Clinical Journal
of Oncology Nursing
®
Suppl. to Dec. 2013, Vol. 17, No. 6 Hematopoietic
Stem Cell
Transplantation
and Multiple
Myeloma:
From the International
Myeloma Foundation
Nurse Leadership Board
The Changing Treatment
Landscape for Multiple
Myeloma, p. 7
An Autologous
Transplantation
Overview, p. 13
Caregivers of Multiple
Myeloma Survivors,
p. 25
Clinical Updates, p. 33
Autologous
Transplantation:
Frequently Asked
Questions, p. 43
www.cjon.org An official journal of the Oncology Nursing Society
Acknowledgment
International Myeloma Foundation Nurse Leadership Board
The International Myeloma Foundation Nurse Leadership Board is a professional nursing partnership representing leading cancer centers and community practices in the United States with the primary mission of understanding and developing strategies to address the
unmet needs of myeloma nurses and their patients. One of the current priorities is addressing the specialty needs of patients undergoing autologous stem cell transplantation and their caregivers. As a part of this goal, this supplement has been developed by members
of the Nurse Leadership Board. It is our hope that the content in this supplement will support the facilitation of care and positively
affect outcomes, including quality of life for patients with myeloma and their caregivers throughout the continuum of care.
B. Nadine Baxter-Hale, MNSc, APN-BC, AOCNP®
University of Arkansas for Medical Sciences
Little Rock, AR
Kathryn Lilleby, RN
Fred Hutchinson Cancer Research Center
Seattle, WA
Page A. Bertolotti, RN, BSN, OCN®
Samuel Oschin Cancer Center at Cedars-Sinai Medical Center
Los Angeles, CA
Patricia A. Mangan, MSN, APRN-BC
Abramson Cancer Center, University of Pennsylvania
Philadelphia, PA
Elizabeth Bilotti, MSN, APRN, BC, OCN®
John Theurer Cancer Center at Hackensack University Medical
Center
Hackensack, NJ
Teresa Miceli, RN, BSN, OCN®
Mayo Clinic, William Von Liebig Transplant Center
Rochester, MN
Kathleen Colson, RN, BSN, BS
Jerome Lipper Multiple Myeloma Center at Dana-Farber
Cancer Institute
Boston, MA
Kena C. Miller, ARNP-BC
Mayo Clinic
Jacksonville, FL
Deborah Doss, RN, OCN®
Jerome Lipper Multiple Myeloma Center at Dana-Farber
Cancer Institute
Boston, MA
Beth Faiman, MSN, APRN-BC, AOCN®
Cleveland Clinic
Cleveland, OH
Elizabeth Finley-Oliver, RN, OCN
H. Lee Moffitt Cancer Center and Research Institute
Tampa, FL
®
Kimberly Noonan, RN, ANP-BC
Dana-Farber Cancer Institute
Boston, MA
Tiffany A. Richards, RN, ANP-BC
University of Texas MD Anderson Cancer Center
Houston, TX
Sandra I. Rome, RN, MN, AOCN®
Cedars-Sinai Medical Center
Los Angeles, CA
Charise L. Gleason, MSN, ANP-C, AOCNP®
Winship Cancer Institute of Emory University
Atlanta, GA
Jacy Spong, RN, BSN, OCN®
Mayo Clinic
Scottsdale, AZ
Sandra Kurtin, RN, MS, AOCN®, ANP-C
The University of Arizona Cancer Center
Tucson, AZ
Joseph D. Tariman, PhD, ANP-BC
Northwestern University
Chicago, IL
Publication of the supplement was made possible through support by Sanofi Oncology
to the International Myeloma Foundation.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Acknowledgment
1
Clinical Journal
of Oncology Nursing®
Editor
Supplement to Volume 17,
Number 6, December 2013
Editorial Staff
Deborah K. Mayer, PhD, RN, AOCN , FAAN
University of North Carolina–Chapel Hill
CJONEditor@ons.org (email)
®
Associate Editors
Carlton G. Brown, PhD, RN, AOCN®, FAAN • Valerie Burger, RN,
MA, MS, OCN® • Ellen R. Carr, RN, MSN, AOCN® • Jennifer C.
Ewing, RN, MSN, NP-C, AOCNP® • Anne H. Gross, PhD, RN,
NEA-BC • Mallori Hooker, RN, MSN, NP-C, AOCNP® • Guadalupe
R. Palos, RN, LMSW, DrPH • Carol A. Sheridan, RN, MSN
Elizabeth M. Wertz Evans, PhD, RN, MPM, CPHQ, CPHIMS,
FHIMSS, FACMPE, Executive Director of Professional Practice
and Programs and Publisher • Bill Tony, BA, CQIA, Director
of Publications • Leslie McGee, BA, Managing Editor • Mike
Minjock, BA, Production and Permissions Manager • Angela
Klimaszewski, RN, MSN, CNE Editor • Barbara Lubejko, RN,
MS, Education Associate • Sean Pieszak, BA, Staff Editor •
Amanda Baker, BS, Jaclyn Enderle, BA, Jessica Moore, BA, BS,
Sarah Reagle, BA, Copy Editors • Natalie Aitken Tooch, Editorial
Assistant
Mission Statements
The Clinical Journal of Oncology Nursing (CJON) is an official publication of the Oncology Nursing Society (ONS) and is directed to
the nurse caring for patients with or at risk for cancer. CJON is a vehicle to advance the mission of ONS, which is to promote excellence
in oncology nursing and quality cancer care. The CJON mission is twofold: (a) to provide practical information necessary to care for
patients and their families across the cancer continuum and (b) to develop publication skills in oncology nurses.
