ACP Guidance for MDT's - Information Services Division
advertisement

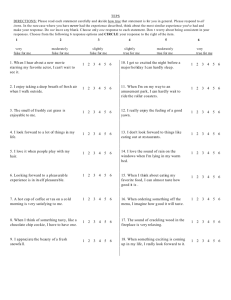
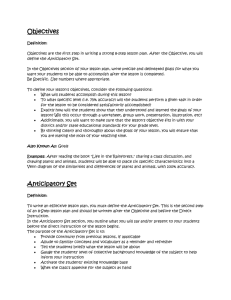
Housing & Social Work Anticipatory Care Aberdeenshire CHP General Practice Community Nursing Patient, Family & Carers Social Care Guidance for Multidisciplinary Teams Distributed March2012 Effective 2nd April 2012 Contents Section 1 Content Introduction 2 Anticipatory Care Planning 3 GP Practice Anticipatory Care Models 4 Anticipatory Care Planning Model 5 Roles 6 Key Questions 7 Future Developments Fig 1 Phases of Anticipatory Care Fig 2 Aberdeenshire Anticipatory Care Planning Model Appendix A Sample Anticipatory Care Plan Appendix B Anticipatory Care Register Appendix C Request for Assessment Form Appendix D Out of Hours Palliative Care Summary Page 1 Introduction 1.0 The purpose of Anticipatory Care is to ensure that individuals, their families and informal support networks are fully deployed in ensuring that people stay as well as possible and that when they need more support the, resilience is built in. The premise behind Anticipatory Care is that most people are responsible for managing their own health and that when additional support is required from statutory services (health and social care), it is enabling in nature and for a fixed time. 1.1 The model of Anticipatory Care developed in Aberdeenshire CHP puts the patient, client or service user, along with their family and unpaid/informal carers firmly at the centre of the process. 1.2 The Aberdeenshire model has focused on people who are currently living in the community, supporting them to remain there safely for longer, with community based services wrapped around them. 1.3 This model of Anticipatory Care Planning is designed to support and exploit a partnership (co-production) approach to working with patients, their families and carers, combining the synergies between the Practice Team (GP), Community Team (DN) and Social Care. 1.4 What is referred to in this document as Anticipatory Care Planning is just one phase of Aberdeenshire CHP’s philosophy of Anticipatory Care. In relation to the management of long-term conditions, including frailty in older age, there are currently four phases of anticipatory care. (Fig 1) Phases of Anticipatory Care Health Improvement Reducing Inequalities Coproduction within the community. Self-Management COPD/Heart Failure P1 Personal Management Plans P2 Anticipatory Care Plans Re-engaging carers into the community P3 End of Life Care P4 P1 Fig 1 1.5 Phase 1 is the self management phase where patients, family and carers can be given the information/knowledge an support to adapt their life style in order that they can stay as well as possible, minimise exacerbations of their condition(s), slow down the advancement of their condition(s) and maximise their engagement in the community, what ever that may be, employment or employability, social activity etc. At the time of writing this guidance, we are targeting two specific conditions, COPD and Heart Failure but this approach would equally apply to any condition including frailty in older age. 1.6 Phase 2, personal management planning, is where the pathology of the condition has advanced, but through prompt action patients can prevent the development of exacerbation to the stage where hospital admission is required. Evidence from early implementer practices has demonstrated that GP consultations can also be reduced amongst this cohort of patients. 1.7 Phase 3, Anticipatory Care Planning, involves planning what further support a patient would require from family and informal carers to stay as well as possible and what short term step up of health or care social care can be provided to prevent an avoidable admission. Where an admission is unavoidable, ensuring admission to the right place (care home or hospital), with an agreed discharge plan already in place. 1.8 Phase 4 is the end of life phase, but once again it is about ensuring the patient remains as well as possible for as long as possible. Ensuring that the patient their family and carers are fully involved in the planning of when, where and how additional support will be provided and ensuring that acute episodes of illness during the palliative phase do not result in preventable admissions or unnecessarily longer lengths of stay in hospital. 1.9 Too often the phases of anticipatory care are seen as an inevitable downward slope with patients requiring more and more services to compensate for their perceived needs. The challenge for us as a health and care system is how do to slow this down; keeping people safely, for the longest possible time at the least intensive stage of Anticipatory Care. Through the development of coproduction initiatives with the natural communities that make up Aberdeenshire, can we in fact help people to halt their progression or reverse back up the slope? 