Measuring change in limb volume to evaluate
advertisement
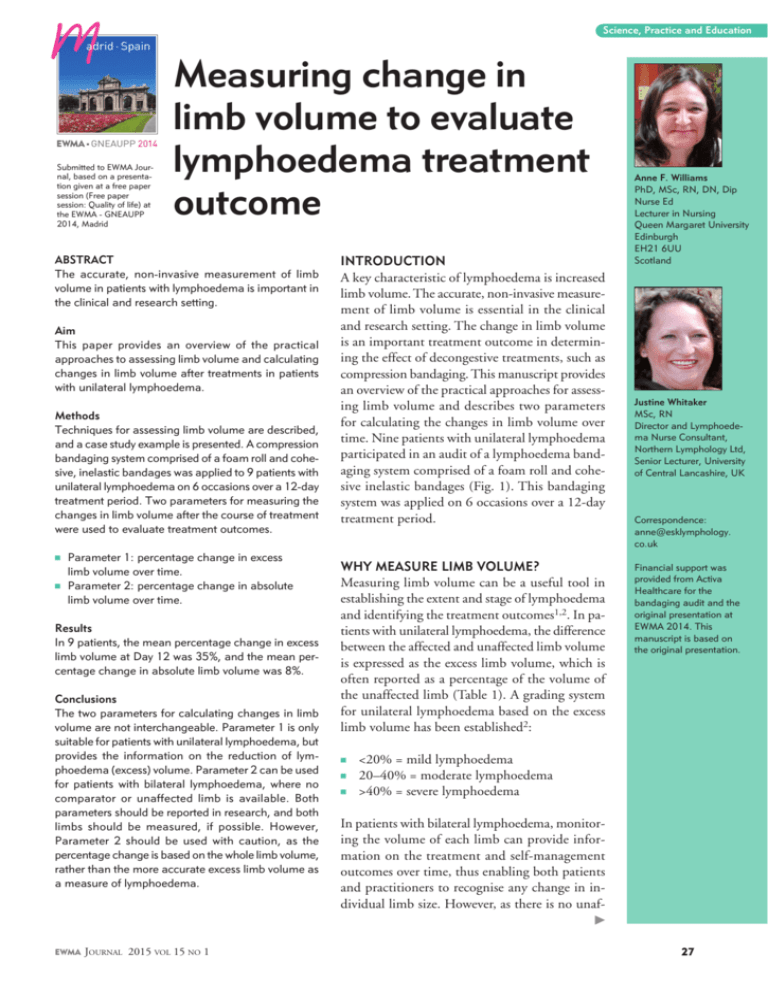
Science, Practice and Education adrid · Spain EWMA n GNEAUPP 2014 Submitted to EWMA Journal, based on a presentation given at a free paper session (Free paper session: Quality of life) at the EWMA - GNEAUPP 2014, Madrid Measuring change in limb volume to evaluate lymphoedema treatment outcome ABSTRACT The accurate, non-invasive measurement of limb volume in patients with lymphoedema is important in the clinical and research setting. Aim This paper provides an overview of the practical approaches to assessing limb volume and calculating changes in limb volume after treatments in patients with unilateral lymphoedema. Methods Techniques for assessing limb volume are described, and a case study example is presented. A compression bandaging system comprised of a foam roll and cohesive, inelastic bandages was applied to 9 patients with unilateral lymphoedema on 6 occasions over a 12-day treatment period. Two parameters for measuring the changes in limb volume after the course of treatment were used to evaluate treatment outcomes. n Parameter 1: percentage change in excess limb volume over time. n Parameter 2: percentage change in absolute limb volume over time. Results In 9 patients, the mean percentage change in excess limb volume at Day 12 was 35%, and the mean percentage change in absolute limb volume was 8%. Conclusions The two parameters for calculating changes in limb volume are not interchangeable. Parameter 1 is only suitable for patients with unilateral lymphoedema, but provides the information on the reduction of lymphoedema (excess) volume. Parameter 2 can be used for patients with bilateral lymphoedema, where no comparator or unaffected limb is available. Both parameters should be reported in research, and both limbs should be measured, if possible. However, Parameter 2 should be used with caution, as the percentage change is based on the whole limb volume, rather than the more accurate excess limb volume as a measure of lymphoedema. INTRODUCTION A key characteristic of lymphoedema is increased limb volume. The accurate, non-invasive measurement of limb volume is essential in the clinical and research setting. The change in limb volume is an important treatment outcome in determining the effect of decongestive treatments, such as compression bandaging. This manuscript provides an overview of the practical approaches for assessing limb volume and describes two parameters for calculating the changes in limb volume over time. Nine patients with unilateral lymphoedema participated in an audit of a lymphoedema bandaging system comprised of a foam roll and cohesive inelastic bandages (Fig. 1). This bandaging system was applied on 6 occasions over a 12-day treatment period. WHY MEASURE LIMB VOLUME? Measuring limb volume can be a useful tool in establishing the extent and stage of lymphoedema and identifying the treatment outcomes1,2. In patients with unilateral lymphoedema, the difference between the affected and unaffected limb volume is expressed as the excess limb volume, which is often reported as a percentage of the volume of the unaffected limb (Table 1). A grading system for unilateral lymphoedema based on the excess limb volume has been established2: Anne F. Williams PhD, MSc, RN, DN, Dip Nurse Ed Lecturer in Nursing Queen Margaret University Edinburgh EH21 6UU Scotland Justine Whitaker MSc, RN Director and Lymphoedema Nurse Consultant, Northern Lymphology Ltd, Senior Lecturer, University of Central Lancashire, UK Correspondence: anne@esklymphology. co.uk Financial support was provided from Activa Healthcare for the bandaging audit and the original presentation at EWMA 2014. This manuscript is based on the original presentation. n <20% = mild lymphoedema