yeasting 1
advertisement
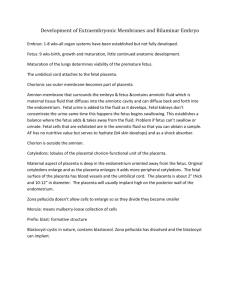
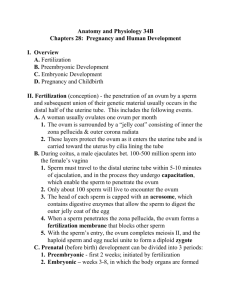
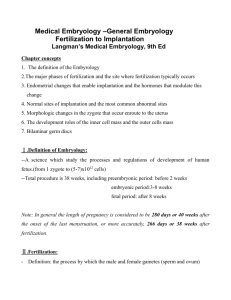
Embryo term is used between 1-8 weeks after which the conceptus is referred to as fetus. After 8 weeks, enter growth and maturation, very little anatomic maturation, all the organs have been formed during embryo but not definitively in size and shape. Lungs maturation determined the survival of the neonate born prematurely around 22-24 weeks. Umbilical cord attaches to fetal side of placenta on the outside. The placenta is the interface between the mother and the fetus Chorion is the outer extra embryonic membrane of the placenta; part of it will become the placenta. Amnion is the extra embryonic membrane surrounding the embryo/fetus; it contains amniotic fluid derived from maternal tissue fluid. It can back diffused from amniotic cavity to Chorion to endometrium (lining of the uterus). Fetus adds fluid to amniotic fluid (fetus urine is not concentrated) at the same time fetus also swallows amniotic fluid that get absorbed in its small intestine, creating a balance. Before skin matures, embryo loses embryonic fluid thru skin and skin keratinizes If fetus cannot swallow, it leads to accumulation of amniotic fluid then polyhydramnios. If fetus cannot add to amniotic fluid, it leads to decrease of amniotic fluid then oligohydramnios. Placenta is used to get rid of wastes from fetus. Fetal cells exfoliate are found in the amniotic fluid, we can examine DNA from these cells collected in the amniotic fluid and get info about the genetic of the fetus, and we can also judge lung maturity using the chemicals present in the fluid. Amniotic fluid has no nutritive value; its main purpose is to maintain the fetus hydrated. The amniotic fluid serves as cushion, fetus has no developing skeleton in them in their first weeks of development, it is mainly cartilaginous, their embryo skeleton is gelatinous (acellular) and cannot withstand the pressure of the uterus placed upon it. The Chorion will then rose rapidly, claim space then amnion and fetus grow within that and the amniotic fluid will provide a buffer for the fetus so that body blows, uterine contraction are not imparted directly to the fetus. The amniotic fluid will also serves as a wedge during parturition when the little one wants to come out. The placenta portion of the Chorion is divided in small lobules called cotyledons; each of them is a functional unit of the placenta. Chorion is tougher than amniotic membrane but amniotic membrane can be durable (amniotic amputations) As placenta develops, it expands out to the periphery, adding more and more tissue to it; leading to more cotyledons of relatively small size. The placenta is about 12 inch diameter plate and 2 inches thick. umbilical cord attached and vessels radiate on fetal surface, around edge is the amnion and chorion, and in middle is thinner tissue which is amnion, twins develop within 1 chorion but each have their own amniotic twin (identical twins-embryo divided early into two separate units) fraternal twins that have derived from separate oocytes will have each their own separate chorion and separate amnion. MRI do not damage fetus but try not to use unless you have to. Shared circulation between the two placentas is not bad in human but can be deleterious in cows No CT scan and x-rays on pregnant woman. High on posterior wall within uterine cavity=implantation Menses is the beginning of a cycle; this is when the endometrium of the previous cycle is lost, that will last approximately 3- days during that time the follicles in the ovaries will continue to develop and release a lot of estrogen so estrogen will cause the lining of the uterus to proliferate to replace what has been lost. About mid cycle, usually one follicle will rupture, releasing one secondary oocyte which will be picked up by the fallopian tube and begin the transport down the uterine tube to the uterine cavity. If it is fertilized, development will begin in the distal portion of the uterine tube. The conceptus will then be transported down the fallopian tube; it takes about a week for that transport to occur. During this time cells are developing via mitosis and are surrounded by zona pellucida. As cells divide, we increase number of cells but each cell become smaller, dividing the cytoplasm and dna component into smaller and smaller unit cytoplasmically but of course the dna is replicating; that adds more and more