Social fobi 2006-04
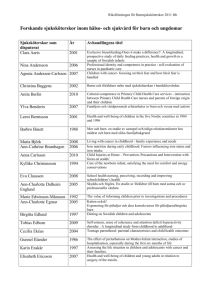
advertisement
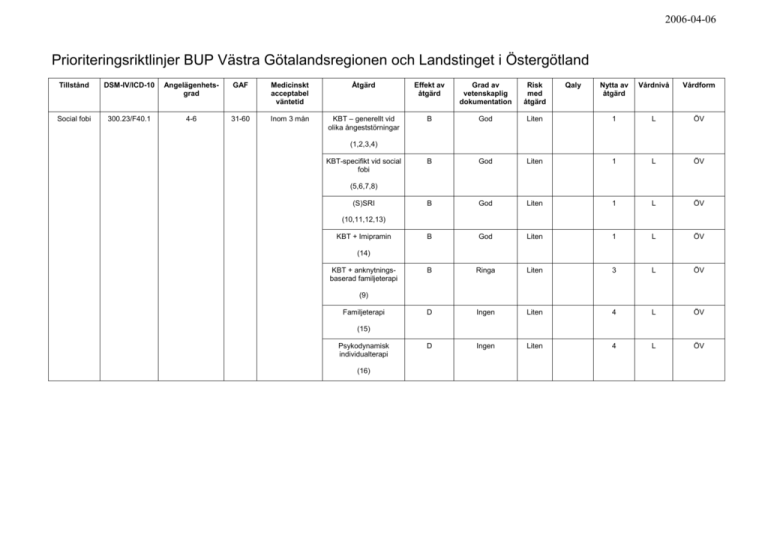
2006-04-06 Prioriteringsriktlinjer BUP Västra Götalandsregionen och Landstinget i Östergötland Tillstånd DSM-IV/ICD-10 Angelägenhetsgrad GAF Medicinskt acceptabel väntetid Åtgärd Effekt av åtgärd Grad av vetenskaplig dokumentation Risk med åtgärd Social fobi 300.23/F40.1 4-6 31-60 Inom 3 mån KBT – generellt vid olika ångeststörningar B God B Qaly Nytta av åtgärd Vårdnivå Vårdform Liten 1 L ÖV God Liten 1 L ÖV B God Liten 1 L ÖV B God Liten 1 L ÖV B Ringa Liten 3 L ÖV D Ingen Liten 4 L ÖV D Ingen Liten 4 L ÖV (1,2,3,4) KBT-specifikt vid social fobi (5,6,7,8) (S)SRI (10,11,12,13) KBT + Imipramin (14) KBT + anknytningsbaserad familjeterapi (9) Familjeterapi (15) Psykodynamisk individualterapi (16) 2006-04-06 Angelägenhetsgrad 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Omedelbart livshot Risk för mycket allvarlig skada, för tidig död, betydande invaliditet och outhärdlig situation Risk för allvarlig skada, bestående men eller mycket låg livskvalitet Risk för förväntad försämring/ej vidmakthållen funktion-ADL-nivå Risk för betydande olägenhet, ökad sjuklighet, förlängd sjukdomsperiod, sänkt livskvalitet Risk för olägenhet, skada, bestående men eller låg livskvalitet Sannolikt ökad risk för försämrad hälsoupplevelse eller icke optimal livskvalitet Möjligen ökad risk för sjuklighet, försämring av funktionsnivå eller livskvalitet Risk för sänkt livskvalitet enligt patientens uppfattning och vetenskap och beprövad kunskap inte motsäger detta Ingen risk för ökad sjuklighet, försämrad funktionsnivå eller försämrad livskvalitet. Global Assessment of Functioning (GAF) För uppskattning/bedömning av patientens vårdbehov (länk). Medicinskt acceptabel väntetid Inom 1 vecka GAF 1-30, inom 3 månader GAF 31-70. Åtgärd Allmänna behandlingsriktlinjer i öppenvård Behandlingsansatsen vid social fobi bör innehålla en för den enskilda patienten lämplig kombination av psykopedagogik, samarbete och konsultation med skola och ev. primärvård samt psykoterapi med barnet och föräldrarna och ev. farmakologisk behandling. Insatsernas målsättning bör vara att 1) förse barnet med färdigheter att hantera oro och ångest 2) minska riskfaktorer och förstärka skyddande faktorer i barnets miljö samt 3) höja funktionsnivå hos barnet och familjen och minska ångestsymtom. Behandlingen läggs upp utifrån det enskilda ärendet. Den generella rekommendationen vid måttlig funktionsnedsättning är att initiera behandling med kognitiv beteendeterapi (KBT) eller KBT i kombination med psykofarmaka vilket framför allt gäller vid allvarligare problematik hos äldre barn och ungdomar. Behandlingen ska omfatta kontakt med föräldrarna och vid psykopatologi hos någon av föräldrarna är det indikerat med KBT-behandling med familjekomponent. Det är viktigt att uppmärksamma de resurser som finns på individ-, familje- och nätverksnivå. En viktig komponent i behandlingen är även vidmakthållande och återfallsförebyggande arbete. Eventuell depression eller suicidalitet måste uppmärksammas. Det saknas riktlinjer för behandlingsuppläggning vid komorbiditet, men komorbiditet utgör inte hinder för framgångsrik behandling. Nedanstående insatser rekommenderas i anslutning till bedömning: Psykopedagogik. Rådgivning/konsultation till föräldrarna, barnet/ungdomen eller skola/vårdgranne. Initial behandling med psykoterapi, företrädesvis KBT (individuellt eller i grupp). Familjeinriktad KBT-behandling är särskilt indikerad vid egen psykopatologi hos en eller båda föräldrarna. Föräldrarnas deltagande bör vara högre när det gäller hög grad av funktionsnedsättning hos barnet, yngre barn och när föräldrarnas förhållningssätt vidmakthåller problematiken. 