Expert Medico-Scientific Evidence before Tribunals
advertisement

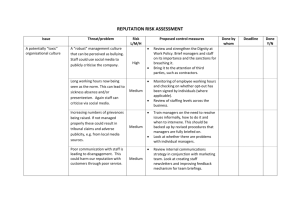
Expert Medico-Scientific Evidence before Tribunals: Approaches to Proof, Expertise and Conflicting Opinions.1 Randall Kune2 Professor Gabriel Kune3 TABLE OF CONTENTS I. INTRODUCTION ..................................................................................................... 1 II. DIFFERENT CONCEPTS OF PROOF ................................................................ 2 A. Legal principles of proof ...................................................................................... 2 B. Scientific Concept of Proof of Cancer Cause...................................................... 4 III. WHO ARE THE EXPERTS? ................................................................................ 7 A. Who are the experts in cancer causation? .......................................................... 7 1. Who are the experts required to prove the general case of cancer causality? .. 7 2. Expert evidence required for the specific case .................................................. 8 B. Rules of expert evidence in tribunals................................................................... 8 1. The expertise rule ............................................................................................... 9 2. The basis rule ................................................................................................... 11 IV. PROCEDURES FOR EVALUATING EXPERT OPINIONS ............................ 12 V. DIFFERENT PERSPECTIVES IN MEDICAL SCIENCE ................................ 15 VI. CONCLUSIONS ................................................................................................... 17 APPENDIX ................................................................................................................. 19 I. INTRODUCTION In performing their function as decision-makers, tribunals can be faced with the question: what caused an injury, illness or disease? Medical-science provides a framework to assess the validity and weight of such claims. We will set out this framework and we hope that in making the framework explicit, we will ease some of the difficulties often expressed by decision-makers when faced with expert medicoscientific evidence. We take as our starting point the contrasting approaches to proof taken on the one hand by medical science, and on the other, by legal or administrative decision-makers. When do they consider that something is “proven”? We will outline the principles of medico-scientific proof using cancer causation as a model. 1 Paper delivered to the Council of Australasian Tribunals, Victorian Chapter, 21 October 2004. LL.B (Hons) LL.M, Barrister, International Institute of Forensic Studies. 3 MD FRACS FRCS (England) FACS, Emeritus Professor of Surgery, University of Melbourne. 2 2 Decision-makers who consider issues illness or disease causation will need to rely on expert medico-scientific opinions, even if it is their own. We will identify the relevant experts in cancer causation. We will then explain a number of principles from the rules of expert evidence as well as some recent procedural reforms in various courts which could greatly assist a tribunal to reach a correct decision efficiently and fairly. These principles would be particularly important if two opposing experts give conflicting opinions. Finally, we will briefly consider two emerging areas being firstly the relationship between life stress and illness and secondly, the forensic evaluation of complementary and alternative medicine. Each area is contentious from a scientific point of view, and is likely to be the source of conflicting expert opinion. Much of the following material may be familiar and even well known to many readers, but “in everything well known something worthy of thought still lurks.”4 II. DIFFERENT CONCEPTS OF PROOF A. Legal principles of proof Generally in courts and tribunals, it is the party who makes a claim or allegation who must establish the factual basis to their claim. And they must do this to a specific standard of proof. In criminal cases, the standard of proof is “beyond reasonable doubt”. In civil cases, the standard is “the balance of probabilities”. Generally for tribunals, unless the rules or governing legislation state otherwise, the standard of proof is one of “reasonable satisfaction”5 but this obligation is variable, depending on the seriousness of the allegations or consequences of an adverse finding.6 Moreover, the standard can be difficult to apply where a tribunal is making its own investigations or relying on its own expert knowledge. Heidegger, M, Nietzsche, Author’s forward, Harper Collins, San Francisco, 1991. See JRS Forbes, Justice in Tribunals, Federation Press, Leichhardt, NSW, 2002 at p157. 