Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
PHLEBOTOMY TODAY
VOLUME 13, ISSUE 4
©2012 CENTER FOR PHLEBOTOMY EDUCATION, INC.
A monthly newsletter
for those who perform,
teach and supervise
blood collection
procedures.
ALL RIGHTS RESERVED.
CLICK HERE TO VIEW OUR COPYRIGHT POLICY.
April, 2012
Avoiding QNS Rejections
Ernst to Conduct Free Web Chats for Premium Subscribers
From the Editor’s Desk
Safety Essentials
Chemical Hygiene
Phlebotomy in the News
Product Spotlight
To the Point® Volume 4 Download
Tip of the Month
An Army of One
Avoiding QNS Rejections
Have you ever submitted an underfilled tube to the laboratory for testing? If so,
you’re not alone. In fact, up to sixteen percent of all rejected samples are due to
being underfilled, making it the second most common reason labs request a
recollection.1 When tubes are underfilled, everyone loses: the workflow of testing
personnel is interrupted, the productivity of those who draw samples suffers, the
physician is denied a timely result, and the patient has to endure another invasive
procedure. Even worse, when underfilled tubes are not rejected, but tested instead,
they can yield results that misrepresent the patient’s status, which has the
potential for catastrophic consequences. Don’t take the chance; reject all
underfilled samples before leaving the patient.
It’s not just about getting enough blood in the tube to run the test; it’s about the
achieving the proper ratio of blood to the additive in the tube. When underfilled,
the concentration of the additive in the final mixture is excessive, which can lead to
erroneous test results. Only when the tube is filled to its stated volume is the
additive’s affect on test results inert.
Page 1 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
To avoid coming up short with “quantity not sufficient” (QNS) specimens, consider
these suggestions and strategies
Skin Punctures
Increase circulation
Prewarming the intended skin puncture
site for three to five minutes has been
shown to increase blood flow to the area up to sevenfold.2 Better blood flow means
less squeezing and a higher quality
sample. Just be sure not to use
compresses that exceed 42° Celsius, as
higher temperatures can burn an infant’s
delicate skin. Gentle massage of the site
also helps increase circulation.
Taking the time to properly prewarm the puncture site can
result in a quicker collection and yield a higher quality
sample.
Image ©2012. Center for Phlebotomy Education, Inc.
Device selection
For heelsticks, incision devices that slice the tissue horizontally rather than
puncture the skin vertically have been shown to produce a better flow of blood
resulting in shorter draw times with less discomfort to the infant. For patients one
year old and above, select a skin puncture/incision device of an appropriate depth
for the patient. Perform the incision/puncture to either the middle or ring finger
perpendicular to the lines of the fingerprint. This aids formation of the blood drops
and helps prevent blood channeling down the fingerprint. 3
Site positioning
Orient the puncture site vertically downward during collection, and gravity will see
to it that drops form right where the blood exits the tissue not running down the
finger, which makes for a messy collection and reduces the quantity of blood you
can harvest. Positioning the limb lower than the plane of the heart also increases
venous pressure and further facilitates blood flow.
Newborn screening (NBS) samples
Underfilled circles is one of the most common
reasons newborn screening cards are rejected.
When rejected, infants lose precious days in their
diagnosis and treatment of life-threatening
disorders. To assure adequate sample volumes,
Page 2 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
wipe away the first drop of blood from the heel
with clean gauze and allow a large drop of blood to
form. Gently touch the filter paper to the freeflowing blood drop, allowing the blood to soak
Incomplete filling of preprinted test circles
may result in insufficient specimen quantity
and testing delays.
Image ©Shutterstock.com
through and completely fill the preprinted circle
on the card. Repeat to fill all test circles. To prevent testing and diagnosis delays
and the trauma of recollections due to inadequate sample volume, fill all circles
from one side of the card, ensuring that the blood has saturated both sides of the
filter paper.
Venipuncture
Don’t rush vein selection
If a median vein in the antecubital area is not readily visible and/or palpable, take
the time to conduct a thorough survey of both arms. By doing so, you can locate
the most prominent vein that offers the highest degree of confidence for a safe,
successful, and complete draw. Alternatively, veins on the back of the hand and
thumb-side of the wrist may be considered.