Articles are to be clear, concise, comprehensive, and well referenced.A manuscript submitted to CJON must only be under consideration to this journal;
the material must be original and not previously published. All submitted
articles are subject to a double-blind peer review. Articles will be judged
on quality of the work and suitability for the CJON audience. For more information about authorship, financial disclosures, manuscript preparation,
permissions, and manuscript submission, see www.cjon.org.
National Office
Oncology Nursing Society
125 Enterprise Dr.
Pittsburgh, PA 15275-1214 USA
Phone: 866-257-4ONS (toll free); +1-412-859-6100
Fax: 877-369-5497 (toll free); +1-412-859-6163
Customer Service: customer.service@ons.org
Clinical Journal of Oncology Nursing: pubCJON@ons.org
ONS website: www.ons.org
Integrity • Innovation • Stewardship
Advocacy • Excellence • Inclusiveness
INDEXING: CJON is indexed in CINAHL®, MEDLINE®, EBSCO Health Source: Nursing/Academic Edition database, PsycINFO, ProQuest Nursing and Allied Health
Source, and OCLC ArticleFirst.
SUBSCRIPTIONS: To become a member and receive a subscription to the Clinical
Journal of Oncology Nursing, call toll free at 1-866-257-4ONS. All subscriptions
will start with the first issue published after the order is received.
BACK COPIES: Back issues are available at a per-copy charge of $10 for individuals
and $25 for institutions. Payments should accompany all orders. Make checks payable to the Oncology Nursing Society and send to ONS, P.O. Box 3830, Pittsburgh,
PA 15230-3830 USA. The content of CJON is included in EBSCO Publishing’s
informational products. For more information, contact EBSCO Publishing at 800653-2726 or www.epnet.com.
PERMISSIONS: Requests for permission to reprint, adapt, photocopy, post online,
or otherwise reuse any or all content from a CJON article should be sent via email
to pubpermissions@ons.org.
REPRINTS: Reprints may be obtained by contacting the YGS Group at 800-2905460 or +1-717-399-1900, ext. 100, or cjon@theYGSgroup.com.
ADVERTISING: Send display advertising, correspondence, insertion orders, and
printing materials to Clinical Journal of Oncology Nursing, East Holly Avenue,
Box 56, Pitman, NJ 08071-0056 USA. For general information, contact the sales
representatives at A.J. Jannetti, Inc. (+1-856-256-2300; +1-856-589-7463, fax). All
advertising is subject to the approval of the publisher.
FINANCIAL DISCLOSURE POLICY: ONS supports the principle of financial disclosure
and has taken steps to ensure that all editors, editorial board members, reviewers, and authors understand the policy and comply with it. A copy of the ONS
Publishing Division Financial Disclosure Policy is available on request by emailing
pubCJON@ons.org.
CHANGE OF ADDRESS: Please contact the ONS National Office.The publisher cannot accept responsibility for undelivered copies.
ONS and the Editorial Board do not assume responsibility for the opinions expressed by
authors or editors, including those stated in the Editorial. Description of products and acceptance of advertising do not indicate or imply endorsement by CJON or ONS. The reader
should not construe anything in this journal as being medical or legal advice nor assume
that any nursing practices described herein will ensure safe and effective patient care.
Websites mentioned in the articles and features are provided for information only. The
hosts are responsible for content and availability.
An employee of a business corporation shall be permitted to make ONS educational
program presentations (oral and written) that feature a product or service of the presenter’s employer if employment and/or financial involvement is fully disclosed. Such
presentations do not imply ONS endorsement of said product or service and must be so
stated by the presenter or author.
ONS publications are originally published in English. Publishers wishing to translate
ONS publications must contact the ONS Publishing Division about licensing arrangements. ONS publications cannot be translated without written permission from ONS.
(Individual tables and figures that are reprinted or adapted require additional permission
from original sources.) Because translations from English may not always be accurate or
precise, ONS disclaims any responsibility for inaccuracies in words or meaning that may
occur as a result of translation. Readers relying on precise information should check the
original English versions.
The Clinical Journal of Oncology Nursing® is a publication of the Oncology Nursing Society. Copyright © 2013 by the Oncology Nursing Society. All rights reserved.
The Clinical Journal of Oncology Nursing® (ISSN 1092-1095) is published bimonthly (February, April, June, August, October, and December) by the Oncology
Nursing Society, 125 Enterprise Drive, Pittsburgh, PA 15275-1214 USA. A yearly subscription is $199 for institutions ($20 extra for international subscriptions).
As part of ONS membership dues, $11.80 are for a one-year subscription to the journal. Periodical postal privileges paid at Pittsburgh, PA, and additional mailing offices. Supplement to Vol. 17, No. 6
POSTMASTER: Send address changes to Clinical Journal of Oncology Nursing, Oncology Nursing Society, 125 Enterprise Drive, Pittsburgh, PA 15275-1214 USA.
Printed in the United States. Please recycle this journal.
