Red Eyes
advertisement
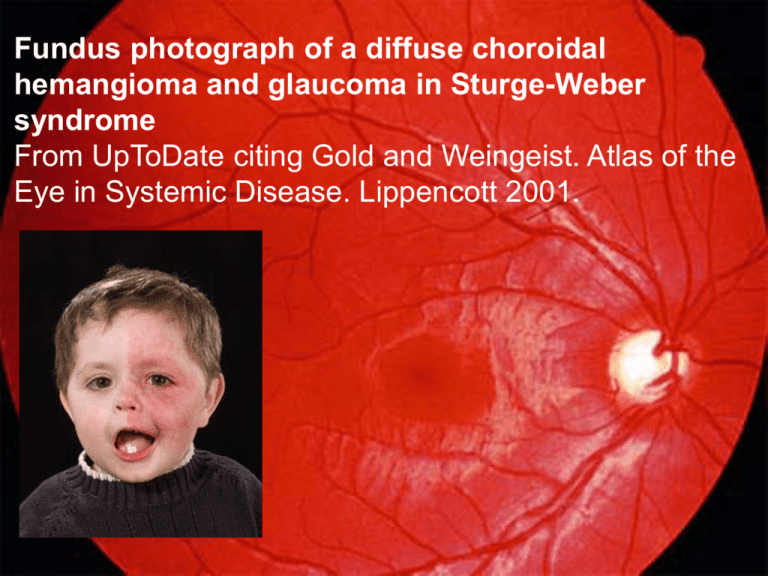
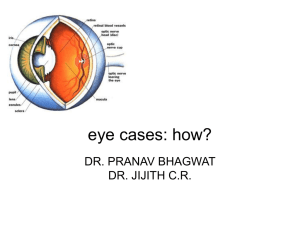
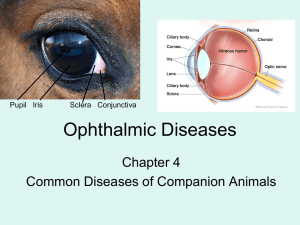
Fundus photograph of a diffuse choroidal hemangioma and glaucoma in Sturge-Weber syndrome From UpToDate citing Gold and Weingeist. Atlas of the Eye in Systemic Disease. Lippencott 2001. Lindsey Yeats, MD Identify red flag symptoms for red eyes Distinguish conditions that require emergent or urgent referral to ophthalmologist 5 yo F h/o eczema with 1 year of red eyes, worse over last month Pruritic, no pain, clear discharge, crusts in AM Worse when plays outside Sometimes it hurts Tried “everything” 6 mo and 4 mo ago had course of Polytrim and erythromycin Using J&J baby shampoo BID x months Tea bags Previously saw Dermatology PMH + mild intermittent asthma, h/o excema Meds: Albuterol prn, Visine ggt Otherwise unremarkable Exam: Afebrile, vitals stable HEENT: bilateral diffuse bulbar and palpebral conjunctival injection, string of mucoid discharge under flipped lid on L. PERRL. No photophobia. Moderate cobblestoning and nasal bogginess Vision 20/30 OU Lids/lashes Chalazion Blepharitis Hordeoleum/Stye Conjunctiva Conjunctivitis ▪ Bacterial ▪ Viral ▪ Allergic ▪ Nonspecific Episcleritis Subconjunctival hemorrhage Cornea Abrasion Foreign Body Infectious (keratitis) Anterior Chamber/Iris Iritis Hypopyon Hyphema Iris/Lens Angle closure Vision affected Foreign body sensation Photophobia Headache Trauma Contact lens wearer Persistent discharge Uncomfortable general appearance Photophobia Pain Pupil Reactivity Fixed at 4-5mm suggests angle closure glaucoma 1-2mm suggests iritis, keratitis, abrasion Examine cornea Area of whiteness or cloudiness suggests bacterial keratitis Look for foreign body Anterior Chamber Hypopyon – cells (usually white) in AC Hyphema – blood in AC for both emergent Ophtho referral (hours) Fundus – usually difficult to examine in pts where it would be helpful (ie glaucoma) Diffuse Palpebral and bulbar – suggests conjunctivitis Ciliary flush Suggests keratitis, iritis, glaucoma Most prominent at limbus and fades outward Hemorrhagic Could be subconjuntival hemorrhage Staining defect – suggests corneal abrasion Opacity - suggests keratitis Grayish opacity - think HSV keratitis Hypopyon – pus in the antierior chamber Refer same day Iritis - inflammation of anterior uveal tract Refer within 1 day Less likely to have FB sensation, and less severe photophobia Corneal abrasion – refer if large, concern for keratitis, unsure if removed FB, not improving 24 hrs, vision change Bacterial keratitis Same day referral FB, pain, photophobia, (& red eye, discharge) corneal opacity or infiltrate Staph, Pseudomonas, Strep Viral keratitis (HSV) Refer within 24 hrs Gray branching opacity with fluorescein Tx with antivirals Acyclovir 400mg 5 times a day Angle closure glaucoma – from increased IOP (vs primary or juvenile, which are more insidious) Usually secondary – angle anomalies (eg, Sturge-Weber syndrome, aniridia, anterior segment dysgenesis), ROP Aphakia (absence of lens) intraocular inflammation tumors trauma glucocorticoids Possible HA, photophobia, general distress, N/V Treatment within hours to prevent vision loss Conjunctivitis Blepharitis Foreign body that can be removed Stye (hordeoleum) Chalazion +- corneal abrasion Subconjunctival hemorrhage NEVER without recommendation from Ophthalmology Rebound vasodilation with Visine (tetrahydrozoline hydrochloride) Given pruritis and environmental triggers with h/o atopy, likely allergic conjunctivitis Tx with patanol. Stopped Visine Had improvement Same day referrals to ophthalmologists for: Concern for hypopyon, hyphema, keratitis/corneal ulcer, glaucoma Symptoms suggestive of need to refer include: Vision discrepancy, FB sensation, photophobia, headache, contact lens wearer Be wary of rebound inflammation with Visine No glucocorticoids Gigliotti F. Acute Conjunctivitis. Pediatr. Rev. 1995;16;203-207. Jacobs, Deborah et al. Evaluation of the red eye. Uptodate.com. Accessed 