n 20–40% = moderate lymphoedema n >40% = severe lymphoedema In patients with bilateral lymphoedema, monitoring the volume of each limb can provide information on the treatment and self-management outcomes over time, thus enabling both patients and practitioners to recognise any change in individual limb size. However, as there is no unaf EWMA Journal 2015 vol 15 no 1 27 Figure 1: Application of the bandaging system, which was comprised of the spiral application of a foam roll* and the figure-of-eight application of the cohesive, inelastic bandages** * Rosidal Soft, Lohmann & Rauscher, Rengsdorf, Germany ** Actico, Activa Healthcare, Staffordshire, United Kingdom fected control limb, the actual (excess) volume of lymphoedema cannot be accurately established in someone with bilateral swelling. Similarly, no fully validated and reliable method exists for establishing the lymphoedema volume in patients with swelling in the head, neck, genitalia, and trunk2. TECHNIQUES FOR MEASURING LIMB VOLUME Various techniques for measuring limb volume have been reported in the literature. n Tape measure n Water displacement n Perometer TAPE MEASURE This is the most practical and portable technique in the therapeutic setting. Most commonly, the limb is marked and measured at 4-cm intervals1. Circumferential measurements are recorded (Table 1), and measurements can be compared over time for each point, thereby 28 Table 1: Recording circumferential measurements in Patient A (a woman with lower limb lymphoedema). The cylinder equation is used. Before treatment After treatment Right limb Left limb Right limb Left limb affected unaffected (cm) affected (cm) unaffected (cm) (cm) DISTAL 21.7 29.0 21.4 25.5 24.0 33.1 23.6 28.5 28.4 38.7 28.1 32.6 33.4 42.2 33.3 38.6 35.5 35.9 43.6 37.5 36.0 44.0 35.8 40.0 35.2 43.1 35.0 39.5 34.0 40.3 37.6 33.7 34.3 41.0 34.0 38.4 Distal limb volume0 2,904 4,524 2,856 3,651 (ml)0 Excess volume (ml)0 1,620 795 % excess0 56% 28% PROXIMAL 38.5 44.0 38.8 41.5 41.2 46.3 41.5 44.1 44.0 49.8 43.2 45.5 48.0 52.0 48.0 47.0 51.9 51.9 51.5 51.6 53.0 57.0 53.2 56.6 55.5 57.9 56.5 57.7 57.5 59.8 57.9 60.2 Proximal limb0 6,145 7,045 6,182 6,609 volume (ml)0 Excess volume (ml)0 899 427 % excess0 15% 7% Total limb volume0 (ml)0 Excess volume (ml)0 % excess0 9,050 11,569 9,038 10,260 2,519 28% - 1,222 14% - EWMA Journal 2015 vol 15 no 1 2 Science, Practice and Education Table 2: Two equations for calculating limb volume Volume of a cylinder: the limb is viewed as a series of cylinder-shaped segments. Volume of each segment = C²/π C is the circumference at the midpoint of a segment with a length of 4 cm. Therefore, the starting point for the first measurement is 2 cm above the wrist or ankle. Total limb volume is determined by the sum of the segment volumes. Volume of a truncated cone: the limb is viewed as a series of truncated cone or frustrum-shaped segments. Volume of each segment = L/12π (C1² + C1 C2 + C2²) C1 and C2 are the circumferences at either end of a segment length (L). The starting point for the measurement is at the wrist or ankle, which represents the first point of the distal truncated cone. Total limb volume is determined by the sum of the segment volumes. Table 3: Limb volume calculations before treatment in Patient A Total limb volume The calculation of total limb volume (ml): Right leg: 9,050 Left leg: 11,569 Excess limb volume comparing affected and unaffected limbs The difference between the limb volume of the affected and unaffected limbs in a patient with unilateral lymphoedema (ml): 11,569 – 9,050 = 2,519 Percentage difference in excess volume The excess limb volume is expressed as a percentage of the unaffected limb volume. This 3 indicates how much larger the affected limb is compared to the unaffected limb. 2,519 x 100 = 28% 9,050 Volume of