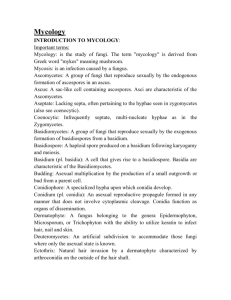
Mycology Manual 11-12
advertisement

Clinical Laboratory Science Program CLS419 – Clinical Microbiology II Mycology Rotation II Manual 2011-2012 CLS419 – Clinical Microbiology II Mycology Manual University of Nebraska Medical Center Clinical Laboratory Science Program Table of Contents Section One Schedule 3-4 Section Two Basics of Mycology 5-21 Yeast 22-31 Section Four Opportunistic Molds 32-40 Section Five Dermatophytes 41-49 Subcutaneous Fungi 50-59 Systemic Dimorphic Fungi 60-67 Section Eight Appendix Mycology Procedures Mycology Lab Worksheet Univ. of WA Mycology Tutor, Table of Contents 68 69-70 71-72 73-74 Section Three Section Six Section Seven CLS419 Clinical Microbiology II Rotation II Mycology Table of Contents Page 1 CLS419 – Clinical Microbiology II Mycology Manual University of Nebraska Medical Center Clinical Laboratory Science Program Section One: Schedule CLS419 Clinical Microbiology II Rotation II Mycology Table of Contents Page 2 Mycology Schedule Reading Assignments: Textbook of Diagnostic Microbiology, Mahon & Manuselis, 4th edition, Chapter 27, pages 603 – 638. Your clinical site will also have a variety of valuable resources such as other textbooks, Mycology atlases (great pictures of fungi), and clinical expertise that you may utilize during this week Websites: University of Washington's Lab Training – Mycology (www.medtraining.org/ltl/) Monday Basics of Mycology Unit Watch lecture on Blackboard Read procedures provided in Manual and on Blackboard Do Study Questions Watch videos on Blackboard o Safety (3:00 minutes) o Scotch Tape Preparation (4:15 minutes) o Tease Preparation (5:00 minutes) o Slide Culture Setup (9:45 minutes) o Slide Culture Take-down (3:00 minutes) Website: Lab Training - Mycology (Univ. of Washington) - Read the following sections (check off as you go from this Table of Contents - 2 pdf pages): o Introduction o Fungal Detection o Organism Identification Yeast Unit Watch lecture on Blackboard Do Case Studies & Study Questions Website: Lab Training - Mycology (Univ. of Washington) - Read the following sections: o Opportunistic Fungi - Overview & Candida albicans o Disease Associations - Superficial Mycoses - Tinea versicolor o Disease Associations - Systemic Mycoses - Cryptococcosis Lab: (Record all results on "Mycology Lab Worksheet" - please document all forms seen) Look at gram stain slides of yeast that are available in your slide box: o Candida albicans o Cryptococcus neoformans Tuesday Opportunistic Molds Unit Watch lecture on Blackboard Do Case Studies & Study Questions Website: Lab Training - Mycology (Univ. of Washington) - Read the following sections: o Opportunistic Fungi - Aspergillus fumigatus, Aspergillus flavus, Rhizopus, Mucor, Alternaria, Fusarium, Penicillium Lab: Look at LPCB preps of opportunistic molds (Record all results on "Mycology Lab Worksheet" - please document all forms seen) that are available in your slide box: o Rhizopus sp. o Aspergillus fumigatus o Aspergillus niger o Penicillium sp. o Fusarium sp. CLS419 Clinical Microbiology II Rotation II Mycology Schedule Page 3 Dermatophytes Unit Watch lecture on Blackboard Do Case Studies & Study Questions Website: Lab Training - Mycology (Univ. of Washington) - Read the following sections: o Disease Associations - Superficial Mycoses - Dematophytosis Lab: Look at LPCB preps of dermatophytes (Record all results on "Mycology Lab Worksheet" - please document all forms seen) that are available in your slide box: o Microsporum canis o Microsporum gypseum o Trichophyton sp. Review previous day’s material Wednesday Subcutaneous Fungi Unit Watch lecture on Blackboard Do Case Studies & Study Questions Website: Lab Training - Mycology (Univ. of Washington) - Read the following sections: o Disease Associations - Subcutaneous Mycoses (Sporotrichosis, Chromoblastomycosis, Mycetomas) o Opportunistic Fungi - Acremonium species Lab: Look at slides of subcutaneous fungi (Record all results on "Mycology Lab Worksheet" - document all forms seen) that are available in your slide box: o Cladosporium, Acrotheca &/or Phialophora forms - LPCB prep o Nocardia sp. - Gram stain o Nocardia sp. - acid fast stain Systemic Dimorphic Fungi Unit Watch lecture on Blackboard Do Case Studies & Study Questions Website: Lab Training - Mycology (Univ. of Washington) - Read the following sections: Disease Associations - Systemic Mycoses - Blastomycosis, Coccidioidomycosis, Histoplasmosis Lab: Look at slides of systemic dimorphic fungi (Record all results on "Mycology Lab Worksheet" - document all forms seen) that are available in your slide box: o Histoplasma capsulatum - mold (LPCB prep) o Histoplasma capsulatum - yeast (GMS stain) o Blastomyces dermatitidis - yeast (LPCB prep) Review previous days’ material Thursday Review: All objectives, case studies, and study questions All learning materials including websites and textbook Mycology Review PowerPoint on Blackboard – recommended that you use this as a “mock practical” Lab: Review all yeast/mold slides Friday Review: All learning materials including websites and textbook Take Mycology Exam and Practical CLS419 Clinical Microbiology II Rotation II Mycology Schedule Page 4 CLS419 – Clinical Microbiology II Mycology Manual University of Nebraska Medical Center Clinical Laboratory Science Program Section Two: Basics of Mycology CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 5 BASICS OF MYCOLOGY Objectives: Upon completion of this CLS 419 unit, the Clinical Laboratory Science student will: 1. Discuss the following requirements of fungi: a. Nutrients b. pH c. Temperature d. Oxygen 2. Compare the two growth forms of fungi: a. Yeast b. Mold 3. Define the following terms: a. Eukaryote b. Prokaryote c. Perfect fungi d. Imperfect fungi e. Hyphae 1) Septate 2) Aseptate (sparsely septate) f. Mycelium 1) Hyaline 2) Dematiaceous g. Dimorphism 4. Identify the following non-reproductive vegetative hyphal structures: a. Favic chandeliers b. Nodular organs c. Racquet hyphae d. Spiral hyphae e. Rhizoids 5. Identify the following asexual reproductive structures: a. Blastoconidia b. Conidia c. Chlamydoconidia d. Arthroconidia e. Sporangium 6. Describe appropriate specimen collection and processing requirements, including appropriate media and incubation for the following: a. Respiratory specimens b. Urine c. Hair, nail and skin scrapings d. Tissue biopsy e. Body fluids f. Exudates (wounds) 7. Interpret the following stains and direct preparations, including the proper uses for each: a. Lactophenol aniline blue 1) Tease mount 2) Scotch tape prep 3)Slide culture b. Potassium hydroxide prep (KOH) CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 6 c. d. e. Methenamine silver stain (GMS) Periodic acid-Schiff stain (PAS) Modified acid fast stain 8. Evaluate the purpose, proper use, inhibitory or selective properties, significant ingredients and colonial appearance of the following media: a. Sabouraud dextrose agar (Emmon’s) b. Mycosel agar c. Inhibitory mold agar (IMA) d. Niger seed agar (TOC) or birdseed agar e. Brain heart infusion with blood agar (BHI) f. Potato dextrose agar g. Cornmeal-Tween 80 agar (CMT) 9. a. Discuss the various approaches used in the laboratory identification of fungal cultures, including: Length of time for growth b. Growth characteristics (media, temperature, etc.) c. Macroscopic appearance d. Microscopic appearance 10. Discuss the appropriateness of anti-fungal susceptibility testing. CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 7 Basics of Mycology I. Introduction A. Mycology is the study of fungi B. Mycoses are fungal diseases 1. Superficial & Cutaneous mycoses a. Involves only hair, skin and nails b. Little or no pathology; main worry is cosmetic effect c. Involves destruction of the keratin of hair, skin and nails d. Primarily caused by the Dermatophytes 2. Subcutaneous mycoses a. Involves skin, muscle and connective tissue immediately below the skin 3. Systemic (deep-seated) / disseminated mycoses a. Caused by pathogenic fungi that are highly virulent b. Involves the deep tissues and internal organs, and has the ability to spread widely throughout the body c. Frequently initial site of infection is the lung 4. Opportunistic mycoses a. Caused by ubiquitous saprophytic (“non-pathogenic”) fungi and occasionally pathogenic fungi, all of which have limited virulence b. Usually see in immunocompromised or debilitated patients c. Causes subcutaneous and disseminated infections C. Patients at risk for fungal infections 1. Immunosuppressed individuals are at highest risk (i.e. AIDS, decreased PMNs) 2. Organ transplant patients and others with previous treatment with corticosteroids, cytotoxic agents, or prolonged antibiotic therapy 3. Patients with malignant neoplasms 4. Patients with various debilitating immunologic and metabolic disorders (i.e. SLE, diabetes) 5. Occupations & activities involving direct skin contact with infected animals/materials and ingestion or inhalation of contaminated aerosols/dust D. Natural habitat is soil and vegetation E. Taxonomy / Classification 1. By disease 2. By class II. Characteristics of Fungi A. Eukaryotic 1. Has a nucleus, nuclear membrane, endoplasmic reticulum, Golgi apparatus, and mitochondria 2. Rigid cell wall containing chitin, mannans, and sometimes cellulose 3. Lacks chlorophyll B. Growth Requirements 1. Nutrients – must absorb from environment since lack chlorophyll 2. pH – prefer neutral but tolerate wide range 3. Temperature – optimal growth at room temperature to 30°C, 37°C for dimorphic yeast 4. Oxygen – most are obligate aerobes 5. Moisture needed to grow, able to survive dry conditions with spores/conidia CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 8 C. Forms 1. Mould / Mold a. Colony – growth of hyphae which form a matt of growth called the mycelium b. Cells – multiple cells forming a filamentous mycelium c. Reproduce either asexually (vegetative sporulation or aerial sporulation) or sexually (sexual sporulation) 2. Yeast a. Colony – bacteria-like, moist, smooth, creamy colonies b. Cells – single, round to oval cells c. Reproduce asexually by budding to form blastoconidia Pseudohyphae – elongation of blastoconidia showing sausage-like constrictions between segments (true hyphae are not constricted at ends) 3. Dimorphism a. Fungi that have the ability to exist in two forms depending on growth conditions b. Generally dimorphic fungi have a mould phase and either a yeast or spherule phase Yeast /tissue phase – grows best at 37°C Mould phase – grows best at room temperature or 30°C D. Structures 1. Hyphae a. Long strand of tube-like structures b. Types Aseptate (or sparsely septate) – without (or very few) transverse walls c. Pigmentation Hyaline – Light colored hyphae and/or conidia (fungi with septate hyphae) due to no pigmentation or brightly pigmented Septate – subdivided into individual cells by transverse walls Dematiaceous – Dark colored (brown-black) hyphae and conidia (fungi with septate hyphae) due to presence of melanin in cell wall 2. Mycelium a. Mass of branching intertwined hyphae forming a matt of growth b. Types Aerial mycelium (also called reproductive mycelium) o Portion of mycelium that projects above the agar surface o Special spore or conidiabearing fruiting bodies derive from this portion Vegetative mycelium o Extends into substratum of agar and is responsible for absorbing water and nutrients CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 9 o Structures Rhizoids – root-like structures that may be located at the base of a sporangiophore or internodally along the hyphae. Favic chandeliers – resemble antlers of a deer, ends are blunt and branched Nodular organs – knots of twisted hyphae Racquet hyphae – resemble tennis racquets with smaller end attached to large end of an adjacent club-shaped hyphae Spiral hyphae – coiled or corkscrew-like turns in hyphae 3. Vegetative reproductive structures Arthroconidia (arthrospores) o Thick-walled barrel-shaped conidia produced by fragmentation of the hyphal strand through the septation points. They may form adjacent to each other or may be separated by alternating empty spaces. Blastoconidia (daughter cells) o Budding forms characteristically produced by yeast o A bud scar (dysjunctor) often remains at point where conidium detached Chlamydoconidia (Chlamydospores) o Formed from pre-existing cells in the hyphae, which become thickened and enlarged o May be found within (intercalary), along the side (sessile), or at the tip (terminal) 4. Aerial reproductive structures (fruiting bodies) Sporangiospores o Spores contained in a closed sac called a sporangium o The sporangium is supported on a base, termed the columella, which is located at the tip of the specialized hyphal segment called the sporangiophore o This type of sporulation is characteristic of the Zygomycetes Conidia o Spores produced on the surface of an elaborate fruiting body supported by a specialized hyphal segment called a conidiophore o The conidiophore can branch into secondary segments called metulae which can become conidia-producing segments called phialides CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 10 Phialoconidia o Conidia which arise from a tube or vase-shaped structure called a phialide o This type of sporulation is characteristic of the Penicillium species Annelloconidia o Conidia which arise from a tube or vase-shaped structure termed a annellide o The tip of the phialide cyclically extends and retracts when conidia form, leaving a succession of scars o Conidia may be formed singly, in long chains, or in tightly bound clusters Macroconidia o Larger, multi-celled conidia that can vary in size and shape o The term “macro” should only be used when smaller conidia are present. Microconidia o Tiny one-celled conidia, usually borne either directly from side of hyphae or supported by a hair-like conidiophore o The term “micro” is used only when larger conidia are present 5. Sexual reproductive structures a. Fungi having a sexual stage are termed “Perfect Fungi” b. Fungi lacking