1.10 The next phases of anticipatory care we need to develop are the challenge of helping family and friends who have cared for people through to the palliative and end of life phases re-engage with their community. Can or should we be using their knowledge and experience to help others? Do we help maximise their engagement in the community, what ever that may be, employment or employability, social activity etc? 1.11 Finally what is the role for Anticipatory Care in health improvement and reducing health inequalities? The ‘Keep Well’ Programme will help to identify patients who are currently unaware that they are at risk of, or already have an undiagnosed long-term condition. This will provide an opportunity to engage people early with the anticipatory approach to care and into the new COPD or Heart Failure pathways. 2 Anticipatory Care Planning Overview 2.1 This guidance focuses on the process for developing Anticipatory Care Plans, phase three in the Phases of Anticipatory Care. 2.2 Although there was little evidence of the benefits of Anticipatory Care Planning when the CHP embarked in partnership with the local authority, upon this approach, there is now both local and national evidence to support this it. 2.3 The Kings Fund produced a report in 2010 which concluded the following amongst its findings: – It is important to be clear which admissions are potentially avoidable and which interventions are likely to be effective. – In primary care, higher continuity of care with a GP is associated with lower risk of admission. – There are several tools available to help identify people at risk of future emergency admission, including computer database models and simple questionnaires. There is no clear advantage of using one tool over another. – Patient self-management seems to be beneficial. – Structured discharge planning is effective in reducing future re-admissions. 2.4 These conclusions are almost replicated in the Aberdeenshire Early Implementation where we have concluded: – Not every patient will benefit from an ACP. – Not every re-admission is avoidable. – The GP is the ‘author’ of approximately 50% of ACP’s. – Multiple admission data combined with local knowledge is the most successful predictor of risk. – Patients appreciate and use both self-management and ACP’s. – The introduction of ACP’s results in up to 8% reduction in Emergency Occupied Bed Days for over 65’s. – The HMDT has a key role in developing ACP’s. 2.5 The conclusion of the Kings Fund Report contains this statement: “The NHS needs to move beyond projects and adopt comprehensive admission avoidance programmes. These programmes need to involve the full spectrum of care providers and should look across the whole system of care.” 2.6 This conclusion could equally be drawn from the work to date across Aberdeenshire CHP with the additional recommendation that admission avoidance programs must build on and support rather than replace the capacity that patients and their informal existing informal care networks. To this end a new Reshaping Care for Older People Local Enhanced Service Agreement to support Anticipatory Care Planning is being funded from the Change Fund. 3 GP Practice Anticipatory Care Models 3.1 With 36 GP Practices and patient lists varying from as large as 20,900 in Inverurie to as small as 550 in Braemar it is impossible to have a “one size fits all” approach to the development and review of Anticipatory Care Plans within GP Practices across Aberdeenshire. 3.2 During the early implementation phase of practice based Anticipatory Care Planning, four models have emerged that allow patients to be identified, plans developed and subsequently reviewed. 3.3 Lead GP Model 1 (Turriff Model) In this model a lead GP is identified for Anticipatory Care Planning who meets regularly (monthly) with the Practice Manager, Community Nurse, aligned Social Care collegues. Together they will review patients and identify those who would benefit from an Anticipatory Care Plan and agree who will take the lead in developing the plan (Intensive Case Manager). Where a GP has been identified the lead GP is responsible for discussing the case with the appropriate GP and ensuring the plan is developed. 3.4 Lead GP Model 2 In this model a lead GP is identified for Anticipatory Care Planning who will review patients and identify those who would benefit from an Anticipatory Care Plan. They will then work with the appropriate member of the practice team to develop the plan based upon the health needs of the patient. 3.5 Whole Practice Model (Banchory Model) In this model the practice team meets on a monthly basis and together, they will review patients and identify those who would benefit from an Anticipatory Care Plan and agree who will take the lead in developing the plan (Intensive Case Manager). This meeting is also used to review the effectiveness of Anticipatory Care Plans for those patients who have been admitted to hospital in the last month. 