PDF Links - J Neurocrit Care
advertisement

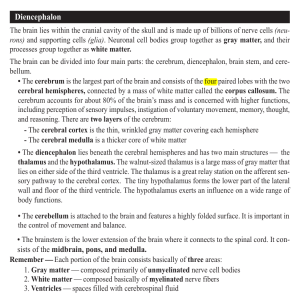
CASE REPORT online © ML Comm J Neurocrit Care 2009;2:56-59 ISSN 2005-0348 A Case of Cerebral Infarction Provoked by Carbon Monoxide Poisoning in Probable Unilateral Moyamoya Disease Sang-Moo Lee, MD, PhD, Heui-Chul Choi, MD, PhD and Jong-Hee Sohn, MD Department of Neurology, Hallym University College of Medicine, Chuncheon Sacred Heart Hospital, Chuncheon, Korea Background: Hemodynamic reserve is known to be reduced in moyamoya disease, which could account for increased susceptibility to cerebral ischemia. We report a case of acute cerebral infarction provoked by carbon monoxide (CO) poisoning in probable unilateral moyamoya disease. Case Report: A 26-year-old woman presented with mental changes followed by left hemiparesis after an exposure to CO. The initial serum carboxyhemoglobin level was 25.2%. She was alert but showed clinical signs of diffuse right hemispheric dysfunction. Brain MRI showed large territorial infarction in the right middle cerebral artery (MCA) and anterior cerebral artery (ACA). Brain MRA and conventional angiogram demonstrated complete occlusion of the proximal part of the right MCA and the ACA, which was suggestive of probable unilateral moyamoya disease. Conclusion: It was likely that cerebral hypoxia induced by CO poisonJ Neurocrit Care 2009;2:56-59 ing produced acute cerebral infarction in a hemodynamically compromised state. KEY WORDS: Moyamoya disease·Cerebral infarction·Carbon monoxide poisoning. Introduction Moyamoya disease (MMD) is a progressive cerebrovascular disease of unknown origin and characterized by progressive occlusion of the terminal portion of the internal carotid and proximal cerebral arteries with the development of typical extensive basal collateral network.1 Major clinical manifestations include repeated ischemic or hemorrhagic strokes and epileptic seizures. It is known that hemodynamic reserve is reduced in MMD, especially in ischemia related symptoms.2 This condition could account for increased potential for susceptibility to cerebral ischemia-hypoxia. Recently, we experienced a case of acute cerebral infarction in a patient with probable unilateral MMD that was provoked by carbon monoxide (CO) poisoning. Case A 26-year-old woman was admitted with a symptom of mental changes followed by left side weakness. She and her friend had suddenly experienced loss of consciousness while taking Address for correspondence: Sang-Moo Lee, MD, PhD Department of Neurology, Hallym University College of Medicine, Chuncheon Sacred Heart Hospital, 153 Gyo-dong, Chuncheon 200704, Korea Tel: +82-33-240-5746, Fax: +82-33-255-1338 E-mail: mooleemd@hallym.or.kr 56 Copyright ⓒ 2009 The Korean Neurocritical Care Society a shower with warm water in a temporary shower room. Although she became alert and oriented 3 hours later, she suffered weakness on the left side limbs and thus visited our hospital. But her friend recovered without neurologic symptoms. On initial physical examination, blood pressure was 140/ 80 mmHg, body temperature 36.1℃ and pulse rate 103/min. There were no remarkable findings on physical examination. On neurologic examination, she was alert, but left side hemineglect was noted on higher cortical function test. On cranial nerves function test, forced conjugate deviation of both eyes to right side, left facial palsy of central type, hypoalgesia on the left face and dysarthria were noted. Mild hemiparesis (Grade IV) and decreased senses of touch and pain were noted on the left side limbs. She had no known risk factors for stroke. Routine laboratory tests including all risk factors for young age stroke were normal. But the initial serum carboxyhemoglobin (COHb) level was 25.2%. Brain CT revealed loss of the graywhite matter interfaces and diffuse low density in the right middle cerebral artery (MCA) and anterior cerebral artery (ACA) territory, which was suggestive of acute cerebral infarction. Under the impression of carbon monoxide