GVHD and had one or more plasma budesonide levels available in their
electronic medical record. All patients received concurrent prophylactic antifungal therapy of
micafungin, voriconazole, posaconazole, or fluconazole. Patients with documented hepatic
GVHD or other hepatic dysfunction or patients receiving a systemic CYP3A4 inhibitor other
than an azole antifungal were excluded. Budesonide doses ranged from 3 mg daily to 9 mg three
times daily. Plasma budesonide level was analyzed using liquid chromatography-tandem mass
spectrometry (LC-MS/MS) with a negative cutoff concentration of 0.04 mcg/dL. The primary
outcome was the comparison of plasma budesonide concentrations. Secondary outcomes
included the calculated percent of total daily budesonide dose absorbed and a calculated
equivalent prednisone dose. Dose-adjusted budesonide concentrations and all other dependent
variables were compared between azole antifungals and the micafungin group using univariate
linear regression analysis. All procedures were conducted under approval by the institutional
review board.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Results: Among the 45 plasma budesonide levels collected in the patients receiving micafungin,
voriconazole, and posaconazole, mean (standard deviation) concentration was 0.35 (0.43)
mcg/dL, 0.92 (0.94) mcg/dL, and 0.28 (0.14) mcg/dL, respectively. In univariate linear
regression analyses, concurrent administration of voriconazole was positively correlated with
plasma budesonide concentration (beta equals 0.725; P equals 0.001), percent of total daily
budesonide dose absorbed (beta equals 0.469; P less than 0.001), and a calculated equivalent
prednisone dose (beta equals 81.580; P equals 0.001). Non-significant correlations were found
between posaconazole and plasma budesonide concentration (beta equals 0.408; P equals 0.229),
percent of total daily budesonide dose absorbed (beta equals 0.180; P equals 0.337), and a
calculated equivalent prednisone dose (beta equals 45.881; P equals 0.229). Fluconazole was
omitted from analysis due to the small sample size (n equals 2).
Conclusion: Concurrent administration of voriconazole and oral budesonide was significantly
associated with an increase in plasma budesonide concentration in patients with acute GI GVHD.
Posaconazole resulted in no significant changes in budesonide bioavailability. The clinical
significance of increased corticosteroid levels in GVHD patients needs to be evaluated in future
studies.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-307
Title: Retrospective review of positive gonorrhea and chlamydia infections in the emergency
department
Primary Author: Allison Hanson, Wayne State University, MI;
Email: ahanson@wayne.edu
Additional Author(s):
Susan L Davis
Rachel Kenney
Angela Kieca
Purpose: Positive chlamydia and gonococcal infections are frequently identified in emergency
departments (ED). ED clinicians choose to treat with empiric or delayed treatment before
microbiology results are finalized. This study will aim to characterize the management of
chlamydia and gonococcal infections in the ED.
Methods: This study will be submitted for Institutional Review Board approval. The proposed
study will be a retrospective cohort of the management of gonorrhea and chlamydia in ED
patients. Patients will be screened using microbiology records from June 1, 2013 until August
31, 2013. All patients over age 18 tested in the ED will be included. Patients not presenting to
the ED, under age 18 and/or have a result for disseminated gonococcus, gonococcal meningitis,
ocular gonococcus and/or gonococcal endocarditis will be excluded. We will assess patient
demographics, insurance status, clinical presentation, diagnosis, and management (empiric
treatment, delayed treatment, follow-up time course, or no treatment) over time. In addition,
information on previous ED visits with positive sexually transmitted infection (STI) results will
be collected. Data to be analyzed includes patient demographics (age, sex, sexual orientation,
pregnancy, type of insurance, ethnicity, number/type of prior STI results, drug allergies),
presence of signs or symptoms indicating STI infection, diagnosis, antibiotic selection and time
course of follow-up. Appropriateness of treatment will be characterized by comparing the
treatment selected with the current Centers for Disease Control STI recommendations. Outcomes
assessed will include retreatment, revisit to the ED or hospital admission with any STI within 30
days.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-308
Title: Effects of continuing clofarabine therapy in adult acute myeloid leukemia (AML) patients
despite liver function test (LFT) abnormalities
Primary Author: Nicole Henige, University of Michigan College of Pharmacy, Michigan;
Email: nhenige@umich.edu
Additional Author(s):
Hyeon Hye Kang
Elizabeth Koselke
Shannon Hough
Shawna Kraft
Purpose: At the University of Michigan Health-System (UHMS) clofarabine is used in adult
acute myeloid leukemia (AML) patients who cannot tolerate standard induction therapy.
Transient liver dysfunction is a common adverse effect. Current parameters for holding treatment
include Tbili > 2 mg/dl, SCr >1.5 mg/dl, and/or AST/ALT > five times the upper normal limit.
Despite such parameters it is standard practice at UHMS to continue treatment based on clinical
evidence of benefit over risk. The objective of this study is to determine if current practice at
UMHS of continuing clofarabine treatment despite LFT elevations results in improved outcomes
of AML patients.
Methods: IRB approval was obtained prior to beginning the study and procedures were
conducted in accordance with HIPPA. This is a retrospective cohort study. Initially, 113 patients
with AML who qualified for the study were identified from UMHS records from January 2010
until July 2013. Inclusion criteria included patients >18 years old diagnosed with AML and
treated with induction clofarabine. Exclusion criteria included patients < 18 years old and
patients > 18 years old treated as pediatric patients. The following data was collected: gender,
age, height, weight, BSA, type of AML, overall risk based on cytogenetics and karyotype,
duration and dose of clofarabine administered, LFTs during clofarabine treatment and the
duration of the elevation, other adverse effects and their severity, response to therapy, and if
applicable duration and dose of cytarabine, duration of remission, and 30 day mortality with
cause of death. Data was recorded using REDCap without patient identifiers and remains
confidential. The categorical data will be analyzed using &#935;2 or Fishers exact test.
Continuous data will be analyzed using the Students t-test (dichotomous variables) or MannWhitney U test (non-parametric variables). All tests will be two sided and p values < 0.05 will be
considered significant.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-309
Title: Evaluation of risk factors for mortality in pediatric patients with blood stream infections
(BSI)
Primary Author: Helen Hong, University of Michigan, College of Pharmacy, Michigan;
Email: hhongsd@umich.edu
Additional Author(s):
Laura Schultz
Teresa Tu
Jerod Nagel
Kristin Klein
Purpose: Several publications have described mortality rates with pediatric BSI, and analyzed
risk factors for acquisition of BSI. However, there is currently no published risk factor analysis
to predict which patients are at high risk for mortality once diagnosed with BSI. Knowledge of
risk factors for mortality may allow for alternate early intervention in high risk patients leading
to improved outcomes.
Methods: Pediatric patients with positive blood cultures from Jan 2010 to Dec 2012 were
evaluated for inclusion. Patients were excluded with contaminated blood culture, which was
defined as skin flora in one of two sets of blood cultures, except for patients with chronic total
parenteral nutrition, neutropenia, transplantation, and located in neonatal intensive care unit at
the time of BSI. Risk factors evaluated in univariate analysis include age, gender, comorbidities,
immunosuppression, payer status, ICU status, infecting organism, source of infection, obesity,
and time until effective antibiotic therapy. Risk factors with p value less than 0.2 on univariate
analysis were included in multivariate logistic regression using SPSS, version 20.0.
Results: 257 patients were included for analysis. 30 day all cause morality rate was 9.33 percent.
Five risk factors yielded p value less than 0.20 after univariate analysis: chronic gastrointestinal
disease (p value equals 0.0013), female gender (p value equals 0.0853), admission to intensive
care unit (ICU) (p value equals 0.055), immunosuppression (p value equals 0.1886), and healthy
weight: defined as 5 to 85th percentile from the Center for Diseases Control and Prevention
growth charts (p value equals 0.1886). After controlling for cofounders through multivariate
logistic regression analysis, ICU admission (OR 3.53, 95 percent CI 1.347 to 9.249, p value
equals 0.010), immunosuppression (OR 2.849, 95 percent CI 1.124 to 7.22, p value equals
0.027), and pediatric patients with healthy weight (OR 2.955, 95 percent CI 1.009 to 8.49, p
value equals 0.048) were statistically significant risk factors for 30 day all cause mortality.
Conclusion: Pediatric patients with blood stream infections with immunosuppression, intensive
care unit admission, and healthy weight are associated with increased risk of 30 day all cause
mortality.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-310
Title: Creating a more accurate measure of inpatient anticoagulation quality
Primary Author: Sandra Hromek, Henry Ford Hospital, Michigan;
Email: bb9427@wayne.edu
Additional Author(s):
Pooja Mehta
James Kalus
Purpose: Measurement of quality of the anticoagulant medication use process is required for all
hospitals and health systems. Frequently, surrogate measures (INR > 5) are used to assess
anticoagulation quality, due to the difficulty in measuring outcomes related to anticoagulation
(bleeding or thrombosis). The objective of this study is to define a new measure of inpatient
anticoagulation quality that reflects patient outcomes more accurately.
Methods: This study will have two phases. The first phase will include patients anticoagulated
with warfarin, heparin or enoxaparin between 2007 and 2012. Patients with bleeding documented
in the discharge summary will be defined as cases. Patients without documented bleeding will be
controls. Cases and controls (n= 200) will be matched based on: (1) anticoagulant and (2) length
of stay plus/minus one day. The presence of inpatient surrogate markers indicative of bleeding
will be assessed for each group, and a univariate analysis conducted. Variables associated with
bleeding (p < 0.2) will be included in a multivariate regression model to determine which
variables are indicative. Variables demonstrating indicative value (OR = 1), will be used to
create a scoring system. In phase two, this score will be tested in a random sample of
anticoagulated patients with unknown bleeding status. Patients will be screened until similar
numbers exist in each strata plus/minus ten patients (n=300). Bleeding rates for each strata will
be evaluated, and based on distribution, a cutpoint for positive bleed will be defined. The
sensitivity, specificity and positive predictive value of the score will be assessed, and a receptor
operating curve (ROC) created. This study has been approved by the IRB.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-311
Title: Review of probiotics in the prevention of antibiotic-associated diarrhea in patients with
community acquired pneumonia: a retrospective study
Primary Author: Amanda Hult, Ferris State Univeristy, Michigan;
Email: hulta@ferris.edu
Additional Author(s):
Ashley Tocco
Purpose: Antibiotics are commonly known to cause diarrhea as an adverse drug reaction. The
objective of this study is to determine if adding probiotics to an antibiotic regimen for patients
greater than or equal to 60 years of age with community acquired pneumonia would reduce the
incidence of antibiotic associated diarrhea.
Methods: This study has been approved by the Institutional Review Board. This study will be a
retrospective chart review looking at the incidence of diarrhea for two cohorts of patients greater
than or equal to 60 years of age with community acquired pneumonia; one cohort of patients that
received antibiotics without probiotics and one cohort of patients that received antibiotics and
probiotics. Patients will be pooled from the Epic system using ICD9 codes for selecting out
patients diagnosed with community acquired pneumonia. The following data will be collected:
patient age, gender, initial CAP antibiotic regimen, number of antibiotics used, duration of
antibiotic therapy for CAP, probiotic added to antibiotic regimen, presence of diarrhea, previous
antibiotic use within 7 days of admission, duration of hospital stay, concurrent infection
requiring antibiotics, probiotic use prior to admission, use of proton pump inhibitor or H2
antagonist, use of laxatives or promotility agents, use of opioids, presence of nasogastric tube,
history of intestinal disease, presence of Clostridium difficile, readmission within 30 days, and
all cause mortality. All patient identifiers will be removed from the data collection sheets and
data will be stored securely.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-312
Title: Accuracy of HAS-BLED Bleeding Risk Score in Predicting Risk of Bleeding in an
Outpatient Anticoagulation Clinic
Primary Author: Emily Kearney, Ferris State University - College of Pharmacy, Michigan;
Email: kearnee3@ferris.edu
Purpose: The HAS-BLED score, a bleeding risk evaluation tool, has demonstrated that there is a
correlation between a higher score and an increased risk of a bleeding event in patients taking
warfarin. The objective of this study is to evaluate the effectiveness of the HAS-BLED score in
identifying patients taking warfarin at the anticoagulation clinic that are at a higher risk of
bleeding by comparing the score of patients that did and did not have a clinical bleed.
Methods: This study will be submitted to the International Review Board for approval. Patients
of the anticoagulation clinic that are at least 18 years of age or older and taking warfarin will be
pooled from the electronic medical record systems for the hospital and anticoagulation clinic.
Those with or without a clinical bleed while on warfarin between February 2013 to October 2013
will be included in the analysis. The following data will be collected: age, gender, HAS-BLED
score with a breakdown of each component that was designated a point. If available, the INR at
the time of the bleed, cause of the bleed, risk factors of the bleed present before it occurred, and
differences in care as a result of the bleed will be collected. All data will be recorded without
patient identifiers. The percentage of patients with a HAS-BLED score of 3 or greater that had a
bleed and those that did not have a bleed will both be calculated. The percentage of patients with
a HAS-BLED score less than 3 that had a bleed and those that did not have a bleed will also both
be calculated.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-313
Title: Student and preceptor perceptions of student performance following addition of self-care
therapeutics course to PharmD curriculum
Primary Author: Bianca Korkis, University of Michigan College of Pharmacy, University of
Michigan College of Pharmacy/Michigan;
Email: bkorkis@umich.edu
Additional Author(s):
Reema Hakim
Purpose: To determine the influence of a self-care therapeutics course on the ability of students
to practice confidently and competently in a community pharmacy setting
Methods: This is a retrospective, investigator-blinded analysis which targeted a total population
of 175 P2 (Class of 2014) and P3 (Class of 2013) students and 33 preceptors who worked with
members of both classes during their community pharmacy introductory practice experience
(IPPE). The Class of 2014 curriculum included a new self-care therapeutics course which was
implemented in their P1 year (winter 2011 semester). The community IPPE occurred during their
P2 year. In contrast, the Class of 2013 curriculum had self-care topics woven throughout the 4semester therapeutics sequence during their P2 and P3 year, with the community IPPE occurring
during P3 year. Both groups of students were sent the same 13-question survey which included
ten Likert-scale and three free-response questions. The preceptors were sent a 15-question survey
which asked them to compare the P2s and P3s. The students and preceptors were asked questions
regarding the students abilities to perform confidently, competently, and independently in a
community pharmacy setting. The survey was created using Qualtrics software and sent to the
students and preceptors at the end of the 2011-12 academic year. Both the students and
preceptors were sent periodic reminders to complete the survey.
Results: The student survey generated a 95% response rate from the Class of 2014, and 52%
response rate from the Class of 2013, for a total response rate of 74%. The students perceptions
of their performance were compared and analyzed between groups. For nearly all questions, a
larger percentage of the P2 class answered positively in terms of their self-perceived level of
confidence, competence, and ability to counsel patients on self-care than the P3 class. For
example, when asked whether they were able to recall and apply information from their
respective curricula about non-prescription medications when counseling, 73.5% of P2s versus
52.0% of P3s answered agree or strongly agree (p=0.1509). A response rate of 64% was
generated by the preceptor survey. When asked whether their students displayed preparedness,
confidence, competence, and independence, 60% answered positively that their P2 students
possessed these qualities; whereas only 2.6% responded negatively (all other responses were
neutral). When asked to compare their P2 and P3 students, 63% of preceptors agreed that P2s
performed similarly or better than the P3s, whereas 37% answered that their P2s performed
worse than their P3s.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: When comparing the Class of 2013 (P3) to the Class of 2014 (P2), it appears that
the addition of a self-care therapeutics course was an important contributor to the P2s greater
level of self-perceived confidence, competence, and ability to counsel patients effectively. These
results were verified by the preceptors perceptions of their students performance in the
community IPPE. Overall, the P2 class (Class of 2014) was more confident, competent, and
prepared to counsel patients on non-prescription medications than the P3 class (Class of 2013)
whose curriculum did not include the stand-alone self-care therapeutics course.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-314
Title: Assessment of the 2010 Food and Drug Administration (FDA) carboplatin dosing cap
recommendation
Primary Author: Rachel Lebovic, University of Michigan College of Pharmacy, Michigan;
Email: rlebovic@umich.edu
Additional Author(s):
Melinda Tran
Erika Howle
Catherine Christen
Shawna Kraft
Purpose: Previous studies have exposed difficulties dosing carboplatin based on renal function,
especially after serum creatinine assays were standardized between 2005 and 2010. The
standardized assays report lower serum creatinine values, which result in higher estimates of
glomerular filtration rates and higher calculations of carboplatin doses. The assay standardization
caused the FDA to create a dosing cap recommendation for carboplatin in 2010. This study aims
to assess whether doses above the FDA carboplatin dosing cap recommendation are associated
with more myelosuppression, treatment delays, and treatment reductions than doses below the
recommendation.
Methods: This study is a single-center retrospective chart review using the electronic medical
records of patients treated with at least three doses of carboplatin between August 1, 2009 and
August 31, 2012. The Institutional Review Board determined this study is exempt from informed
consent. Patients' electronic medical records will be reviewed to see if they were dosed above or
below the FDA recommendation to place them into the experimental or control group,
respectively. Primary endpoints will be platelet count, neutrophil count, number of treatment
delays, and number of reduced future doses. A sample size of 150 patients will be used to detect
a 20 percent difference between the groups and attain 80 percent power with a p-value of 0.05.
Categorical data will be analyzed using chi-square or Fisher exact tests. Continuous data will be
analyzed with the Student t test for dichotomous variables or Mann-Whitney U test for nonparametric variables. All tests will be two-sided and p values less than 0.05 will be considered
statistically significant.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-315
Title: Respiratory Viral Infection in Children: Potential Links between Adenovirus and Asthma
Primary Author: Adam Loyson, University of Michigan College of Pharmacy, Michigan;
Email: loysonad@umich.edu
Additional Author(s):
Krystal Sheerer
Kristin Klein
Jason Weinberg
Purpose: Respiratory viral infection (RVI) is a major trigger for wheezing episodes in infants
and asthma exacerbations in children. Respiratory syncytial virus and rhinovirus infections
during infancy have been associated with increased risks of asthma later in childhood; however,
little is known about long-term effects of early adenovirus (Ad) infection and outcomes, such as
asthma. We sought to characterize the epidemiology of RVI in children at our institution and
determine if early Ad infection increased the risk of developing asthma.
Methods: We retrospectively analyzed results of all assays for respiratory viruses (e.g., viral
cultures, antigen testing, polymerase chain reactions) in patients <18 years of age performed
from October 2000 to September 2010. Electronic medical records for patients with respiratory
virus testing were queried for ICD-9 codes corresponding to adenovirus, respiratory syncytial
virus, bronchiolitis, viral pneumonia, asthma/RAD, cough and wheezing. We compared the
incidence of asthma in children with Ad infection identified during the first two years of life to
the incidence in a control group of children matched by age who had negative respiratory tests
during the same time period.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-316
Title: Vancomycin Consensus Guidelines Application and Serum Concentration Target
Attainment
Primary Author: Danfeng Ni, Eugene Applebaum College of Pharmacy and Health Sciences,
Wayne State University, Michigan;
Email: nidaphne@gmail.com
Additional Author(s):
Kyle Rising
Anthony Casapao
Ryan Mynatt
Michael Rybak
Purpose: The Vancomycin Consensus Guidelines (VCG) recommends vancomycin (VAN)
dosing based upon serum trough concentrations with a target therapeutic range from 15-20 mg/L.
However, higher doses and prolonged VAN therapy have been associated with an increased
incidence of nephrotoxicity. Currently, limited data are available on the degree of compliance
with the guideline recommendations. This study was designed to assess vancomycin target
attainment at Detroit Receiving Hospital, a level-one trauma center, and to evaluate patient
characteristics associated with VAN-related nephrotoxicity.
Methods: Electronic medical records of patients receiving VAN therapy at Detroit Receiving
Hospital were reviewed from January 2012 to August 2012. Adult patients receiving &#8805; 72
hours of VAN treatment for a confirmed infection by the prescriber with at least one VAN
trough concentration were included. Patients baseline demographics including age, body mass
index (BMI), serum creatinine, and co-morbidities were obtained. Information related to VAN
therapy including dosage, serum trough concentration, and duration of therapy were also
documented. The primary outcomes of this study were documentation of VAN target attainment
(TA) and nephrotoxicity as defined by the VCG. Of interest, the Risk, Injury, Failure, Loss, and
End Stage Renal Disease (RIFLE) criteria and Acute Kidney Injury Network (AKIN) criteria of
nephrotoxicity were also assessed. Secondary outcomes included all cause mortality, readmission
at 30 days and length of stay.
Results: Out of 1,404 patients screened, 291 met inclusion criteria. 87 (29.9%) patients reached
TA of 15-20mg/L within the first 72 hours of therapy; however, 132 (45.4%) achieved TA
anytime during course of VAN. Patients that experienced nephrotoxicity per VCG, RIFLE, and
AKIN definitions were 9.3% (27/291), 12% (35/291) and 6.9% (20/291), respectively. 25.5%
(83/291) received a nephrotoxic agent concomitantly. There was a significant association with
RIFLE and AKIN in relation to the initial VAN trough (p=0.011 and p=0.008, respectively) but
not with VCG. In comparison between initial VAN trough groups of &#8805;15mg/L there was
no statistical difference for VCG and AKIN definition for nephrotoxicity compared to no
nephrotoxicity (p=0.059 and p=0.054, respectively). The RIFLE definition for nephrotoxicity
was significantly associated with troughs >15mg/L compared to troughs <15mg/L (16% vs. 5%;
p=0.005). By logistic regression, patients had an aOR 3.5 (95% CI, 1.3-9.4) to experience
nephrotoxicity defined by the RIFLE criteria when their initial VAN trough was
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
&#8805;15mg/L (p=0.004). Another predictor of nephrotoxicity by RIFLE criteria was
concomitant nephrotoxic agent with an aOR 2.4 (95% CI, 1.0-4.6); p=0.021. Of interest, an
initial VAN trough of &#8805;15 mg/L was not a predictor for nephrotoxicity as defined by the
VCG or AKIN criteria.
Conclusion: Despite recommendations from the VCG, approximately one-third of the patients
receiving VAN therapy achieved target attainment within 72 hours of initiating therapy and
slightly less than one-half of the patients achieved target attainment anytime during therapy. This
reflects the complexity of VAN dosing as patients vary in their baseline characteristics and
disease conditions as well as the need for more accurate dosing protocols. Patients with initial
VAN trough concentration of &#8805;15mg/L are more likely to experience nephrotoxicity as
defined by RIFLE definition but not by the VCG or AKIN definitions.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-317
Title: Assessing the effect of pharmacist case managers faxed discharge information on primary
care physician and community pharmacist communication
Primary Author: Uhunoma Osazuwa, University of Michigan College of Pharmacy, Michigan;
Email: unosazuw@umich.edu
Additional Author(s):
Barry L. Carter
Karen B. Farris
Purpose: Medication errors during transitions of care can lead to preventable adverse drug
events. In order to improve care transitions, collaboration and communication among health care
providers is critical. The purpose of this study was to determine if pharmacists and primary care
physicians (PCP) who received additional discharge information when patients return to the
community after hospital discharge were more likely to communicate about that patient than
those who received no additional discharge information. Furthermore, the study determined
whether pharmacies performing advanced clinical services and activities were more likely to
communicate with physicians about patients following discharge.
Methods: Patients from the Iowa Continuity of Care (COC) Study were randomized to an
enhanced intervention, minimal intervention or control group. For the enhanced intervention
group, a pharmacist case manager (PCM) provided a number of interventions within the hospital
and then faxed a discharge plan to the patients physician and community pharmacist. There was
no communication outside of the hospital for the minimal and usual care groups. As part of the
study, investigators included surveys to the physician and community pharmacists of each of the
enrolled patients. In addition, each pharmacy completed a structure survey to assess the level of
advanced clinical services and activities they provided. This study examined these data, using
responses from 315 community pharmacists, 150 physicians, and pharmacy structure data for
203 patients to analyze communication between pharmacists and physicians as well as the level
of services provided by the pharmacies. Institutional review board approval was obtained to
analyze these data.
Results: The frequency of communication between pharmacists and PCPs according to
pharmacists showed that 51 (16.2%) pharmacists reported contacting the PCP about a drug
related problem (DRP). Of the 51 patients whose pharmacists communicated with the PCPs, 18
(35.3%) were in the enhanced group while 33 (64.75%) were in the minimal/control group, yet
there was no statistically significant difference by study group (p=0.18) between pharmacist
responses to communicating with the PCP about a drug-related problem (DRP). Of the 37
patients whose pharmacists communicated with the PCPs, 12 (32.4%) went to advanced
pharmacies and 25 (67.6%) went to non-advanced pharmacies, and non-advanced pharmacies
were more likely to contact a physician about a DRP (p=0.04). However, there was no
statistically significant difference (p=0.286) in pharmacist communication by study group among
patients going to advanced or non-advanced pharmacies.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Controlling for advanced services in the pharmacy, the provision of faxed discharge
information to pharmacists and physicians for the patients in the enhanced study group of the
Iowa COC study did not lead to increased communication about the patient when compared to
those without the faxed information in the minimal/control groups. An explicit hand-off, either
verbal or electronic, should be considered in future studies to alert providers to the important
issues that patients may have during transitions of care.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-318
Title: Assessing peoples knowledge, attitudes, and habits regarding medication disposal
Primary Author: Courtney Peacock, University of Mississippi School of Pharmacy,
Mississippi;
Email: cjpeacockbird@gmail.com
Additional Author(s):
James J Pitcock
Purpose: A number of patients keep unused and expired medications in their homes, but most of
these patients are unaware of what to do with these medications due to a lack of clear guidelines
regarding correct disposal methods. The purpose of this study was to determine peoples
knowledge, opinions, and habits regarding the storage and disposal of their expired and/or
unused medications.