Match equipment to the vein
Veins collapse when collectors choose equipment inappropriate for the diameter
and condition of the vein. Hand veins are usually more delicate and smaller than
veins of the antecubital area, as are veins in geriatric, pediatric, and oncology
patients. Such veins also exhibit a greater tendency for hematoma formation
during collection, which requires immediate termination of the draw. When
drawing from small or fragile veins, use a 23-gauge needle or winged collection set
in combination with a syringe. A syringe allows the collector to control the amount
of pulling pressure applied, improving the chances of a successful venipuncture
compared to an evacuated tube system in which 100% of the tube’s vacuum is
transferred to the interior of the vein, risking collapse.
Correct a sluggish draw
Allowing a sluggish draw to proceed is likely to lead to an underfilled (and
hemolyzed) sample. Instead, make adjustments that might increase the blood flow
into the tube or syringe. A sluggish draw can be due to selecting the wrong
Page 3 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
equipment (see above), a collapsed vein, or improper needle placement.
If using a syringe assembly and the draw is sluggish, reduce the pulling pressure
on the plunger, wait a moment or two, then pull back more gently. The vein could
have collapsed, and the pause may be all that’s necessary to allow it to release
from the bevel. If that fails, the needle is probably not placed properly. If you
perceive the needle has passed through the vein during insertion, stop pulling on
the plunger and slightly withdraw the needle. Pull the plunger back gently once
again. If your perception was correct, blood should flow into the syringe properly.
If not, salvaging the puncture may not be possible.
If you perceive to be too shallow, release the plunger, anchor the vein and advance
the needle slightly. Pull on the plunger gently. If the blood flow does not increase,
further advancement might be necessary. If an adequate flow cannot be
established, additional needle relocation should only be attempted according to
facility policy and the standards published by the Clinical and Laboratory
Standards Institute’s venipuncture document (H3).
If using a tube holder assembly, the same conditions may be preventing an
adequate flow. An additional cause could be a tube without the proper vacuum. If
blood does not flow into the tube, remove the tube and apply another one of the
same type. If blood still doesn’t flow adequately, the vein has likely collapsed or
the needle is improperly positioned. When using a tube holder assembly, it’s
difficult to salvage a collapsing vein because the negative pressure applied to the
vein’s interior cannot be controlled as it can when using a syringe. Use a smaller
volume tube instead, which has lesser vacuum. If needle placement is suspect,
remove the tube from the interior needle so that its vacuum is not being applied,
then move the needle backward or forward, depending on your perception of its
misplacement as described above. Apply the tube. If the flow cannot be adequately
established, a repeat venipuncture may be necessary.
Sluggish draws should never be allowed to continue. When they cannot be
corrected, abandon the venipuncture attempt. The sample will likely be rejected
due to hemolysis and you’ll have to recollect it anyway. Select another site, a
different device, or both and repeat the venipuncture.
Adhere to minimum fill volumes
Haste makes waste, especially when additive tubes are removed prematurely from
the tube holder during filling. When additive tubes are underfilled, the effect on
the sample and patient care is significant: 4,5,6,7
Page 4 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
Underfilled tubes containing glycolytic inhibitors (gray stoppers) can be
rejected for hemolysis;
Underfilled EDTA tubes exhibit changes in
hematocrits, MCVs, and red blood cell
morphology;
Underfilled sodium citrate tubes produce falsely
lengthened coagulation times, which lead to lifethreatening medication adjustments;
Underfilled heparin tubes render inaccurate
ALT, amylase, AST, lipase, and potassium
results;
Underfilling some heparinized plasma tubes
leads to the binding of electrolytes and troponin
to heparin;
Underfilled EDTA tubes have an
incorrect blood-to-additive ratio that if
tested, may produce inaccurate results.
Image ©2012. Center for Phlebotomy
Education, Inc.
Underfilling clot-activator tubes can cause
erroneous results in some immunoassays due to the higher concentration of
clot activator and/or silicone;
Underfilled blood culture bottles delay the detection of causative agents of
bacteremia and septicemia and the administration of proper antibiotic
therapy.
To reduce the risk of specimen rejection due to short draws and ensure the proper
blood-to-additive ratio, follow your tube manufacturer’s recommendations. Fill
tubes to their stated volume, holding the tube in place in the tube holder until
blood flow has ceased. For added visual verification, some manufacturers provide
minimum fill indicators on their tubes to show the blood volume necessary to
assure a quality sample.
