CASE 19
advertisement

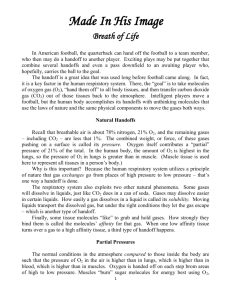
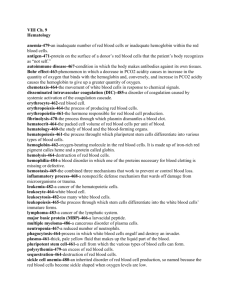
❖ CASE 19 A 23-year-old man with no medical problems is brought to the emergency center by family members who found him to be confused, nauseated, short of breath, and complaining of a headache. The patient was found in the basement of their home next to a furnace, where he was trying to stay warm on a cold winter day. On examination, the patient is lethargic and confused. His lips appear a bright pink. A urine drug screen is obtained and is negative. His serum carboxyhemoglobin level is elevated. The patient is diagnosed with carbon monoxide poisoning and is admitted to the hospital for further treatment. ◆ ◆ ◆ What is the mechanism by which carbon monoxide causes hypoxia? In which direction (right or left) would the hemoglobin–oxygen dissociation curve shift with fetal hemoglobin compared with adult hemoglobin? What is the most common way in which carbon dioxide is transported in venous blood? 154 CASE FILES: PHYSIOLOGY ANSWERS TO CASE 19: OXYGEN-CARBON DIOXIDE TRANSPORT Summary: A 23-year-old man has confusion, nausea, shortness of breath, and headache after being found near a furnace in the basement. The patient has clinical and laboratory findings consistent with carbon monoxide poisoning. ◆ Hypoxia with carbon monoxide: Decreased oxygen-binding capacity of hemoglobin. ◆ ◆ Fetal hemoglobin–oxygen dissociation curve: Shift to the left. Most common way carbon dioxide is transported in the blood: Bicarbonate (HCO3-). CLINICAL CORRELATION Carbon monoxide is a gas that is produced commonly by internal combustion engines, fossil-fuel home appliances (heaters, stoves, furnaces), and incomplete combustion of nearly all natural and synthetic products. Poisoning with carbon monoxide, if a person is exposed for a long period, can be fatal. Symptoms include headache, shortness of breath, confusion, impaired judgment, nausea, respiratory depression, coma, and even death. It is particularly a challenging problem because the gas is odorless and colorless; also, because the hemoglobin molecule is saturated, the patient is “pink” but hypoxemic. Carbon monoxide is inhaled through the lungs and binds to the oxygenbinding site of hemoglobin with a significantly higher affinity than does oxygen. The combination of carbon monoxide and hemoglobin makes carboxyhemoglobin, which can be measured in a patient’s blood. The elevation of the carboxyhemoglobin level may give some indication of the severity of the disease. After a person’s removal from the carbon monoxide exposure, the carbon monoxide slowly dissociates and is excreted through the lungs. Treatment of the poisoning includes removal from the carbon dioxide exposure and the administration of 100% oxygen (non-rebreather mask). At times patients need intubation (coma, seizures, or cardiovascular instability) or treatment with hyperbaric oxygen (extremely elevated carboxyhemoglobin levels). APPROACH TO OXYGEN-CARBON DIOXIDE TRANSPORT Objectives 1. 2. 3. Know about the structure and function of hemoglobin. Understand the hemoglobin–oxygen dissociation curves and the factors which may change them. Know about carbon dioxide transport in the blood. 155 CLINICAL CASES Definitions Oxygen carrying capacity of blood: The sum of the amount of dissolved O2 plus the amount of O2 bound to hemoglobin in the presence of 100% O2. Oxygen content of blood: The sum of the amount of dissolved O2 plus the amount of O2 bound to hemoglobin at any given PO2. Bohr effect: In the presence of CO2 hemoglobin has a lower binding affinity for O2. Because of the Bohr effect, increasing CO2 or lowering the pH of the blood decreases the O2 affinity of hemoglobin favoring O2 release. Haldane effect: Deoxygenation of hemoglobin increases its ability to bind CO2. DISCUSSION Oxygen Transport Metabolism consumes O2 and produces CO2. Gas exchange in the lungs occurs when blood passing through the pulmonary capillaries releases CO2 and takes up O2. The arterial concentrations of CO2 and O2 are in equilibrium with their concentrations in the alveolar compartment. The gas concentration in the blood is expressed as its partial pressure, and its content is determined by its partial pressure and its solubility in blood. The solubility of oxygen in aqueous solution is low, and the amount of O2 that can be