Nursing 1902 The Newborn and the Family Part II
advertisement
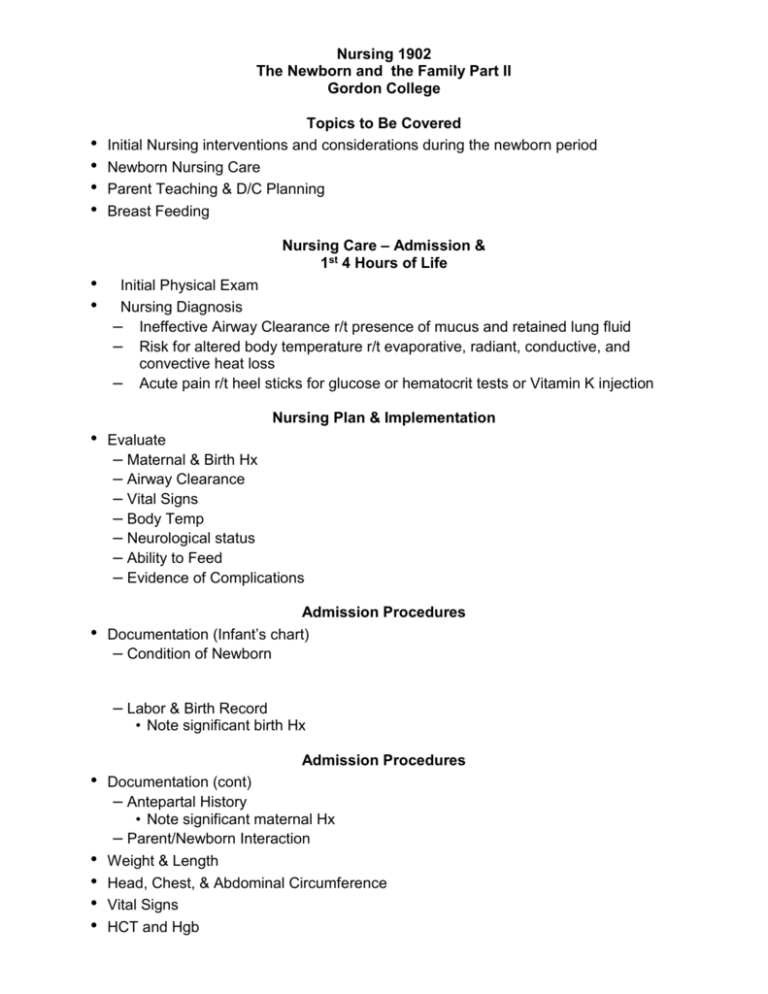
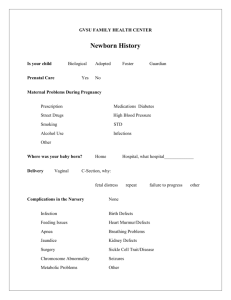
Nursing 1902 The Newborn and the Family Part II Gordon College • • • • Topics to Be Covered Initial Nursing interventions and considerations during the newborn period Newborn Nursing Care Parent Teaching & D/C Planning Breast Feeding Nursing Care – Admission & 1st 4 Hours of Life • • Initial Physical Exam Nursing Diagnosis – Ineffective Airway Clearance r/t presence of mucus and retained lung fluid – Risk for altered body temperature r/t evaporative, radiant, conductive, and convective heat loss – Acute pain r/t heel sticks for glucose or hematocrit tests or Vitamin K injection Nursing Plan & Implementation • • Evaluate – Maternal & Birth Hx – Airway Clearance – Vital Signs – Body Temp – Neurological status – Ability to Feed – Evidence of Complications Admission Procedures Documentation (Infant’s chart) – Condition of Newborn – Labor & Birth Record • Note significant birth Hx Admission Procedures • • • • • Documentation (cont) – Antepartal History • Note significant maternal Hx – Parent/Newborn Interaction Weight & Length Head, Chest, & Abdominal Circumference Vital Signs HCT and Hgb Admission Procedures • Clear Airway & Stable VS • • • • • • • Neutral Thermal Environment Optimal range 36.4C to 37.2C (97.5F to 99F) Hypothermia Unclothed under Radiant Warmer Cover Head Bath after temp & VS stable (2-4hrs) Temp rechecked after bath, if stable → OC If temp falls <36.4C(97.5F) → radiant warmer Vitamin K - Aquamephyton • • • Prophylaxis Prevents hemorrhage d/t low prothrombin levels R/T absence of gut bacterial flora which influences production of Vit K • • • • • Erythromycin Prohpylaxis for Neisseria gonorrhea 0.5% erythromycin 1% tetracycline Opthalmic solution of povidone iodine 2.5% Also effective against chlamydia Neonatal Distress • Signs First Feeding • • Breast fed infants Formula fed infants Parent/Newborn Attachment • • Eye contact Interactive bath Newborn Care • • • • • • • • • • • • Maintain Cardiopulmonary status Maintain NTE Promote Hydration/Nutrition Promote Skin Integrity Prevent Complications Promote Safety Circumcision Maintain Cardiopulmonary Status VS every 6-8 hrs Back to Sleep Bulb syringe for secretions Cardiorespiratory monitors prn Indicators of risk: Maintain NTE • • • • Dressed Double blankets Hat Hypothermia Promote Hydration/Nutrition • • • • • Document I&O Early & Frequent Feedings Weigh @ Same time each day Assess Breastfeeding techniques Assess Bottle feeding techniques Promote Skin Integrity • • • • Initial Bath Clean between diaper changes Remove cord clamp within 24 hours Cord care Prevent Complications • • • • • NB @ continued risk for: Hemorrhage Cardiac symptoms Infection Pallor Cyanosis not relieved by oxygen Prevent infection HAND WASHING • • • • • Promote Safety Compare identification numbers on ID bands Sensors Only allowing staff with proper identification to transport baby Having baby accompany parent when leaving room Report suspicious people Circumcision • 1999 AAP recommendation • • • Contraindications Circumcision – Nurse’s Role Provide parents with information Risks & Outcomes of Circumcision Hygenic practices of uncircumcised males Foreskin and glans connected @ birth and separate gradually until complete between 3-5 yrs NEVER force skin to retract Gently test for retraction during daily bath After retraction occurs – gentle washing of glans with soap and water • Prior to Circumcision • During Circumcision • Post-circumcision • Parent Teaching Apply petroleum at diaper changes If bleeds – apply pressure (if cont – call MD) Glans normally has granulation tissue during healing Report S&S of infection Plastibells fall off within 8 days No ointments while bell in place Parent Teaching • • • • • • • • Picking up the newborn Back to Sleep Bathing Cord Care Temperature Assessment Bulb Syringe Swaddling the