a sexual stage are termed “Fungi Imperfecti” c. Sexual sporulation requires 2 specialized fertile cells (having undergone meiosis) to merge and have nuclear recombination occur on the aerial hyphae Ascospores o Sexual spores (meiotic division) produced in a sac-like structure called an ascus. The ascus is the sexual mother cell that forms ascospores inside and may be protected on the outside by an cleistothecium. The cleistothecium is a protective sac within which asci and ascospores form. Oospores o Fusion of 2 morphologically identical cells from different hyphal segments Zygospores o Fusion of 2 morphologically identical cells from the same hyphal structure o Zygomycetes reproduce sexually in this manner III. Specimen Collection & Transport A. Specimen types and collection 1. Blood and bone marrow a. Acquire by sterile technique b. Inoculate biphasic agar-broth bottles designed specifically for fungal cultures CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 11 2. CSF a. Acquire by sterile technique and transport in sterile container b. Centrifuge and use sediment to make slides and inoculate media c. Keep at room temperature is culture setup is delayed 3. Cutaneous: Hair, nail and skin scrapings a. Hair Use Wood’s lamp to see infected areas. Pull out hair by roots with sterile tweezers. If no fluorescence, pull out hairs that are broken and scaly Transport in sterile container b. Nails Clean with 70% alcohol Scrape away and dispose of outer layers of nail Sample from beneath the nail plate to obtain softened material from nail bed, or collect shavings from deeper portions Place into sterile container c. Skin Clean with 70% alcohol If lesion present, scrape the actively growing edge Scrape areas that look most infected 4. Respiratory: bronchial washings, sputum, throat, transtracheal aspirates a. Early morning specimen is best b. 24 hour collections unacceptable (bacterial overgrowth) c. Transtracheal aspirate should eliminate throat flora d. Prepare slides for stains 5. Tissue biopsies a. Collected by physician and should be kept moist with sterile saline in a sterile container until processed b. Should include normal tissue and tissue from the center and edge of lesion c. Inspect tissue for granules and areas of pus and necrosis d. Mince tissues for inoculation to media especially if Zygomycetes are suspected 6. Urine a. Early morning clean catch or catheterized specimen is best b. 24 hour collections unacceptable (bacterial overgrowth) c. Centrifuge specimen and inoculate media with sediment 7. Vaginal, uterine cervix, prostatic secretions a. Acquire by sterile technique and transport in sterile container 8. Wounds, subcutaneous lesions, mucocutaneous lesions, exudates a. Acquire by sterile technique and transport in sterile container b. From cysts and abscesses, material should be aspirated if possible c. Examine for granules B. Specimen Collection Issues 1. Collect from area most likely to be affected 2. Use sterile technique, avoid contamination with hands 3. Specimen must be adequate, reduces contamination 4. Keep specimen moist 5. Specimen must be properly labeled 6. Exact source/site aids in identification 7. Specimen must be delivered promptly to lab and processed quickly a. Prevents overgrowth of bacteria and ubiquitous molds b. Pathogenic molds can be slow growers c. Yeast multiply quickly so refrigerate if delay in setting up culture CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 12 IV. Direct Examination of Specimens Provides rapid preliminary report and immediate presumptive diagnosis to guide the physician in treatment Special morphological characteristics may give clues to the identity of the causative agent Aids in selection of special media to inoculate specimen to Direct exam may show evidence of infection despite negative cultures Allows for observation of yeast phase of dimorphic organisms May indicate need for more than one type of direct examination to be performed A. Saline wet mount 1. Phase-contrast microscope is valuable or can use low light 2. Look for fungal elements such as: a. Budding yeast with pseudohyphae (Candida) b. Broad base budding yeast (Blastomyces dermatitidis) c. Spherules (Coccidioides immitis) d. Capsules (Cryptococcus neoformans) B. Lactophenol aniline blue (LPAB) wet mount 1. Phenol kills organisms 2. Lactic acid preserves fungal structures 3. Aniline blue stains the chitin in fungal cell walls 4. LPAB prep can be made permanent 5. Look for fungal elements C. Potassium hydroxide (KOH) preparation (10%) 1. Hair, skin or nail specimens KOH dissolves the keratin to make fungi more visible 2. Specimens containing cellular material such as sputum or vaginal secretions KOH dissolves the cells in background to make yeast / fungal elements more visible 3. Procedure a. Add a drop of 10% KOH to specimen on slide. Coverslip. Gentle heating may aid in dissolving debris If specimen is thick, it may take 15-30 minutes to dissolve b. Observe under low light or with phase-contrast microscope D. Gram stain 1. Fungi stain gram positive 2. Look for yeast and fungal elements such as pseudohyphae 3. True fungi are 2-3 times wider than GPR’s and will not stain solidly inside 4. Capsule around yeast can prevent the definitive staining of the yeast itself E. Acid-fast stain 1. Nocardia is partially positive with a modified Kinyoun acid-fast stain 2. Ascospores of Saccharomyces cerevisiae are acid-fast positive F. India ink preparation 1. Used to observe for capsules around yeast (esp. Cryptococcus neoformans) 2. Procedure a. Mix small drop of India ink with a drop of specimen and coverslip. (Strive for a thin smear) b. Let sit (up to 10 minutes) to allow cells to settle c. Observe under microscope with condenser adjusted for maximum light. Look for a clear capsule around yeast. Background is dark. CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 13 G. Calcofluor white stain 1. Binds to polysaccharides in fungal cell walls 2. Fluoresces when exposed to UV light 3. 10% KOH can be added to dissolve background 4. Procedure a. Add drop of Calcofluor White stain to specimen on slide. Coverslip. b. Allow to sit approximately 3 minutes. c. Use a fluorescent microscope and look for apple green fluorescence. H. Tissue / Histological stains 1. Wright’s stain – look for intracellular yeast in tissue and bone marrow (Histoplasma capsulatum) 2. Gomori Methenamine Silver (GMS) stain – fungi, Pneumocystis, and Actinomyces stain black against a green background 3. Periodic Acid Schiff (PAS) stain – fungal elements are magenta against a light pink or green background V. Selection and Inoculation of Culture Media A. Safety 1. Tube media preferred over plate media a. Tube media will not dry out over long incubation periods b. Reduces chance for fungal reproductive structure to become airborne and contaminate the room and people c. Never use plates when suspect Coccidioides immitis (extremely infectious and aerosols may be inhaled) 2. ALWAYS work under a biological safety cabinet 3. Wear gloves and lab coat 4. Autoclave specimens and inoculated media when finished 5. Disinfect work area daily B. Primary isolation media for fungi 1. Goal is to isolate all possible pathogens 2. Generally want 2 types of media – a nonselective media and a selective media (with antibiotics to inhibit growth of bacteria and enriched for more fastidious fungi) 3. Ingredients required for fungal growth include carbon, nitrogen, vitamins, minerals and amino acids 4. Nonselective Media a. Brain heart infusion (BHI) with/without 5% blood Primary recovery of saprophytic and dimorphic fungi Useful for isolation of Histoplasma and Nocardia (media containing blood) Useful to convert dimorphic molds from mold to yeast phase when incubated at 35ºC Antibiotics (cycloheximide & chloramphenicol) can be added to make media selective for dimorphic moulds b. Inhibitory mold agar (IMA) The best medium to isolate fungal opportunists from a non-sterile site Primary recovery of dimorphic pathogenic fungi and saprophytic fungi that are inhibited by cycloheximide Chloramphenicol & gentamicin inhibit growth of bacteria c. Sabouraud’s brain heart infusion agar (SABHI) Primary recovery of saprophytic and dimorphic pathogenic fungi, particularly fastidious strains CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 14 5. Selective Media a. Mycosel agar Selective for isolation of dermatophytes Chloramphenicol inhibits bacteria and Nocardia Cycloheximide inhibits rapid saprophytes and: o Aspergillus fumigatus (25-60%) o Cryptococcus neoformans o Candida krusei o Pseudallescheria boydii o Candida tropicalis o Nocardia asteroids o Candida parapsilosis o Piedraia hortae o Trichosporon beigelii (cutaneous) b. Dermatophyte test medium (DTM) Screening media for dermatophytes pH change causes the phenol red indicator to change from yellow to red Contains antibiotics 6. Incubation temperature a. 30ºC is best (room temperature = 25ºC, is acceptable, some fungi may multiply slower at this temperature) b. 37ºC may inhibit some fungi, but necessary for yeast phase of dimorphic fungi 7. Incubation time a. Hold cultures for 4-6 weeks, examining twice weekly for growth b. Dependent on media, temperature and inhibitors in the specimen 8. Incubation atmosphere a. Moist – 40-50% relative humidity b. Ambient air C. Subculture and special identification media for fungi 1. Once fungi have grown on primary culture, one frequently needs to subculture for complete isolation and identification 2. Media a. Sabouraud dextrose agar (SDA) Supports growth of all fungi (except Histoplasma and Nocardia) Consists of dextrose, peptone, agar and water pH 5.6 to inhibit bacteria which prefer pH 7.2 b. Neutral Sabouraud dextrose agar (Emmon’s modification) Subculture yeast, allows for better maintenance of yeasts Less dextrose and a neutral pH compared to regular SDA c. Cornmeal-Tween 80 agar (CMT) Promotes hyphal and blastoconidia formation Observe pseudohyphae & chlamydoconidia production by Candida albicans Enhances pigment of Trichophyton rubrum when 1% glucose is added Procedure o With loop, make one streak into the agar down the center of an area and 3 or 4 parallel cuts across the first ½ inch or 1 cm apart, holding the inoculating wire at about a 45º angle to dilute inoculum. o Incubate 24-72 hours at 30ºC o After incubation, place coverslip on surface of the agar, covering inoculation streaks o Examine growth through the coverslip with the microscope using the 10x and 40x objectives. Look for the most characteristic morphology near the outer edges of the coverslip. CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 15 d. Niger seed agar or Birdseed agar Used for isolation of Cryptococcus neoformans from contaminated specimens Cryptococcus neoformans produces phenoloxidase enzymes. These enzymes break down the substrate caffeic acid forming a brown pigment e. Tween 80 / Oxgall / caffeic acid agar (TOC) Observe brown pigment production by Cryptococcus neoformans Can observe germ tube production by Candida albicans Better chlamydoconidia development than Cornmeal/Tween 80 f. Potato dextrose agar Stimulates spore formation and pigmentation Used to subculture fungi for slide culture and observe for colony morphology VI. Examining the Fungal Culture A. Differentiating Pathogenic fungi 1. Growth rate is 10 days or more (slow growers) 2. Growth on Mycosel agar 3. Color: dull buff, brown, mousey gray 4. Dimorphic a. Mold phase grows at 30°C (room temperature) b. Yeast phase grows at 35°C on BHI agar B. Identification of fungi 1. Growth rate a. Rapid = 1-5 days b. Intermediate = 6-10 days c. Slow = 11-28 days 2. Colonial morphologic features a. Appearance (topography) Rugose – colonies have deep furrows irregularly radiating from the center Umbonate – colonies have a button-like central elevation Verrucose – colonies have a wrinkled, convoluted surface Flat b. Texture Cottony (wooly) – very high, dense aerial mycelium Glabrous (waxy) – smooth surface due to no aerial mycelium (yeast-like) Granular (powdery) – flat and crumbly due to dense conidia production Velvety – colonies produce low aerial mycelium c. Pigmentation Observe color on both surface of colony and on reverse side of plate 3. Microscopic morphologic features a. Most definitive means of identification b. Evaluate: Shape Method of production Arrangement of conidia/spores Size and color of hyphae CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 16 4. Microscopic techniques for evaluating fungi a. Tease mount Procedure o Using two sterile teasing needles, transfer a portion of colony (middle third) to a slide o Gently tease mycelium apart with teasing needles o Add a drop of Lactophenol aniline blue stain o Coverslip and observe for fruiting structures under light microscope at 10x and 40x Advantage o Perform and examine immediately after maturation Disadvantage o Structural morphology is disturbed b. Scotch tape preparation Procedure o Lightly touch transparent scotch tape, sticky side down, to surface of colony and then removing it o Place a drop of Lactophenol aniline blue stain onto a slide o Affix tape, sticky side down, into the stain on the slide o Observe for fruiting structures under light microscope at 10x and 40x Advantages o Perform and examine immediately after maturation o Retains juxtaposition of spores and hyphal elements Disadvantages o Prep is not easily preserved (view within 30 minutes and then discard slide) o Contamination can occur c. Slide culture Procedure o Place glass slide on 2 wooden sticks in Petri dish (gauze or paper towel under sticks moistened with sterile water) o Using sterile scalpel, cut 1 cm x 1 cm square of SAB or Potato dextrose agar and place on slide. Two pieces of agar can be placed on the slide to provide duplicate cultures. o Inoculate the 4 sides of the agar with mould using teasing needles or sterile wooden stick o Place coverslip on top of agar o Tape plate shut and incubate at room temperature (22°C) o Examine for growth periodically & add more water as needed to keep moist o When conidia / spores are