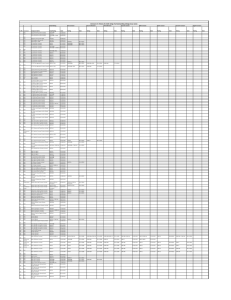
years of experience by field in intensive care specialties
advertisement
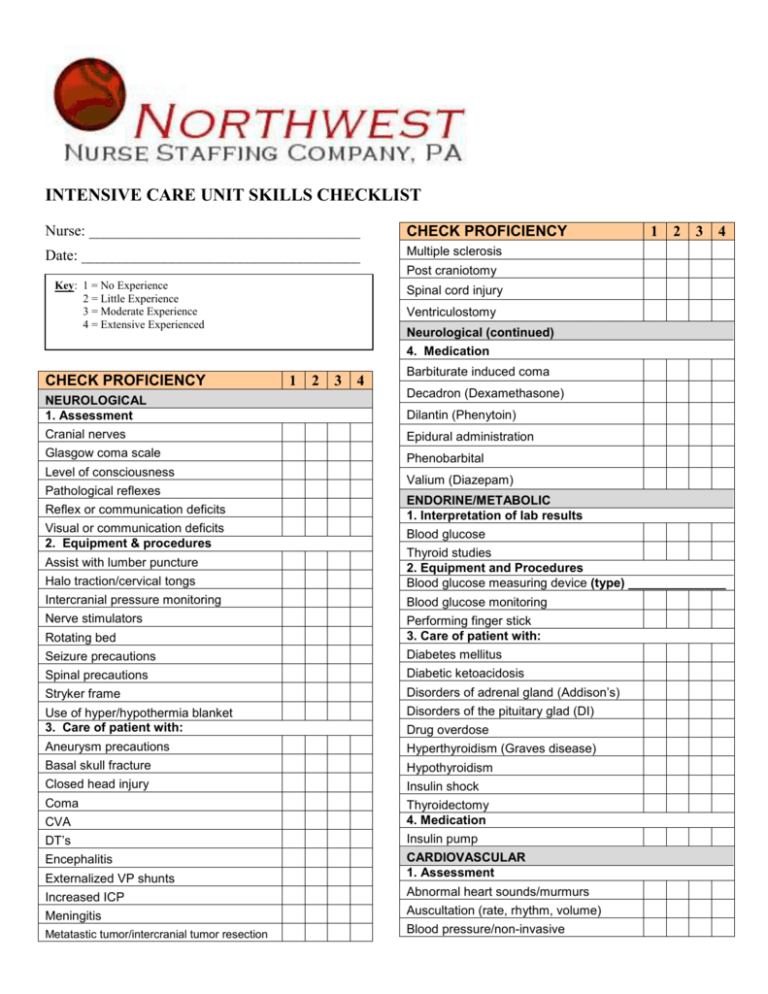
INTENSIVE CARE UNIT SKILLS CHECKLIST Nurse: ____________________________________ CHECK PROFICIENCY Date: _____________________________________ Multiple sclerosis 1 2 3 4 Post craniotomy Key: 1 = No Experience 2 = Little Experience 3 = Moderate Experience 4 = Extensive Experienced Spinal cord injury Ventriculostomy Neurological (continued) 4. Medication CHECK PROFICIENCY NEUROLOGICAL 1. Assessment 1 2 3 4 Barbiturate induced coma Decadron (Dexamethasone) Dilantin (Phenytoin) Cranial nerves Epidural administration Glasgow coma scale Phenobarbital Level of consciousness Pathological reflexes Valium (Diazepam) Reflex or communication deficits ENDORINE/METABOLIC 1. Interpretation of lab results Visual or communication deficits 2. Equipment & procedures Blood glucose Halo traction/cervical tongs Thyroid studies 2. Equipment and Procedures Blood glucose measuring device (type) ______________ Intercranial pressure monitoring Blood glucose monitoring Nerve stimulators Rotating bed Performing finger stick 3. Care of patient with: Seizure precautions Diabetes mellitus Spinal precautions Diabetic ketoacidosis Stryker frame Disorders of adrenal gland (Addison’s) Use of hyper/hypothermia blanket 3. Care of patient with: Disorders of the pituitary glad (DI) Aneurysm precautions Hyperthyroidism (Graves disease) Basal skull fracture Hypothyroidism Closed head injury Insulin shock Coma Thyroidectomy 4. Medication Assist with lumber puncture CVA DT’s Drug overdose Externalized VP shunts Insulin pump CARDIOVASCULAR 1. Assessment Increased ICP Abnormal heart sounds/murmurs Meningitis Auscultation (rate, rhythm, volume) Blood pressure/non-invasive Encephalitis Metatastic tumor/intercranial tumor resection INTENSIVE CARE UNIT SKILLS CHECKLIST CHECK PROFICIENCY 1 2 3 4 CHECK PROFICIENCY Doppler Permanent Pulses/circulation checks 2. Interpretation of lab results Temporary Transthoracic (epicardial) Cardiac enzymes & isoenzymes Ventricular assist device (RVAD or LVAD) Coagulation studies 3. Equipment & procedures Assist with: 4. Care of patient with: Arterial line insertion Central line insertion Open chest emergency CARDIOVASCULAR (continued) Abdominal aortic aneurysm repair Acute MI Cardiac arrest Cardiac tamponade Congestive heart failure (CHF) EP study & ablation PA catheter/Swan Ganz Insertion Heart transplant Pericardocentesis Immediate post open-heart surgery Transesophageal echocardiogram Infective endocarditis Automatic internal cardioverter defibrillator Myocardial contusion Cardioversion Pericarditis CAVH-D Hemodynamic monitoring: Post AICD insertion Post arthrectomy (DCA) Cardiac index Cardiac output CVP monitoring Femoral artery sheath removal MAP PA/Swan-Ganz Post commssurotomy, valve repair/replacement Post intracoronary stent placement Post Percutaneous ballone valvuloplasty Post rotoblade Pre/post angioplasty PCW pressure Pre/post cardiac cath 5. Medications PVR Amiodarone (Cordarone) Radial a-line Atropine SVO2 Bicarbonate SVR Bretylium (Bretylol) Intra aortic balloon pump Monitoring: 12 lead EKD interpretation Arrhythmia interpretation Lead placement Rhythm strip assessment Set up and rerun 12 lead EKD Pacemaker: External Digoxin (Lanoxin) Diltiazem (Cardizem) Dobutamine (Dobutrex) Dopamine (Intropin) Epinephrine (Adrenalin) Esmolol (Brevibloc) Inocor (Amrinone) Lidocaine (Xylocaine) Nipride (Nirtoprusside) 1 2 3 4 INTENSIVE CARE UNIT SKILLS CHECKLIST CHECK PROFICIENCY Procainamide (Pronestyl) 1 2 3 4 CHECK PROFICIENCY Reteplase recombinant (Retavase) Aspiration Strepokinase Laryngospasm TPA (Alteplase) Tension pneumothorax Verapamil (Calan, Isoptin, Verelan) PAIN MANAGEMENT Use of Pleurevac or Thoraclex drainage 1. Assessment of pain level tolerance 2. Care of patient with: Use of wather seal drainage O2 therapy & medication delivery systems: Ambu bag and mask Epidural anesthesia/analgesia ET Tube IV conscious sedation Face masks Patient controlled analgesia PULMONARY Nasal cannula 1. Assessment Trach collar Adventitious breath sounds Portable O2 tank Ventilator management: Rate and work of breathing 2. Interpretation of lab results External CPAP Arterial blood gases 1. Equipment & Procedures IMV Air leak troubleshooting: Pressure Support Medicinal chest tube removal PULMONARY (continued) Pleural chest tube removal Airway management devices/suctioning: High frequency jet ventilation PEEP Weaning modes & T-piece weaning 4. Care of patient with: Acute pneumonia ARDS Endotracheal tube/suctioning Chest Trauma Extubation COPD Nasal airway/suctioning Fresh Tracheostomy Oximetry Lobectomy Sputum specimen collection Lung transplant Tracheostomy/suctioning Pneumonectomy Assist with: Pulmonary edema/hypertension Bronchoscope Pulmonary embolism Chest tube insertion Status asthmaticus Emergency Trachoestomy Thoracotomy Thoracentesis Tuberculosis 2. Medications Establishing an airway: 1 2 3 Identification/intervention for respiratory complications: Assist with intubation Alupent (Metaproterenol sulfate) Oral airway insertion Aminophylline (Theophylline) 4 INTENSIVE CARE UNIT SKILLS CHECKLIST CHECK PROFICIENCY 1 2 3 4 CHECK PROFICIENCY Bronkosol (Isoetharine hydrochloride) Female Corticisteriods Male Ventolin (Albuterol) RENAL/GENITOURINARY Supra-pubic 4. Care of patient with: 1. Assessment Acute renal failure Arterio venous fistula/shunt CAVH Dialysis Fluid balance 2. Interpretation of lab results Hemodialysis BUN & creatinine Peritoneal dialysis Electrolytes 3. Equipment & procedures Renalrejection syndrome Bladder irrigations Urinary diversion (ileal conduit nephrostomy) Insertion & care of straight & Foley catheter: Urinary tract infection Nephrectomy TURP 3-way Foley Total Number of Years in Intensive Care Unit: _____________________ Field YEARS OF EXPERIENCE BY FIELD IN INTENSIVE CARE SPECIALTIES Years Medical Neurology Cardiothoracic Cardiovascular PACU Burn Neuro Coronary Care Age Group YEARS OF EXPERIENCE BY AGE GROUP Years Newborns (birth – 30 days) Infants (30 days – 1 year) Toddler (1-3 years) Preschooler (3-5 years) School Children (5-12 years) Adolescents (12-18 years) Young Adults (18-39 years) Middle aged adults (39-64 years) Senior Adults (64+ years) 1 2 3 4 INTENSIVE CARE UNIT SKILLS CHECKLIST The information I have provided is true and accurate to the best of my knowledge. I authorize Northwest Nurse Staffing to release this Skills Checklist to client hospitals as needed in relation to my employment. Print name: Signature: _________________________________ Date: _____________________________________