Use a discard tube
If you are using a winged collection (butterfly) set and a sodium citrate tube is the
first or only tube you are collecting, apply a discard tube long enough to evacuate
the air from the tubing so that the patient’s tube isn’t underfilled. Then apply the
tube to be tested. In order for blue-top tubes to yield accurate results, a 90 percent
fill volume is required.8 Stock pediatric or low/partial-draw tubes
Page 5 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
In difficult-draw situations, tubes with smaller draw volumes can mean the
difference between an acceptable sample and a redraw. However, collectors should
keep in mind that partial-draw tubes may fill more slowly because of their lower
vacuum by comparison.4
Perform a skin puncture
When blood cannot be obtained from the antecubital area or alternative sites, it
may be permissible to perform a capillary collection, based on the test(s) ordered.
Two wrongs don’t make a right
Collectors who repeatedly come up short in sample collection due to collapsed
veins, improper needle placement, hematoma formation, and inappropriate device
selection may be tempted to combine the contents of two or more underfilled tubes
and submit it for testing. Don’t even think about it... not even if they contain the
same additive. Not only does this practice increase the employee’s risk for
occupational exposure to bloodborne pathogens, it at least doubles the
concentration of the additive, wreaking havoc with the results. When two or more
tubes masquerade as one properly filled tube in the testing laboratory, the
potential for erroneous results can lead to a harmful outcome for the patient.
Remember, combining the contents of two underfilled additive tubes doesn’t equal
one properly filled tube.
References
1. Lippi G, Salvagno GL, Montagnana M, et al. Phlebotomy Issues and Quality Improvement in
Results of Laboratory Testing. Clin Lab. 2006;52(5–6):217–30.
2. CLSI. Procedures and Devices for the Collections of Diagnostic Capillary Blood Specimens;
Approved Standard—Sixth Edition. H04-A6. Clinical and Laboratory Standards Institute,
Wayne, PA, 2008.
3. McCall R, Tankersley C. Phlebotomy Essentials, Fourth Edition. Lippincott Williams & Wilkins,
Philadelphia, 2008.
4. Arzoumanian L. Tech Talk. July 2011:10(2). BD Global Technical Services. BD Diagnostics,
Franklin Lakes, NJ.
5. Wu A. Tietz Clinical Guide to Laboratory Tests, Fourth Edition. Saunders Elsevier, St. Louis,
MO, 2006.
6. CLSI. Tubes and Additives for Venous Blood Specimen Collection; Approved Standard—Fifth
Edition. H1-A5. Clinical and Laboratory Standards Institute, Wayne, PA, 2003.
7. Donnelly JG, Soldin SJ, Nealon DA, Hicks JM. Is heparinized plasma suitable for use in routine
biochemistry? Pediatr Pathol Lab Med. 1995 Jul-Aug;15(4):555–9.
8. CLSI. Collection, Transport and Processing of Blood Specimens for Testing Plasma-Based
Page 6 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
Coagulation Assays and Molecular Hemostasis Assays; Approved Guideline—Fifth Edition.
H21-A5. Clinical and Laboratory Standards Institute, Wayne, PA, 2008.
Ernst to Conduct Free Web Chats
for Premium Subscribers
Beginning this month, premium subscribers will be invited to join live web chats
where they can interact with the Center’s Executive Director, Dennis J. Ernst,
MT(ASCP). The first 100 registered Phlebotomy Today premium subscribers will
hear the latest industry news and be able to ask their most pressing phlebotomyrelated questions. Information about the first web chat, scheduled for Tuesday,
April 24, 2012 (1pm EST) will be provided to premium subscribers by email.
Single and institutional subscribers who update their subscriptions to premium will
automatically become eligible for Ernst’s web chat. All Phlebotomy Today
premium subscribers receive the institutional version of Phlebotomy Today with
facility-wide forwarding privileges, and access to Phlebotomy Central, the most
comprehensive online body of knowledge on blood specimen collection.
Click here for more information.
From the Editor’s Desk
As Phlebotomy Today enters its 13th year, you
might think that there’s nothing left for us to
write about. Truth be told, we think that every
month. Then the muses come along and sprinkle
their magic dust on us and poof! A feature comes
to mind... then a Tip of the Month... then this
column... and before you know it we’ve made
another deadline and our insatiable and grateful
readers are satisfied. Sometimes the muse comes in the form of a subscriber
looking for an article on a subject about which we haven’t written. Such is the
case with this month’s feature.
