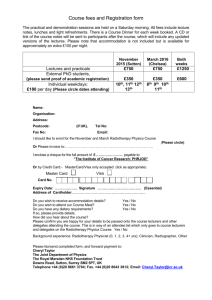
INFORMATION FOR PATIENTS RECEIVING HORMONE

ProtecT study
Your Guide to
Radiotherapy Treatment
This information booklet is designed for men receiving radiotherapy treatment within the ProtecT study. It explains what will happen to you when you have radiotherapy and how you will be looked after in the future.
What is radiotherapy?
Radiotherapy is the use of x-rays to treat cancer. This treatment works by destroying the cancer cells in the prostate gland. The type of radiotherapy you will be having is called ‘conformal radiotherapy.’ The aim of conformal radiotherapy is to deliver the Xrays directly onto the tumour to destroy the cancer cells and avoid damage to surrounding tissue and organs. Some normal cells will be affected by radiotherapy but they repair themselves more effectively than cancer cells. It has been shown that, in general, radiotherapy is more effective if men have hormone treatment before and during the treatment, and so you will be offered hormone treatment as part of your radiotherapy.
You may also have heard of brachytherapy. This is a form of radiotherapy where small radioactive ‘seeds’ are placed in the prostate which emit X-rays. Brachytherapy is one of a number of possible treatments not available within the ProtecT study. You have been accepted for the study because in your case there is no evidence that brachytherapy is any more effective than high-dose conformal therapy (the type that we are offering you), and indeed, only some men who are suitable for conformal radiotherapy might be suitable for brachytherapy. There have not been enough studies of the outcome following brachytherapy for us to believe that it is as good as conformal radiotherapy. If you wish to discuss this further, please talk to the specialist nurse, urologist or radiotherapist.
What will happen to me when I have hormone treatment?
The purpose of hormone therapy is to shrink the prostate and the cancer by stopping the production of male hormones (particularly testosterone). Quite soon after you have been allocated to or decided to have radiotherapy, you will be started on a 3-week course of
2 02/10/2003
tablets which begin to reduce your hormone levels. After about 4-10 days, you will be given your first hormone therapy injection.
Injections will be given once a month before and during the radiotherapy treatment.
Hormone therapy can have some side-effects which usually stop when the treatment is stopped. While you are having the hormone injections, you will probably become impotent (you will not be able to have an erection). You may also find that you feel tired, may gain weight, have hot flushes and breast enlargement or tenderness. If you experience these symptoms, you may want to discuss them with the specialist nurse or your GP. They should disappear when you stop the hormone injections.
What will happen to me when I have radiotherapy?
Conformal radiotherapy requires a period of detailed planning to ensure the X-rays are targeted accurately onto the prostate. Your first or second appointment will be for a CT (computerised tomography) scan and possibly also an MRI (magnetic resonance imaging) scan.
The CT and MRI scans will enable the radiotherapist to plan exactly where the x-ray treatment will be directed. You will usually be asked to lift up your shirt and loosen your trousers and will be given a towel to cover you once you are in position. It is important that you lie in the same position and stay as still as possible during the treatment.
Radiotherapy treatment is given in many short doses, called fractions, to avoid damage to healthy cells. Treatment for localised prostate cancer is usually divided into 37 fractions. Your actual treatment will take about 15-20 minutes each day for about seven to eight working weeks. You do not have treatment at the weekends.
Radiotherapy treatment is painless. A radiographer will take you into the treatment room and you will be positioned correctly for treatment. The radiographers will observe you on TV monitors outside the room and if you need to, you can attract their attention.
The radiotherapy machine will rotate around your body and give the
X-ray treatment in different directions as programmed by the
3 02/10/2003
computer. The machine does make some noise but there is often some music playing in the treatment room.
Once your treatment is finished you can get dressed and go home.
During your treatment you will be seen at least once every fortnight by one of the specialists to see how you are coping with the treatment and any side effects.
What are the side effects of radiotherapy?
Radiotherapy can result in some side effects that start straight away and get better (common, early effects) and others that continue or start six months to two years after treatment (rarer, late effects).
