ARTICLE IN PRESS
+
MODEL
Radiography (2008) xx, 1e7
available at www.sciencedirect.com
journal homepage: www.elsevier.com/locate/radi
Radiographic interpretation of the appendicular
skeleton: A comparison between casualty officers,
nurse practitioners and radiographers
Liz Coleman a,*, Keith Piper b
a
Radiology Department, Royal Surrey County Hospital, Egerton Road, Guildford, Surrey GU2 7XX, United Kingdom
Allied Health Professions Department, Canterbury Christ Church University, Canterbury,
Kent CT1 1QU, United Kingdom
b
Received 25 October 2007; revised 27 November 2007; accepted 5 December 2007
KEYWORDS
Image interpretation;
Appendicular skeleton;
AFROC;
Casualty officer;
Nurse practitioner;
Radiographer
Abstract Aim: To assess how accurately and confidently casualty officers, nurse practitioners and radiographers, practicing within the emergency department (ED), recognize and
describe radiographic trauma within an image test bank of 20 appendicular radiographs.
Method: The participants consisted of 7 casualty officers, 13 nurse practitioners and 18 radiographers. All 20 radiographic examinations selected for the image test bank had been acquired
following trauma and included some subtle, yet clinically significant abnormalities. The test
bank score (maximum 40 marks), sensitivity and specificity percentages were calculated
against an agreed radiological diagnosis (reference standard). Alternative Free-response Receiver Operating Characteristic (AFROC) analysis was used to assess the overall performance
of the diagnostic accuracy of these professional groups. The variation in performance between
each group was measured using the analysis of variance (ANOVA) test, to identify any statistical significant differences in the performance in interpretation between these groups. The
relationship between the participants’ perceived image interpretation accuracy during clinical
practice and the actual accuracy of their image test bank score was examined using Pearson’s
Correlation Coefficient (r).
Results: The results revealed that the radiographers gained the highest mean test bank score
(28.5/40; 71%). This score was statistically higher than the mean test bank scores attained by
the participating nurse practitioners (21/40; 53%) and casualty officers (21.5/40; 54%), with
p < 0.01 and p Z 0.02, respectively. When compared with each other, the scores from these
latter groups showed no significant difference (p Z 0.91). The mean ‘area under the curve’
(AUC) value achieved by the radiographers was also significantly higher (p < 0.01) in comparison to the AUC values demonstrated by the nurse practitioners and casualty officers, whose
results, when compared, showed no significant difference (p Z 0.94). The radiographers’ results demonstrated a moderate positive correlation (r Z 0.51) between their clinical practice
* Corresponding author. Tel.: þ44 1483 571122x4165.
E-mail address: lizcoleman@hotmail.co.uk (L. Coleman).
1078-8174/$ - see front matter ª 2007 The College of Radiographers. Published by Elsevier Ltd. All rights reserved.
doi:10.1016/j.radi.2007.12.001
Please cite this article in press as: Coleman L, Piper K, Radiographic interpretation of the appendicular skeleton: A comparison between
casualty officers, nurse practitioners and radiographers, Radiography (2008), doi:10.1016/j.radi.2007.12.001
ARTICLE IN PRESS
+
MODEL
2
L. Coleman, K. Piper
estimations and their actual image test bank scores (p Z 0.02); however, no significant correlation was found for the nurse practitioners (r Z 0.41, p Z 0.16) or casualty officers (r Z 0.07,
p Z 0.87).
Conclusion: The scores and values achieved by the radiographers were statistically higher than
those demonstrated by the participating nurse practitioners and/or casualty officers. The
results of this research suggest that radiographers have the ability to formally utilise their
knowledge in image interpretation by providing the ED with a written comment (initial interpretation) to assist in the radiographic diagnosis and therefore replace the ambiguous ‘red
dot’ system used to highlight abnormal radiographs.
ª 2007 The College of Radiographers. Published by Elsevier Ltd. All rights reserved.