Methods: Surveys were distributed to 150 adults ages 18 and older at Walgreens pharmacies in
the Jackson, Mississippi metropolitan area. Surveys included a True/False exam assessing
participants knowledge about medication disposal, a questionnaire to determine participants
opinions regarding medication disposal, and some multiple choice questions to assess how and
why people dispose of their medications. Exam scores and questionnaire results were assessed
using Students t-test and Fishers exact test, respectively. Statistical significance was set at a pvalue of less than 0.05.
Results: Of the 150 study participants, 58% were female, 27% were Caucasian, 50% were under
the age of 50 years, and 67% had a college degree. Survey results showed that when people
dispose of their prescription and OTC medications, the most common method is by throwing
them away with regular garbage. The second most common disposal method is flushing
medications down the toilet. The average score of the True/False exam was 54.13%. Regarding
medication disposal, females were found to have significantly more positive opinions than males
(69.9% vs 64.3%; p=0.0125). People ages 50 and older have a significantly more positive overall
opinion about medication disposal compared to younger people (72.9% vs 62.2%; p=0.0001).
Individuals over 50 are also significantly more likely than younger people to be interested in
disposing of their medications at a pharmacy drug take-back day in the future (p=0.015) and to
believe that drop-off medication disposal programs are a convenient way to dispose of
medications (p=0.043).
Conclusion: According to my study, the general population does not possess knowledge about
proper medication disposal techniques. Females and older populations (ages 50 and older) are
more interested in proper medication disposal methods compared to males and/or those under the
age of 50. These populations may be inclined to take advantage of DEA drug take-back days, but
the general population could potentially benefit from education about these drug take-back days
as well as proper disposal techniques.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-319
Title: Clinical efficacy of fosfomycin following formulary approval and guideline
implementation for the treatment of urinary tract infections (UTIs)
Primary Author: Jennifer Pisani, University of Michigan College of Pharmacy, Michigan;
Email: jmpisa@umich.edu
Additional Author(s):
Jerod Nagel
Jennifer Heidmann
Laraine Washer
Tejal Gandhi
Purpose: Fosfomycin is active against extended-spectrum beta-lactamase (ESBL) producing
Enterobacteriaceae and vancomycin-resistant Enterococci (VRE) and is a cost-effective oral
antibiotic compared to traditional UTI treatment options. However, there is limited data
describing the implementation process, prescribing trends, and associated clinical and economic
outcomes following formulary approval.
Methods: This single center retrospective study evaluated fosfomycin prescribing from Jan to
Dec 2011 following formulary approval and guideline implementation. Approval for this study
was obtained from the institutional review board (IRB). Fosfomycin patients were matched to
historic cohorts based on pathogen, renal function and lower-tract UTI. Demographics, UTI
symptoms and labs, antibiotic prescribing, antibiotic costs, and clinical outcomes were evaluated.
Results: A total of 86 patients were evaluated: 43 patients in the fosfomycin and control groups.
The majority of patients received fosfomycin for the treatment of VRE (45.6 percent) and ESBL
Enterobacteriaceae (16.3 percent). Patients with a combination of allergies or documented
resistance to first line agents also received fosfomycin to treat Enterococcus (25.6 percent),
Enterobacteriaceae (7.8 percent) or multiple organisms (4.7 percent). Uncomplicated and
complicated lower tract UTIs accounted for 93 percent and 7 percent of fosfomycin prescribing,
respectively. 79 percent, 7 percent and 14 percent received 1, 2 and 3 doses of fosfomycin,
respectively. Doxycycline, nitrofurantoin, sulfamethoxazole/trimethoprim, meropenem and
linezolid were the most common antibiotics prescribed in the cohort group, with an average
duration of therapy of 5 days. Fosfomycin was associated with similar clinical success rates (95
vs 95 percent, P greater than 0.99) and recurrence rates (4.7 vs 4.7 percent, P greater than 0.99).
Additionally, the mean antibiotic cost saving per patient was 135 dollars and 6 cents by utilizing
fosfomycin instead of traditional antibiotics utilized prior to formulary approval.
Conclusion: Adding fosfomycin to formulary resulted in similar clinical success rates and lower
cost for the treatment of complicated and uncomplicated lower tract UTIs.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-320
Title: Structured review of medications with a black box warning utilized in an inpatient setting
Primary Author: Mindy Prasad, University of Michigan College of Pharmacy, Michigan;
Email: mwilfong@umich.edu
Additional Author(s):
Burgunda V. Sweet
Scott L. Ciarkowski
Margo Farber
Vincent D. Marshall
Purpose: The purpose of this study was to develop and test a scoring tool to assist in
determining whether an FDA-issued black box warning (BBW) should be incorporated into the
warning application process of clinical decision support (CDS) software thereby alerting
prescribers of the BBW at the time of order entry. It is hypothesized that having an objective
system for identifying, categorizing, and applying the most critical BBWs into clinically useful
notifications will facilitate the decision-making process for action needed when new BBWs are
identified.
Methods: The top 200 most commonly prescribed drugs in 2011 were identified and cross
referenced to identify those that had FDA-issued BBWs. Five different drug/BBW combinations
were analyzed by the investigator team to identify factors that may contribute to patient safety
concerns specific to the inpatient setting: potential severity of harm, likelihood of the event
occurring, and perceived volume of use. A scoring tool was developed and applied by the study
team to seven different drug/BBW combinations. Results were compared and adjustments made
to the scoring tool. The revised tool was then applied by the investigator team to 18 new
drug/BBW combinations to ensure consistent use of the tool. After validation, the tool was sent
to 26 drug information practitioners through a regional list serve. Respondents were asked to
apply the tool to ten unique drug/BBW combinations (pramlintide, fondaparinux, promethazine,
celecoxib, epoetin alfa, clindamycin, quetiapine, methotrexate, metoprolol, and
fluticasone/salmeterol), and to note whether the given drug/BBW was incorporated into CDS at
their institution. Results were assessed through descriptive statistics. This study had IRB
exemption; participation was voluntary.
Results: Thirteen drug information clinicians responded to the survey (50% response rate),
scoring each of the ten individual drug/BBWs in four different categories (severity of event,
likelihood of event while inpatient, prescriber awareness of BBW, and volume of use). A
summative score for each respondent, by drug/BBW, was calculated by multiplying the scores
for severity, likelihood, and volume. An average summative score was determined for each
drug/BBW. Average scores across each of the ten drug/BBW combinations ranged from 6.7 to
18.9 points. Scores fell into three distinct categories: low scores (<10) included metoprolol and
flucticasone-salmeterol, medium scores (10-14) included clindamycin, quetiapine, and
methotrexate, and high scores (>14) included pramlintide, fondaparinux, promethazine,
celecoxib, and epoetin alfa. The highest score was for pramlintide (18.9) and the lowest score
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
was for fluticasone-salmeterol (6.7). Average scores from respondents aligned closely with
scores assigned by the research team, suggesting that the tool was consistently applied by nave
users.
Conclusion: The scoring tool offered an objective way to evaluate drug/BBW combinations and
has the potential to serve as a guide for formulary decision makers regarding the need to
communicate with prescribers about a given drug/BBW, whether through inclusion of BBW
information into CDS or through some other means. Further study with more drug/BBWs and
larger numbers of respondents would offer further validation of the tool.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-321
Title: Linezolid utilization review: does targeted feedback improve pharmacist accountability?
Primary Author: Siddikur Rahman, Wayne State University, Michigan;
Email: rahmansiddikur@gmail.com
Additional Author(s):
Kelli Cole
Rachel Kenney
Susan Davis
Purpose: At our institution, pharmaceutical care is provided by pharmacy-driven Patient Care
Teams (PCTs). One responsibility of each PCT is management of antimicrobials, including
identifying opportunities for de-escalation and conversion from intravenous (IV) to oral (PO)
administration. Linezolid is particularly targeted due to its high bioavailability and broad
spectrum, and pharmacists can play a key role in the use of this agent throughout the hospital.
The objective of this study is to evaluate the frequency and time to pharmacist-initiated
interventions on linezolid use based on specific PCTs.
Methods: This is an institutional review board approved descriptive and retrospective study. All
inpatients with an active order for linezolid between January 1, 2013 and June 30, 2013 will be
included in the study and patients who received less than 24 hours of linezolid will be excluded.
Subjects will be grouped according to one of the four PCTs responsible for their care based on
their location in the hospital: Surgery, ICU, General Medicine, and Specialty
Medicine/Oncology. Included patients will be evaluated for the presence of pharmacist-initiated
intervention opportunities such as discontinuation, de-escalation, and IV to PO conversion, with
the primary outcome of characterizing linezolid use for all patients within each PCT. Deescalation opportunity is defined as evidence of an organism grown on culture that was
susceptible to amoxicillin/ampicillin, vancomycin, or another narrower-spectrum agent active
against that particular organism. Oral conversion is defined as meeting our institution criteria for
pharmacist-initiated IV to PO conversion. Time to completion of these interventions will also be
assessed. All analyses will be descriptive. Categorical variables will be presented as n (%).
Continuous variables will be presented as mean (range) or median (interquartile range, IQR), as
appropriate based on distribution (normal vs. not normal).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-322
Title: Evaluation of daptomycin use in a community hospital to achieve cost savings
Primary Author: Karl Renius, Ferris State University, Michigan;
Email: Reniusk@ferris.edu
Purpose: Daptomycin is effective in treating many gram-positive infections. However, routine
use of daptomycin increases hospital formulary expenses. The purpose of this study was to
reveal patterns of daptomycin use and develop strategies to curb costs.
Methods: A retrospective electronic medical record review of 136 patients who received
daptomycin was conducted. Daptomycin use was reviewed in context of laboratory values,
mortality, prescribed medications, indications, length of therapy, physician consults, and patient
outcomes.
Results: The mean duration of daptomycin therapy was 4.06 days. Rationale for daptomycin use
primarily included included step-up therapy from vancomycin (62.5%),documented vancomycin
allergy (21.3%), and initiation of outpatient therapy prior to discharge (19.9%). Nine patients
were candidates for ceftaroline therapy in place of daptomycin. Of the 21 patients who received
one dose of daptomycin prior to discharge, 17 (81%) were escalated from vancomycin therapy.
Conclusion: Potential areas for cost savings were elucidated. These included initiation of
outpatient daptomycin therapy outside of the hospital setting, diligent antimicrobial stewardship,
and increased use of ceftaroline when appropriate.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-323
Title: Liposomal bupivacaine versus standard therapy to control postoperative pain in adults
following open abdominal surgery.
Primary Author: Ryan Rogoszewski, Ferris State University, Michigan;
Email: rogoszr@ferris.edu
Additional Author(s):
Curtis Smith
Purpose: Local anesthetics are a prominent form of pain relief in the surgical setting. Liposomal
bupivacaine (LPSB) is a sustained-release, injectable form of bupivacaine approved for
postsurgical pain in patients undergoing hemorrhoidectomy and bunionectomy. The sustained
duration of action make it a potential option in the prevention of postsurgical pain in other
surgical settings including breast augmentation, total knee arthroplasty, and open colectomy. The
purpose of this study is to examine the effectiveness of perioperative administration of LPSB in
controlling postsurgical pain in open abdominal surgeries, compared to standard therapy.
Methods: Patients aged 18 and over at a single clinical site, who had received LPSB between
January and September 2013, were identified using electronic pharmacy records. Those patients
undergoing open abdominal surgery were further evaluated. Pain scores were reviewed from 096 hours after surgery (in intervals) or until discharge, whichever occurred first. Other data
collected included the amount of time to first dose of opioid, number of morphine equivalents
consumed in the 96 hours following surgery (or until discharge) and length of stay. Readmission
to hospital, surgeon, anesthesiologist, number of comorbidities, and other analgesics received
(i.e. tramadol, acetaminophen, ibuprofen, and ketorolac) were also recorded and monitored. This
group was then compared to matched individuals undergoing open abdominal surgery whom had
received conventional pain management without LPSB. This research received approval from the
local Institutional Review Board as exempt from review. Patient consent was not needed for this
research because of its exempt status. Forty-six patients were enrolled in each group. Data will
be presented.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-324
Title: Comparison of patient-perceived pharmacist relationships between practice settings,
including an independent retail pharmacy, 340B FQHC pharmacy, and a free medical clinic
without an on-site pharmacy
Primary Author: Christina Salib, Ferris State University College of Pharmacy, Michigan;
Email: salibc@ferris.edu
Additional Author(s):
Christina Salib
Susan Devuyst-Miller
Purpose: This study is designed to assess patient perception regarding the availability, trust
level, knowledge-base, and empathetic value of pharmacists. The results from the various
practice settings will be compared to determine which pharmacy setting has better patientpharmacist relationships. In terms of availability and empathy, this study aims to identify which
clinical setting results in patients trusting their pharmacists more, asking more questions about
their healthcare and medications, and feeling more connected to their pharmacist. The practice
settings involved can identify ways they are successfully meeting patient needs and target efforts
towards enhancing pharmacist-patient relationships.
Methods: The data was collected within a two-month time period, from June 20th to August
20th 2013. Participating settings included Shiawassee Free Medical Clinic, Lafayette Drugs, and
Cherry Street Heart of the City Pharmacy. The subject population was English-speaking patients
over the age of 18, including pregnant women and individuals with mental and physical
disabilities. Those excluded were minors under the age of 18, prisoners, and non-English
speakers. The student pharmacist traveled to the practice settings to recruit patients using an
Institutional Review Board approved consent form/survey invitation. Subjects privacy was, and
is, protected through unidentified, anonymous surveys. Once consent forms were signed, the
student read the surveys to the patients and collected their responses. Responses were collected
via paper by the student researcher. Survey forms were labeled with the location, but were not
linked to the patient. The questionnaires were scanned as PDF files, and then shredded. The data
was stored on a password-protected computer and converted to password-protected Microsoft
Word files. Microsoft Excel was used to compile survey responses. The survey/questionnaire
data was analyzed using the SPSS (IBM) statistical analysis software.
Results: Research is in progress. A total of 80 surveys were collected, and completed, within the
two-month collection period; 23 from Shiawassee Free Clinic, 24 from Lafayette Drugs, and 33
from Cherry Street pharmacy. Based on the patient survey interviews, anticipated results
demonstrate that patients receiving care at Lafayette Drugs, an independent retail pharmacy,
showed that they trusted, were comfortable, and had a defined relationship with their pharmacists
in comparison to the free medical clinic and the 340B pharmacy.
Conclusion: Research is in progress.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-325
Title: Relationship of CAV-1 polymorphisms in metabolic syndrome associated lipid
abnormalities in schizophrenia patients
Primary Author: Sahar Seyedin, University of Michigan College of Pharmacy, Michigan;
Email: seyedin@umich.edu
Additional Author(s):
Kyle J. Burghardt
Vicki L. Ellingrod
Purpose: For individuals with a diagnosis of schizophrenia, the risk of developing metabolic
syndrome is twice that of the general population. At the heart of metabolic syndrome are
perturbations in lipid homeostasis that place schizophrenia patients at risk for CVD. Caveolaes
are cell surface plasma membrane invaginations that aid in the regulation of cholesterol
homeostasis. Caveolin-1, the protein contained within the caveolae, has been suggested to play a
vital role in the transcytosis and storage of plasma lipoprotein. Aberrant polymorphisms of
Caveolin-1 (CAV-1), suggest a relationship between this gene and dyslipidemia. The purpose of
this study was to investigate the relationship between genetic variation within CAV-1
(rs4730751 A/C allele), and elevated low-density lipoproteins (LDL), triglycerides and total
cholesterol in schizophrenia patients who are taking psychotropic medications. We hypothesized
that patients with the CAV-1 CC genotype would have greater plasma levels of LDL,
triglycerides and total cholesterol compared to schizophrenia patients with the A allele.
Methods: This IRB-approved cross-sectional study investigated subjects diagnosed with
schizophrenia or schizoaffective disorder who were taking psychotropic medication and had
been stable for at least 6 months. After informed consent was obtained, a fasting blood sample
was collected to measure plasma lipid levels and DNA was extracted from a whole blood
sample. Polymorphisms were determined through the use of pyrosequencing and subjects were
stratified into CAV-1 CC genotype and CAV-1 A allele groups (AA or AC). Elevated LDL,
triglycerides and total cholesterols levels were defined as > 130 mg/dL, > 150 mg/dL, and > 200
mg/dL respectively. The primary endpoints were plasma levels of LDL, triglycerides and total
cholesterol in both CC genotype and A allele groups. A general regression analysis was
performed to examine the relationship between the plasma LDL, triglycerides and total
cholesterol as dependent variables, while genotype, age, gender, and interactions were used as
independent variables. A p-value < 0.05 was considered statistically significant. All statistical
analyses were performed using JMP from SAS software, version 10.0.2.
Results: A total of 235 subjects were originally tested and 20 subjects were unable to be
genotyped due to sample fatigue. From the remaining 215 patients, 86 (40%) were female, 110
(51%) were smokers, and 122 (57%) were Caucasian. The mean age was 45 +/- 13.5 years. The
CC genotype group consisted of 125 (58%) patients and the A allele group comprised of 90
(42%) patients. The CAV-1 genotype was in Hardy Weinberg disequilibrium (p>0.05). The
mean LDL was 104 mg/dL for genotype CC and 108 mg/dL for A allele groups. The mean
triglyceride and mean total cholesterol levels displayed similar findings. In general, results
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
indicated there was no statistically significant relationship between CAV-1 genetic
polymorphisms and LDL (P=0.6), triglycerides (P=0.6) and total cholesterol (P=0.8) levels.
Conclusion: In conclusion, no relationship was found between the CAV-1 rs4730751 variant
and overall lipid levels in patients with schizophrenia treated with antipsychotics. Although the
results of this study were overall negative, the utilization of genetic differences in an individuals
DNA for future studies may prove otherwise. With the growing use of pharmacogenomics,
future studies may shed some light on valuable information and help clinicians assess
cardiovascular risk when determining appropriate psychotropic medication.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-326
Title: Impact of pharmacist-driven heart failure patient education on readmission rates
Primary Author: Malissa Shapas, Wayne State University, Michigan;
Email: mshapas@gmail.com
Additional Author(s):
Larry Diamond
Sin-Ling T. Jennings
Purpose: The prevalence of congestive heart failure (CHF) in the U.S. is more than 5 million
people, accompanied by nearly 34.4 billion dollars in annual healthcare costs. CHF is also
complicated with historically low adherence to medications and lifestyle modifications.
Therefore, education programs have been implemented by nurses, and have been shown in
literature to be beneficial in improving adherence and readmission rates. We aim to explore the
impact of pharmacist-driven educational programs to further reduce readmission rates. Our
objective is to assess the impact of a pharmacist-driven education program for patients
discharged with congestive heart failure on 30-day readmission rates.
Methods: We will retrospectively assess patients admitted to a local community hospital for
CHF. Patients are selected to undergo heart failure patient education by a daily report generated
by an administrative nurse practitioner for the International Classification of Diseases (ICD),
ninth edition code 428.0 for congestive heart failure, unspecified. The nurse practitioner will
interview the selected patients and determine their eligibility for a pharmacist-driven patient
education. Education and medication informational handout is provided on any of the following
medications the patient is discharged on: beta-blockers, angiotensin converting enzyme (ACE)
inhibitors, angiotensin II receptor blockers (ARBs), diuretics, aldosterone antagonists,
hydralazine and isosorbide dinitrate. Patients educated by a pharmacist are followed for 30 days
post-discharge to determine readmission occurred. The following data that will be analyzed from
a patients electronic medical record chart: admission date, date education was provided by a
pharmacist, date of readmission within 30 days of discharge. Patients readmitted within 30 days
will then be sub-analyzed to reason for readmission. All data will be recorded without patient
identifiers and maintained confidentially. We hypothesize that patients that received pharmacistdriven patient education will have lower readmission rates than patients that did not receive
education.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-327
Title: Adjusted-dose versus full-dose daptomycin for the treatment of vancomycin-resistant
Enterococcal bacteremia in morbidly obese patients
Primary Author: Jennifer Smith, University of Michigan College of Pharmacy, Michigan;
Email: jennysmi@umich.edu
Additional Author(s):
J. L. Nagel
R. Bendali-Amor
T. Gandhi
L. Washer
Purpose: Daptomycin single-dose pharmacokinetic studies demonstrate considerable increases
in Cmax and AUC among obese patients compared to normal weight patients when dosed using
actual body weight (ABW). Additionally, obesity is a risk factor for myotoxicity with
daptomycin dosing based on ABW, which led the authors of one publication to recommend
utilizing ideal body weight (IBW) when calculating daptomycin dosing. There is currently no
data evaluating clinical outcomes of infections treated with adjusted-dose daptomycin. The
purpose of this study was to evaluate the clinical outcomes of morbidly obese patients with VRE
bacteremia treated with adjusted-dose daptomycin compared to those treated with full-dose
daptomycin.
Methods: This single-center retrospective study evaluated all morbidly obese patients (BMI
greater than 30 kg/m2) with VRE bacteremia treated with daptomycin from September 2010 to
May 2012. Patients receiving 6 mg/kg daptomycin based on ABW were compared to those
receiving 6 mg/kg based on AdjBW (defined as 0.35-0.5[ABW-IBW] + IBW). Patients receiving
other doses were excluded. Patient demographics, comorbidities, treatment regimens, antibiotic
cost and clinical outcomes (30-day all-cause mortality, length of stay, microbiologic clearance,
recurrent bacteremia and toxicity) were evaluated.
Results: 47 patients were included in the final analysis: 31 with ABW daptomycin and 16 with
AdjBW daptomycin. Demographics, including weight (101 vs 109 kg, p=0.172) and BMI (35.5
vs 36.6 kg/m2, p=0.612), were similar between ABW and AdjBW groups, respectively. Thirtyday all-cause mortality (25 vs 19%, p=0.676), length of stay (41.8 31.0 vs 26.6 21.0 days,
p=0.84), mean time to microbiologic clearance (2.24 vs 2.6 days, p=0.536), recurrent bacteremia
(3 vs 13%, p=0.26), any creatinine kinase elevation from baseline (45 vs 38%, p=0.758) and
myalgia or rhabdomyolysis (3.2 vs 0%, p>0.99) were also similar between ABW and AdjBW
groups, respectively. However, the AdjBW group was associated with a mean daptomycin cost
saving of $1,822 per patient.
Conclusion: This pilot study suggests utilizing daptomycin based on adjusted body weight may
result in similar clinical outcomes while decreasing daptomycin cost. These results support
further evaluation in large-scale trials.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-328
Title: Cardiovascular risk assessment for adults with and without developmental disabilities
Primary Author: Patrick Spoutz, University of Michigan, Michigan;
Email: pspoutz@gmail.com
Additional Author(s):
Steven Erickson
Purpose: Individuals with developmental disabilities (DD) are living longer than ever before.
Consequently, they are now facing a unique set of challenges associated with the diseases of
aging. Though some studies have addressed the prevalence of coronary heart disease (CHD) risk
factors in those with DD, to date no studies have examined overall levels of CHD risk in this
population and comparing their CHD risk to that of the general population. This project was
designed to perform this comparison and examine potential gaps in key metrics of care between
those with DD and general populations at a major academic medical center.
Methods: This study uses Framingham risk analysis to calculate the overall level of CHD risk
for individuals with developmental disabilities inside a major academic medical center. This
retrospective cross-sectional study was conducted using data on patient-specific CHD risk
factors retrieved from the electronic medical record. Levels of CHD risk in the DD outpatient
population were compared against a random sample of general medicine outpatients without DD.
Additional outcome metrics include the percentage of patients lacking a record of a basic lipid
panel. Descriptive data are presented as means with standard deviation or frequency and percent.
Comparisons between groups are made using Students t-Test for continuous variables and Chi
square for categorical variables.
Results: This study consisted of 181 individuals with DD and 103 individuals without DD. The
average age of the DD sample was 49.6 versus 54.5 (P equals 0.006) for non DD patients. The
DD population was 47.0 percent female compared to 64.1 percent of the non DD sample, P
equals 0.01. With respect to cardiovascular risk factors, the DD population demonstrated a nonsignificantly lower rate of smoking, hypertension diagnosis, total, LDL, and HDL cholesterol.
Though also not statistically significant, diagnosis of stroke was more common in the DD
sample, (5.6 percent to 1.9 percent, P equals 0.15). For males, 10 year Framingham risk scores
were lower in the DD sample, 6.08 percent compared to 7.49 percent, though this value was not
statistically significant (P equals 0.1). No differences were seen in 10 year Framingham risk
scores for females (1.5 percent compared to 2.1 percent for the DD and general samples,
respectively, P equals 0.38). Lastly, patients with DD had a lower rate of cholesterol monitoring.
There were 44.4 percent of DD patients lacking cholesterol records within the last two years,
compared to only 18.5 percent of the general population.
Conclusion: Though not statistically significant, males with DD appear to have lower 10 year
Framingham risk than males in the general population, while women with DD had levels of risk
similar to the general population. Individuals with DD also had a lower rate of cholesterol
monitoring than the general population.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-329
Title: Monoamine oxidase inhibitors combined with other antidepressants: a case series
Primary Author: Samantha Thomas, University of Michigan College of Pharmacy, Michigan;
Email: thomassj@umich.edu
Additional Author(s):
Mirae Shin
Melvin McInnis
Jolene Bostwick
Purpose:
Methods:
Results:
Conclusion:
Case Report: This case series reviewed patient cases in which monoamine oxidase inhibitors
(MAOIs) were used in combination with other antidepressants in order to 1) describe and
evaluate the outcomes when combination therapies have been used, 2) determine the cause of
adverse reactions and assess for confounding variables that may have been contributing factors,
and 3) share experiences of these patients in order to add to the literature on MAOI combination
therapy in individuals with treatment resistant depression.