Early effects: many will experience a change in bowel habits during treatment, including some diarrhoea, bleeding and and urge to go; or urinary symptoms such as having to go more often during the day and night, or going with discomfort. The diarrhoea is often mild and changing your diet to low fibre may be all that is required to control it. A low fibre diet means reducing the amount of fruit, vegetables and bran you eat. A more detailed diet is available from the radiotherapy staff should you require it. If the diarrhoea is persistent your specialist can prescribe medication to help. Increasing the amount of fluids you drink will help urinary symptoms. It may also help to drink water with alcohol and to avoid drinking tea, coffee, spirits or fizzy drinks as these can irritate the bladder and make the symptoms worse. Your urine may be checked regularly to rule out any infection. There are drug treatments that can help to ease these symptoms if they become troublesome. Tiredness is also often experienced. It is a good idea to take it easy while you are having radiotherapy treatment and afterwards. The tiredness should wear off when you stop the treatment, but if you are concerned about it, talk to your doctor or specialist nurse.
These early effects tend to come on and get worse during the treatment period, but most will settle and go away a few weeks after treatment finishes.
4 02/10/2003
Late effects: these are noticed by only about 5 in 100 men undergoing conformal radiotherapy. They may be early effects that do not get better on their own, or they may develop 6 months to 2 years after treatment. Bowel symptoms are the most common, although urinary symptoms can also occur, including, very rarely, incontinence. While treatments are available to help, these late effects may continue and not get better - but it is important to remember this only happens to a small number of men.
As indicated above, hormone treatment will usually cause impotence
(the inability to have an erection). Impotence can also be caused by the radiotherapy treatment itself. It is difficult to be precise about the risk of impotence following radiotherapy. The best data that we have suggest that about 4 men in every 10 having radiotherapy will be impotent afterwards. However, the risk of impotence varies depending on the level of sexual activity before the treatment and the damage that is done to the blood supply by the radiotherapy treatment. If you have any concerns about sexual function, please discuss these with the doctor or specialist nurse. There are a number of treatments that can help if you find that you are impotent after treatment, e.g. viagra or apomorphile with hormones.
Some people may develop a skin reaction whilst having radiotherapy, often between the buttocks. It is important to wash the treated skin gently every day and pat dry. Do not use creams, moisturiser or talcum powder, and keep the treated skin away from direct sunlight or heat such as sun lamps. If a reaction does occur, your doctor, specialist nurse or radiographer will be able to advise on the best method of treatment and provide you with ointment if necessary.
What happens after the radiotherapy treatment finishes?
Once you have completed the course of radiotherapy, you will be given an appointment with the doctor or specialist nurse in the
ProtecT study review clinic after approximately 6 weeks. You will then be seen every 3 or 6 months.
During these appointments a blood test will be taken to measure your PSA (prostate specific antigen) level. This measures the activity
5 02/10/2003
in the prostate and is useful to assess whether the cancer has been destroyed by the radiotherapy. You will have the opportunity to discuss any worries or concerns that you may have about your treatment.
Can I keep a record of my PSA results?
We have provided a chart at the end of this booklet so that you can plot your PSA levels. After radiotherapy treatment, the PSA level will usually fall to less than one. The level could rise slightly after hormone treatment stops. The chart can be filled in each time you have a PSA test result. This will allow you to have a record to hand of your own PSA results and any changes that have occurred.
It is important to remember that the aim of the radiotherapy treatment was to destroy the cancer cells and in the majority of cases, this will be successful. However, in a small number of cases, a small part of the tumour may not have been destroyed and may begin to grow. It is important to remember that prostate cancer is slow growing in most men and any change may happen over a long time period. Further treatment is unlikely to be necessary in most cases, but may be needed if there is detectable change over a short time period.
In the ProtecT study, we aim to monitor all patients so that we can identify any changes in the cancer long before you experience any symptoms. The PSA test is the most sensitive way to do this. We will be keeping a very close eye on your PSA levels. The next section explains how we will decide if the cancer is changing and what we would do if this does happen.
How can you tell that the cancer is changing or growing?
The ProtecT protocol guidelines set out levels of change in PSA which may indicate that the cancer is growing and which would then need further investigation. Following radiotherapy, if your PSA is seen to rise, you will have a further PSA test. If you have three consecutive tests which show a rise in PSA level, each at least one month apart you would be invited to a special ‘review’ appointment with the study urologist.
6 02/10/2003
Review appointment with the study urologist
At the review appointment the study urologist will review the pattern of PSA levels and discuss them with you. The urologist will also consider two other factors: a) Clinical stage
The clinical stage is an assessment of where the cancer is in the prostate, particularly whether it is still inside the gland. Measures are usually made using trans-rectal ultrasound (TRUS). You had this when you had the biopsy. The urologist may ask you to have a
TRUS (This will not require you to have a repeat biopsy). b) Grade
A Gleason grade score gives an indication of how quickly the cancer is likely to grow. The grade is assessed by examining tissue taken at biopsy. A pathologist examines the tissue under a microscope and gives each area of tissue a score from 1 to 5. A near-normal appearance will be given a low score (1 or 2). In the case of more active cancer, in which the structure of the tissue is very disrupted, the cancer will be scored 3 to 5. To get a complete picture, a number of samples of tissue are examined and each is scored. The grades of the two most common types are then added together to give a score with a maximum of 10. For example a Gleason grade score of 3 + 3 =
6 would indicate a medium grade cancer, a score of 2 + 1 = 3 a low grade cancer and a score of 4 + 4 = 8, a higher grade cancer.