6 JRS Forbes, above n5, at 159. 4 5 3 When a tribunal is considering the medico-scientific criteria of proof, it must bear in mind that a medical possibility of causation can allow a decision-maker to find causation proved as a probability in all the circumstances.7 The most important legal decision on this question was given in the context of medico-scientific evidence about renal cell carcinoma from exposure to asbestos. In Seltsam Pty Ltd v McGuiness,8 Chief Justice Spigelman in the New South Wales Court of Appeal made it clear that: 9 “evidence of possibility, including epidemiological studies, should be regarded as circumstantial evidence which may, alone or in combination with other evidence, establish causation in a specific case.” Circumstantial evidence of disease causation would include medico-scientific evidence about general causation, which we will discuss shortly. If this evidence amounts to more than a possibility, then causation can be found proved on the balance of probabilities or even higher standards. So decision-makers can find causation proved to this standard where there is scientific uncertainty or “significant scientific dispute” about the cause of a disease.10 The reason for this is clear. The decision-making process in a tribunal is limited by its very nature:11 “…limited in its ambition to find the ultimate or abstract truth, and limited in the fact-finding process. The [tribunal] is constrained by various pragmatic and systemic fetters such as the rules of [procedural fairness], and the need for a decision. Courts, [tribunals] and the law generally aim to achieve the correct social result rather than to determine the abstract truth, as scientists do.” 7 See EMI (Australia) Ltd v Bes [1970] 2 NSWR 238 at 242 (Herron CJ). [2000] NSWCA 29. 9 Seltsam Pty Ltd v McGuiness (2000) NSWCA 29 at [89]. 10 Seltsam Pty Ltd v McGuiness (2000) NSWCA 29 at [94]. 11 Kune, R & Kune, GA, “Proof of cancer causation and expert evidence: Brining science to the law and law to science” (2003) 11 JLM 112. Emphasis added. 8 4 B. Scientific Concept of Proof of Cancer Cause How does science go about proving that a particular exposure, such as solar radiation, is a cause of a particular cancer, such as skin cancer? Who are the experts required to prove that link? In this paper, we use cancer as the model in the proof of a causal link, but emphasise that a similar structure would serve equally well to prove causal factors in other chronic conditions, such as heart attacks. The concept that human cancers have well-defined causes is relatively recent, and its foundation was laid in 1950 by establishing the connection between smoking and lung cancer.1213 There have been major advances in our understanding of cancer causation since, and very briefly, and greatly summarised, the current mainstream scientific view of cancer development is as follows.14 There are several known causes, which vary from one cancer to the next, usually multiple inherited and/or acquired during life, such as smoking, radiation, asbestos, etc. CAUSES Repeated damage to the genetic material (DNA) of dividing cell leads to GENETIC CHANGES INCLUDING MUTATIONS Result in transformation in structure and function of cells from NORMAL CELL PRECANCEROUS CELL CANCER CELL Wynder EL and Graham EA. “Tobacco Smoking as a Possible Etiologic Factor in Bronchogenic Carcinoma. A Study of 654 Proved Cases” (1950) 143 JAMA 329. 13 Doll R and Hill, AB. “Smoking and Carcinoma of the Lung. Preliminary Report” (1950) 2 Brit Med J 739. 14 Kune GA. “The Home Health Guide to a Cancer-Free Family”. Michelle Anderson Publishing, Melbourne 2003 at 3–9. 12 5 The cancer cells are then further damaged, resulting in further mutations, they can then multiply uncontrollably, invade surrounding tissues, spread elsewhere in the body, and eventually kill the individual. This change from a normal cell to a cancer cell is usually slow, takes place over several years and sometimes over decades. For instance, the smallest diagnosable breast cancer, which is about one cubic centimetre, has been calculated to have been present as a cancer for 5 years, on average.15 So what does science require in order to establish a general case of proof of causality? There is no one single test which will show causality beyond doubt. One needs several pieces of evidence to prove a causal connection, let’s say between smoking and cancer of the throat, or radiation and leukaemia. The following criteria would be regarded as important in 2004:16 1) There is a statistically significant positive association between a particular cancer and a particular exposure. • Although a statistically significant positive association is an important beginning in proof of a causal link, by itself such association does not prove causation. We require additional proof. 