Information was gathered from the medical charts of 29 patients treated with an MAOI in
combination with one or more antidepressants at a large, Midwestern academic hospital. Data
including patient demographics, indication, past medication trials, duration of therapy, other
serotonergic medications, tolerability, symptom control, and reasons for discontinuation were
documented and reviewed.
Combinations used include MAOI + trazodone (16), MAOI + TCA (4), MAOI + bupropion (2),
MAOI + mirtazapine (1), MAOI + SSRI (1), and MAOI + 2 other antidepressants (5). A total of
6 patients received combination therapy with improvement in mood and no or minimal/tolerable
adverse effects. Adverse effects resulted in discontinuation in 10 patients, including 3 possible
cases of serotonin syndrome. Other known reasons for discontinuation include lack of benefit or
effectiveness, increased suicidality, patient decision, and preparation for ECT.
The most common combinations seen among patients were MAOIs combined with either
trazodone, a TCA, or both. The average duration of therapy for combination therapy with
trazodone was 21 months and the majority of patients receiving TCA combination therapy
remained on the regimen, with the exception of 2 cases.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Inadequate response to standard antidepressant medications is common and combined
therapeutic approaches are frequent. This review of combined MAOIs with other antidepressants
found that 20% of patients improved significantly with no complications and 30% showed side
effects that required discontinuation of the MAOI. The remaining patients tolerated the
combination well, but with modest improvement in mood.
This case series suggests that when used under close supervision and under the care of an
experienced clinician in psychiatry, combination therapy may be a consideration for the
management of treatment resistant depression in patients not responding to monotherapy or other
combinations of antidepressants.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-330
Title: Graduating pharmacy students impressions of a Doctor of Pharmacy program
Primary Author: Hoai-Phuong Tran, University of Michigan College of Pharmacy, Michigan;
Email: hoaitran@umich.edu
Additional Author(s):
Jordan Whelan
Nancy A. Mason
Purpose: In the 2011 American Association of Colleges of Pharmacy (AACP) Graduating
Student Survey, our College of Pharmacy's scores on questions related to overall impressions of
the program showed a considerable drop compared to previous years. Concerned with these
unsatisfactory responses, the College took immediate action to identify factors influencing
students' perceptions of its PharmD program. The purpose of this study was to assess student
impressions of our College's Doctor of Pharmacy program in greater depth, using the AACP
Graduating Student Survey as a basis for more detailed questions.
Methods: A paper survey, entitled the P4 Exit Survey, was developed with questions
encompassing students' overall impressions involving three general domains: 1) students'
preparedness to enter pharmacy practice, 2) students' perception of pharmacy as a profession,
and 3) students' perception of our College of Pharmacy. Each section consisted of a main
question that related to a general domain followed by a free-response portion. Included in each
section were also subsequent statements regarding potential factors influencing students'
responses to the main questions. Using a 4-point Likert scale where 4 = strongly agree, 3 =
agree, 2 = disagree and 1 = strongly disagree, the frequency, mean and standard deviation for
each survey statement were determined. In order to gain a better understanding of factors that
had the greatest impact on students' answers, a factor analysis using Pearson product-moment
correlation was performed. In addition, students' free responses were qualitatively analyzed and
common themes were tabulated. Chi-squared tests were used to compare the frequencies of
results for questions that were common among the P4 Exit Survey and AACP Graduating
Student Surveys for our College and national schools. The level of significance was set at p <
0.05.
Results: Of the 63 graduating students contacted, 61 (96.8%) completed the survey. The results
showed that 95% of respondents felt prepared to enter practice; this was 6% greater than the
level of agreement in our College's 2011 Graduating Student Survey. Respondents noted
Advanced Pharmacy Practice Experiences (APPEs) and specialized clinical rotations as positive
factors in their preparation. In contrast, Introductory Pharmacy Practice Experiences (IPPEs) and
career guidance were indicated least often as factors influencing students' preparation. A total of
95% of respondents indicated that they would study pharmacy again; this result was significantly
higher than the response to the same question on our College's 2011 survey (75%, p = 0.006) and
the national 2012 survey (82%, p = 0.024). Position flexibility and autonomy were major
motivators for choosing pharmacy again, while a major deterrent was the saturated job market.
For the question regarding whether they would choose the same college of pharmacy again,
respondents to this survey demonstrated the highest percentage of agreement (92%) among the
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
comparator surveys. Respondents noted the strong alumni support and small class sizes as
reasons for choosing our College again.
Conclusion: Graduating students from our College of Pharmacy had overwhelmingly positive
perceptions regarding their quality of education. Our College continues to do well in providing
students with strong APPEs, specialized clinical rotations, and alumni support. Areas in which
our College may improve include more challenging and consistent IPPEs as well as the
development of a structured career service. Overall, students felt that our College sufficiently
prepared them for pharmacy practice, and the vast majority would choose to study pharmacy
here again.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-331
Title: Changing the way pharmacists educate their patients: a concierge-style approach to patient
education
Primary Author: Jessica Traster, Henry Ford Hospital, Michigan;
Email: jtraste1@hfhs.org
Additional Author(s):
Nadia Haque
James Kalus
Margi Shah
Melinda Staton
Purpose: It has been shown that providing patients with education when preparing for discharge
improves outcomes and reduces readmissions in many patient populations. It is also thought that
it can improve patient satisfaction with their hospital experience. The responsibility of patient
education is shared by pharmacists, especially with medications. Currently, pharmacists in our
institution utilize a traditional approach to provide this education, which involves going to the
patients room when it is convenient for the pharmacist. The purpose of this study is to assess the
impact of a concierge-style approach to pharmacist-provided education on patient knowledge
and satisfaction.
Methods: The institutional review board approved this randomized controlled trial. Inpatients
will be included in the study who are being treated in an internal medicine unit with one or more
of the following chronic disease states: hypertension, congestive heart failure, diabetes mellitus,
or chronic obstructive pulmonary disease. Forty patients will be enrolled in each of the four
study groups. Patients will be randomized to receive traditional pharmacist-provided education,
including a baseline knowledge assessment and educational session on medications related to the
patients target diagnosis. Patients enrolled in the study arm will involve an initial visit to set up
an appointment at which the baseline knowledge assessment and educational session will be
performed. Both groups will be approached at least one day after the education was provided to
perform a follow-up assessment. The primary endpoint is patient knowledge of their medication
use, dose, and side effects in the experimental versus traditionally educated groups based on
assessment with the Agency for Healthcare Research and Quality (AHRQ) Discharge
Knowledge Assessment Tool. Secondary outcomes will be evaluated using subgroup analyses to
determine patient follow-up and medication adherence. Statistical analyses of both primary and
secondary outcomes will be performed with the Chi-Square test.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-332
Title: The Effects of a Leadership Development Workshop on First-Year Pharm.D. Student
Involvement in Student Organizations at the University of Michigan College of Pharmacy
Primary Author: Mandi Tsoi, University of Michigan College of Pharmacy, Michigan;
Email: matsoi@umich.edu
Additional Author(s):
Valerie Wersching
Nancy Mason
Purpose: In the next 5-10 years, it is predicted that there will be a shortage of pharmacy leaders
in the field. For this reason, it is important to encourage and develop leadership skills in
pharmacy school curricula as this may help foster future leaders in the pharmacy profession. A
before and after study was conducted to determine the extent of association between giving a
leadership development workshop prior to the start of P1 year and active involvement in student
organizations in the P1 year.
Methods: Prior to a leadership development workshop given during the P1 orientation in August
2012, the incoming P1 class of 2016 was given a survey to assess personal attitudes on
leadership, and their own leadership qualities. After the survey, a one-hour leadership
development workshop was given to expose the these subjects to leadership opportunities offered
at both the College and University levels, and strategies to participate in leadership roles through
involvement in student organizations. At the end of the academic year in April, the same survey
was given to the class of 2016 with the addition of a questionnaire assessing each subjects
participation in student organizations. To compare this class with one that did not have the
leadership workshop, the same survey was given to the class of 2015 at the end of their P1 year.
Results: At the end of their respective P1 years, the class of 2016 (who had the leadership
workshop) was significantly more positive than the class of 2015 in their perceptions of: 1)
whether our College of Pharmacy provided enough opportunities for leadership development
(72% vs. 51% agreeing respectively, p=0.005) and 2) whether our College emphasizes the
importance of leadership (87% vs. 82% agreeing respectively, p=0.026). Additionally, the class
of 2016 was more active in student organizations, is taking on more leadership roles after P1
year, and had more informal leadership experiences during their P1 year compared to the class of
2015. In comparing the beginning of the P1 year to the end of the P1 year for the class of 2016,
significant changes were noted for their response to their ability to set long term goals which
decreased from 92% at the beginning of the academic year to 82% at the end of the academic
year (p=0.024). Also, a significant reduction was identified for their response to the statement
that a leader recognizes a need for change and does something about it (95% at the beginning of
the academic year vs. 91% at the end of the academic year [p=0.009]).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The class of 2016 is more actively involved in student organizations as a whole
compared to the class of 2015. They also felt that the College of Pharmacy provides more
opportunities and emphasizes the importance of leadership development. A possible contributing
factor to these findings includes the leadership development workshop that was given during
orientation for the class of 2016, which encouraged active involvement in student organizations
during pharmacy school.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-333
Title: Therapeutic anticoagulation with enoxaparin: should obese patients receive adjusted
weight-based dosing?
Primary Author: Caitlin Turnbull, University of Michigan College of Pharmacy, Michigan;
Email: catealex@umich.edu
Additional Author(s):
Elizabeth Messana
Purpose: Currently, there is conflicting evidence to guide the practice of dosing enoxaparin in
obese patients. It is recommended that therapeutic dosing be based on total body weight,
however many obese patients receive an initial dose below the recommended weight-based dose.
Additionally, obese patients that actually receive recommended weight-based doses have been
shown to have an increased incidence of bleeding as compared to those who receive lower doses.
The primary purpose of this study was to evaluate weight-based dosing requirements in obese vs.
non-obese patients necessary to achieve therapeutic anti-Xa levels.
Methods: The institutional review board approved this single-center, retrospective cohort study.
Patients were enrolled if they were over the age of 18, received treatment with enoxaparin
between January 1, 2006 and May 31, 2011 and had at least one accompanying anti-Xa level
drawn. Pregnant patients and those with a creatinine clearance of less than 30 were excluded.
Demographic information including height, weight, age, and gender was collected, along with
serum creatinine, all enoxaparin doses administered, and associated anti-Xa levels. Patients were
stratified into two cohorts: obese (body mass index greater than or equal to 30) and non-obese
(body mass index less than 30). Dosing requirements in patients with therapeutic anti-Xa levels,
along with mean doses by weight in patients with sub- and supratherapeutic anti-Xa levels, were
compared between cohorts.
Results: There were 124 patients included in this study: 83 obese patients and 41 non-obese
patients. Demographics between the two cohorts were similar and only anti-Xa levels that were
drawn at appropriate times were evaluated. In patients with therapeutic anti-Xa levels, the mean
enoxaparin dose by weight was significantly lower in obese vs. non-obese patients (0.91 mg/kg
vs. 1.16 mg/kg, p < 0.001). However, mean anti-Xa levels in these groups were not statistically
different (obese: 0.699 IU/mL vs. non-obese: 0.669 IU/mL, p = 0.30). For patients with
supratherapeutic anti-Xa levels, there was no statistically significant difference in mean dose by
weight between groups (obese: 0.98 mg/kg vs. non-obese: 1.03 mg/kg, p = 0.378). Additionally,
significantly more obese patients had at least one toxic anti-Xa level, drawn at any time,
compared with non-obese patients (35% vs. 20%, p = 0.032).
Conclusion: Obese patients with a body mass index greater than or equal to 30 may require
weight-based doses of enoxaparin that are less than 1 mg/kg to achieve therapeutic anti-Xa
levels.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-334
Title: Precision of First-Dose Transdermal Fentanyl Prescribing in an Academic Medical Center
Primary Author: Katherine Veltman, University of Michigan, Michigan;
Email: kveltman@umich.edu
Additional Author(s):
John Clark
Purpose: Transdermal fentanyl (TDF) is a unique medication allowing for constant pain relief
for chronic severe pain. Previous studies have shown that when a TDF prescription is incorrectly
prescribed, 8% of patients will be harmed and 0.3% of patients will die as a direct result of the
prescription. It is unclear whether UMHS prescribers are following FDA guidelines when
prescribing TDF. The primary objective of this study was to determine whether health care
providers are prescribing TDF in accordance to FDA-approved guidelines, including adhering to
absolute contraindications and using the dosing guidelines for first-dose prescribing.
Methods: In a retrospective, single center, descriptive study, charts of patients prescribed TDF
between 2010 and 2011 were examined for accuracy in dosing and adherence to absolute
contraindications. Inclusion criteria included age of 18 or older, filling a TDF prescription
between 2010 and 2011 at the Health System Outpatient Pharmacies, and first dose prescribing
by health system physicians. Exclusion criteria included incomplete information on previous
analgesia. Patients were considered to be appropriate candidates for TDF if they had chronic
non-surgical pain, were on opioids for at least one week prior to initiation of TDF, and were not
issued TDF for use on an as-needed basis.
Results: 200 patients were reviewed and 106 were included in the study. Of these 106 patients,
69.8% had at least one prescribing discrepancy occur. The most common discrepancy was
incorrect dosing at 53.8%, with 24.5% of all patients overdosed and 29.3% of all patients
underdosed. Of the overdosed patients, 17.9% were not indicated for any dose of TDF based on
previous opioid usage. A total of 34 prescriptions were prescribed to patients with
contraindications for use. Breakthrough pain medication was not prescribed for 16% of patients.
Conclusion: Based on these findings, the majority of TDF prescriptions written at this health
system are either dosed incorrectly or prescribed to patients not appropriate for TDF use. This
indicates that patients are being placed at risk for harmful outcomes, including death. An
intervention to encourage appropriate prescribing will be needed to help prevent adverse
outcomes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-335
Title: Incidence of nephrotoxicity in adult patients treated with nafcillin for methicillin
susceptible staphylococcus aureus (MSSA) infections or empiric treatment of severe cellulitis.
Primary Author: Mark Wagner, Ferris State University, Michigan;
Email: wagnerm3@ferris.edu
Additional Author(s):
Michael Tiberg
Purpose: Antistaphylococcal penicillins like nafcillin are highly bactericidal for treating patients
with MSSA infections. It has equivalent efficacy to methicillin, and many clinicians believe
nafcillin has little or no risk of nephrotoxicity. Current literature contains limited records on the
incidence of nephrotoxicity with nafcillin, citing primarily case reports. The purpose of this
study is to determine the incidence of nephrotoxicity resulting from the administration of
nafcillin.
Methods: This is a retrospective observational study monitoring patients from September 2010
through September 2013. It will be submitted to the Institutional Review Board for approval. All
adult patients who received nafcillin for the treatment of MSSA will be reviewed for signs or
symptoms of nephrotoxicity. Exclusion criteria include patients who were administered nafcillin
for surgical prophylaxis, treated for less than 72 hours, or discharged to a facility not associated
with our own. Data will be collected through electronic medical records. Demographic data
collected will included age, gender, serum creatinine and blood urea nitrogen before and after the
initiation of nafcillin, nafcillin dose, fever greater than 38 degrees Celsius, maculopapular rash,
eosinophil levels greater than 0.6 mg/dL, hematuria, proteinuria, leukocyturia, nephrotoxic
medications, and any comorbid renal conditions including diabetes, heart failure, hypertension,
nephrolithiasis, and kidney disease. RIFLE criteria will be analyzed. Nephrotoxicity will be
defined as a significant change in renal function, classified as a serum creatinine increase of 0.3
mg/dL or greater, currently defined by the 2012 Kidney Disease Improving Global Outcomes
guidelines as stage one acute kidney injury. The combined data will be analyzed to determine the
most likely cause of nephrotoxicity.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-336
Title: Barcode verification by certified pharmacy technicians as an alternative to pharmacists
visual checks during dispensing
Primary Author: Bryan Wang, University of Michigan College of Pharmacy, Michigan;
Email: bclwaw@gmail.com
Additional Author(s):
James Stevenson
Phillip Brummond
Purpose: Barcode verification has been well documented as an effective tool in enhancing the
safety and efficiency of the medication dispensing process. The purpose of this study is to
establish the safety of barcode verification in place of the current practice of a pharmacist visual
check in the final stage of the medication dispensing process.
Methods: This study was deemed exempt from review by the institutional review board (IRB)
because it does not fit the definition of human subjects research requiring IRB approval. This
study will be performed at a large academic teaching hospital. A satellite pharmacy within the
health care system will be chosen as the site of the study. We will measure: 1) medication
dispensing errors made by pharmacists that are detected by barcode verification; 2) medication
dispensing errors made by barcode verification that are detected by the pharmacist; 3) the total
number of medications processed during each measurement period (to calculate error rates). The
medications involved in this study will be restricted to unit dose products. We will compare the
error proportions between the current system and the barcode system using an unpooled, singletailed, z test with a p value of &#8804; 0.05 as significant. The data will be analyzed using
appropriate statistical software to determine if technician operated barcode scanning is superior
or equivalent in safety to the pharmacist visual check.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-338
Title: Valproic acid and metabolic syndrome in institutionalized mental health patients on
antipsychotics
Primary Author: Silu Zuo, University of Michigan College of Pharmacy, Pharm.D Student,
University of Michigan College of Pharmacy;
Email: szuo@umich.edu
Additional Author(s):
Brant E Fries
Kristina L Szafara
Randolph E Regal
Purpose: Valproic acid is one of the most commonly used antiepileptic medications worldwide,
and is also a key mood stabilizer used in bipolar disorder and dementia. This study assesses
whether or not valproic acid potentiates metabolic side effects in patients with psychiatric
disorders on concomitant antipsychotics. Valproic acid alone has been shown to cause weight
gain, dyslipidemia, hypertension, and diabetes. Patients with psychiatric disorders, especially
those on 2nd generation (atypical) antipsychotics, already are at increased risk of these metabolic
effects. A secondary purpose is to determine if a dose-response relationship with between
valproic acid and metabolic side effects exists.
Methods: This is a cross-sectional study conducted using data collected on all patients in the
four state-operated psychiatric hospitals in Michigan using a comprehensive assessment
instrument, the interRAI Mental Health. Data were collected about patients baseline
characteristics such as gender, age, race, current medications, and disease states. The broad
assessment included both physical and cognitive measures as well as complete drug profile for
748 patients. The data were coded and entered into a confidential database at the University of
Michigan Department of Gerontology, with patients appropriately de-identified. All patients who
took both valproic acid and antipsychotics (N=200) will be compared to a control group of
patients who took antipsychotics without valproic acid (N=426). Patients will be compared on
the presence of the following indicators of metabolic syndrome: weight gain, high BMI (BMI >
30), very high BMI (BMI > 40), diagnosed with any diabetes mellitus, prescribed statin
medication hyperlipidemia or dyslipidemia, hypertension, and the combination of any 3 factors:
weight gain, high BMI, statin prescribed, and hyper- or dyslipidemia. Analysis will also include
assessment of the effect of valproic acid daily dosage on metabolic effects by assessing quartiles
of daily doses.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-339
Title: Evaluation of adherence to fingolimod monitoring recommendations: A retrospective
review
Primary Author: Ereny Bassily Atia, College of Medicine and Haealth Sciences, UAE
University, Alain, Abudhabi, UAE.;
Email: erenybassilly@hotmail.com
Additional Author(s):
Nicole Gebran
Miklos Szolics
Medhat Elsaid
Purpose: Fingolimod is an oral medication approved for the treatment of relapsing multiple
sclerosis (MS). It is the first oral agent with a novel mechanism of action. Clinical assessments
including an ECG which is required before the first dose and after a 6-hour monitoring period,
risk of infections, pulmonary function tests, liver function test, blood pressure, and macular
examination are considered mandatory for therapy safety monitoring. The primary objective of
this review is to provide information regarding adherence to manufacturers recommended
monitoring with fingolimod. Secondary objectives include safety assessment of reported adverse
drug reactions. The intent is to achieve a favorable benefits/risks profile and gain a valuable
treatment option for relapsing MS.
Methods: A retrospective observational electronic medical chart review was performed.
Fingolimod therapy monitoring tests were retrospectively reviewed from May 2011 to August
2013. Case selection included all adult patients receiving fingolimod treatment for relapsingremitting multiple sclerosis, including both patients who initiated therapy at the site of the study
or other sites and then continued their treatment at the study site. Medical records were analyzed
to determine if there was full adherence to monitoring recommendations prior to treatment, post
initial dose and upon follow-up. The study was approved by the District Research Ethics
Committee; recommendations were shared with the hospitals Pharmacy and Therapeutics
committee.
Results: Eleven patients were reviewed with an age range of 22-40 years, 45 percent of whom
were males and 55 percent females. All patients who had initiated their treatment, at our center,
had their CBC, transaminase and bilirubin, VZV antibody titer and macular examinations
completed. In addition, all female patients were screened for pregnancy. All patients had their
baseline and 6-hour follow-up ECG performed. However, none of the patients had their baseline
pulmonary function tests done. It is worth noting that, 45 percent of patients had started their
treatment abroad; accordingly data regarding baseline tests was missing. As for follow-up
assessment, 100 percent of patients had done their CBC, transaminase and bilirubin tests and
their regular blood pressure monitoring while only 45 percent of patients had their
ophthalmological examination performed. Two adverse reactions were reported: elevated liver
enzymes and leukopenia.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Our results indicate an acceptable adherence to manufacturers monitoring
recommendations imposed on fingolimod therapy. This includes electrocardiogram monitoring
before treatment and continuously for 6 hours after the first dose, along with hourly blood
pressure and heart rate evaluations and examination of the ocular fundus at baseline and 3-4
months after initiation of treatment with fingolimod. Insufficient compliance with pulmonary
function test screening and follow-up monitoring was highlighted and discussed with the
neurology team for further improvement. A long-term safety and efficacy assessment of
fingolimod use in this patient population will follow.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-340
Title: Know Your Diabetes Risk. Pharmacy Students educating adults about their risk for prediabetes in a community pharmacy setting
Primary Author: Sheldon Chow, University of Alberta, Faculty of Pharmacy and
Pharmaceutical Sciences, Edmonton, Alberta;
Email: sheldon3@ualberta.ca
Additional Author(s):
Hoan Linh Banh
Andrew Cave
Nancy Letassy
Ken Cor
Purpose: The purpose of this study is to see if it is feasible to educate adults in a community
pharmacy about their risk of pre-diabetes/diabetes. We also want to determine the most common
risk factors for pre-diabetes/diabetes in adults who come to the pharmacy.
Methods: Fourth year pharmacy students (voluntary participation in the research project) on
their experiential rotations in community pharmacies will invite adults or older to participate in
the study. Once participants are identified, they will be given a letter of information to gain
consent. The student will ask the participant to complete the Canadian Diabetes Association risk
assessment questionnaire. Once completed, the pharmacy student will review the risk for
diabetes with the patient and steps to reduce their risk. Data will be collected and encrypted.
Study forms will be stored in a secure filing cabinet located in the University of Alberta, Faculty
of Pharmacy and Pharmaceutical Sciences.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-341
Title: Development and validation of severity criteria for drug-related problems in chronic
kidney disease patients
Primary Author: Patricia Quintana Barcena, Faculte de Pharmacie, Universite de Montreal;
Email: pg.quintana-barcena@umontreal.ca
Additional Author(s):
Anne Lord
Ghaya Jouini
Lyne Lalonde
Purpose: Chronic kidney disease (CKD) patients are reported to have a mean of 3.5 drug-related
problems (DRPs) per patient. However, the information about DRPs severity remains scarce.
The aim of this project is to develop and evaluate the psychometric properties of a set of criteria
for the evaluation of DRPs severity in CKD patients from a community pharmacy perspective.
Methods: A team of clinicians (n=4) and researchers (n=3) developed an initial list of criteria
based on the type of interventions required to manage DRPs in community pharmacy.
Thereafter, ten community pharmacists were consulted individually to complete and fully adapt
the criteria to community pharmacy practice. Finally, a group of community pharmacists (n=4),
hospital pharmacists (n=4), family physicians (n=2) and nephrologists (n=2) rated in parallel the
appropriateness of each criteria. Criteria with uncertain appropriateness were discussed and their
final status was defined by consensus.
Results: Three levels of severity (mild, moderate and severe) were defined and each level was
further categorized in two sub-levels. At each level, specific pharmaceutical interventions
required to manage DRPs were listed. These include patients education, information
transmission to health-care providers, writing of a pharmaceutical opinion, specific patients
monitoring and follow-up, and patients referral to their physician or to the emergency
department.
Conclusion: The criteria are the results of a collaborative work involving community
pharmacists as well as CKD experts. It is unique and specific to actual clinical practices in
community pharmacy. Their reliability, validity and responsiveness are currently under
evaluation. If satisfactory, these criteria will constitute a new tool for pharmacy practice
research.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-342
Title: Identifying potential drug interactions in chronic kidney disease patients
Primary Author: Alessandra Batista Marquito, Center of Interdisciplinary Studies, Research
and Nephrology Treatment (NIEPEN), Juiz de Fora, Brazil, Center Hiperdia Minas, Juiz de Fora,
Brazil.;
Email: alemarkito@yahoo.com.br
Additional Author(s):
Fernando Antonio Basile Colugnati
Rogerio Baumgratz de Paula
Marcus Gomes Bastos
Rodrigo Martins Abreu
Purpose: Individuals with chronic kidney disease (CKD) use different classes of drugs and
therefore constitute a risk group for drug related problems, including drug interactions (DI). The
purpose of this study was to evaluate the pharmacotherapeutic profile of individuals with CKD in
order to identify potential drug interactions.