Introduction
The majority of Emergency Department (ED) X-ray departments within the United Kingdom (UK) operate a ‘red dot’
scheme to highlight radiographic trauma to the referring
practitioner.1 However, unless evidence of radiographic
trauma is generally obvious, clarification or identification
of the abnormality (as indicated by the red dot) may be
required from the radiographer. As a result, some radiology
departments now provide the ED practitioners with a written
opinion of the radiographic appearances.2,3 This initiative is
strongly supported by the Society and College of Radiographers (SCoR, UK), who stated in 2004 (p. 4) that ‘‘.the widespread and popular implementation of ‘red dot’ systems
should now be encouraged to evolve into an expectation
that a first line interpretation (e.g. radiographer comment)
should be a standard expectation of all radiographers, incorporated in pre-registration training and become accepted as
normal practice’’.4
The evolution of the nurse practitioner’s role enables
these professionals to hold a more autonomous post that
involves the assessment, treatment and discharge of patients, extending the nursing role beyond conventional
boundaries.5,6 This has increased the number of professional groups that request and interpret ED radiographs as
part of their normal working practice, a role traditionally
undertaken by a senior house officer (SHO) or casualty officer. Many nurse practitioners have formed an established
role within the ED, however, there is at present, no requirement to gain further qualifications.7 There is also no nationally accepted training scheme in place for SHOs beginning
their rotation within the ED department.8 However, the
diagnosis and subsequent treatment of the patient often
relies upon the accuracy of the radiographic interpretation
by the ED practitioners.
Performance studies to date that have compared the
image interpretation accuracy of casualty officers and
nurse practitioners reveal little, if any difference in the
accuracy between these professional groups.9e12 These
papers generally regarded the casualty officers as the
‘benchmark comparator’ and appeared to imply that nurse
practitioners who achieved comparable scores of accuracy
were then deemed to possess a satisfactory and safe level
of practice in image interpretation.1
Over 20 years ago, a study by Berman 13 compared the
image interpretation ability of casualty officers and radiographers. The casualty officers achieved a mean accuracy of
88.9%, which was similar to the performance achieved by
the radiographers (87.4%). Since then the majority of the
published research appears to report upon the image interpretation accuracy of radiographers independently or in
comparison to radiologists.14,15 A more recent study by
Piper and Paterson16 compared the image interpretation
ability of radiographers and nurses (working in either ED
or a Minor Injuries Unit (MIU)), yet to date there has been
no study published which has compared the performance
of casualty officers, nurse practitioners and radiographers.
Aims
To investigate
if there was any significant difference in the performance between the casualty officers, nurse practitioners and radiographers when interpreting a bank of
20 appendicular skeleton (trauma) images, in terms of:
(a) the image test bank score, sensitivity and specificity;
(b) the area (A1) under the Receiver Operating Characteristic (ROC) curve (AUC) generated following
Alternative Free-response ROC (AFROC) analysis;
if there was any correlation between the confidence
and performance demonstrated by the three different
professional groups, in terms of their perceived level
of accuracy during normal working practice and the
image test bank score demonstrated during this study.
Methodology
Ethical approval
Appropriate approval for this research to be undertaken
was gained from the Research and Development (R&D)
department within the NHS Trust and the Local Research
Ethics Committee (LREC).
Radiograph selection
All 20 skeletal examinations selected for the test bank were
based on a selection of images similar to those utilised in
two previous studies (Table 1).10,16 The radiographic cases
required for the test bank were generated from an image
library within the radiology department of an NHS trust in
South East England. The original anonomised reports were
retained for all images selected and three further reports
Please cite this article in press as: Coleman L, Piper K, Radiographic interpretation of the appendicular skeleton: A comparison between
casualty officers, nurse practitioners and radiographers, Radiography (2008), doi:10.1016/j.radi.2007.12.001
ARTICLE IN PRESS
+
MODEL
Radiographic interpretation of the appendicular skeleton
Table 1
Radiographic test bank
1. Salter Harris I fracture of distal radius
2. Minimally displaced fracture at the base of second
proximal phalanx
3. Comminuted fracture at the base of fifth metacarpal
with displaced fractures at the base of fourth and fifth
distal phalanges
4. Dislocation of calcaneocuboid joint
5. Perilunate dislocation and scaphoid fracture
6. Normal thumb
7. Calcaneal fracture
8. Normal elbow
9. Normal hand
10. Elbow with elevated fat pads, no fracture (lateral view)
11. Minimally displaced colles’ fracture of distal radius
12. Normal ankle of 14-year old
13. Buckle fracture of distal radius
14. Undisplaced posterior malleolar fracture
15. Lipohaemarthrosis on knee film (lateral view only)
16. Fracture of third metatarsal
17. Fracture of neck of fourth metacarpal
18. Dislocation of first carpometacarpal joint
19. Normal foot of 14-year old
20. Normal shoulder
were obtained from a consultant radiologist with many
years of skeletal reporting experience, a senior radiology
registrar and an advanced practitioner radiographer with
five years of plain film reporting experience. A consensus
of diagnosis was reached on all images selected and an
expected answer (reference standard) generated for all
cases. Each individual case was defined as abnormal if
a clinically significant radiographic finding was apparent
as outlined in Table 1. Cases 6, 8, 9, 12, 19 and 20 were
classified as normal. These decisions were all agreed prior
to observation by the study participants.