3.6 Practice Management Model (Peterhead Model) In this model the practice management team use the 65+ Multiple Admission data to identify patients who may benefit from and Anticipatory Care Plan and request that the GP with whom the patient is registered, develop a plan with the patient. This is the most data reliant and data driven of the models in use within the CHP. 3.7 Each of these models has advantages and disadvantages associated with them and as Anticipatory Care Planning rolls out across Aberdeenshire other models may emerge. The one consistent message that has emerged from the Early Implementers is that the involvement of Social Care colleagues in the identification of potential recipients and development of plans, improves both the process and outcome for patients. 4 Anticipatory Care Planning Model 4.1 Preparation Phase This phase of the process is used to introduce the Anticipatory Care Planning to the practice and once established Anticipatory Care Planning is maintained through the Maintenance Phase. The Practice Team (GP/Practice Nurse), supported by The Health and Community Care Team (HCCT), identifies those patient/clients who will benefit most from an Anticipatory Care Plan, the local options available to support them, and puts them on the register. The early implementer practices have identified that between 3-3.5% of patients over 65 will benefit from and ACP. Early implementers have identified the monthly multiple admission data for over 65’s as the most reliable data set to use in combination with local knowledge about patients. The latest version of all age SPARRA provides a useful quarterly external assurance 4.2 Planning & Review Phase The HCCT identifies the most appropriate member of the team to act as the Intensive Case Manager. For the Frail Elderly, where the issues are predominantly health this will be the GP or DN, where the issues are predominantly social this will be the Care Manager or Home Care Supervisor. In the absence of a Single Shared Assessment, the Intensive Case Manager may instigate it. Experienced Intensive Case Managers will initially meet with the patient/client and where possible their relatives and/or carers. The focus of the meeting is on enabling the patient/client to stay at home or as close to home as possible, and how they can work with their GP and HCCT to maintain or improve their health. The discussion is focused on developing a plan at one of four levels, self-care (focusing on what patients/clients can do for themselves), initiating or increasing community care (social or medical) to supplement informal arrangements, care within a community facility (hospital or care/nursing home) or admission to an acute hospital. Less experienced Intensive Case Managers may discuss available options with the Practice Team before meeting the patient/client. There may be a requirement at this stage to revisit the patient/client to amend/finalise plans. 4.3 Implementation Phase Finalised plans once agreed with the patient/client are faxed or e-mailed to GMed (norma.reid@nhs.net), and copies placed in the Yellow Folder (SSA) and the Patients Notes. Where an SSA is not present/not required the ‘Message in a Bottle’ system has been used. 4.4 Maintenance Phase New patients will be identified through the regular Practice Team review process and HCCT meetings, as well as a range of systems such as; Condition Specific Management Plans or ACP’s, via screening processes (Staywell) or through the Community Hospital HMDT as part of the discharge planning process. Aberdeenshire CHP Anticipatory Care Planning Model Preparation Phase Discussion using Multiple Admission Data & Local Knowledge (supplemented by SPARRA quarterly) Planning & Review Phase Implementation Phase Meet with Patient/Client (Family/carers) Agree Draft Plan Identify patients who will benefit from ACP Populate Register Allocate Intensive Case Manager e-mail ACP to G-Med Finalise Plan with Patient/Client Discussion and agreement with Practice Team Copy to Patient Notes Copy in Yellow Folder Initiate/Review SSA Identifying New Patients/Clients HCCT Meetings Multiple Admission Data Staywel (LTC Pathways) Condition Specific ACP’s Maintenance Phase Fig 2 Community Hospital HMDT 5 Roles 5.1 There are essentially two main reasons that a person may be admitted to hospital, one being a breakdown in their social care arrangements, whether formal or informal, and the other being a breakdown in their health. 5.2 No matter which model of Anticipatory care Palming is adopted the GP Practice is responsible for identifying patients who would benefit from an Anticipatory Care Plan, developing and maintaining the Anticipatory Care Register within the practice and providing the CHP with quarterly data about the number of active Anticipatory Care Plans in place (Appendix B). 5.3 The GP Practice is responsible for ensuring that agreed plans are shared with the Out of Hours Service (G-Med). 5.4 The GP Practice is responsible for ensuring that Anticipatory care Plans are reviewed regularly (a minimum of annually). 