evident, carefully lift coverslip off agar using forceps and place onto slide containing a drop of lactophenol aniline blue stain (coverslip can be sealed with fingernail polish to keep slide permanently) o Observe under light microscope at 10x and 40x Advantages o Fungal elements are grown and maintained in their original juxtaposition, making identification easier o Two mounts from one culture, so you can view one slide and if necessary, leave the other slide to incubate longer Disadvantages o Technical expertise required CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 17 o o VII. Must wait for fungus to mature on inoculated media before identification can occur Zygomycetes grow past coverslip before forming reproductive structures Serologic Diagnosis of Fungal Disease Generally performed only in select reference laboratories A. Immunodiffusion 1. Aspergillus 2. Blastomyces 3. Histoplasmosis B. Complement fixation 1. Blastomyces 2. Coccidioidomycosis 3. Histoplasmosis C. ELISA 1. Aspergillus D. EIA 1. Blastomyces 2. Candida E. Latex agglutination 1. Cryptococcus (more sensitive than India Ink Stain in CSF) 2. Candida F. Fluorescent antibody 1. Pneumocystis VIII. Molecular Diagnosis of Fungal Disease A. Probes 1. Used to identify: a. Histoplasma capsulatum b. Blastomyces dermatitidis c. Coccidioides immitis d. Cryptococcus neoformans IX. Antifungal Susceptibility Testing A. Appropriateness 1. CLSI has released 3 methods for fungal testing a. Yeast testing b. Mould testing c. Disk diffusion testing (microtiter and Etest) 2. Concerns a. Lack of established breakpoints for most fungal agents b. Emergence of antifungal resistance CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 18 B. Anti-fungal classes and agents 1. Polyenes a. Amphotericin B (primary antifungal agent used today) 2. Azoles a. Fluconazole (primary antifungal agent in treating yeast infections) b. Intraconazole c. Voriconazole 3. Candins a. Caspofungin CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology Page 19 Basics of Mycology – Study Questions 1. True or False. Fungi resemble plants in that both contain chlorophyll. 2. True or False: Arthroconidia reproduce by fragmentation. 3. The two growth forms of fungi include: a. Yeast and hyphae b. Yeast and mould c. Blastoconidia and mould d. Conidia and hyphae 4. A mass of branching intertwined hyphae forming a matt of growth is known as: a. Hyphae b. Conidia c. Mycelium d. Favic chandeliers 5. Blastoconidia that have elongated are known as: a. Hyphae b. Pseudohyphae c. Arthroconidia d. Racquet hyphae 6. The India ink stain is used to detect what part of a yeast cell? a. Chlamydoconidia b. Pseudohyphae c. Blastoconidia d. Capsule 7. A fungus that has a yeast phase that grows at 35°C and a mold phase that grows at 30°C is referred to as: a. Dimorphic b. Polymorphic c. Bimorphic d. Anamorphic 8. The purpose for using a KOH preparation when doing a direct examination for fungi is to: a. Dissolve the keratin to unmask the fungus elements b. Stain the hyphae and conidia of the fungi c. Reveal capsules that may be found around yeast cells d. Kill any bacteria that may be present in the specimen 9. In the Lactophenol aniline blue stain, what reagent stains the chitin in the fungal cell wall? a. Aniline blue b. Phenol c. Lactic acid d. Glycerol 10. What is the atmospheric requirement for fungi to grow? a. Anaerobic b. Ambient air c. 5-10% CO2 d. >10% CO2 CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology – Case Studies & Study Questions Page 20 11. Of the following techniques, which one is the best for maintaining the juxtaposition of the fungal elements and can be kept in the laboratory permanently? a. Tease preparation b. Scotch tape preparation c. Slide culture 12. Which of the following approaches is NOT used in the identification of fungi? a. Growth rate b. Colony morphology c. Microscopic appearance d. Methylene blue stain 13. What is/are the benefits to performing a direct mount examination on every specimen submitted for fungal culture? a. Allows you to send out an immediate preliminary report to the primary care provider so they can initiate treatment or look for other diagnoses b. Enables you to know if special media needs to be inoculated c. Allows you to observe the yeast phase of dimorphic organisms d. May provide a clue as to the identity of the causative agent without having to wait for the fungus to incubate e. All of the above 14. Match the media with its general use (answers can be used more than once and items can have more than one answer): _____ Mycosel agar a. Nonselective, primary isolation media b. Demonstrate phenol-oxidase enzyme c. Promotes blastoconidia, chlamydospores and hyphal formation d. Selective media e. Stimulates spore formation and pigmentation f. Used to demonstrate yeast phase of dimorphic fungi _____ Sabouraud’s Dextrose agar _____ Brain Heart Infusion agar _____ Cornmeal Tween 80 agar _____ Inhibitory Mold agar _____ Niger Seed agar _____ Potato Dextrose agar 15. Match the image with its descriptive term. _____ Mycelium a. d. _____ Nodular organ _____ Spiral hyphae b. e. _____ Racquet hyphae _____ Favic chandelier CLS419 Clinical Microbiology II Rotation II c. Mycology Basics of Mycology – Case Studies & Study Questions Page 21 16. Match the picture of the asexual structure with its descriptive term. _____ Blastoconidia _____ Arthroconidia a. d. _____ Macroconidia _____ Microconidia b. _____ Phialoconidia e. _____ Sporangiospores c. 17. List three general rules for good collection of fungal specimens. 18. A nurse calls you and asks how to collect a toenail sample for a fungal culture. Give complete instructions that you would give to the nurse. Then describe a basic outline of what process you as a clinical laboratory scientist will follow relating to direct examination, specimen processing and fungal culture setup when you receive the specimen in the lab. CLS419 Clinical Microbiology II Rotation II Mycology Basics of Mycology – Case Studies & Study Questions Page 22 CLS419 – Clinical Microbiology II Mycology Manual University of Nebraska Medical Center Clinical Laboratory Science Program Section Three: Yeast CLS419 Clinical Microbiology II Rotation II Mycology Yeast Page 23 YEAST Objectives: Upon completion of this CLS 419 unit, the Clinical Laboratory Science student will: 1. Describe the following characteristics common to yeast: a. Gram stain morphology b. Colony morphology c. Growth rate 2. Describe the following structures seen in yeasts: a. Blastoconidia b. Arthroconidia c. Chlamydoconidia d. Germ tube e. Capsule f. Pseudohyphae 3. Explain the principle of the following tests, including the interpretation of results: a. Germ tube production b. Antigen testing c. Urease d. Niger seed agar (TOC) e. Carbohydrate utilization 4. a. b. c. d. e. Differentiate Candida albicans from Candida glabrata, based on the following: Cornmeal-Tween-80 agar Germ tube Rapid trehalose assimilation Colony morphology on Sheep Blood Agar Gram stain/wet prep 5. Describe the specific growth requirements of Malassezia furfur. 6. Correlate the clinical, epidemiological and laboratory findings associated with the following infections: a. Candida albicans 1) Cutaneous (diaper rash, onychomycosis) 2) Mucocutaneous (thrush, vaginitis, pulmonary and alimentary infections) 3) Systemic (UTI, diabetics, endocarditis) b. Candida species 1) Opportunistic infections c. Cryptococcus neoformans 1) Respiratory infections 2) Meningitis d. Candida glabrata 1) Urinary tract infections e. Malassezia furfur 1) Tinea versicolor 2) Systemic infections associated with nutritional lipid supplements CLS419 Clinical Microbiology II Rotation II Mycology Yeast Page 24 YEAST I. General Characteristics A. Can isolate from almost any specimen 1. Generally considered normal flora 2. Opportunistic pathogen B. Unicellular C. Reproduction 1. Asexual a. Blastoconidia (budding yeast) Pseudohyphae = elongated blastoconidia b. Arthroconidia 2. Sexual a. Ascospores (acid fast positive = Saccharomyces species) D. Direct examination 1. Observe for reproductive structures 2. Gram stain: large, gram-positive budding yeast and pseudohyphae 2. India ink prep: observe for capsules around cells (Cryptococcus) E. Growth 1. Rate: 2-3 days on Sheep Blood Agar and most other nonselective primary isolation media 2. Temperature: 22-37°C (best at 30°C) F. Colony morphology 1. Appearance a. Similar to bacterial colony b. Moist, smooth 2. Texture a. Can be glabrous (waxy), mucoid, butter-like, wrinkled, or velvety b. Can see filaments around perimeter of colony 3. Color a. White, cream, tan (rarely pink or salmon) 4. May be confused with Staphylococcus species a. Yeast grow on sheep blood agar b. Yeast are catalase positive and coagulase negative just like Staph epi c. MUST confirm with Gram stain or LPAB stain II. Yeast Identification Methods A. Germ Tube Production 1. First test performed upon isolation of yeast 2. Most important and easiest test to perform to identify yeast 3. Procedure a. Emulsify small amount of yeast in tube containing 0.5-1.0 ml sterile serum (rabbit, fetal calf, or human) b. Incubate at 35°C for 2.5-3.0 hours c. Place one drop of suspension on a slide, coverslip, and examine microscopically on 40x for long tube-like projections (germ tubes) extending out from the yeast cells. d. Do not confuse germ tube with pseudohyphae (constricted at point of attachment) CLS419 Clinical Microbiology II Rotation II Mycology Yeast Page 25 Germ Tube Parallel sides Non-septate No constriction at point of attachment Pseudohyphae Not necessarily parallel May be septate Constricted at point of attachment B. Microscopic morphology on Cornmeal-Tween 80 agar (CMT) 1. When germ tube is negative, subculture yeast to CMT agar 2. Refer to “Basics of Mycology” lecture (p. 15) for procedure 3. Observe microscopically for characteristic features of chlamydoconidia, blastoconidia, pseudohyphae and arthrospores C. Niger Seed Agar (Birdseed agar) 1. Observe for pigment production 2. Cryptococcus neoformans produces dark brown colonies on agar due to phenol oxidase activity which decomposes melanin in yeast cell walls. D. Biochemical Tests a. Urease production Positive: Cryptococcus sp. (rapid), Trichosporon sp., Rhodotorula sp. Negative: Candida sp., Geotrichum sp. b. Carbohydrate assimilation Ability of yeast to utilize a particular carbohydrate as a sole source of carbon in the presence of oxygen Look for growth or no growth c. Carbohydrate fermentation Ability of yeast to utilize a carbohydrate anaerobically Byproducts are alcohol and CO2, look for gas d. Commercial identification systems Manual kit method examples include API 20C, API YeastIdent Automated method examples include MicroScan Rapid Yeast Ident, Vitek 2 YST card III. Clinically Significant Yeast A. Candida albicans and other Candida species 1. Normal flora of skin, mucous membranes and intestinal tract 2. Leading opportunistic fungal infection in man a. Candidiasis (Candidosis, Moniliasis) Mucocutaneous (most common) o Thrush (oral) o Vaginitis o Bronchial and pulmonary o Alimentary o Chronic mucocutaneous Cutaneous o Areas of profuse sweating or immersion in water o Skin – severe diaper rash o Nails - oncychomycosis Systemic o Most devastating o UTI o Endocarditis o Septicemia CLS419 Clinical Microbiology II Rotation II Mycology Yeast Page 26 b. Factors predisposing to infection Immunocompromised Malignancy Prolonged antibiotic therapy Lupus Diabetes Pregnancy and use of birth control pills Age – infancy and old age Damaged skin barrier – catheters, burns, wounds c. Etiologic agents Candida albicans – number one fungal isolate in laboratory Other medically important species that can cause opportunistic infections: o Candida (Torulopsis) glabrata o Candida parapsilosis o Candida tropicalis o Candida krusei o Candida stellatoidea 3. Identification a. Candida albicans Germ tube: positive within 3 hours (95% of time) CMT: Clustered blastoconidia at septa of pseudohyphae, terminal chlamydoconidia CHO assimilation: sucrose positive b. Candida stellatoidea Germ tube: positive within 3 hours CMT: Blastoconidia, pseudohyphae, terminal chlamydoconidia CHO assimilation: sucrose negative c. Candida (Torulopsis) glabrata Second most common cause of urinary yeast infections Germ tube: negative at 3 hours CMT: Only blastoconidia, no pseudohyphae CHO assimilation: only glucose and trehalose positive d. Candida tropicalis Germ tube: rarely positive in 3 hours CMT: Sparse single or short-chained blastoconidia anywhere along pseudohyphae, rare chlamydospores CHO assimilation: sucrose positive e. Candida krusei Germ tube: negative at 3 hours CMT: Tree-like branching of abundant blastoconidia from the septa of elongated pseudohyphae (“crossmatchsticks” appearance) f. Candida parapsilosis species complex Germ tube: negative at 3 hours CMT: Few single or small clustered blastoconidia at or between septa of thin curved pseudohyphae. Sometimes giant pseudohyphae may be observed CLS419 Clinical Microbiology II Rotation II Mycology Yeast Page 27 B. Cryptococcus neoformans 1. Causes Cryptococcosis a. Inhale yeast and develop mild respiratory infection b. Primary pulmonary disease – debilitated patients, overwhelming or continual exposure - pneumonia c. Meningitis – organism has predilection for brain and meninges d. Septicemia e. Major cause of opportunistic infection in AIDS patients 2. Isolated from soil contaminated by pigeon droppings (major source), fruits, milk, plants, feces of normal humans 3. Identification a. Direct examination Gram stain: very large and round budding yeast, may not stain well if polysaccharide capsule present India ink stain o Positive 50% of time in CSF o Aids in viewing polysaccharide capsule b. Colony morphology – mucoid due to capsules c. Germ tube: negative at 3 hours d. CMT: large, round blastoconidia, no pseudohyphae e. Urease: rapidly positive (within 3 hours) f. Niger seed agar, TOC agar Cryptococcus neoformans: brown pigment Other Cryptococcus species and other yeasts: no brown pigment g. Serological testing Cryptococcal antigen test o Indirect agglutination test o Antibody to polysaccharide capsule is coated onto latex particles o Test for antigen (capsule) in CSF and serum o More sensitive than India Ink prep C. Geotrichum candidum 1. Causes Geotrichosis – pulmonary disease in immunocompromised patients 2. Disease state is similar to Candida – often pulmonary or mimics thrush (mucocutaneous) 3. Not a true yeast, is really a mold 4. Identification a. Germ tube: negative at 3 hours b. CMT: arthroconidia and true hyphae c. Urease: negative D. Malassezia furfur 1. Causes Tinea versicolor (Pityriasis versicolor) a. Superficial fungal infection b. Infection of the horny layer of the epidermidis c. Characterized by reddish-brown, brown or white scaly patches on skin d. Lesions fluoresce yellow under Wood’s lamp 2. Also can cause septicemia in patients receiving lipid therapy by IV 3. Identification a. KOH preparation of skin scrapings: clusters of thick-walled, round budding yeast and short, straight or angular mycelial fragments (spaghetti and meatball appearance) b. Lipophilic: in order to culture organism, must overlay culture media with olive oil (growth occurs in 24 hours) CLS419 Clinical Microbiology II Rotation II Mycology Yeast Page 28 Yeast Case Study #1 A 45-year old pigeon breeder, who recently received a renal transplant (and thus was on immunosuppressive steroids), complained to his physician of headache, dizziness, blurred vision, and a stiff neck. Specimens of purulent cerebrospinal fluid were sent to the microbiology laboratory. A carefully examined Gram stain of the CSF sediment was negative; however, on brain heart infusion agar with blood at 30ºC, a white, mucoid yeast rapidly grew. The organism was inhibited on brain heart infusion agar with blood, gentamicin, cyclohexamide and chloramphenicol. 