2006-04-06 Tillägg av psykofarmakologisk behandling (företrädesvis (S)SRI) till KBT-behandling när det gäller hög grad av funktionsnedsättning, äldre barn och när annan behandling ej kan genomföras (barnet eller förälder vill ej delta i behandling). Psykodynamisk individualterapi. Vid behov - samarbete med skola, barnomsorg, primärvård etc. Bedömning av eventuell depression och suicidalitet bör göras i den initiala kontakten och återkommande under behandlingen. Allmänna riktlinjer vid behandling i slutenvård Slutenvård kan behövas vid mycket svåra ångesttillstånd med kraftig funktionsnedsättning och/eller suicidrisk. Slutenvård kan även bli aktuellt vid svåra tillstånd om familjen eller omgivningen inte kan ta ansvar för och trygga den unges tillstånd och/eller behandling i öppenvård har misslyckats och rekommenderad behandling inte kan genomföras i en mindre restriktiv miljö. Målet med slutenvård är att häva de akuta ångestsymtomen och initiera eller planera för fortsatt behandling i öppenvård. Beroende på barnets ålder och problematik kan psykofarmakologisk behandling bli aktuell under vårdperioden. Beskrivning av specifika metoder Kognitiv beteendeterapi (KBT) KBT är en målorienterad och tidsbegränsad psykoterapi. Behandlingen syftar till att hjälpa barnet att utveckla strategier för att hantera ångest. Terapin vid ångeststörningar hos barn och ungdomar innehåller huvudsakligen sex komponenter: hantering av kroppsliga symtom, psykopedagogik, kognitiva strategier, problemlösning, exponering och återfallsprevention. Målet för behandlingen är att barnet ska kunna hantera normala nivåer av ångest, utveckla större självständigt och bli mindre funktionsnedsatt. Det har gjorts över tjugotalet kontrollerade studier av behandling av ungdomar i ålder 6-17 år med ångestsyndrom (för en översikt se Comptom, 2002). Mellan 60-90 % av de behandlade barnen visar kliniskt signifikant förbättring. Långtidsuppföljningar visar på kvarstående effekt mätt vid 1, 3, 6, och 7.4 års-uppföljning efter avslutad behandling. Behandlingsmodellerna är manualiserade och kan användas för grupp- eller individualbehandling. Det finns inte stöd för att någon av behandlingsmodellerna skulle vara mer effektivt än det andra. Compton, S. N., Burns, B. J., Egger, h. L., Robertson, E. (2002). Review of the evidence base for treatment of childhood psychopathology: Internalizing disorders. Journal of Consulting and Clinical Psychology, 70, 1240-1266. 1. Barrett, P.M., Dadds, M.R., Rapee, R.M. (1996). Family treatment of childhood anxiety: a controlled trial. Journal of Consulting and Clinical Psychology, 64, 333-342. Abstract A family-based treatment for childhood anxiety was evaluated. Children (n = 79) aged 7 to 14 who fulfilled diagnostic criteria for separation anxiety, overanxious disorder, or social phobia were randomly allocated to 3 treatment conditions: cognitive-behavioral therapy (CBT), CBT plus family management (CBT+ FAM ), and waiting list. The effectiveness of the interventions was evaluated at posttreatment and at 6 and 12 months follow-up. The results indicated that across treatment conditions, 69.8% of the children no longer fulfilled diagnostic criteria for an anxiety disorder, compared with 26% of the waiting-list children. At the 1 2-month follow-up, 70.3% of the children in the CBT group and 95.6% of the children in the CBT + FAM group did not meet criteria. Comparisons of children receiving CBT with those receiving CBT+ FAM on self-report measures and clinician ratings indicated added benefits from CBT+ FAM treatment. Age and gender interacted with treatment condition, with younger children and female participants responding better to the CBT+ FAM condition. 2. Mendlowitz, S. L., Manassis, K., Bradley, S. et al. (1998). Cognitive-behavioral group treatments in childhood anxiety disorders: The role of parental involvement. Journal of American Academy of Child and Adolescents Psychiatry, 38, 1223-1229. Abstract Examined (1) the effect of a cognitive-behavioral group intervention on anxiety, depression, and coping strategies in school-age children (aged 7-12 yrs) with Axis I anxiety disorders; and (2) the effect of parental involvement on treatment outcomes. 68 children and their parents were randomly assigned to 1 of 3 12-wk treatment conditions: parent and child intervention, child-only intervention, and parent-only intervention. Child anxiety, depression, and coping strategies were assessed before and after treatment. All treatment groups reported fewer symptoms of anxiety and depression posttreatment and changes in their use of coping strategies. Children in the parent and child intervention used more active coping strategies posttreatment compared with children in the other 2 treatment conditions. Parents in this treatment condition reported a significantly greater improvement in their children's 2006-04-06 emotional well-being than parents in the other treatment conditions. Cognitive-behavioral group interventions reduced symptoms of anxiety and depression in school-age children with anxiety disorders. Concurrent parental involvement enhanced the effect on coping strategies. 