The examinations were acquired following trauma and
featured radiographs of the arm distal to, and inclusive of
the shoulder and radiographs of the leg, distal to, and
inclusive of the knee. The test bank included images that
demonstrated radiographic trauma outside the primary
area of interest, as well as those that included more than
one radiographic injury. This was used to test the observers’
‘satisfaction of search’ and ‘failure to search’ errors.17,18
Participants were informed that some of the images were
normal, to be consistent with normal clinical practice.
Observer groups
A total of 38 participants, all of whom were based in the
same district general hospital, completed the interpretation of the image test bank. The study group consisted of 18
radiographers (Bands 5 and 6), 13 nurse practitioners and
one cohort of 7 casualty officers. All the radiographers
rotate within the ED X-ray department and participate in
the ‘red dot’ scheme. All nurse practitioners in the study
request and interpret radiographs. From the sample demographics it was found that 67% of the radiographers had five
years or more radiography experience, compared with 31%
of the nurse practitioners who had held their current position for the equivalent length of time.
3
Data collection
All participants completed the image test bank independently. A numbered answer booklet and an additional information sheet were issued to each participant. Patient
details were removed from each image which were numbered and accompanied by a brief clinical history in the
corresponding numbered answer booklet. The clinical history was based on that provided at the time of the original
referral and identified the symptomatic anatomical area on
the corresponding image.
Participants were asked to specify if the radiographic
examination was normal or abnormal, giving the certainty
of their decision using a five-point scale (definitely normal,
probably normal, possibly abnormal, probably abnormal or
definitely abnormal). Participants were also instructed that
all answers, other than those considered to be ‘definitely or
probably normal’ were to be supported by text that
identified the nature and location of the abnormality.
Before the image interpretation began the participants
were asked to clarify their present position, title and grade
and then specify, on a scale of 1e10, how accurately they
perceived their image interpretation skills to be during
normal working practice. The answer booklets were randomised before marking and the additional information
sheets were not made available at this time, ensuring that
the scorers were blind to the profession of individual
participants. All answer booklets were marked by the first
author (LC), an experienced radiographer specialised in
plain film reporting, and the first 10% of the answer booklets
were also marked by a second scorer independently. The
second scorer (KP) is an experienced academic radiographer
and the director of established post-graduate radiography
programmes. The scoring system was followed and produced clear agreement of scores, however, any discrepancies or queries that arose was discussed and resolved to
maintain consistency.
Data analysis
Test bank scores
The films were marked using a scoring system employed in
similar studies.10,16,19 A maximum score of two marks were
available for each question. Full marks were awarded if the
image was correctly classified as normal or abnormal, and if
both the location and description of the radiographic abnormality or abnormalities were correct. One mark was
awarded when the answer was partially correct.16 No marks
were deducted for poor spelling or abbreviations. A maximum total of 40 marks per participant was therefore
possible.
Comparison of estimated and actual accuracy
The relationship between the participants’ perceived
accuracy during clinical practice and the actual accuracy
of their image test bank score was examined using Pearson’s Correlation Coefficient (r) and the significance
calculated.20
Please cite this article in press as: Coleman L, Piper K, Radiographic interpretation of the appendicular skeleton: A comparison between
casualty officers, nurse practitioners and radiographers, Radiography (2008), doi:10.1016/j.radi.2007.12.001
ARTICLE IN PRESS
+
MODEL
4
Sensitivity and specificity
The accuracy of a diagnostic test is measured by sensitivity
and specificity.21 Sensitivity is the proportion of positive
cases correctly identified as being abnormal; conversely
specificity is the proportion of negative cases correctly
identified as being normal.22 Accuracy is defined as true
positives and true negatives divided by all results.23 To enable these calculations to be completed each response was
marked as a true positive (TP), true negative (TN), false
positive (FP) or false negative (FN) classification.18 Some
answers, if partially correct were awarded fractional marks
(for instance, 1/2 TP and 1/2 FN).19 This occurred when
a radiographic abnormality was detected or described,
but the observer failed to identify all key elements that
had been agreed in the expected answer (reference standard). Where partial marks were awarded, the constituent
partial marks amounted to one full mark.
AFROC performance
Alternative Free-response Receiver Operating Characteristic (AFROC) analysis was used to assess the correct localisation of true positive events. AFROC methodology will
allow for multiple abnormalities on a film, and therefore
more than one observed response for every image.24 The
data collated from the results of the image interpretation
were coded and processed using a web-based calculator.25
This produced an AFROC curve to enable direct visual comparison between the accuracy of the three professional
groups. The measure of accuracy, based on the area under
the curve (AUC or A1), can range from a value of 0.0 to
1.0.21
Statistical analysis of values
The variation in performance between each group, in terms
of image test bank score, sensitivity, specificity and AUC
value, was measured by use of the analysis of variance
(ANOVA) statistic and a web-based calculator.26,27
Results
The results shown in Table 2 reveal that the radiographers
gained the highest mean test bank score (28.5/40; 71%).