1. Which disease do you suspect? Circle the letter of the correct answer. a. Candidiasis b. No disease – organism was a laboratory contaminant c. Cryptococcosis d. Histoplasmosis 2. Give three reasons for choosing your answer to question #1. 3. If the yeast was significant, why was it not observed on the CSF Gram stain? 4. If your answer to question #1 was not “b”, what three tests would you perform to speciate the yeast? CLS419 Clinical Microbiology II Rotation II Mycology Yeast – Case Studies & Study Questions Page 29 Yeast Case Study #2 Directions - Within CLS419 Clinical Microbiology II, go to Assignments, Clinical Rotation – Mycology, and then Yeast Unit. Go to the corresponding case study to view the microscopic examples for each case. Click on an image to see an enlarged view. Answer the following short answer or single answer multiple choice questions for each case. This organism was isolated from the sputum of a HIV+, 37-year-old male with a CD4 cell count of <200/mm3. The organism grew on SDA (25ºC), and blood & chocolate agar (35ºC), at 24 hours of incubation. 1. Presumptively identify the fungus. 2. Which of the following conventional tests should be performed to confirm the identification? A. Germ tube production, slide culture B. Germ tube production, urease production C. Phenol oxidase activity (Birdseed or Niger seed agar), urease production D. Slide culture, urease production Due to the identification of the fungus in the patient’s sputum, a CSF was submitted for direct antigen testing. Look at the test results on Blackboard. The test utilizes two latex suspensions: Antigen latex – detects polysaccharide capsule Normal globulin latex – detects interfering substances in specimen which cause a false + reaction Each specimen and control is tested with both latex suspensions, except for the ‘normal globulin positive control which is tested only with the normal globulin latex. 3. The direct antigen test results indicate the patient’s CSF is: A. Negative for antibodies to the polysaccharide capsule B. Negative for the polysaccharide capsule C. Positive for antibodies to the polysaccharide capsule D. Positive for the polysaccharide capsule CLS419 Clinical Microbiology II Rotation II Mycology Yeast – Case Studies & Study Questions Page 30 Yeast Study Questions 1. Match the yeast with its key identifying characteristic: ____ Candida parapsilosis a. Short-chained blastoconidia anywhere along pseudohyphae b. Thick capsule c. Cross-matchsticks blastoconidia d. Terminal chlamydospores e. Giant pseudohyphae ____ Candida krusei ____ Candida tropicalis ____ Candida albicans ____ Cryptococcus neoformans 2. Identify the structures shown in these two drawings. a. ____________________ b. ____________________ c. ____________________ d. ____________________ D 3. What key test is used to definitively identify Candida albicans? a. Gram stain b. Germ tube c. Colony morphology d. KOH preparation 4. The number 1 fungal agent isolated in the clinical laboratory is: a. Malassezia furfur b. Cryptococcus neoformans c. Candida albicans d. Candida glabrata 5. What disease(s) does Candida albicans cause? a. Mucocutaneous infections b. Cutaneous infections c. Systemic infections d. All of the above 6. Which yeast, in order to grow on culture media, requires olive oil to be overlaid the media? a. Malassezia furfur b. Cryptococcus neoformans c. Candida albicans d. Candida glabrata 7. True or False: All Candida albicans produce germ tubes and chlamydospores. 8. True or False: A germ tube is constricted at its point of attachment to the mother cell. CLS419 Clinical Microbiology II Rotation II Mycology Yeast – Case Studies & Study Questions Page 31 9. Which yeast can be identified when the germ tube is negative and carbohydrate assimilation of glucose and trehalose? a. Cryptococcus neoformans b. Candida albicans c. Candida stellatoidea d. Candida glabrata 10. What are pseudohyphae? 11. What steps are taken to identify yeast in the clinical laboratory? CLS419 Clinical Microbiology II Rotation II Mycology Yeast – Case Studies & Study Questions Page 32 CLS419 – Clinical Microbiology II Mycology Manual University of Nebraska Medical Center Clinical Laboratory Science Program Section Four: Opportunistic Molds CLS419 Clinical Microbiology II Rotation II Mycology Opportunistic Molds Page 33 OPPORTUNISTIC MOULDS Objectives: Upon completion of this CLS 419 unit, the Clinical Laboratory Science student will: 1. Discuss the following characteristics common to opportunistic molds: a. Rapid growth b. Airborne c. Opportunistic pathogens d. Frequent laboratory contaminants 2. Discuss the following characteristics common to the Zygomycetes: a. Asexual reproductive structures b. Aseptate hyphae (sparsely septate) c. Mycelial growth 3. Identify the following fungi using macroscopic and microscopic morphology: a. Absidia species b. Mucor species c. Rhizopus species d. Aspergillus fumigatus e. Aspergillus flavus f. Aspergillus niger g. Penicillium species h. Fusarium species i. Alternaria species 4. Correlate the clinical, epidemiological and laboratory findings associated with the following infections: a. Zygomycetes 1) Zygomycosis 2) Predisposing conditions (diabetes) b. Aspergillus fumigatus/Aspergillus flavus 1) Aspergillosis a) Allergic bronchopulmonary (farmer’s lung) b) Colonizing (fungus ball) c) Invasive forms c. Aspergillus niger 1) Swimmer’s ear d. Fusarium species 1) Mycotic keratitis CLS419 Clinical Microbiology II Rotation II Mycology Opportunistic Molds Page 34 OPPORTUNISTIC MOLDS I. Basic Characteristics A. Rapid growers – initial growth at 2-3 days with mature colonies in 4-5 days B. Found in soil (saprobic) and conidia/spores are airborne C. Opportunistic pathogens 1. Normally inhaled – dependent upon body’s response after inhalation 2. Immunocompromised patients are susceptible (AIDS, cancer, transplant) D. Treatment 1. Can be very toxic 2. Important to determine if isolate is a contaminant or causing disease 3. Examine tissue or isolate from more than one body site to determine pathogenesis II. Aseptate (sparsely septate) opportunistic molds A. Zygomycetes 1. Identification a. Colony morphology Lid lifters o Mycelium very cottony (wooly) b. Microscopic examination Asexual reproductive structures o Sporangiospores inside sporangium o Broad, irregular width, ribbon-like aseptate hyphae o Rhizoids 2. Clinical Significance a. Causes Zygomycosis b. Predisposition Diabetics in ketoacidosis Malnutrition Immunosuppressed Prolonged antibiotic therapy (decrease normal flora) c. Pathogenesis Inhale spores Infects nasal sinuses (nasal discharge is black) Spreads to adjacent blood vessels Causes necrosis and vascular thrombosis (blood clots) Can migrate to brain and meninges which can lead to rapidly fatal meningoencephalitis (2-10 days after infection) 3. Examples a. Absidia species Colony morphology – cottony texture, initially white becoming gray to gray-brown Microscopic – Internodal rhizoids (root-like hyphae) b. Mucor species Colony morphology – cottony texture, initially dirty-white becoming mousy-brown to gray Microscopic – No rhizoids CLS419 Clinical Microbiology II Rotation II Mycology Opportunistic Molds Page 35 c. Rhizopus species Most common zygomycete causing human disease Colony morphology – cottony texture, initially white becoming grey to brown Microscopic – Nodal rhizoids II. Septate opportunistic molds A. Dematiaceous hyphae 1. Hyphae and/or conidia are dark colored due to melanin-like pigment with septations 2. Colonies are dark gray, brown, or black, wooly, hairy, or velvety surface with smoky gray to jet black on reverse 3. Identification of genus/species is accomplished by microscopic examination a. Dark yellow-brown mycelium composed of uniform hyphae with parallel walls and distinct sepations 4. Example a. Alternaria species Colony morphology: shades of gray to brown to black, texture is downy to cottony Microscopic exam: short chains of large, smoothwalled, multicelled, macroconidia separated by both cross and longitudinal septa. Macroconidia are drumstick-shaped with elongated beak of one conidium butting against the rounded blunt end of the next. Pathogenesis: Chronic fungal sinusitis, can become systemic in immunosuppressed patients B. Hyaline hyphae 1. Hyphae and/or conidia are light colored with septations 2. Identification of genus/species is accomplished by microscopic examination 3. Examples a. Aspergillus species Second most isolated fungus in the clinical laboratory Causes Aspergillosis o Predisposed: debilitated and immunocompromised patients o Pathogenesis: inhale conidia develop sinusitis or bronchopulmonary disease can invade surrounding blood vessels becomes systemic (acute and fatal). It is very invasive and has a rapid process for spreading. o Can also be non-invasive in form of fungal ball and allergic fungal infections o Most susceptible include bone marrow and transplant recipients, hematologic malignancies, and immunocompromised (90% mortality rate) Identify by evaluating colony morphology (distinct outer margin with a white apron at the advancing area of growth) and microscopic arrangement of conidia on the phialides and vesicle to speciate Aspergillus fumigatus o Most common pathogenic Aspergillus species o Colony morphology: Initially white, eventually turning some shade of blue-green, green-gray, or green-brown; texture: granular to cottony o Microscopic exam: Single row of phialides on the top half of a club-shaped vesicle producing long chains of spherical conidia that tend to bend inward towards a center axis. Conidiophore is long, smooth-walled, and derives from a foot cell. CLS419 Clinical Microbiology II Rotation II Mycology Opportunistic Molds Page 36 Aspergillus niger o Can cause swimmer’s ear o Colony morphology: Initially white to yellow, then turning black (salt and pepper appearance) due to jetblack conidia, reverse is buff or yellow-gray (rules out dematiaceous), texture is cottony o Microscopic exam: Double row of phialides covering entire vesicle (radiate head). Single and short chains of conidia extend from phialides and when mature are roughened. Conidiophore is smooth-walled and derives from a foot cell. Aspergillus flavus o Colony morphology: some shade of yellow, yellowgreen, or yellow-brown; texture is granular to cottony o Microscopic exam: Single or double row of phialides cover entire vesicle radiating in all directions. Conidiophore is long with distinct roughening of wall proximal to junction of vesicle (when mature) and derives from a foot cell. b. Penicillium species Colony morphology: initially velvety and white, as matures becomes granular with various shades of green or bluegreen (yellow and yellow-brown can also be seen) Microscopic exam: conidiophores branch into metulae and then phialides (tips are blunt), from the tips of the phialides emerge chains of spherical conidia (“brush-like” or “skeleton fingers”) c. Fusarium species Most common cause of mycotic keratitis Colony morphology: Woolly or cottony, initially white and later becomes lavender, rose-red, or magenta on surface and reverse Microscopic exam: Macroconidia are 2-5 celled (separated by traverse septa), sickle-shaped (“canoes”) with a distinctive foot cell at the point of attachment d. Sepedonium species Must distinguish from Histoplasma capsulatum, a dimorphic fungus Colony morphology: Waxy and white colony rapidly becomes velvety with lemon color having a peripheral fringe, and white reverse. Microscopic exam: Single or clustered, thick-walled, smooth to rough macroconidia at the ends of simple or branched conidiophores CLS419 Clinical Microbiology II Rotation II Mycology Opportunistic Molds Page 37 Opportunistic Mold Case Studies Directions - Within CLS419 Clinical Microbiology II, go to Assignments, Clinical Rotation – Mycology, and then Opportunistic Mold Unit. Go to the corresponding case study to view the microscopic examples for each case. Click on an image to see an enlarged view. Answer the following short answer or single answer multiple choice questions for each case. Case 1 This organism was isolated from blood-tinged, nasal discharge of a diabetic, 65-year-old male. Growth was detected after 2 days of incubation at 25ºC on Sabouraud dextrose agar (SDA), with no growth on Mycosel agar. 1. Identify this fungus. 