Methods: Cross-sectional and observational study that evaluated prescriptions of 558 CKD
patients followed in CENTER HIPERDIA / NIEPEN / UFJF, between January 2011 and
December 2011. The analysis included individuals aged over 18 years on two or more drugs in
their last visit to the clinic. The interactive potential of the drugs was traced based on
MICROMEDEX database. Variables evaluated were sex, age, smoking, alcohol consumption,
number of medications, CKD stage, body mass index (BMI), underlying diseases and
comorbidities. A logistic regression analysis was applied to determine the factors associated with
the DI and the results are shown as odds ratios (OR). The research was approved by the Federal
University of Juiz de Fora Ethics Committee.
Results: Among 558 patients evaluated, there was a predominance of males (54.7%), seniors
(69.4%), overweight and obese individuals (66.7%) and CKD stage 3 (47.5%). Comorbidities
most prevalent were hypertension (68.5%) and diabetes mellitus (31.9%). Potential drug
interactions were diagnosed in 74.9% of these prescriptions. A total of 1364 MIs were observed,
with 229 (16.8%) of greater severity and 5 (0,4%) contraindicated. Interactions of moderate
severity or less were identified respectively in 1049 (76.9%) and 81 (5.9%) prescriptions. It was
observed that the probability of an DI increased 2.5 times for each additional drug (CI = 2.18 to
3.03). Obesity (p=0,001), diabetes (p=0.018), hypertension (p=0.013) as well as advanced stage
of CKD (p=0.003) were strongly associated with the occurrence of DI.
Conclusion: Drug combination in individuals with CKD, specially in advanced stages of the
disease, was related to high prevalence of potentially serious DI.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-343
Title: A Case Report on Decreased Prothrombin Time-International Normalized Ratio (PT-INR)
Associated with Concurrent Use of Artemisia asiatica 95% ethanol ext. tablet and Warfarin
Primary Author: Junglim Kim, School of Pharmacy, Daegu Catholic University, Daegu, South
Korea;
Email: haeuner@naver.com
Additional Author(s):
Yura Lee
Junghyun Bae
Jaebak Yoo
Bokyung Moon
Case Report: Warfarin is the most commonly used anticoagulant medication. In warfarin
therapy, close International Normalized Ratio (INR) monitoring is required due to its very
narrow therapeutic window. Close INR monitoring is also required during the initiation or
discontinuation of the medication which interaction with warfarin is unknown. The Artemisia
asiatica 95% ethanol ext. tablet prescribed for gastritis treatment is one of these medications,
unknown for its interactions with warfarin. Warfarin is an antagonist of vitamin K, and Artemisia
asiatica was reported to contain a large amount of vitamin K. We therefore suspect that there
might be a possibility of drug interaction between Artemisia asiatica ext. tablet and warfarin.
We report the case of a patient who showed changes in INR after co-administration of Artemisia
asiatica ext. tablet and warfarin. A 78-year-old female inpatient on warfarin therapy for Cerebral
infarction, due to embolism of the middle cerebral artery, appeared to become resistant to
warfarin after previously maintaining good control on 4mg daily in the range of INR 2.5~3. Her
INR did not rise above 2 even when her warfarin dose was increased to 8mg. That resistance
lasted for about a week, and the period overlapped with that of the administration of the
Artemisia asiatica ext. tablet. The Artemisia asiatica ext. tablet was suspected to be the cause of
this resistance, and two days after its discontinuation, the INR rose by 0.9. On the third day, INR
escalated by 0.23 even though the warfarin dose was decreased to 5mg. From three days before
initiation to four days after discontinuation of the Artemisia asiatica ext. tablet, no other
alteration of medications was made and there was no particular change in food as well. Drug
interactions between Artemisia asiatica ext. tablet and warfarin have not yet been proven. Aside
from vitamin K, there might be able to exist other factors. We report this case with expectation
that more research will be conducted.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-344
Title: First case reported of successful rapid desensitization procedure to the antibody-drugconjugate brentuximab vedotin in one patient with refractory hodgkin disease
Primary Author: Christopher Boin, Hospital center of Mulhouse, France;
Email: christopher.boin@ch-mulhouse.fr
Additional Author(s):
Marie Chemin
Dana Gerghus
Olivier Aujoulat
Mario Ojeda-Uribe
Purpose: Hypersensitivity reactions (HSRs) to antibody-drug conjugates (ADC) preclude further
administration in humans regardless the underlying mechanism involved. Rapid desensitization
(RD) is a process that involves gradually increasing the rate and the concentration of medication
administration over several hours. It may allows a safer re-administration of monoclonal
antibodies (MoAb) after HSRs. However this method has not been used extensively for ADC.
We report here our experience with the use of a RD protocol in one patient with Hodgkin
Disease (HD) who experienced a severe HSR to Brentuximab Vedotin (BV) and who had no
more treatment option.
Methods: In collaboration with Castells and al. we adapted their 12-step, 6 hour RD protocol
(Brennan J Allergy Clin Immunol 2009) to a 16-step protocol in order to re-administer BV to a
34-year-old patient with HD (stade IV-B) who presented a severe HSR during the second
administration of BV (dose 1.8 mg/kg). After oral pre-medication with cetirizine 10 mg, aspirin
500 mg, montelukast 10 mg and ranitidine 150 mg, 4 bags of BV (each one of 250mL in
0.9%NaCl) were administered intravenously (i.v.) in 16 consecutive steps; each step increasing
the rate of BV administration by 2 to 2.5 fold. Solution 1 was a 1000-fold dilution of the final
target concentration (step 1-4), solution 2 was a 100-fold dilution (step 5-8), solution 3 was a 10fold dilution (step 9-12), and concentration of solution 4 was calculated by subtracting the
cumulative dose of step 1 to 12 from the total target dose (step 13-16). Steps 1 to 15 each took 15
minutes and step 16 was prolonged to complete the target dose. Patient gave his informed
consent before the procedure.
Results: 9 RD procedures were performed to this patient over 6 months. Average duration of
each procedure was 7 hours. During the first RD procedure (RD1), 10 minutes after starting step
15, the patient presented a mild reaction (chills, tachycardia, reduction in O2aS). He responded
well to intravenous antihistamines and corticosteroids, but the infusion had to be stopped. During
RD2, the total target dose was reduced from 1.8mg/kg to 1mg/kg. Although the patient presented
another mild reaction at the beginning of the step 16 which prompted us to stop it, we could restarted RD2 at step 15 after administration of antihistamines and corticosteroids. For subsequent
RDs, the following protocol modifications were made: pre-medication with antihistamines and
corticosteroids was systematically added at step 13 and a new step was created between 15th and
16th steps. Thus the total number of steps we adopted for this RD procedure was 17. In addition,
the total target dose was increased progressively from 1.0 to 1.8 mg/kg (RD2 1.0 ; RD3 1.5 ;
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
RD4 1.8). The following courses were administered without any reaction. After RD4 and RD8,
anti-tumor response to BV was assessed. In both opportunities PET-SCAN was in favour of a
near complete response.
Conclusion: No unexpected toxicity occurred during this RD protocol. Despite BV is an ADC,
adverse reactions observed were mild and similar to those occurring with monoclonal antibodies.
In our opinion this protocol offers an efficacy alternative to patients requiring a treatment with
BV who have experienced clinically significant HSR to this ADC.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-345
Title: Proton Pump Inhibitors (PPIs) prescription in medicine wards : analysis of relevance and
economical impact
Primary Author: Elsa Montagutelli, Centre Hospitalier de Blois, France;
Email: elsa.monta@gmail.com
Additional Author(s):
Mathilde Emonet
Jean-Francois Husson
Farhad Kazemi
Corinne Harnois
Purpose: PPIs is the third most sold generic therapeutic class in 2011 in France. Their
prescription is a common practice at hospital. To evaluate the relevance of these prescriptions,
we determined the rate of unjustified long-course prescriptions, their potential consequences for
patients and the associated costs.
Methods: For a given day, we analyzed PPIs prescriptions from 3 medicine wards at hospital to
determine whether they were initial or continuing prescriptions, and if they were justified by
medical history or co-prescriptions. Computerized prescriptions were analyzed with the help of
patients records and prescribers opinion. A short bibliographic study and an interview with a
gastroenterologist enabled us to define PPIs right use conditions, potential consequences of their
misuse and expenses caused by unjustified long-course prescriptions.
Results: Of 100 patients, 33 (1/3) had a PPI prescription which was justified in only 60% of
cases: 36% (n=12) were justified by past medical history or context and 24% (n=8) by coprescriptions. 27% of prescriptions (n=9) were unjustified as the invoked reason was not
considered as valid. No reason was found for 12% of cases (n=4). The main consequence of
these unjustified prescriptions is a decreased absorption for drugs like acetylsalicylic acid or
levothyroxin, and consequently a risk of reduced efficacy. PPIs prescription outside the
recommended range of indications is justified in some specific situations such as association
with antiplatelets or anticoagulants with several risk factors. Among the 33 PPI prescriptions of
this study, 9 corresponded to none of the situations considered as acceptable. These unjustified
long-course prescriptions lead to increased health expenses by 113 to 130 per patient per year.
Conclusion: For a given day, 1/3 of patients have a long-course PPI prescription, which is not
justified in more than 1 case of 4. More than exposing patients to a risk of interactions, this
practice leads to an increase in health costs. As by prescribers are not fully aware of appropriate
use conditions, an information campaign would help minimizing the misuse of these drugs and
consequently improving patients global care.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-346
Title: Intravitreal methotrexate in the management of serpiginous choroiditis. A case report:
compounding and results.
Primary Author: Inmaculada Vallejo-Rodriguez, Hospitales universitarios de Granada,
Granada;
Email: ivr451@yahoo.es
Additional Author(s):
Sol P. Cortes
Jorge Hernandez-Magdalena
Salud Caparros-Romero
Elena Puerta-Garcia
Case Report: The serpiginous is a rare, bilateral, chronic and recurrent idiopathic inflammatory
disease affecting the inner choroid and retinal pigment epithelium. Subsequent destruction of the
retina leads to a permanent visual disability, especially when the disease involves the central
macula. The treatment is controversial. Different systemic drugs have been used, such as
prednisone, cyclosporine, azatioprine and cyclophosphamide. If the evolution is desfavourable,
biologic therapy with a TNF inhibitor is an alternative. Another option is the intravitreal (IVT)
use of methotrexate (MTX). We describe a pharmaceutical compounding for a patient with
serpiginous choroiditis refractory to oral immunosuppressive treatment, in whom the use of oral
corticosteroids was contraindicated. After subconjuntival administration of triamcinolone, no
improvement was noted, so she was prescribed IVT MTX off-label.
Firstly, the patient gave her informed consent because it was an indication not authorized in
Spain.
Work in a vertical unidirectional flow cabinet (VUFC).Take 0.4ml from a vial of MTX
containing 50mg/2 ml. Make up to 1ml with normal saline in a 1 mL syringe and wave (A). Take
0.4 ml from A, make up to 1 ml with normal saline in a 1 ml syringe and wave (B). Take 0.2 ml
from B in the 0.3 ml syringe, insert a sterile stopper and put into a sterile bag. Seal it
immediately, protect it from light and label it. Conservation conditions: 7 days protected from
light and refrigerated.
An IVT MTX injection of 400 mcg in 0.1 ml was administered in each eye at seven-day interval.
MTX injections were well tolerated and did not cause any discomfort, improved visual acuity
and reduced cystoid macular edema.
We conclude that IVT MTX injections may provide such an alternative local therapy, are easy to
prepare, have minimum side effects and are cheap.
The use of IVT MTX seems effective in the management of the serpiginous choroiditis.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-347
Title: Heterogeneity of EGFR status in metastatic lung adenocarcinoma
Primary Author: Cristina Perez Ramirez, Pharmacogenetics Unit. Pharmacy Service.
University Hospital Virgen de las Nieves, Granada.Spain;
Email: cristi2611@hotmail.com
Additional Author(s):
Marisa Canadas Garre
Eduardo Villar Alvarez
Adela Madrid Paredes
Miguel Angel Calleja Hernandez
Case Report: Mutations in the tyrosine kinase domain of the epidermal growth factor receptor
(EGFR) gene are highly correlated with response to EGFR tyrosine kinase inhibitor (TKI)
therapy. The possibility of tissue heterogeneity occurrence of EGFR mutation within tumour is
potentially an important consideration, as it might influence the results of mutation screening.
A case report is presented of a patient diagnosed with lung adenocarcinoma. Discordant status of
EGFR mutations in longitudinally-collected samples was observed, with the original biopsy and
citology tested as negative and a follow up cytology tested as positive.
A 65 years female with antecedents of smoking during 25 years (1.5 packs/day) and 7 years as
ex-smoker presented mild haemoptysis in April 2011. Positron emission tomography/computed
tomography (PET/TC) revealed a neoplastic mass in the upper lobe of the right lung (LRL), with
metastatic adenopathies in the lower lobe of right lung and mediastinum. Bronchial brushing and
biopsies were collected by Fiberoptic Bronchoscopy. EGFR testing (exon 19 deletions,
G719A/G719C/G719S mutations in exon 18 and L858R mutation in exon 21) was performed in
both biopsy and cytology, both resulting native EGFR.
With the diagnosis of stage IV Lung Adenocarcinoma and native EGFR, the patient was treated
with 4 cycles of Cisplatin (75 mg/m2/day) and Pemetrexed (500 mg/m2/day) each 21 days, with
tumour progression confirmed by PET/TC in Sep 2011.
Transbronchial Needle Aspiration of the upper LRL lesion revealed an EGFR mutation in exon
21 (L858R). Patient was then treated with Erlotinib 150 mg/day with clinical improvement until
Jan 2012, when X-ray evaluation showed tumour progression. The patient was then treated with
Afatinib as off-label use, with great clinical improvement. The patient resulted exitus after
respiratory failure on Oct 2012.
This case report shows the importance of good quality sampling and analysis of different foci to
avoid false negatives when testing EGFR for therapy selection in lung adenocarcinoma.
Discordant status of EGFR mutations can be observed in longitudinally-collected samples.
Therefore, it would be necessary to determine several different tumour and metastatic foci,
assuring a better knowledge of the tumour genetic profile and minimizing false negative results.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Patients with an initial native EGFR could be beneficiate with a TKI treatment instead of a
conventional chemotherapy if heterogeneity of the tumor is confirmed.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-348
Title: Contributing factors for adherence and non-adherence to treatment in a Puerto Rican IBD
population and the resultant gain-framed messages
Primary Author: Glorimar Rivera-Quinones, University of Puerto Rico-School of Pharmacy,
Puerto Rico;
Email: glorimar.rivera3@upr.edu
Additional Author(s):
Frances M Rodrguez-Cintron
Mayra L Vega-Gerena
Riviam J Perez-Rodriguez
Giselle Sanchez-Pabon
Purpose: Adherence to medications in patients with Inflammatory Bowel Disease (IBD) has
been studied in different countries. Several investigators have been interested in determining the
risk and predictive factors associated to medication adherence in these patients. However, none
such study has been conducted in the Puerto Rican population. The aim of this study is to
determine contributing factors for adherence and non-adherence to treatment in a Puerto Rican
IBD population. A secondary aim is to develop gain-framed messages for Puerto Rican patients
with IBD based on the factors identified.
Methods: The study proposed is a cohort investigation that consists of three parts: recruitment of
IBD patients, evaluation of adherence and administration of questionnaires to selected patients,
and data analysis. Selected patients who meet the inclusion criteria will receive an informative
sheet and will be evaluated by the Morisky Medication Adherence Scale 8 (MMAS-8) to
discriminate adherent patients from non-adherent patients. Subsequently, they will complete
another questionnaire to determine contributing factors for compliance and non-compliance with
the medication regimen. Gain-framed messages will be created to promote disease prevention
behaviors and medication adherence, and will be based on the contributing factors identified. All
data analysis will be anonymous and performed considering all the variables. A Pearsons chisquare and Mann-Whitney test will be performed for the categorical and ordinal variables,
respectively. A p-value equal or less than 0.05, will be considered statistically significant.
Results: The results for this research are pending.
Conclusion: The conclusion for this research is pending.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-349
Title: Variables associated with therapeutic success of chronic hepatitis B
Primary Author: Rodrigo Martins Abreu, Clinical Division, Hepatology Branch, Department of
Gastroenterology, University of Sao Paulo School of Medicine., Sao Paulo, Brazil.;
Email: rma@usp.br
Additional Author(s):
Eduardo Remor
Vanusa Barbosa Pinto
Flair Jose Carrilho
Suzane Kioko Ono
Purpose: Evidence shows that the treatment of chronic infection with hepatitis B virus (HBV)
can suppress viral load, which should be as low as possible. Among the factors directly linked to
therapeutic success is adherence to treatment. Although medication adherence is an important
variable, few studies are available regarding the use of nucleos(t)ide analogues in clinical
practice. It is very important to improve intervention strategies of health services and evaluate
them from understanding the factors associated with adherence. The purpose of this study was to
evaluate the presence of associations between variables that explain the chronic hepatitis B
treatment adherence.
Methods: It is a cross-sectional study conducted from December 2010 to August 2011. We
evaluated 183 patients with chronic hepatitis B treated with adefovir, entecavir, lamivudine and /
or tenofovir. We collected socio-demographic information, related to treatment and records
relating to the dispensing pharmacy. Adherence to treatment was assessed by the "Assessment of
adherence to antiviral therapy questionnaire for chronic hepatitis B patients" (CEAT-VHB),
adapted and validated for this group of patients. The research was approved by the Ethics
Committee and it was obtained for all subjects the informed consent. Statistical tests were used
to verify the presence of associations between treatment adherence (or not) with categorical
variables (chi-square) and quantitative (Mann-Whitney).
Results: The CEAT-VHB identified 56.8% (104) of patients on treatment adherence. Among the
socio-demographic factors, it was observed that patients in treatment adherence were older (p =
0.0035). Concerning the variables related to antiviral treatment, there is an association between
group adherence and patients' reports of difficulty in following treatment (p = 0.005). Of the 104
patients in adherence group, 13% reported difficulty in following treatment. On the other hand,
the 79 patients in non-adherence group, only 30% reported this difficulty, suggesting that the
patients do not recognize their difficulty, but this failure is revealed by CEAT-VHB. It was
verified that the problems related to drugs dispensation (lack of the antiviral and / or not
withdrawal of the same by the patient) do not showed association with the adherence and nonadherence groups (p > 0.05). The other variables did not differ between groups (p > 0.05).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: We can verify that treatment adherence was low, with age as an important variable
for the patient to remain in long-term adherence. According to preliminary results, we suggest
that it is important an ongoing program of health promotion and guidance on taking drugs to try
to increase adherence to treatment of chronic hepatitis B.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-350
Title: Attitude of Saudi population toward weight loss medication and herbals.
Primary Author: Hajar Alghamdi, King saud university, kingdom of saudi arabia;
Email: hajar.18@hotmail.com
Additional Author(s):
Ebtihal Alblowi
Lina Ali
Miad Alqahtani
Sheikah Al-Aujan
Purpose: To assess the attitude of Saudi population toward weight loss products.
Methods: An online survey was carried out using internet-based document collaboration system
(Google Docs) Data were collected from Jan to Feb 2013. The survey was shared using social
networks. The study population includes male and female aged between 18 -60 years. The survey
consisted of seven questions on demographic characteristics and 21 closed and open ended
questions
Results: 2998 participants responded to the survey, the majority 1946 (64.7%) were in the age
group 18-28 years and predominantly females 2384 (79.3%). 990 (33%) of the participants have
used either medications or herbal remedies for weight loss. (504) 50.9% have indicated that they
would advice other people to use it, 355 (35.9%) have said that they have reached the desired
weight and 257 (26%) had experienced side effects from the medications/herbal remedies. Only
234 (23.6%) of those who use Medications/herbal remedies for weight loss seek information
from pharmacist or physicians. Medications/herbal remedies use for weight loss was found to be
associated with female, age group (18-28), university level of education and obesity (P <0.001).
The most common herbal preparation used was Apple cider tablet 168(16.9%). Orlistat 159
(16%) was the most common medication used for weight loss. The most common side effect 158
(15.9%) experienced due to herbal remedies/medications use was weakness and lethargy.
Conclusion: To avoid the risk and harms associated with weight loss products the practice of
Saudi population toward weight loss products need to be improved.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-351
Title: Parenteral nutrition with or without a fish oil supplement: a meta-analysis.
Primary Author: Vera Kim, Seou National University, Seoul;
Email: vera_kim90@hotmail.com
Additional Author(s):
Wan Gyoon Shin
Purpose: Intravenous lipid emulsions enriched in fish oil containing n-3 polyunsaturated fatty
acids (PUFA) are widely used in nutritional supplements and industrial lipid solutions.
Alternative lipid emulsions utilize in combination have demonstrated potential benefits in terms
of reduced impacts on clinical endpoints, oxidative stress and differential effects on cellmediated immunity and inflammation. This study aimed to investigate the treatment benefits of
lipid emulsion enriched with and without fish oil in hospitalized adult patients by performing a
meta-analysis of randomized controlled trials.
Methods: Electronic databases including PubMed, Embase, Cochrane Central Register of
Controlled Trials were searched to find relevant randomized controlled trials from 1996 to July
2013. Search strategy included the use of validated filter for identifying RCTs, combined with
searching keywords. Additionally, we conducted a manual search of abstracts from
bibliographies of relevant articles. We included randomized controlled trials comparing the
clinical outcomes (mortality, infection rate, length of hospital stay, length of intensive care unit
stay and mechanical ventilator days) of parenteral nutrition supplemented with fish oil vs.
without fish oil in critical ill patients. After independent quality assessment and data extraction
by two reviewers, meta-analysis was conducted by Review Manager 5.2 software (Cochrane
Collaboration, Copenhagen, Denmark).
Results: A total of 39 RCTs, 35 fully published trials and 4 trials published in abstract form with
2015 patients identified. Meta-analysis demonstrated that a parenteral nutrition supplemented
with fish oil was significantly superior to lipid emulsions without fish oil when considering
infection rate (risk ratio=0.66, p=0.002), length of hospital stay (mean difference=-2.89,
p<0.0001) and length of intensive care unit stay (mean difference=-2.11, p<0.00001). While no
difference were found the 2 groups when considering the mortality (risk ratio=0.66, p=0.002),
and as for duration of mechanical ventilation days (mean difference=-3.08, p=0.0005).
Conclusion: Through these results, we conclude that parenteral nutrition supplemented with fish
oil in hospitalized patients decreases infection rate, hospital stay and intensive care unit, but still
has no effect on mortality and mechanical ventilation days.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-352
Title: Dose adjustment of dipeptidyl peptidase 4 inhibitors in patients with renal failure
Primary Author: Sejung Shin, Deokseong Women's University, Seoul Korea;
Email: honpel17@gmail.com
Additional Author(s):
Nayeoung Kim
Mijung Koo
Younjoo Jung
Purpose: Dipeptidyl peptidase 4 inhibitors(DPP4Is) are new compounds targeting incretin
hormone system and improve glucose control without hypoglycemia or weight gain. DPP4Is
predominantly have renal excretion, two thirds of each dose eliminated as unchanged form in the
urine. Therefore patients with reduced renal function require DPP4Is dose adjustment and kidney
function test periodically. This study assessed appropriate use of DPP4Is for controlling type 2
diabetes patients based on serum creatinine(SCr).
Methods: This study screened patients starting sitagliptin(n=223) or vildagliptin(n=217) in our
hospital using electronic medical records from January 2012 to June 2012 retrospectively. We
evaluated the initial dose of DPP4Is which was appropriate one based on SCr level. We checked
whether drug dose is appropriate on drug approval information of Ministry of Food and Drug
Safety and Micromedex (version 2.0).
Results: Thirty five patients(7.95 percent) of the 440 had no data about SCr before starting
DPP4Is. Among the 405 patients who measured SCr before administration, 14 patients(3.46
percent) received uncontrolled dose. Among them, 13 patients had moderate renal failure and 1
patients had severe renal failure.
Conclusion: Most of patients received appropriate dose based on renal function. We studied,
7.95 percent of patients did not take the kidney function test and 3.46 percent of them didn't
adjust drug dosage. That may cause adverse effects of these DPP4Is. Diabetes is a chronic
progressive disease with major complications including nephropathy. Therefore periodic kidney
function test and active interventions of health care providers are required.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-353
Title: Study on improving adverse drug reactions (ADR) monitoring system at medical center
Primary Author: Moonok Ahn, Kyung Hee University, Seoul, Korea;
Email: gertrudise@hanmail.net
Additional Author(s):
Youngsuk Cho
Mijung Koo
Younjoo Jung
Hyokeun Jeong
Purpose: Most of the patients at our hospital are aged and have multiple symptoms, which
makes them take various kinds of drugs at several different departments. Moreover, they tend to
visit other medical centers or clinics where they take several medications. Accordingly, ADR is
frequently observed and reported. However, a system for actual evaluating and properly
monitoring the ADR has not been established in our medical center. In this study, to complement
ADR monitoring system we performed the survey in our facilities.
Methods: We have conducted surveys to 103 patients who have been randomly selected among
those outpatients who visited our hospital for a month in September, 2012. This survey has been
performed on a face-to-face contact basis by our research team members using questionnaires
about experiences, management of ADR and patients needs for ADR monitoring system.