A manager was looking for something in the literature to supplement the
implementation of her LEAN project on samples rejected by the laboratory for
being “quantity not sufficient.” Because the published literature, including our
own archives, was QNS on the subject, we went to work filling the proverbial
Page 7 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
Tube of Preanalytical Knowledge. Since we’re an industry of acronyms, we’ll
call that TPK.
Something else that’s QNS is the amount of time we get to interact regularly.
That’s why starting this month I’m making myself available to premium
subscribers by way of web chats. The first 100 who respond to my personal
invitation—going out later this week as an email to eligible subscribers—will
have my undivided attention for an hour on April 24, Tuesday of National
Medical Laboratory Professionals Week. I’ll preface the chat with an industry
update, new developments I’m aware of affecting the preanalytical world, and
any kind of scuttlebutt I think you might find interesting. Invitations are
exclusive to our premium subscribers, so now’s the time to upgrade.
Another QNS that’s also a perpetual preanalytical problem is respect and
appreciation of those who draw blood samples for our labs. Many of you do an
incredible job recognizing the front line, without whom there would be no
specimens to test. Others, well, let’s face it: we can all do better. So when you
celebrate National Medical Laboratory Professionals Week later this month,
don’t forget the phlebotomists.
One way to recognize them is to give them our new window cling. It lets them
proudly proclaim “I’m a professional, I’m a perfectionist, I’m a phlebotomist.”
Another way is to print and post our phlebotomy Tip of the Month from last
year that puts them on the pedestal they deserve. “You’re a Phlebotomist” can
be accessed here.
Since it’s April, my speaking calendar is as full as I’ll let it get. I’m likely to be
at a conference near you. (Sorry, Alaska and Hawaii. I won’t be that close.
Maybe next year.) This year, you’ll find me at podiums or trade shows in
Kentucky, Nevada, Georgia, California, Virginia, Indiana, Maryland, Maine,
and Ontario. If you can’t make it to any these events, we can always reconnect
this fall when I resume my Phlebotomy Best Practices webinar series. I’ll
announce dates and topics this summer.
So between web chats, webinars, conference lectures, and newsletters, you
have a multitude of ways to reach out to us for information. If these avenues
aren’t enough, you can always interact with us on Facebook, call us or send
me an email. For me and my staff, it’s all about making sure your TPK isn’t
QNS.
Respectfully,
Page 8 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
Dennis J. Ernst MT(ASCP), Editor
phlebotomy@phlebotomy.com
Safety Essentials
Chemical Hygiene
A couple of months ago, I wrote about OSHA’s Bloodborne
Pathogens Standard, which applies to anyone who collects
clinical blood samples in the United States. When I perform
safety rounds with phlebotomists, I also focus on some
other OSHA standards, OSHA’s Chemical Hygiene (or
Laboratory Standard), and the Hazard Communication
Dan Scungio, MT (ASCP), SLS
Standard. Whether or not you spend time in the clinical
laboratory, it may come as a surprise to you that there is
information about chemical hazards that you need to know.
The Hazard Communication Standard states that you have a right to know about
all of the dangers in your workplace, and your employer is responsible to train you
about the risks in order to provide a safe working environment. One way to do that
is to be educated about any chemicals or reagents that are stored or used in your
work area. In blood collection areas, there may be cleaning supplies (such as
bleach), peroxides and rubbing alcohols, and the Chemical Hygiene Standard
applies to these as well. Through your facility’s Chemical Hygiene Plan, a Chemical
Hygiene Officer should be named, and that person is responsible for managing and
updating an inventory of all chemicals stored and used. If you do not know who
that person is, make sure you find out.
Container labeling is an important aspect of the Chemical Hygiene Plan. All
chemicals are required to have a label that contains the identity of the chemical,
the manufacturer, hazard warnings, and target organs affected if exposed.
Secondary containers used to pour off or store chemicals, such as 10% bleach
solution for routine disinfection, need to be properly labeled as well with the name
of the chemical, concentration, route of entry, health hazard, physical hazard,
target organs affected, lab name, lot number and expiration date. Alternatively,
secondary containers can be identified by chemical name and a completed National
Fire Protection Association (NFPA) or Hazardous Materials Identification System
(HMIS) label.
