chapter 17 - Nursing Pharmacology
advertisement
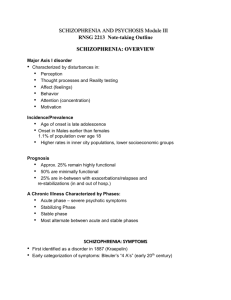
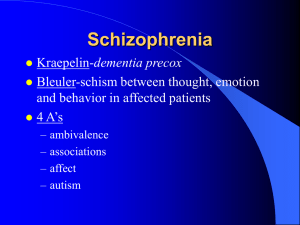
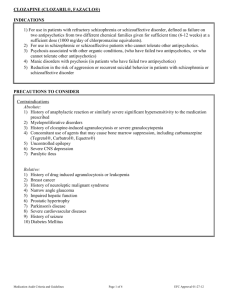
CHAPTER 17 DRUGS FOR PSYCHOSES LEARNING OUTCOME 1 Explain theories for the etiology of schizophrenia. Concepts 1. The nature of psychoses may be acute or chronic and can include such things as delusions, hallucinations, illusions, or paranoia. Delusions are firm ideas and beliefs not founded in reality. Hallucinations are seeing, hearing, or feeling something that is not there. Illusions are distorted perceptions of actual sensory stimuli. Paranoia is an extreme suspicion and delusion that individuals are being followed and that others are trying to harm them. Generally, an individual has disorganized behavior and difficulty relating to others. 2. Psychoses may be classified as an acute psychotic episode, which may occur over hours or days. Chronic psychoses develop over months or years. 3. Psychoses may be attributed to genetic, neurological, and environmental factors. Family members may have been afflicted. An individual may have imbalances in the neurotransmitters in specific areas of the brain, which may be the cause of this disorder. Environmental factors may include brain damage, overdoses of certain medications, chronic alcoholism, and drug addiction. 4. Schizophrenia is a type of psychosis characterized by abnormal thoughts and thought processes, disordered communication, withdrawal from other people and the outside environment, and severe depression. Individuals are at a high risk for suicide. LEARNING OUTCOME 2 Compare and contrast the positive and negative symptoms of schizophrenia. Concepts 1. Schizophrenia is the most common psychotic disorder, with symptoms first appearing in early adulthood. For men, those symptoms peak between age 15 and age 24; for women, between 25 and 34 years. 2. Many symptoms will appear, with some seemingly sudden and others developing over time. These symptoms can include hallucinations, delusions, or paranoia. Also, the patient exhibits strange and irrational behavior; severe depression, alternating rapidly between extreme hyperactivity and stupor; and attitudes of indifference or detachment toward life activities. Deterioration of personal hygiene and/or job or academic perfor mance is seen. Withdrawal from social and interpersonal relationships is also observed. 3. Schizophrenia is characterized by positive and negative symptoms, and proper diagnosis of these symptoms is important for selection of the appropriate antipsychotic drug. Positive symptoms add on to normal behavior and include hallucinations, delusions, and a disorganized thought or speech pattern. Negative symptoms subtract from normal behavior and include lack of interest, motivation, responsiveness, and pleasure in daily activities. Many schizophrenics exhibit an indifferent personality. Symptoms of schizophrenia seem to be associated with the dopamine type 2 receptor. The antipsychotic medication attaches to the dopamine type 2 receptor site and reduces the symptoms of schizophrenia. 4. There is a condition known as schizoaffective disorder. The patient with this condition exhibits symptoms of both schizophrenia and mood disorder. The symptoms include distorted perceptions, hallucinations, and Adams_IRM Ch 17-1 delusions and may be followed by extreme depression. LEARNING OUTCOME 3 Discuss the rationale for selecting a specific antipsychotic drug for the treatment of schizophrenia. Concepts for Lecture 1. An accurate diagnosis of schizophrenia must be made, as other conditions related to drug use, brain neoplasm, infections, or hemorrhage can cause psychotic-like symptoms. 