Outline Case History Case History MRI Spinal Cord Compression
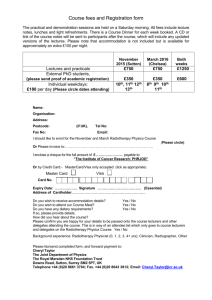
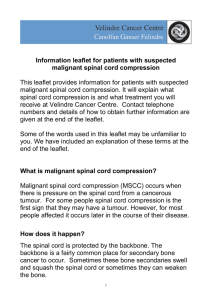
advertisement

CAGPO Conference – October 25, 2014 Outline Goal: To discuss the clinical features and management of 3 oncologic emergencies Radiotherapy for Oncologic Emergencies Dr. David Palma, MD, MSc, PhD Radiation Oncologist, London Health Sciences Centre Clinician-Scientist, Ontario Institute for Cancer Research 1. Spinal Cord Compression 2. Superior Vena Cava Obstruction 3. Brain Metastases Case History Case History 57 year old woman with a history of breast cancer presents with a 1-week history of band-like numbness across her abdomen X-rays show a ‘winking owl sign’ Over the past day, she reports bilateral leg weakness and is unable to ambulate Calls you for an opinion MRI Spinal Cord Compression MRI confirms spinal cord compression due to a metastasis to the thoracic spine The tip of the adult spinal cord usually lies at the L1 level, below this are the nerve roots of the cauda equina Up to 5% of patients with cancer will develop spinal cord compression Most commonly lung, breast, myeloma, prostate 1 Clinical Features Early recognition of cord compression is crucial for preservation of neurologic function Diagnosis is often delayed: • Median history of back pain is 2 months • Median history of neurologic symptoms is 14 days Back pain (up to 95%), may be radicular Motor weakness: progressive Sensory loss Bladder/bowel: usually urinary retention Investigations Pearl #1: Clinical Exam is Crucial Scenario #1- High Cord Comp Inspection • Dyspneic • Unsteady posture Tone • Increased in extremities Strength • Decreased in all groups in all limbs Reflexes • Hyperreflexic deep tendon reflexes Sensation • sensory level in upper thorax MRI is preferred CT does not clearly demonstrate the cord or epidural space, but can be helpful for obvious cases Scenario #2- Low Cord Comp Inspection Uncomfortable – unable to stand Tone/palpation • increased tone in legs • ?Decreased rectal tone Strength • Decreased in legs [test L3, L4, L5, S1 dermatomes] Reflexes • Hyperreflexic deep tendon reflexes in legs Sensation • Decreased in legs and peri-anal area [test L3, L4, L5, S1 dermatomes] Scenario #3- Cauda Equina • Inspection ?Fasciculations/wasting Tone/palpation • Decreased tone in legs • Decreased rectal tone • Palpable full bladder Strength • Decreased in legs [test L3, L4, L5, S1 dermatomes] Reflexes • Hyporeflexic deep tendon reflexes in legs – may be unilateral, specific e.g. ankle jerks Sensation • decreased in legs and peri-anal area [test L3, L4, L5, S1 dermatomes] • 2 Practical Approach Give 10 mg IV dexamethasone and 4 mg IV/PO q6h Would this patient be a radiation therapy and/or surgical candidate? • Yes-> call radiation oncology or neurosurgery on call to discuss case Potential treatment plan exists • -> call radiology to ask for urgent MRI Pearl #2: Start Steroids While Awaiting MRI Treatment The most important predictor of neurologic status after treatment is neurologic status before treatment Usually about 1/3 ambulatory at time of treatment Goals: • pain control • • avoid complications from local progression preserve neurologic function Pearl #3: Surgery if Possible RCT: Spinal Cord Compression • • • • • Patchell RCT: Primary Endpoint 101 patients with MESCC, nonchemosensitive One neurological sign or symptom Not paraplegic for >48h MESCC in one single area (can be contiguous) Life expectancy > 3 months Lancet 2005 Lancet 2005 3 Patchell RCT: Other Endpoints External Beam Radiotherapy • • • Usually a short course of radiotherapy (10 fractions or fewer), either after surgery or alone Most patients experience pain relief and maintain neurologic function Stereotactic radiotherapy is an option at some centres but not yet evaluated by rigorous trials Lancet 2005 Treatment Algorithm Prognosis Median survival is short: approximately 6 months Better in patients with: • Fewer metastases, no organ mets • • • • Slow progression of neurologic symptoms Radiosensitive tumors Ambulatory at treatment Long interval since original diagnosis Case 2 Imaging A 54 year-old man with a history of lung cancer resected 2 years ago, presents with a 5-day history of facial edema, bilateral arm edema, and shortness of breath CXR reveals a mediastinal mass Found to have tumor recurrence in the mediastinum, compressing and invading the superior vena cava 4 SVCO - Anatomy SVCO - Histology Non-malignant: Thrombosis, Infection, Fibrosis SVCO - Presentation SVCO - investigations Imaging: • Often abnormal chest-xray • CT usually