Newborn Car Seat Safety • Newborn Screening • Immunization (Hep B) Newborn Nutrition Nutritional Needs • • • • 105 to 108 kcal/kg/d Fluid requirements = 140 to 160 mL/kg/d Fe stores dependent upon Maternal intake Formula fed infants ↑weight faster than breast fed babies Breast Milk Feeding • Colostrum • Transitional Milk • Mature milk • Foremilk • Hindmilk Breastfeeding Advantages Immunologic Advantages • Protection a/g common infections until • Secretory IgA • Breast milk is non-allergenic Nutritional Advantages • Improved digestion and absorption when compared to formula • Some proponents believe that it is the best milk for brain development • High cholesterol in breast milk = production of enzymes to metabolize cholesterol lending to a decrease in harmful long-term effects • Provides infant with more minerals than formulas • Breast milk is lower in Fe than formula, however, it is more readily absorbed from breast milk than formula • Vitamins NOT lost through processing and heating Psychosocial Advantages • • Maternal-infant attachment Increased feelings of maternal well-being Contraindications & Disadvantages of Breastfeeding Types of Formula • Cows milk protein • Soy protein – based • Specialized formulas • • • • • Potential Problems – Formula feeding Formula Prepared Improperly Allergic Reactions Always use Fe fortified formulas Constipation r/t Fe NO Cow’s milk until 12mths of age • • • • • • • Cultural Considerations Many cultures DO NOT offer colostrum Asians give boiled water until “milk flows” Hmong women believe in supplementation but not in expressing their own breast milk Most muslims breastfeed because the Koran encourages it until 2 yrs African Americans emphasize “plentiful feeding” – solid foods early Mexicans – fat baby = healthy baby and “spoiling is encouraged NURSES SHOULD EVALUATE THE CULTURAL PRACTICE AND ONLY INTERVENE IF IT IS HARMFUL TO THE BABY! Client Education for Breast feeding Basics of Milk Production • • • • • Milk production = demand Milk stored in sinuses under areola Adequate maternal fluid intake required Milk supply established by frequent feedings (Q 1 ½ to 3hrs) Letdown reflex • • • • Positioning baby at breast Baby’s entire body towards mother Mother in comfortable position w/arms supported Direct nipple straight into baby’s mouth Brush infant’s mouth w/breast to stimulate rooting reflex Procedure for feeding • • • • • • • • • • • Avoid time limits Allow nursing at first breast until breast is empty Insert finger into baby’s mouth to break suction Burp baby between breasts Burp baby again at end of feeding Wash nipple with warm water and dry Helpful Hints Assure baby is awake Alternate beginning breast Rotate baby’s position Avoid supplemental formula feedings until supply established Check w/ healthcare provider before taking medications Storage of Breast Milk • • • • • • • Refrigerated milk Store in clean plastic containers NOT glass Freezer compartment Self – contained freezer Separate deep freeze Thaw in warm water Never microwave or use boiling water to defrost • • • • • • • • Drugs and Breastfeeding Most drugs pass into breast milk Almost all appear in small amounts in breast milk Very few drugs contraindicated Avoid long acting drugs Consider absorption rates and peak blood levels when administering drugs Observe infant for drug reactions Use single-symptom drugs vs. multi-symptom drugs ALWAYS discuss with healthcare provider! Client Education for Formula Feeding • • • • • • • • Hold for all feedings Point bottle nipple directly into mouth on top of the tongue Nipple should be full of liquid at all times Burp at intervals Newborns frequently spit small amounts DO NOT overfeed Teach formula preparation Teach bottle cleaning, storage, etc… • • • • • • • Nutritional Assessment of Infant Nutritional Hx from parent Weight gain Wet & Soiled Diapers Growth chart % Physical Exam No more than 32oz per day At least 108 kcal/kg/d (20 cal/30 mL of formula)