2) Characteristics of the association. The causal link in this positive association is strengthened if: i) The risk level is high. ii) The association is reproduced by several studies. iii) There is a dose response effect, that is, the higher the dose, the higher the risk. iv) Statistical correction for known confounders leaves the risk level unchanged. DeVita VJ Jr, Hellman S and Rosenberg SA. “Cancer. Principles and Practice of Oncology” 3rd Ed Lippincott, Philadelphia 1989 at 1200–1202. 16 Kune GA. “Causes and Control of Colorectal Cancer. A Model for Cancer Prevention”. Kluwer Academic Publishers, Boston 1966 at 1–12. 15 6 3) Animal models, usually done on rats or mice show that the exposure results in tumour or excessive tumour formation. So the above three criteria attempt to answer the question of causality, the question why a cancer has developed. The causal link is further strengthened by the next two sets of criteria which attempt to answer the question how a cancer develops, that is, the mechanisms of carcinogenesis. 4) Structural cell changes. Looked at under the microscope, a carcinogen will transform a normal cell, to a precancerous cell, and then to a cancer cell. 5) Biological mechanisms demonstrated. These concepts range from the simple to the complex. i) The time frame is appropriate. A simple but important consideration, given that most cancers take several years and even decades to develop. Also, there is the issue of an appropriate latent period between exposure and cancer diagnosis, which, for example, in exposure to asbestos and the diagnosis of mesothelioma is about 20 or 25 years. ii) Mode of action of the carcinogen, such as tar in tobacco, has been demonstrated experimentally. iii) There is a sequence of molecular genetic changes and mutations, as demonstrated by gene technology. Based on these 5 sets of criteria, a very approximate summary table has been constructed with practical examples, in order to indicate the level of confidence a medical scientist might have in relation to causality with different exposures and different cancers. 7 Table. Causal Likelihood of Certain Exposures and Related Cancers.17 Example Causal Statistically Qualities of Animal Structural Biological Likelihood significant association experiment cell changes mechanisms Positive Positive Positive Positive Positive scientific scientific scientific scientific scientific evidence evidence evidence evidence evidence exists exists exists exists exists Positive Positive Scientific No positive No positive in farmers scientific scientific evidence is scientific scientific and prostate evidence evidence equivocal evidence evidence cancer exists exists exists exists Positive No positive No positive No positive No positive power lines scientific scientific scientific scientific scientific and evidence evidence evidence evidence evidence childhood exists exists exists exists exists positive association Smoking and Proven cancer Pesticide use Overhead Likely Possible leukaemia Cellular Unlikely at No positive No positive No positive No positive Scientific phones and present scientific scientific scientific scientific evidence is cancer of the evidence evidence evidence evidence equivocal brain exists exists exists exists III. WHO ARE THE EXPERTS? A. Who are the experts in cancer causation? 1. Who are the experts required to prove the general case of cancer causality? It is clear that we need to rely on evidence by experts from widely different disciplines: Cancer Epidemiologists know about cancer cause in humans, a lot about statistics and may or may not have medical training – they will answer Criteria 1 and 2. 17 Kune R and Kune G, above n11. 8 Carcinogenesis Experts. Experimental scientists working in the laboratory, usually not medically trained who can answer Criteria 3 and 5. Molecular Biologists. Experimental scientists, working in the laboratory. Knowledgeable on the genetics of cancer development, may or may not have medical training, can answer genetic aspects of Criteria 5. Cancer Pathologists. Medically trained pathologists who look under the microscope and can tell us about Criteria 4, the structural cell changes that lead from a normal cell into a cancer cell. Other Experts depending on the issue, such as Radiation Physicists, Occupational Health etc. 2. Expert evidence required for the specific case Here we need Clinical Oncologists, experts who are medically