sufficient for diagnosis Histology • 60% of patients have no history of cancer • Often bronchoscopy, mediastinoscopy, EBUS, VATS SVCO - Treatment Goals: • Improve symptoms, treat underlying disease SVCO is an oncologic emergency for some patients • Patients with stridor due to airway obstruction, severe laryngeal edema, or cerebral edema • In others, after assessment in ER/cancer centre, there is often time for a full diagnostic work-up Pearl #4: SVCO treatment is histology-based AND there is usually time to get histology 5 Grading Severity SVCO - Treatment Treatment depends on histology • Steroids – only helpful for lymphoma, or if edema Chemotherapy for sensitive tumors • • Lymphoma, SCLC, germ cell tumors Clinical response is usually rapid Radiation Therapy • 60-80% rate of resolution by 2 weeks Endovascular stents • For severe cases Algorithm Case 3 A 58-year old man presents with a 3-day history of headache, nausea, and right-sided weakness His medical history is remarkable for stage I NSCLC lung cancer treated 4 years prior with surgery Brain Metastases Overview Brain metastases occur in 10-30% of patients with cancer Comprise the majority of intracranial tumors As therapy for primary tumors improves and patients live longer, rates of brain metastasis are increasing Primary sites: • • • • • • Lung 50% Breast 15% Melanoma 10% Colon/rectum 5% Other primary 10% PUK 10% Some tumors almost never metastasize to brain: prostate, esophagus, oropharynx, and nonmelanoma skin cancer 6 Overview Treatment Most common site of metastasis is at grey/white junction • Some tumors have unique distribution Can present with nearly any neurological symptom • Headaches • Seizures • Altered mental status • Nausea/vomiting • Motor/sensory deficit Without treatment, survival is about 4 weeks. Goals: • Improve neurological status • Long-term tumor control Symptomatic: • Steroids to reduce edema • Anticonvulsants Don’t forget about issues around driving Management Symptomatic Treatment • Corticosteroids • • • • • reduce vasogenic edema by stabilising the BBB Usually administered QID, but the biological half-life is 3654 hours. BID or QD dosing is reasonable. Sx improvement in 6-24hrs, max effect in 3 days. 70% of patients will respond. Anti-convulsants • A 1999 meta-analysis concluded that there is no benefit with prophylactic use of anti-convulsants for brain metastases. Management Dependent upon: • Location, size and number of metastases • Patient age, performance status, neurological status Extent of extracranial disease Previous response of tumor to therapy • Modalities available: Surgery • • • • • Stereotactic Radiosurgery Radiotherapy Chemotherapy/hormone therapy (limited) Solitary Brain Metastases In the setting of a solitary brain metastasis, surgical resection or stereotactic radiation improves survival compared to just providing palliative whole brain radiotherapy For patients with 2-3 metastases, surgery or stereotactic radiation may improve quality of life and reduce the risk of neurological death Pearl #5: For a solitary brain met, ablation or resection improves survival 7 Multiple Brain Metastases Prognosis 70% of patients have multiple mets WBRT alone is standard (increases survival to 3-6 months) Surgery can be considered if one lesion is large and life-threatening Kaal et al, Lancet Neurol 2005:4:289 Treatment Algorithm Whole Brain Radiotherapy First published experience of WBRT in Cancer 1954 by Jen-Hung Chao. Most common treatment today is: 2 opposing lateral radiation beams Dose: 3000/10 (2000/5) Whole Brain Radiotherapy Hippocampal Sparing: the next generation? 50% of patients will improve in neurological functioning, 70-80% will improve or remain stable. Response rates for individual symptoms will vary: headache 80%; cranial nerve palsies much lower • Responses occur in 2-4 weeks. • Nevelsky JACMP 2013 8 The Bottom Line (on one slide) 1. Spinal cord compression requires a detailed neurologic examination to guide imaging, early initiation of steroids, and advocating for early MRI and assessment by neurosurgery and radiation oncology 2. For patients with SVCO, there is usually sufficient time to obtain a proper diagnosis and plan. Treatment depends on histology and severity of symptoms CAGPO Conference – October 25, 2014 Radiotherapy for Oncologic Emergencies Dr. David Palma, MD, MSc, PhD Radiation Oncologist, London Health Sciences Centre Clinician-Scientist, Ontario Institute for Cancer Research 3. Some patients with brain metastases are long-term survivors. Treatment decisions are based on number of metastases and overall RPA prognostic score. 9