different segments of the limb The limb is divided into the distal and proximal segments, and the total volume, excess volume, and percentage excess volume are reported for each segment. This is particularly useful if the swelling is not evenly distributed (for example, below the knee only). Distal segment volumes (ml) Proximal segment volumes (ml) Affected distal segment: 4,524 Unaffected distal segment: 2,904 Excess volume of distal segment: 1,620 % excess volume of distal segment: 1,620 x 100 = 56% 2,904 Affected proximal segment: 7,045 Unaffected proximal segment: 6,145 Excess volume of proximal segment: 899 % excess volume of proximal segment: 899 x 100 = 15% 6,145 EWMA Journal 2015 vol 15 no 1 giving precise information on the distribution of swelling and changes in limb circumference. Any change in limb circumference may indicate an increased or reduced fluid volume. These changes may also be influenced by the alterations in muscle mass, fat tissue, and tissue fibrosis. As such, an unaffected limb should always be measured as the control, as symmetrical change can be expected in response to factors, including exercise and weight loss. Circumferential measurements can be entered into computer software programmes or pre-programmed calculators to calculate limb volume and, in unilateral swelling, excess limb volume. Most commonly, two formulae are used to calculate the volume (Table 2), although the limb is rarely shaped like a true cylinder or truncated cone (frustrum). The calculation of the limb volume, excess volume, and percentage excess volume can be established for the whole limb, distal segments, and proximal segments, thus providing specific information on the distribution of oedema within the limb (Table 1). In the example shown in Table 1, the excess volumes before treatment at the distal and proximal sections of the limbs are very different (56% and 15%, respectively). This indicates an uneven distribution of swelling, which is not evident in the whole limb volume excess figure of 28%. When the measurement method is precise and standardised, evidence indicates that circumferential methods are valid and reliable3,4,5 (Table 4). The actual limb volume achieved will depend on the size and shape of each limb segment and the method of calculation6-8. The formulae (cylinder or truncated 29 Table 4: Tips for achieving accuracy using the tape measure method • Consistent limb position • Consistent tape type, width, and tension: some practitioners use a pre-tensioned tape to standardise • Accurate and consistent marking of the starting and subsequent measurement points throughout the limb: for example, marking the starting point as a consistent distance from the base of the nail bed of the middle finger • Standardisation of the measurement as below and above the marked point • Consistent number of measurement points used • Measurements by the same operator at the same time each day Table 5: Using two outcome parameters to calculate changes in limb volume after treatment in Patient A Parameter 1: Parameter 2 Pre-treatment excess volume: 2,519 ml Pre-treatment absolute volume of the affected leg: 11,569 ml Post treatment excess volume: 1,222 ml Post-treatment absolute volume of the Change in excess volume: affected leg: 10,260 ml 2,519 – 1,222 = 1,297 ml % change in excess volume: 1,297 x 100 = 52% 2,519 Change in absolute volume of the affected leg: 11,596 – 10,260 = 1,336 ml % change in absolute volume: 1,336 x 100 = 15.5% 11,596 cone) must be used consistently and are not interchangeable5,7. The hand or foot is not included in the calculation of limb volume, although approaches to measuring the hand have been explored9. WATER DISPLACEMENT METHOD This method is often viewed as the gold standard2 and is mainly used in research. It relies on measuring the