trained cancer specialists, who can apply the general concepts of cancer cause to the individual in question, and fit it into the specific medical circumstances of that person. We emphasise that this sort of structure would apply equally to other medicoscientific areas of proof and expert evidence coming to tribunals, such as heart attacks, work injuries, road injuries etc. B. Rules of expert evidence in tribunals For tribunals, the rules of evidence are generally more persuasive than binding. This is true at common law,18 and for most statutory tribunals.19 The primary procedural obligation of tribunals is to accord natural justice to each party.20 But as Justice Evatt noted in a High Court decision from early last century:21 The rules of evidence are not automatically “imported’ by the rules of natural justice. See, for instance, R v Deputy Industrial Relations Commission; ex p. Moore [1965] 1 QB 456 at 488; Re Pochi & Minister for Immigration and Ethnic Affairs (1979) 26 ALR 247 at 256; Re Gyngell; ex p Hardiman (1980) ALJR 314. 19 Refer, for example, to the legislation and rules in the appendix. 20 Australian Broadcasting Tribunal v Bond (1990) 170 CLR 321. 21 R v The War Pensions Entitlement Appeals Tribunal (1933) 50 CLR 228 at 256 per Evatt J. 18 9 “… this does not mean that all rules of evidence may be ignored as of no account. After all, they represent the attempt made, through many generations, to evolve a method of inquiry best calculated to prevent error and elicit truth. No tribunal can, without grave danger of injustice, set them on one side and resort to methods of inquiry which necessarily advantage one party and necessarily disadvantage the opposing party.” To generalise from what His Honour was saying, there are good reasons why a tribunal, to comply with their obligations of natural justice, should apply certain rules of evidence in particular cases or particular types of cases. It is along this line of reasoning that we argue that where a tribunal needs to rely on expert evidence, then the essential rules of expert evidence should also be applied. The rules of primary importance are the expertise rule and the basis rule. While we referring to rules which limit the admissibility of evidence, our analysis can be applied equally to the task of the tribunal in determining the weight to be given to that opinion once it is either admitted into evidence or otherwise brought to the attention of the tribunal for the purpose of making its decision.22 1. The expertise rule An opinion is an inference based on facts and assumptions. In determining what caused an illness or disease, expert opinion evidence is relevant where the decisionmaker is “not equipped to decide the relevant issues”23 because the proper inferences “stand outside an area in which common experience can be a touchstone.”24 An expert witness does not need to be “a leading or even senior practitioner in the field”25 but they will only be an expert if “the sufficiency and the relevance of [their] specialised skills” will assist the decision-maker in drawing the proper inference.26 22 Kirkpatrick v Commonwealth (1985) 62 ALR 533. Murphy v The Queen (1989) 167 CLR 94 at 131 per Dawson J. 24 EMI (Australia) Ltd v Bes (1970) 2 NSWR 238 at 242 per Herron CJ. 25 Freckelton, I & Selby H, Expert Evidence: Law, Practice, Procedure and Advocacy, 2nd ed, Law Book Co, Pyrmont, NSW, 2002, at 23. 26 Freckelton, I & Selby H, above n25, at 23. 23 10 A tribunal is entitled to act on its own knowledge (including scientific expertise)27 if that knowledge is relevant and the tribunal complies with the requirements of natural justice. For a medico-scientific opinion to be relevant, we suggest that it must be given by somebody who falls within the category of “expert”, and we have identified the specific experts with respect to cancer causation. If the tribunal intends to rely on its own expert opinion or expert opinion that it has itself sought, then the parties must have adequate notice of this, and an opportunity to respond to it.28 If the opinion is mistaken, or lacks a basis in facts before the tribunal, then the tribunal may be acting without evidence,29 and consequently making a fundamental error.30 A recent survey of Judges on expert evidence by the Australian Institute of Judicial Administration found that the phenomenon of experts exceeding the parameters of their expertise occurs frequently and in most jurisdictions in which experts give evidence.31 Tribunals need to be vigilant for the straying expert. Indeed the Chief Justice of the High Court has said that:32 “Experts who venture ‘opinions’ (sometimes merely their own inferences of fact), outside their field of specialised knowledge may invest those opinions with a spurious appearance of authority, and legitimate processes of factfinding may be subverted.” 