Contents
Supplement to the Clinical Journal of Oncology Nursing
Feature Articles
17
The Changing Landscape of Multiple Myeloma:
Implications for Oncology Nurses
Sandra Kurtin, RN, MS, AOCN®, ANP-C
and Beth Faiman, MSN, APRN-BC, AOCN®
13
Autologous Hematopoietic Stem Cell Transplantation
for Patients With Multiple Myeloma: An Overview for Nurses
in Community Practice
Teresa Miceli, RN, BSN, OCN®, Kathryn Lilleby, RN,
Kimberly Noonan, RN, ANP-BC, Sandra Kurtin, RN, MS, AOCN®, ANP-C,
Beth Faiman, MSN, APRN-BC, AOCN®, and Patricia A. Mangan, MSN, APRN-BC
25
Caregivers of Multiple Myeloma Survivors
Sandra Kurtin, RN, MS, AOCN®, ANP-C, Kathryn Lilleby, RN,
and Jacy Spong, RN, BSN, OCN®
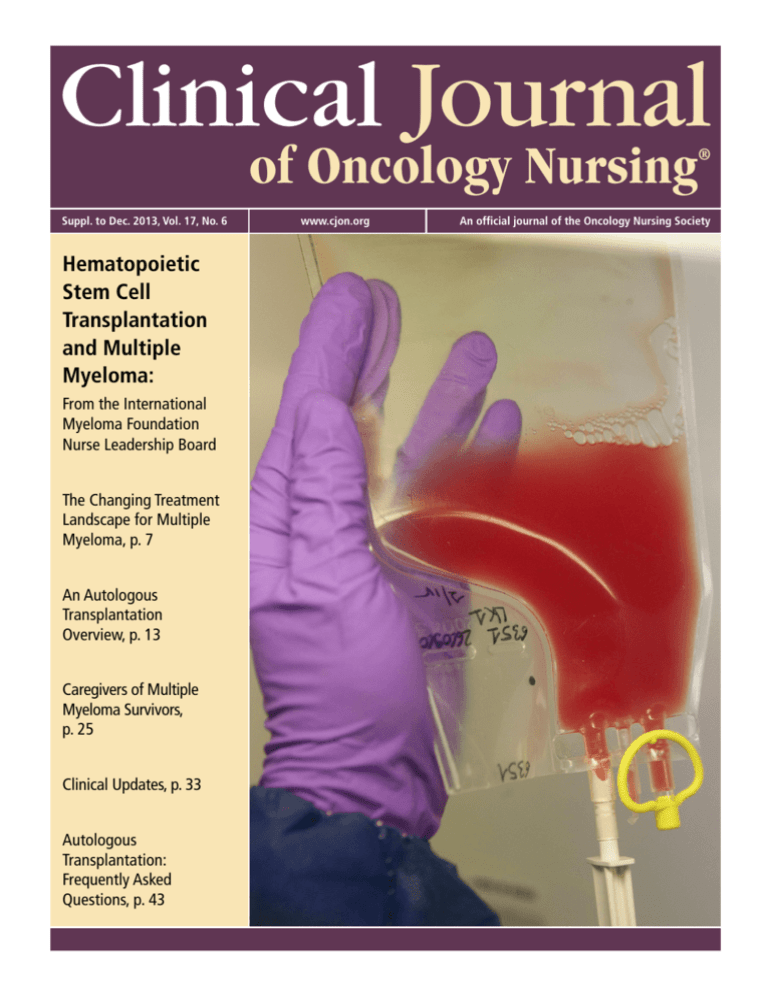
Cover: © Owen Franken/Photographer’s Choice RF/Getty Images
About the Cover
33
Clinical Updates in Blood and Marrow Transplantation
in Multiple Myeloma
Beth Faiman, MSN, APRN-BC, AOCN®, Teresa Miceli, RN, BSN, OCN®,
Kimberly Noonan, RN, ANP-BC, and Kathryn Lilleby, RN
43
Autologous Hematopoietic Stem Cell Transplantation
for Multiple Myeloma: Frequently Asked Questions
Patricia A. Mangan, MSN, APRN-BC, Charise F. Gleason, MSN, ANP-C, AOCNP®,
and Teresa Miceli, RN, BSN, OCN®
Multiple myeloma is a plasma cell neoplasm noted
for excess paraprotein secretion and organ effects
such as renal, bone, bone marrow, neurologic, and
immune dysfunction. Autologous hematopoietic
stem cell transplantation (above) is an important
treatment option for patients with multiple myeloma.
The articles in this supplement will analyze, from
an oncology nurse viewpoint, the autologous
hematopoietic stem cell transplantation procedure as
well as the changing landscape of multiple myeloma
care, processes to support caregivers, blood and
marrow transplantation updates, and frequently
asked questions oncology nurses may have about the
transplantation process.
Publication of this supplement was made possible through support from Sanofi Oncology to the International Myeloma Foundation.
How to Use DOIs: All Clinical Journal of Oncology Nursing articles and features include a digital object identifier (DOI). When added to the end of
http://dx.doi.org/, a DOI can be used to locate a print piece online. For example, adding the DOI 10.1188/13.CJON.34-40 to http://dx.doi.org/ results
in http://dx.doi.org/10.1188/13.CJON.34-40, which can be used like any other web address to retrieve an article online.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Contents
5
n Introduction
The Changing Landscape of Multiple Myeloma:
Implications for Oncology Nurses
Sandra Kurtin, RN, MS, AOCN®, ANP-C, and Beth Faiman, MSN, APN-BC, AOCN®
Scientific advancements relative to diagnostic evaluation, risk-adapted treatment selection, and supportive care strategies for multiple myeloma (MM) have been developed in the past decade, which
provides hope for patients living with MM. However, the disease remains incurable for the majority
of patients, and continued clinical trials are necessary to refine existing therapeutic strategies and
develop new approaches to treatment. Hematopoietic stem cell transplantation (HSCT), in particular
autologous HSCT, remains an important component in the overall treatment paradigm for MM. This
requires a well-organized team approach with ongoing communications and collaboration with
community providers and other specialists. The majority of care for patients with MM is provided
in the outpatient setting, relying on the active participation of both the patient and caregiver(s) for
© ISM/Phototake
successful clinical outcomes. This supplement is prepared by members of the International Myeloma Foundation Nurse
Leadership Board, which is dedicated to improving the care of patients with MM and their caregivers. The introduction
serves to provide an overview of MM today and to summarize the articles included in this supplement.
