Chapters 16, and 27
advertisement
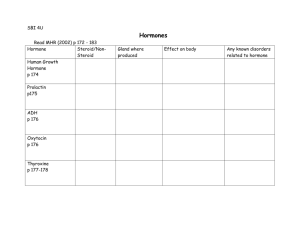
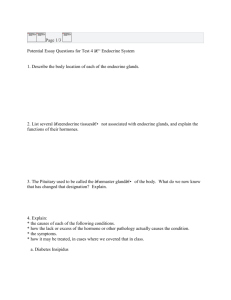
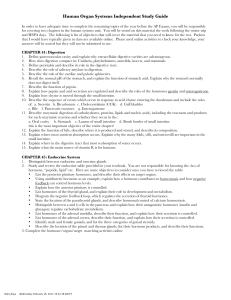
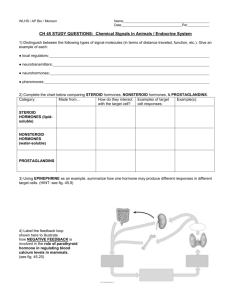
Objectives – Ch 16 The Endocrine System: An Overview 1. Define an endocrine gland, and list the major endocrine glands of the body and their locations. Hormones 2. Define a hormone, and describe the chemical categories of hormones. 3. Explain the relationship of hormones to target cells, and the types of changes that result in target cells in response to hormone stimulation. 4. Describe the second messenger systems used by amino acid-based hormones. 5. Explain the mechanism of intracellular activation used by steroid hormones and thyroid hormone. 6. Examine the factors that determine target cell activation, and compare how the cell uses up-regulation and down-regulation to alter its responsiveness to hormones. 7. Identify the factors that affect circulating hormone concentration, and the differences in the time required for the effects of hormones to be seen in target cells. 8. Underscore the three types of hormone interaction on target cells. 9. Discuss the three types of stimuli that promote or inhibit the release of hormones, and the effect of nervous system modulation. Major Endocrine Organs 10. List the hormones produced by the major endocrine organs, the factors controlling their release, and their effects on target cells. Other Hormone-Producing Structures 11. Name the hormones produced by other organs of the body, their source, and effects. Developmental Aspects of the Endocrine System 12. Indicate the embryonic origins of endocrine glands and the chemical classes of hormones produced by each embryonic tissue. 13. Describe environmental effects on hormone secretion or activity. 14. Explain the age-related changes that occur to endocrine organ structure or secretion. I. The Endocrine System: An Overview (p. 604; Fig. 16.1) A. Endocrine glands are ductless glands that produce and release hormones to the blood through diffusion. B. Endocrine glands may be strictly endocrine, such as the pituitary, thyroid, parathyroid, adrenal, pineal and thymus; or they may be organs that have hormone production as one of many functions, such as the pancreas, gonads, hypothalamus, and others. II. Hormones (pp. 605–611; Figs. 16.2–16.4) A. Chemistry of Hormones (p. 605) 1. Hormones are long-distance chemical signals that are secreted by the cells to the extracellular fluid and regulate the metabolic functions of other cells. 2. Most hormones are amino acid based, but gonadal and adrenocortical hormones are steroids, derived from cholesterol. B. Mechanisms of Hormone Action (pp. 605–609; Figs. 16.2–16.3) 1. Hormones typically produce changes in membrane permeability or potential, stimulate synthesis of proteins or regulatory molecules, activate or deactivate enzymes, induce secretory activity, or stimulate mitosis. 2. Nearly all amino acid-based hormones exert their effects through an intracellular second messenger that is activated when a hormone binds to a membrane receptor. 3. Steroid hormones are lipid soluble and diffuse into the cell, where they bind to intracellular receptors, migrate to the nucleus, and activate specific target sequences of DNA. C. Target Cell Specificity (p. 609) 1. Cells must have specific membrane or intracellular receptors to which hormones can bind. 2. Target cell response depends on three factors: blood levels of the hormone, relative numbers of target cell receptors, and affinity of the receptor for the hormone. 3. Target cells can change their sensitivity to a hormone by changing the number of receptors. D. Half-Life, Onset, and Duration of Hormone Activity (pp. 609–610) 1. The concentration of a hormone reflects its rate of release, and the rate of inactivation and removal from the body. 2. The half-life of a hormone is the duration of time a hormone remains in the blood, and is shortest for water-soluble hormones. 3. Target organ response and duration of response vary widely among hormones. E. Interaction of Hormones at Target Cells (p. 610) F. 1. Permissiveness occurs when one hormone cannot exert its full effect without another hormone being present. 2. Synergism occurs when more than one hormone produces the same effects in a target cell, and their combined effects are amplified. 3. Antagonism occurs when one hormone opposes the action of another hormone. Control of Hormone Release (pp. 610–611; Fig. 16.4) 1. Most hormone synthesis and release is regulated through negative feedback mechanisms. 2. Endocrine gland stimuli may be humoral, neural, or hormonal. 