Taken together the stage and grade of a cancer help to predict how the cancer might behave. But the stage and grade are only guides to what might happen and cancers do not always behave in the way that might be expected from their stage and grade. While on average a higher grade cancer is likely to grow more quickly than a lower grade cancer, it is still not clear which treatment would be best for those with a higher grade cancer.
If the urologist decides after examining these factors that the cancer is changing, all the risks and possible outcomes of each of the treatments available to you will be discussed with you again so that you can decide what you would like to do. You will also be able to
7 02/10/2003
discuss these issues with others if you would like to – for example the specialist nurse or a radiotherapist. An appointment could also be arranged in response to any other concerns that you have.
What treatments would be available if the cancer starts to spread?
As we have indicated above, the aim of the monitoring after radiotherapy treatment is to ensure that we are aware of any changes in the cancer at an early stage. If the cancer did start to grow, your treatment options would be to have hormone treatment and close monitoring or to have active monitoring with no immediate treatment.
Hormone therapy:
The purpose of hormone therapy is to shrink the remaining prostate cancer by stopping the production of male hormones (particularly testosterone). This can be achieved by removing the testicles or by taking or injecting medication. It is possible that this treatment may also limit the growth and spread of the prostate cancer. Hormone therapies usually cause sexual impotence (the inability to have an erection), can lead to weight-gain and other side effects including tiredness, hot flushes and breast enlargement and tenderness.
Again, we would explain to you in detail the advantages and disadvantages of these treatments and give you as much time as you want to reach a decision.
If the cancer does spread, it does not necessarily mean that you will experience any symptoms, but over a long period some symptoms relating to the growth of the cancer may occur. These may include urinary symptoms or pain from the development of other tumours
(also called metastases), usually in the bones. The treatment for metastases in the bones is hormone therapy. It is important to emphasise that the development of such symptoms among men in the ProtecT study will be very rare – but it is possible and this is why it is covered in this booklet.
As you get older
It is also important for you to know that urinary symptoms become increasingly common in men (and women) as they grow older.
8 02/10/2003
Symptoms include having difficulty passing urine, or having to go often, including having to get up at night. Such symptoms are usually caused by the normal growth of the prostate that happens as men age. In a small number of cases, however, such symptoms may be caused by the growth of the cancer. Other symptoms such as blood in the urine may require further investigation – if you experience this, you should go to your GP or mention it to the urologist or specialist nurse when you see them. There are drug treatments that can ease urinary symptoms. If they become very troublesome, you might also be able to have an operation – a transurethral resection of the prostate. It is also important for you to remember that aches and pains in your bones may also become more common as you get older. It is unlikely that you will develop tumours in your bones, but if you are worried about bone pains, contact your GP or ProtecT study nurse.
At any time following your treatment, you may request a fast-track appointment with the ProtecT study nurse, to discuss any symptoms that concern you.
Conclusion
This information booklet has outlined what radiotherapy treatment in the ProtecT Study will involve and what may happen in the future once you have embarked upon this treatment. We have covered what the treatment options may be if the cancer does spread.
However it is important to remember that most men having radiotherapy will make a good recovery and get on with normal life without having to worry about prostate cancer.
Some of the information provided in this booklet differs from that provided by a number of cancer charities and other sources. This is because at present the evidence surrounding the effectiveness of prostate cancer treatments is uncertain – that is why we are carrying out the ProtecT Study. During the course of the study it is possible that further information may become available which would allow us to advise you differently with regard to particular treatments. If this happens we will arrange a special appointment to let you know.
9 02/10/2003
Approximately six months after you were allocated to or chose your treatment, you will receive a follow-up questionnaire in the post to complete. A pre-paid envelope will be provided. You will then be seen once a year by the ProtecT study team to find out how you are getting on and you will be asked to complete an annual questionnaire. Please remember that at any time, if you have any questions, worries or concerns, you are welcome to ask to see the
ProtecT nurse co-ordinating the follow-up care of radiotherapy patients.
10 02/10/2003
Record of PSA levels over a five year period
0 1 2 3
Years since radiotherapy
4 5
11
12