27 See Kalil v Bray [1997] 1 NSWLR 256 at 262 (Street CJ) and 265 (Moffitt P). R v Milk Board; Ex p Tomkins [1944] VLR 187 at 197. See also Collector of Customs (Tas) v Flinders Island Community Association (1985) 7 FCR 205 at 211 (Full Fed Crt). Notice may of course be implicit if it should have been obvious to the parties that the tribunal would do so: Minister for Health v Thompson (1985) 8 FCR 213 at 217 and 224. 29 Collector of Customs (Tas) v Flinders Island Community Association (1985) 60 ALR 717; 7 FCR 205. 30 See JRS Forbes, above n5, at p78-9. 31 Freckelton, I, Reddy, P & Selby H, Australian Judicial Perspectives on Expert Evidence: An Empirical Study, Australian Institute of Judicial Administration, Melbourne, 1999 at 34. 32 HG v The Queen (1999) 197 CLR 414 at [44] (Gleeson CJ). While the concept of “specialised knowledge” is part of the definition of expertise within the Evidence Act 1995 (Cth), the concept of expertise at common law could be seen as “specialised knowledge” to the same degree. See, for instance, Murphy v The Queen (1989) 167 CLR 94. 28 11 How is this to be applied in assessing the expertise of medico-scientific witnesses? In Seltsam v McGuiness, Chief Justice Spigelman said:33 “I would have no difficulty with a medical practitioner drawing on and assessing epidemiological studies. I have great difficulty with an epidemiologist expressing an opinion about causation in the individual case.” His Honour does not provide a reason. With respect, this statement should not be applied as a generalisation. If a medical practitioner is giving expert opinion evidence about the proper interpretation of epidemiological studies, then the question remains whether they are sufficiently expert in that area to do so. 2. The basis rule Similarly to the risks to a correct decision posed by the straying expert, so too opinions given without a proper basis risk “appearing to hold a value which they actually do not command”34 and could potentially be irrelevant to a decision. The basis rule has been called the “prime duty of experts in giving opinion evidence: to furnish the trier of fact with criteria enabling the evaluation of the validity of the expert’s conclusions.”35 The leading case on the basis rule is the judgment in the New South Wales Court of Appeal case of Makita v Sprowles by His Honour Justice Heydon, now a member of the High Court. His Honour stated that the basis rule requires the expert not only to state the information they relied on, but also to “reveal the whole of the manner in which it was dealt with in arriving at the formation of the expert’s opinion.”36 33 Seltsam Pty Ltd v McGuiness (2000) NSWCA 29 at [150]. Freckelton, I, et al., above, n31, at 35. 35 Makita (Australia) Pty Ltd v Sprowles [2001] NSWCA 305 at [59] per Heydon JA. 36 Makita (Australia) Pty Ltd v Sprowles above, n35, at [79] per Heydon JA. 34 12 In other words, the expert must provide the facts, assumptions and the reasoning process which contributed to the inference being drawn by the expert.37 The rationale for the rule is clear. It is for the decision-maker to weigh the facts and determine the probabilities. They cannot do this with respect to expert opinion if they are not properly informed of the expert’s reasoning process.38 If an expert complies with the basis rule, and states all assumptions (including disputed facts or legal propositions), this would appear to have the coincident effect of avoiding any breach of the so-called ultimate issue,39 if that rule has a separate existence anymore. Procedural reforms in the Federal and Family Courts, as well as VCAT, and the Victorian Supreme Court have required expert witnesses to set out in their reports the basis of their opinion, as well as their expertise.40 IV. PROCEDURES FOR EVALUATING EXPERT OPINIONS Judges in the AIJA survey noted the difficulties they had in evaluating expert evidence.41 These difficulties are compounded when tribunals must evaluate two or more conflicting expert opinions, and even more so with respect to causation when experts from different fields reach different conclusions. In the context of cancer causation, these difficulties were noted in the Federal Court case of Tobacco Institute of Australia Ltd v Australian Federation of Consumer Organisations.42 The Consumer Federation had sough injunctive relief against the Tobacco Institute to prevent further publication of an advertisement which stated that there was a lack of scientific proof that passive smoking caused disease in non37 This is the position at common law and under the federal Evidence Act. Makita (Australia) Pty Ltd v Sprowles, above n35, at [67] per Heydon JA. 39 Eggleston, Sir Richard, Evidence, Proof and Probability, 2nd ed., 1983 at 147, cited with approval by in Arnotts Ltd v Trade Practices Commission (1990) 24 FCR 313 (Full Fed Crt) at 350. 