Table 3 compares the performance of the three groups
and demonstrates that this score was statistically higher
than the mean test bank scores attained by the participating nurse practitioners (21/40; 53%) and casualty officers
(21.5/40; 54%), with p < 0.01 and p Z 0.02, respectively.
When compared with each other, the scores from these latter groups showed no significant difference (p Z 0.91).
The specificity values follow a similar pattern. The
radiographers’ mean value (80.5%) was significantly higher
than those achieved by the nurse practitioners (54%,
p < 0.01) and the casualty officers (57%, p Z 0.04), whose
values were not significantly different from each other
(p Z 0.99).
A significant difference (p Z 0.03) was demonstrated, by
ANOVA testing (Table 3), between the mean sensitivity
values achieved by the three groups. The radiographers’
L. Coleman, K. Piper
sensitivity (67%) was significantly higher (p Z 0.02) in comparison to the mean sensitivity demonstrated by the nurse
practitioners (49%) and approached statistical significance
(p Z 0.06) when compared to the sensitivity achieved by
the casualty officers (51%), whose results when compared
to the nurse practitioners showed no significant difference
(p Z 0.86), as seen in Table 3.
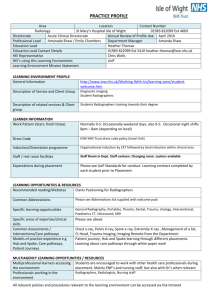
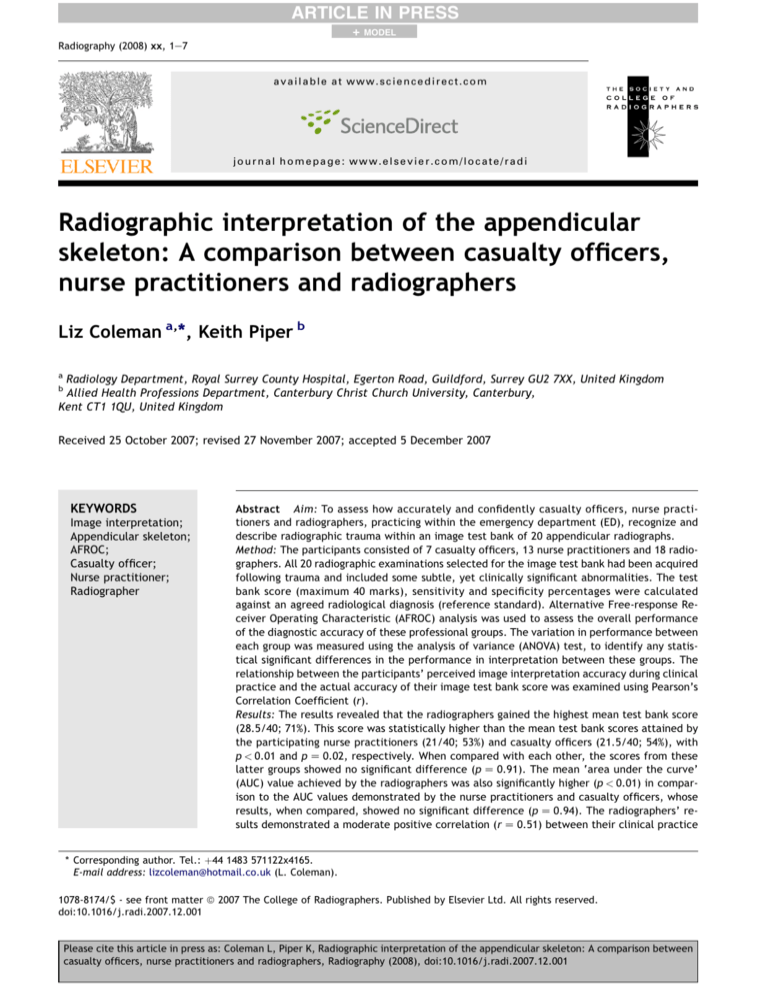
The mean AUC value of 0.75 achieved by the radiographers was found to be significantly more accurate (p < 0.01)
in comparison to the AUC values of 0.58 and 0.54 achieved
by the nurse practitioners and casualty officers, respectively. The closer the AUC to 1.0, the more accurate the
classification, therefore, a curve lying above and to the
left of another shows greater accuracy in the related classification system.28 Typical AFROC curves that represent the
accuracy achieved by all three groups are shown in Fig. 1.