2. This class of fungus has __________ hyphae and an asexual reproductive structure called a ___________________. A. Aseptate/sparsely septate, sporangium B. Dematiaceous, septate C. Hyaline, rhizoid D. Septate, phialide 3. Macroscopically, this fungus’ colony is described as: A. Rapidly growing, flat, velvety B. Rapidly growing, wooly to cottony C. Slow growing, yeast-like D. Slow growing, granular to powdery 4. This class of fungi is the causative agent of ________________which is associated with infection of the __________________________. A. Aspergillosis, lower-respiratory tract presenting as allergy, colonization or systemic infections B. Chromoblastomycosis, upper-respiratory tract which may become systemic C. Dermatophytosis; hair, skin and nails D. Zygomycosis, nasal sinuses spreading to the eyes and brain via blood vessels Case 2 This fungus was isolated from the lung of a 35-year-old female lymphoma patient. Growth was detected after 3 days of incubation at 25ºC on SDA, with no growth on Inhibitory mold agar. 1. Identify this fungus. 2. Microscopic characteristics of this fungus include: A. Dematiaceous septate hyphae, phialides radiate from vesicle B. Hyaline aseptate/sparsely septate hyphae, sporangiums C. Hyaline septate hyphae, macroconidia produce phialoconidia described as a “paint brush” D. Hyaline septate hyphae, phialides cover upper 2/3 of vesicle 3. Some species of this genus are the etiologic agents of: A. Aspergillosis, presenting as allergy, colonization or systemic infections B. Chromoblastomycosis, presenting as an upper-respiratory tract infection which may become systemic C. Dermatophytosis; an infection of hair, skin and nails D. Opportunistic, subcutaneous fungemia CLS419 Clinical Microbiology II Rotation II Mycology Opportunistic Molds – Case Studies & Study Questions Page 38 Case 3 This fungus was isolated from the sputum of a 35-year-old male. A brown colony was detected at 72 hours of incubation at 25ºC on SDA, with no growth on Mycosel agar. 1. Identify this fungus. 2. Microscopic characteristics of this fungus include: A. Dematiaceous aseptate/sparsely septate hyphae, chaining microconidia B. Dematiaceous septate hyphae, chaining macroconidia w/cross and longitudinal septa C. Hyaline septate hyphae, microconidia radiate from vesicle D. Hyaline septate hyphae; multicelled conidia 3. Clinically, this fungus is considered to be a/an: A. Contaminant, possible association with allergies and superficial mycosis B. Etiologic agent of subcutaneous mycosis C. Primary cause of upper-respiratory tract infections & mycotic keratitis D. Primary cause of upper-respiratory tract infections & swimmer’s ear Case 4 This organism was isolated from an inflamed cornea of a 14-year-old male contact lens wearer. Growth was detected on SDA on day 3 of incubation at 25ºC with no growth on Mycosel agar. 1. Identify this fungus. 2. Clinically, this fungus is considered to be a/an: A. Contaminant, non-pathogenic B. Contaminant, possible association with allergies and superficial mycosis C. Etiologic agent of subcutaneous mycosis D. Primary cause of mycotic keratitis & also fungemia w/disseminated infection in immunocompromised 3. A medical student submitted to the laboratory a Mycosel slant inoculated at bedside with corneal scrapings he had collected from a 20-year-old female inpatient. He indicated that the physician was trying to rule out mycotic keratitis. What is the next best step? A. Incubate the slant at 35 C for two weeks. B. Reject the culture as corneal scrapings are inappropriate specimens to culture C. Request another scraping be performed in order to inoculate a primary isolation media without cycloheximide D. Request another scraping be performed in order to inoculate Lowenstein-Jensen and ReganLowe media Case 5 This organism was isolated from the sputum of a 50-year-old female who has smoked an average of 1/2 to 1 pack of cigarettes per day for 25 years. Growth was detected on SDA on day 3 of incubation at 25ºC with no growth on SDA w/cycloheximide & antibiotics. 1. Identify the fungus. 2. Clinically, this fungus is considered to be a/an: A. Contaminant, rarely an opportunistic pathogen B. Etiologic agent of subcutaneous mycosis C. Infectious agent often presenting as allergy, colonization or systemic infections D. Primary cause of upper and lower-respiratory tract infections CLS419 Clinical Microbiology II Rotation II Mycology Opportunistic Molds – Case Studies & Study Questions Page 39 Opportunistic Mold Study Questions 1. Match the drawing of a zygomycete with the name of the structure. _____ Hyphae or Stolon _____ Rhizoid _____ Sporangium 2. Match the drawings of the zygomycete with their genus name. _____ Absidia _____ Mucor _____ Rhizopus A. B. C. 3. Which of the following possess conidia with vertical and horizontal cross-walls? a. Alternaria species b. Cladosporium species c. Fusarium species d. Sepedonium species 4. Key characteristic(s) of the opportunistic molds include: a. Frequent lab contaminants b. Rapid growers c. Grow at 25-30°C d. All of the above 5. A key characteristic about the colony morphology of the Zygomycetes is: a. Black pigmentation b. Granular texture c. Peppered appearance d. Lid lifters 6. A key characteristic about the colony morphology of Aspergillus niger is: a. White pigmentation b. Granular texture c. Peppered appearance d. Lid lifters 7. Which opportunistic mold can cause farmer’s lung (fungal ball), allergic reactions, sinusitis, and become invasive to affect multiple organ systems? a. Aspergillus fumigatus b. Aspergillus niger c. Fusarium species d. Rhizopus species 8. True or False: Opportunistic molds will grow on Mycosel agar. CLS419 Clinical Microbiology II Rotation II Mycology Opportunistic Molds – Case Studies & Study Questions Page 40 9. Complete the table: Mold Hyphae appearance (Septate / Sparsely septate) Hyphae color (Dematiaceous / Hyaline) Mucor species Rhizopus species Aspergillus species Alternaria species Penicillium species CLS419 Clinical Microbiology II Rotation II Mycology Opportunistic Molds – Case Studies & Study Questions Page 41 CLS419 – Clinical Microbiology II Mycology Manual University of Nebraska Medical Center Clinical Laboratory Science Program Section Five: Dermatophytes CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes Page 42 DERMATOPHYTES Objectives: Upon completion of this CLS 419 unit, the Clinical Laboratory Science student will: 1. Define the clinical term “tinea”. 2. Differentiate Trichophyton mentagrophytes and Trichophyton rubrum based on the urease and in vitro hair penetration reactions. 3. Correlate the clinical, epidemiological and laboratory findings, including macroscopic and microscopic morphology and growth rate associated with the following organisms: a. Microsporum canis b. Microsporum gypseum c. Microsporum audouinii d. Epidermophyton floccosum e. Trichophyton mentagrophytes f. Trichophyton rubrum CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes Page 43 DERMATOPHYTES I. Characteristics A. Epidemiology – worldwide distribution 1. Anthropophilic – found primarily in humans 2. Zoophilic – found primarily in animals such as cats and dogs (man easily infected) 3. Geophilic – found primarily in soil B. Clinical Significance 1. Causes Tinea (Latin for “worm” or “ringworm”), also referred to as dermatophytoses – infections that involve the superficial areas of the body, including the hair, skin and nails 2. Dermatophytes break down and utilize keratin as a source of nitrogen (but unable to penetrate the subcutaneous tissue) 3. Body areas affected a. Skin i. Tinea corporis (ringworm of the body) – any and all common dermatophytes may be involved in this type of infection ii. Tinea pedis (ringworm of the feet) – athlete’s foot iii. Tinea cruris (ringworm of the groin area) – jock itch b. Hair i. Tinea capitis (ringworm of hair and/or scalp) o Ectothrix hair invasion – chains of arthroconidia outside the hair shaft ii. Tinea barbae (ringworm of beard hair) o Ectothrix hair invasion – chains of arthroconidia outside the hair shaft iii. “Black dot” ringworm o Endothrix hair invasion – chains of arthroconidia inside the hair shaft iv. “Favic” ringworm o Endothrix hair invasion – hyphae rather than conidia invade hair shaft c. Nails i. Tinea unguium (ringworm of the nails) Dermatophyte Microsporum Trichophyton Epidermophyton Skin X X X Hair X X Nails X X C. Relatively rapid growing molds that can be distinguished by certain differences in colonial morphology and in the relative production of macroconidia and microconidia. In common practice, six species of dermatophytes cause more than 98% of human dermatophytoses. II. Laboratory Diagnosis A. Specimen collection 1. Hair Hair should be plucked, not cut, from the edge of the lesion. Choose hairs that fluoresce under a Wood's lamp or, if none fluoresce, choose broken or scaly ones. Place infected hair into Petri dish 2. Skin Skin should be washed well and then scraped from the margin of the lesion onto folded black paper Place skin scrapings into Petri dish CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes Page 44 3. Nails Nail scrapings are obtained from the nail bed or from infected areas after the outer layers are discarded Place scrapings of infected nails into Petri dish B. Direct examination of clinical material 1. 10% KOH preparation a. For hair, skin and nails b. Detect presence of fungal elements 2. Calcofluor white stain a. For hair, skin and nails b. Detect presence of fungal elements 3. Wood’s Lamp a. For hair only b. Positive – bright yellow-green fluorescence Microsporum canis Microsporum audouinii c. Negative – no fluorescence Microsporum gypseum Trichophyton species C. Culture of clinical material 1. Specimen processing a. Nails are scraped or minced into small pieces b. Hair is cut into short segments 2. Media a. Each specimen is divided between at least two types of culture media b. The use of antibiotics will inhibit the overgrowth of bacteria and incorporation of cycloheximide will prevent the overgrowth of the rapidly growing saprophytic fungi c. Brain heart infusion (BHI) or Sabouraud’s brain heart infusion agar General purpose fungal media d. Mycosel Good growth – clue that may have a dermatophyte 3. Growth requirements a. Generally 25-30°C Exception: Trichophyton verrucosum requires 35°C b. Ambient air c. Visible growth can occur as soon as 3-4 days, with mature growth between 1-3 weeks d. Cultures must be examined frequently for 4 weeks D. Identification 1. Growth rate – 1-3 weeks (medium rate) 2. Colony morphology 3. Microscopic morphology: Hyaline, septate hyphae, presence or absence of macroconidia and microconidia a. Scotch tape preparation and tease prep - quick way to identify at least to genus level b. Slide culture Use Potato dextrose and Cornmeal dextrose o Encourages sporulation o Enhances pigment production Incubate at least 7 days Able to get to the Genus level of ID; possibly species level Many labs will just report to the Genus level CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes Page 45 4. Physiologic tests a. Able to speciate the fungi b. Urea hydrolysis Incubate 2-3 days on Christensen’s Urea Agar Used to differentiate between Trichophyton rubrum (negative) and Trichophyton mentagrophytes (positive) c. Hair perforation test Sterile hair is incubated at 25ºC with mold for 10-14 days in moist chamber Observe hair microscopically for presence or absence of conical perforations of the hair shaft Used to differentiate between Trichophyton rubrum (negative) and Trichophyton mentagrophytes (positive) d. Growth on rice grain media Microsporum audouinii will not grow All other Microsporum species will grow e. Vitamin requirements Some Trichophyton species require vitamins (thiamine and inositol) to grow Trichophyton verrucosum and T. violaceum III. Etiologic agents A. Microsporum species 1. Clinical Significance a. Invades hair and skin only 2. Microsporum canis a. Colony morphology i. Growth at 3-5 days (rapid) ii. Flat with feathery edges; initially white and silky, later develops lemon-yellow pigment at periphery iii. Reverse: lemon yellow or yellow-brown b. Microscopic examination i. Macroconidia: echinulate (spiny surface), thick-walled, spindle-shaped, multicelled (3-15), tapering distal ends often pointed and slightly turned to one side at tip ii. Microconidia: rarely seen, small, hyaline, tear-drop or elliptical shape, borne laterally directly from hyphae c. Causes tinea capitis, tinea corporis, often from contact with dogs and cats i. Hair will fluoresce under Wood’s Lamp 3. Microsporum gypseum a. Colony morphology i. Growth at 3-5 days (rapid) ii. Flat, initially white but turning fawn-brown (cinnamon) to reddish-brown, granular as conidia are produced iii. Reverse: light tan b. Microscopic examination i. Macroconidia: moderately thick-walled, rough surface, elliptical, rounded tip, and multi-celled (up to 6) ii. Microconidia: few or absent c. Causes ectothrix tinea capitis i. Hair will NOT fluoresce under Wood’s Lamp CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes Page 46 4. Microsporum audouinii a. Colony morphology i. Growth at 2 weeks (slow) ii. Downy white to salmon-pink iii. Reverse: tan to salmon-pink b. Microscopic examination i. Sterile hyphae: terminal chlamydospores, Favic chandeliers, and pectinate bodies ii. Macroconidia: rarely seen – bizarre-shaped iii. Microconidia: rare or absent c. Causes gray-patch tinea capitis in children i. Hair will fluoresce under Wood’s Lamp B. Epidermophyton species 1. Clinical Significance a. Invades skin and nails only b. Causes tinea cruris, tinea unguium 2. Epidermophyton floccosum a. Colony morphology i. Growth at 3-5 days (rapid) ii. Flat, initially gray-white then develops khaki-green center that tends to be folded; periphery is yellow to yellow-tan with feathered edges; granular as conidia develop iii. Reverse: yellowish brown with observable folds b. Microscopic examination i. Macroconidia: abundant, large, smooth