Chapter 9 A and B Questions
advertisement
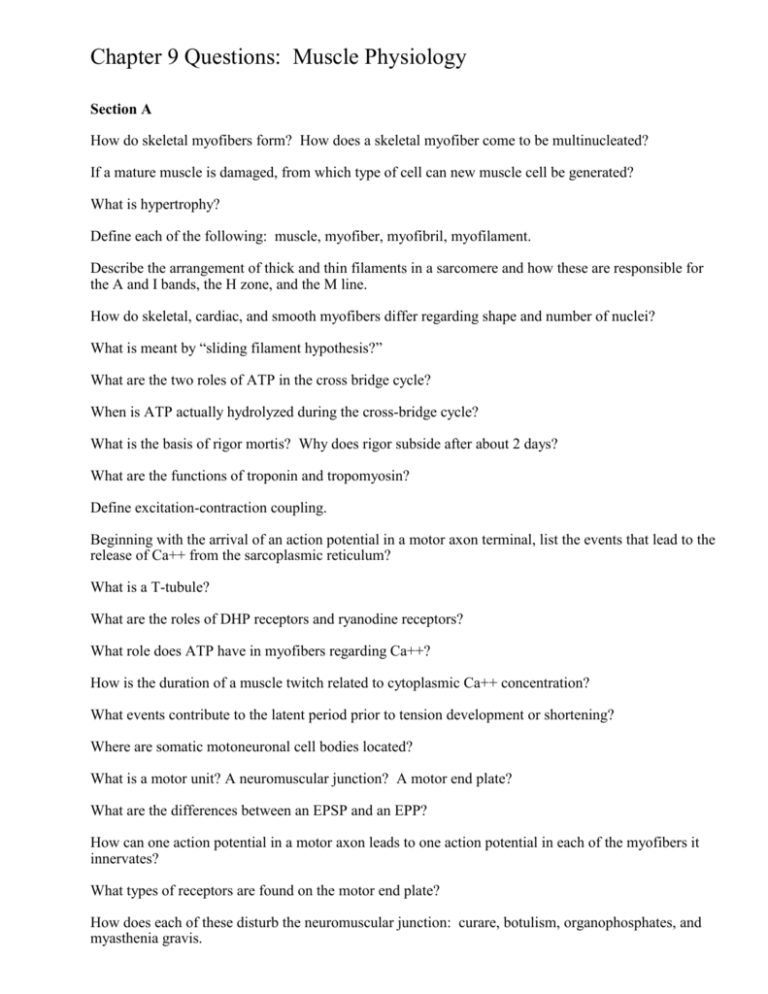
Chapter 9 Questions: Muscle Physiology Section A How do skeletal myofibers form? How does a skeletal myofiber come to be multinucleated? If a mature muscle is damaged, from which type of cell can new muscle cell be generated? What is hypertrophy? Define each of the following: muscle, myofiber, myofibril, myofilament. Describe the arrangement of thick and thin filaments in a sarcomere and how these are responsible for the A and I bands, the H zone, and the M line. How do skeletal, cardiac, and smooth myofibers differ regarding shape and number of nuclei? What is meant by “sliding filament hypothesis?” What are the two roles of ATP in the cross bridge cycle? When is ATP actually hydrolyzed during the cross-bridge cycle? What is the basis of rigor mortis? Why does rigor subside after about 2 days? What are the functions of troponin and tropomyosin? Define excitation-contraction coupling. Beginning with the arrival of an action potential in a motor axon terminal, list the events that lead to the release of Ca++ from the sarcoplasmic reticulum? What is a T-tubule? What are the roles of DHP receptors and ryanodine receptors? What role does ATP have in myofibers regarding Ca++? How is the duration of a muscle twitch related to cytoplasmic Ca++ concentration? What events contribute to the latent period prior to tension development or shortening? Where are somatic motoneuronal cell bodies located? What is a motor unit? A neuromuscular junction? A motor end plate? What are the differences between an EPSP and an EPP? How can one action potential in a motor axon leads to one action potential in each of the myofibers it innervates? What types of receptors are found on the motor end plate? How does each of these disturb the neuromuscular junction: curare, botulism, organophosphates, and myasthenia gravis. Based on your knowledge of the fate of acetylcholine in the neuromuscular junction, what drug might one use to treat myasthenia gravis? How is it possible for a muscle to contract but not shorten? What is the difference between isometric and isotonic contractions? Give an example of each. What is a lengthening contraction? Can sarcomeres ever “push,” or can they only “pull?” Define twitch. What events occur during the latent period? Why don't all muscles have the same contraction time? How does load affect latent period, velocity of shortening, duration of twitch, and distance shortened? Under what conditions of load will contractions be isometric or lengthening? What is the difference between summation and tetanus? Why is the peak tetanic tension so much greater than peak twitch tension? What is the optimal length of a muscle and what is the significance of optimal length plus or minus 30%? What are the functions of creatine phosphate and creatine kinase? What is the theory upon which athletes supplement with creatine? What type of athlete might benefit from creatine supplementation? What is the source of ATP for the first 5-10 minutes of exercise? for the next 30 minutes? for longer than 30 minutes? What