Page 9 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
Knowledge of how to interpret Material Safety Data Sheets (MSDS) and ready
access to these important documents 24/7 should be part of your initial and annual
safety training program. If there is a chemical spill or exposure, using MSDS is
your best resource for treating the affected employee or cleaning up a potentially
hazardous spill.
If you work in a clinical laboratory, you already know there are many chemicals
and reagents present that can pose a safety risk. Just remember that if you work in
a blood collection center or as a traveling phlebotomist, there may be chemicals in
those environments as well. Make sure you are properly educated about the
existing hazards and how to respond should there be a chemical spill or exposure.
If this is news to you, ask your employer how OSHA’s Hazard Communication and
Chemical Hygiene Standards can keep you safe. Bibliography
1. US Department of Labor and Occupational Safety and Health Administration (OSHA). 29 CFR
1910.1200 Hazard Communication. Link. Accessed 3/26/12.
2. US Department of Labor and Occupational Safety and Health Administration (OSHA). 29 CFR
1910.1450 Occupational Exposure to Hazardous Chemicals in Laboratories. Link. Accessed
3/26/12.
3. US Department of Labor and Occupational Safety and Health Administration (OSHA).
Hazardous Chemicals in Labs, OSHA Fact Sheet. Link. Accessed 3/26/12.
Got a safety question? You can contact Dan Scungio, “Dan the Lab Safety Man” at
samaritan@cox.net
Follow us on...
Phlebotomy in the News
Ernst Stresses a Culture of Safety in Reducing Needlesticks
Advance for Medical Laboratory Professionals — Dennis J. Ernst MT(ASCP),
Page 10 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
executive director of the Center for Phlebotomy Education Inc, shares his thoughts
on the reduction of accidental needlesticks realized since the passage of
Needlestick Safety and Prevention Act in 2000 and the need to focus on behavior
changes through ongoing education as the next step to improved safety.
Full Story
EU Directive Mandates Sharps Injury Prevention
Personnel Today — The European Union (EU) Directive on sharps injury
prevention due to be implemented into national law in the United Kingdom (UK)
by May 2013 will require healthcare organizations to take steps to protect their
staff. The Directive requires exposure to be prevented through the use of safetyengineered medical devices, such as needles, phlebotomy devices and intravenous
catheters that incorporate shielding or retraction of the needle; implementing safe
procedures for using and disposing of sharps; providing sharps containers as close
as feasible at the point of use; and a ban on recapping. An estimated one million
sharps injuries occur in the European Union each year, representing a serious
occupational hazard to healthcare workers across Europe, with 68% of those
injuries in the UK caused by hollow-bore needles. Studies reveal that the highest
risk of injury is associated with venous blood draws (>38%), and that only 20% to
50% of all sharps injuries are reported.
Full Story
Phlebotomy School Represents Milestone for Kenya
Business Daily — In February, Kenya opened its first School of Phlebotomy and
Specimen Collection that will train students in occupational safety and clinical and
laboratory procedures, with emphasis on reducing accidental needlestick injuries.
The institution also plans to offer refresher courses and in-services to healthcare
workers. The school, located at Kenya Medical Training College, Nairobi campus, is
the first in East Africa and was established through a partnership of the
government with medical technology company Becton Dickinson, the Centre for
Disease Control, and Jhpiego — an affiliate of Johns Hopkins University.
Full Story
Lab Testing as Close as Your Car
Dark Daily — Ford Motor Company and Toyota Motor Corporation are among
those in the auto industry that are working with healthcare device companies to
create in-vehicle medical testing capabilities so that individuals with chronic
illnesses or medical disorders can manage their condition from behind the wheel.
Full Story
Page 11 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
Study Shows Lower Hand Hygiene Rates with Glove Use
OSHA Healthcare Advisor — A study observing over 7,000 patient contacts at 15
hospitals in the United Kingdom found that overall, hand hygiene compliance
among healthcare workers was 47.7%. But compliance dropped to 41% when gloves
were worn. The study was published in the December 2011 issue of Infection
Control and Hospital Epidemiology.
Full Story
Phlebotomists Key in Preventing Preanalytical Errors
Advance for Administrators of the Laboratory — Because collectors can alter test
results by the manner in which they draw, handle, transport, and process blood
samples, Dennis J. Ernst MT(ASCP), executive director of the Center for
Phlebotomy Education Inc, considers phlebotomists, and phlebotomy supervisors
and educators crucial in the global war against preanalytical errors.