3. Silverman, W. K., Kurtines, W. M., Ginsburg, G. S. et al. (1996). Treating anxiety disorders in children with group cognitive-behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 67, 995-1003. Abstract A randomized clinical trial evaluated the therapeutic efficacy of group cognitive-behavioral therapy (GCBT) versus a wait-list control (WLC) condition to treat anxiety disorders in children. Results indicated that GCBT, with concurrent parent sessions, was highly efficacious in producing and maintaining treatment gains. Children in GCBT showed substantial improvement on all the main outcome measures, and these gains were maintained at 3-, 6-, and 12-month follow-ups. Children in the WLC condition did not show improvements from the pre- to postwait assessment point. These findings are discussed in terms of the need to continue to advance the development of practical, as well as conceptual, knowledge of efficacious treatment for anxiety disorders in children. 4. Cobham, V. E., Dadds, R. M., Spence, S. H. (1998). The role of parental anxiety in the treatment of childhood anxiety. Journal of Consulting and Clinical Psychology, 66, 893-905. Abstract Sixty-seven children aged 7-14 who met diagnostic criteria for an anxiety disorder were assigned to conditions according to parental anxiety level. Within these conditions, children were randomly assigned to 1 of 2 treatments: child-focused cognitive-behavioral therapy (CBT) or child-focused CBT plus parental anxiety management (CBT + PAM). At posttreatment, results indicated that within the child-anxiety-only condition, 82% of the children in the CBT condition no longer met criteria for an anxiety disorder compared with 80% in the CBT + PAM condition. Within the child + parental anxiety condition, 39% in the CBT condition no longer met criteria compared with 77% in the CBT + PAM condition. At followup, these differences were maintained, with some weakening over time. Results were not consistent across outcome measures. The interpretation and assessed with self-report inventories. Assessments were done pre-, post-, and 1-year following treatment. Results showed that both treatment conditions did significantly better than the control condition, whereas the treatment groups did equally well on most measures, and the effects were maintained at follow-up. The implications of these results are discussed. KBT-modeller specifikt vid social fobi Behandlingsmodeller specifika för social fobi hos barn och ungdomar har prövats. Specifika komponenter är t.ex. social färdighetsträning och social problemlösning. Även skolbaserad KBT-behandling har prövats. 5. Hayward, C., Varady, S., Albano, A. M. et al. (2000). Cognitive-behavioral group therapy for social phobia in female adolescents: Results of a pilot study. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 721-726. Abstract To examine the efficacy of cognitive-behavioral group therapy for adolescents (CBGT-A) in females with social phobia and the effect of this treatment on the risk for major depression. METHOD: Female adolescents with social phobia (N = 35) were randomly assigned to treatment (n = 12) or no treatment (n = 23) groups. Assessments were conducted at baseline, after treatment, and at a 1-year follow-up. RESULTS: Eleven subjects completed treatment. Sixteen weeks of treatment produced a significant improvement in interference and reduction in symptoms of social anxiety. There was a significant reduction in the number of subjects meeting DSM-IV criteria for social phobia in the CBGT-A versus the untreated group; however, at the 1-year follow-up there were no significant differences by treatment condition. There was also suggestive evidence that treatment of social phobia lowers the risk for relapse of major depression among those with a history of major depression. Combining social phobia and major depression as the outcome produced more robust treatment effects in the 1-year follow-up. CONCLUSIONS: This pilot study provides evidence for a moderate short-term effect of CBGT-A for treating female adolescents suffering from social phobia and indicates that treatment of social phobia may result in a reduction of major depression. 