5.5 Care Managers and/or Local Area Co-ordinator (LAC’s), are responsible for working with patients and their carers to identify and facilitate solutions that mitigate the impact of the breakdown of care arrangements that could result in an otherwise avoidable admission (Appendix A). It is important to remember that solutions are not always transferable from one area or community to another as facilities and services available in the Banff and Buchan areas my not be available in Mar. 5.6 Healthcare staff (GP’s, DN’s AHP’s etc) are responsible for working with patients and their carers to identify and facilitate solutions to mitigate the impact of the breakdown of a patients health that could result in an otherwise avoidable admission (Appendix A). Where patients are not known to social care teams and social care input may be required, the request for assessment form should be used (Appendix C) 5.7 The Hospital Multi-Disciplinary Team has a responsibility for identifying those patients who would benefit from an Anticipatory Care Plan on discharge, and making recommendations to the appropriate GP Practice and aligned Health and Community Care Team. 6 Key Questions 6.1 The key questions that must be asked when developing an Anticipatory Care Plan are: Has due consideration been given to the existing or potential informal care arrangements before considering statutory services? Will the patient benefit from an Anticipatory Care Plan? (The patient and their carers must benefit from the plan) Are there local accessible services that will support the plan? (Then plan must be deliverable) Does the plan support or replace informal care arrangements? (Plans that replace informal care should be time limited) Does the plan prevent admission? (If not does it direct admission appropriately) Does the plan facilitate earlier discharge? (Unavoidable admissions should have an estimate length of stay) 7 Future Developments 7.1 Early implementation of the new Key Information Summary (KIS) will commence in June 2012 across NHS Grampian. The early implementer practice within Aberdeenshire is Banchory. Although we do not no the final format of the KIS based Anticipatory Care Plan it will be based upon the Out of Hours Palliative Care Summary (Appendix D). 7.2 The roll out of KIS will inevitably have an impact on how anticipatory care plans are shared with patients and their relatives, out of hour’s services and local authority colleagues. However the process of developing a plan with the patient and carers and the relationships required in developing an anticipatory care plan will remain the same. 7.3 The perceived benefits of KIS are: Speed of sharing information Twice daily update to KIS from GP System Ease of access to the plan across the health system Wider range of professionals have access (including SAS) Standard presentation of ACP across NHS Grampian and NHS Scotland 7.4 There are two potential disadvantages with the new format of the KIS based ACP: It will be less user friendly for patients and carers It will not be electronically sharable with Local Authority Colleagues during the initial role out. Appendix A Housing & Social Work Aberdeenshire CHP Anticipatory Care Plan Name: Harry Potter DOB: 01/07/1941 CHI: 0107415678 Address: Dumbledoor Den, Womping Willow Lane Godricks Hollow GH10 1HW SSA: Yes No Care First Ref: Likely Reasons for Admission 1. Illness or incapacity of wife (Jinny), who is Harry’s main carer 2. Failure of COPD Personal Management Plan Intensive Case Manager: Review Date: Significant Information Deloris Umbridge District Nurse Brief History 28/03/09 Senile Macular Degeneration Malg neop prostrate Hyperthyroidism Rheumatoid Arthritis Hip Replacement Neurotic depression COPD Self Medicating Yes No Insulin Yes No Warfarin Yes No General Practitioner: Last Hospital Admission: Albus Dumbledoor 17/10/2008 Medication Details Significant sight problems Cognitive problems Isolated locality Relies on wife for total care including administering drugs as prescribed PTO Appendix A Housing & Social Work Aberdeenshire CHP Anticipatory Care Plan Illness or incapacity of wife (Jinny), who is Harry’s main carer In hours Mr Potter can be supported through day-care and home care. Out of hours admission to Turriff Community Hospital the maximum of 72 hours to enable additional care package to be set up by the Health and Community Care Team. Failure of COPD Personal Management Plan Admit to Turriff Community Hospital for Oxygen Therapy and IV Antibiotics. Estimated length of stay 3 days. Deloris Umbridge District Nurse Intensive Case Manager Date:28/10/08 Appendix B Aberdeenshire CHP Anticipatory Care Register CHI Number Forename Surname Address Post Code SSA Intensive Case Manager LTC Plan Self Medicating Isulin Warfarin Review Date OOH Faller Appendix C Aberdeenshire Council Care Management & Home Care Request for Assessment Form Please fully complete all sections of this form. This will help us to deal with the request appropriately. Patient / Patient Details Full Name Date of Request Full Address (include Post Code) Telephone Number CHI Number Date of Birth Gender Is Patient aware of the Request? Does Patient live alone? Has Patient given consent for the request? If No, provide full names of all people living at property and their relationship to Patient:Name