amount of water that is displaced from a container when the limb or part of the limb is submerged. This provides information on the volume of the whole limb, including the hand or foot, and can be used to accurately measure the hand or foot alone7. The total volume of each limb can be used to calculate the excess and percentage excess volume of the whole limb, hand, or foot. This is generally not practical for clinical use. Circumferential measurements have been shown to correlate well with water displacement3,5,10,11, although the reported volumes from water displacement are often slightly lower than those from the circumferential measurements4. Therefore, the methods are not interchangeable. 30 PEROMETER METHOD (OPTOELECTRONIC PLETHYSMOGRAPHY) This device uses infra-red sensors to measure the limb7, 12. The limb is placed within a frame that does not touch the limb but is moved along the length of the limb. The method has some disadvantages, as it is expensive, is only suitable for the clinical setting, and relies on the patient being able to hold the limb steady in a specific position: for example, the arm is generally abducted. The machine provides various readings, including limb volume, and 5 produces a visual representation of the limb, which may be particularly useful for patient education. Tan et al.13 examined the agreement between a vertically orientated perometer and the tape measure method in volunteer legs. He concluded that the methods were reliable but not interchangeable, as the tape measure overestimated the limb volume in comparison to the Perometer. CALCULATIONS OF LIMB VOLUME Details of limb volume, excess limb volume, and percentage excess volume of the limb, as well as sections of the EWMA Journal 6 2015 vol 15 no 1 Science, Practice and Education Table 6: Use of Parameter 2 to calculate the percentage change in absolute limb volume Example 1: Example 2: Limb volume before treatment: 10,000 ml Limb volume before treatment: 16,000 ml Limb volume after treatment: 8,000 ml Limb volume after treatment: 14,000 ml Reduction in limb volume: 2,000 ml Reduction in limb volume: 2,000 ml Expressed as a percentage of the starting Expressed as a percentage of the starting treatment volume: treatment volume: 2,000 x 100 = 12.5% 2,000 x 100 = 20% 10,000 16,000 Table 7: Measuring limb volume change in nine patients with unilateral lymphoedema during a 12-day course of lymphoedema bandaging Parameter 1: Change in excess limb volume ID1 ID2 ID3 ID4 ID5 ID6 ID7 ID8 ID9 Mean Excess volume (ml) at Day 1 (pretreatment) Excess volume (ml) at Day 12 (posttreatment) Change in excess volume (ml) % change in excess volume 1,788 1,789 3,501 1,446 1,708 3,485 4,182 4,760 5,650 3,145 1,045 968 2,581 1,107 471 2,536 3,736 2,295 4,944 2,187 -743 -821 -920 -339 -1,237 -949 -446 -2,465 -706 -958 -42 -46 -26 -23 -72 -27 -11 -52 -12 -35 Parameter 2: Change in absolute volume of the affected limb Before After Change % treatments: treatments in limb change affected : affected volume in limb limb volume limb (ml) volume (ml) volume (ml) 8,709 11,995 11,021 10,396 8,631 9,135 13,376 13,399 17,039 11,522 7,966 11,174 10,101 10,057 7,394 8,483 12,966 10,931 16,222 10,588 limb such as the distal and proximal segments, can be calculated (Tables 1 and 3). Practitioners must understand the implications of any data which are obtained through software packages or calculators. This ensures that (1) circumferential measurements are taken at the correct intervals with a precise starting point, (2) data are correctly entered, and (3) any feedback that is given to patients or recorded for the clinic or research purposes is accurate. The formula for a cylinder requires the first circumferential measurement to be taken at 2 cm above the wrists or ankle (midpoint of the cylinder). The frustrum