6. Beidel, D. C., Turmer, S. M., Morris, T. L. (2000). Behavioral treatment of childhood social phobia. Journal of Consulting and Clinical Psychology, 89, 1072-1080. Abstract 2006-04-06 Sixty-seven children (ages 8 and 12) with social phobia were randomized to either a behavioral treatment program designed to enhance social skills and decrease social anxiety (Social Effectiveness Therapy for Children, SET-C) or an active, but nonspecific intervention (Testbusters). Children treated with SET-C were significantly more improved across multiple dimensions, including enhanced social skill, reduced social fear and anxiety, decreased associated psychopathology, and increased social interaction. Furthermore, 67% of the SET-C group participants did not meet diagnostic criteria for social phobia at posttreatment compared with 5% of those in the Testbusters group. Treatment gains were maintained at 6-month follow-up. The results are discussed in terms of treatment of preadolescent children with social phobia and the durability of treatment effects. 7. Spence, H., Donovan, C., Brechman-Toussaint, M. (2001). The treatment of childhood social phobia: The effectiveness of a social skills training-based, cognitive-behavioral intervention, with and without parental involvement. Journal of Child Psychology and Psychiatry, 41, 713-726. Abstract 50 children (aged 7-14 yrs) with a principal diagnosis of social phobia were randomly assigned to either child-focused cognitive-behavior therapy (CBT), CBT plus parent involvement, or a wait list control (WLC). The integrated CBT program involved intensive social skills training combined with graded exposure and cognitive challenging. At posttreatment, significantly fewer children in the treatment conditions retained a clinical diagnosis of social phobia compared to the WLC condition. In comparison to the WLC, children in both CBT interventions showed significantly greater reductions in children's social and general anxiety and a significant increase in parental ratings of child social skills performance. At 12-mo follow-up, both treatment groups retained their improvement. There was a trend towards superior results when parents were involved in treatment, but this effect was not statistically significant. 8. Masia, C., Klein, R. G., Storch, E. et al. (2001). School-based behavioral treatment for social anxiety disorder in adolescents: Results of a pilot study. Journal of the American Academy of Child and Adolescents Psychiatry, 40, 780-786. Abstract To provide preliminary estimates of feasibility and effectiveness for school-based behavioral treatment in adolescents with social anxiety disorder. METHOD: Six adolescents with social anxiety disorder were treated in a 14-session group treatment program conducted at their school. Assessments were conducted at baseline and after treatment. RESULTS: All participants were classified as treatment responders (markedly or moderately improved). Half of the participants did not meet diagnostic criteria for social phobia after treatment. Clinician severity ratings, as measured by the Anxiety Disorders Interview Schedule for Children for DSM-IV: Child Version and the Liebowitz Social Anxiety Scale for Children and Adolescents (LSAS-CA), decreased significantly after intervention, with effect sizes of 2.5 and 1.8, respectively. All LSAS-CA scale scores decreased significantly after treatment. Selfreported social phobia symptoms on the Social Phobia and Anxiety Inventory for Children were not significantly reduced. Fear and avoidance ratings of the 10 most feared situations significantly decreased after treatment, with effect sizes of 1.5 for anxiety and 2.1 for avoidance. CONCLUSIONS: This study provides preliminary support for the promise of schoolbased behavioral intervention for treating social phobia in adolescents. The school environment may be a rich and innovative setting for implementation of behavioral treatment because this is the setting where adolescents with social phobia endure the most distress. KBT med anknytningsbaserad familjeterapi Behandlingsprinciperna är desamma som vid KBT generellt men anpassade för ungdomar. Syftet med behandlingen är att hjälpa ungdomen att utveckla autonomi från föräldrarna på ett konstruktivt sätt. I kontakten med föräldrarna arbetar man med kommunikation och familjedynamik. Syftet är också att hjälpa föräldrarna att balansera mellan att ge trygghet och uppmuntra självständighet samt att bryta mönster som vidmakthåller ångestsymtomen. Metodiken finns endast prövad i en randomiserad och kontrollerad studie. 