Relationship to Patient GP Details GP’s Name Practice Name Address GP’s Telephone Number Contact Regarding Assessment Who should be contacted regarding the Assessment? Relationship to Patient Details of Person Making the Request Name Address Telephone Number Email Address Contact Telephone Number Designation Patient’s Medical Condition Please specify the Patient’s medical condition(s) previous and present relevant conditions Is Patient’s condition terminal or do they require palliative care? If yes, has a DS1500 form been completed? Is Patient self medicating? Does Patient have any communication or capacity issues? Reason for Assessment Please provide as much detail as possible:- What support is currently being provided or was provided prior to hospital admission? Has Patient been referred to another If yes please specify Service? e.g. Physio, Rehab OT, Speech Therapy, Rehab and Reablement etc Hospital Discharge Details Estimated Date of Discharge Is Patient continuing to receive medical, nursing or rehabilitative input? Aberdeenshire Council Use Only Date request received Carefirst ID (if known) Name Designation Is more Information Required? Proceed to Single Shared Assessment? 07/09/11 (v2) Please Specify e.g. GP, family, community nurse, etc If No, please indicate reason Appendix D OUT OF HOURS SPECIAL PATIENT ALERT – PALLIATIVE CARE Patient’s Name: Address: Main Carer: Relationship: Carer Tel No: District Nurse: Date of Birth AND CHI: Tel No: Access issues? General Practitioner: Practice: Contact GP OOH? Yes No GP Home Tel/Mobile/Pager: Main Diagnoses & Date: What is the patient’s understanding of Diagnosis? Prognosis? What is the carer’s understanding of Diagnosis? Prognosis? Resuscitation discussed? Yes No Resuscitation Appropriate OR Do Not Resuscitate Policy agreed Relevant problems and management – current and anticipated: Catheter/continence products in home? Yes No Moving and handling equipment in home? Yes No Relevant drugs, doses and allergies: Palliative Care Kardex completed? Yes No Syringe driver in use? Yes No Emergency drugs left in home: Patient’s preferred place of care: Home Nursing Home Community Hospital Hospital Hospice If admission necessary, please admit to Additional information/comments Form completed by Name: Job title: Date: Revision due: “Palliative Care Form Completed” entered into OOH computer system? Yes No PLEASE SEND AND/OR FAX TO G-MED Fax No: (01224) 558 077 OUT OF HOURS SPECIAL PATIENT ALERT – PALLIATIVE CARE Example Patient’s Name: Harry Potter Address: Dumbledoor Den, Womping Willow Lane Godricks Hollow GH10 1HW Date of Birth AND CHI: 01/07/1941 0107415678 Tel No: 07224 704997 Main Carer: Jinny Potter Relationship: Wife Carer Tel No: 07224 704997 District Nurse: Deloris Umbridge General Practitioner: Albus Dumbledoor Practice: Godricks Hollow Medical Centre Contact GP OOH? Yes NoX Access issues? Isolated locality not available GP Home Tel/Mobile/Pager: on Satellite Navigation Main Diagnoses & Date: Senile Macular Degeneration; Malg neop prostrate; Hyperthyroidism Rheumatoid Arthritis ; Hip Replacement; Neurotic depression COPD What is the patient’s understanding of Diagnosis? Although Harry has been involved in discussion he has difficulty remembering Prognosis? Although Harry has been involved in discussion he has difficulty remembering What is the carer’s understanding of Diagnosis? Fully aware of diagnosis Prognosis? Fully aware of prognosis and assisted in the development of ACP Resuscitation discussed? YesX No Resuscitation Appropriate OR Do Not Resuscitate Policy agreed X Relevant problems and management – current and anticipated: Significant sight problems Cognitive problems Relies on wife for total care including administering drugs as prescribed Likely Reasons for Admission are: Illness or incapacity of wife (Jinny), who is Harry’s main carer Failure of COPD Personal Management Plan Catheter/continence products in home? Yes No N/A Moving and handling equipment in home? Yes No N/A Relevant drugs, doses and allergies: Harry is not able to self medicate Palliative Care Kardex completed? Yes No Syringe driver in use? Yes No Emergency drugs left in home: As per COPD Self Management Plan Patient’s preferred place of care: Home X Nursing Home Community Hospital Hospital Hospice If admission necessary, please admit to: Turriff Community Hospital Additional information/comments ACP 1 Illness or incapacity of wife (Jinny), who is Harry’s main carer In hours Mr Potter can be supported through day-care and home care. Out of hours admission to Turriff Community Hospital the maximum of 72 hours to enable additional care package to be set up by the Health and Community Care Team. 2 Failure of COPD Personal Management Plan Admit to Turriff Community Hospital for Oxygen Therapy and IV Antibiotics. Estimated length of stay 3 days. Form completed by Name: Deloris Umbridge Job title: DN Team Leader Date: 27/02/2012 Revision due: 27/08/2012 “Palliative Care Form Completed” entered into OOH computer system? Yes No PLEASE SEND AND/OR FAX TO G-MED Fax No: (01224) 558 077