3. Nervous system modulation allows hormone secretion to be modified by the nervous stimulation in response to changing body needs. III. Major Endocrine Organs (pp. 611–636; Figs. 16.5–16.18; Tables 16.1–16.3) A. The Pituitary Gland (Hypophysis) (pp. 611–618; Figs. 16.5–16.6; Table 16.1) 1. The pituitary gland is connected to the hypothalamus via a stalk, the infundibulum, and consists of two lobes: the anterior pituitary, or adenohypophysis, and the posterior pituitary, or neurohypophysis. 2. There are six adenohypophyseal hormones and one prohormone. a. Growth hormone (GH) stimulates body cells to increase in size and divide. b. Thyroid stimulating hormone (TSH) is a tropic hormone that stimulates normal development and secretion of the thyroid gland. c. Adrenocorticotropic hormone (ACTH) stimulates the adrenal cortex to release corticosteroid hormones. d. Follicle-stimulating hormone (FSH) stimulates gamete production. e. Leutinizing hormone (LH) promotes ovulation in females and production of gonadal hormones. f. Prolactin stimulates milk production in females, and may enhance testosterone in males. g. Pro-opiomelanocortin (POMC) is a prohormone that is the source of adrenocorticotropic hormone and two opiates. 3. Two neurohormones are synthesized by the hypothalamus and secreted by the posterior pituitary. a. Oxytocin acts on the smooth muscle of the uterus and breast to cause uterine contractions during childbirth and milk let-down during nursing. b. Antidiuretic hormone (ADH) acts on kidney tubules to promote increased water reabsorption. B. The Thyroid Gland (pp. 619–623: Figs. 16.7–16.9; Table 16.2) 1. The thyroid gland consists of hollow follicles with follicle cells that produce thyroglobulin, and parafollicular cells that produce calcitonin. 2. Thyroid hormone consists of two amine hormones: thyroxine (T 4) and triiodothyronine (T3), that act on all body cells to increase basal metabolic rate and body heat production. 3. Calcitonin is a peptide hormone that lowers blood calcium by inhibiting osteoclast activity, and stimulates Ca21 uptake and incorporation into the bone matrix. C. The Parathyroid Glands (pp. 623–624; Figs. 16.10–16.11) 1. The parathyroid glands contain chief cells that secrete parathyroid hormone, or parathormone. D. The Adrenal (Suprarenal) Glands (pp. 624–630; Figs. 16.12–16.15; Table 16.3) 1. The adrenal glands, or suprarenal glands, consist of two regions: an inner adrenal medulla and an outer adrenal cortex. 2. The adrenal cortex produces corticosteroids from three distinct regions: the zona glomerulosa, the zona fasciculata, and the zona reticularis. a. Mineralocorticoids, mostly aldosterone, are essential to regulation of electrolyte concentrations of extracellular fluids. b. Aldosterone secretion is regulated by the renin-angiotensin mechanism, fluctuating blood concentrations of sodium and potassium ions, and secretion of ACTH. c. Glucocorticoids are released in response to stress through the action of ACTH. d. Gonadocorticoids are mostly weak androgens, which are converted to testosterone and estrogens in the tissue cells. 3. The adrenal medulla contains chromaffin cells that synthesize epinephrine and norepinephrine. E. The Pancreas (pp. 630–633; Figs. 16.16–16.18) 1. The pancreas is a mixed gland that contains both endocrine and exocrine gland cells. a. Glucagon targets the liver where it promotes glycogenolysis, gluconeogenesis, and release of glucose to the blood. b. Insulin lowers blood sugar levels by enhancing membrane transport of glucose into body cells. F. The Gonads (pp. 633–634) 1. The ovaries produce estrogens and progesterone. 2. The testes produce testosterone. G. The Pineal Gland (pp. 634–636) 1. Secretes melatonin, a hormone derived from serotonin, in a diurnal cycle. 2. Indirectly receives input from the visual pathways in order to determine the timing of day and night. H. The Thymus (p. 636) 1. IV. The thymus produces thymopoietin, thymic factor, and thymosin, which are essential for the development of T lymphocytes and the immune response. Other Hormone-Producing Structures (p. 636; Table 16.4) A. The atria of the heart contain specialized cells that secrete atrial natriuretic factor resulting in decreased blood volume, blood pressure, and blood sodium concentration. B. The gastrointestinal tract contains enteroendocrine cells throughout the mucosa that secrete hormones to regulate digestive functions. C. The placenta secretes estrogens, progesterone, and human chorionic gonadotropin, which act on the uterus to influence pregnancy. D. The kidneys produce erythropoietin, which signals the bone marrow to produce red blood cells. E. The skin produces cholecalciferol, an inactive form of vitamin D3. F. Adipose tissue produces leptin, which acts on the CNS to produce a feeling of satiety, and resistin, an insulin antagonist. V. Developmental Aspects of the Endocrine System (pp. 636–637, 640) A. Endocrine glands derived from mesoderm produce steroid hormones; those derived from ectoderm or endoderm produce amines, peptides, or protein hormones. Objectives – Ch 27 Male Reproductive System 1. Explain the function of the testes. Describe the function of the penis. 