dissolved in normal plasma, or the O2 content, at 37∞C is 0.3 mL/100 mL at a normal arterial partial pressure of 100 mm Hg. The O2 content of plasma is much too low to meet a person’s metabolic demands; however, hemoglobin greatly increases the amount of O2 the blood can carry. The O2-carrying capacity of blood is dependent on the hemoglobin concentration. At saturating oxygen levels, hemoglobin binds about 1.34 mL of O2 per gram of hemoglobin. Normal blood has about 15 g of hemoglobin per 100 mL; thus, at saturation, the amount of O2 bound to hemoglobin is 15 g Hb ¥ 1.34 mL O2/g Hb ¥ 100% saturation = 20.1 mL O2/100 mL blood The amount of O2 bound at saturation is the O2-binding capacity of hemoglobin. The normal arterial PO2 is about 100 mm Hg. At this partial pressure, hemoglobin is 97.5% saturated and the amount of O2 that is bound is 15 g Hb ¥ 1.34 mL O2/g Hb ¥ 97.5% saturation = 19.6 mL O2/100 mL blood The total amount of O2 in the blood is the sum of the dissolved O2 and the bound O2: O2dis = 0.3 mL/100 mL blood O2bound = 19.6 mL/100 mL blood O2content = 19.9 mL/100 mL blood 156 CASE FILES: PHYSIOLOGY The majority of O2 is transported in the blood bound to hemoglobin. Any factors that influence the amount of functional hemoglobin will influence O2 transport in the blood. Hemoglobin is the major blood protein constituent; it is contained within the red cells of the blood and is central to gas transport and maintenance of hydrogen ion homeostasis and acid–base balance. It is a tetrameric complex of two a subunits and two b subunits, each of which binds an O2 molecule. The binding of the first oxygen to hemoglobin causes a structural shift that favors the binding of additional oxygen molecules. This cooperativity yields a characteristic sigmoidal affinity curve for O2 binding. Several important physiologic parameters contribute to the binding affinity of hemoglobin for O2 and affect the shape of the curve. Variables such as temperature, pH, and CO2 alter the binding affinity for O2. The structural shift induced by O2 binding alters the ionization state of important amino acid residues, causing a shift in their H+ dissociation constant (pKa ). O2 binding results in a decreased affinity of hemoglobin for H+ and a release of H+ from the molecule. The reaction is readily reversible and is in equilibrium. Thus, not only does O2 binding or release cause a change in [H+], the H+ concentration influences O2 binding by hemoglobin. Although seemingly minor, the O2 binding affinity of hemoglobin is pH-dependent and is important to the overall physiologic function of hemoglobin. Also, hemoglobin contributes to H+ ion homeostasis by becoming a weaker acid (higher affinity for H+) upon O2 dissociation. This shift in the pKa is the basis of both the Haldane effect and the Bohr effect. Finally, hemoglobin also binds CO2 with the formation of carbamino groups. The binding is weak and readily reversible but has two important consequences: The binding of CO2 alters O2 affinity, and hemoglobin contributes to CO2 transport in the blood. An increase in H+ or PCO2 will shift the O2 dissociation curve to the right with a resultant decrease in the affinity for O2. This phenomenon is known as the Bohr effect. Another important regulator of the O2 binding affinity of hemoglobin is 2,3-diphosphoglycerate (DPG). DPG is produced by red cells and is increased during hypoxia. An increase in DPG shifts the affinity curve to the right, decreasing the affinity for O2 and favoring oxygen release in the tissues (See Figure 19-1). The effect of pH, PCO2, temperature, and 2,3-DPG on O2 binding to hemoglobin is central to gas transport by the blood. Figure 19-1 is the oxygenbinding curve of hemoglobin. Because of the steeply sigmoidal nature of the curve through much of the physiologic range, even slight changes in the binding affinity for O2 can cause large changes in the percent of O2 saturation at a given PO2. Thus increases in H+, CO2, temperature, or 2,3-DPG will cause O2 dissociation from hemoglobin. Conversely, a decrease in any of these factors will increase the affinity for O2 favoring its binding to hemoglobin. 