There is no significant difference between the mean AUC
values achieved by the nurse practitioners and casualty officers; therefore one illustrative AFROC curve is included
to represent the accuracy achieved by these two groups.
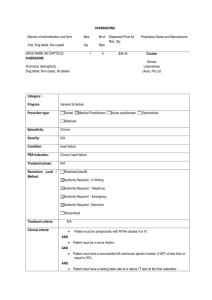
The radiographers’ results demonstrated a moderate
positive correlation (r Z 0.51) between their clinical practice estimations and their actual test bank scores
(p Z 0.02); however, no significant correlation was found
between the nurse practitioners’ (r Z 0.41, p Z 0.16) and
casualty officers’ (r Z 0.07, p Z 0.87) clinical practice estimations when compared to their actual test bank scores, as
can be seen in Table 4.
Discussion
The test bank scores achieved by the casualty officers and
nurse practitioners in this research are comparable to those
scores achieved in similar studies.10,16 The nurse practitioners in this research achieved a mean test bank score
of 53% comparing reasonably well with the nurse practitioners in the study by Meek et al.10 who gained a marginally
more accurate mean test bank score of 57%. The nurse
practitioners in the study by Piper and Paterson16 achieved
similar results in their pre- and post-training mean scores of
53% and 64%, respectively. The casualty officers who participated in this research and the study by Meek et al.10 also
appeared to follow this trend giving comparable results.
The inexperienced casualty officers in the study by Meek
et al.10 achieved a mean test bank score of 50% followed
closely by the casualty officers in this research who gained
a mean test bank score of 54%.
This research, and both the studies by Meek et al.10 and
Piper and Paterson16 shared many common features; all
studies were based on the same scoring system, all images
were of the appendicular skeleton, all images were supplied with a brief clinical history, all participants could
achieve a maximum of 40 marks in their test bank score
and several of the images used in this research replicated
those used in the studies by Meek et al.10 and Piper and
Paterson.16 These similarities appear to reflect in the similarity of the scores that were achieved.
The mean test bank scores achieved by the casualty
officers and nurse practitioners in this research are similar
to the results reported by these professionals in other
studies.10,16 However, a significant difference (p Z 0.02
Please cite this article in press as: Coleman L, Piper K, Radiographic interpretation of the appendicular skeleton: A comparison between
casualty officers, nurse practitioners and radiographers, Radiography (2008), doi:10.1016/j.radi.2007.12.001
ARTICLE IN PRESS
+
MODEL
Radiographic interpretation of the appendicular skeleton
Table 2
5
Test bank scores, sensitivity, specificity and AUC values
Group
Statistics
Test bank score
(max. 40)
Sensitivity (%)
Specificity (%)
AUC
Radiographers
Mean
SD
95% CI
28.5
4.5
26.4e30.8
67
13.4
60.3e73.7
80.5
16.2
72.5e88.6
0.75
0.1
0.7e0.8
Nurse practitioners
Mean
SD
95% CI
21
4.5
18.1e23.6
49
11.7
42.2e56.4
54
20.0
41.9e66.1
0.58
0.1
0.5e0.7
Casualty officers
Mean
SD
95% CI
21.5
5.4
16.5e26.5
51
11.9
40.0e62.0
57
30.6
28.8e85.4
0.54
0.1
0.5e0.6
and p < 0.01, respectively) was seen when the mean test
bank scores achieved by the casualty officers (54%) and
nurse practitioners (53%) in this research were compared
with the mean test bank score of 71% achieved by the
radiographers in this research. The radiographers’ mean
test bank score is also similar to the post-training mean
test bank score of 73% achieved by the radiographers in
the study by Piper and Paterson,16 who also found the
radiographers’ results to be significantly higher than the
post-training mean test bank score of 64% achieved by
the nurse practitioners.
The ‘area under the curve’ (AUC or A1 as denoted in
AFROC analysis) values achieved in this research were
very similar to the AUC values identified in the study by
Piper and Paterson.16 However, a marked difference was
seen when comparison was made with the higher AUC
values reported in a previous study by Overton-Brown and
Anthony.29 When the assessment method of these studies
were compared, it was found that the standard Receiver
Operating Characteristic (ROC) observer performance approach used in the study by Overton-Brown and Anthony29
was not as rigorous as the more accurate Alternative
Free-response Receiver Operating Characteristic (AFROC).
