Managing abnormal liver function tests
advertisement

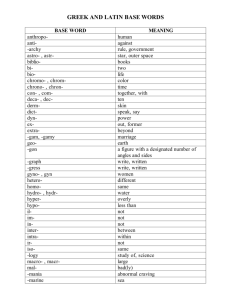
Forum Research Managing abnormal liver function tests A practice audit led to clear guidance on dealing with abnormal liver function tests in a primary care practice, writes Alan Barry Managing abnormal liver function tests results is an almost daily task for GPs around the country. Minor abnormalities in otherwise healthy patients are regularly discovered. How should we manage these abnormal blood test results? When should we investigate this group of patients and when should we refer them for a specialist opinion? My uncertainty prompted me to audit our surgery, and how we had been managing newly discovered asymptomatic patients with abnormal liver function tests. British Society of Gastroenterology guidelines On researching this area, I discovered the British Society of Gastroenterology (BSG) guidelines for managing such a group of patients. It is a document designed to help hospital physicians and GPs alike manage asymptomatic patients with abnormal liver function tests. The document does not include abnormalities of synthetic liver function tests, namely albumin and INR. It provides a suggested algorithm, which can be used as a guideline in practice. A number of interesting points were made in this document: • A majority of asymptomatic patients with abnormal liver function tests will have liver disease, and a proportion will have significant disease • Abnormal liver function tests in symptomatic and asymptomatic patients should be managed in a similar fashion • Any degree of abnormality should be considered for investigation, as even minor abnormalities can be associated with liver disease • Abnormalities should be investigated if persisting for more than six months. The audit With these guidelines in mind, I performed an audit in our practice. Any patient with abnormal liver function test results (bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma glutamyltransferase (gGT) Table 1 Algorithm for the management of abnormal LTFs Clinical situation Action suggested Management suggested Increased bilirubin Recheck with conjugated bilirubin, exclude haemolysis Reassure as likely Gilbert’s syndrome Increased gGT only Alcohol advice, consider medications Alcohol abstinence Reassure – NO further investigations Alkaline phosphatase and/or AST/ALT > two times upper limit of normal 1. Alcohol abstinence 2. Stop hepatotoxic drugs if possible 3. Advise weight loss if BMI > 25 4. Check gGT if only alkaline phosphatase abnormal 5. Recheck in three to six months and if persistently abnormal: →Liver screen: • Full history • HbsAg • HCVAb • Alpha1 anti-trypsin • Autoimmune profile • Ferritin and transferrin saturation • Copper and caeruloplasmin →Ultrasound Modified from BSG guidelines 2006 for the practice audit FORUM March 2011 43 Liverfunctions/Barry/JMC./NH2* 1 01/03/2011 10:11:45 or alkaline phosphatase), who did not have symptoms suggestive of liver disease, and who had not had an abnormal result in the past, was included. I collected data from July to November 2007. I analysed the charts and kept a record of what management plans were put in place to deal with these patients. Following a discussion with the other GPs in the practice, we attempted to implement an algorithm, based on the BSG guidelines, into our practice after the first arm of the audit had been completed. In our practice, the algorithm was modified slightly, such that any degree of abnormality was included, and not just those that were twice the upper limit of normal. With this new practice algorithm in mind, I subsequently collected data on suitable patients between March and June 2008. Again, only asymptomatic adults with ‘new’ abnormal liver function tests were included. Results The total number of asymptomatic patients with abnormal liver function tests between July and November 2007 was 25. When I reviewed the charts of these patients, nine had a management plan in keeping with the suggested algorithm by the BSG. Of the remaining 16 patients, 12 simply had isolated, abnormally raised bilirubin levels. After the attempted implementation into the practice of the suggested algorithm for managing these patients, 14 patients between March and June 2008 were identified with new abnormal liver function tests. Of these 14, 11 were managed in accordance with our modified algorithm. Guidance This was a small audit that will hopefully provide clear guidance on dealing with this common scenario in our practice. It is interesting to note how few ‘new’ abnormal liver function test results were seen during both periods. A large proportion of the results were isolated, mildly elevated bilirubin levels. These were not further assessed. Should we be keeping track of all of our patients with mildly elevated bilirubin levels and arranging follow-up? There were relatively few abnormal AST and ALT results. The management of asymptomatic patients with abnormal liver function tests, in our practice, was largely in accordance with the suggested BSG guidelines, both before and after the algorithm was implemented. I feel that the algorithm was easy to follow and allows GPs to manage this commonly encountered situation with some confidence, ensuring that liver disease is not missed and also that appropriate referrals to hepatology clinics are made. It is, however, only a suggested algorithm. There are a number of other recommendations on the management of abnormal liver function tests available. The BSG guidelines, as they were easy to read and had a suggested algorithm, were chosen and adopted for the purpose of this audit in our practice. Alan Barry is in practice in Blackrock, Co Dublin For the full BSG guidelines on abnormal LFTs see: www.bsg.org.uk/pdf_word_docs/ablft_draft05.doc Liverfunctions/Barry/JMC./NH2* 2 02/03/2011 09:04:46