Microhematocrit Determination SOP
advertisement
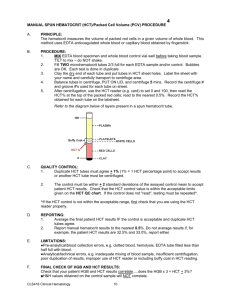
Document Number: Pro64-C-02 Effective (or Post) Date: 23 Jan-09 Review History Date of last review: Na Reviewed by: Heidi Hanes SMILE Comments: This document is provided as an example only. It must be revised to accurately reflect your lab’s specific processes and/or specific protocol requirements. Users are directed to countercheck facts when considering their use in other applications. If you have any questions contact SMILE. Author: Penny Stevens Copy _____ of ___ Effective Date: HEMATOLOGY SECTION D. MANUAL TESTS D.3. MICROHEMATOCRIT DETERMINATION D.3.1. PRINCIPLE: 1. When anticoagulated whole blood is centrifuged, the space occupied by the packed red blood cells is defined as the hematocrit (HCT), and is expressed as the percent of red blood cells in a volume of whole blood. Because of its simplicity and reproducibility, the hematocrit is one of the more accurate hematology tests. 2. A low hematocrit can be an indicator that the patient is suffering from anemia i.e., blood loss, iron deficiency, B12 or folic acid deficiency, hemoglobin disorders and Thalassemia. A high hematocrit can be an indicator that the patient is suffering from Polycythemia. D.3.2. SPECIMENS: 1. Whole blood anticoagulated with EDTA or heparin is acceptable. 2. Capillary blood collected in heparinized capillary tubes may also be used. 3. If anticoagulated whole blood requires a manual HCT, a plain (non-anticoagulated) capillary tube must be used to avoid over-anticoagulation of the specimen. D.3.3. EQUIPMENT & REAGENTS Equipment: 1. Plastic Clad Micro Hematocrit Tubes, Plain. Check for uniformity and gf damage before placing into service. 2. Sealing clay Page 1 of 7 D. Manual Tests D.3. Microhematocrit Determination 3. Microhematocrit reader device 4. Microhematocrit centrifuge D.3.4. CALIBRATION: Not Applicable D.3.5. QUALITY CONTROL: 1. A control is run daily using a commercial normal whole blood control with a known value. Document the value, and enter the value into (your laboratory system). 2. Verify that the result obtained is within range for the control used. If the result is out of range, repeat the procedure. When the result becomes out of range for second time, notify the Hematology supervisor immediately. Document action taken. 3. All tests are run in duplicate to eliminate errors caused by leakage. 4. The results of duplicate hematocrit determinations should agree within + 2%. If results obtained are not within this tolerance limit, the entire procedure must be repeated. All other results are acceptable providing the normal control is within range. 5. Everytime that the lot number is changed, control should be run 20 times before using the new lot number of control for verification of the reference range. Annotate values. D.3.6. PROCEDURE: 1. Mix the sample well and fill two (2) capillary tubes approximately two-thirds full. 2. Seal the dry end with sealing clay. 3. Place capillary tubes in opposite slots of microhematocrit centrifuge with the clay-filled ends against gasket. Be sure to note position number on the (your laboratory system) labels, if spinning specimens from more than one patient. 4. Place the head cover on centrifuge; tighten securely and close the top. Centrifuge the capillary tubes using the predetermined maximum packing time. 5. Open the lid, remove the cover, and remove capillary tubes one at a time. 6. Using a microhematocrit reading device (Refer to figure 1, page 2, Maximum Packing Time SOP), determine the HCT. Buffy coat should not be included in the reading, which should be taken below the buffy coat (Grayish-red layer of leukocytes and platelets). Page 2 of 6 D. Manual Tests D.3. Microhematocrit Determination 7. Results should agree within + 2% for the patient's two samples. 