157 CLINICAL CASES 100 100 98 97 N 90 Shift to the left: Hypothermia Hypocapnia Alkalosis ↓2,3 DPG 70 N 80 70 Shift to the right: Hyperthermia Hypercapnia Acidosis 2,3-DPG N 60 A 50 90 60 ↓ % Hemoglobin saturation 80 91 50 40 40 30 30 20 20 10 10 0 27 0 10 20 30 40 50 60 PO2 (mm Hg) 70 80 90 0 100 Figure 19-1. Oxygen dissociation curve with shifts based on various factors. Carbon Dioxide Transport The transport of CO2 by the blood occurs through several different mechanisms. CO2 has a higher solubility than does O2; therefore, a larger fraction is carried as dissolved CO2. More important, CO2 spontaneously reacts with water to form carbonic acid: CO2 + H2O Æ H2O CO3 Æ H+ + HCO3Carbonic acid dissociates to H+ and HCO3-. The enzyme carbonic anhydrase catalyzes this reaction and is contained in red cells. CO2 freely diffuses into the red cell and reacts with water to form H+ and HCO3−. The HCO3− is transported rapidly out of the red cell by the Cl−/ HCO3− exchanger in the red cell membrane. The H+ remains in the cell and is in part buffered by the hemoglobin. Physiologically, this arrangement works to advantage because the increase in H+ favors the dissociation of bound O2 (Bohr effect). At the same time, dissociation of O2 causes hemoglobin to become a weaker acid (higher affinity for H+), increasing the buffer capacity of hemoglobin. About twothirds of metabolically produced CO2 undergoes this reaction and is carried to the lungs as HCO3-. % O2 saturation 100 Alveolus 80 CO2 60 CO2↓ 40 H+↓ O2 20 0 0 20 40 60 80 100 120 PO2 (mm Hg) Cl– CO2 + H2O H+ + HCO3– H+ + HbO2 CO2 CO2 + HbO2 HHb + O2 O2 H+ + HbCO2 + O2 Pulmonary capillary 80 ↓ 60 CO2 40 H+ ↓ % O2 saturation 100 20 0 0 20 40 60 80 100 120 PO2 (mm Hg) CO2 + H2O CO2 Cl H+ + HCO3– H+ + HbO2 CO2 CO2 + HbO2 HHb + O2 O2 H+ + HbCO2 + O2 Pulmonary capillary Figure 19-2. Gas transport from actively metabolizing tissue and the lungs. Tissue production of CO2 in the peripheral capillary will cause CO2 to diffuse into the red cell. In the red cell, CO2 will react with H2O via the action of carbonic anhydrase to form H+ and HCO3−. The HCO3− is transported out of the cell in exchange for Cl−. Both CO2 and H+ will facilitate O2 release by causing a shift in the O2 dissociation curve of hemoglobin, lowering its O2 affinity. At the same time, O2 dissociation will increase the affinity of Hb for H+ and CO2. As the blood enters the pulmonary capillary, the arterial O2 will rise decreasing the affinity for CO2. CO2 will diffuse down its concentration gradient into the alveolus resulting in HCO3− reacting with H+ to form CO2. As H+ and CO2 fall, the O2 affinity of hemoglobin increases facilitating oxygenation. CLINICAL CASES 159 Hemoglobin also binds CO2 directly through the formation of carbamino groups on terminal amines. There is no cooperativity of CO2 binding, and the dissociation curve is much flatter over the normal physiologic range. The binding affinity for CO2 is dependent on the O2 concentration. Increasing O2 causes a shift to the right with a decrease in affinity for CO2. The effect is known as the Haldane effect. Physiologic Relevance Physiologically, the Bohr effect and the Haldane effect are important in the understanding of gas transport, O2 delivery to tissues, and H+ homeostasis (summarized in Figure 19-2). In metabolically active tissues, there is increased production of CO2, which freely diffuses into the red cell. In the red cell, twothirds of the CO2 is converted by carbonic anhydrase to H2CO3 which dissociates to H+ and HCO3-. The HCO3- is transported into the blood in exchange for Cl-. The elevation in CO2 and H+ will favor release of O2 from hemoglobin, facilitating O2 delivery to the tissue. The blood leaving the tissue will have elevated H+, CO2 and HCO3-. In the lungs, O2 diffuses into the pulmonary capillary and CO2 diffuses into the alveolar compartment. In the red cell, the increase in O2 drives the release of CO2 from the hemoglobin. The fall in CO2 reverses the reaction of HCO3- and H+ to form H2CO3 which is converted to CO2 and H2O. The fall in both H+ and CO2 increase the affinity for O2, favoring maximal saturation of the hemoglobin. COMPREHENSION QUESTIONS [19.1] A 32-year-old woman is theorizing that breathing 100% oxygen should increase the amount of oxygen in her blood about fivefold, because room air is composed of approximately 21% oxygen. Which of the following statements is the most accurate answer to her hypothesis? A. The amount of oxygen carried by her hemoglobin probably will increase markedly, but the amount soluble in her serum will remain the same. B. The amount of oxygen carried in her blood will not rise appreciably. C. The amount of oxygen in her blood will rise about fivefold. D. The partial pressure of oxygen in her blood probably will remain unchanged. 