2. The antipsychotic agents do not cure mental illness, and the patient’s symptoms remain in remission only as long as the patient chooses to take the drug. There is no single drug of choice for schizophrenia. Two basic categories of drugs for psychoses are conventional antipsychotic and atypical antipsychotic. The conventional antipsychotic agents include the phenothiazines and phenothiazine-like drugs. The conventional antipsychotic is sometimes called first-generation or typical antipsychotic. They work to treat the positive signs of schizophrenia, such as hallucinations and delusions. They have been used in treatment of psychoses for 50 years. Atypical antipsychotic agents are newer alternatives to phenothiazines and control both positive and negative symptoms of schizophrenia. Antipsychotic drugs are sometimes referred to as neuroleptics. Prototype Drug chlorpromazine (Thorazine) haloperidol (Haldol) LEARNING OUTCOME 4 Explain the importance of patient drug compliance in the pharmacotherapy of schizophrenia. Concepts Management of severe mental illness is difficult. Antipsychotic medications control the symptoms but do not cure the disease. Patients with schizophrenia do not see themselves as abnormal and have difficulty understanding the need for medication. Symptoms of psychosis can be controlled by specific antipsychotic medications. The patient’s symptoms can be controlled as long as the patient takes the medication. Many undesirable side effects are produced. The patient then does not want to comply with the medication regimen, causing more agitation, distrust, and frustration. Selection of the appropriate medication is based on clinician experience, the occurrence of side effects, and the needs of the patient. LEARNING OUTCOME 5 Describe the nurse’s role in the pharmacologic management of schizophrenia. Concepts 1. The role of the nurse in treatment using any type of antipsychotic medications involves careful monitoring of the patient’s condition and providing education as it relates to the prescribed drug treatment. Many body systems are affected and can interact with drugs and alcohol. The nurse must obtain a complete health history, including any long-term physical problems (e.g., seizure disorders, cardiovascular disease), medication use, allergies, and lifestyle information, such as whether the patient smokes or uses alcohol, illegal drugs, caffeine, or herbal preparations. This allows for individualized treatment and may minimize the possibility of adverse reactions. Obtain a baseline health assessment, including liver and kidney function, vision problems, and mental status and, lastly, monitor for extrapyramidal symptoms and report to the physician immediately, as the medication may need to be discontinued. Ch 17-2 Adams_IRM 2. Conventional (typical) antipsychotics: Monitor for decrease of psychotic symptoms. Monitor for side effects such as drowsiness, dizziness, lethargy, headache, blurred vision, skin rash, diaphoresis, nausea/vomiting, anorexia, diarrhea, menstrual irregularities, depression, hypotension, or hypertension. Monitor for anticholinergic side effects. Monitor for alcohol, illegal drug, and caffeine use. Monitor for cardiovascular changes. Monitor for smoking. Monitor for seizures and patient’s environment. 3. Atypical antipsychotic: Monitor RBC and WBC and hematologic side effects. Observe for side effects and anticholinergic side effects. Monitor for decrease of psychotic symptoms and alcohol or illegal drug use as well as caffeine and nicotine use. Monitor the elderly closely. LEARNING OUTCOME 6 Explain the symptoms associated with extrapyramidal side effects of antipsychotic drugs. Concepts 1. Extrapyramidal symptoms (EPS) include lip smacking (tardive dyskinesia); spasms of the face, tongue, or back muscles; facial grimacing; involuntary upward eye movements; jerking motions (acute dystonias); extreme restlessness (akathisia); stooped posture; shuffling gait; and tremors at rest (Parkinsonism symptoms). 2. A possible life-threatening side effect is neuroleptic malignant syndrome (NMS). In this condition, the patient suffers a toxic reaction to therapeutic doses of an antipsychotic drug. The patient exhibits elevated tempera ture, unstable blood pressure, profuse sweating, dyspnea, muscle rigidity, and incontinence. Observe and report to the physician immediately. LEARNING OUTCOME 7 For each of the drug classes listed in Drugs at a Glance, know representative drug examples, and explain their mechanism of action, primary actions, and important adverse effects. Concepts 1. Phenothiazines: Prototype drug: phenothiazine chlorpromazine (Thorazine). The mechanism of action is thought to act by preventing dopamine and serotonin from occupying their receptor sites in certain regions of the brain. The action blocks the excitement associated with the positive symptoms of schizophrenia, although they differ in their potency and side effects. Primary use is for severe mental illness. The significant adverse effects include acute dystonia, akathisia, Parkinsonism, tardive dyskinesia, anticholinergic effects, sedation, hypotension, sexual dysfunction, and neuroleptic malignant syndrome. (See Table 17.2 for a full description of each symptom.) 