The menstrual cycle
advertisement
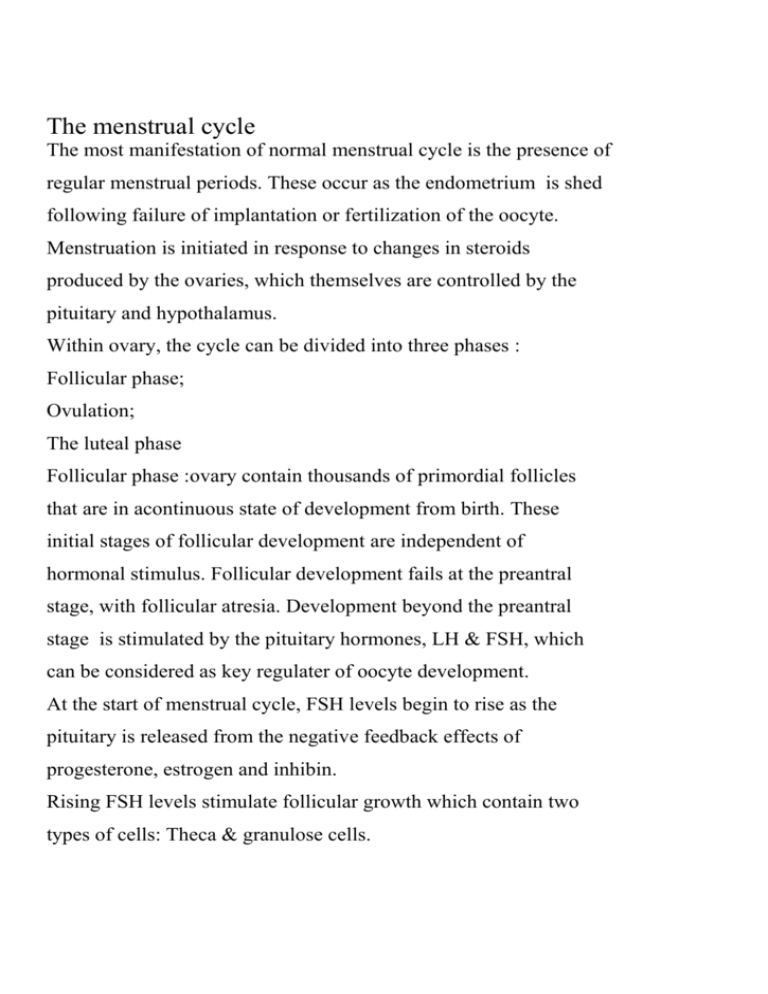
The menstrual cycle The most manifestation of normal menstrual cycle is the presence of regular menstrual periods. These occur as the endometrium is shed following failure of implantation or fertilization of the oocyte. Menstruation is initiated in response to changes in steroids produced by the ovaries, which themselves are controlled by the pituitary and hypothalamus. Within ovary, the cycle can be divided into three phases : Follicular phase; Ovulation; The luteal phase Follicular phase :ovary contain thousands of primordial follicles that are in acontinuous state of development from birth. These initial stages of follicular development are independent of hormonal stimulus. Follicular development fails at the preantral stage, with follicular atresia. Development beyond the preantral stage is stimulated by the pituitary hormones, LH & FSH, which can be considered as key regulater of oocyte development. At the start of menstrual cycle, FSH levels begin to rise as the pituitary is released from the negative feedback effects of progesterone, estrogen and inhibin. Rising FSH levels stimulate follicular growth which contain two types of cells: Theca & granulose cells. Within the theca cells, LH stimulates the production of androgens from cholesterol , within granulose cells ,FSH stimulate conversion of androgens to estrogens (aromatization) . also FSH is responsible for proliferation of granulose cells. Androgen production within the follicle may also regulate development of the preantral follicle. Low androgens level enhance aromatization & then increase estrogen production. Incontrast , high androgen levels inhibit aromatization & produce follicular atresia . A delicate balance of FSH& LH is required for early follicular development . In early menstrual cycle, the LH levels is low & FSH is high . if the LH levels are high , theca cells produce large amounts of androgens causing follicular atresia. The developing follicles grow & only one of these follicles is destined to grow to pre-ovulatory follicle & be released at ovulation ( dominant follicle). The dominant follicle secrete estradiol& inhibin. So FSH level decline in response to negative feedback effect of estradiol. The hypothalamus, via the pulsatile secretion of GnRH, stimulate pituitary LH & FSH secretion. Production of GnRH not only has a permissive effect on gonadotrophin production , but alterations in amplitude & frequency of GnRH pulsation throughtout the cycle are also responsible for some fine tuning of goadotrophin production. The response of the pituitary is not constant but is modulated by ovarian hormones ( estrogen& progesterone). In late follicular phase , serum levels of estrogen are high so that a positive feedback effect is triggered thus generating the periovulatory LH Surge. In contrast to the effects of estrogen , low levels of progesterone have a positive feedback effect on pituitary LH& FSH secretion. Such levels are generated immediately prior to ovulation, and contribute to the FSH surge . High levels of progesterone such as those seen in the luteal phase inhibit pituitary gonadotrophin. In late follicular phase , as the dominant follicle develops further , follicular estrogen production increases. The estrogen exerts a positive feedback effect on pituitary LH secretion. LH levels increase at first slowly ( day 8day12 of the cycle) & then more rapidly after day 12. LH induces luteinization of granulose cells in the dominant follicle, so progesterone is produced. Progesterone amplifies the positive feedback effect of estrogen on pituitary LH secretion, leading to a surge of LH. Ovulation occurs 36 hours after onset of the LH surge . the LH surge is one of the best methods by which the time of ovulation can be determined. The periovulatory FSH surge is induced by positive feedback effects of progesterone. In addition to the rise in LH , FSH& estrogen that occur around ovulation , a rise in serum androgen levels also occurs .these androgens are derived from stimulatory effect of LH on theca cells, particularly those of the non dominant follicle. Release of ovum from follicle is coordinated by LH ,FSH & PROGESTERONE WHICH STIMULATE PROTEOLYTIC enzyme and prostaglandin. Luteal phase ; production of progesterone from corpus luteum within ovary. The corpus luteum is derived from the granulose cells & from some theca cells which differentiate to become theca lutein cells. The production of progesterone from corpus luteum is dependent on pituitary LH secretion. The corpus luteum remain 14 days and then regression if no pregnancy occur. As that estrogen, progesterone &inhibin decline , FSH is released from pituitary from the negative feedback effects of these hormones. On the endometrium: Proliferative phase : within endometrium , the stroma & glands growth which increase thickness of endometrium from 0.5mm at menstruation to 3.5-5mm at the end of the proliferative phase. Secretory phase: is characterized by endometrial glandular secretory activity, increase glands and spiral arteries tortuosity, in the late secretory phase, irreversible decidualization of stroma and leads to endometrial apoptosis and menstruation unless pregnancy occurs. Mensturation: is initiated by withdrawal of estrogen & progesterone. It is initiated by arteriolar vasoconstriction( 75% of endometrium is shed. Menstruation ceases as the damaged spiral arteries vasoconstriction and endometrim regenerates. Fibrinolysis inhibit scar formation ( breakdown the blood clot& then repair of the endometrium and new blood vessels formation – angiogenesis-