8. Enter results into (your laboratory system). NOTE: Visible hemolysis of the sample after centrifugation must be documented in (your laboratory system). D.3.7. CALCULATIONS: Not Applicable D.3.8. INTERPRETATIONS & REPORTING RESULTS: A sticker is recorded on the microhematocrit log with the value and initials of technician. Result value in (your laboratory system). Refer to panic values next to normal values for critical results. The results will be reported immediately to the requesting Physician, clinic or ward, and documented on (your laboratory system). (Refer to the Critical Values SOP). D.3.9. PROCEDURAL NOTES: 1. SOURCES OF ERROR: 1.1. Excess anticoagulant decreases the HCT value because of shrinkage of erythrocytes. 1.2. Insufficient mixing of blood before obtaining the HCT sample may decrease or increase the HCT, depending on which part of the specimen is drawn principally into microhematocrit tube. 1.3. Improper sealing of capillary tube decreases the HCT because of leakage of specimen, erythrocyte loss is greater than plasma loss. 1.4. Inadequate centrifugation or allowing tubes to stand too long after centrifugation increases the HCT. Results should be read within ten (10) minutes of centrifugation. 1.5. Including the buffy coat in the reading increases the HCT. 1.6. Improper use of the HCT reader may increase or decrease the HCT, due to parallax (the apparent difference in position of an object, as seen separately by one eye and then the other, or by changing the position of the head). 1.7. Trapped plasma (the small amount of plasma that remains in the erythrocyte portion of the spun HCT even when proper centrifugation is used) may cause the HCT to be falsely increased. 1.8. Certain abnormal erythrocyte shapes (e.g., spherocytes and sickle cells) inhibit complete packing. Page 3 of 6 D. Manual Tests D.3. Microhematocrit Determination 1.9. Dehydration can falsely increase HCT because of fluid loss, which causes a decrease in plasma volume. 1.10. When obtaining blood specimen, leaving the tourniquet on the arm too long causes hemoconcentration, which falsely increases HCT. 1.11. Difficult venipuncture or skin puncture may introduce interstitial fluid to the sample, causing a falsely decreased HCT. 1.12. Hemolysis also causes a false decrease in HCT. 2. NORMAL VALUES: AGE <1 day 1-3 days 2 weeks 1 month 2 months 6 months 2 years 2yrs - 6yrs 6yrs 12yrs 12yrs 18yrs male female Adult male female REF LOW 42 45 41 33 28 31 33 34 REF HIGH 60 67 65 55 42 41 39 40 PANIC LOW 37 39 35 27 20 25 25 25 PANIC HIGH 65 72 71 61 50 50 50 50 35 45 25 58 36 37 50 45 20 20 60 60 42 37 52 47 20 20 60 60 D.3.10. APPENDICES: 1. SOP Validation Form and SOP Change Control 2. SOP Approval 3. Microhematocrit Maintenance Quality Control Worksheet D.3.11. REFERENCES: 1. Gunn, Veronica L.; Nechyba, Christian; The Harriet Lane Handbook; Mosby Book Publisher, 2002, Pages 284 – 285. 2. Brown, Barbara A.; Hematology: Principles and Procedures, Sixth Edition; Lea and Febriger book Publisher, 1993, pages 85-87. Page 4 of 6 D. Manual Tests D.3. Microhematocrit Determination 3. Lotspeich-Steininger; Clinical Hematology: Principles, Procedures, Correlation, C. V. Mosby Book Publisher, 1992, Pages 110-112. SOP VALIDATION SOP NAME: D.3. Microhematocrit Determination Clear and specific title and principle: Comments: yes / no All necessary supplies, equipment, and materials are listed: Comments: yes / no SOP is sufficiently detailed to be understood but not overly complex: Comments: SOP text adequately describes process/procedure: Comments: SOP accomplishes purpose: Comments: yes / no yes / no yes / no Reviewed by: (Name & Title) Signature: __________________ Date: __________________ SOP CHANGE CONTROL Date Change QA Page 5 of 6 OIC Med. Dir. D. Manual Tests D.3. Microhematocrit Determination Page 6 of 6 D. Manual Tests D.3. Microhematocrit Determination SOP APPROVAL SIGNATURE DATE PREPARER QA COORDINATOR LABORATORY OIC MEDICAL DIRECTOR ANNUAL REVIEW REVIEWER SIGNATURE DOCUMENT COPY CONTROL LOCATIONS DATE REVIEWER SIGNATURE DATE DATE: ___________# COPIES __________ DATE SOP RETIRED: __________ Page 7 of 6