Results: Out of 103 patients, 57 patients (55percent) experienced ADR. Out of those 57 patients,
43 patients (75.4 percent) had been consulted with and treated by medical professionals (doctors,
pharmacists, or nurses). And 29 patients (50.9 percent) who had ADR repeatedly experienced
similar side-effects caused by the drugs. Out of those 29 patients, 19 patients (65.5 percent) had
been consulted with medical professionals about their ADR. But only 7 patients (12.3 percent) of
those 57 patients who experienced ADR have recognized the names of drugs that caused ADR.
In order to avoid these repeated occurrences of ADR, 47 patients (82.5 percent) out of 57 ADR
exposed have responded that ADR monitoring system is in need. Seventy three patients (70.9
percent) out of 103 patients answered that either hospitals or pharmacy departments should
systematically monitor ADR.
Conclusion: Through this research, we come to realize that ADR-related information at our
hospital has not properly accumulated and that, whenever ADR is found, the symptoms have
been individually treated by specialists in a case by case manner. We have reached a conclusion
that, in order to prevent the repeated occurrence of ADR, ADR monitoring system should be
activated under the electronic medical records (EMR) where all the medial staffs can share
records related to ADR. Issuing a Medication Safety Card can be a useful means of informing
any medical professionals of the ADR-related symptoms of target patients.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-354
Title: Inhibitory effects of astaxanthin, beta-cryptoxanthin, canthaxanthin, lutein, and zeaxanthin
on 5 UDP-glucuronosyltransferases (UGTs) enzyme activities in vitro
Primary Author: Yufen Zheng, College of Pharmacy, Seoul National University;
Email: cathy8521@hotmail.com
Additional Author(s):
WAN GYOON SHIN
SOO KYUNG BAE
Purpose: Consumption of nutrients including food, beverages, and dietary supplements may
alter the effects of drugs people take. Of these, astaxanthin, beta-cryptoxanthin, canthaxanthin,
lutein and zeaxanthin are the major beneficial xanthophylls for human health. In this study, we
examined the inhibitory effects of these five xanthophylls on various 5 UDPglucuronosyltransferases (UGTs) activities in human liver microsomes.
Methods: We chose estradiol (10 uM), trifluoperazine (40 uM), serotonin (4000 uM), propofol
(100 uM), and zidovudine (100 uM) as substrates of UGT1A1, UGT1A4, UGT1A6, UGT1A9,
and UGT2B7, respectively. Test compounds, human liver microsomes (HLMs) (0.25 mg/ml),
100 mM Tris-HCl buffer (pH 7.5), MgCl2 (5 mM), substrate, and alamethicin (25 ug/ml) were
pre-incubated on ice to allow alamethicin pore formation in vitro for 30 min. Incubations were
commenced with the addition of UDPGA (5 mM) and incubated at 37C. Three different
concentrations of estradiol (5, 10 and 20 uM) were used to study the kinetic inhibitory parameter
on UGT1A1. The respective metabolites of the five substrates and internal standards were
measured by LC-MS/MS system.
Results: beta-cryptoxanthin, canthaxanthin and zeaxanthin showed inhibitory effects on
UGT1A1 with IC50 values 23.68, 36.74 and 42.57 uM, respectively, IC50 of beta-cryptoxanthin
and lutein on UGT1A4 were 28.66 and 29.94 uM, respectively. The Ki of beta-cryptoxanthin on
UGT1A1 was 30.43 uM, which was much more than the highest concentration of betacryptoxanthin in human volunteers.
Conclusion: Based on these results, these five xanthophylls may not occur food-drug interaction
by 5 UGTs in vivo.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-355
Title: Long-term Adherence to Adjuvant Hormonal Therapy of Anastrozole in Breast Cancer
Patients
Primary Author: Damkyung Lee, Ewha Womans University, College of Pharmacy;
Email: dami089@nate.com
Additional Author(s):
SEONGYEON SEO
HYANGSOOK KIM
JOOYEON LEE
BYOUNGKOO LEE
Purpose: Adherence to long-term treatment of hormonal therapy is important to maintain the
effects of medication and reduce the risk of recurrence. The aim of this study was to assess the
rate of adherence to adjuvant hormonal therapy of anastrozole in breast cancer patients and
determine factors associated with adherence for a period of 5 years.
Methods: Electronic medical record and pharmacy records for the breast cancer patients with a
first-time prescription from January 2005 to December 2008 in Seoul National University
Hospital (SNUH) were retrospectively reviewed. Patients follow-up was until September 2013.
Male breast cancer patients or diagnosed as metastatic breast cancer before anastrozole therapy
were excluded. Adherence was defined as a medication possession ratio (MPR) of 80% and
MPR was calculated as the number of total prescription days divided by the fixed interval of 5
years (1825 days). If the patient was prescribed other hormonal therapy before anastrozole, fixed
interval was adjusted considering previous treatment duration. A gap of 180 days or more in
medication coverage was defined as a treatment discontinuation. Adherence rate was estimated
using a Kaplan-Meier analysis. A Cox proportional hazard analysis was used to identify clinical
variables affecting non-adherence. Variables with a p-value <0.05 were considered as
statistically significant. Independent variables used for evaluate the association with adherence
include age, marital status, level of education, BMI, side effect, treatment type, department of
prescription, prescription refill interval, time since surgery, type of surgery, tumor grade, tumor
stage, radiation, chemotherapy, bisphosphonate, calcium supplements, and painkiller. All
analyses were carried out using SPSS 21.
Results: Overall, 634 breast cancer patients with a first-time anastrozole prescription from
January 2005 to December 2008 were identified in the SNUH records. Among those patients, 3
patients were excluded because of male and 53 patients because of metastases before the first
anastrozole prescription. Therefore, 578 patients were included the final analysis. Of 578 study
population, 451 (78.02%) patients took anastrozole monotherapy and 124 (21.00%) patients
switched from tamoxifen. About one-third patients (n=178 of 578, 30.80%) were non-adherent
over the 5-year treatment period. Mean MPR was 78.87%. According to a Cox proportional
hazard analysis, relative factors were age greater than or equal to 50 (HR=0.405; 95% CI [0.2080.788]), 180 days refill interval rather than 90 days (HR=0.525; 95% CI [0.317-0.869]),
existence of side effects (HR=1.595; 95% CI [1.110-2.292]), and calcium supplements
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
(HR=0.440; 95% CI [0.304-0.637]). Most cases of side effects (n=244 of 285, 85.61%) were
musculoskeletal events such as arthralgia, arthritis, backache, bone pain, osteoporosis.
Conclusion: Non-adherence of anastrozole as a hormonal therapy for breast cancer patients is
high. This study showed that patients younger than 50 (p<0.008)) or patients who had 90 days
refill interval rather than 180 days (p<0.012) were more likely to discontinue their therapy before
the end of 5-year treatment. And side effects (p<0.012) was associated with decreased adherence
but concomitant calcium supplements at the same time (p<0.000) positively affect adherence. In
order to make improved outcome of hormonal therapy, further attentions are required.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-356
Title: Analysis of Drug-induced-hyponatremia in Elderly Patients who Conducted
Comprehensive Geriatric Assessment and Development of a Hyponatremia Risk Assessment
Tool
Primary Author: Soh-mee Park, Ewha Womans University, College of Pharmacy, Seoul, South
Korea;
Email: ssomi_vv@naver.com
Additional Author(s):
Kyung-suk Choi
Eun-sook Lee
Kwang-il Kim
Byung-koo Lee
Purpose: Hyponatremia, defined as serum sodium concentration less than 135mmol/L, is one of
the most frequently observed electrolyte disorders in clinical practice. Especially, diuretics and
selective serotonin reuptake inhibitors (SSRIs), which are commonly prescribed to the elderly
patients as the first line drugs of hypertension and major depressive disorder respectively, often
induce hyponatremia as an adverse drug reaction. The objective of this study is to analyze the
results of comprehensive geriatric assessment in patients with drug-induced-hyponatremia and to
develop a hyponatremia risk assessment tool for the elderly, which estimates probability of
hyponatremia.
Methods: The Institutional Review Board approved this retrospective observational study.
Among inpatients aged above 65 who were hospitalized at geriatric center and conducted
comprehensive geriatric assessment (CGA) from January 2007 to September 2013, patients with
blood sodium concentration less than 135mmol/L will be selected. Through electronic medical
records, we will review serum sodium concentration, sodium osmolarity, urine sodium
concentration, urine osmolarity, diagnosis, underlying disease, medication, and nursing records
to identify drug-induced-hyponatremia patients in accordance with the Naranjo Algorithm,
which will be the subject group of this study. In addition, patients with heart failure, chronic
renal disease, and liver cirrhosis will be excluded. To verify the clinical effects of hyponatremia
in the subject group, the results of CGA including evaluation of activities of daily living,
cognition, depression, mobility, risk of falls, nutrition, and delirium will be compared to those of
the control group with normal serum sodium concentration. Furthermore, we will analyze the
correlation of hyponatremia and risk factors selected based on a literature review, such as age,
gender, BMI, serum potassium concentration, renal function, operation within 3 months, and the
number of medications. Finally, with the statistically significant factors, we intend to propose a
hyponatremia risk assessment tool for elderly patients.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-357
Title: Is Prophylactic Corticosteroid Use in Docetaxel Therapy Safe?
Primary Author: Ka-eun Yoo, Ewha Womans University, College of Pharmacy;
Email: kaeun_y@naver.com
Additional Author(s):
Rae-young Kang
Hyang-sook Kim
Ju-yeon Lee
Byung-koo Lee
Purpose: Docetaxel is a highly effective anticancer agent in a variety of solid tumors, including
breast cancer, lung cancer and prostate cancer. The administration of docetaxel requires
dexamethasone to prevent hypersensitivity reactions and fluid retentions. However, although
there are concerns about the risk of several steroid-related side effects such as hyperglycemia and
infections caused by the high-dose of corticosteroids in clinical practice, limited studies
addressed the side effects associated with dexamethasone in docetaxel therapy. Therefore, the
objective of this study was to investigate the incidence of corticosteroid induced adverse
reactions during docetaxel therapy and to identify its possible risk factors.
Methods: This study was conducted through retrospective chart review and approved by local
Institutional Review Board. Cancer patients who received docetaxel only or docetaxel based
combination therapy from July, 2011 to June, 2012 at department of medical oncology in Seoul
National University Hospital were included. Patients demographic status, laboratory values, all
prescribed records of docetaxel and dexamethasone, ever treatment for cancer including prior or
concurrent radiotherapy, surgery within 1 month, chemotherapy regimen, clinical stage, cancer
site, and comorbidities were collected to identify steroid induced adverse effect and related risk
factors. As regard to adverse effect of steroids, hyperglycemia was defined as a random glucose
level >200mg/dL, more than twice. All documented episodes of infection required treatment with
antibiotics were regarded as infection episode. The severity of hyperglycemia and infections
were assessed based on Common Terminology Criteria for Adverse Events(ver 4.0). The
characteristics of the patients with or without hyperglycemia or infections were compared. The
predictors or risk factors of both adverse events were determined respectively using a
multivariable logistic regression analysis. A p-value<0.05 was considered significant and all
statistical tests were performed with SPSS for Windows (version 21).
Results: A total number of 632 patients were identified as receiving docetaxel treatment during
study period. Among these patients, 482 patients received 3-weekly docetaxel, 145 patients
weekly docetaxel, 5 patients altered regimen. All patients received dexamethasone for
prophylaxis. Eighty six patients(13.61%) experienced hyperglycemia. Among those patients, 63
patients(9.97%) had never treated with hypoglycemic agents before. Nevertheless, only 8
patients were documented as diagnosed newly steroid induced diabetes mellitus on medical
record and treated with hypoglycemic treatments. Weekly or cumulative steroid dose were not
significantly different between patients with and without hyperglycemia. The average time of
hyperglycemia-onset was approximately 50days after starting docetaxel treatment. Cumulative
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
corticosteroid dose until the onset of hyperglycemia was 116.63mg(median,
range:[32.57,337.76]). A multivariable logistic regression analysis showed that age, height and
weight were independent risk factors for hyperglycemia, whereas cumulative or weekly dosage
of steroid was not. A total of 255 cases of infection episode occurred in 187 patients(29.59%)
with 189 cases of grade 3 and 5 cases of death. Cumulative corticosteroid dose and treatment
duration were higher in patients with infection than those in patients without infection(246.15mg
vs 220.20mg p=0.021, 117.53days vs 105.76days p=0.021). Treatment duration and weekly
corticosteroid dosage were determined as independent risk factors for infection.
Conclusion: Overall, we discussed to determine the incidence and risk factors for adverse events
regarding corticosteroid use in docetaxel therapy. In this study, steroid dosage was not found as a
risk factor for developing hyperglycemia. However, long duration and high weekly dosage of
dexamethasone are shown as risk factors for infection. Also, further prospective randomized
controlled trials are needed to validate the effect of dosage for steroids on development of
adverse effect including hyperglycemia and infection in patients on docetaxel therapy.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-359
Title: Frequency of CES1 (rs8192935) gene polymorphism in oral anticoagulated patients
Primary Author: Enrique Jimenez Varo, Complejo Hospitalario de Granada. Pharmacogenetics
Unit., Spain;
Email: ejimenezvaro@gmail.com
Additional Author(s):
Marisa Canadas Garre
Antonia Moreno Casares
Nuria Martinez Casanova
Miguel Angel Calleja Hernndez
Purpose: Dabigatran is considered the alternative to coumarin derivates in preventing stroke and
systemic embolism in adult non-valvular atrial fibrillation patients. This new oral anticoagulant
is a prodrug, which is rapidly activated by carboxylesterases (CES1) into its active metabolite.
Two polymorphisms (rs2244613 and rs8192935) in the CES1 have been described in a
subanalysis of the RE-LY study. These polymorphisms are associated with peak and trough
concentrations of dabigatran, respectively. About 33% of Europeans are carriers of the variant,
the CES1 gene single nucleotide polymorphism (SNP) rs2244613; however, the population
frequency of rs8192935 SNP has not been described. Our aim was to describe the population
frequency of the rs8192935 SNP in anticoagulation South of Spain patients.
Methods: Genotypic distribution of CES1 rs8192935 was analyzed in 81 anticoagulated patients
with thromboembolic diseases treated with acenocoumarol, dabigatran and rivaroxaban treated at
Complejo Hospitalario de Granada. Genotyping was performed by direct sequencing.
Results: A total of 81 patients were genotyped, 55, 6% male (45/ 81). Atrial fibrillation was
presented in 65,43% of the patients (53/81), deep vein thrombosis in 9,87% (8/81), and the
remaining patients presented other thromboembolic diseases (20/81; 24,69%). Genotype
frequency obtained of CES1 rs8192935 was 49, 4% CC (40/81), 43, 2% CT (35/81) and 7, 4%
TT (6/81). Allele frequency was 70, 99% for C allele (115/162) and 29, 01% for T allele
(47/162). CES1 genotype was in Hardy-Weinberg equilibrium in this population..
Conclusion: Polymorphic allele (T) was presented in a ratio of 2:1.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-360
Title: Clinical efficacy of Ustekinumab in moderate-severe autoimmune inflammatory diseases
Primary Author: Maria Del Mar Maldonado Montoro, Complejo Hospitalario de Granada.
Pharmacogenetics Unit, Spain;
Email: marblue3@hotmail.com
Additional Author(s):
Marisa Canadas Garre
Elena Puerta Garcia
Miguel Angel Calleja Hernandez
Purpose: Ustekinumab is a fully human monoclonal antibody targeting the common p40 subunit
shared by interleukin (IL)-12 and IL-23. This pathway is common in some autoimmune diseases
as Psoriasis (Ps), Psoriatic arthritis (PsA) and disease Crohn (CD). Ustekinumab is approved for
Psoriasis by FDA and EULAR, but not for PsA and Crohn, despite clinical efficacy has been
demonstrated in several trials.Our aim was to evaluate the clinical efficacy of Ustekinumab in
moderate-severe Ps, PsA and CD in recently published clinical trials.
Methods: Literature review of clinical trials evaluating Ustekinumab clinical efficacy for
moderate-severe Ps, PsA and CD published in the last five years. The assessment of
effectiveness was determined considering the following endpoints: Psoriasis Area Severity Index
(PASI) 75, Number Needed to Treat (NNT), Physician's global assessment (PGA) and
Dermatology Life Quality Index (DLQI) in Ps; the American College of Rheumatology score
(ACR20) and PASI 75 in PsA; Crohn Disease Activity Index (CDAI) in CD.
Results: Eight clinical trials were evaluated, published from dates 2008 to 2013. Clinical
efficacy of Ustekinumab for Ps was evaluated in four studies (Phoenix1, Phoenix2, Accept,
Pearl), for PsA three studies were found (Summit1, Summit2, Gottlied) and for CD one study
(Sandborn). For Ps, 45mg or 90mg Ustekinumab subcutaneously administered during 12 weeks
demonstrated average clinical efficacy compared to placebo groups, according to PASI 75 values
66.4%-75.7%, (p<0.0001); NNT resulted 2/2 (45mg/90mg) for Phoenix1 and 2/1 (45mg/90mg)
for Phoenix2. Ustekinumab demonstrated higher efficacy than Etanercept, according to Accept
study (p<0.001; NNT 9/6). In Asian patients, clinical efficacy of Ustekinumab compared to
placebo was also found (PASI 75: 67.2%-5% (p<0.001); PGA: 70.5%-8.3%; DLQI: -11.0-0.0
(p<0.001)) according to Pearl study. For PsA, 45mg or 90mg Ustekinumab subcutaneously
administered during 12 or 24 weeks, response achieved was ACR20: 42%-49.5% (p<0.0001) and
PASI 75: 52%-62.4% (p<0.0001), according to Summit1, Summit2 and Gottlied trials. For CD,
90mg subcutaneous or 4.5mg/Kg intravenous administered during 4 weeks, resulted in CDAI:
52.9% and placebo 30.2% (p<0.02) in patients previously treated with conventional or biology
therapy. For Infliximab-non responder CD patients, CDAI values were 43% for subcutaneous
and 54% for intravenous administration.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Patients with moderate-severe Ps, PsA and CD treated with Ustekinumab achieved
clinical efficacy, significantly higher than anti TNF-alpha therapy. Although efficacy results
were less satisfactory for CD, Ustekinumab showed greater efficacy in patients who previously
failed to respond to Infliximab.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-361
Title: Use of herbal medicines during pregnancy: focus on adverse reactions and newborn
Primary Author: Kosar Raoufinejad, Department of Clinical Pharmacy, Faculty of Pharmacy,
Tehran University of Medical Sciences, Tehran, Iran., Tehran;
Email: kosaraoofi@yahoo.com
Additional Author(s):
Kheirollah Gholami
Mohammadreza Javadi
Hassan Torkamandi
Mehdi Rajabi
Purpose: Herbal medicines are becoming more popular among pregnant women despite the lack
of scientific-based evidences of their safety and efficacy during pregnancy. Several studies
worldwide have assessed the use of these kinds of medicines in pregnancy; however, only a few
studies have considered the adverse reactions of these drugs and their potential effects on the
newborns as well. This study aimed to explore the use of herbal medicines during pregnancy
among a group of women based on their socio-demographic characteristics, adverse reactions of
these drugs in mothers, and ultimately their possible effects on the neonates.
Methods: In this cross-sectional and retrospective study, 400 postpartum women, who provided
informed consent, and their singleton newborns were recruited during the first few days of
postnatal period at the hospital. Data were collected in the course of face-to-face interviews by a
pharmacist and completion of questionnaires including some parts: maternal socio-demographic
characteristics, medical history, pregnancy-related morbidities, herbal and conventional
medicines used during pregnancy, consulting health-system professionals about the herbals use,
and substance-abuse history. Questions were used to gather all the relevant data for up to one
month before pregnancy. Herbal drugs were defined based on WHO definitions. The causality
and severity of each reported adverse drug reaction of herbals were evaluated by WHO scale and
Hartwig scale, respectively. Each subject was interviewed individually and several particular
questions and checklists were arranged to help the mother to remember the required details.
Maternal hospital files and notes were verified to increase the accuracy of the obtained
information. Medical notes and reports of all newborns were also scrutinized for neonatal
characteristics and problems from birth to discharge.
Results: Of all 409 eligible women, 400 (97.8 percent) agreed to participate. At least one herbal
medicine was used by 325 (81.2 percent) interviewed subjects. The use of herbal drugs was
significantly (P less than 0.05) higher among the more-educated, employed, and primiparous
women. Mint, frankincense, flixweed, and olive oil were the most commonly used herbal
preparations. Majority of these administrations were based on information from nonprofessionals
(49.1 percent) or self-medication (29.6 percent), without consulting the health-system
professionals (74.2 percent). Vitamins and minerals, anti-infectives, and gastrointestinal drugs
were on the top of the list of conventional medicines. Nausea, vomiting, and heartburn were the
most reported adverse reactions of herbal drugs, all mild and mainly possible (77.0 percent).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Regarding the neonates, jaundice and respiratory distresses were the most prevalent problems
detected. Considering gestational age, birth weight, Apgar score, and neonatal complications,
there were no significant differences between the newborns of herbal-users and non-users of
herbal medicines.
Conclusion: This study indicates that taking herbal and conventional drugs is common among
pregnant women. Although not always safe, herbal products are mostly used according to
personal judgments without informing the health-care professionals, since they are often believed
as natural and safe. Pregnancy-care providers should be aware of the potential risks and benefits
of the commonly used herbal medicines by pregnant women, and ask them about the use of these
drugs as well as conventional drugs. In addition, safety and efficacy of herbal medicines and
their probable interactions with conventional medicines need to be investigated more in large
clinical trials.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-362
Title: Efficacy of two educational interventions on adverse drug reactions for practicing nurses:
a three-armed randomized controlled trial
Primary Author: Fahimeh Naderi, Research Center for Rational Use of Drugs, Tehran
University of Medical Sciences, NA;
Email: fahimeh.naderi90@gmail.com
Additional Author(s):
Naser Hadavand
Amir Sarayani
Mohammadreza Javadi
Molouk Hadjibabaie
Purpose: Spontaneous reporting of adverse drug reactions (ADR) has a main role in
pharmacovigilance systems. However, contribution of health care professionals to reporting
remains to be insufficient. In clinical settings, nurses are the most available professionals who
mainly administer medicines and monitor patients signs and symptoms. Nevertheless, their role
in spontaneous reporting of ADRs has not been well recognized in health systems. Lack of
training and limited knowledge about ADRs could be considered as a major barrier to their
contribution to reporting. In the present study, we compared two educational methods to improve
nurses knowledge about ADRs associated with the most frequently used medicines in a tertiary
cardiology hospital.
Methods: We designed a three-armed randomized controlled trial comparing one-day didactic
lecture, brain storming workshop and a delayed-intervention control group. The study was
conducted in Shaheed Rajayi Heart Center, Tehran, Iran in 2013. Clinical pharmacists prepared
and delivered the educational content. Prior to implementing the study protocol, two pilot
sessions were conducted to harmonize the educational content. Stratified random sampling was
used to randomize all the nurses working in the hospital (634 participants) in four groups (pilot
plus study groups). Outcomes of the study were assessed based on Moore et al 2009 framework
including participation, satisfaction and declarative/procedural knowledge. The main outcome
(knowledge) was evaluated using a validated questionnaire immediately before, immediately
after and three months after each session. Participants satisfaction was assessed only after each
meeting using a separate questionnaire. Data were collected from the control group at the
beginning of the trial and before attending their educational session which was conducted at the
end of the trial. Nurses who did not participate in any of the three data collection points and
those who did not attend the whole training session were excluded. Data were analyzed using
appropriate tests including t-test, Mann-Whitney, Chi-square, and ANOVA.
Results: There was no significant difference between three groups at baseline regarding
knowledge scores and demographic characteristics. Mean rates of participation was 37.7% for
the lecture-based sessions and 47.5% for the workshop-based sessions. The knowledge scores
significantly improved for both study groups immediately after the meetings (p values<0.001).
The scores were significantly higher for the lecture-based group after the meeting (p=0.01). At
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
the three-month follow-up, scores of both groups decreased significantly (p values<0.001) but
the magnitude of knowledge loss was significantly higher in the lecture-based group than the
workshop-based group (-13.015.9% vs. -5.715.1%, p=0.02). In comparison to the control group,
scores of the lecture-based and workshop-based groups improved significantly at follow-up (p
values<0.001). Interestingly, the knowledge scores significantly improved during the trial in the
control group. Regarding satisfaction, participants in the workshop-based intervention were
significantly more satisfied with the instructional design and opportunities for discussion (p
values<0.01).
Conclusion: An educational intervention by clinical pharmacists can improve nurses knowledge
about ADR. Short-term effects of a lecture-based intervention could be higher than a workshopbased intervention but the retention of knowledge could not be guaranteed. Future studies should
evaluate the effects of mixed-method and long-term educational interventions for practicing
nurse.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-363
Title: Randomized controlled pharmacist intervention study to reduce drug-related problems and
readmissions among old people with dementia
Primary Author: Maria Gustafsson, Umea University, Umea;
Email: maria.gustafsson@pharm.umu.se
Additional Author(s):
Bettina Pfister
Jeanette Jonsson
Hugo Lovheim
Purpose: Drug prescribing among old people is high and often inappropriate. The use of
inappropriate drugs has been associated with an increased risk of hospitalization - studies have
shown that up to 30% of hospital admissions are directly related to drug-related problems. Older
people are at increased risk for adverse drug reactions, and especially vulnerable are older people
with dementia. Positive effects has been shown when a pharmacist is added to a ward team, but
to our knowledge, no one has studied the effectiveness of pharmacist interventions in reducing
drug-related problems and readmissions among people with dementia.
