No01ClinicalRecords - College of Physical Therapists of BC
advertisement

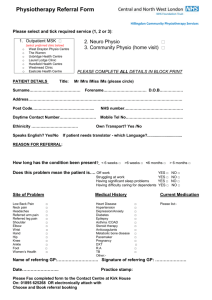
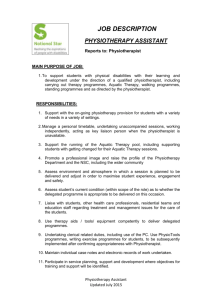
CLINICAL PRACTICE STATEMENT # 1 (Issued: January 2000 - Replaces: May, December 1999; April, October 1984) The practice of physiotherapy includes the recording of services provided to each client. To provide a complete record for communication and medical/legal purposes, the physiotherapist shall ensure that: 1. Client identification appears on every page. 1. Record the client's name and date of birth and/or identification number. 2. All pages of the record are numbered sequentially 3. All entries are legibly written and permanent, typewritten, or stored in a computer system. 1. If handwritten, use ballpoint ink. Pencil or felt tips are not considered permanent. 2. If stored in a computer system, the system must: 1. display the recorded information visually; 2. enter each client record via the client’s name and date of birth; 3. print a separate record for each client; 4. visually display and print the recorded information for each client in chronological order; 5. provide reasonable protection against unauthorized access; 6. provide automatic back-up and recovery of files, or otherwise protect against loss of, damage to, and inaccessibility of information; 7. maintain an audit trail which records the date and time of each entry and subsequent change, preserves the original content when changes are made and identifies the person making the entry and rendering the service. 4. All entries are dated and signed. 1. Record full date (preferably write the name of the month.) 2. Sign in full after the initial assessment entry of each physiotherapist. Subsequent chart entries shall be initialled or signed according to facility guidelines. The intent is to identify the writer of each entry. 3. Include entry of physiotherapist’s professional title where required. 5. Information is recorded at the time of the event or as soon as possible and in chronological sequence. 1. Omission of any significant information could be interpreted in a court of law as evidence that an event did not occur, e.g. skin test. 2. In settings where appointment times are not scheduled, it is recommended that the time treatment was provided be recorded. 6. Abbreviations, symbols and terminology used are recognized by professional peers. 7. Corrections or alterations are made according to standardized methods. 1. Draw a thin, straight line through each line of the incorrect/inaccurate entry leaving it legible. 2. Write the word ERROR in the margin beside the entry. 3. Date and initial. 4. Enter the correct information. 5. Date and sign the correct information. 8. The minimum documentation contains: 1. Client identification; 2. Name of referring practitioner if referral is received; 3. Assessment: Documentation needed in the client record. KEY: R - Required - Rec.- Recommended 1. Subjective History: R - Notation of presenting symptoms, including location, quality and behaviour Rec. - Client’s treatment expectations R - History of presenting complaint including past history, treatment and response R - Pertinent medical history R - Pertinent X-ray and laboratory reports R - Relevant surgical history R - Medications R - Occupation R - Recreational activities R - Concurrent treatment 2. Objective Findings: R - Notation of physical findings relevant to the presenting symptoms, both measurable and observable Include as relevant, for example: ROM Muscle strength Specific tests Oedema Skin appearance Posture Gait analysis Functional ability Mental status – orientation to time, person, place and including inappropriate client behaviour and/or harassment of the therapist Cardio-respiratory status 3. R - Analysis – physical therapy diagnosis and major problems 4. The treatment plan for the client including the specific treatment protocol, an indication of whether, and to whom, treatments might be delegated, a record of any home treatments, the particulars of any referral, and any advice/education/warnings/ precautions given (may use copies of handouts provided to the client). 5. Subsequent treatment visits. Documentation needed if change in client status or treatment: R - Response to treatment. R - Subjective reassessment. R - Objective reassessment. R - Treatment provided, including advice. Rec. - Future treatment plan – if different from above. 6. Discharge summary. Documentation recommended: 1. Subjective history. 2. Objective history 3. Response to treatment. If not included, the last entry in the record will be considered as the discharge summary. 7. Statistical or other information required by law or employing agency. 1. Where a person receives a written referral from a medical or dental practitioner, a copy of the referral must be included in the treatment record. 2. The treatment record shall contain written evidence of any communication with referring health care practitioners or other third parties. 9. The reason for incomplete documentation is recorded, i.e. the client did not keep further appointments. 10. All client information is kept confidential. 1. No information is given about a client to a person other than the client or his or her representative except with the consent of the client or his or her representative or as required or allowed by law. 2. A physiotherapist is only required to appear in court when subpoenaed. 11. There is currently no statute of limitations in B.C. Physical Therapists working in hospitals do have the protection of the six year ultimate limitation period although hospital records are generally retained for 10 years from date of last admission. The College’s requirement for retention of records is a minimum of 6 years from the date of the last entry, with the exception of minors and newborns, which should be retained to the age of majority (19 years in BC) plus 6 years = 25 years. While this is a minimum standard, practitioners should assess their own practices and should be aware that there are circumstances in which the usual limitation period for personal injury of two years can be extended, particularly where the client is not immediately aware that an injury has occurred or where there is an allegation of sexual misconduct. If a registrant has concerns about specific cases, they should seek advice from their insurer or solicitor. 12. When the record is destroyed it is by effective shredding, burning, computer or video erasure. 13. Where facilities utilize "Charting by Exception" or "Clinical Pathways" procedures, copies of the related policies and procedures should be retained and all employees should receive orientations. Physical Therapist should be involved in formulating such policies and procedures to ensure that the minimal record keeping requirements are maintained. N.B.These standards are not applicable for group education/maintenance programs such as postnatal exercise classes, stroke clubs. References Record Security, Canadian College of Health Record Administrators The Record That Defends Its Friends, Care Communications, 1987 Standards for Clinical Documentation, unpublished paper, Karanne Stoutenburg,Liason to APMP from Health Record Association of B.C. Standards for Hospital Physiotherapy Services, CPA Standards of Practice re Physiotherapy Treatment Records, Board of Directors of Physiotherapy, Ontario, revised 1987.