Sandra Kurtin, RN, MS, AOCN®, ANP-C, is a nurse practitioner and clinical assistant professor of medicine in the Hematology/Oncology Division of the University
of Arizona Cancer Center in Tucson, and Beth Faiman, MSN, APN-BC, AOCN®, is a nurse practitioner in the Taussig Cancer Center at the Cleveland Clinic in
Ohio. The authors received editorial support from Alita Anderson, MD, with Eubio Medical Communications in preparation of this article supported by Sanofi
Oncology. The authors are fully responsible for content and editorial decisions about this article. Kurtin serves as a consultant for Celgene Corporation, Novartis
Pharmaceuticals, Millennium: The Takeda Oncology Company, and Onyx Pharmaceuticals. Faiman has no financial relationships to disclose. The content of this
article has been reviewed by independent peer reviewers to ensure that it is balanced, objective, and free from commercial bias. No financial relationships
relevant to the content of this article have been disclosed by the independent peer reviewers or editorial staff. Kurtin can be reached at sandra.kurtin@uahealth
.com, with copy to editor at CJONEditor@ons.org. (Submitted July 2013. Revision submitted September 2013. Accepted for publication September 12, 2013.)
Digital Object Identifier:10.1188/13.CJON.S2.7-11
M
ultiple myeloma (MM) is a plasma cell neoplasm
characterized by excess paraprotein secretion
with secondary organ effects including renal,
bone, bone marrow, neurologic, and immune
dysfunction. About 22,350 new cases of MM
are projected in 2013 (12,440 men, 9,910 women), with 10,710
deaths (6,070 men, 4,640 women) (Wallin & Larson, 2011).
Risk factors for MM include advanced age, male gender, obesity, and African American descent (American Cancer Society
[ACS], 2013; Perotta et al., 2013). The incidence of MM in 2013
in African American men was estimated at 14.4 per 100,000,
more than double the 6.6 per 100,000 for Caucasian men (ACS,
2013). Similarly, African American women are more likely to
develop MM compared to Caucasian women (9.8 per 100,000
versus 4.1 per 100,000). MM is listed as the 10th most common
type of cancer for both African American men and women, the
10th leading cause of cancer death in men, and the seventh
leading cause of cancer death in women (National Cancer
Institute [NCI], 2010). The cause of the increased incidence in
the African American population has not been explained and
emphasizes the need for continued investigation into genetic
predisposition to this disease.
Previous studies evaluating occupational exposure in MM
have been limited by small sample size and variable measures
for exposure to selected chemical compounds. Perotta et al.
(2013) conducted a pooled analysis of five international casecontrolled studies, including 1,959 patients with MM and 6,192
control participants, evaluating the association of occupational
chemical exposure and the incidence of MM. Among a wide
range of work categories, gardeners, plant nursery workers, and
crop farmers were the most likely to be exposed to pesticides
and showed a 50% increased risk of developing MM in this
analysis (odds ratio [OR] = 1.5, 95% confidence interval [CI]
[0.9, 2.3]). Metal processors (OR = 1.55, 95% CI [0.98, 2.35])
and women working in the housekeeping or cleaning professions (OR = 1.32, 95% CI [1, 1.76]) also showed increased risk
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • The Changing Landscape of Multiple Myeloma
7
Implications for Practice
u
Understanding the current approach to the treatment of
multiple myeloma can help oncology nurses provide optimal
situations for their patients.
u
Knowing the disease characteristics for multiple myeloma,
smoldering myeloma, and monoclonal gammopathy of undetermined significance can aid in early detection.
u
Examining the impact novel agents have had on improving
survival for patients with multiple myeloma can help oncology nurses, patients, and caregivers understand possible
treatment choices.
attributed to exposure to a range of potentially harmful substances such as arsenic, cadmium, lead, and various cleaning
solutions. The data emphasize the need to continue efforts in
identification of risk factors for MM and pursuit of opportunities
to develop prevention strategies.
Disease and Treatment
The disease continuum of MM encompasses distinct clinical
diagnoses, each defined by clinical and diagnostic criteria (see
Figure 1). Monoclonal gammopathy of undetermined significance is an asymptomatic premalignant condition that precedes
myeloma and does not require immediate treatment (Rajkumar,
2010). A 1% per year risk exists of progressing to MM; however,
the overall risk of progression to MM or a related plasma cell
disorder is higher in patients with higher paraprotein levels,
an abnormal kappa/lambda serum-free light chain ratio, and
non–immunoglobulin-G (IgG) subtypes (Agarwal & Ghobrial,
2012; Rajkumar, 2010; Rajkumar et al., 2005). Smoldering my-
Nonmalignant
Accumulation
Malignant
Transformation
eloma (SM) is a more advanced premalignant and asymptomatic
precursor to MM with distinct clinical findings and a greater
risk of progression to MM (Rajkumar, 2010). Clinical trials are
ongoing to evaluate the role of disease-modifying treatment in
the setting of SM.
Treatment is indicated when a patient has active MM with evidence of end-organ damage as defined by the CRAB criteria (Calcium elevation, Renal dysfunction, Anemia, and Bone disease).
The overall goal for treatment of MM is a complete response,
with an acceptable level of toxicity and quality of life (Palumbo
& Cavallo, 2012). Achieving a complete response has been
identified as a key factor in improved progression-free survival
and overall survival; however, achieving a complete response
does not imply eradication of the malignant clone. Survival of
patients with MM has improved significantly through continued
clinical investigation, the evolution of molecular and genetic
profiling, novel therapies, risk-adapted treatment selection, and
better supportive care (see Figures 2 and 3). Despite these advances, MM remains incurable for the majority of patients with
expected relapses, each with unique clinical characteristics,
patient attributes, and treatment options (Palumbo & Anderson,
2011; Siegel & Bilotti, 2009) (see Figure 4).