thin-walled, multi-celled (2-5), clavate (club-shaped), and borne singly or in clusters of 2-4 ii. Microconidia: absent C. Trichophyton species 1. Clinical Significance a. Invades hair, skin, and nails 2. Trichophyton mentagrophytes a. Colony morphology i. Growth at 3-10 days ii. Varies: granular and cottony varieties; cottony type initially white, then tan, granular type initially white or off-yellow, then tan/brown iii. Reverse: buff to reddish brown b. Microscopic examination i. Macroconidia: smooth, thin walls, cigar or pencil-shaped, and multi-celled (4-5); numerous or rare depending upon strain ii. Microconidia: many round to globe-like (may be tear-shaped) borne in loose grapelike clusters or laterally along hyphae, spiral hyphae in 30% of isolates c. Causes tinea corporis, tinea capitis, tinea barbae d. Urea hydrolysis: positive e. Hair perforation test: positive 3. Trichophyton rubrum a. Colony morphology i. Growth at 2 weeks ii. Varies from white downy to pink granular; rugal folds common iii. Reverse: yellow when young; however, wine red color commonly develops with age (thus named rubrum) CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes Page 47 b. Microscopic examination i. Macroconidia: usually absent, smooth, thin-walled, multi-celled, & pencil-shaped ii. Microconidia: usually teardrop, most commonly borne along sides of hyphae giving “birds on a fence” appearance c. Causes tinea corporis, tinea pedis, tinea cruris, tinea capitis d. Urea hydrolysis: negative e. Hair perforation test: negative CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes Page 48 Dermatophyte Case Studies Directions - Within CLS419 Clinical Microbiology II, go to Assignments, Clinical Rotation – Mycology, and then Dermatophyte Unit. Go to the corresponding case study to view the microscopic examples for each case. Click on an image to see an enlarged view. Answer the following short answer or single answer multiple choice questions for each case. Case 1 This fungus was isolated from scrapings of a thickened, discolored fingernail. Growth was detected at two weeks of incubation at 25ºC on both SDA & Mycosel agar. 1. Identify the fungus. 2. What direct exam procedure can be performed on a portion of the nail scrapings to preliminarily determine if fungal elements are present? A. Gram stain B. Iodine wet preparation C. KOH preparation D. Modified acid-fast stain 3. Clinically, this fungus is considered to be part of the _____________ group, which is able to infect: A. Dermatophyte; hair, skin and nails B. Microsporum, all tissue containing keratin C. Opportunistic, any type of tissue D. Subcutaneous, superficial and subcutaneous tissue Case 2 This fungus was isolated from a seven-year-old female's "ringworm-type" lesion. After a week of incubation at 25ºC, the organism grew on SDA & Mycosel agar exhibiting a reddish pigment on the reverse side of the agar. 1. Identify the fungus. A. Acremonium sp. B. Epidermophyton sp. C. Microsporum sp. D. Trichophyton sp. 2. What test(s) can be utilized to speciate this organism? A. Carbohydrate assimilation panel, phenol oxidase activity B. Cornmeal Tween 80 agar morphology, modified acid fast staining reaction C. Gomori-methenamine-silver nitrate and Periodic Acid-Schiff staining reactions D. In vitro hair penetration, urea hydrolysis &/or Trichophyton Agars Case 3 This fungus was isolated from the hair of a nine-year-old boy. The mold grew on both SAB & Mycosel agar exhibiting a flat, granular, light tan to cinnamon colony at 5 days of 25ºC incubation. 1. Identify this fungus. 2. This genus will infect: A. All tissue types B. Hair, skin and nails C. Hair and skin D. Skin and nails CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes – Case Studies & Study Questions Page 49 Case 4 This fungus was isolated from a small, circular skin lesion on the back of a 14-year-old boy. The mold grew on both primary fungal isolation media, as well as media containing cycloheximide at 5 days of 25ºC incubation. The colony was irregularly shaped with a bright yellow reverse. 1. Identify this fungus. CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes – Case Studies & Study Questions Page 50 Dermatophyte Study Questions 1. Match the dermatophytes with their microscopic identifying characteristics. Dermatophyte ____ Microsporum canis ____ Microsporum gypseum ____ Microsporum audouinii ____ Epidermophyton floccosum ____ Trichophyton mentagrophytes ____ Trichophyton rubrum Microscopic Characteristics a. Rare bizarre-shaped macroconidia and rare or absent microconidia b. Rare smooth, thin-walled, multi-celled, & pencilshaped macroconidia and many teardrop microconidia that line up singly along hyphae c. Many rough, thick-wall, multicelled macroconidia that are spindle-shaped with a curved pointed tip, and few or absent microconidia d. Rare thin smooth-walled, multicelled macroconidia that are pencil-shaped, and many hyaline, spherical or teardrop microconidia in grape-like clusters e. Large thin, smooth walls, multi-celled macroconidia that are club-shaped and cluster together from hyphae, and absent microconidia f. Many rough, moderately thick-wall, multicelled macroconidia that are elliptical with a rounded tip, and few or absent microconidia 2. In what ways can Trichophyton mentagrophytes and Trichophyton rubrum be differentiated from each other? a. Colony morphology b. Urease production c. Hair penetration test d. All of the above 3. What is the purpose of the KOH preparation when examining skin scrapings? 4. Check what types of infections each dermatophyte genus can cause: Dermatophyte Skin Hair Nails Microsporum Trichophyton Epidermophyton CLS419 Clinical Microbiology II Rotation II Mycology Dermatophytes – Case Studies & Study Questions Page 51 CLS419 – Clinical Microbiology II Mycology Manual University of Nebraska Medical Center Clinical Laboratory Science Program Section Six: Subcutaneous Fungi CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi Page 52 SUBCUTANEOUS FUNGI Objectives: Upon completion of this CLS 419 unit, the Clinical Laboratory Science student will: 1. Define the following terms: a. Chromoblastomycosis b. Mycetoma 1) Actinomycotic 2) Eumycotic c. Sulfur granules 2. Differentiate the three types of conidia formation seen with the etiologic agents of chromoblastomycosis: a. Phialophora b. Cladosporium c. Acrotheca 3. Differentiate between Nocardia, Streptomyces, Actinomyces and Mycobacterium species based on: a. Gram stain morphology b. Acid fast stain (modified) c. Oxygen requirements d. Growth in/on: 1) Non-inhibitory fungus media 2) Blood agar 3) Lowenstein-Jensen 4) Thioglycollate broth 4. Correlate the clinical, epidemiological and laboratory findings, including macroscopic and microscopic morphology, and growth associated with the following infections: a. Phialophora verrucosum 1) Chromoblastomycosis b. Cladophiliaophora carrionii 1) Chromoblastomycosis c. Fonsecaea species 1) Chromoblastomycosis d. Sporothrix schenckii 1) Sporotrichosis e. Acremonium species 1) Eumycotic mycetoma f. Actinomyces species 1) Actinomycotic mycetoma g. Nocardia species 1) Nocardiosis 5. Differentiate Sporothrix schenckii from the opportunist Acremonium species. CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi Page 53 SUBCUTANEOUS FUNGI I. Basic Characteristics A. Growth rate 1. Varies: 1-4 weeks (medium to slow rate) B. Identification 1. Colony morphology 2. Microscopic morphology – 3 groups a. Dematiaceous septate hyphae (majority, black molds) b. Hyaline septate hyphae c. Branching nocardioform bacteria C. Clinical Significance 1. Epidemiology a. Found in soil and on plants b. Most are saprophytic (nonpathogenic) 2. Pathogenesis a. Acquire by mechanical means – traumatic penetration of foreign objects such as splinters, thorns, and sticks into the deep layers of the skin b. Ability to elicit disease is extremely variable – depends upon: i. Type of tissue involved ii. Immune system of host iii. Amount of exposure c. Formation of a lesion at site of penetration i. Involvement of skin, subcutaneous tissue, fascia, tendons, muscles, and bone ii. RARELY: dissemination to visceral organs via lymphatic system II. Laboratory Diagnosis A. Specimen collection 1. Skin scrapings 2. Aspirated debris 3. Tissue biopsy 4. Pus/drainage from lesion 5. Sputum, BW B. Direct examination of clinical material 1. 10% KOH preparation a. Detect presence of fungal elements, budding yeast, sclerotic bodies, ascospores 2. Calcofluor white stain a. Detect presence of fungal elements 3. Histological stains a. Methenamine silver stain b. Fontana-Masson stain c. Hematoxylin-eosin stain 4. Gram stain a. Detect presence of fungal elements, budding yeast, branching GPR 5. Modified acid fast stain CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi Page 54 C. Culture of clinical material 1. Specimen processing a. Sulfur granules must be crushed before culturing b. Tissue grinding (when necessary) 2. Media a. Each specimen is divided between at least two types of culture media b. The use of antibiotics will inhibit the overgrowth of bacteria and incorporation of cycloheximide will prevent the overgrowth of the rapidly growing saprophytic fungi c. Sabouraud’s Dextrose Agar General purpose fungal media d. Inhibitory Mold Agar General purpose fungal media selective for fungi e. Mycosel Agar Subcutaneous molds may be inhibited by antibiotics in media 3. Growth requirements a. Generally 25-30ºC b. Ambient air c. Visible growth can occur as soon as 5-10 days, with mature growth between 2-4 weeks d. Cultures must be examined frequently for 6 weeks D. Identification 1. Colony morphology 2. Microscopic examination a. Scotch tape preparation and tease prep b. Slide culture III. Diseases and their etiologic agents A. Chromoblastomycosis 1. Etiologic agents (black molds) o Fonsecaea species o Phialophora verrucosum o Cladophialophora carrionii 2. Distribution o Most occur in tropical and subtropical regions of world o Occasional case in temperate regions including U.S. o Agricultural workers most prone to infection 3. Clinical disease o Chronic fungal infection acquired via traumatic inoculation o Primarily involves skin and subcutaneous tissue (of mainly feet and legs) o Develop papule at site of infection that slowly spreads to form warty or tumor-like lesions (cauliflower-like) o Brown sclerotic bodies, non-budding structures occurring singly or in clusters, seen in tissues is diagnostic for chromoblastomycosis o Secondary infection and ulceration may occur CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi Page 55 4. Conidial structures (types of sporulation) a. Acrotheca (rhinocladiella) type i. Conidial heads with sympodial arrangement of conidia, with primary conidia giving rise to secondary conidia (looks like test tube brush) b. Cladosporium type i. chains of dark-staining elliptical conidia that are branching. The conidia often show scars (dysjunctors) at points of attachment. Branched conidium-bearing cells appear like a shield due to having 3 scars (note arrow in diagram on next page) c. Phialophora type i. Flask-shaped phialides with collaret at tip (vase-like) ii. Conidia – oval, one-celled, occurring at the tips of phialides in balls (flowers in a vase) 5. Fonsecaea pedrosoi and Fonsecaea compacta a. Colony morphology i. Growth at 2-4 weeks ii. Colony is brownish black, gray black or jet black in color, texture downy iii. Reverse: similar to surface (often jet black) b. Microscopic examination i. Dematiaceous (brown) septate hyphae ii. Conidiophores cylindrical, slightly inflated at the tip iii. Polymorphous mold – produces several types of sporulation Acrotheca (rhinocladiella) type sporulation Cladosporium type sporulation Phialophora type sporulation 6. Phialophora verrucosum a. Colony morphology i. Growth at 2-4 weeks ii. Colony is dark gray, brown or black, velvety to wooly texture iii. Reverse: similar to surface (often jet black) b. Microscopic examination i. Hyaline to dematiaceous septate hyphae ii. Phialophora type sporulation only 7. Cladophialophora carrionii a. Colony morphology i. Growth at 1-4 weeks ii. Colony is dark olive brown to brownish-black, texture is velvety iii. Reverse: similar to surface (often jet black) b. Microscopic examination i. Dematiaceous septate hyphae ii. Cladosporium type sporulation only Microscopic exam: CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi Page 56 B. Mycetoma 1. Types and their etiologic agents a. Eumycotic (fungal) mycetoma White grain: Pseudallescheria boydii, Acremonium falciforme Black grain: Madurella mycetomatis, Exophiala jeanselmei b. Actinomycotic (bacterial) mycetoma Nocardia, Streptomyces, Actinomyces 2. Distribution a. Most occur in tropical and subtropical regions of world b. Infections in temperate regions do occur (including U.S.) 3. Clinical disease a. Chronic granulomatous infection b. Triad of symptoms Swelling (tumefactions) of subcutaneous tissue causing tumor-like deformities Multiple sinus tracts (fistula) that tunnel through subcutaneous tissue to surface Drainage contains sulfur granules (vary in color, contain polysaccharide material and mycelium) c. Slowly progresses to involve bone, muscle, or other contiguous tissue 4. Eumycotic (Fungal) Mycetoma etiologic agents a. Acremonium falciforme Colony morphology o Growth at 1-3 weeks o Colony is grayish brown becoming grayish-violet; texture is glabrous to lightly downy, sometimes powdery o Reverse: pale Microscopic examination o Hyaline septate hyphae o Phialides solitary long and narrow, typically with a septum at the base and a scarcely visible collaret at the apex o Conidia oblong to ovoid, unicellular, often accumulating in clusters at the apices of the phialides 5. Actinomycotic (Bacterial) Mycetoma etiological agents a. Nocardia species Colony morphology on routine agar (BAP, CHOC, SAB, BHI) o Aerobic growth at 2-3 days o Extremely variable Adherent Some isolates beta-hemolytic on BAP Wrinkled Often dry, chalky-white appearance to orange-tan pigment Crumbly Colony morphology on LJ agar o Aerobic growth at 2-7 days o