Full Story
Product Spotlight
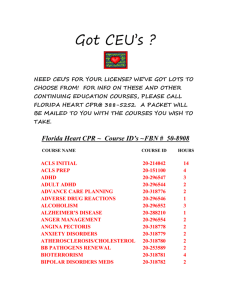
NEW CE Offering! To the Point® Volume 4 Download
The Center for Phlebotomy Education announces the
release of Volume 4 in its popular To the Point ® CE
library of downloads. Volume 4 is a single PDF
containing three articles on various phlebotomy
topics with corresponding test questions. Articles in
Volume 4 include:
Preanalytical Errors that Occur Before Specimen Collection
Preanalytical Errors that Occur During Specimen Collection
OSHA Update
The To the Point ® series provides two affordable continuing education options: 1)
for managers to implement in-house, and 2) for individual phlebotomists and
other healthcare professionals who draw blood samples to meet their continuing
education requirements by obtaining formal P.A.C.E. ® credit.* For in-house use,
managers/instructors distribute the lesson and quiz, then grade their
staff/student’s answers as an internal education exercise.
Page 12 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
Highly researched and regularly updated, all material provided is current and
consistent with the latest CLSI standards and OSHA guidelines.
*To earn a total of 3.0 contact hours of P.A.C.E. ® credit, users simply purchase
the P.A.C.E. ® version of the download, read all three articles, record their
answers to the corresponding test questions and lesson evaluations, and submit
the completed form to us for processing. A test score of 70% or higher for each
article is required.
Click here to order and download.
Tip of the Month
An Army of One
Phlebotomists are freedom fighters. As defenders of specimen quality and patient
safety, day in and day out, you battle a common enemy that seeks to steal the life,
liberty, and longevity of your patients: medical errors. A pervasive foe, medical
errors claim the lives of nearly 100,000 hospitalized patients in the U.S. each year.
Because preanalytical errors account for 60% to 70% of all errors that occur
throughout the total testing process, facilities need highly skilled and trained
phlebotomists on the frontlines in order to win this war. Armed with the
standards, the preanalytical realm is the phlebotomist’s area of expertise, where
you fight against patient and specimen misidentification, and improper collection
and processing techniques.
Many of the laboratory errors that can occur are stealth in nature and can only be
prevented by an Army of One, the phlebotomist. For example:
A surgeon can’t review a lab report and know the potassium was falsely
elevated due to the patient excessively pumping his fist.
The Micro Lab can’t process four filled blood culture bottles and know they
were incorrectly collected from a single venipuncture, or that the site wasn’t
properly cleansed.
The Stat Lab can’t determine the tubes drawn during a flurry of activity in
the ED were mislabeled.
The pediatrician who referred a rambunctious toddler for outpatient lab work
isn’t aware that prolonged tourniquet application skewed the concentration
Page 13 of 17
Phlebotomy Today Copyright 2012. Center for Phlebotomy Education. www.phlebotomy.com. April, 2012. Institutional
of proteins, potassium, and packed cell volume reported.
The Chemistry Lab can’t look at a green-top tube and know it was spiked
with EDTA that carried over when the Order of Draw wasn’t followed.
The Coag Lab may not know that vibration from some pneumatic tube
transport systems can affect blue-top tubes by activating platelets, altering PT
and APTT results.
A hospitalist can’t know a venipuncture above an active IV site falsely
elevated her inpatient’s glucose level.
The Infection Control Officer may not identify lapses in hand hygiene during
patient phlebotomy procedures as a contributor to rising hospital acquired
infections.
To those of you who tirelessly promote patient safety, combat specimen collection
errors, confront complacency, and lead a crusade for ongoing phlebotomy
continuing education, we salute you. When facilities recognize the crucial
contributions phlebotomy teams make in the war against preanalytical errors and
bravely defend their presence, they free themselves and their patients from many
medical errors. In doing so, such bold actions give the phrase “land of the free and
the home of the brave” a whole new meaning.
Post this Tip!
To print an attractive display of this Tip for posting in collection areas,
bulletin boards, break rooms, etc.
printer-friendly (pdf) version.
Notice: Do not respond to this e-newsletter.
Responding to the email address from which this newsletter is sent will result in the deletion
of your address from our mailing list. If you would like to send an email to the editor, send it
to phlebotomy@phlebotomy.com.
CE Questions
1. The second most common reason laboratories reject blood specimens and
Page 14 of 17