2. List and discuss the function of the male accessory ducts and glands. Physiology of the Male Reproductive System 3. Define the male sexual response. Describe the process of spermatogenesis. 4. Identify the hormonal regulation of the male reproductive function. 5. Name the male secondary sex characteristics and explain the role of testosterone in their formation. Female Reproductive System 7. Indicate the function of the ovaries. 8. Describe the function of the female reproductive duct system. 9. Identify the function of the female external genitalia. 10. Discuss the mammary glands and breast cancer. Physiology of the Female Reproductive System 11. Explain the process of oogenesis. Discuss the ovarian cycle including its three phases and their major events. 12. Indicate the hormonal interactions of the ovarian cycle. 13. Describe the uterine cycle. 14. Identify the effects of estrogen and progesterone on the development of structures and physiological processes other than the ovarian cycle. Sexually Transmitted Diseases 15. Discuss the causative agents and modes of transmission of gonorrhea, syphilis, chlamydia, genital warts, and genital herpes. Developmental Aspects of the Reproductive System: Chronology of Sexual Development 16. Identify what determines sex. 17. Discuss the process of sexual differentiation as it occurs in the developing embryo. 18. Explain the descent of the gonads. 19. Define and discuss puberty and menopause. I. Anatomy of the Male Reproductive System (pp. 1064–1070, Figs. 27.1–27.4) A. The scrotum is a sac of skin and superficial fascia that hangs outside the abdominopelvic cavity at the root of the penis and houses the testes. 1. Provides an environment three degrees below the core body temperature. 2. Responds to temperature changes. B. The testes are the primary reproductive organ of the male, producing both sperm and testosterone. 1. The testes are divided into lobules with seminiferous tubules inside, where sperm are produced. 2. Interstitial cells are found in the connective tissue surrounding the seminiferous tubules and produce testosterone. C. The penis is the copulatory organ, designed to deliver sperm into the female reproductive tract. 1. The penis is made of an attached root, a free shaft or body that ends in the glans. 2. The prepuce, or foreskin, covers the penis and may be slipped back to form a cuff around the glans. 3. Internally the penis contains the corpus spongiosum and the corpora cavernosum, two erectile tissues. D. The Male Duct System 1. The epididymis consists of a highly coiled tube that provides a place for immature sperm to mature and to be expelled during ejaculation. 2. The ductus deferens, or vas deferens, carries sperm from storage sites in the epididymis, through the inguinal canal, over the bladder, and into the ejaculatory duct. 3. The urethra is the terminal portion of the male duct system and carries both urine and sperm (not at the same time) to the exterior environment. E. Accessory Glands F. 1. The seminal vesicles lie on the posterior bladder wall and their alkaline secretion accounts for 60% of the volume of semen consisting of fructose, ascorbic acid, a coagulating enzyme (vesiculase), and prostaglandins. 2. The prostate gland is responsible for producing a milky, slightly acidic fluid containing citrate, several enzymes, and prostate-specific antigen, making up about one-third of the semen. 3. The bulbourethral glands, or Cowper’s glands, produce a thick, clear mucus prior to ejaculation that neutralizes any acidic urine in the urethra. Semen is a milky white, somewhat sticky mixture of sperm and accessory gland secretions that provides a transport medium for sperm. II. Physiology of the Male Reproductive System (pp. 1070–1079, Figs. 27.5–27.10) A. Male Sexual Response 1. Erection, enlargement, and stiffening of the penis results from the engorgement of the erectile tissues with blood triggered during sexual excitement. 2. Ejaculation is the propulsion of semen from the male duct system triggered by the sympathetic nervous system. B. Spermatogenesis is the series of events in the seminiferous tubules that produce male gametes (sperm or spermatozoa). 1. Meiosis consists of two consecutive nuclear divisions and the production of four daughter cells with half as many cells as a normal body cell. a. Meiosis I reduces the number of chromosomes in a cell from 46 to 23 by separating homologous chromosomes into different cells. b. Meiosis II resembles mitosis in every way, except the chromatids are separated into four cells. 