Methods: This is a randomized controlled study where we are investigating if medication
reviews performed by a pharmacist as part of a ward team can reduce drug-related problems and
hospital readmissions among people 65 years or older with dementia. We also want to
investigate if costs associated with hospital visits can be reduced and nursing home placement
delayed. Four hundred and sixty patients will be recruited and randomized to control (usual care)
and intervention group (pharmacist involved). The study is being performed at internal medicine
and orthopaedic wards at two hospitals in northern Sweden, Umea University Hospital and
Skelleftea Hospital. Data about the number of readmissions and visits to the emergency room
will be collected during the six-month follow-up. Frequency of drug-related readmissions is the
primary endpoint of the study. Whether or not a readmission is drug-related will be judged by a
group of experts, consisting of pharmacists and physicians specialised in clinical pharmacology
and internal medicine; these are blinded. The study is approved by the Regional Ethical Review
Board in Umea (2011-148-31M), registered at Clinicaltrial.gov (NCT01504672) and will adhere
to the CONSORT criteria for clinical trials.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-364
Title: Evaluation of vancomycin-resistant enterococcal urine isolates at a tertiary medical center
Primary Author: Marla Koch, South Carolina College of Pharmacy, SC;
Email: kochm@email.sc.edu
Additional Author(s):
Celeste R. Caulder
Nicole Smith
P. Brandon Bookstaver
Purpose: The increase in incidence of vancomycin-resistant enterococcus (VRE) has led to
prescribing newer, costly therapies including daptomycin and linezolid. The purpose of this
study is to report antimicrobial regimens utilized in microbiologic confirmed VRE UTis,
evaluate antimicrobial susceptibilities and examine patient-related outcomes.
Methods: All non-pregnant, adult subjects with a confirmed VRE UTI were screened for study
inclusion from January 2006 through December 2011. Beginning in late 2010, susceptibility
testing of all VRE isolates was performed via E-test for fosfomycin, daptomycin, and
doxycycline. Additional susceptibility data were obtained through automated reporting with
Vitek II system. Subject data, collected retrospectively using the electronic medical record,
included patient, urinalysis, microbiology, and treatment characteristics. The primary objective
was to describe antimicrobial therapy for VRE UTis and determine susceptibility profiles of
routinely screened agents. Secondary endpoints include the percent of treatment failures and
antibiotic-related c;osts.
Results: A total of 215 encounters were included during the 6 year study period. The average
subject age was 58 years and 30.2% were male. Approximately 37% of patients presented with
community acquired infection and 27% presented febrile. Polymicrobial isolates were observed
in 31.6% of cases. More than half of patients (50.7%) received active antimicrobial therapy as
follows: daptomycin (n=S4), linezolid (n=44), doxycycline (n=7). The mean length of treatment
was 8.72 days and the median was 7 days for the primary antibiotic. There was no difference in
treatment duration among agents and only 11cases prompted a therapy change. Microbiology
susceptibilities for fosfomycin (n= 73), daptomycin (n=73) and doxycycline (n=73) resulted in
MIC90 of 128, 4, and 24 respectively.
Conclusion: Use of daptomycin and linezolid for VRE urine cultures was high at our institution
prompting a targeted stewardship initiative. Fosfomycin may represent a reasonable alternative
for treatment.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-365
Title: A medication use evaluation of acetylcysteine and determination of the potential for cost
savings associated with intravenous to enteral conversion.
Primary Author: Rebecca Van Vleck, University of New Mexcio College of Pharmacy, New
Mexcio;
Email: RVanVleck@salud.unm.edu
Additional Author(s):
Richard D'Angio
Preeyaporn Sarangarm
Purpose: Acetylcysteine is available in a variety of dosage forms including intravenous, enteral,
and nebulized solutions. Common uses for intravenous and enteral acetylcysteine are for the
treatment of known and unknown acetaminophen overdoses and for the prevention of contrastinduced nephropathy (CIN). For the treatment of acetaminophen overdoses, the intravenous and
enteral formulations are associated with similar clinical outcomes. Administration of the drug
enterally may also be safer than intravenous administration as it avoids the potential for infusionrelated side effects. The purposes of this study were to: 1) describe the use of intravenous and
enteral acetylcysteine at a University Medical Center, 2) evaluate if patients who received the
drug intravenously could have received the drug enterally and 3) determine the potential cost
savings for intravenous to enteral conversion in eligible patients.
Methods: Patients admitted to the University of New Mexico Hospital (UNMH) in 2012 and
received intravenous or enteral acetylcysteine were included in our study. Patients were excluded
if they received acetylcysteine by a route other than intravenous or enteral, or if they were treated
in an outpatient clinic. Patients were evaluated for acetylcysteine indications and the total
amount received. Patients that received the drug intravenously were considered eligible for the
enteral formulation if they met our hospitals guidelines for intravenous to enteral conversion.
Potential cost savings were estimated using the difference in average acquisition costs for
intravenous and enteral formulations multiplied by the number of milligrams of intravenous
acetylcysteine eligible for conversion.
Results: During the 1-year study period, 167 patients received intravenous or enteral
formulations of acetylcysteine. The indications for acetylcysteine included: prevention of CIN in
86 patients, treatment of acetaminophen overdose in 52 patients, treatment of polysubstance
exposure in 22 patients and treatment of non-acetaminophen related acute liver injury in 7
patients. Fifty-nine patients received acetylcysteine via the enteral route, 107 patients received
the intravenous formulation, and 3 patients received acetylcysteine via both routes. Seventy-two
of the 107 patients who received the intravenous formulation met our criteria for enteral
administration, representing a potential for $11,107 in cost savings.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The most common uses for acetylcysteine in our study were for the prevention of
CIN, the treatment of known acetaminophen overdose, and the treatment of polysubstance
exposure. The most common route of was intravenous and this was used exclusively in sixtyfour percent of the patients. Approximately two-thirds of the patients who received the
intravenous form of acetylcysteine met our hospitals criteria for intravenous to enteral
conversion. Administering acetylcysteine via the enteral route in eligible patients has the
potential to result in substantial cost-savings.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-366
Title: Volume expansion with six percent hydroxyethyl starch 130/0.4 versus standard volume
expanders following cardiac surgery
Primary Author: Delaram Bahmandar, Roseman University of Health Sciences, Nevada;
Email: dbahmandar@student.roseman.edu
Additional Author(s):
Kathryn Permoda
Ragini Bhakta
Purpose: Voluven (6% hydroxyethyl starch 130/0.4) is an intravenous plasma volume expander
approved for the treatment and prophylaxis of hypovolemia in adults and children. Compared to
alternative hydroxyethyl starch solutions, data suggest that Voluven may result in less
coagulopathy and renal dysfunction due to its low molecular weight and degree of substitution.
Compared to alternative volume expanders, however, Voluven may lead to increased bleeding
risk and need for transfusion. The objective of this study is to determine if Voluven is associated
with increased risk for coagulopathy and renal dysfunction in patients undergoing cardiac
surgery compared to those receiving alternative volume expanders.
Methods: This is a single-center, retrospective, observational study enrolling adult inpatients
undergoing cardiac surgery at St. Rose Dominican Hospitals Siena Campus. A list of adult
cardiac surgery patients admitted between May 2013 through December 2013 will be obtained,
with data retrospectively collected through computerized patient charts. Data collection for each
patient will include demographics, pre-operative laboratory values, peri-operative laboratory
values, post-operative laboratory values (0-48 hours after surgery), amount of Voluven received,
amount of chest-tube drainage, Voluven used during surgery, transfusion requirements,
alternative fluids received during surgery and pre- and post-operative vitals (0-48 hours after
surgery). Outcomes to be assessed include change in renal function from baseline, as well as
need for transfusion between each cohort.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-367
Title: Pharmacy placement on a medical mission in Ghana, a student's perspective
Primary Author: Rhea Conlu, Roseman University of Health Sciences, Nevada;
Email: rconlu@student.roseman.edu
Additional Author(s):
Inessa Miretsky
Alexander Gilmer
Nightingale Meyou
Christina M. Madison
Purpose: Each year over 6,000 groups of 10-100 individuals travel worldwide for medical
missions. Work the World, a program based out of the United Kingdom (UK) hosts medical,
nursing, pharmacy, dental, physical therapy, and radiography students and professionals in the
following countries: Asia, Africa, and South America. This project was designed to outline the
importance and benefits of medical missions for allied health students and professionals, as well
as to summarize challenges faced and how to overcome them both prior to and during the
medical mission.
Methods: Prior to embarking on a medical mission abroad, it is advisable to set out personal
goals for the trip. In addition, travelers should receive the necessary vaccinations and
prophylactic medications specific to the destination region. Learning a few phrases in the native
language is a great way to help communicate with patients as well as to earn their respect. Above
all, it is important to always keep an open mind while in the host country. Students in the UK are
strongly encouraged to complete an elective placement abroad. This is a practice that students in
the United States (US) would benefit from as well. It is a way to gain a unique perspective on
healthcare abroad and appreciation for healthcare in the US.
Results: The healthcare system in Ghana faces several key challenges, including lack of
resources such as diagnostic testing and limited medication options. In the community setting,
the pharmacist takes on a provider role, becoming responsible for providing not only the proper
medication but at times making a correct diagnosis as well. With pharmacists in the States
currently seeking provider status, this aspect was especially interesting and exciting. Student
pharmacists on placement are able to work in the hospital dispensary, observe consultations and
help counsel patients in the HIV clinic, attend and contribute to general medicine ward rounds,
participate in out-patient diabetes and hypertension clinics, as well as do community outreach
events.
Conclusion: International medical missions impart student pharmacists and other health
professionals with the translatable ability of improved cultural competency as it relates to an
increasingly diverse patient population. Participation in a medical mission is an opportunity for
healthcare professionals and student pharmacists to bridge this gap in a way that can then be
applied in their own clinical practice.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-368
Title: Retrospective study comparing linezolid and daptomycin for the treatment of Vancomycin
Resistant Enterococcus urinary tract infections
Primary Author: Alexander Gilmer, Roseman University of Health Sciences, Nevada;
Email: agilmer@student.roseman.edu
Additional Author(s):
Bhavin Patel
Diane Rhee
Purpose: Vancomycin-resistant Enterococcus (VRE) is one of the main group of organisms
responsible for causing urinary tract infections (UTIs) in the hospital setting. Currently, linezolid
is approved to treat VRE infections, but it has not been clinically studied in the treatment of UTI
due to VRE. However, its pharmacokinetics indicate it would be a viable option for to treat VRE
UTIs. The objective of this study is to compare the treatment of VRE UTIs using linezolid versus
daptomycin.
Methods: This retrospective, observational study will be approved by the Institutional Review
Board at Roseman University of Health Sciences. Laboratory records obtained on patients
admitted to Desert Springs Hospital from January 2009 through December 2012 will be used to
identify patients with a positive urinalysis and urine culture growing Enterococcus sp. Patients
will be included if they were 18 years or older at the time of infection, were treated with
linezolid or daptomycin for equal to or greater than 48 hours. Patients will be excluded from the
study if they were pregnant, had a concurrent infection, had a concurrent growth of bacteria in
their urine culture greater than the amount of Enterococcus sp. grown , were treated with
antibiotics other than daptomycin or linezolid or treated for less than 48 hours. The primary
outcome measure will be clinical cure, as defined by white blood cell (WBC) count less than
10,000 WBC, temperature less than 37 degrees Celsius, and, if collected, a negative follow-up
urinalysis and/or urine culture. The secondary outcome will be time to clinical cure.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-369
Title: Medication use evaluation of rivaroxaban for stroke prevention in patients with atrial
fibrillation at a community hospital
Primary Author: Inessa Miretsky, Roseman University of Health Sciences, Nevada;
Email: imiretsky@student.roseman.edu
Additional Author(s):
Zalak Shah
Ragini Bhakta
Purpose: Rivaroxaban is a relatively new oral anticoagulant which has been FDA approved for
use in primary and secondary stroke prevention in patients with non-valvular atrial fibrillation
with a CHADS2 score of 1 or higher. A medication-use-evaluation (MUE) was conducted in
order to determine whether rivaroxaban was being used appropriately and at the correct dose by
cardiologists at a community hospital, as well as to determine its relative safety profile with
respect to bleeding risk.
Methods: The institutional review board approved this non-interventional retrospective analysis
of data; informed consent was not required. A list of patients who received rivaroxaban from
February 2012 through July 2013 was generated by the pharmacy computer system and all study
information was obtained from patients electronic records. Men and women who received a daily
rivaroxaban dose of 20 mg or 15 mg were included in this study; those who were on rivaroxaban
prior to hospital admission as well as patients undergoing a planned cardioversion were excluded
from analysis. The primary objective measure was appropriate indication for rivaroxaban use.
Additional data points included proper dose adjustment from 20 mg daily to 15 mg daily for
impaired renal function and safety profile of the drug with respect to bleeding risk.
Results: Data was collected for a total of 85 patients, fourteen of which had been taking
rivaroxaban prior to hospital admission and were excluded from final analysis. Rivaroxaban was
used for the appropriate indication in 61 patients (71.8%). It was properly dose adjusted
according to impaired renal function in 77 patients (90.6%); 8 patients (9.4%) had a drop in
hemoglobin of 2 or more units but without any other bleeding associated adverse effects, and
only 1 patient (1.2%) experienced major bleeding, which was defined as fatal bleeding or
bleeding in a critical organ. Of the patients in whom rivaroxaban was used inappropriately, 6 had
atrial fibrillation but with a CHADS2 score of 0, 8 had venous thromboembolism (VTE), 3 had
atrial flutter, 1 had ventricular fibrillation, 1 had valvular disease, and 5 had no atrial fibrillation
with indication for anticoagulation being unclear.
Conclusion: Use of rivaroxaban by cardiologists in this community hospital was appropriate in
the majority of cases and did not appear to be associated with an increased risk of bleedingrelated adverse outcomes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-370
Title: Exploring the association between diabetes and tuberculosis: impact on culture conversion
and requirements of drug therapeutic monitoring
Primary Author: Chandni Patel, Roseman University of Health Sciences, Nevada;
Email: cpatel@student.roseman.edu
Additional Author(s):
Nisha G Patel
Rhea Conlu
Christina Madison
Purpose: Diabetics are at a 30% higher risk for developing tuberculosis in their life time than
non-diabetics because this disease state causes them to be immunocompromised. Patients who
are indicated for therapeutic drug monitoring include those who have not shown clinical
improvement for at least two months of therapy based on appropriate weight-based dosing.
Diabetics have delayed/impaired medication absorption from inadequate glucose control
therefore they take longer to culture convert/culture negativity. This study aims to evaluate
patients with tuberculosis and diabetes on time to culture negativity or culture conversion in
addition to assessing the need to conduct therapeutic drug monitoring.
Methods: This study has been submitted and approved by the Roseman University of Health
Sciences Institutional Review Board. In this retrospective study electronic medical records are
being accessed via WebTB, an electronic medical record maintained by the Southern Nevada
Health District. Patient records will be reviewed and those with the diagnosis of both
tuberculosis and diabetes will be identified. The primary endpoint is to evaluate diabetics with
tuberculosis on time to culture negativity and the secondary endpoint is to assess the need to
conduct therapeutic drug monitoring. A data collection form will be utilized to extract the needed
information to address both the primary and secondary endpoints.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-371
Title: Legal dilemmas in dispensing: use of beta-lactams in patients with penicillin allergies
Primary Author: Nyssa Stant, Roseman University, Nevada;
Email: nstant@student.roseman.edu
Additional Author(s):
Jeani M. Pulsipher
Mark R. Neufeld
Bronsen K. Kawewehi
Meghan N. Jeffres
Purpose: Approximately 250 million antibiotics were prescribed in the US in 2010; over 40
percent were beta-lactams. Penicillin allergies occur in 10 percent of Americans. These statistics
result in large numbers of beta-lactam antibiotics prescribed to patients with a penicillin allergy.
Pharmacists must weigh the risk of allergic reaction with the risk of recommending a potentially
inferior alternative. The purpose of this project is to review court cases and identify legal
precedent of using beta-lactams in a patient with a penicillin allergy. The goal is to educate
practicing pharmacists so they are able to make more informed decisions.
Methods: Search terms included penicillin allergy and penicillin allergic reaction. All federal
and state court cases were searched in Google Scholar Law, West Law, and LexisNexus. Cases
were included if patients had a history of penicillin allergy and subsequently received a penicillin
(PCN), cephalosporin (CEPH), or carbapenem. PCN is defined as the entire class of penicillins
and penicillin refers to the specific antibiotic. CEPH is defined as the class of cephalosporin.
Results: One-hundred and eighty cases were screened and five met inclusion criteria. There were
no court cases in which a pharmacist was identified as a defendant. Defendants included
physicians, a dentist, and a hospital. Three court cases were identified involving patients with a
history of a penicillin allergy and treated with either penicillin or amoxicillin. In two of the cases
the prescribers were found guilty, and the third case was dismissed due to improper filing by the
plaintiff. Two cases were identified involving patients with a history of a penicillin allergy and
treated with a CEPH. The first case was settled out of court when it became apparent the
physician had not appropriately assessed the severity of the penicillin allergy. In the second case,
the hospital was found not guilty after a patient with a penicillin allergy received ceftriaxone for
the treatment of pneumonia. The not guilty verdict was due to lack of evidence proving crosssensitivity between ceftriaxone and penicillin.
Conclusion: Court precedent dictates pharmacists should refrain from dispensing PCN
antibiotics to patients with PCN allergies. The precedent regarding the use of a CEPH is not as
clear. When making a decision to dispense a CEPH to patients with PCN allergies, pharmacists
should take additional steps to assess the severity of the allergic reaction, ensure the antibiotic is
appropriate for the diagnosed infection, and inform the patient of the potential for allergic
reactions. Pharmacists with an understanding of legal precedent will be able to make more
informed decisions when caring for the large population of patients who have PCN allergies.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-372
Title: Stress related gastrointestinal bleeding in hospitalized patients with chronic liver disease
Primary Author: Jennica Stein, Roseman University of Health Sciences, Nevada;
Email: jstein@student.roseman.edu
Additional Author(s):
Jonathan Warta
Thomas Von Dohlen
Sean Barclay
Meghan Jeffres
Purpose: International normalized ratio (INR) and platelet count are typical markers of
coagulopathy used to identify patients at an increased risk for stress related upper gastrointestinal
bleed (GIB). Patients with chronic liver disease (CLD) often experience increased INR and
decreased platelet levels, however they also have a changes which increase their ability to clot,
including decreased production of anticoagulants and up regulation of von Willebrand factor.
Thus, coagulopathy defined by INR and platelet count may not be accurate markers in patients
with CLD. This study determines the incidence and characteristics associated with GIB in
patients with CLD and coagulopathy.
Methods: This retrospective study was conducted at a 450 bed county teaching hospital. Adult
patients admitted from January 1st, 2008 through January 1st, 2013 with an International
Classification of Diseases 9 (ICD-9) code for CLD were screened for inclusion and enrolled if
they also had coagulopathy, defined as a platelet count less than 50,000 per microliter and/or an
INR greater than 1.5. Patients who experienced a GIB 48 hours prior to or 24 hours following
admission were excluded. Primary analysis compared patients who developed a stress related
upper GIB to those who did not. Stress related upper GIB was defined as a bleed located in the
esophagus, stomach, or duodenum which occurred during inpatient admission and was
documented in the medical record.
Results: Inclusion criteria were met in 557 patients and 26 patients (4.7 percent) were identified
with an upper GIB during their hospital stay. INR greater than 1.5 occurred in 424 (76.1 percent)
patients and platelets less than 50,000 per microliter were identified in 266 (47.8 percent)
patients. In a univariate logistic regression neither INR level greater than 1.5 (odds ratio [OR]
1.35, 95 percent confidence interval [CI], 0.73 - 8.84) nor platelet count less than 50,000 per
microliter (OR 1.11, 95 percent CI, 0.73 - 8.84) were found to be significant predictors for stress
related GIBs. There was no difference between the rates of stress ulcer prophylaxis in the GIB
group compared with patients who did not bleed (65.4 percent versus 65.0 percent, p equal to
1.00). Patient characteristics associated with an upper GIB were portal hypertension (65.4
percent versus 18.3 percent; p less than 0.001), esophageal varices (53.8 percent versus 19.1
percent; p less than 0.001), and renal disease (26.7 percent versus 10.8 percent; p equal to 0.022).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Portal hypertension, esophageal varices, and renal disease were strongly correlated
to incidence of GIB in the observed population. These variables could be used to assess level of
risk for GIB in patients with CLD. SUP was not found to be associated with a decreased rate of
GIB, calling into question the utility of SUP in this patient population. Additional research
should be conducted addressing the use of SUP in patients with CLD, and the use of traditional
markers of coagulopathy (INR and platelet count) as indicators for increased risk of GIB should
be reevaluated in patients with CLD.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-373
Title: Practice habits of community pharmacists in the management of antibiotic prescriptions
for patients with penicillin allergies
Primary Author: Thomas von Dohlen, Roseman University of Health Sciences, Nevada;
Email: tvondohlen@student.roseman.edu
Additional Author(s):
Jude A Ngang
Alexander M Gilmer
Rashidat O Sanni
Bhavin Patel
Purpose: Approximately 10 percent of the US population reports a penicillin allergy. The
severity and pathophysiology of the allergic reaction is often unknown to the patient. The
community pharmacist must weigh the risk of provoking an allergic reaction by filling a
prescription of a beta-lactam with the risk of avoiding beta-lactams and recommending a more
costly or unnecessarily broad-spectrum alternative antibiotic. This study will identify the practice
habits of community pharmacists in the management of prescriptions for penicillin and
cephalexin for patients with a history of penicillin allergies.
Methods: We created a survey with 22 questions and submitted it to major pharmacy chains
throughout the US for distribution to practicing pharmacists. The survey includes two vignettes
with three multiple-choice questions. Each vignette presents a patient with a penicillin allergy
who has a prescription for either penicillin or cephalexin for the treatment of strep throat. Three
variations of each vignette included differing severity of allergic reactions ranging from
unknown to anaphylactic. The pharmacist is asked their most likely course of action based on the
given information. The survey will also collect demographic data and perceived legal
consequences. All data will be collected anonymously through an electronic survey. In each
vignette, a beta-lactam is the practitioners drug of choice to treat the patient.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-374
Title: Lymphogranuloma venereum (LGV) a rare STD: Review of a case report
Primary Author: Rachel Abrams, Long Island University, New York;
Email: rachel.abrams@my.liu.edu
Additional Author(s):
Stanley Wang
Antony Q. Pham
Purpose: Lymphogranuloma venereum (LGV), a sexually transmitted infection caused by
Chlamydia trachomatis serotype L1, L2, or L3, historically, has been an uncommon sexual
transmitted infection in the United States and industrialized countries. The true incidence in the
United States is not known as mandatory reporting is currently not required by the Centers for
Disease Control and Prevention (CDC). This project is set to discuss the incidence of LGV in a
27 year old HIV positive male who presented to the New York Harbor Healthcare System
Department of Veterans Affairs Manhattan with recurrent symptoms due to LGV.
Methods: A comprehensive evaluation using PubMed was utilized to review primary literature
and identify case reports of LGV. This review was further applied to assess the patient case.
Results: According to the primary literature, LGV is most common among males who have sex
with males. In a retrospective case control study, the strongest risk for LGV is HIV
seropositivity. Outbreaks have been reported in several large cities including London and New
York. The signs and symptoms can differ from person-to-person which makes the diagnosis
extremely difficult. In this patient, he presented to the hospital with recurrent symptoms and was
tested for sexually transmitted diseases. His laboratory results were negative for gonococcus and
syphilis but his urine and serology testing for Chlamydia were positive. He had an enlarged left
inguinal lymph node measuring 35.5mm without surrounding fluid and an anal fistula which are
two common signs of LGV. After careful testing, he was diagnosed with LGV, a rare STD
known in the Chlamydia family. The patient was discharged on the known treatment of
doxycycline 100mg PO twice daily for 21 days. Two weeks later the patient was contacted by
telephone and reported complete resolution of his rectal symptoms and enlarged inguinal lymph
node.
Conclusion: Although known to be historically uncommon and rare in the United States,
sporadic outbreaks of the lymphogranuloma venereum (LGV) has occurred in industrialized
countries including the United States. LGV presents with genital ulcers and papules, followed by
unilateral or bilateral inguinal lymphadenopathy. Patients may present with rectal ulceration and
anal ulceration. Left untreated, tissue damage and scarring may result as complications.
Diagnosis of LGV is based on clinical presentation, exclusion of other possible etiologies, and
culture, direct immmunofluorescence, or nucleic acid detection using lymph node or genital
specimens. Recommended treatment is doxycycline 100mg PO twice a day for 21 days.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-375
Title: Retrospective evaluation of quality measures in the treatment of community-acquired
pneumonia
Primary Author: Joseph Ahmed, D'youville College School of Pharmacy, New York;
Email: ahmedj21@dyc.edu
Additional Author(s):
Danny Kubit
Vy Bui
James Fenner
Nicole Cieri
Purpose: The Joint Commission on Accreditation, Health Care and Certification (JCAHO) in
collaboration with the Centers for Medicare & Medicaid Services (CMS) have created the
Specifications Manual for National Hospital Inpatient Quality Measures such that both
organizations have common measures of healthcare quality. This allows for synchronization of
data collection efforts in order to improve healthcare delivery. This studys purpose is to
determine how well current treatment practices for community acquired pneumonia (CAP) at
Millard Fillmore Suburban Hospital meet these quality measures. Adherence to the Infectious
Disease Society Association CAP guidelines and hospital specific quality measures will also be
evaluated.