40 See Federal Court Guidelines for Expert Witnesses in Proceedings in the Federal Court, 19 March 2004, particularly section 2; Family Law Rules 2004 Rule 15.63; VCAT, Practice Note 2 – Expert Evidence, particularly section 3; Supreme Court (General Civil Procedure) Rules 1996 Rule 44.03. 41 Freckelton, I, et al., above n31, at 54-55. 42 (1992) 111 ALR 61 (Full Fed Crt). 38 13 smokers. The judgment of Justice Hill in the Full Court includes an interesting passage, when comparing epidemiological evidence with carcinogenesis evidence. His Honour said:43 “At the heart of the difficulties which beset a court attempting to deal with the matter is the fact that the scientific community comprises experts from different disciplines, each of which has its own methodology … Each discipline approaches the investigation of causes of disease from a different perspective. It is not possible to accept one approach as in some way preferable to the other.” How do we move towards a resolution to these problems? A preliminary step is to realise that tribunals have discretion over the procedures they employ in the conduct of a hearing. This discretion is subject to the principles of natural justice, and commonly the requirement that hearings proceed with as little formality and technicality as the circumstances permit.44 Natural justice requires that a party be informed of the substance of allegations against them.45 Whether a tribunal should require written reports for expert opinion depends on the appropriate meeting point between the competing demands of natural justice and the requirement that proceedings take place with “as little formality and technicality” as the circumstances permit. Much will depend on the expertise possessed by the tribunal and the parties themselves (as with certain professional disciplinary tribunals). If expert reports are to be considered by the tribunal, then is the tribunal required to give pre-hearing disclosure of those reports? Where a document is long or complicated, a summary may be insufficient to comply with the requirements of 43 (1992) 111 ALR 61 at 118. Refer, for example, to legislation and rules listed in the appendix. At common law, a tribunal has discretion over its own procedures subject to complying with its own governing rules, and the principles of natural justice: See Collier v Hicks (1830) 2 B & Ad 663; 109 ER 1290; Bhenke v Wechsel Johnstone (1885) 2 QLJR 85; TA Miller Ltd v Minister of Housing and Local Government [1968] 1 WLR 992 at 995. 45 Johnston v Miller (1937) 59 CLR 467 at 487. 44 14 natural justice, and in such a case there should be pre-hearing disclosure.46 We say this knowing that in the absence of some specific rule or practice note by a tribunal to the contrary, there is no right to pre-hearing access to the evidence itself.47 But in a complex question of causation, how else is a party to properly respond to medicoscientific opinion? What is more, there would be little to gain in surprising a party with an expert medico-scientific report. This was recognised in the context of court proceedings by judges who responded to the AIJA survey:48 “After weighing up the opportunity and utility of cross-examination by surprise, on the one hand, and the early identification and focus upon the real matters of disagreement between experts, on the other, judges’ preferences decidedly inclined towards the latter.” A tribunal could consider adopting procedures recently introduced in a number of jurisdictions, aimed to reduce the difficulties commonly encountered by adjudicating bodies hearing evidence from multiple experts. The first reform is a pre-trial procedure, and depending on the jurisdiction can require opposing experts to confer with each other, and provide a joint report on what is agreed between them, what is not, the reason for any such disagreement, and what action can be taken to resolve this if possible.49 With respect to the procedure at a hearing, we refer specifically to the most recent procedural reforms in Rule 15.70 of the 2004 Family Court Rules.50 This rule includes the following possible procedures during the hearing. That: an expert witness clarify their evidence after cross-examination; the expert witness give evidence only after all or certain factual evidence relevant to the question has been led, including after a party has closed its case; 46 See, for instance, Official Solicitor to the Supreme Court v K [1965] AC 201. We refer to “evidence”, as opposed to particulars of the allegations. 