Autologous hematopoietic stem cell transplantation (AHSCT)
remains an important treatment option for MM. Transplantation eligibility is based on well-established clinical criteria and
should be considered at the time of diagnosis. Exposure to melphalan and other stem cell toxic agents must be avoided prior to
stem cell collection (National Comprehensive Cancer Network
[NCCN], 2013). Allogeneic HSCT remains investigational and
is generally reserved for patients with higher-risk disease who
have failed AHSCT and currently available novel therapies. It
should only be considered within the context of a clinical trial
(NCCN, 2013; NCI, 2010). The results of ongoing and future allogeneic HSCT trials will further elucidate the role of nonmyeloablative or reduced-intensity conditioning regimens in this setting.
Aggressive and Stromal
Independent
Plasma
Cell
Leukemia
Multiple Myeloma Precursor Diseases
MGUS
• Less than 3 g M protein
• Less than 10% clonal BMPC
• No multiple myelomarelated end-organ damage
• 1% per year risk of
progression to multiple
myeloma
Smoldering Myeloma
• 3 g or greater M protein
• Less than 10% clonal BMPC
• No multiple myeloma-related
end-organ damage
• 10% per year risk of progression to multiple myeloma in
the first five years
Multiple Myeloma
• Greater than 10% clonal BMPC
• M protein in serum and/or urine
• More than one CRAB feature of disease-related organ damage
C: Calcium elevation: greater than 11.5 mg/L or ULN
R: Renal dysfunction: serum creatinine greater than 2 mg/dl
A: Anemia: Hb less than 10 g/dl or 2 g less than normal
B: Bone disease: lytic lesions or osteoporosis
BMPC—bone marrow plasma cells; Hb—hemoglobin; M protein—monoclonal protein; MGUS—monoclonal gammopathy of undetermined significance;
ULN—upper limit of normal
Note. Based on information from Agarwal & Ghobrial, 2012; Durie et al., 2003; Kuehl & Bergsagel, 2002; Vacca & Ribatti, 2006.
FIGURE 1. Multiple Myeloma Disease Characteristics
Note. From “Laboratory Measures for the Diagnosis, Clinical Management, and Evaluation of Treatment Response in Multiple Myeloma,” by S. Kurtin, 2010,
Journal of the Advanced Practitioner in Oncology, 1, p. 201. Copyright 2010 by Harborside Press. Reprinted with permission.
8
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
Implications for Clinical Practice
the caregiver role for the patient with MM, common attributes
of caregiver stress or strain, and guidelines for assessment of
caregiver stress. Strategies for empowering the caregiver and
resources and tools to promote self-management are provided.
Population Surviving
Population Surviving
HSCT requires planning and coordination from the time a
patient is considered a candidate for transplantation through
the post-transplantation period. The logistics
of preparation, treatment, follow-up, expected
treatment-emergent adverse events, coordination
A. Survival Curve for Patients Grouped by Year of Diagnosis
of care within and between settings, financial
1.0
implications, and the patient-caregiver dynamics
0.9
must all be considered. The International Myeloma
Foundation Nurse Leadership Board is committed to
0.8
Median overall survival:
improving the lives of patients living with MM; thereMore than 6 yearsa
0.7
fore, this supplement provides a clinical guide to
0.6
the care of patients with MM undergoing HSCT. The
primary focus is on AHSCT. This series of articles
0.5
also provides tools for forming a partnership with
0.4
patients and caregivers to improve self-management
0.3
p < 0.001
capabilities and, ultimately, improve quality of life
and clinical outcomes.
0.2
Miceli et al. (2013) provides a road map to AHSCT
Median overall
0.1
for the patient with MM. A detailed description of
survival: 4.6 years
0
the role of AHSCT in the treatment of MM; eligibility
012345678910
criteria; and pretransplantation, peritransplantation,
and post-transplantation considerations for patients,
Follow-Up From Diagnosis (Years)
caregivers, and providers in multiple settings is of2001–2005
2006–2010
fered. As previously mentioned, the patient undergoing AHSCT will receive a bulk of his or her care in
the outpatient setting, and much of this will occur
B. Survival Curve for Patients by Status of Receipt of Novel Agents at Diagnosis
in the patient’s community.
1.0
Clinical guidelines are included to provide the
0.9
community oncology professional with tools to as0.8
sist in collaborative management of patients with
Median overall
MM undergoing AHSCT. Given the heterogeneity of
0.7
survival: 7.3 years
the MM population, an individualized approach to
0.6
therapy is necessary, and variability in treatment ap0.5
proaches based on patient-specific factors is common.
The article by Mangan, Gleason, and Miceli (2013)
0.4
addresses the frequently asked questions pertaining
0.3
to common decision points in the process of HSCT,
0.2
such as: Who are good candidates for AHSCT? What
Median overall
is the optimal timing of an AHSCT? What is the role
0.1
survival: 3.8 years
of allogenic-HCT in the treatment of MM? And what
0
is the role of maintenance therapy following AHSCT?
01 2 34 56 78910
Faiman, Miceli, Noonan and Lilleby (2013) provide
Follow-Up From Diagnosis (Years)
an update on scientific developments pertaining
to the process of HSCT relative to MM. Common
Received novel agent at diagnosis
preparative regimens, techniques for stem cell moNo novel agent at diagnosis
bilization and collection, and management of the
a
patient in the peritransplantation and immediate
Not yet reached
post-transplantation period are described.