Methods: The DYouville College Institutional Review Board approved this retrospective study.
All data collected will be de-identified for evaluation. Patients will be identified based on
treatment with empiric antibiotic therapy for a diagnosis or differential diagnosis of CAP.
Retrospective data will be collected only on patients meeting inclusion criteria. Patients above
the age of 18 will be included. ICU patients and patients on antibiotics for other types of
diagnosed infections such as hospital-acquired pneumonia, health care-associated pneumonia,
ventilator associated pneumonia, and urinary tract infections will be excluded. The following
data will be collected: age, gender, history of present illness, admission date, discharge date,
information regarding sputum cultures, information regarding urine antigen tests, information
regarding blood cultures, time of antibiotic initiation, chest x-ray results, intravenous (IV)
antibiotic start and stop dates, oral (PO) antibiotic start and stop dates, and antibiotic
streamlining. Calculated data will include hospital stay duration, duration of IV antibiotics,
duration of PO antibiotics, total duration of antibiotics, time to first blood culture drawn, number
of sputum cultures drawn, and time to initiation of antibiotics from admission. Appropriateness
of empiric and streamlined antibiotics will be assessed based on diagnosis and culture results.
Results: Results still pending.
Conclusion: Conclusion still pending.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-376
Title: Cost analysis of high- vs. low-dose intravenous immune globulin (IVIG) in kidney
transplant recipients with pre-transplant donor specific anti-human leukocyte antibodies (DSA).
Primary Author: Leah Andress, University at Buffalo, New York;
Email: leahandr@buffalo.edu
Additional Author(s):
Georgia Di Fiore
Kwaku Marfo
Purpose: Patients with pre-transplant DSA are at higher risk for antibody mediated rejection
(AMR). IVIG is a useful treatment in desensitizing renal allograft recipients. High prices of IVIG
place a burden on transplant medical centers as well as the healthcare system. Lower-dose IVIG
induction regimens may offer healthcare cost savings. The aims of this retrospective review were
to examine the effectiveness of lower dose IVIG induction and analyze cost savings associated
with lower dosing in kidney transplant recipients with pre-transplant DSA.
Methods: The institutional review board approved this retrospective medication use evaluation.
Medical records of kidney transplants recipients with pre-transplant DSA who received IVIG as
part of their induction therapy were reviewed. Baseline demographic characteristics and clinical
outcomes such as acute rejection episodes and IVIG effect on DSA levels post-therapy were
analyzed. To determine cost savings from IVIG therapy, total cost per treatment was calculated
using total doses of IVIG per patient multiplied by the drug acquisition cost for IVIG
(Gammunex/Gammagard) at our medical center.
Results: We categorized 66 DSA positive kidney transplant patients into two groups, low-dose
IVIG (those who received less than/equal to 1.5g/kg total of IVIG for induction) and high-dose
IVIG (those who received greater than 1.5g/kg total of IVIG for induction). Mean IVIG doses
were 1.3 plus/minus 0.4 g/kg and 2.4 plus/minus 0.6 g/kg for low-and high-dose groups,
respectively (P equals 0.0001). No significant differences existed between groups with respect to
mean age, rate of previous transplants, mean class I PRA, or mean class II PRA. Mean pretreatment DSA number and mean DSA MFI were higher for the high-dose group (2 plus/minus 1
and 3398 plus/minus 3323, versus 1.5 plus/minus 0.8 and 2214 plus/minus 1210). Most recent
mean DSA and MFI were also higher for the high-dose group (0.6 plus/minus 0.9 and 4924
plus/minus 4419, versus 0.3 plus/minus 0.6 and 2660 plus/minus 2721). Last mean creatinine
was 1.5 plus/minus 0.7 mg/dL for the low- dose group and 1.3 plus/minus 0.3 mg/dL for the
high-dose group. High-dose patients experienced increased incidence of acute allograft rejection
(16.7 percent vs. 4.5 percent). Potential cost savings of 243,000 dollars was estimated if all 66
pre-transplant DSA positive patients received induction with less than/equal to1.5g/kg of IVIG.
Conclusion: Low-dose IVIG was just as effective as high-dose IVIG in preventing acute renal
allograft rejection in pre-transplant DSA positive patients. Significant cost-savings from the
healthcare system perspective can be achieved with low-dose IVIG induction. However,
prospective studies evaluating both efficacy and safety of IVIG induction in kidney transplant
recipients with pre-transplant DSA is warranted.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-377
Title: Effect of antibiotic use on length of hospitalization in acute pancreatitis
Primary Author: Brittany Andruszko, SUNY at Buffalo, New York;
Email: bna4@buffalo.edu
Additional Author(s):
Brian Kersten
Ashley Woodruff
Purpose: The use of prophylactic antibiotics in patients with acute pancreatitis is controversial.
Past studies have demonstrated a reduction in mortality after using prophylactic antibiotics in
patients with acute pancreatitis, however recent meta-analyses have shown no difference in
mortality or other complications. These studies were done in severe or necrotizing pancreatitis,
and this differs from most hospital admissions for acute pancreatitis which are mild to moderate.
The purpose of this study was to determine if there was a difference in length of hospitalization
between patients with mild to moderate acute pancreatitis who were given antibiotics and those
who were not.
Methods: Institutional review board approval was obtained. A retrospective cohort including
men and women age 18 and older with a primary or secondary diagnosis of pancreatitis upon
hospital admission were included. Other inclusion criteria were admission to a general medical
floor and documentation of a computed tomography (CT) scan of the abdomen. Patients with a
CT Severity Index Score greater than 6, Bedside Index for Acute Pancreatitis (BISAP) Score
greater than 2, necrotizing pancreatitis, or those admitted to the intensive care unit were
excluded. Those patients who received antimicrobial treatment within 3 months prior to
admission or who had any positive cultures during their hospitalization were also excluded. The
primary study outcome was to determine if there was a difference in hospital length of stay for
patients with mild to moderate acute pancreatitis who received antibiotics versus those who did
not receive antibiotics. The secondary study outcomes were to compare in-hospital mortality and
adverse events, as evidenced by the incidence of Clostridium difficile (C. diff), between the two
arms. It was determined that 29 subjects per study arm would yield 80 percent power to detect a
20 percent difference in length of hospitalization with a 2-tailed alpha level of 0.05.
Results: A total of 29 subjects were included in the antibiotic study arm and 50 subjects were
included in the arm that did not receive antibiotics. There was a significant difference in length
of hospitalization for patients who received antibiotics compared to those who did not, 5.42 days
versus 3.84 days; p less than 0.001, respectively. There was no in-hospital mortality in either
arm, and no positive C. diff toxin assays were reported. Five subjects (17 percent) in the
antimicrobial arm received carbapenems, and 14 subjects (48 percent) received
piperacillin/tazobactam during their hospitalization.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Patients treated with prophylactic antibiotics had significantly longer lengths of
hospitalization than those who were not treated with antibiotics. These results favor current
guidelines which do not recommend the use of prophylactic antibiotics in patients with acute
pancreatitis. The high percentage of broad-spectrum antibiotic use illustrates a need for
antimicrobial stewardship to reduce antibiotic usage in this patient population.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-378
Title: Efficacy and safety of ticagrelor compared to higher loading doses of clopidogrel in
patients with acute coronary syndromes who underwent percutaneous coronary intervention
Primary Author: Syed Arafath, Arnold & Marie Schwartz College of Pharmacy and Health
Sciences Long Island University, New York
Email: syed.arafath@my.liu.edu
Additional Author(s):
Barry Steinzaig
Nadiya Korobova
Purpose: The PLATO trial looked at ticagrelor at a 180 mg loading dose vs clopidogrel at a 300
mg loading dose. No previous studies directly compared the effects of using a loading dose of
600 mg of clopidogrel vs a loading dose of 180 mg of ticagrelor. The objective of this study is to
compare efficacy and safety and to look at the outcomes of administering clopidogrel at a 600
mg loading dose and ticagrelor at a 180 mg loading dose to patients with Acute Coronary
Syndrome who underwent Percutaneous Coronary Intervention.
Methods: This study has been approved by the Institutional Review Board. Patients who are 18
years of age or older, who underwent Percutaneous Coronary Intervention with a diagnosis of
Acute Coronary Syndrome and received a 600 mg loading dose of clopidogrel or 180 mg loading
dose of ticagrelor were identified through pharmacy dispense reports and catheterization
databases. A total of 100 patients (50 patients received clopidogrel and 50 patients received
ticagrelor) were included in this study. Patients who received clopidogrel for non-cardiovascular
related disease states, or were not continued on maintenance doses of clopidogrel or ticagrelor
were excluded from this study. Consent letters for calls through certified mail were mailed to
participating patients. Patients were informed that their identities would remain confidential and
their participation is voluntary. Information collected will include demographics, diagnosis, past
medical history, concomitant antiplatelet and antithrombotic therapy, renal and hepatic function,
concomitant cardiovascular medications, timing of administration for clopidogrel or ticagrelor
loading doses, cardiovascular events. The primary efficacy endpoint will be a composite of death
from cardiovascular causes, non-fatal myocardial infarction or stroke at 1 year from index
Percutaneous Coronary Intervention. The primary safety endpoint includes incidence of major
and minor bleeding events.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-379
Title: Oral Vancomycin Dosing in the Treatment of Clostridium Difficile Infection: A
Retrospective Comparison of Doses
Primary Author: Stephen Argiro, St. John's University College of Pharmacy and Health
Sciences, New York;
Email: stephen.argiro08@gmail.com
Additional Author(s):
Karen Tang
Bruce Hirsch
Donna Sym
Purpose: Nosocomial infectious diarrhea is a major concern in patients with prolonged
hospitalizations. Clostridium difficile is a primary cause of this healthcare acquired infection and
the elderly are especially at risk. The IDSA/SHEA guidelines recommend oral vancomycin 125
mg 4 times daily for 10-14 days for the initial episode of severe Clostridium difficile infection
(CDI) and 500 mg 4 times daily with or without metronizazole 500 mg intravenously every 8
hours for 10-14 days for severe complicated CDI. Although not recommended by the guidelines,
an oral dose of vancomycin 250 mg 4 times daily is frequently prescribed. This retrospective
chart review will evaluate if oral vancomycin 250mg four times daily has any benefit or
additional risks in comparison to the 125mg four times daily dosing regimen.
Methods: A report of patients receiving oral vancomycin solution between the date of 1/1/12
and 12/31/12 was generated by Sunrise Clinical Manager. Only adult patients with
documentation of CDI by positive PCR test and receiving oral vancomycin 125 mg every 6
hours or 250 mg every 6 hours were included. Pregnant women, patients receiving other
medications for the treatment of CDI (i.e metronidazole, rifaximin, fidaxomycin, cholestyramine,
IVIG, probiotics) or oral vancomycin 500 mg 4 times daily for severe complicated CDI were
excluded. The following information will be collected for each patient: medical record number,
age, gender, medication dose, date of admission, date of discharge, length of stay, length of
treatment, white blood cell count at diagnosis and at discharge, serum creatinine at baseline, at
diagnosis, and at discharge, concurrent antibiotics during treatment, readmission for CDI within
30 days of discharge, and readmission for CDI within 90 days of discharge. Investigators will
then compare the data between these groups of patients to determine if the higher dose has any
benefit over the IDSA/SHEA recommended dose of 125 mg four times daily and if there are any
additional side effects.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-380
Title: The clinical implications of assessing platelet responsiveness to aspirin using whole blood
platelet aggregation versus urinary 11-dehydrothromboxane testing
Primary Author: Jeffrey I Baron, University at Buffalo, New York;
Email: jibaron@buffalo.edu
Additional Author(s):
Erica S Westphal
Michelle M Rainka
Francis M Gengo
Vernice E Bates
Purpose: Over the past 30 years aspirin use has played a major role in preventative therapy for
cerebrovascular events. However, one of the largest problems with individualized antiplatelet
therapy is that clinicians lack a proven method to measure platelet response to antiplatelet
therapy. Results from this study could provide insight into the efficacy of whole blood platelet
aggregometry in conjunction with11-dehydrothromboxane B2 (TXB2) testing as well as their
efficacy separately in preventing ischemic strokes and/or transient ischemic attacks (TIAs). It
will also provide a perspective on the clinical decisions in antiplatelet therapy made based on
each testing procedure.
Methods: This study was approved by the University at Buffalos Institutional Review Board.
Males and females ages 18-90 years old, who have been on an aspirin regimen for at least two
weeks and are having whole blood platelet aggregation tests as part of their normal care will be
included. Informed consent will be obtained. Participants must also have had a confirmed stroke
or TIA within the past 3 months so that ABCD2 and ESSEN stroke risk scores can be calculated.
Those who have used NSAIDs, have a history of alcohol abuse or any systemic disorder that
could affect platelet function, or recently consumed any alcohol will be excluded. Urine samples
will be tested for aspirin compliance by diluting the urine with ferric chloride; the remaining
urine will be sent for TXB2 testing. Platelet aggregation will be conducted using collagen 1.0
and 5.0 ug/ml and arachidonate 0.5mM, measured in ohms of resistance. Study endpoints are
ohms of resistance and pg/mg levels of urinary thromboxane. Data analysis will consist of a Chi2
test to determine if there is a significant difference in the proportion or patients called
sensitive/resistant by each test and a Spearmans correlation to correlate urinary TXB2 and
platelet aggregation results.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-381
Title: Establishing beyond use dating for radiopharmaceuticals: quality control for
technetium99m sestamibi, technetium99m diethylene triamine pentaacetate (Tc99m DTPA), and
technetium99m albumin aggregated (Tc99m MAA).
Primary Author: Jessica Bente, St. John's University, NY;
Email: Bente.jessica@gmail.com
Additional Author(s):
Thomas Boland
Purpose: Currently, manufacturers of radiopharmaceuticals provide nuclear pharmacies with
strict preparation and expiration guidelines for their products in order to ensure compliance with
USP standards. In order to deviate from the manufacturers compounding guidelines,
radiopharmacies would need to establish beyond use dating (BUD). Should BUD be established,
it would provide radiopharmacies with cost saving measures and an opportunity to offer patient
flexibility without compromising quality of care. The purpose of this study is to verify the
radiochemical stability of technetium99m sestamibi, technetium99m diethylene triamine
pentaacetate (Tc99m DTPA), and technetium99m albumin aggregated (Tc99m MAA) beyond
the manufacturers recommended expiration time.
Methods: All products were prepared according to USP 797 guidelines, and varied in total
activity according to company protocol. Radiochemical stability was quantified by calculating
the percentage of Tc99m tagged to the products Sestamibi, DTPA, and MAA at hours 0, 6, and
18 post preparation. Quality control for radiochemical purity was performed using instant thin
layer chromatography (ITLC). Quality control was performed on 5 samples of each
radiopharmaceutical over the span of 0-18 hours post preparation for a 5 day period.
Results: For all products, the USP standard of radiochemical purity was 90%. The company
standard of radiochemical purity for Tc99m Sestamibi and Tc99m MAA was 92% and Tc99m
DTPA was 95%. The manufacturer expiration time for Tc99m Sestamibi and Tc99m MAA was
6 hours post preparation and Tc99m DTPA was 12 hours post preparation. The mean tagged
product of Tc99m Sestamibi at 0 hours was 97.89%, 6 hours 96.48%, and 18 hours 93.96%. The
mean tagged product of Tc99m DTPA at 0 hours was 98.53%, 6 hours 95.72%, and 18 hours
89.23%. A 3 day follow-up study was performed on Tc99m DTPA examining 3 samples at hours
0 and 18 post preparation. The mean tagged product at 0 hours was 99.35% and 18 hours
97.91%. The mean tagged product of Tc99m MAA at 0 hours was 99.12%, 6 hours 98.62%, and
18 hours 90.24%, with an outlier of 79.79% at 18 hours on Day 2 and no 18 hours data on Day 4.
For Days 1, 3, and 5 the mean tagged product of Tc99m MAA at 18 hours was 93.72%.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The objective of this study was to verify the radiochemical stability of Tc99m
Sestamibi, Tc99m DTPA, and Tc99m MAA beyond the manufacturers recommended expiration
time. The above findings have demonstrated that BUD can be established for both Tc99m
Sestamibi and Tc99m MAA at 18 hours according to USP and company standards. Although the
original study did not establish BUD of Tc99m DTPA at 18 hours, the follow-up study did
establish BUD of 18 hours according to USP and company standards. Future studies will need to
be conducted in order to validate these results.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-382
Title: Evaluation of the utilization of pharmacy interns conducting medication reconciliation in
the emergency department
Primary Author: Jessica Beyer, University at Buffalo School of Pharmacy, New York;
Email: jtbeyer@buffalo.edu
Additional Author(s):
Alyssa Pignato
Juliana Zschoche
Elizabeth Dodds-Ashley
Purpose: Medication errors place a large financial burden on the health care system. However,
some of this burden can be alleviated when medication errors are reduced by conducting
effective medication reconciliation. The purpose of this study was to determine the impact
pharmacy interns and potentially pharmacists can have on medication errors when conducting
medication reconciliation in the emergency department (ED) at the University of Rochester
Medical Center (URMC).
Methods: The research subjects review board approved this retrospective, quality improvement
study. All patients, male and female over the age of 18, who had a pharmacy intern conduct their
medication reconciliation while admitted to the ED between June 25 and August 17, 2012 were
reviewed. Data was extracted from an existing database maintained for quality assurance
purposes at URMC. This study evaluated the number of medication discrepancies identified
which was further analyzed based on the type of discrepancy such as incorrect schedule,
incorrect route, incorrect dose, deleted medication, added medication, and incorrect medication.
Additionally any calls which were made to family, community pharmacies, doctors, or other
location in order to confirm a patient's medications were analyzed and evaluated. Phone calls
were made following patient interviews if the patient was unable to provide a full medication list.
Results: A total of 751 patients had medication reconciliation performed by a pharmacy intern.
Of those 751 patients, 7,297 medications were reviewed, an average of 9.72 medications per
patient. Over the period of the project 3,022 interventions were made. Adding and deleting
medications from patients medication profiles were the main interventions (56.5% and 70.2%
respectively). However, numerous patients also had medications listed with the incorrect
schedule, dose, and route (7.2%, 21.6%, and 0.3% respectively). A total of 251 phone calls were
made in order to clarify patients current medications. The majority of calls were made to
community pharmacies (63.6%).
Conclusion: Pharmacy interns conducting medication reconciliation in an ED can have a
considerable impact on the number of medication interventions which can be made, potentially
reducing the number of medication errors. Results from this quality improvement study
demonstrated the utility of decentralized pharmacists in the ED with respect to medication
reconciliation. Further investigation is needed to determine clinical outcomes of these
interventions.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-383
Title: Student educational benefit, professional development, and satisfaction when participating
in an international medical brigade
Primary Author: Gregory Blette, D'Youville College School of Pharmacy, New York;
Email: blettg19@dyc.edu
Additional Author(s):
Lindsey Zawierucha
Michelle Lewis
Kirsten Butterfoss
Purpose: Student development both in and out of the classroom, didactic as well as real-world
experience, is paramount to the projected success of these future practitioners. The objective of
this study is to determine if there is a benefit of participation in an international medical brigade
on a students education and professional growth in the field of pharmacy as well as to assess
their personal satisfaction with the experience. Students participated voluntarily and performed
many different duties while on the brigade. Impact on the students professional development was
measured in order to determine usefulness as an APPE and IPPE rotation activity.
Methods: Students attending the DYouville College School of Pharmacy were invited to apply
for an international medical brigade IPPE or APPE, depending on professional class year, to
Tena, Ecuador. Selected students traveled on a 10-day brigade that visited six underserved
villages with little or no access to healthcare. The brigade was made up of volunteers primarily
from two different colleges and included physicians, nurses, pharmacists, translators, student
pharmacists, nursing students, and general volunteers. Upon completion of the brigade, students
were asked to complete a survey assessing their perceived benefit to their education and
professional development as well as their personal satisfaction with the experience. There was
also a section for student input regarding the strengths and weaknesses of such experiences and
how they could be improved upon. The results, once compiled, are to be used in assessing and
improving the current medical brigade as well as for evaluating the implementation of new
international interdisciplinary brigade rotations into the IPPE/APPE curriculum at the DYCSoP.
The proposal for this project is exempt from IRB approval based on its intent for quality control
purposes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-384
Title: Evaluation of the use of stress ulcer prophylaxis (SUP) in a medical intensive care unit
(MICU)
Primary Author: Vy Bui, D'Youville College School of Pharmacy, New York;
Email: vy.n.bui@gmail.com
Additional Author(s):
Eric Kalita
Darowan Akajagbor
Purpose: Stress ulcer prophylaxis (SUP) is routinely used to prevent the development of stress
related mucosal disease (SMRD) in medical intensive care unit (MICU) patients. The American
Society of Health- System Pharmacists (ASHP) published guidelines in 1999 to direct the
appropriate use of SUP in critically ill patients. The purpose of this study is to evaluate the
appropriateness of SUP therapy in the MICU at Upstate University Hospital based on the ASHP
guidelines and current clinical evidence.
Methods: This prospective study is considered a quality assurance review and therefore does not
require the institutions institutional review board approval. The study will include patients
admitted to the MICU that received a proton pump inhibitor (PPI) or a histamine-2 receptor
antagonist (H2RA) for SUP prophylaxis. The reviewers will exclude patients that received PPIs
or H2RAs for indications such as gastrointestinal reflux disease (GERD), erosive esophagitis or
gastritis, gastrointestinal bleed or other indications supported by the medical literature. The
following data will be collected and analyzed: patient age, gender, admitting diagnosis,
comorbidities, dose, formulation and duration on SUP, patient specific risk factors for SUP based
on the ASHP guideline, discharge or transfer date, and length of stay in the ICU. To evaluate
appropriateness of SUP usage, analyzed data will be compared against the predefined risk factors
as stated in the ASHP guideline.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-386
Title: Safety of high dose intravenous continuous infusion of midazolam in refractory status
epilepticus
Primary Author: Fiona Cheung, St. John's University, New York;
Email: fiona.cheung08@stjohns.edu
Additional Author(s):
Christine Lesch
J Michael Schmidt
Jan Claassen
Christopher G. Zammit
Purpose: Continuous infusion midazolam (ci-MDZ) is one of the antiepileptic agents of choice
for patients in refractory status epilepticus (RSE). Common complications associated with
prolonged benzodiazepine use include respiratory depression and hypotension. Anecdotally, we
have observed the occurrence of unexplained metabolic acidosis in patients receiving high dose
continuous infusion midazolam. This may be due to the acidic solvent required to buffer the
solution. The objective of this research project is to determine the incidence of metabolic
acidosis in patients with refractory status epilepticus requiring ci-MDZ and determine if an
association with higher doses exists.
Methods: This was a retrospective, single-center analysis including 49 patients who received ciMDZ between 2007 and 2011, approved by the Institutional Review Board. Patients were
excluded from this study if they were in cardiac arrest preceding their episode of RSE or initiated
on continuous infusion midazolam at an outside institution and information regarding dosages,
electroencephalography (EEG), or clinical response is unavailable. Data collected includes
demographics (age, sex, weight, date of birth, ethnicity, baseline Glasgow Coma Scale scores,
and previous stroke), concurrent medication history, midazolam use (dose and time of
administration), basic metabolic panels, liver function tests, and arterial blood gases. The
primary endpoint is incidence of metabolic acidosis after continuous midazolam infusion
initiation. The secondary endpoint is to evaluate factors associated with metabolic acidosis and
describe vasopressor use for midazolam-induced hypotension.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-387
Title: Correlation between vitamin D supplementation and fall prevention in long-term care
residents
Primary Author: Laura Conrad, D'Youville College School of Pharmacy, NY;
Email: conral22@dyc.edu
Additional Author(s):
Laura Pochylski
Kevin Mills
Purpose: The American Geriatrics Society (AGS) Clinical Practice Guideline for Prevention of
Falls in Older Persons recommends the use of vitamin D supplementation in the elderly
population, especially in those that are proven to be vitamin D deficient. This population is
highly susceptible to falls, which may increase mortality. The objective of this study is to
determine the extent to which vitamin D supplementation has on fall rates in long-term care
residents at Degraff Skilled Nursing Facility.
Methods: This retrospective study has conditional approval by the DYouville College
Institutional Review Board. Current residents in the long-term care facility will be included in
the study. Residents will be excluded if they are under the age of 65 and/or receiving
rehabilitation therapy at this site. The following data will be collected via the electronic medical
record system: patient age, gender, Brief Interview for Mental Status (BIMS) score, vitamin D
dosage for residents on a vitamin D regimen, vitamin D levels (if applicable), pertinent past
medical history (osteoporosis, fractures, multiple sclerosis), fall history since January 1, 2012
(includes all residents admitted prior to and after this date), and medications that are recognized
by AGS to predispose the elderly to falls. All data will be recorded without patient identifiers
and maintained confidentially. Fall rate will be calculated based on the number of falls
experienced for each patient over 6 month periods. Data will be evaluated to determine if fall
rates are decreased in elderly residents receiving vitamin D supplementation compared to
residents not on a vitamin D regimen.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-388
Title: Risk Evaluation and Mitigation Strategies with Elements to Assure Safe Use: Lessons
Learned in the Effective Management of Drug Risk
Primary Author: Michael Cronin, St. John's University, Queens, NY;
Email: mcronin63@gmail.com
Purpose: The Food and Drug Administration Amendments Act (FDAAA) of 2007 gave the
FDA the authority to require a Risk Evaluation and Mitigation Strategy (REMS) for medicines
with serious safety concerns. Since its inception over 200 REMS programs have been approved.