Colony is orange and wrinkled Gram stain o GPR – beaded, branching, fine, delicate filaments with fragmentation Partially acid fast positive CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi Page 57 b. Streptomyces species Colony morphology on routine agar (BAP, CHOC, SAB, BHI) o Aerobic growth at 3-10 days o Variable Glabrous or waxy heaped colonies Morphology varies Gram stain o GPR – extensive branching with chains and spores o Does not fragment easily Acid fast negative c. Actinomyces species Colony morphology on AnaBAP o Anaerobic growth at 3-10 days o Most colonies are small, smooth, flat, convex, gray-white, and translucent with entire margins A. israelii & A. gerencseriae – white, opaque, may resemble a “molar tooth” A. odontolyticus – turns red after several days in ambient air and may be beta-hemolytic Gram stain o GPR – branching, beaded or banded, thin, filamentous Acid fast negative C. Sporotrichosis 1. Etiologic agents a. Sporothrix schenckii 2. Distribution a. Worldwide b. Found on living or dead vegetation c. Farmers, nursery workers, gardeners, florists, miners 3. Clinical disease a. Known as the “rose gardener’s” disease b. Chronic subcutaneous infection c. Primary lesion starts as a small, non-healing ulcer (on hand or finger) d. With time, nodular lesions of skin or subcutaneous tissue at point of contact develop e. Later, can involve lymphatic channels and lymph nodes draining the region f. Only rarely, can the disease disseminate (systemic) g. Also, a pulmonary infection may be seen 4. Sporothrix schenckii a. Cultivation of mold phase i. Media and growth requirements Sabouraud’s and Inhibitory Mold agars – good growth at 3-5 days Incubate at 25-30ºC in ambient air for up to 2-4 weeks ii. Colony morphology Whitish to black colony on surface and reverse Texture glabrous, moist CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi Page 58 iii. Microscopic morphology Hyaline, septate hyphae Conidiophores little differentiated from vegetative hyphae Flowerette arrangement: conidia hyaline to brown, ovoid, thin-walled, grouped in rosettes at the tip of the conidiophore. Conidia are attached to conidiophore by an individual, delicate, threadlike structure (denticle) Sleeve arrangement: brown conidia, ovoid or sometimes triangular, thick-walled, attached directly to the sides of hyphae Can be confused with Acremonium (no yeast phase) b. Cultivation of yeast phase i. Media and growth requirements Brain heart infusion agar supplemented with blood Incubate at 35ºC in ambient air for 1-5 days i. Colony morphology Cream to beige colony with creamy texture iii. Microscopic morphology Yeast ovoid, elongate or cigar-shaped, producing one or several buds CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi Page 59 Subcutaneous Fungi Case Studies Directions - Within CLS419 Clinical Microbiology II, go to Assignments, Clinical Rotation – Mycology, and then Subcutaneous Fungi Unit. Go to the corresponding case study to view the microscopic examples for each case. Click on an image to see an enlarged view. Answer the following short answer or single answer multiple choice questions for each case. Case 1 This organism was isolated from a 35-year-old female's arm lesion. The Gram stain is of growth obtained at 35ºC. The wet preparations are of growth obtained at 25ºC. 1. Identify this fungus. 2. A common way humans become infected with this organism is by having contact with: A. Cats and dogs B. Pigeons C. Poultry D. Rose bushes 3. Clinically, this organism is most associated with a lesion: A. Developing at the site of infection, spreading via the lymphatic system; may become systemic B. Developing as a result of systemic spread following a respiratory infection C. Remaining localized to the area of initial contact resulting in a single lesion D. Remaining localized to tissue that contains keratin Case 2 Shown are direct specimen stains of drainage from an edematous, foot wound from a 60-year-old farmer. 1. Based on the clinical and laboratory information, what genus would you suspect? A. Actinomyces sp. B. Aspergillus sp. C. Mycobacterium sp. D. Nocardia sp. CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi – Case Studies & Study Questions Page 60 Subcutaneous Fungi – Study Questions Matching: 1. Match each of the following types of sporulation with its description. Sporulation type ____ Cladosporium ____ Phialophora ____ Acrotheca Description a. Production of flask-shaped or urn-shaped phialides ranging from 4 to 7 um in length, terminating in a collarette from the neck of which tight clusters of hyaline conidia are formed. b. Short chains of conidia arise from short denticles that are attached laterally to the sides of conidiogenous cells, which are borne sympodially in circumferential arrangement. c. Hyphae are freely branching, forming long chains of darkstaining, elliptical conidia. A scar (dysjunctor) is formed where each conidium becomes detached 2. Match the fungi with their microscopic characteristics. Fungi ____ Sporothrix schenckii ____ Acremonium species Microscopic Characteristics a. Mold phase has delicate hyphae producing fruiting heads characterized by several tiny, elliptical conidia arranged in a daisy petal fashion at the tip of a delicate conidiophore. Yeast phase has elongated, cigar-shaped blastoconidia. b. Mold phase has septate hyphae with slender phialides tapering at the end and giving rise to a cluster of conidia. There is no yeast phase. 3. Match each of the following diseases with its description. Disease ____ Chromoblastomycosis ____ Eumycotic mycetomas ____ Actinomycotic mycetomas Description a. Caused by true fungi, with symptoms including swelling, sinus tracts and sulfur granules b. Caused by true fungi with symptoms including tumor-like lesions with sclerotic bodies found in the tissues c. Caused by a group of branching, gram-positive, filamentous bacteria, with symptoms including swelling, sinus tracts and sulfur granules Multiple Choice: 4. Which of the following fungi are able to produce all three types of sporulation (cladosporium, phialophora, and acrotheca)? a. Phialophora b. Cladophialophora c. Fonsecaea d. All of the above CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi – Case Studies & Study Questions Page 61 5. Differentiate between the following fungal-like or branching bacteria including gram stain morphology, growth requirements (media and atmosphere), and acid-fast reaction. Bacteria Gram stain Media of choice Atmospheric requirements Acid fast reaction Nocardia species Streptomyces species Actinomyces species Mycobacterium species CLS419 Clinical Microbiology II Rotation II Mycology Subcutaneous Fungi – Case Studies & Study Questions Page 62 CLS419 – Clinical Microbiology II Mycology Manual University of Nebraska Medical Center Clinical Laboratory Science Program Section Seven: Systemic Dimorphic Fungi CLS419 Clinical Microbiology II Rotation II Mycology Systemic Dimorphic Fungi Page 63 SYSTEMIC DIMORPHIC FUNGI Objectives: Upon completion of this CLS 419 unit, the Clinical Laboratory Science student will: 1. Explain the laboratory process of converting dimorphic fungi from mold to yeast. 2. Correlate the clinical, epidemiological and laboratory findings, including macroscopic and microscopic morphology at both room temperature and 370 F and growth rate, for the following organisms: a. Histoplasma capsulatum b. Blastomyces dermatitidis c. Coccidioides immitis d. Sporothrix schenkii 3. Differentiate Histoplasma capsulatum from the opportunist Sepedonium species. 4. Discuss the use of molecular diagnostics in the identification of dimorphic fungi. CLS419 Clinical Microbiology II Rotation II Mycology Systemic Dimorphic Fungi Page 64 Systemic Dimorphic Fungi I. Basic Characteristics A. Dimorphic – two morphological stages 1. Mycelial stage at 25-30ºC 2. Parasitic stage (yeast or spherule) in human host (35-37ºC) 3. Definitive diagnosis: must demonstrate both stages (prove dimorphism) B. Epidemiology 1. Found primarily in North America (except Paracoccidioides is in South America) 2. Soil, decaying vegetation, bird and bat droppings C. Clinical Significance 1. Man is incidental host 2. Pathogens 3. Acquire by inhalation and develop respiratory infection 4. Can then become systemic a. Involvement of internal organs including lymph nodes, bone, subcutaneous tissue and skin b. May be asymptomatic c. Immunocompromised and long-term corticosteroid therapy patients most prone 5. Diseases / Etiologic agents a. Histoplasmosis / Histoplasma capsulatum b. Blastomycosis / Blastomyces dermatitidis c. Coccidioidomycosis / Coccidioides immitis II. Histoplasmosis A. Etiologic agent 1. Histoplasma capsulatum a. Endemic in Missouri, Mississippi, and Ohio River deltas B. Pathogenesis 1. 95% of cases are asymptomatic 2. Infection begins in lung and eventually invades the reticuloendothelial system 3. Can disseminate to lymphatic tissue, liver, spleen, kidneys, meninges, and heart (esp. in immunocompromised patients) C. Laboratory Diagnosis 1. Specimens a. Sputum, blood, bone marrow b. Urine, oral lesion scraping, lymph node biopsy, liver, etc. 2. Direct detection methods a. Giemsa or Wright’s stains i. Look for small, round to oval yeast cells within mononuclear cells (intracellular) ii. Must distinguish from Leishmania and Toxoplasma b. Calcofluor white stain c. PAS, Methenamine silver stain, H&E stain on tissue sections i. Observe for intracellular yeast cells 3. Cultivation of mold phase a. Media and growth requirements i. Sabouraud’s and Inhibitory Mold agars – good growth at 2-4 weeks If many organisms present, may see growth at soon as 3-5 days ii. Mycosel agar – no growth iii. Incubate at 22°C in ambient air for up to 4-6 weeks CLS419 Clinical Microbiology II Rotation II Mycology Systemic Dimorphic Fungi Page 65 b. Colony morphology i. White colony becoming brownish on the surface and yellowish on reverse ii. Texture wooly to granular c. Microscopic morphology i. Hyaline, septate hyphae ii. Macroconidia are unicellular, hyaline, thick-walled, smooth or warty (tuberculate) iii. Microconidia are unicellular, hyaline, with wall smooth or rough iv. This is the diagnostic form v. Can be confused with Sepedonium species (does not have yeast phase) 4. Cultivation of yeast phase a. Media and growth requirements i. Blood enriched media such as BHI ii. Incubate at 35°C in ambient air for 2-4 weeks b. Colony morphology i. Creamy texture with cream color on surface and reverse c. Microscopic morphology i. Small budding yeast measuring 2-4 um in length 5. Serological testing a. Double immunodiffusion (exoantigen test) b. Complement fixation III. Blastomycosis A. Etiologic agent 1. Blastomyces dermatitidis a. Endemic in Mississippi and Ohio River basins B. Pathogenesis 1. Causes an acute or chronic suppurative and granulomatous infection 2. Infection begins in lung by inhaling conidia or hyphal elements 3. Can spread and involve lungs, long bones, soft tissue and skin C. Laboratory Diagnosis 1. Specimens a. Cutaneous lesions b. Sputum c. Biopsy of affected organ 2. Direct detection methods a. KOH and Calcofluor White preparation i. Look for large, spherical, refractile yeast that have a double-contoured wall and buds connected to the parent cell by a broad base ii. Size is 8-15 um 3. Cultivation of mold phase a. Media and growth requirements i. Sabouraud’s and Inhibitory Mold agars – good growth at 1-4 weeks ii. Mycosel agar – no growth iii. Incubate at 22°C in ambient air for up to 4-6 weeks b. Colony morphology i. White, tan, or brown colony on surface, reverse is pale to brownish ii. Texture cottony or glabrous CLS419 Clinical Microbiology II Rotation II Mycology Systemic Dimorphic Fungi Page 66 c. Microscopic morphology – nondescript i. Hyaline, septate hyphae ii. Conidiophores are short, unbranched iii. Conidia are borne on short lateral branches that are ovoid to dumbbell shaped 4. Cultivation of yeast phase a. Media and growth requirements i. Cottonseed conversion agar ii. Incubate at 35°C in ambient air for 1 week b. Colony morphology i. White to beige colony that is creamy, granular to verrucose in texture c. Microscopic morphology i. Yeast with refractile walls, budding on a broad base ii. This is the diagnostic form 5. Other test methods a. Serological testing i. Double immunodiffusion (exoantigen test) b. Nucleic acid amplification assay i. Replacing serological testing IV. Coccidioidomycosis (San Joaquin Valley Fever) A. Etiologic agent 1. Coccidioides immitis a. Endemic in San Joaquin Valley, CA; Maricopa and Pima counties of AZ, and southwestern TX B. Pathogenesis 1. 60% of infections are asymptomatic and have self-limited respiratory tract infections 2. Infection begins in lung by inhaling arthroconidia (very infectious – 10 conidia inhaled will infect) 3. Can disseminate (1%) with extension to visceral organs, meninges, bone, skin, lymph nodes, and subcutaneous tissue C. Laboratory Diagnosis 1. Specimens a. Sputum b. Biopsy of affected organ 2. Direct detection methods a. KOH preparation, Calcofluor white stain i. Look for nonbudding, thick-walled spherule, 30-60 μm in diameter, containing either granular material or numerous small nonbudding endospores ii. Will not see a yeast form b. PAS, Methenamine silver stain, H&E stain on tissue sections 3. Cultivation of mold phase a. BIOHAZARD to lab workers, use strict safety precautions when examining cultures (must do all work in biological safety hood, wear gown, gloves and mask, and seal all culture plates) b. Media and growth requirements i. Sabouraud’s, Mycosel and Inhibitory Mold agars – good growth at 3 days to 3 weeks ii. Blood agar – growth iii. Incubate at 22°C in ambient air for up to 4 weeks CLS419 Clinical Microbiology II Rotation II Mycology Systemic Dimorphic Fungi Page 67 c. Colony morphology i. Rapid growth ii. White to gray colonies (sometimes beige, pink, cinnamon, yellow or brown) on surface, reverse pale, sometimes orange, or pale to dark brown ii. Texture wooly to glabrous d. Microscopic morphology i. Hyaline, septate hyphae ii. Conidiophores absent iii. Arthroconidia unicellular, rectangular to barrel shaped, often somewhat wider in diameter than the hyphae, alternating with empty cells (disjunctors) e. Mold phase will grow at both 22°C and 35°C 4. Cultivation of spherule phase a. Not recommended i. Use of special media incubated at 42ºC ii. Experimentally infect lab animals and perform tissue biopsy 5. Other test methods a. Serological testing i. Double immunodiffusion (exoantigen test) b. Nucleic acid amplification assay CLS419 Clinical Microbiology II Rotation II Mycology Systemic Dimorphic Fungi Page 68 Systemic Dimorphic Fungi Case Studies Directions - Within CLS419 Clinical Microbiology II, go to Assignments, Clinical Rotation – Mycology, and then Systemic Dimorphic Fungi Unit. Go to the corresponding case study to view the microscopic examples for each case. Click on an image to see an enlarged view. Answer the following short answer or single answer multiple choice questions for each case. Case 1 This fungus was isolated from a left, lower-lobe lung biopsy from a 17-year-old woman. The woman started experiencing pulmonary symptoms in Chicago after living in Phoenix, Arizona for three years. A mature colony was noted on day 4 of incubation at 25ºC. 1. Identify this fungus. 