cells but because the cells are still surrounded by zone pellucida, they cannot emerge so each cell is getting smaller. During this time the cells are organizing themselves and as the conceptus enters the uterine cavity, a little cavity develops within the cells here; this cavity is called a blastocoel (blast means primitive/formative structure). The cells at this level form what is called a blastocyst and the space within the blastocyst is called a blastocoel (coel is short for coelom which means a body cavity). As cells enter the uterus cavity, the zona pellucida breaks down and dissolves allowing the conceptus to become in contact with the lining of the endometrium and begin to implant. 2 weeks after ovulation, the corpus luteum degenerates and its function of producing progesterone ends. Progesterone role was to ripen and maintain the endometrium. Estrogen produced by developing follicles causes regeneration of endometrium. The corpus luteum effect of producing progesterone only lasts 14 days after ovulation causing endometrium to degenerates- shift to menses period and beginning of new cycle. Uniform /constant period here is between the time of ovulation and onset of next menstrual period, the variable time is between onset period and ovulation. First thing conceptus has to do is going to be putting out substances that will notify the mother body of its presence so that the mother body maintains the corpus luteum to maintain progesterone to maintain endometrium so that the conceptus has a place to live. During follicle development, zona pellucida is produce partially by the oocytes and partially by the cells surrounding it called corona radiate. Zona pellucida is acellular substance surrounding the oocytes; it controls/monitors the environment the oocytes is developing in. later on it will help to guide the spermatozoids in fertilizing the oocytes, will hold the first mitotic cells together preventing them from wondering away, it will prevent implantation until the conceptus is hold enough to implant properly, then disappears. The conceptus = product of fertilization= embryo proper and extra embryonic tissues Corona radiate are follicular cells that are released with the oocytes, they make the ovulated mass easy for the uterus to handle. Spermatozoa that have made it to the cervical canal, thru the uterine cavity into the uterus tube and had travelled a distance of about 8-10 inches in the fallopian tube will approach the ovulated mass which is emitting signal. 1st sperms that come in contact with oocytes, will release their acrosomal enzymes which will digest the corona radiate. This will allow others sperms approaching at later time to be able to make contact with the z. pellucida that has chemical receptors on it to help sperms to dock and attach to z.pellucida and then release their acrosomal enz which will digest a path trough z.pellucida. a sperm makes it thru z.pellucida, fuse with oocytes membrane: upon membrane fusion, mitochondria+nucleus of sperm move in cytoplasm of oocytes, triggering of cortical reaction where enz that were in vesicles at the periphery of oocyte membrane are released- chemical changes in z.pellucida- sperms can no longer digest their way thru. Oocyte retracts a little bit from z.pellucida creating a gap between z.pellucida and outer cell membrane of oocyte. Peristaltic movements push egg down uterine cavity, as egg is moving down it releases chemicals that will diffuse thru fluid and get picked up by blood supply within uterine tube then circulate within the mother there are the pregnancy factors that early tests are based upon. About 5-6 days after fertilization, conceptus moves into uterine cavity, loses z.pellucida, swells up and enlarges, developing the blastocoel. About day 7, it will start implantation in uterus. When we begin to see and outer and inner cell mass, those cells are no longer multipotent, the outer cell mass will become supportive tissue and the inner will become embryo proper. Endometrium= mucosal lining of the uterus, consists of glandular epithelium, acellular stroma and maternal blood vessels Myometrium= muscular wall of uterus Implantation= growing into or moving into another structure. Here it means the moving of conceptus from uterine cavity into the stroma of endometrium. Human and primates have interstitial implantation; the conceptus ends up within the interstitial intercellular space of endometrium, it loses contact with uterine cavity (becoming kind of invasive as