11/23/09. Leibowitz HM. The Red Eye. NEJM 2000;343(5):345-51. Olitsky, S and J Reynolds. Overview of glaucoma in infants and children. Accessed 11/23/09. Images: http://www.eyecaretyler.com/art/glaucoma.gif http://www.thefrogaffair.com/store/images/0720123.jpg http://www.jeffmann.net/NeuroGuidemaps/redeye-iritis.jpg http://k43.pbase.com/o4/45/520345/1/58148772.IMG_4720bw.jpg http://www.ich.ucl.ac.uk/gosh_families/information_sheets/sturge_w eber_syndrome/image1.jpg Images cont. http://biomed.science.ulster.ac.uk/vision/sites/vision/IMG/gif/figure_3. gif http://www.brightonvisioncenter.com/News/acanth_keratitis.jpg http://wpcontent.answers.com/wikipedia/commons/thumb/a/a0/Hypo pyon.jpg/190px-Hypopyon.jpg http://thm-a01.yimg.com/image/970ef64fe909cfa6 http://www.lowvision.com/wpcontent/uploads/direct/eye_anatomy_diagram_3.gif A 16-year-old boy presents with a very swollen, painful right knee. He is a soccer player, but there is no history of recent injury. During the interview, you notice the boy has injected conjunctivae. Of the following, further evaluation MOST likely will reveal A. alopecia areata B. Gottron papules C. Kayser-Fleischer rings D. malar rash E. urethritis A 14-year-old girl presents to your office with complaints of a red and "irritated" eye for the past 12 hours. She wears contact lenses, but has not worn them since the previous evening. Her pain and inflammation have continued to worsen despite removing the contact lenses. On physical examination, you note diffuse moderate injection of the bulbar conjunctiva of the left eye. Her extraocular motions and pupillary reflexes are normal. Results of funduscopic examination are normal. There is no discharge. Fluorescein examination reveals diffuse uptake of stain but no evidence of corneal abrasion. Of the following, the MOST appropriate next step in the management of this child is to A. apply a soft patch to the eye and refer to an ophthalmologist within 2 to 3 days B. arrange for urgent consultation with an ophthalmologist C. prescribe an ophthalmic antibiotic and ask her to return for re-examination in 2 to 3 days D. prescribe no antibiotics but ask her to return for re-examination in 2 to 3 days E. prescribe ophthalmic antihistamine drops You decide to treat for bacterial conjunctivitis: Tx options in a newborn ▪ Erythromycin ointment Child ▪ Erythromycin ointment ▪ Polytrim B drops if does ok with drops ▪ Ofloxacin if refractory or severe Adolescent ▪ Same + oral/IM tx of STIs Treat dry eyes Allergen avoidance Olopatadine (Patanol or Pataday) good first line prescription if OTC not working Antihistamine and mast-cell stabilizer A 2-week-old girl presents to the clinic with a history of drainage from her right eye. Her mother states that she noticed "the white part of her eye" turning red yesterday, but today the eye was redder and swollen with some drainage. The infant was born at term via normal spontaneous vaginal delivery without complications and is the mother's second child. The mother denies any illness or sexually transmitted disease during her pregnancy, but states that she did smoke one quarter pack of cigarettes per day. Physical examination reveals an afebrile, healthy-appearing female whose only abnormality involves her right eye. The upper and lower eyelids are slightly swollen, and her conjunctiva is erythematous, with a nonpurulent-appearing discharge. You suspect she has neonatal conjunctivitis due to Chlamydia trachomatis. Of the following, the MOST sensitive method for establishing the diagnosis is conjunctival culture detection of eosinophilia on a complete blood count Giemsa staining of conjunctival scrapings nucleic acid amplification test of conjunctival cells serum immunoglobulin G testing for C trachomatis Sorry, the preferred response is : nucleic acid amplification test of conjunctival cells 5 yo F h/o asthma with 2 days of R eye pain, mild erythema, rubbing, but not her usual itchiness. No vision changes. No discharge. Squinting on R, but no complaints of light. Helped with Patanol x 2 hr.