9. Siqueland, L., Rynn, M., Diamond, G. S. (2005). Cognitive behavioral and attachment based family therapy for anxious adolescents: Phase I and II studies. Journal of Anxiety Disorders, 19, 361-381. Abstract The goals of these two studies were to assess the acceptability and feasibility as well as to gather preliminary efficacy data on a modified combination cognitive behavioral (CBT) and attachment based family therapy (ABFT) for adolescents (ages 12–18), with the primary diagnosis of generalized (GAD), social phobia (SP), and separation (SAD) anxiety disorders. In Phase I, CBT was modified for an adolescent population and ABFT was modified for working with anxious adolescents in combination with CBT. Therapists were trained for both conditions and eight patients were treated as an open trial pilot of combined CBT-ABFT with positive results. In Phase II, 11 adolescents were randomly assigned to CBT alone or CBT and family based treatment (CBT-ABFT). Participants were evaluated at pre, post, and 6–9 months follow-up assessing diagnosis, psychiatric symptoms and family functioning. 2006-04-06 Results indicated significant decreases in anxiety and depressive symptoms by both clinical evaluator and self-reports with no significant differences by treatment. Sixty-seven percent of adolescents in CBT no longer met criteria for their primary diagnosis at post treatment as compared to 40% in CBT-ABFT with continued improvement of 100 and 80% at follow-up with no significant differences between treatments. Both CBT and CBT-ABFT appear to be promising treatments for anxious adolescents and more treatment development and evaluation is needed. (S)SRI Under senare år har flera behandlingsstudier visat god effekt vid (S)SRI-behandling av ångesttillstånd hos barn och ungdomar. Den s.k. RUPP-studien, samt två studier av blandade ångesttillstånd visade att aktiv behandling var bättre än placebo. Effekten på de tre ingående diagnoserna separationsångest, social fobi och generaliserat ångestsyndrom var lika god. i en 6-mån uppföljning. Många svarade positivt på behandling med fluvoxamin eller fluoxetin som tillägg till psykoterapi. Behandlingstider på minst 6 mån rekommenderas samt att nedtrappning görs långsamt och under flera månader. Behandling med (S)SRI ges tillsammans med KBT. Om kompetens eller resurser för kvalificerad KBT saknas, bör vid svårare tillstånd (S)SRI erbjudas tillsammans med psykosocial behandling. Behandling med (S)SRI medför risk för emotionell labilitet, självskador och självmordstankar/självmordsförsök. Sannolikt beror detta på att (S)SRI preparaten initialt kan ge ökad ångest och aktivering. Se även riktlinjer för behandling med (S)SRI vid depression. 10. Reinblatt, S. P., Walkup, J. T. (2005). Psychopharmacologic treatment of pediatric anxiety disorders. Child Adolesc Psychiatr Clin N Am, 14, 877-908. Abstract This article reviews the psychopharmacologic treatment of child and adolescent anxiety disorders and is divided into the following sections: historical background, general treatment principles, obsessive-compulsive disorder, other anxiety disorders, including separation anxiety disorders, generalized anxiety disorder, and social phobia, elective mutism, and posttraumatic stress disorder and specific phobia. Short-term and long-term psychopharmacologic treatment strategies are reviewed, as are approaches for managing comorbidity and treatment-refractory cases. This article is organized by diagnostic categories rather than by medication classes to emphasize the clinical perspective. [References: 164] 11. RUPP-group. (2001). Fluvoxamine for the treatment of anxiety disorders in children and adolescents. The Research Unit on Pediatric Psychopharmacology (RUPP) Anxiety Study Group. New England Journal of Medicine, 344, 1279-85. Abstract BACKGROUND: Drugs that selectively inhibit serotonin reuptake are effective treatments for adults with mood and anxiety disorders, but limited data are available on the safety and efficacy of serotonin-reuptake inhibitors in children