The participants in the study by Overton-Brown and Anthony29 may have identified an abnormality; however, it
Table 3
may not have been the true abnormality. The study by
Overton-Brown and Anthony29 also excluded films of the
shoulder, elbow and knee. These exclusions and the simple
use of ROC methodology may well account for the higher
values reported in the study. Research has shown that the
ability to indicate a radiographic abnormality varies greatly
in comparison to the ability to write a comment to convey
this appearance.30
The mean specificity achieved by the radiographers in
this research was greater or very similar to the mean
specificity achieved by the radiographers in several recognized articles.16,30e32 The mean sensitivity of the radiographers in this research was relatively low in comparison to
the mean values of sensitivity achieved by these professionals in similar studies.31e33 However, much of the literature found that the values of sensitivity increased
immediately after a period of training.16,30e33 The sample
demographics obtained from the participants of this study
revealed that none of the radiographers had received any
in-house image interpretation teaching in the last six
months. Other research found that a radiographer’s ability
to accurately identify abnormalities reduced six months
after training was completed,32 suggesting that training
is essential if radiographers are to increase their ability
to correctly identify abnormalities on positive films.
Statistical comparison of performance measures
Measure
Group
ANOVA
Tukey multiple
comparison test
(p value)
Radiographers
(Group A)
Nurse practitioners
(Group B)
Casualty officers
(Group C )
F
p
Test bank score (max. 40)
28.5
21
21.5
6.6
<0.01
Sensitivity (%)
67
49
51
4.2
0.03
Specificity (%)
80.5
54
57
4.2
0.03
AUC (A1)
0.75
0.58
0.54
7.3
<0.01
A
A
B
A
A
B
A
A
B
A
A
B
vs
vs
vs
vs
vs
vs
vs
vs
vs
vs
vs
vs
B:
C:
C:
B:
C:
C:
B:
C:
C:
B:
C:
C:
p < 0.01
p Z 0.02
p Z 0.91
p Z 0.02
p Z 0.06
p Z 0.86
p < 0.01
p Z 0.04
p Z 0.99
p < 0.01
p < 0.01
p Z 0.94
Please cite this article in press as: Coleman L, Piper K, Radiographic interpretation of the appendicular skeleton: A comparison between
casualty officers, nurse practitioners and radiographers, Radiography (2008), doi:10.1016/j.radi.2007.12.001
ARTICLE IN PRESS
+
MODEL
6
L. Coleman, K. Piper
AFROC curves
1
AUC = 0.77 (Illustrative curve).
Mean: radiographers = 0.75
0.9
True positive fraction
0.8
AUC = 0.58 (Illustrative curve).
Mean: NPs and COs; 0.58
and 0.54, respectively
0.7
0.6
0.5
0.4
0.3
0.2
Radiographers
0.1
Nurse practitioners
/ casualty officers
0
0
0.2
0.4
0.6
0.8
1
False positive fraction
Figure 1
Illustrative AFROC curves.
There appears to be limited research available that
identifies the sensitivity and specificity of casualty officers
and nurse practitioners in their accuracy of image interpretation. The study by Freij et al. 9 that documents
this information found these professionals achieved similar
scores of sensitivity and specificity; however, a marked
difference was seen when these values were compared to
those achieved by the nurse practitioners and casualty officers in this research, whose scores were notably lower.
Upon closer inspection of the methodology used in the
study by Freij et al.,9 it was found that those casualty officers and nurse practitioners were involved in an audit
assessment during normal clinical practice, as opposed to
interpretation of an image test bank. Although the results
of this research were based on a small sample of images,
not representative of clinical practice, the test bank was
intended to be sufficiently discriminatory to adequately
assess the performance of the professional groups. The results in this research may appear low in comparison to the
findings of Freij et al.,9 however, this may be misleading, as
a study by Brown,34 which used both audit and test bank
Table 4
methodologies, found a correlation between the apparently
low test bank scores (pre: 63.5%; post: 69.8%) and audit
accuracy (pre: 82.9%; post: 90%), before and after training
(pre-test: r Z 0.82, p Z 0.04; post-test: r Z 0.77, p Z 0.08)
for a small group of radiographers.
‘Failure to search’ and ‘satisfaction of search’ accounted for a common error within all three groups in this
research. All participants identified the fracture at the base
of the fourth metacarpal; however, the majority of the
radiographers (67%), nurse practitioners (85%) and all of the
casualty officers failed to note the fractures at the base of
the fourth and fifth distal phalanges.