Note. Patients diagnosed from 2006–2010 are living longer than those diagnosed
The availability of a caregiver is a prerequisite to
from 2001–2005. The majority of the survival gains were among those older than
HSCT eligibility. Caregivers may include spouses
age 65 years. Novel drugs (thalidomide, bortezomib, lenalidomide) used at diagnosis
helped patients live longer.
or other family members, friends, or volunteers.
These individuals play a critical role in the effective
FIGURE 2. Novel Agents Improve Survival
management of the patient prior to, during, and
Note. From “Continued Improvement in Survival in Multiple Myeloma and the Impact of
following an HSCT. Caregiver stress and strain are
Novel
Agents” by S. Kumar, A. Dispenzieri, M. Gertz, M. Lacy, J. Lust, S. Hayman . . . S.V.
common and may have a negative effect on the qualRajkumar, 2012. Retrieved from http://myeloma.org/pdfs/ASH2012_Kumar_3865.pdf.
ity of life of the patient and the caregiver. Kurtin,
Copyright 2012 by the American Society of Hematology. Reprinted with permission.
Lilleby, and Spong (2013) review key components of
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • The Changing Landscape of Multiple Myeloma
9
Multiple Myeloma Therapy Introduction
1950
1960
1958
Melphalan
1970
U.S. Food and Drug Administration Approval
1980
1962
Prednisone
1990
1983
Autologous
transplantation
1969
Melphalan plus prednisone
1996
Bisphosphonates
1986
High-dose dexamethasone
2010
2000
2006
Plerixafor
2013
Pomalidomide 3rd line
2003
Bortezomib 3rd line
2012
Carfilzomib 3rd line
Bortezomib SQ
2005
Bortezomib 2nd line
2006
Lenalidomide plus dexamethasone 1st line
Lenalidomide plus dexamethasone 2nd line
2008
Bortezomib frontline
2007
Doxorubicin plus
bortezomib frontline
SQ—subcutaneous
Note. Bisphosphonates and plerixafor are supportive care medications. All other types listed here are treatments.
FIGURE 3. Timeline for Multiple Myeloma Drug Development
Conclusion
The scientific advances in the field of MM relative to the pathobiology of the disease, identification of potential new targets for
therapy, mechanisms of resistance, and integration of new agents
into the existing treatment paradigm are ongoing. Integrating
these changes into clinical practice and anticipating continued
developments is a challenge for the oncology professional.
HSCT remains an important component of the treatment paradigm. Familiarity with eligibility criteria, pretransplantation
evaluation, the actual transplantation process, and supportive
care for the patient throughout the treatment continuum
Aggressive and Stromal
Independent
Nonmalignant
Accumulation
M protein
(grams)
10
Asymptomatic
Symptomatic
Active
myeloma
5
2
Clonal Evolution
Malignant Transformation
MGUS or
smoldering
myeloma
Relapse
Refractory
relapse
Plateau
remission
M protein—monoclonal protein; MGUS—monoclonal gammopathy of undetermined significance
Time
Note. Variable timeline dependent on individual risk factors, including genetic and phenotype changes.
Note. Based on information from Agarwal & Ghobrial, 2012; Durie et al., 2003; Kuehl & Bergsagel, 2002; Siegel & Bilotti, 2009; Vacca & Ribatti, 2006.
FIGURE 4. Multiple Myeloma Disease Trajectory and Relapse
Note. From “Laboratory Measures for the Diagnosis, Clinical Management, and Evaluation of Treatment Response in Multiple Myeloma,” by S. Kurtin, 2010,
Journal of the Advanced Practitioner in Oncology, 1, p. 203. Copyright 2010 by Harborside Press. Adapted with permission.
10
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
will improve the care of patients with MM undergoing HSCT.
Integrating tools and strategies for patient and caregiver selfmanagement as well as caregiver support will improve the active participation and quality of life for both groups. Continued
engagement and collaboration with oncology professionals in
support of the patient and caregiver and in robust scientific
discovery will be necessary to effectively integrate these new
techniques or strategies into the MM treatment and supportive
care paradigm.
The authors gratefully acknowledge Brian G.M. Durie, MD,
Robert A. Kyle, MD, and Diane P. Moran, RN, MA, EdM, senior
vice president of strategic planning at the International Myeloma
Foundation, for their critical review of the manuscript.
References
Agarwal, A., & Ghobrial, I.M. (2012). Monoclonal gammopathy of
undetermined significance and smoldering multiple myeloma: A
review of the current understanding of epidemiology, biology,
risk stratification, and management of myeloma precursor disease. Clinical Cancer Research, 19, 985–994. doi:10.1158/1078
-0432.CCR-12-2922
American Cancer Society. (2013). Cancer facts and figures 2013.