Currently, FDA and multiple stakeholder groups representing patients, healthcare systems,
physicians, pharmacists, nurses and drug sponsors are examining ways to standardize and
integrate these risk mitigation programs into their work flow. This review of REMS that have
specific Elements to Assure Safe Use (ETASU) is aimed to assist in developing best practices in
their implementation and assessment.
Methods: Each distinct REMS with ETASU was reviewed and classified according to the
indication, risk to be mitigated, stated REMS goals, and ETASU tools that were employed. The
various ETASU tools were stratified by the target audience (prescriber, healthcare facility,
pharmacy, and/or patient) and whether documentation of safe use conditions was required. The
REMS goals were analyzed by whether the goal was directly linked to an action aimed at
mitigating the specified risk or was meant to provide information regarding the risk. The tools
employed by each REMS were analyzed by the type of risk to be mitigated and how they
contributed to achieving the programs goals. Each ETASU tool was categorized based on
whether its application involved an interventional behavior such as laboratory testing, special
monitoring, restricting use or promoting early detection of a risk, or was intended to educate the
physician and patient. The implementation plan for each REMS was reviewed to assess the
impact of the program on the healthcare deliver system. Only publicly available information of
the most recent REMS document posted on the FDA website was used for these analyses.
Results: Most REMS with ETASU (65%) have a combination of risk mitigation and educational
goals. Five general risk categories emerged, with preventing fetotoxicity (25%) as most
common. 79% of ETASU REMS employ prescriber-based tools, which include performing
laboratory testing (e.g., pregnancy, hepatic enzymes) or monitoring (e.g., ophthalmologic
examinations, documenting vaccination). 50% of ETASU REMS employ pharmacy tools
including the provision of Medication Guides, special counseling, verifying prescriber and/or
patient enrollment prior to filling a prescription. Healthcare facility tools were used in 29% of the
ETASU REMS including facility enrollment and attestation of the ability to manage the risk and
assure appropriate dispensing of the medication. Finally 71% of ETASU REMS use various
conditions of safe use such as verification or attestation forms, completion of checklists,
enrollment in databases, or using authorization forms or stickers to accompany prescriptions.
65% required enrollment from two or more healthcare provider categories indicating that most
REMS with ETASU require significant involvement from multiple stakeholders within the
healthcare delivery system.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: The REMS reviewed in this study varied from programs requiring behaviors that
can be measured and directly reduce the known risk to those where the risk cannot be reduced in
frequency or severity and rely on knowledge acquisition, restricted distribution and provider selfcertification and attestation. Whether the application of the REMS tools leads to better
management and subsequent mitigation of a risk is unknown. Implementation of many of the
REMS tools such as attestation forms and pharmacy stickers are outside of normal health care
delivery workflows and need better integration to reduce burden on the healthcare delivery
system.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-389
Title: Pediatric Education across US Pharmacy Schools: What is being taught and how?
Primary Author: Elizabeth Dahl, University at Buffalo School of Pharmacy and Pharmaceutical
Sciences, New York;
Email: emdahl@buffalo.edu
Additional Author(s):
David Hutchinson
William A Prescott
Purpose: To determine the extent pediatrics is taught at US PharmD programs and secondarily,
to characterize what pediatric content is being taught and how it is being taught.
Methods: A 40-question online survey was sent to a total of 128 accredited and candidate status
PharmD programs in the US and its territories. The survey was distributed on 5/7/2013 and it
closed on 7/2/2013. The survey responses were downloaded into Microsoft Office Excel
spreadsheet (Redmond, WA). If the curriculum of the responding program included pediatric
content, information about the extent and type of required didactic coursework, elective didactic
coursework, and experiential teaching related to pediatrics, as well as the instructional
methodologies used to teach pediatrics were requested. Frequency and descriptive statistics were
used to characterize the extent pediatrics is taught, what pediatric content is being taught, and
how it is being taught at US PharmD programs. Results were compared to the 2005 pediatric
curricula recommendations published by the Pediatric Practice and Research Network of the
American College of Clinical Pharmacy (ACCP).
Results: A total of 86/128 programs responded to the survey (67.2% response rate).
Demographics of responding programs were similar to US PharmD programs as a whole. Eightyone programs (94.2%) indicated pediatric topics were included within their required didactic
curriculum. The mean number of contact hours dedicated to pediatric topics was 21.9 hours.
Approximately three-quarters of programs did not meet the 25 contact-hour standard set by
ACCP. Types of instruction most commonly employed to teach pediatric topics in the required
curricula included lecture (91.8%) and case-based (87.7%). A stand-alone pediatric elective was
offered by 61.0% of programs. The mean contact time was 25.9 hours, with 75% of PharmD
programs meeting the ACCP recommendation of more than 16 hours. Types of instruction most
commonly employed to teach pediatric topics in the elective curricula were lecture (75.6%) and
case-based (71.1%). Forty-one of the 77 responding programs (53.2%) offered a pediatric
introductory pharmacy practice experience (IPPE). Pediatric-focused advanced pharmacy
practice experiences (APPE) were offered by 97.4% of programs. A mean number of 22
pediatric APPE rotations were offered, with a mean of 27 students completing a pediatric
rotation annually. Programs indicated that an average of 39.3 hours per week were dedicated to
this rotation.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: Almost all responding programs incorporated pediatrics within the required didactic
curricula, but most did not meet ACCP standards. Stand-alone pediatric elective courses were
common, and when offered, provided an adequate number of contact hours. However,
approximately one-third of programs did not offer a pediatric elective. Almost all responding
programs offered a pediatric-focused APPE, but due to the limited quantity of these experiences,
only one-fifth of students completed a pediatric-focused APPE prior to graduation. Continued
expansion of pediatric-focused didactic and experiential curricula across US PharmD programs
is recommended to meet ACCP recommendations.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-390
Title: Student Attitudes Regarding Active- or Team-based Learning versus Traditional (lecturebased) Classes
Primary Author: Sonia Dhanjal, D'Youville College School of Pharmacy, New York;
Email: soniadhanjal7@gmail.com
Additional Author(s):
Kofi Asante
Brandilynn Sieminski
Purpose: To assess students attitude toward active- or team-based learning compared to
traditional or lecture based learning. Student pharmacists enrolled at the DYouville College
School of Pharmacy. Students in their first three years were included.
Methods: The sample population included student pharmacists in their 1st, 2nd or 3rd year
attending D'Youville College School of Pharmacy during the 2012-2013 academic year in the
fall semester with active- or team-based instruction and traditional instruction experience. Data
was collected from a cross sectional survey comprised of 8 statements. All survey statements
regard the utility of active- or team-based learning compared to traditional learning. Student
subjects voluntary informed consent was obtained via completion of the student survey. Students
were asked to complete the survey in the classroom setting during a Collaborative Learning
Practicum class. Surveys were collected and data was compiled.
Results: We hypothesized the result to be 50/50 in terms of students who prefer active learning
and those who do not prefer it. The results showed that majority of the student pharmacists felt
the team-based learning facilitated their understanding of the material and application to real life
scenarios. The activities were appropriate to support the learning objectives of the respective
classes, and allowed them to clarify any information pertaining to the subject. Student
pharmacists, however, did point out that active team based learning is more appropriate for some
courses than others. Appropriate classes included: Pharmacotheraputics, Collaborative Learning
Practicums, Principles of Drug Action, and Biostatistics and Literature Evaluation classes.
Student attitudes toward active team-based learning and traditional lecture-based learning is split.
The majority of student pharmacists also felt active learning aided in the clarification of subject
material as well as prepares them for real-life experience.
Conclusion: Student attitudes toward active team based learning and traditional lecture based
learning is split. For the majority of students, active learning aids in the clarification of subject
material as well as prepares them for real-life experience. Because the concept of team based
learning is still relatively new, further studies need to be conduction to see the positive trend of
active team based learning.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-391
Title: Evaluation of rivaroxaban use at a large tertiary care university affiliated hospital
Primary Author: Helen Dong, St. John's University, NY;
Email: helen.h.dong@gmail.com
Additional Author(s):
Hanlin Li
Fiona Cheung
Tran Tran
Purpose: Rivaroxaban is a new factor Xa inhibitor that is noninferior to warfarin in the
prevention of stroke in patients with nonvalvular atrial fibrillation. Although rivaroxaban has a
similar rate of major bleeding as compared to warfarin, it is associated with significantly more
gastrointestinal bleeding. This drug utilization evaluation intends to assess the incidence of major
bleeding related to rivaroxaban use in patients with atrial fibrillation and to ensure rivaroxaban is
being prescribed appropriately at our institution.
Methods: The Institutional Review Board approved this retrospective chart review. All data
were recorded without patient identifiers and maintained confidentially. The chart review was
performed for 400 adult patients aged 18 and older who were administered any dose of
rivaroxaban in the hospital between January 1, 2012 and July 31, 2013. We included atrial
fibrillation patients who received rivaroxaban for stroke prevention. We excluded patients who
received rivaroxaban for other indications, and patients for whom rivaroxaban was ordered but
never administered. The primary outcome is the percent of patients on rivaroxaban experiencing
a major bleed while at our hospital. The secondary outcomes include the percent of patients
prescribed rivaroxaban for appropriate indications, the percent of time rivaroxaban was
accurately administered based on dose adjustments provided by manufacturer recommendations,
and the incidence of documented minor bleeds.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-392
Title: Management of infections caused by extended-spectrum beta-lactamase Klebsiella
pneumoniae in a teaching hospital
Primary Author: Esther Drillman, Long Island University, New York;
Email: stdrillman@gmail.com
Additional Author(s):
Sharone Aragon
Anna Nogid
Purpose: The emergence of drug resistant (MDR) gram-negative pathogens has been a rising
concern in the United States and across the world in the last decade. The available treatment
options are extremely scarce; therefore, the management of MDR gram-negative infections is
challenging. The objective of this study is to describe clinical and microbiologic response rates
of patients who were treated for infections caused by MDR gram-negative pathogens,
specifically Klebsiella pneumoniae.
Methods: This study was submitted to the Long Island University and Brookdale University
Hospital and Medical Center (BUHMC) Institutional Review Boards where IRB approval was
obtained. A retrospective chart review using a data collection form was performed. Patients with
cultures positive for carbapenem-resistant Klebsiella pneumonia from January 1, 2011 through
December 31st, 2012 were identified using the hospital's microbiology database and considered
for inclusion into the study. Patients were included if they had a cultures positive for
carbapenem-resistant Klebsiella pneumonia, received effective antibiotic treatment for at least 48
hours, and were at least 18 years old. Patients with cultures positive for carbapenem-resistant
Klebsiella pneumonia documented to be non-pathogenic were excluded from the analysis. The
following data was collected: patient demographics, concomitant and previous antibiotic
exposure, including dose, frequency, and duration of therapy, culture results, laboratory
parameters, clinical parameters, and length of hospital and ICU stay. Clinical outcomes were
classified as positive, negative, or indeterminate. Microbiologic outcomes were assessed in
patients with follow-up cultures upon completion of antibiotic therapy. Outcomes were judged as
positive or negative. The final disposition of each patient at the end of the study was noted as
well.
Results: Forty four patients were screened for inclusion in the study and twenty seven were
included for analysis. The average age of the patients was about seventy years old, most were
females as well as nursing home patients. Clinical outcomes were determined for each patient
and it was noted that 17 patients had positive outcomes, 7 had negative outcomes, and 3 resulted
in indeterminate outcomes. In terms of microbiologic response rates, of the 25 patients who
received follow-up cultures, 23 patients had a positive outcome and 3 had a negative outcome.
Of The most common adverse effects seen in patients included in the study were AST elevation
(48.1%), ALT elevation (40.7%), and alkaline phosphatase elevation (51.9%). When examining
the aforementioned adverse effects at three times the upper limit of normal, lower percentages
were noted; 18.5% for AST elevation, 11.1% for ALT elevation, and 14.8% for alkaline
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
phosphatase elevation. Monotherapy was used in 11 patients with 3 positive clinical outcomes, 5
negative outcomes, and 3 indeterminate results. Combination therapy was used in 16 patients, 4
of which had positive outcomes and 12 of which had negative outcomes.
Conclusion: No treatment option was superior in improving clinical and microbiological
outcomes in carbapenem-resistant Klebsiella pneumoniae bacteremia. After analyzing the data, it
was noted that positive microbiologic outcomes were more likely than positive clinical
outcomes; however, it was not correlated with mortality. Additionally, stratification of the
patients treatment regimens with combination vs. monotherapy highlighted that combination
therapy was not associated with improved outcomes.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-393
Title: Perceptions of Doctor of Pharmacy candidates on a potential behind-the-counter class of
medications
Primary Author: Kristen Fodero, University at Buffalo School of Pharmacy and
Pharmaceutical Sciences, New York;
Email: kefodero@buffalo.edu
Additional Author(s):
Erin Slazak
Purpose: The implementation of a proposed third class of behind-the-counter (BTC)
medications could have significant implications on the future of pharmacy practice. Current
literature evaluating this proposed class of medications reflects the opinions of practicing
pharmacists; however, if BTC medications are the future of pharmacy then understanding the
current opinions of Doctor of Pharmacy (Pharm.D.) candidates, who represent the future of
pharmacy practice is also important. The purpose of this study is to gain a better understanding
of the current opinions of Pharm.D. candidates regarding this proposed class of medications and
to identify any perceived barriers to its successful implementation.
Methods: This study was submitted to the Social and Behavioral Sciences Institutional Review
Board and was approved. Pharm.D. candidates in their second, third and fourth professional year
were given the opportunity to participate in an online survey administered using the online
survey program, Vovici. The survey consisted of 14 questions that were either multiple choice or
Likert Scale. Background characteristics of respondents including graduation year, pharmacy
practice experience and post-graduation plans were also collected to assess level of therapeutic
knowledge and familiarity with the current community pharmacy practice environment. The
remaining questions assess perceived competency and willingness to participate in a BTC
program. Respondents were also asked specifically about 8 different categories of medications
that may be considered for inclusion in a BTC class of medications. Overall responses will be
used to identify any potential barriers which may prevent the successful implementation of a
BTC class of medications. Data will be analyzed using Microsoft Excel and MiniTab.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-394
Title: Modeling of lactic acidosis risk post contrast dye in leukemia patients treated with
metformin
Primary Author: Minna Fung, University at Buffalo, School of Pharmacy and Pharmaceutical
Sciences;
Email: mfung2@buffalo.edu
Additional Author(s):
Zachary Wintrob
Geoffrey Brown
Meir Wetzler
Alice Ceacareanu
Purpose: Metformin survival benefit has long been documented in solid tumor bearing patients
with diabetes mellitus (DM). Furthermore, in vitro studies on acute myelogenous leukemia
(AML) cells suggest metformin decreases proliferation and induces apoptosis. Clinical benefit of
metformin in hematologic cancers, however, remains unobserved because it is routinely
substituted by insulin. This substitution aims to minimize lactic acidosis risk from frequent
contrast dye administration, which results in decreased renal clearance. While lactic acidosis is
immediately fatal, insulin leads to poorer outcomes from enhanced leukemic cell proliferation.
Thus, our study purpose is to determine the safety of metformin reinitiation in this population.
Methods: This study was approved by the Institutional Review Board (EDR 193511). Clinical
and outcomes data for all patients both diagnosed with AML (January 2003 through December
2012) and having baseline DM were provided by the hospitals Leukemia Group. Additional
information including treatment, laboratory, and computed tomography scans were abstracted
from individual electronic medical records. We are currently in progress of computing individual
renal clearance versus time profiles using the Cockcroft Gault equation. This will serve as the
independent variable in a previously described two compartment structural pharmacokinetic
(PK) model of metformin proven to accurately predict both the immediate and sustained release
formulations drug concentration versus time profiles at all prescribed doses. We will utilize this
published model to simulate, by nonparametric bootstrap (n of 1000), PK profiles of metformin
both with and without the window of metformin discontinuation recommended by the contrast
dye package insert. Lactic acidosis will be considered possible if the simulated metformin
plasma concentration exceeds 5 milligrams per liter, the upper limit proposed by the literature.
Such approach would evaluate the actual risk for lactic acidosis induced by the administration of
contrast dye if insulin would not be substituted for metformin.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-395
Title: A comparison of in vitro platelet inhibition of ticagrelor in obese and nonobese volunteers
Primary Author: Arthur Fyles, University at Buffalo School of Pharmacy and Pharmaceutical
Sciences, NY;
Email: artfyles@gmail.com
Additional Author(s):
Nicholas Norgard
Scott Monte
Gina Sutedja
Purpose: Obesity is a risk factor for cardiovascular morbidity and mortality due to
atherothrombotic events and has been associated with a poor pharmacodynamic response to the
P2Y12 inhibitor clopidogrel. It is unknown whether obesity effects the pharmacodynamic profile
of the ticagrelor, a direct acting P2Y12 inhibitor. The objective of this study is to determine if
there is a correlation between body mass index (BMI) and the in vitro effects of ticagrelor,
another P2Y12 inhibitor.
Methods: Prior to initiation, the study will be submitted to the Institutional Review Board for
approval. The study will compare in vitro ticagrelor pharmacodynamics in two groups of
subjects: 1) healthy volunteers with a BMI 18-30 and 2) obese individuals with a BMI >35
scheduled to undergo bariatric surgery. Pharmacodynamic data of obese patients have been
collected in a prior study. Blood samples from study subjects will be incubated in 0 to 100
nanomolar concentrations of ticagrelor. Platelet aggregation will then be measured at 6 minutes
of exposure to ADP using whole blood impedance aggregometry. Dose response curves will be
compared between groups using Graphpad Prism 6 software.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-396
Title: Characterizing antibiotic prescribing patterns for acute respiratory tract infections in
infants and young children with and without cystic fibrosis
Primary Author: Aubrey Gawron, University at Buffalo School of Pharmacy and
Pharmaceutical Sciences, Buffalo;
Email: aagawron@buffalo.edu
Additional Author(s):
Justin C. Kanaley
Drucy S. Borowitz
William A. Prescott
Purpose: Bacteria and viruses are both common causes of respiratory tract infection in patients
with cystic fibrosis (CF). Effectively treating pulmonary bacterial infection in CF is important
for preserving lung function. However, because routine exposure to antibiotics is known to
increase the risk for developing bacterial resistance later in life, judicial use of these antibiotics is
necessary. The purpose of this study is to characterize antibiotic prescribing patterns in infants
and young children with and without CF in order to provide practical information to help
clinicians make well-informed decisions regarding antibiotic treatment in the young CF
population.
Methods: This was a multicenter retrospective medical record review designed to investigate the
mean/median number of antibiotic courses in CF infants/young children compared to
infants/young children without CF who were less than two years of age for upper (URTI) and/or
acute lower respiratory tract infections (LRTI). This study was conducted at 2 CF centers and 2
outpatient pediatrician offices in 2 cities within the same geographic region. Subjects who were
younger than 2 years of age during the period of August 1, 2003 and July 31, 2012 were eligible
for inclusion. Subjects were included if they had at least one office visit or call to the prescriber
(encounter) associated with a chief complaint suggestive of a URTI) or LRTI and/or at least one
URTI/LRTI ICD9 codes. All statistical analyses were conducted with SAS version 9.3 (Cary,
NC) assuming a two-sided alpha of 0.05. Students t-test was used to compare
continuous/parametric data and the Mann-Whitney test was used to compare
ordinal/nonparametric data between the groups. The University of Rochester Institutional
Review Board and the University at Buffalo Health Sciences Children and Youth Institutional
Review Board approved this study on 1/29/2013 and 6/11/2013, respectively.
Results: Seventy-five subjects were included: 15 with CF and 60 without CF (site #1 results
complete and presented herein). At the initial visit, CF and non-CF subjects ranged in age from
0.06-1.91 and 0.05-1.8 years, respectively. There were 4.9 encounters per subject in the CF
group verses 2.6 encounters per subject in the non-CF group (p-value=0.0005). In the CF group,
53 (71.6 percent) encounters resulted in an antibiotic being prescribed, while 14 (9.1 percent)
encounters in the non-CF group resulted in an antibiotic prescription. The mean number of
antibiotics prescribed per encounter in the CF group was 0.72 plus/minus 0.45 and in the non-CF
group was 0.09 plus/minus 0.29 (p-value=0.0001). The median number of antibiotics prescribed
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
per encounter in the CF group was 1 (range, 0 to 1) and in the non-CF group was 0 (range, 0 to
1). Of the 53 antibiotic prescriptions in the CF group, 51 (96.2 percent) were for CF with
pulmonary manifestations. The most commonly prescribed antibiotics in the CF group were
sulfamethoxazole/trimethoprim and amoxicillin/clavulanate, while the most commonly
prescribed antibiotic in the non-CF group was amoxicillin.
Conclusion: URTI/LRTI encounters among infants/young children with CF were 8-times more
likely than encounters among non-CF subjects to result in an antibiotic prescription. This is not
an unexpected finding given that bacterial colonization is common in the CF population, in
whom antibiotic treatment is appropriate. When antibiotics were utilized in symptomatic infants
and young children with CF, they were directed against the most commonly isolated pathogens
of the studied age group, were dosed appropriately, and were used for adequate duration.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-397
Title: Use of lipid lowering medications among human immunodeficiency virus (HIV)-infected
patients with substance related disorder
Primary Author: Jie Gu, University at Buffalo, School of Pharmacy and Pharmaceutical
Sciences/ New York;
Email: jiegu@buffalo.edu
Additional Author(s):
Qing Ma
Ran Zhou
Purpose: (1) To investigate the association between lipid lowering therapies (LLT) and
substance related disorder (SRD) in human immunodeficiency virus (HIV) patients. (2) To
evaluate the association between LLT and protease inhibitors (PIs).
Methods: The study cohorts were selected from four different institutions: Cleveland (CL),
Miami (MI), New York City (NY) and Rochester (RO) during 2003 to 2007 through the TDM
database (TDM.buffalo.edu) in June 2011. The codes of International Classification of Disease9th Edition were used to identify study subjects with HIV/acquired immune deficiency. The
National Drug Codes were not only used to identify the subjects using LLT, but also were used
to distinguish different classes of LLT and highly active antiretroviral therapy (HAART). The
classification of SRD group was based upon individual reporting, and we investigated the
association between LLT and SRD status as well as the association between LLT and PIs in the
main analyses. Subgroup analyses targeting the LLT group were performed subsequently to
confirm the main analyses results and to further evaluate the association between HAART and
SRD status. Statins and fibric acid derivatives utilizations were the particular interests of this
study.
Results: A total of 276 (n=276) HIV+ patients were enrolled in the study; the sample included a
total of 130 (n=130) SRD+ patients (n=38 on LLT vs. n=92 on none LLT) and a total of 146
(n=146) SRD- patients (n=75 on LLT vs. n=71 on none LLT). Although main analyses have
demonstrated a statistically significant relationship between LLT and SRD status (29.23% vs.
51.37%, p=0.003), the finding was not observed in the subgroup analyses. Contrary to the preexisting literatures, the non-nucleoside reverse transcriptase inhibitor (NNRTI) was associated
with higher statins and fibrates use compared to the PI-based regimens (64.29% vs. 31.20%,
p=0.0001). However, the results of subgroup analyses were not able to support such observation
(90.63% vs. 89.02%, p=1.00). Statins were the most commonly prescribed medication (66%),
followed by fibric acid derivatives (24%), omega-3 fatty acid (5%), cholesterol absorption
inhibitor (3%) and nicotinic acid (2%) regardless of the SRD statuses and HAART classes. The
SRD+ subjects were more likely to smoke and use alcohol, cocaine and methadone (87.69% vs.
26.71%, p<0.0001; 36.15% vs. 22.60%, p=0.019; 21.54% vs. 0.68%, p<0.0001; 20.77% vs.
10.27%, p=0.0241) in addition to receive more LPV therapies compared to the SRD- patients
(25% vs. 7.79%, p=0.022).
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
Conclusion: SRD status and PIs both had no impacts on LLT utilization.
ASHP 2013 Midyear Clinical Meeting
Student Poster Abstracts
1-398
Title: Reversing roles: students present a continuing education program on diabetic survival
skills counseling
Primary Author: Carol Hanna, Arnold & Marie Schwartz College of Pharmacy and Health
Sciences, New York;
Email: carol.hanna@my.liu.edu
Additional Author(s):
Mariya Elterman
Johnny Wong
Aleksandr Rozovskiy
Elaena Quattrocchi
Purpose: Providing appropriate diabetes education is essential in helping diabetics manage their
disease and incorporate the necessary skills into their daily activities. This is one component of a
continuing education program that was delivered by pharmacists in conjunction with student
pharmacists. The program was designed to enhance pharmacists knowledge and analyze the
effectiveness of student pharmacists as educators. Information was delivered by lecture, video
presentation, and a hands-on workshop. Pharmacists were evaluated on their knowledge about
basic diabetes survival skills, counseling points, and ability to use blood glucose meters and
insulin pens, before and after the program to assess for improvement.
Methods: The continuing education program was held on September 22, 2013. The pharmacists
were provided with a preliminary, anonymous, electronic audience response survey regarding
counseling practices and general diabetes knowledge points before each lecture and workshop.
This program was unique in that faculty members trained pharmacists to help patients manage
their diabetes through lecturing and educational videos that were developed by the faculty
member and students. The student pharmacists created scripts for and acted out all scenarios in
the videos shown. The series of educational videos created focused on counseling diabetics on
survival skills, including how pharmacists should counsel newly diagnosed type 1 diabetics,
blood glucose monitoring, hypoglycemia and its treatment, traveling with diabetes, and
preventing an insulin medication error involving U-500 regular insulin. The next portion of the
program involved a hands-on workshop, during which the pharmacists were given a chance to
demonstrate their ability to use a blood glucose meter and insulin pen. Student pharmacists
facilitated the work