2. Summary of Events in the Seminiferous Tubules a. Spermatogenesis begins when the spermatogonia divide to produce type A daughter cells that maintain the stem cell line, and type B daughter cells that get pushed toward the lumen to become primary spermatocytes and ultimately sperm. b. Each primary spermatocyte undergoes meiosis I to produce two secondary spermatocytes, which then undergo meiosis II to form spermatids. c. Spermiogenesis is a streamlining process that strips the spermatid of excess cytoplasm and forms a tail resulting in a sperm with a head, a midpiece, and a tail. d. The sustentacular cells, or Sertoli cells, form a blood-testis barrier that prevents membranebound antigens from escaping into the blood-stream. C. Hormonal Regulation of Male Reproductive Function 1. Brain-testicular axis refers to the relationship and interactions between the hypothalamus, anterior pituitary gland, and the testes. a. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which controls the release of the anterior pituitary hormones follicle-stimulating hormone (FSH) and luteinizing hormone (LH) in males. b. FSH indirectly stimulates spermatogenesis. c. LH, also called interstitial cell-stimulating hormone (ICSH), stimulates the interstitial cells to produce testosterone. d. Locally testosterone acts as a final trigger for spermatogenesis. e. T estosterone inhibits hypothalamic release of GnRH and acts directly on the anterior pituitary gland to inhibit gonadotropin release f. Inhibin is produced by the sustentacular cells and released when sperm count is high. 2. Mechanism and Effects of T estosterone Activity a. T estosterone is synthesized from cholesterol and exerts its effects by activating specific genes to be transcribed. b. T estosterone targets accessory organs (ducts, glands, and penis) causing them to grow and assume adult size and function. c. T estosterone induces male secondary sex characteristics: pubic, axillary, and facial hair, deepening of the voice, thickening of the skin and increase in oil production, and an increase in bone and skeletal muscle size and mass. III. Anatomy of the Female Reproductive System (pp. 1079–1087, Figs. 27.11–27.18) A. The ovaries are the primary reproductive organs of the female. 1. The ovaries produce the female gametes (ova or egg) and the sex hormones (estrogens and progesterone). 2. The paired ovaries are found on either side of the uterus and are held in place by several ligaments. 3. Saclike structures called ovarian follicles consist of an immature egg, called an oocyte, encased by one or more layers of different cells. 4. Follicles at different stages are distinguished by their structure as primordial follicles, primary follicles, secondary follicles, and Graafian or vesicular follicles. 5. Ovulation occurs each month in adult women when one of the maturing follicles ejects its oocyte from the ovary. 6. The ruptured follicle transforms into a glandular structure called the corpus luteum, which eventually degenerates. B. The Female Duct System 1. The uterine tubes, or fallopian tubes or oviducts, form the beginning of the female duct system, receive the ovulated oocyte, and provide a site for fertilization to take place. 2. The uterus is a hollow, thick-walled muscular organ that functions to receive, retain, and nourish a fertilized ovum. a. The uterus is supported by the mesometrium, the lateral cervical ligaments, the uterosacral ligaments, and the round ligaments. b. The wall of the uterus is composed of three layers: the perimetrium, the myometrium, and the endometrium. 3. The vagina provides a passageway for delivery of an infant and for menstrual blood, and also receives the penis and semen during sexual intercourse. C. The external genitalia, also called the vulva or pudendum, include the mons pubis, labia, clitoris, and structures associated with the vestibule. D. Mammary glands are present in both sexes but usually function only in females to produce milk to nourish a newborn baby. 1. Mammary glands are modified sweat glands that are really part of the integumentary system. 2. Breast cancer usually arises from the epithelial cells of the ducts and grows into a lump in the breast from which cells eventually metastasize. IV. Physiology of the Female Reproductive System (pp. 1088– 1096, Figs. 27.19–27.22, Table 27.1) A. Oogenesis is the production of female gametes called oocytes, ova, or eggs. 1. A female’s total egg supply is determined at birth and the time in which she releases them extends from puberty to menopause. 2. In the fetal period the oogonia multiply rapidly by mitosis, become primordial follicles, and then become primary follicles that begin the first meiotic division. 3. After puberty a few oocytes are activated each month, but only one will continue meiosis I, ultimately producing two haploid cells, a polar body, and a secondary oocyte. 