Retrieved from http://www.cancer.org/research/cancerfactsfig
ures/cancerfactsfigures/cancer-facts-figures-2013
Durie, B.G., Kyle, R.A., Belch, A., Bensinger, W., Blade, J., Boccadoro, M., . . . Van Ness, B. (2003). Myeloma management
guidelines: A consensus report from Scientific Advisors of the
International Myeloma Foundation. Hematology Journal, 4,
379–398. doi:10.1038/sj.thj.6200312
Faiman, B., Miceli, T., Noonan, K., & Lilleby, K. (2013). Clinical update
in bone marrow transplantation in multiple myeloma. Clinical
Journal of Oncology Nursing, 17(Suppl., 2), 33–41. doi:10.1188/13
.CJON.S2.33-41
Kuehl, W.M., & Bergsagel, P.L. (2002). Multiple myeloma: Evolving
genetic events and host interactions. Nature Reviews: Cancer,
2, 175–187. doi:10.1038/nrc746
Kumar, S., Dispenzieri, A., Gertz, M., Lacy, M., Lust, J., Hayman, S.,
. . . Rajkumar, S.V. (2012). Continued improvement in survival
in multiple myeloma and the impact of novel agents [Abstract
3972]. Retrieved from http://myeloma.org/pdfs/ASH2012_
Kumar_3865.pdf
Kurtin, S., Lilleby, K., & Spong, J. (2013). Caregivers of multiple
myeloma survivors. Clinical Journal of Oncology Nursing,
17(Suppl., 2), 25–32. doi:10.1188/13.CJON.S2.25-32
Mangan, P., Gleason, C., & Miceli, T. (2013). Autologous hematopoietic stem cell transplantation for multiple myeloma: Frequently asked questions. Clinical Journal of Oncology Nursing,
17(Suppl., 2), 43–47. doi:10.1188/13.CJON.S2.43-47
Miceli, T., Lilleby, K., Noonan, K., Kurtin, S., Faiman, B., & Mangan, P. (2013). Autologous hematopoietic stem cell transplantation for patients with multiple myeloma. An overview for
nurses in community practice. Clinical Journal of Oncology
Nursing, 17(Suppl., 2), 13–24. doi:10.1188/13.CJON.S2.13-24
National Cancer Institute. (2010). SEER stat fact sheets: Myeloma.
Retrieved from http://seer.cancer.gov/statfacts/html/mulmy.html
National Comprehensive Cancer Network. (2013). NCCN Clinical
Practice Guidelines in Oncology: Multiple myeloma [v.1.2013].
Retrieved from http://www.nccn.org/professionals/physician_
gls/f_guidelines.asp#myeloma
Palumbo, A., & Anderson, K. (2011). Multiple myeloma. New
England Journal of Medicine, 364, 1046–1060. doi:10.1056/
NEJMra1011442
Palumbo, A., & Cavallo, F. (2012). Have drug combinations supplanted stem cell transplantation in myeloma? Blood, 120,
4692–4698. doi:10.1182/blood-2012-05-423202
Perotta, C., Kleefeld, S., Staines, A., Tewari, P., De Roos, A.J., Baris, D.,
. . . Cocco, P. (2013). Multiple myeloma and occupation: A polled
analysis by the International Multiple Myeloma Consortium. Cancer Epidemiology, 37, 300–305. doi:10.1016/j.canep.2013.01.008
Rajkumar, S.V. (2010). Multiple myeloma: 2011 update on diagnosis, risk-stratification, and management. American Journal of
Hematology, 86, 57–65. doi:10.1002/ajh.21913
Rajkumar, S.V., Kyle, R.A., Therneau, T.M., Melton, L.J., Bradwell,
A.R., Clark, R.J., . . . Katzmann, J.A. (2005). Serum free light chain
ratio is an independent risk factor for progression in monoclonal
gammopathy of undetermined significance. Blood, 106, 812–817.
doi:10.1182/blood-2005-03-1038
Siegel, D.S., & Bilotti, E. (2009). New directions in therapy for
multiple myeloma. Community Oncology, 6(Suppl., 3), 22–30.
Vacca, A., & Ribatti, D. (2006). Bone marrow angiogenesis in multiple myeloma. Leukemia, 20, 193–199. doi:10.1182/blood-2005
-03-1038
Wallin, A., & Larson, S.C. (2011). Body mass index and risk of multiple myeloma: A meta-analysis of prospective studies. European
Journal of Cancer, 47, 1606–1611. doi:10.1016/j.ejca.2011.01.020
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • The Changing Landscape of Multiple Myeloma
11
n Article
Autologous Hematopoietic Stem Cell
Transplantation for Patients With Multiple Myeloma:
An Overview for Nurses in Community Practice
Teresa Miceli, RN, BSN, OCN®, Kathryn Lilleby, RN, Kimberly Noonan, RN, ANP-BC, Sandra Kurtin, RN, MS, AOCN®, ANP-C,
Beth Faiman, MSN, APRN-BC, AOCN®, and Patricia A. Mangan, MSN, APRN-BC
Autologous hematopoietic stem cell transplantation (AHSCT) is approved for the treatment
of select solid tumors, autoimmune disorders, and most hematologic malignancies. Multiple
myeloma (MM) is the most common indication for AHSCT. Despite improvement in response
and survival rates in the era of novel agents, AHSCT remains an important treatment option
for patients with MM who are eligible. Clinical management of patients with MM requires a
multidisciplinary approach that incorporates healthcare professionals in a number of clinical
© iStockphoto.com/dra_schwartz
settings as well as caregivers and the patient. Patients about to undergo AHSCT are generally
referred to tertiary care centers that specialize in ASCT. Pre- and post-transplantation treatments and long-term follow-up
often are managed by a community-based referring oncologist in collaboration with the transplantation team. Oncology
nurses play an integral role in the care of patients with MM in each clinical setting. This article aims to provide nontransplantation oncology nurses with guidelines for education, clinical management, and support of patients with MM
undergoing AHSCT with a primary focus on the pre- and post-transplantation period.