with anxiety disorders. METHODS: We studied 128 children who were 6 to 17 years of age; who met the criteria for social phobia, separation anxiety disorder, or generalized anxiety disorder; and who had received psychological treatment for three weeks without improvement. The children were randomly assigned to receive fluvoxamine (at a maximum of 300 mg per day) or placebo for eight weeks and were evaluated with rating scales designed to assess the degree of anxiety and impairment. RESULTS: Children in the fluvoxamine group had a mean (+/-SD) decrease of 9.7+/-6.9 points in symptoms of anxiety on the Pediatric Anxiety Rating Scale (range of possible scores, 0 to 25, with higher scores indicating greater anxiety), as compared with a decrease of 3.1+/-4.8 points among children in the placebo group (P<0.001). On the Clinical Global Impressions-Improvement scale, 48 of 63 children in the fluvoxamine group (76 percent) responded to the treatment, as indicated by a score of less than 4, as compared with 19 of 65 children in the placebo group (29 percent, P<0.001). Five children in the fluvoxamine group (8 percent) discontinued treatment because of adverse events, as compared with one child in the placebo group (2 percent). CONCLUSIONS: Fluvoxamine is an effective treatment for children and adolescents with social phobia, separation anxiety disorder, or generalized anxiety disorder. 12. Walkup, J., Labellarte, M., Riddle, M. A. et al. (2002). Treatment of pediatric anxiety disorders: an open-label extension of the research units on pediatric psychopharmacology anxiety study. Journal of Child and Adolescent Psychopharmacology, 12, 175-88. Abstract 2006-04-06 BACKGROUND: An 8-week placebo-controlled study, the Research Units on Pediatric Psychopharmacology Anxiety Study, documented beneficial effects of fluvoxamine in the treatment of pediatric social anxiety, separation anxiety, or generalized anxiety disorders. Following completion of this study, participants were invited to enter a 6-month open-label treatment phase designed to examine three issues: (a) long-term maintenance of response in fluvoxamine responders, (b) acute response to fluoxetine in fluvoxamine nonresponders, and (c) acute response to fluvoxamine in placebo nonresponders. METHODS: Participants aged 6-17 years meeting criteria for social anxiety, separation anxiety, or generalized anxiety disorders previously treated in an 8-week placebo-controlled trial (n = 128) were offered open treatment. Changes in symptoms of anxiety during open treatment were assessed in three groups: (a) fluvoxamine responders maintained on fluvoxamine, (b) fluvoxamine nonresponders changed to fluoxetine, and (c) placebo nonresponders changed to fluvoxamine. Response was defined based on Clinical Global Impression criteria. RESULTS: During 6 months of continued open treatment, anxiety symptoms remained low in 33 of 35 (94%) subjects who initially responded to fluvoxamine. Among 14 fluvoxamine nonresponders switched to fluoxetine, anxiety symptoms appeared significantly improved in 10 (71%) subjects. Finally, among 48 placebo nonresponders, 27 (56%) showed clinically significant improvement in anxiety on fluvoxamine. CONCLUSION: The current findings concerning extended treatment of pediatric anxiety disorders are only preliminary, because treatment was uncontrolled. Results suggest that an initial fluvoxamine response is likely to be retained with continued treatment, that some fluvoxamine nonresponders may respond to fluoxetine, and that some placebo nonresponders may respond to fluvoxamine. 13. Walkup, J. T., Labellarte, M. J., Riddle, M. A. et al. (2003). Searching for moderators and mediators of pharmacological treatment effects in children and adolescents with anxiety disorders. Journal of American Academy of Child and Adolescent Psychiatry, 42, 13-21. Abstract OBJECTIVE: To examine whether age, gender, ethnicity, type of anxiety disorder, severity of illness, comorbidity, intellectual level, family income, or parental education may function as moderators and whether treatment adherence, medication dose, adverse events, or blinded rater's guess of treatment assignment may function as mediators of pharmacological treatment effect in children and adolescents with anxiety disorders. METHOD: The database of a recently reported double-blind