48 Freckelton, I, et al., above n31, at 6. 49 See Federal Court Rules Order 34A Rule 3(2)(a) & (b), Federal Court Guidelines for Expert Witnesses in Proceedings in the Federal Court, 19 March 2004, section 3; Family Law Rules 2004 Rule 15.69 and Schedule 5 Experts’ Conferences; VCAT, Practice Note 2 – Expert Evidence, particularly section 5; Supreme Court (General Civil Procedure) Rules 1996 Rule 44.06. 50 The Federal Court has similar rules: Federal Court Rules Order 34A Rule 3(c) – (i). 47 15 each expert witness is to be available to give evidence in the presence of each other; each expert witness give evidence about the opinion given by another expert witness; or cross-examination of an expert witness is to be conducted by putting to each expert witness, in turn, each question relevant to one issue at a time, until the cross-examination of all witnesses is completed. These are interesting and novel procedures devised specifically to help decisionmakers resolve problems of comprehension and evaluation when faced with conflicting expert opinion evidence. Procedures like these could be used by tribunals either on a case-by-case basis or by the establishment of model procedural rules for particular types of cases. V. DIFFERENT PERSPECTIVES IN MEDICAL SCIENCE Two subjects which, in their own way, are contentious regarding proof are now introduced, the first being the relationship between life stress and illness, and the second involves the forensic evaluation of complementary or alternative medical treatments (CAM). They are areas where there is likely to be conflicting expert opinions, less basis for some of those opinions, and perhaps questionable expertise. A. Stress and Illness Here stress is defined as the occurrence of serious life events, such as death of a spouse or child, divorce or major work stresses. There is evidence that these can lead to the onset of serious illness, such as cancer or heart attacks, and these events have been rated scientifically on a stress scale.51 There is a small body of epidemiologic evidence which shows a statistically significant positive association between these serious depleting life events, such as Rahe RH and Arthur RJ. “Life Change and Illness Studies: Past History and Future Directions” (1978) 4, JU Human 3–15. 51 16 bereavement, and the subsequent diagnosis of cancer. The individual’s response, as gauged by the degree and duration of upset, also needs to be considered with the event.52 Moreover, these stressful events only show an association with cancer if they are present just 2 or 3 years prior to diagnosis. 53 Given the many years it takes for a cancer to develop, these stresses occur at a time when a tiny, perhaps microscopic and symptomless cancer, is very likely already present. Life stresses alone have never been shown to be a primary cause of cancer, but rather a trigger or a precipitating factor for the growth of such a pre-existing tiny cancer. The proof of the association between life stress and illness, such as heart attack or cancer, is however contentious for several reasons: 1. The scientific evidence is incomplete and the number of properly conducted studies are few. Also, several studies show null results. The possible mechanisms of action have not been extensively studied. 2. Medico-Scientific ethos has not been sympathetic to the concept that stress can precipitate illness. Measurement of an individual’s response to stressful events is difficult. 3. Who are the experts to provide evidence in relation to stress and cancer? To argue the general concept we need an Epidemiologist and a Behavioural Scientist, such as a research oriented Psychologist. To argue the specific case we need a Clinical Oncologist and a Clinical Psychologist. B. Complementary and Alternative Medicine (CAM) Turning now to proof in relation to forensic issues centring on complementary or alternate forms of treatment, it is important to realise nearly half of all Australians 52 53 Kune GA, above n16, at 217–228. Kune GA, above n16, at 222–228. 