The results from this research found the casualty
officers and nurse practitioners ability to interpret radiographs was not as accurate as they perceived, as seen in
Table 4. A moderate positive correlation was found between the radiographers’ estimate of their image interpretation abilities during normal working practice when
compared to their test bank score (p Z 0.02). However,
no correlation was found for the casualty officers or nurse
practitioners (p Z 0.87 and p Z 0.16, respectively). This
suggests that radiographers may be more realistic in their
abilities, when compared to casualty officers and nurse
practitioners who appear to overrate their ability in image
interpretation, which could potentially lead to misdiagnosis. Although, the lack of correlation between the confidence in, and accuracy of, clinical prediction has been
noted previously in the field of medical decision making,35
the reasons for this phenomenon are complex.36
Conclusion
The radiographers in this research produced significantly
higher scores during the image interpretation test in
comparison to both the casualty officers and nurse practitioners who participated in this study. This may not be
surprising as radiographers generally have the most experience in viewing radiographic images when compared to
both nurse practitioners and casualty officers. Interpretation of radiographic images is only one aspect of the role
undertaken by casualty officers and nurse practitioners, yet
understanding, performing and undertaking interpretation
of plain film images is the fundamental basis of radiography. However, in normal clinical practice, it is the casualty
Comparison of mean estimated and actual accuracy
Group
Statistics
Accuracy (%)
Clinical practice
estimation
Actual test
bank score
Pearson’s
correlation
coefficient (r)
p value
Radiographers
Mean
SD
95% CI
67.8
12.6
61.5e74.1
71.5
11.2
65.9e77.0
0.51
0.02
Nurse practitioners
Mean
SD
95% CI
63.9
12.6
56.2e71.4
52.1
11.2
45.3e58.9
0.41
0.16
Casualty officers
Mean
SD
95% CI
64.2
14.0
51.4e77.2
53.8
13.4
41.4e66.2
0.07
0.87
Please cite this article in press as: Coleman L, Piper K, Radiographic interpretation of the appendicular skeleton: A comparison between
casualty officers, nurse practitioners and radiographers, Radiography (2008), doi:10.1016/j.radi.2007.12.001
ARTICLE IN PRESS
+
MODEL
Radiographic interpretation of the appendicular skeleton
officers and nurse practitioners who routinely interpret
images and document their findings as part of their role in
diagnosing and treating ED patients.
The results of this research suggest that radiographers
have the ability to formally utilise their knowledge in image
interpretation by providing the ED with a written comment
(initial interpretation) to assist in the radiographic diagnosis
and therefore replace the ambiguous ‘red dot’ system used
to highlight abnormal radiographs. It is suggested that the
comment form should comprise a succinct range of tick box
options, with space for additional comments. This would
allow radiographers to develop their vocabulary and comment structure as knowledge and confidence builds.
Maximising the role of the radiographer would possibly
improve job satisfaction and provide stimulus for further
education and development, by recognizing the value of
the radiographer as a vital member of the ED team. It
is vitally important that radiographers feel supported in
this role and it is crucial that continuous training and audit
is undertaken for this to be successful.
The results of this research, although similar to previous
findings, constitute a relatively small sample of data that
may not be representative of the image interpretation
abilities of these professionals in clinical practice; however,
the image test bank was designed to assess the performance and knowledge in image interpretation of these
three groups. The performance of these professional groups
may differ throughout the UK, therefore caution should be
applied regarding the generalisation of the findings.
References
1. Hardy M, Barrett C. Interpretation of trauma radiography by
radiographers and nurses in the UK: a comparative study. Br
J Radiol 2004;77:657e61.
2. Keane D. Radiographer reporting. Paper presented at the European Congress of Radiology; 2005.
3. Snaith B. Are trusts replacing the red dot? Br J Radiol 2003;
(UKRC Suppl.):46e7.
4. Evans R. UK council meeting report. Synergy News; June 2004::4.
5. McLaren P. The evolution of the nurse practitioner. EvidenceBased Healthc Public Health 2005;9:265e6.
6. Read S, Jones N, Williams B. Nurse practitioners in accident
and emergency departments: what do they really do? BMJ
1992;305:1466e70.
7. Mason S, Fletcher A, McCormick S, Perrin J, Rigby A. Developing assessment of emergency nurse practitioner competence e
a pilot study. J Adv Nurs 2005;50(4):425e32.
8. Morris F, Cope A, Hawes S. Training in accident and emergency:
views of senior house officers. BMJ 1990;300:165e6.
9. Freij RM, Duffy T, Hackett D, Cunningham D, Fothergill J.
Radiographic interpretation by nurse practitioners in a minor
injuries unit. J Accid Emerg Med 1996;13:41e3.
10. Meek S, Kendall J, Porter J, Freij R. Can accident and emergency nurse practitioners interpret radiographs? A multicentre
study. J Accid Emerg Med 1998;15:105e7.