placebo-controlled trial of fluvoxamine in 128 youths was analyzed. With a mixed-model random-effects regression analysis of the Pediatric Anxiety Rating Scale total score, moderators and mediators were searched by testing for a three-way interaction (strata by treatment by time). A two-way interaction (strata by time) identified predictors of treatment outcome. RESULTS: No significant moderators of efficacy were identified, except for lower baseline depression scores, based on parent's (but not child's) report, being associated with greater improvement (p < .001). Patients with social phobia (p < .05) and greater severity of illness (p < .001) were less likely to improve, independently of treatment assignment. Blinded rater's guess of treatment assignment acted as a possible mediator (p < .001), but improvement was attributed to fluvoxamine, regardless of actual treatment assignment. Treatment adherence tended to be associated (p = .05) with improvement. CONCLUSIONS: In this exploratory study, patient demographics, illness characteristics, family income, and parental education did not function as moderators of treatment effect. Social phobia and severity of illness predicted less favorable outcome. Attribution analyses indicated that study blindness remained intact. The presence of concomitant depressive symptoms deserves attention in future treatment studies of anxious children. Kognitiv beteendeterapi i kombination med antidepressiva läkemedel Det har gjorts en studie av imipramin och KBT för barn med ångest, depression och skolvägran. Resultaten visar att Imipramin i kombination med KBT är signifikant bättre än placebo och KBT. 14. Bernstein, G. A., Borchardt, C. M., Perwien, A. R. et al. (2000). Imipranine plus cognitive-behavioral therapy in the treatment of school refusal. J Am Acad Child Adolesc Psychiatry, 39, 276-83. Abstract OBJECTIVE: To investigate the efficacy of 8 weeks of imipramine versus placebo in combination with cognitive-behavioral therapy (CBT) for the treatment of school-refusing adolescents with comorbid anxiety and major depressive disorders. METHOD: This was a randomized, double-blind trial with 63 subjects entering the study and 47 completing. Outcome measures were weekly school attendance rates based on percentage of hours attended and anxiety and depression rating scales. RESULTS: Over the course of treatment, school attendance improved significantly for the imipramine group (z = 4.36, p < .001) but not for the placebo group (z = 1.26, not significant). School attendance of the imipramine group improved at a significantly faster rate than did that of the placebo group (z = 2.39, p = .017). Over the 8 weeks of treatment, there was a significant difference between groups on attendance after controlling for baseline attendance; mean attendance rate in the final week was 70.1% +/- 30.6% for the imipramine group and 27.6% +/- 36.1% for the placebo group (p < .001). Defining remission as 75% school attendance, 54.2% of the imipramine group met this criterion after treatment compared with only 16.7% from the placebo group (p = .007). Anxiety and depression rating scales decreased significantly across treatment for both groups, with depression on the Children's Depression Rating Scale-Revised decreasing 2006-04-06 at a significantly faster rate in the imipramine group compared with the placebo group (z = 2.08, p = .037). CONCLUSIONS: Imipramine plus CBT is significantly more efficacious than placebo plus CBT in improving school attendance and decreasing symptoms of depression in school-refusing adolescents with comorbid anxiety and depression. Familjeterapi Familjeterapeutisk behandling är som regel problemorienterad, salutogent inriktad och tidsbegränsad. Syftet är att hjälpa familjen att komma tillrätta med dysfunktionella samspelsmönster så att problem kan lösas, hinder för utveckling undanröjas och resurser frigöras för barnets fortsatta utveckling och välbefinnande. Det finns inga specifika metoder utarbetade för behandling av ångestsymtom. Familjeterapi kan ha betydelse för att minska stress inom familjen som annars kan vidmakthålla ångestproblematiken. 