is oxygen debt and how is it repaid? How would one know it is being repaid? Is ATP depletion responsible for muscle fatigue? If not, what is? What determines whether a myofiber is fast-twitch or slow-twitch? Compare and contrast the three types of skeletal myofibers with respect to source of ATP, abundance of mitochondria, capillary blood supply, myoglobin content, glycogen content, rate of fatigue, fiber diameter, and motor unit size. Explain why slow twitch oxidative fibers are the most resistant to fatigue. Which muscles of the body have small motor units and what advantage does this confer? Which muscles of the body have large motor units and why? What factors control whole muscle tension? Which types of motor units are recruited first, second, and third? How is myofiber type related to the order in which motor units are recruited? What terms apply to the loss of muscle mass that occurs when a person experiences damage to the nerve serving a muscle? What is disuse atrophy? In response to physical training how does a muscle change? by an increase in myofiber number? by an increase in myofiber diameter? by a change in the number of motor units? by a change in fiber type? by an increase in capillaries? Is the effect governed by the type of exercise (weight lifting vs "iron man" training?) What is the probable explanation for muscle cramps? What is hypocalcemic tetany and what is the mechanism of action? For persons with myasthenia gravis, how might neostigmine be beneficial? Why might thymectomy be useful? What is the principle underlying plasmapheresis to treat myasthenia gravis? Smooth muscle By which type of neurons are smooth muscles innervated? Describe the organization of contractile proteins in smooth myofibers. How does excitation-contraction coupling occur in smooth muscles? In particular, how is the role of calcium different? How can a smooth muscle maintain tension with a very low rate of consumption of ATP? What is the source of Ca++ for excitation-contraction coupling in smooth muscles? Why do twitches in smooth muscle last so long? What is smooth muscle tone? Smooth myofibers can sustain graded potentials. How does this affect tension development? What is a pacemaker potential? Other than neurotransmitters, what else can influence smooth muscle contractions? How do synapses and the distribution and number of neurotransmitter and hormone receptors in smooth muscles differ from the neuromuscular junction of skeletal myofibers? How can nervous activity induce smooth muscle relaxation? What does stretching a smooth muscle usually lead to? Why? Compare and contrast single unit and multi-unit smooth muscles? Where is each type found? Cardiac muscle Are cardiac myofibers striated? What are intercalated disks and what purpose do they serve? What are the sources of Ca++ in excitation-contraction coupling for cardiac myofibers? Why can’t cardiac myofibers undergo tetanic contractions? Why would this be lethal? How long does an action potential last in a cardiac myofiber? By what structure is an action potential transmitted from one cardiac myofiber to the next?