intoxication and acute right MCA and ACA territorial infarction, pure oxygen was supplied and intravenous rt-PA was started. Brain MRI (Fig. 1) showed findings consistent with the brain CT, and MRA showed occlusion of the right proximal MCA and the ACA. Conventional cerebral 4-vessel angiographic study demonstrated complete occlusion of the supraclinoid portion of the Cerebral Infarction by Carbon Monoxide in Moyamoya ▌SM Lee, et al. FIGURE 1. T2-weighted (A), T1-weighted (B), diffusion-weighted (C), and apparent diffusion coefficient (D) axial MRI show acute cerebral infarction mainly involving diffuse cerebral cortex in right middle cerebral arterial and anterior cerebral arterial territory. A B C D right ICA with extensive collateral vessels, which was suggestive of probable unilateral moyamoya disease (Fig. 2). Oral antiplatelet treatment was continued for 2 weeks after thrombolysis, and then she discharged with minimal higher cortical dysfunction. Discussion Carbon monoxide is a colorless, non-irritant, odorless, ubiquitous environmental gas, and CO intoxication is a serious phenomenon that can potentially lead to acute hypoxia and death. CO is produced in fires, by generators, car exhaust systems, heating system obstruction and endogenously as a neurotransmitter.3 Clinical symptoms of CO intoxication are headache, nausea, vomiting, tachypnea, lethargy, fatigue, syncope, seizure, confusion, unconsciousness, and death. Formation of COHb causes a decrease in oxyhemoglobin saturation leading to cellular hypoxia and death, giving rise to many of the symptoms of CO poisoning.4 This patient seemed to be exposed to CO produced by incomplete combustion of gas for water heating. Acute brain injury by CO toxicity may largely arise from hypoxia secondary to hypoxemia.4,5 Studies with mice, however, have shown that initial cerebral blood flow increases wi- thin minutes of CO exposure. Blood flow remains elevated until loss of consciousness, when transient cardiac compromise causes blood pressure to decrease.6 Also hypoxia is only seen in animals when COHb levels are very high (>70%) and the cardiovascular and cerebrovascular homeostatic response is overwhelmed. These findings suggest that brain hypoxia is probably not an initial feature of CO poisoning.3 There exists ample evidence that cerebral hemodynamics are disturbed locally in MMD.7,8 These hemodynamic disturbances include reduced cerebral blood flow, reduced cerebral perfusion pressure and prolonged circulation time.9,10 And hypercapnic reactivity, defined as the percent change in cerebral blood flow per mmHg change in pCO2, and cerebral hemodynamic reserve capacity to acetazolamide is also known to be reduced in MMD.2,11 Moreover the distribution of cerebral blood flow in MMD shows a dominant posterior distribution in contrast to dominant anterior distribution in normal control subjects.1,9 These hemodynamic changes could account for increased potential for susceptibility to cerebral ischemia and more frequent damage in anterior circulation than posterior circulation. Likewise, acute tissue hypoxia induced by COHb related hypoxemia could provoke acute cerebral infarction of anterior cerebral circulation in this patient. Because her friend 57 J Neurocrit Care ▌2009;2:56-59 A C B D had normal cerebral hemodynamics, she could recover without neurologic deficit. Many ischemic symptoms of the MMD are usually provoked by hyperventilation in relation to crying, exercise, eating hot food and in hot weather.12,13 Hyperventilation induced hypocapnia leading to vasoconstriction of small cerebral vessels is a possible explanation.13 But in spite of careful history taking, she had suffered no previous ischemia-related symptom before this event. And common infarction patterns in MMD are large hemispheric infarction predominantly in watershed zone, and subcortical infarction in the centrum semiovale and in the distal beds of the MCA and ACA.14 Considering predominant cortical infarction pattern and past medical history, cerebral infarction