17 have taken a form of CAM treatment in any one year, and this is increasing.54 Acupuncture, naturopathy, homeopathy, massage, Shiatsu or chiropractic treatment, vitamins, herbs, other nutritional supplements, aromatherapy, pranic healing, yoga, pilates, the list is endless. Who are the experts to give evidence on claims of effectiveness, or on claims of damage due to adverse side effects? On the one hand, there are the medico-scientists and medical practitioners, often with little factual knowledge of these treatments (although this is improving), who for various reasons can be biased against such treatments. On the other hand, there is now in Australia an army of practitioners and sellers of these complementary alternate products, some knowledgeable and well trained, some who seem entrepreneurial, some who at times make extraordinary claims of benefit. Some satisfactory results of CAM have been reported, such as from acupuncture, chiropractic and some herbal preparations. However, the effectiveness and adverse side-effects of many of these products and procedures have not been properly tested and the mechanisms of action are often unknown.55 Our view is that the way forward from this difficult situation needs to be research-led and evidence-based.56 However, there are major challenges to this when contrasted with mainstream treatments such as pharmaceuticals. These challenges include problems with controlled studies, lack of funding for research, lack of training in research methods, not to mention different philosophies of what constitutes health and healing.57 VI. CONCLUSIONS Courts have often stressed the intuitive nature of decisions about causation. Yet decisions cannot be an intuitive free-for-all, but must be based on principle. From the Brooks PM. “Undergraduate Teaching of Complementary Medicine” (2004) 181 MJA at 275. House of Lords, Select Committee on Science and Technology “Complementary and Alternative Medicine” Sixth Report, Summary, 21 November 2000. 56 House of Lords, Select Committee on Science and Technology, above n55. 57 House of Lords, Select Committee on Science and Technology, above n55. 54 55 18 question of proof, to the relevant rules and procedures, it is always the principle or rationale behind the rule which is of importance in tribunals, particular when the requirements of natural justice can vary with the circumstances of each case. We have set out the principles which we believe a tribunal should consider when faced with the need to evaluate medico-scientific evidence, and we have put forward a framework of how the medical scientist approaches proof, who might be the experts to provide this proof, and emerging issues which are contentious even for science at present. So many Australians are using Complementary and Alternative Medicines and therapies, yet there has been little analysis of whether regulation is effective or appropriate for many modalities, and courts and tribunals have had surprisingly little opportunity to examine the scientific and forensic issues raised above. These areas will be increasingly important in the years to come. Of course, avoiding court or tribunal proceedings can be as simple as education. Even once proceedings are commenced, the tribunal no doubt would be assisted by an expert witness educated in the expectations of the tribunal, and in the obligations of expert witnesses themselves. Bodies such as the International Institute of Forensic Studies are making inroads into this area with forensic accountants, forensic engineers and soon hopefully other non-law professionals. Certainly more education is to be encouraged. We greatly appreciate the opportunity to present this paper to the Council of Australasian Tribunals, and we conclude by reciting one of the many commendable objects of the Council as listed in its constitution, being “to develop best practice or model procedural rules based on collective experience of what works”, and we hope that we have contributed to this in some small way. 19 APPENDIX Statutes, Regulations and Rules on evidence and procedures of Victorian tribunals who are registered with the Council of Australasian Tribunals: i. Chinese Medicine Registration Board of Victoria. Chinese Medicine Registration Act 2000 (Vic) s51. ii. Chiropractors Registration Board of Victoria. Chiropractors Registration Act 1996 (Vic) s48. iii. Dental Practice Board of Victoria. Dental Practice Act 1999 (Vic) s50. iv. Legal Professional Tribunal. Legal Practice Act 1996 (Vic) ss407 (duty to act fairly), 408(1) (evidence and procedure). v. Medical Practitioners Board of Victoria. Medical Practice Act 1994 (Vic) s52, and s38G (for Performance Review panel) vi. Mental Health Review Board of Victoria. Mental Health Act 1986 (Vic) ss24(1) & (3). vii. Nurses Board of Victoria. Nurse Act 1993 (Vic) s50. viii. Psychologists Registration Board of Victoria. Psychologists Registration Act 2000 (Vic) s51. ix. Victorian Civil and Administrative Tribunal. VCAT Act 1998 (Vic) ss98(1), (3) & (4), and Practice Note VCAT 2 - Expert Witnesses. x. Victims of Crime Assistance Tribunal. Victims of Crime Assistance Act 1996 (Vic) ss31 (standard of proof), 32 (act expeditiously), 38(1) & (3) (evidence & procedure).