4. The secondary oocyte stops in metaphase II and if a sperm penetrates it, it will complete meiosis II, producing a second polar body and a large ovum. B. The ovarian cycle is the monthly series of events associated with the maturation of the egg. 1. The follicular phase is the period of follicle growth typically lasting from day 1 to 14. 2. Ovulation occurs when the ovary wall ruptures and the secondary oocyte is expelled. 3. The luteal phase is the period of corpus luteum activity, days 14–28. C. Hormonal Regulation of the Ovarian Cycle 1. During childhood, the ovaries grow and secrete small amounts of estrogen that inhibit the release of GnRH until puberty, when the hypothalamus becomes less sensitive to estrogen and begins to release GnRH in a rhythmic manner. 2. Hormonal Interactions During the Ovarian Cycle a. On day 1 of the cycle, levels of GnRH rise and stimulate increased production and release of FSH and LH. b. FSH and LH stimulate follicle growth and maturation, and estrogen secretion. c. Rising levels of estrogen in the plasma exert negative feedback on the anterior pituitary, inhibiting release of FSH and LH. d. Estrogen exerts positive feedback on the anterior pituitary resulting in a burst of LH triggering ovulation and transforming the ruptured follicle into the corpus luteum. e. Rising plasma levels of progesterone and estrogen exert a negative feedback on LH and FSH release. f. LH levels fall and luteal activity ends; the corpus luteum degenerates dropping the levels of estrogen and progesterone and the cycle starts again. D. The uterine (menstrual) cycle is a series of cyclic changes that the uterine endometrium goes through each month in response to changing levels of ovarian hormones in the blood. 1. The menstrual phase takes place on days 1–5 typically, and is the time when the endometrium is shed from the uterus. 2. The proliferation phase (days 6–14) is the time in which the endometrium is rebuilt once again becoming velvety, thick, and well vascularized. 3. The secretory phase (days 15–28) is the phase in which the endometrium prepares for implantation of an embryo. E. Extrauterine Effects of Estrogens and Progesterone 1. Rising estrogen levels promote oogenesis and follicle growth in the ovary, as well as growth and function of the female reproductive structures. 2. Estrogens also cause the epiphyses of the long bones to close during growth spurts in puberty. 3. The estrogen-induced secondary sex characteristics of females include growth of breasts, increased deposition of subcutaneous fat in the hips and breast, widening and lightening of the pelvis, growth of pubic and axillary hair, and metabolic changes. 4. F. Progesterone works with estrogen to establish and help regulate the uterine cycle, and promotes changes in cervical mucus. In the female sexual response, the clitoris, vaginal mucosa, and breasts become engorged with blood; the nipples erect; vestibular glands increase in activity; and the final phase is orgasm. V. Sexually Transmitted Diseases (pp. 1096–1097, Fig. 27.23) A. Gonorrhea is caused by Neisseria gonorrhoeae bacteria, which invade the mucosae of the reproductive and urinary tracts. B. Syphilis is caused by Treponema pallidum, a bacteria that easily penetrate intact mucosae and abraded skin, and enter the lymphatics and the bloodstream. C. Chlamydia is the most common sexually transmitted disease in the U.S. and is caused by the bacteria Chlamydia trachomatis. D. Genital warts are caused by a group of about 60 viruses known as the human papillomavirus (HPV). E. Genital herpes is generally caused by the herpes simplex virus type 2, which is transferred via infectious secretions. VI. Developmental Aspects of the Reproductive System: Chronology of Sexual Development (pp. 1097–1102, Figs. 27.24– 27.26) A. Embryological and Fetal Events 1. Sex is determined by the sex chromosomes at conception; females have two X chromosomes and males have an X and a Y chromosome. 2. Sexual Differentiation of the Reproductive System a. The gonads of both males and females begin to develop during week 5 of gestation. b. During week 7 the gonads begin to become testes in males, and in week 8 they begin to form ovaries in females. c. The external genitalia arise from the same structures in both sexes, with differentiation occurring in week 8. 3. About two months before birth the testes begin their descent toward the scrotum, dragging their nerve supply and blood supply with them. B. Puberty is the period of life, generally between the ages of 10 and 15 years, when the reproductive organs grow to adult size and become functional. C. Ovarian function declines gradually with age; menstrual cycles become more erratic and shorter until menopause, when ovulation and menstruation stop entirely.