2. What structures would you expect the histologic stains of this lung biopsy to reveal? A. Ascospores B. Broad-based, budding yeast C. Endosporulating spherule D. Small, single budding yeast Case 2 Shown is a Periodic-Acid-Schiff (PAS) stain of a lung biopsy from a 58-year-old male who complained of a chronic, productive cough. He smoked two to three packs of cigarettes a day for the last 35-40 years. Upon x-ray, a homogeneous mass was noted in his left lung. The wet preparations are of the organism growth after 12 days of 35ºC incubation. 1. Identify this fungus. 2. The microscopic morphology of this organism’s growth at 25C characteristically exhibits: A. Alternating arthroconidia B. Indistinctive septate hyphae with small, round or pear-shaped conidia on conidiophores C. Rosette-like clusters of microconidia around tapered conidiophore D. Tuberculate macroconidia w/clustered microconidia Case 3 Shown is a Gomori-methenamine silver stain of caseous, lung lesion material from a 20-year-old female. The wet preparations are from growth on Inhibitory mold agar after 16 days incubation at 25ºC. 1. Identify this fungus. 2. Clinically, this organism presents as a(an) A. Lesion developing at the site of infection, spreading via the lymphatic system; may become systemic B. Localized cutaneous lesion that rarely spreads to the respiratory tract C. Nonpathogenic contaminant D. Respiratory infection that may exhibit systemic spread CLS419 Clinical Microbiology II Mycology Rotation II Systemic Dimorphic Fungi – Case Studies & Study Questions Page 69 Systemic Dimorphic Fungi – Study Questions Five fungal species share the common characteristics of growing in a mold form at ambient (room) temperature and in a yeast form when incubated at 35°C. These “dimorphic” fungi also are obligate pathogens for humans with the potential for causing disseminated, deep-seated infections. They generally are slow growing when recovered from clinical specimens and can be identified either by recognizing the microscopic morphology of the mold form when recovered in cultures or by detecting the characteristic yeast or spherule forms in stained tissue sections. 1. Give a brief description of the microscopic features of both the mold and yeast forms of the following species of dimorphic fungi: Dimorphic fungi Mold form Yeast form Blastomyces dermatitidis Histoplasma capsulatum Coccidioides immitis 2. What culture criteria are used to determine if an unknown isolate might be suspected of being a dimorphic mold? a. Slow grower (2-4 weeks) b. Grows as mold at 22°C and converts to yeast form at 35°C c. Grows on media containing antifungal agents d. All of the above e. A and B only 3. For Histoplasmosis, Coccidioides and Blastomyces infections, the common body site where infection begins is: a. Bladder b. Brain c. Lungs d. Liver 4. Discuss three safety precautions that should be met when working with the mold forms of systemic pathogens. 5. Compare and contrast the colony and microscopic characteristics of Histoplasmosis capsulatum and Sepedonium species CLS419 Clinical Microbiology II Mycology Rotation II Systemic Dimorphic Fungi – Case Studies & Study Questions Page 70 CLS419 – Clinical Microbiology II Mycology Manual University of Nebraska Medical Center Clinical Laboratory Science Program Section Eight: Appendix CLS419 Clinical Microbiology II Rotation II Mycology Appendix Page 71 Mycology Procedures 10% KOH Preparation 1. Add a drop of 10% KOH to specimen on slide. Coverslip. Gentle heating may aid in dissolving debris If specimen is thick, it may take 15-30 minutes to dissolve 2. Observe under low light or with phase scope Calcofluor White Stain 1. Add drop of Calcofluor White stain to specimen on slide. Coverslip. 2. Allow to sit approximately 3 minutes. 3. Use a fluorescent scope and look for apple green fluorescence. Cornmeal Tween 80 Morphology 1. With loop, make one streak into the agar down the center of an area and 3 or 4 parallel cuts across the first ½ inch or 1 cm apart, holding the inoculating wire at about a 45º angle to dilute inoculum. 2. Incubate 24-72 hours at 30ºC 3. Place coverslip on surface of the agar, covering inoculation streaks 4. Remove petri dish lid and examine through the coverslip with the microscope using the 10x and 40x objectives. Look for the most characteristic morphology near the edge of the coverslip. Germ Tube 1. Emulsify small amount of yeast in tube containing 0.5-1.0 ml serum (rabbit, fetal calf, or human) 2. Incubate at 35ºC for 3 hours 3. Place one drop of suspension on a slide, coverslip, and examine microscopically (40x) for long tube-like projections (germ tubes) extending out form the yeast cells. 4. Do not confuse germ tube with pseudohyphae (constricted at point of attachment) Pseudohyphae Germ Tube Parallel sides Not necessarily parallel Non-septate May be septate No constriction at point of attachment Constricted at point of attachment (sausage shaped) India Ink Preparation 1. Make a .5 McFarland suspension of yeast in sterile saline 2. Place one drop of suspension with one drop of India ink (be careful with ink) on microscope slide. (Strive for a thin smear) 3. Coverslip (drain on paper towels if coverslip is “floating”). 4. Let sit (up to 10 minutes) to allow cells to settle 5. Observe microscopically using 10x and 40x objective with condenser adjusted for maximum light. Look for a clear capsule around yeast. CLS419 Clinical Microbiology II Rotation II Mycology Appendix Page 72 Urease 1. Streak slant using sterile loop (use LOTS of organism) 2. Incubate at 35ºC 3. Observe at 3 hours and at 24 hours. Scotch Tape Preparation 1. Lightly press transparent scotch tape to colony 2. Affix tape to slide that has a drop of lactophenol cotton blue stain on it 3. Observe under light microscope at 10x and 40x Slide Culture 1. Setup equipment and supplies: Petri dish, paper towel, sterile water, two sticks, two microscope slides, coverslips. Place slide on 2 sticks in Petri dish (gauze or paper towel under sticks moistened with sterile water) 2. Using sterile scalpel, cut square of Sab-dex agar or Potato Dextrose agar smaller than coverslip and place on slide. Two pieces of agar can be placed on the slide to provide duplicate cultures. 3. Inoculate all four SIDES of agar square with mold (use dissecting needles to pick up mold) 4. Place a coverslip on top of each agar square 5. Make sure paper towel (or filter paper) is WET with excess water in bottom of Petri dish 6. Tape plate and incubate at room temperature 3-5 days. 7. When good amount of growth is evident, remove coverslip and place on slide containing a drop of lactophenol cotton blue stain Do just one coverslip in case mold is not mature enough Coverslip can be sealed with fingernail polish 8. Observe for characteristic fungal structures under light microscope using 10x and 40x objectives. Tease Preparation 1. Transfer piece of colony to slide and tease apart with dissecting needles 2. Add lactophenol cotton blue stain and coverslip 3. Observe under light microscope at 10x and 40x CLS419 Clinical Microbiology II Rotation II Mycology Appendix Page 73 University of Nebraska Medical Center Clinical Laboratory Science Program CLS419 – Microbiology II Mycology Lab Worksheet Please document the Gram stain smears, LPAB preps, and other slides that you evaluate during your Lab Activities each day. This worksheet is for your use to keep track of what you need to look at each day and to have a record of what you saw to help you study. You may want to include drawings of fungi and any other information that is helpful to you. You will be tested over your objectives (these organisms are NOT the only ones on the exam). Slide boxes may differ in organisms, you may not have all slides present in your box or you may have additional organisms/slides to add to your list. This exercise is to gain experience with microscopy work in mycology. Slide ID Fungus seen (and other information) Colony morphology on SAB agar? Stain Type: Organism: Stain Type: Organism: Stain Type: Organism: Stain Type: Organism: Stain Type: Organism: CLS419 Clinical Microbiology II Rotation II Mycology Appendix Page 74 Slide ID Fungus seen (and other information) Colony morphology on SAB agar? Stain Type: Organism: Stain Type: Organism: Stain Type: Organism: Stain Type: Organism: Stain Type: Organism: Stain Type: Organism: Stain Type: Organism: CLS419 Clinical Microbiology II Rotation II Mycology Appendix Page 75 Mycology Tutor, Table of Contents Introduction Overview Mycology Taxonomy Safety Fungal Detection Direct Techniques India Ink Microscopic Procedure – 3 steps (videos) KOH Microscopic Procedure – 2 steps (videos) KOH/Calcofluor Gram Stain Gram-Weigert Stain Histologic Stains Isolation Techniques Isolation media Selective media Organism Identification Yeasts Macroscopic Background Color Shape Texture Differential Media Microscopic Wet Mount Microscopic Mycology Tutor, University of Washington Procedure – 4 steps (videos) Germ Tube Microscopic Procedure Germ tube formation (2 videos) Corn Meal Agar Microscopic Procedure – 2 steps (videos) Ascospore Stain Biochemicals Assimilation tests Automated instruments Enzymatic testing Further testing Molds Macroscopic Background Growth rates (video) Color Texture Differential tests Microscopic Background Stains Tease preparation Procedure – 4 steps (videos) Scotch tape preparation Procedure – 5 steps (videos) Slide Culture Procedure – 5 steps (videos) Hair perforation Conidiogenesis Background Blastoconidia (video) Annelloconidia (video) Phialoconidia (video) Poroconidia (video) Aleurioconidia (video) Chlamydoconidia (video) Sporangiospores (video) Disease Associations Superficial Mycoses Tinea versicolor Clinical presentation Direct exam Malassezia furfur Macroscopic Microscopic (video) Tinea nigra Clinical presentation Phaeoannellomyces werneckii Macroscopic Microscopic White piedra Clinical presentation Trichosporon beigelii Macroscopic Microscopic Dermatophytoses Clinical presentation Direct examination Epidermophyton floccosum Macroscopic Mycology Appendix Microscopic Microsporum canis Macroscopic Microscopic Trichophyton mentagrophytes Macroscopic Microscopic Trichophyton rubrum Macroscopic Microscopic Trichophyton tonsurans Macroscopic Microscopic Subcutaneous Mycoses Sporotrichosis Clinical presentation Sporothrix schenckii Macroscopic: room temp Microscopic: mold phase (video) Microscopic: yeast phase Chromoblastomycosis Clinical presentation Direct examination Cladophialophora carrionii Macroscopic Microscopic Fonsecaea species Macroscopic Microscopic (video) Phialophora verrucosa Macroscopic Microscopic (video) Page 76 Mycetomas Clinical presentation Pseudallescheria boydii Macroscopic Sexual stage Asexual stage Exophiala jeanselmei Macroscopic Microscopic (video) Filamentous bacteria Phaeohyphomycosis Clinical presentation Wangiella dermatidis Macroscopic Microscopic Cladophialophora bantiana Macroscopic Microscopic Exophiala spp. Macroscopic Microscopic Phialophora richardsiae Macroscopic Microscopic Systemic Mycoses Cryptococcosis Clinical presentation Direct examination Cryptococcus neoformans Macroscopic Microscopic Blastomycosis Clinical presentation Direct examination Blastomyces dermatitidis Mycology Tutor, University of Washington Macroscopic: room temp Microscopic: room temp Microscopic: 37 degrees Coccidioidomycosis Clinical presentation Direct examination Coccidioides immitis Macroscopic: room temp Microscopic Histoplasmosis Clinical presentation Histoplasma capsulatum Macroscopic: room temp Microscopic: room temp (video) Microscopic: 37 degrees Paracoccidioidomycosis Clinical presentation Paracoccidioides braziliensis Macroscopic: room temp Microscopic: room temp Microscopic: yeast phase (video) Opportunistic Fungi Overview Common Opportunists Candida albicans Macroscopic Direct examination Microscopic Aspergillus fumigatus Macroscopic Microscopic Animation (video) Aspergillus flavus Macroscopic Microscopic Animation (video) Rhizopus species Macroscopic Microscopic Mucor species Macroscopic Microscopic Pneumocystis carinii Less Common Opportunists Acremonium species Macroscopic Microscopic Animation (video) Alternaria species Macroscopic Microscopic Animation (video) Chrysosporium species Macroscopic Microscopic Chaetomium species Macroscopic Microscopic Curvularia species Macroscopic Microscopic Animation (video) Epicoccum species Macroscopic Microscopic Mycology Appendix Fusarium species Macroscopic Microscopic Paecilomyces species Macroscopic Microscopic Animation (video) Penicillium species Macroscopic Microscopic Animation (video) Phoma species Macroscopic Microscopic Pithomyces species Macroscopic Microscopic Scopulariopsis species Macroscopic Microscopic Ulocladium species Macroscopic Microscopic Animation (video) Exams Take Exam 1 Page 77