Chapter 14 Autonomic Nervous System
advertisement

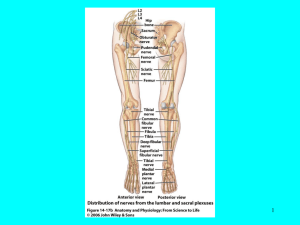
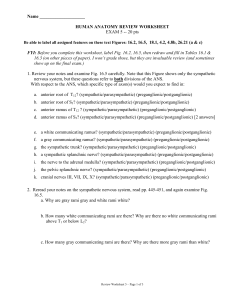
Chapter 14 Chapter 15 Autonomic Nervous System Neural Integration Lecture # 33, 34 Objectives: 1. Define autonomic nervous system and explain its relationship to the peripheral nervous system as a whole. 2. Compare the somatic and autonomic nervous systems relative to effectors, efferent pathways, and neurotransmitters released. 3. Compare and contrast the general functions of the parasympathetic and sympathetic divisions. 4. For the parasympathetic and sympathetic divisions, describe the site of CNS origin, locations of ganglia, and general fiber pathways. 5. Define cholinergic and adrenergic fibers, and list the different types of cholinergic and adrenergic receptors. 6. State the effects of the parasympathetic and sympathetic divisions on the following organs: heart, blood vessels, gastrointestinal tract, lungs, adrenal medulla, and external genitalia. 7. Describe the levels of control of autonomic nervous system functioning. 8. Define EEG and distinguish between alpha, beta, theta, and delta brain waves. 9. Compare and contrast the events and importance of slow-wave and REM sleep. 10. Describe consciousness clinically. Autonomic Nervous System: motor division of PNS Consists of motor neurons that innervate smooth and cardiac muscle and glands. Motor units of ANS consist of two neuron chains and the muscles they innervate. Hypothalamus is in control. Divided into sympathetic and parasympathetic divisions. Preganglionic neuron: found in brain or spinal cord; preganglionic axon is lightly myelinated and synapses with postganglionic neuron. The postganglionic neuron begins in ganglion outside of CNS. Postganglionic neuron: The postganglionic, unmyelinated neuron begins in ganglion outside of CNS and extends to the effector. Conduction, obviously, is slower, due to lack of myelination. Neurotransmitters: Norepinephrine (NE) is released by postganglionic neurons of the sympathetic division. Acetylcholine (ACh) is released by postganglionic neurons of the parasympathetic division, and all preganglionic neurons of the ANS. Dual Innervation: The same visceral organs are served by both divisions to counterbalance each other’s activities and to maintain homeostasis. Parasympathetic Division: usually in control of our visceral organs; works during nonstressful situations. Nicknamed the “feed or breed” response. Body energy use is low. Effects are of short duration and localized. Nerves originate from the craniosacral region of the spinal cord. Ganglia are close to organs, making preganglionic neurons long and postganglionic neurons short. Sympathetic Division: works during stressful situations. Nicknamed the “flight or fight” response. Body energy use is high. Effects are of long duration and widespread (effuse). Nerves originate from the thoracolumbar region of the spinal cord. Ganglia are located in a chain close to spinal cord (white chain ganglia), making preganglionic neurons short and postganglionic neurons long. Cholinergic fibers: those fibers which release Ach (the parasympathetic pre/postganglionic and the sympathetic preganglionic) and the receptors for such. The receptors come in two types: 1. Nicotinic: ACh binding is stimulatory, found in all ganglionic neurons. 2. Muscarinic: ACh binding is either stimulatory or inhibitory; found on all effector cells that are parasympathetic target organs and sweat glands. Adrenergic fibers: those fibers which release NE (sympathetic postganglionic) and the receptors for such. The receptors come in two types: 1. alpha (): effect of NE/epinephrine is stimulatory. 2. beta (): effect of NE/epinephrine is inhibitory (except the receptors of cardiac muscle which are stimulatory). Effects of Divisions Target Organ/System Parasympathetic effects Sympathetic effects Eye (iris) Stimulates constrictor muscles to constrict pupil Stimulates secretory activity Stimulates dilator muscles to dilate pupil Inhibits secretory activity No innervation Stimulates sweating Glands (lacrimal, nasal, pancreas, salivary, gastric) Sweat glands Adrenal medulla No innervation Arrector pili muscle No innervation Heart muscle Decreases rate; slows and steadies heart Constrict Stimulates release of epinephrine Stimulates to contract (goosebumps) Increases rate and force of heartbeat Dilate Contraction of wall of bladder, relaxes sphincters, promotes voiding Constricts bronchioles Relaxation of bladder wall, constricts sphincters, inhibits voiding Dilates bronchioles Digestive tract organs Increases peristalsis and secretion of digestive juices, relaxes sphincters Liver No innervation Gall bladder Kidney Causes gall bladder to contract to expel bile No innervation Decreases activity of glands and muscles of digestive system and constricts sphincters Epinephrine stimulates release of glucose into blood Relaxes Penis Erection Vagina/clitoris Vasodilation Heart: coronary blood vessels Bladder/urethra Lungs Blood vessels Causes vasoconstriction, decreases urine output Ejaculation Contraction of vagina, increases mucus No effect; vessels return to normal Vasoconstriction, raises diameter following sympathetic blood pressure, dilates stimulation vessels leading to skeletal muscles Autonomic Control: hypothalamus is the boss, but the reticular formation exerts the most direct influence. EEG: records some aspects of the continuous electrical activity of neurons. Brain Waves I. Alpha: low amplitude, slow, synchronous. Brain is in “idle”. Calm, relaxed state of wakefulness (hitting the snooze alarm). II. Beta: rhythmic, more irregular than alpha and higher frequency. Awake and mentally alert, as when we concentrate (like what you should be doing right now). III. Theta: more irregular than beta, common in children (until the age of eight when they take on the beta pattern), and abnormal if present in adults who are awake. IV. Delta: high amplitude, low frequency, deep sleep, RAS is anesthetized; indicates brain damage in awake adults. Sleep I. Slow-wave: cycles of nonREM sleep. During first 30-45 minutes of sleep. Must occur for REM sleep to occur. 4 stages of NREM. II. REM: 90 minutes into sleep, EEG waves become more alpha-like (awake) and REM has begun. Body temperature, heart rate, respiration, and blood pressure all increase. Oxygen use by the brain is greatest. Eyes move, but other skeletal muscle is inhibited. Most dreaming occurs during REM. Nightmares/night terrors occur in stage 3-4 of sleep. Consciousness: the conscious perception of sensations, voluntary initiation and control of movement. Stages/levels: 1) alertness 2) drowsiness/lethargy 3) stupor 4) coma involves simultaneous activity of large areas of cerebral cortex. Superimposed on other types of neural activity Holistic and totally interconnected: a memory recalls several routes Fainting or syncope: inadequate cerebral blood flow from low blood pressure, hemorrhage or stress. Epilepsy: a torrent of electrical discharges of groups of neurons. Genetic, trauma, stroke, fever, watching Pokemon, etc. Absence seizures (petit mal): expressionless, young children Grand mal: convulsive seizures Auras may occur prior to seizure Treat with anticonvulsives, vagus nerve stimulator, sever corpus callosum, hemispherectomy