160 [19.2] CASE FILES: PHYSIOLOGY A 56-year-old man is admitted to the coronary care unit (CCU) for an acute inferior wall myocardial infarction. The cardiologist is trying to optimize the oxygen delivery to the myocardial tissue. Supplemental oxygen is provided by nasal cannula at 3 L/min. Which of the following best describes the oxygen-carrying capacity of whole blood? A. Dependent on the alveolar PO2 B. The amount of O2 dissolved in the blood C. The sum of the dissolved O2 plus the amount bound to hemoglobin D. The sum of the dissolved O2 plus the amount of O2 bound to hemoglobin under saturating conditions E. Limited by O2 diffusion [19.3] In the case above, the patient had been sleeping in a small room at his house heated with a space heater. He suffered from carbon monoxide poisoning. The carbon monoxide has bound to hemoglobin and reduced its oxygen-binding capacity. Which of the following best describes the PO2 level in the patient’s arterial blood when the paramedics were called to evaluate him? A. Dependent on the alveolar PO2 B. Dependent on the amount of CO bound to hemoglobin C. Increased from normal because of displaced oxygen from hemoglobin D. Reduced from normal because of the CO bound to hemoglobin [19.4] O2 binding to hemoglobin in the pulmonary capillary is inhibited by which of the following? A. B. C. D. CO2 dissociation from hemoglobin Diffusion of CO2 from pulmonary capillary to alveolus Reaction of bicarbonate with H+ Shift to more acidic pH than is found in venous blood Answers [19.1] B. Because the vast majority of oxygen content in blood is carried by hemoglobin, breathing 100% oxygen will increase the partial pressure of oxygen but will not affect the content or oxygen-carrying capacity. [19.2] D. The oxygen-carrying capacity is the total amount of oxygen that can be carried by blood. The capacity is measured under saturating conditions for O2. Therefore, the maximum amount of dissolved oxygen and the maximal amount of bound oxygen are obtained. It is dependent on the amount of hemoglobin in the blood. CLINICAL CASES 161 [19.3] A. The O2 concentration is dependent only on the partial pressure of O2 in the gas phase in contact with the blood, or the alveolar PO2. The binding capacity of the blood is compromised because CO binding to hemoglobin blocks O2 binding; therefore, the total amount of oxygen will be reduced, but not its concentration. [19.4] D. In the pulmonary capillary, CO2 diffusion down its concentration gradient into the alveolar compartment shifts the entire equilibrium to promote O2 binding to hemoglobin. The fall in CO2 in the capillary leads to the dissociation of CO2 from hemoglobin. The fall in CO2 also causes a shift in the equilibrium of the CO2-HCO3- buffer driving the reaction of H+ and HCO3- toward CO2 production with an increase in the pH. Both the fall in CO2 and the rise in pH increase the oxygenbinding affinity of hemoglobin. PHYSIOLOGY PEARLS ❖ ❖ ❖ ❖ The O2 content of arterial blood is the sum of the amount of dissolved O2 plus the amount of O2 bound to hemoglobin. The O2 concentration is the partial pressure of O2 in the blood and is determined by the partial pressure of O2 in the alveolar compartment. About two-thirds of the CO2 produced by metabolism is transported by the blood in the form of HCO3-. The HCO3- is produced from the reaction of CO2 with water and catalyzed by carbonic anhydrase in the red cells. The remaining CO2 is either dissolved or bound to hemoglobin. The affinity of O2 binding to hemoglobin is dependent on the pH, [CO2], temperature, and 2,3-DPG. The combined effects of pH and [CO2] favor O2 dissociation in the tissues and binding of O2 in the pulmonary capillary. In conditions such as anemia and CO poisoning, the O2 concentration of arterial blood can be normal. The O2 content is lower than normal because the amount of hemoglobin or its oxygen-binding capacity is reduced. REFERENCE Powell FL. Oxygen and carbon dioxide transport in the blood. In: Johnson LR, ed. Essential Medical Physiology. 3rd ed. San Diego, CA: Elsevier Academic Press; 2003:289-298. This page intentionally left blank