oppose to other animals where the conceptus stay in the uterine cavity without implantation in endometrium) Implantation is not a one way but reciprocal: the endometrium is releasing substances that attract the conceptus; the conceptus is releasing substances that will trigger changes within endometrium. They are working back and forth, with proper coordination we will have a successful implantation; if it not coordinated there will be no implantation. Some chemicals are utilized to interfere with the reciprocal interaction such as birth control pills, IUD. Decidua= fall away; it is altered endometrium stroma. As conceptus invades stroma, the stroma will be stimulated to change its structure/nature. The fibroblast will become enlarge and have more glycogen substances within them, they will be factors that decrease the ability of the lymphocytes to recognize foreign materials. At time of parturition, most of decidua is lost as part of after birth hence its name. It has 3 portions: Decidua basilis: altered endometrium between conceptus and Myometrium Decidua capsularis: altered endometrium between conceptus and uterine cavity, making a capsule over the conceptus at implantation site. It is temporary, as the conceptus enlarges, the blood supply to d.capuslaris will be compromised, perfusion will drop and the tissue will degenerate. But by that time the conceptus is well anchored in d.basilis and is also approaching the size that will allow it to be making contact with the whole wall of the uterine cavity so there is no danger of dislodging the conceptus when d.capsularis degenerate. Decidua parietalis: rest of altered endometrium Decidual reaction occurs at implantation site but eventually all the endometrium undergoes a decidual reaction. The inner cell mass of the conceptus will become embryoblast and give rise to the embryo proper. The embryoblast can be further divided into epiblast and hypoblast. Epiblast=most numerous, will ultimately give rise to ectoderm, mesoderm and endoderm of embryo proper Hypoblast= temporary cell layer, will give rise to extra embryonic mesoderm The outer cell mass also called trophoblast (tropho= to feed or support), they differentiate into 2 types of tissues: - Cytotrophoblasts= individualized discrete cells, they tend to be reserved cells that will develop into something else and they will become depleted or reduce in number as development proceed. They will merge together, their cell membranes will open up and their cytoplasm will merge to give rise to the anatomic syncytium known as the syncytiotrophoblast - Syncytiotrophoblast= syncytium is a multinucleated cytoplasmic mass or cell. It is a differentiated specialized tissue. It is the secreting portion of placenta and produces placental hormones (steroid hormones, proteins hormones, etc) it is the part of the placenta that will come in contact with maternal blood. Lacuna=membrane bound spaces within the syncytiotrophoblast; it is empty at the beginning but will ultimately contained maternal blood and will be known as the intervillin space within the placenta. They will coalesce to form large spaces. On the inside of the Cytotrophoblasts (outer cell mass), hypoblastic cells (inner cells) have migrated down and are given rise to extra embryonic mesoderm. As implantation continues, cytotrophoblastic cells proliferate and begin to grow into Syncytiotrophoblasts- more syncytio in the process. As they grow in, extra mesoderm follows (1st thing we see are column of cytotropho growing into syncytiotropho then the later become kind of hollow as extra mesoderm grows in and finally embryonic blood vessels will develop within extra mesoderm (these are extra embryonic blood vessels and will link up with circulatory system developing within the embryo proper). With time the cytotro will continue to migrate to the syncytio, come to the outside where they will continue to proliferate and spread between syncytio and decidua. Before the cytotro shell develops, the endometrium has changed into decidua; it can no longer recognize foreign substances. Syncytio come in contact with maternal blood and tissue. Syncytio does not elaborate antigens but cytotro does elaborate antigens Cytotro come in contact with maternal tissue but not maternal blood. Primary chorionic villi will consist of syncytio + cytotro, 2ry will be syncytio+cyto+extra mesoderm, 3ry= syncytio+ cyto+ extra mesoderm+embryonic fetal blood vessels. These are hanging into the blood filled intervillin space.