2. Nonphenothiazines: Prototype drug: haloperidol (Haldol). The mechanism of action is believed to be the same as the phenothiazines; that is, by blocking of the dopamine type 2 receptor, thus reducing the symptoms. Primary use is for severe mental illness. Significant adverse effects are identical to the phenothiazines, although the degree to which a particular effect occurs depends on the specific drug. In general, the nonphenothiazine agents cause less sedation and fewer anticholinergic side effects than Thorazine but exhibit an equal or even greater incidence of extrapyramidal signs. 3. Atypical Antipsychotics: Prototype drug: clozapine (Clozaril). The mechanism of action is largely unknown, but these drugs are thought to act by blocking several different receptor types in the brain. The atypical agents block dopamine type 2 receptors as well as serotonin and alpha-adrenergic receptors. The primary use is for severe mental illness. This classification treats both the positive and negative symptoms of schizophrenia. The adverse effects are fewer with this type of medication, but the obesity and the risk factors associated with it need to be monitored. Adams_IRM Ch 17-3 Prototype Drug chlorpromazine (Thorazine) haloperidol (Haldol) risperidone (Risperdal) LEARNING OUTCOME 8 Categorize drugs used for psychoses based on their classification and drug action. Concepts 1. Conventional (Typical) Antipsychotic Agents: Phenothiazines are thought to act by preventing dopamine and serotonin from occupying their receptor sites in certain regions of the brain. The action blocks the excitement associated with the positive side effect. Examples are Mellaril, Serentil, and Prolixin. Nonphenothiazines are believed to act by the same mechanism as the phenothiazines; that is, by blocking of the dopamine type 2 receptor, thus reducing the symptoms. Examples are Taractan, Loxitane, and Navane. 2. Atypical Antipsychotics: The action is largely unknown, but they are thought to act by blocking several different receptor types in the brain. The atypical agents block dopamine type 2 receptors as well as serotonin and alpha-adrenergic receptors. This classification treats both the positive and negative symptoms of schizophrenia. Examples are Seroquel, Risperdal, and Zyprexa. LEARNING OUTCOME 9 Use the nursing process to care for patients receiving drug therapy for psychoses. Concepts 1. Assessment: Monitor patients’ condition, noting the positive and negative symptoms associated with schizophrenia and other behaviors associated with mental illness. Obtain baseline health assessment including vital signs, height and weight, history of past mental illness, and lifestyle information on smoking and use of illegal drugs, alcohol, and caffeine. Also include current medications and dietary habits. Obtain baseline blood and urine samples as ordered by the physician. Assess the patient’s and the family’s knowledge of psychoses and the medication regimen. 2. Nursing diagnosis: Anxiety related to symptoms of psychosis, side effects of medication; Knowledge Deficit related to new medication regimen; Noncompliance related to lack of understanding and continued use of alcohol and caffeine-containing products. 3. Planning: Goal for patients receiving antipsychotic therapy is to remain compliant with medication regimen and remain free of psychotic symptoms. 4. Implementation: Encourage compliance with medication regimen. Provide additional education regarding medication regimen, such as consultation with clinical pharmacist, written and/or visual education material, and follow-up in local outpatient psychiatric clinics. Evaluation: An ideal outcome criterion for evaluation of the plan of care is the patient to remain free of symptoms related to psychoses. Patients verbalize the importance of taking prescribed medications to assist them in their continued management of the disease. Ch 17-4 Adams_IRM