formula requires measurements at the end of each segment, so the first circumference is taken directly at the wrist or ankle. ESTABLISHING THE CHANGE IN LIMB VOLUME AFTER TREATMENT In a patient with unilateral lymphoedema, reporting excess volumes before and after treatments also enables a calculation of absolute and percentage change in excess limb volume in relation to the pre-treatment excess volume (Table 5). This is the most accurate representation EWMA Journal 2015 vol 15 no 1 -743 -821 -920 -339 -1,237 -652 -410 -2,468 -817 -934 -9 -7 -8 -3 -14 -7 -3 -18 -5 -8 of the actual change in the amount of lymphoedema in the affected limb and is particularly useful for research and audit purposes. When a patient has bilateral lymphoedema, the excess volume cannot be calculated. Instead, the reduction in absolute limb volume may be expressed as a percentage of the pre-treatment 7 total limb volume in each affected limb. However, this does not provide precise details of the lymphoedema volume or change in the lymphoedematous component of the limb. As shown in Table 5, two outcome parameters were used to calculate the changes in the affected limb of a patient with unilateral lymphoedema. The two methods produced very different results. Although Parameter 1 relied on the unaffected leg as a control, the result from Parameter8 2 was influenced by the initial volume of the limb.This is further illustrated in the examples given in Table 6 where two limbs have each reduced by 2000mls, although the calculation of percentage change, based on the initial limb volumes of 10,000mls and 16,000mls, are very different. Importantly, it is impossible to know how much of an initial limb volume is due to lymphoedema in a patient with bilateral swelling. 31 APPLICATION IN AN AUDIT Nine patients with unilateral lower limb lymphoedema participated in an audit of a bandaging system incorporating the spiral application of a foam roll and the figureof-eight application of cohesive, short-stretch bandages14. The patients were bandaged over 12 days with a total of 6 applications of the bandaging system (Fig. 1). The limb volume was calculated using the formula for a cylinder before and after the 12-day treatment course. Circumferential measurements were taken at 4-cm intervals along the affected and unaffected limb, starting 2 cm above the ankle. These data were entered into a spreadsheet to calculate the limb volume, excess volume, and % excess volume. The changes in limb volume in the 9 patients (Table 7) were expressed using two parameters. n Parameter 1: percentage change in excess limb volume over time. n Parameter 2: percentage change in absolute limb volume over time. RESULTS The results from the 9 patients with unilateral lymphoedema show a mean reduction in the excess limb volume of 35% (range 11–72%) when Parameter 1 was used (Table 7). This was similar to the mean reduction of excess volume of 33.5%, which was reported by Badger et al.15 in a study of 31 patients after 18 days of bandaging. Using Parameter 2, the mean reduction in the absolute limb volume in the 9 patients who took part in the audit was 8% (Table 7). CONCLUSIONS The two parameters for calculating the change in limb volume yielded different results and were not interchangeable. Our results suggest that Parameter 1 is only suitable for patients with unilateral lymphoedema, but provides information on the reduction in lymphoedema volume. Parameter 2 may be used for patients with bilateral lymphoedema, where no comparator (unaffected) limb is available. Both parameters should be reported in research, and both limbs should be measured. However, Parameter 2 should be used with caution, as the percentage reduction is based on the whole limb volume. The accurate representation of limb volume reduction cannot be achieved