15. Carr, A. (2001). Evidence-based practice in marital and family therapy. In family therapy - concepts, process and practice. s. 500-502. John Wiley and Sons Ltd. England. Psykoanalys och psykodynamisk psykoterapi Psykodynamisk psykoterapi kan ske i form av lekterapi för barn eller samtalsterapi (individuellt eller i grupp) när det gäller ungdomar. I terapin ges barnet/ungdomen möjlighet att inom ramen för relationen till terapeuten arbeta igenom olösta inre konflikter, återta projektioner och på så sätt komma till rätta med ångesten. Innan terapin påbörjas görs bedömning av barnets/den unges och föräldrarnas möjlighet att tillgodogöra sig behandlingen samt av de yttre förutsättningarna för kontakten. Parallellt med terapin har också föräldrarna en behandlingskontakt med undantag av en del fall med äldre ungdomar. Man eftersträvar dock alltid att föräldrarna är införstådda med behandlingen även om de inte själva deltar. Vanligen sträcker sig psykodynamisk terapi över en tidsperiod av ca två år men i barnpsykiatrisk praxis sker även psykodynamiskt inriktad behandling över kortare tid. Det saknas kontrollerade studier för att kunna uttala vetenskapligt stöd för psykodynamisk psykoterapi vid ångeststörningar. Metoden har dock stor beprövad erfarenhet. 16. Target, M., Fonagy, P. (1994). Efficacy of psychoanalysis for children with emotional disorder. American Academy of Child and Adolescents Psychiatry, 33, 3, 361-371. Abstract This is the second report from a chart review of 763 cases of child psychoanalysis and psychotherapy at the Anna Freud Centre. METHOD: Three hundred fifty-two children and adolescents were identified who met DSM-III-R criteria for emotional disorders or who had sleep or somatoform symptoms with marked emotional disturbance. Two hundred fifty-four were treated in full psychoanalysis, the remainder one to three times per week, for an average of 2 years. Outcome was indicated by diagnostic change and by change in overall adaptation, measured by the Children's Global Assessment Scale (CGAS). RESULTS: Of those treated for at least 6 months, 72% showed reliable improvement in adaptation, 24% still had some diagnosis at termination, and 15% still had an emotional disorder. Simple phobias were most likely to remit, and depressed children were least likely to return to normal CGAS levels. Children younger than 11 years were considerably more likely to be well at the end of treatment. Intensive treatment generally led to greater improvements, independently of age and treatment length. Certain disorders, and more severe pathology, required intensive treatment; 50% of severe cases showed no improvement in psychotherapy. Thirty-one percent of variance in CGAS change could be predicted, and greater than 50% when diagnostic groupings were examined separately. CONCLUSION: Despite methodological limitations, the study identifies predictors of improvement (e.g., younger age, phobic symptoms, intensity and length of treatment) and shows that severe or pervasive pathology requires intensive analytic help. Effekt av åtgärd A. Sjuklighet - död kan förhindras B. Tillståndet kan botas C. Sjuklighet påverkas mycket, överlevnaden förlängs D. Sjukligheten påverkas i viss utsträckning E. Ingen effekt, F. Risk för försämring 2006-04-06 Grad av vetenskaplig dokumentation för effekt baserad på studier av barn och ungdomar God = Två eller flera oberoende relevanta RCT med statistisk signifikanta och entydiga resultat eller metaanalyser med entydiga resultat, Viss = Flera kontrollerade studier eller enstaka mindre RCT med entydiga resultat eller större RCT med divergerande resultat. Ringa = Fallserier vid olika centra och/eller enstaka kontrollerade studier eller enstaka RCT med motsägelsefulla resultat. Ingen = Enstaka fallbeskrivningar. Risk med åtgärd Stor Risk Måttlig risk Liten risk Om möjligt anges andelen riskpatienter, exempelvis < 5% Qaly Kostnad per kvalitetsjusterade levnadsår alternativt vunnet levnadsår. Låg < 100 000 kr/QALY alternativt vunnet levnadsår Måttlig 100 000 – 500 000 kr/QALY alternativt vunnet levnadsår Hög 500 000 – 1 miljon kr/ QALY alternativt vunnet levnadsår Mycket hög > 1 miljon kr/QALY alternativt vunnet levnadsår Ej bedömningsbar Nytta av åtgärd Sammanvägning av beprövad erfarenhet, effekt av åtgärd, grad av vetenskaplig dokumentation, risk med åtgärd och kostnadseffektivitet. Bedöm graden av nytta från 1-4, där 1 är stor och 4 är liten. Vårdnivå L = Länssjukvård R = Regional vård H = Högspecialiserad vård Vårdform SV = Slutenvård ÖV = Öppenvård