11. Sakr M, Angus J, Perrin J, Nixon C, Nicholl J, Wardrope J. Care of
minor injuries by emergency nurse practitioners or junior doctors: a randomised controlled trial. Lancet 1999;354:1321e6.
12. Tachakra S, Deboo P. Comparing performance of ENP’s and
SHO’s. Emerg Nurse 2001;9(7):36e9.
13. Berman L, deLacey G, Twomey E, Twomey B, Welch T, Eban R.
Reducing errors in the accident department: a simple method
using radiographers. BMJ 1985;290:421e2.
7
14. Brealey S, Scally A, Hahn S, Thomas N, Godfrey C, Crane S.
Accuracy of radiographers red dot or triage of accident and
emergency radiographs in clinical practice: a systematic
review. Clin Radiol 2006;61(7):604e15.
15. Brealey S, Scally A, Hahn S, Thomas N, Godfrey C,
Coomarasamy A. Accuracy of radiographer plain film reporting in clinical practice: a meta-analysis. Clin Radiol 2005;
60(2):233e41.
16. Piper K, Paterson A. Initial image interpretation of appendicular skeletal radiographs: a comparison between nurses and
radiographers. Radiography, in press. doi:10.1016/j.radi.
2007.10.006.
17. Berbaum KS. Satisfaction of search in diagnostic radiology.
Invest Radiol 1990;25(2):133e40.
18. Renfrew DL, Franken EA, Berbaum KS, Weigelt FH,
Abu-Yousef MM. Error in radiology: classification and lessons
in 182 cases presented at a problem case conference. Radiology 1992;183:145e50.
19. Piper KJ, Paterson AM, Godfrey RC. Accuracy of radiographers’
reports in the interpretation of radiographic examinations of
the skeletal system: a review of 6796 cases. Radiography
2005;11:27e34.
20. Miller S. Experimental design and statistics. 2nd ed. London:
Methven & Co Ltd; 1984.
21. Obuchowski NA. Receiver operating characteristic curves and
their use in radiology. Radiology 2003;229(1):3e8.
22. Robinson PJA. Radiology’s Achilles heel: error and variation in
the interpretation of accident and emergency radiographs. Br J
Radiol 1997;70:1085e98.
23. Goddard P, Leslie A, Jones A, Wakeley C, Kabala J. Error in
radiology. Br J Radiol 2001;74:949e51.
24. Chakraborty D. Statistical power in observer-performance
studies: comparison of the receiver operating characteristic
and free-response methods in tasks involving localization.
Acad Radiol 2002;9(2):147e56.
25. Eng J. ROC analysis: web-based calculator for ROC curves.
Baltimore: John Hopkins University [updated 2006 May 24].
Available from: <www.jrocfit.org> [accessed 22.06.06].
26. Rorden C. EZANOVA: web-based calculator for analysis of
variance (version 0.97). Available from: <www.mricro.com>
[accessed 22.06.06].
27. Bland M. An introduction to medical statistics. 3rd ed. Oxford:
Oxford University Press; 2000.
28. Anthony D. Receiver operating characteristic analysis: an overview. Nurse Res 1996;4(2):75e88.
29. Overton-Brown P, Anthony D. Towards a partnership in care:
nurses’ and doctors’ interpretation of extremity trauma
radiology. J Adv Nurs 1998;27(5):890e6.
30. Hardy M, Culpan G. Accident and emergency radiography:
a comparison of radiographer commenting and ‘red dotting’.
Radiography 2007;13:65e71.
31. McConnell JR, Webster AJ. Improving radiographer highlighting
of trauma films in the accident and emergency department
with a short course of studydan evaluation. Br J Radiol
2000;73:608e12.
32. Mackay S. The impact of a short course of study on the performance of radiographers when highlighting fractures on trauma
radiographs: ‘‘the red dot system’’. Br J Radiol 2006;79:468e72.
33. Hargreaves J, Mackay S. The accuracy of the red dot system:
can it improve with training? Radiography 2003;9:283e9.
34. Brown V. An investigation of radiographer’s abnormality detection skills focusing on the appendicular skeleton in a trauma
department of a district general hospital. MSc thesis. Canterbury Christ Church University; 2003.
35. Kee F. Confidence limits and the limits of confidence. QJM
2000;93:121e4.
36. Dowie J, Elstein A. Professional judgment. a reader in clinical
decision making. Cambridge University Press; 1994.
Please cite this article in press as: Coleman L, Piper K, Radiographic interpretation of the appendicular skeleton: A comparison between
casualty officers, nurse practitioners and radiographers, Radiography (2008), doi:10.1016/j.radi.2007.12.001