using Parameter 2, where the extent of lymphoedema is unknown, as a comparison with the unaffected limb is not possible. However, both parameters are useful in the clinical setting to monitor changes in the limb volume over time. To ensure accuracy, practitioners should use standardised, valid, and reliable approaches when assessing limb volume change. Limb volume measurements should be used in conjunction with other quality of life measures and patient-reported outcomes to provide a more holistic perspective on progress and change. Future work could involve the use of a larger dataset to examine the correlations between different approaches to quantifying limb volume reduction. REFERENCES 1. Lymphoedema Framework. Best Practice for the Management of Lymphoedema, International consensus. London: MEP Ltd.; 2006. Available at: http://ewma.org/fileadmin/user_upload/EWMA/ Wound_Guidelines/Lymphoedema_Framework_Best_ Practice_for_the_Management_of_Lymphoedema.pdf [Accessed 03.11.14]. Bilateral and Unilateral Limb Edema. Phys Ther 2007;87(10):1362-8. measurements for lymphoedema: implications for the SNAC trial. ANZ J Surg 2008;78(10):889-93. 6. Sitzia J. Volume measurement in lymphoedema treatment: examination of formulae. Eur J Cancer Care (Engl) 1995;4:11–6. 12. Adriaenssens N, Buyl R, Lievens P, Fontaine C, Lamote J. Comparative study between mobile infrared optoelectronic volumetry with a Perometer and two commonly used methods for the evaluation of arm volume in patients with breast cancer related lymphedema of the arm. Lymphology 2013;46(3):132-43. 2. International Society of Lymphology (ISL). The diagnosis and treatment of peripheral lymphoedema. Consensus document of the International Society of Lymphology. Lymphology 2013;42:1-11. 3. Sander AP, Hajer NM, Hemenway K, Miller AC. Upper-extremity volume measurements in women with lymphedema: a comparison of measurements obtained via water displacement with geometrically determined volume. Phys Ther 2002;82:1201-12. 4. Taylor R, Jayasinghe UW, Koelmeyer L, et al. Reliability and validity of arm volume measurements for assessment of lymphedema. Phys Ther 2006;86:205–14. 5. Mayrovitz HN, Macdonald J, Davey S, Olson K. & Washington E. Measurement Decisions for Clinical Assessment of Limb Volume Changes in Patients With 32 7. Stanton AWB, Badger C, Sitzia J. Non-invasive assessment of the lymphedematous limb. Lymphology 2000;33:122-35. 8. Katz-Leurer M, Bracha J. Test-retest reliability of arm volume measurement in women with breast cancer-related lymphoedema. J Lymphoedema 2012;7(2):8-13. 9. Borthwick Y, Paul L, Sneddon M, McAlpine L, Miller C. Reliability and validity of the figure-of-eight method of measuring hand size in patients with breast cancer-related lymphoedema. Eur J Cancer Care 2013;22:196-201. 10. Karges JR, Mark BE, Stikeleather SJ, Worrell,TW. Concurrent validity of upper extremity volume estimates: comparison of calculated volume derived from girth measurements and water displacement volume. Phys Ther 2003;83:134–14. 11. Tewari N, Gill PG, Bochner MA, Kollias J. Comparison of volume displacement versus circumferential arm 13. Tan C-W, Coutts F, Bulley C. Measurement of lower limb volume: Agreement between the vertically orientated perometer and a tape measure method. Physiotherapy 2013;99(3): 247-51. 14. Whitaker J, Williams A, Pope D, Charles H, Muldoon J. Sub-bandages pressures and comfort in a lymphoedema bandaging system with a foam layer and cohesive short stretch bandages. Poster at Harrogate Wound Care Conference, 2013. 15. Badger C, Peacock J, Mortimer P. A randomisedcontrolled parallel-group clinical trial comparing multi-layer bandaging followed by hosiery versus hosiery alone in the treatment of patients with lymphedema of the limb. Cancer 2000;7:2832-38. EWMA Journal 2015 vol 15 no 1