was likely to be caused by hypoxia provoked by CO poisoning. The most common site of involvement in CO poisoning is the globus pallidus. And the caudate nucleus, putamen, and thalamus are occasionally involved.15 Central nervous system neurons are vulnerable to hypoxic-ischemic insult because they have the highest oxygen and glucose demands. Acute and intense CO poisoning can lead to diffuse hypoxic-ischemic en- 58 FIGURE 2. Right carotid artery anteroposterior (A) and lateral (B) angiograms show occlusion at supraclinoid portion with basal and leptomeningeal collateral vessels. Left carotid artery anteroposterior (C) and lateral (D) angiograms disclose normal finding. cephalopathy mainly involving the gray matter.16 The involved region of infarction in this patient was distributed mainly in cerebral cortex. This pattern of involvement has been reported very rarely in acute CO poisoning.15 In acute CO intoxication, there is a predilection for the temporal lobe and hippocampus, which is different from this patient.15 Cerebral infarction mainly involving cerebral cortex suggests that underlying mechanism is hypoxia-ischemia resulting from poor hemodynamic reserve in this probable unilateral MMD patient. Conclusion This case is an acute cerebral infarction provoked by CO poisoning in a patient with probable unilateral MMD. We should consider that any conditions that produce acute hypoxemia-hypoxia could aggravate ischemic symptoms of MMD. Among these conditions, CO intoxication may be included. REFERENCES 1. Yonekawa Y, Kahn N. Moyamoya disease. Adv Neurol 2003;92:113-8. Cerebral Infarction by Carbon Monoxide in Moyamoya ▌SM Lee, et al. 2. Tatemichi TK, Prohovnik I, Mohr JP, Correll JW, Quest DO, Jarvis L. Reduced hypercapnic vasoreactivity in moyamoya disease. Neurology 1998;38:1575-81. 3. Gorman D, Drewry A, Huang YL, Sames C. The clinical toxicity of carbon monoxide. Toxicology 2003;187:25-38. 4. Berent AC, Todd J, Sergeeff J, Powell LL. Carbon monoxide toxicity: a case series. J Vet Emerg Crit Care 2005;15:128-35. 5. Piantadosi CA. Perspective: carbon monoxide poisoning. N Engl J Med 2002;347:1054-5. 6. Thom SR. Carbon monoxide-mediated brain lipid peroxidation in the rat. J Appl Physiol 1990;68:997-1003. 7. Nariai T, Senda M, Ishii K, Wakabayashi S, Yokota T, Toyama H, et al. Posthyperventilatory steal response in chronic cerebral hemodynamic stress: a positron emission tomography study. Stroke 1998;29: 1281-92. 8. Kuwabara Y, Ichiya Y, Sasaki M, Yoshida T, Masuda K, Ikezaki K, et al. Cerebral hemodynamics and metabolism in moyamoya disease-a positron emission tomography. Clin Neurol Neurosurg 1997;99 suppl 2:S74-8. 9. Okawa A, Yoshimoto T, Suzuki J, Sakurai Y. Cerebral blood flow in moyamoya disease. Part 1: Correlation with age and regional distribution. Acta Neurochir (Wien) 1990;105:30-4. 10.Taki W, Yonekawa Y, Kobayashi A, Ishikawa M, Kikuchi H, Nishizawa S, et al. Cerebral circulation and metabolism in adults’ moyamoya disease--PET study. Acta Neurochir (Wien) 1989;100:150-4. 11.Joo SP, Kim TS, Lee JH, Lee JK, Kim JH, Kim SH, et al. Moyamoya disease associated with Behcet’s disease. J Clin Neurosci 2006;13: 364-7. 12.Kim HY, Chung CS, Lee J, Han DH, Lee KH. Hyperventilation-induced limb shaking TIA in Moyamoya diaseae. Neurology 2003;60:137-9. 13.Spengos K, Tsivgoulis G, Toulas P, Vemmos K, Vassilopoulos D, Spengos M. Hyperventilation-enhanced chorea as a transient ischaemic phenomenon in a patient with moyamoya disease. Eur Neurol 2004; 51:172-5. 14.Bruno A, Yuh WT, Biller J, Adams HP Jr, Cornell SH. Magnetic resonance imaging in young adult with cerebral infarction due to moyamoya. Arch Neurol 1988;45:303-6. 15.O’Donnel P, Buxton PJ, Pitkin A, Jarvis LJ. The magnetic resonance imaging appearances of the brain in acute carbon monoxide poisoning. Clin Radiol 2000;55:273-80. 16.Lo CP, Chen SY, Lee KW, Chen WL, Chen CY, Hsueh CJ, et al. Brain injury after acute carbon monoxide poisoning: early and late complications. AJR Am J Roentgenol 2007;189:W205-11. 59