Teresa Miceli, RN, BSN, OCN®, is a bone marrow transplantation nurse coordinator and assistant professor of nursing in the College of Medicine in the William
von Liebig Transplant Center at the Mayo Clinic in Rochester, MN; Kathryn Lilleby, RN, is a clinical research nurse at the Fred Hutchinson Cancer Research Center
in Seattle, WA; Kimberly Noonan, RN, ANP-BC, is an adult nurse practitioner at the Dana-Farber Cancer Institute in Boston, MA; Sandra Kurtin, RN, MS, AOCN®, ANPC, is a nurse practitioner and clinical assistant professor of medicine in the Hematology/Oncology Division of the University of Arizona Cancer Center in Tucson;
Beth Faiman, MSN, APRN-BC, AOCN®, is a nurse practitioner in the Taussig Cancer Center at the Cleveland Clinic in Ohio; and Patricia A. Mangan, MSN, APRN-BC
is a nurse lead in the Department of Hematologic Malignancies and Bone Marrow and Stem Cell Transplant Programs in the Abramson Cancer Center at the
University of Pennsylvania in Philadelphia. The authors received editorial support from Alita Anderson, MD, with Eubio Medical Communications, and Joyce Divine,
PhD, with ScienceFirst LLC, in preparation of this article supported by Sanofi Oncology. The authors are fully responsible for content and editorial decisions about
this article. Kurtin is a consultant for Celgene Corporation, Novartis Pharmaceuticals, Millennium: The Takeda Oncology Company, and Onyx Pharmaceuticals.
Mangan has received honoraria from Celgene Corporation, Millennium: The Takeda Oncology Company, Onyx Pharmaceuticals, and Sanofi-Aventis. Miceli, Lilleby,
Noonan, and Faiman have no financial relationships to disclose. The content of this article has been reviewed by independent peer reviewers to ensure that it
is balanced, objective, and free from commercial bias. No financial relationships relevant to the content of this article have been disclosed by the independent
peer reviewers or editorial staff. Miceli can be reached at miceli.teresa@mayo.edu, with copy to editor at CJONEditor@ons.org. (Submitted July 2013. Revision
submitted September 2013. Accepted for publication September 8, 2013.)
Digital Object Identifier:10.1188/13.CJON.S2.13-24
H
ematopoietic stem cell transplantation (HSCT) is
an accepted treatment for selected autoimmune
and nonmalignant disorders, solid tumors, and hematologic malignancies. High-dose chemotherapy
(HDC) is used in these settings to provide intensive
cytotoxic therapy with the goal of eliminating malignant cells.
However, the toxic effects of treatment are not specific to malignant cells alone, but affect all fast-growing cells. This results in
expected side effects, most significantly bone marrow ablation
(Antin & Yolin Raley, 2009). As such, reconstitution of the bone
marrow and hematopoietic function using either autologous
(patient’s own) or allogeneic (related or unrelated donor) stem
cells is integral to the treatment process. In both procedures,
stem cells are collected prior to receiving HDC, processed,
stored, and then infused into the patient following HDC.
Without stem cell “rescue” following HDC, patients would not
recover bone marrow function, causing significant risk of mortality from life-threatening infection, bleeding, or anemia (Antin
& Yolin Raley, 2009; Bensinger, 2009; Kumar, 2009; Rodriguez,
2010b). The general process for HSCT is found in Figures 1 and
2 and further discussed in Faiman, Miceli, Noonan, and Lilleby
(2013), published on pages 33–41 of this supplement.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Overview for Nontransplantation Nurses
13
Multiple Myeloma Overview
Multiple myeloma (MM) is a malignant plasma cell disorder.
Plasma cells produce immunoglobulin, which are proteins
critical to the protective immune response. Immunoglobulins
consist of a heavy chain (IgG, IgA, IgM, IgD, IgE) and a light
chain (kappa or lambda) (Mangan, 2010). In MM, atypical
plasma cells produce excess quantities of one of these proteins,
referred to as paraproteins, monoclonal proteins, or M proteins.
The patient-specific myeloma subtype is categorized by the
involved immunoglobulin (heavy chain and light chain) (e.g.,
IgG kappa). Several factors are thought to play a role in the malignant transformation of plasma cells, including chromosome
changes, molecular characteristics, and elements that affect
the bone marrow microenvironment such as cytokine abnormalities. Many of these factors are thought to have prognostic
significance (Palumbo & Anderson, 2011).
The diagnosis of MM is based on the presence of greater
than 10% atypical plasma cells in the bone marrow, presence
of a monoclonal protein in the peripheral blood and/or urine,
and additional laboratory and clinical findings (Durie et al.,
2006; Kyle et al., 2003). The common clinical manifestations
of MM are the byproduct of excess paraprotein and its impact
on the cellular environment and organs, and include anemia,
fatigue, hypercalcemia, bone disease, bone pain, renal dysfunction, and decreased immune function (Kyle et al., 2003;
Mangan, 2010).
Pretransplantation Phase
u
Mobilization
and Collection
• Induction therapy; sideeffect monitoring
• Referral to transplantation
center for consideration of
transplantation eligibility
• Patient and caregiver
AHSCT education
• Determination of AHSCT
insurance coverage
• Arrange support.
MM is the second most common hematologic malignancy,
but is the most common indication for autologous HSCT (AHSCT)
(Pasquini & Wang, 2011). Multiple studies demonstrate a survival benefit associated with AHSCT; therefore, AHSCT is considered the standard of care for eligible patients (Attal, 1996;
Giralt et al., 2009; Kumar, 2009). Allogeneic HSCT (allo-HSCT)
differs from AHSCT in that marrow created by donor cells can
promote new immune activity in the recipient, providing a
graft-versus-host disease (or antimyeloma) effect. Allo-HSCT is
associated with high treatment-related morbidity and mortality and should only be pursued in the setting of a clinical trial
(Bensinger, 2009; Lokhorst et al., 2010). Therefore, the focus
of these guidelines will be directed toward AHSCT.
Treatment From Induction to Post-Transplantation Recovery
When designing the plan of care for a patient with MM, all
treatment options should be considered. Every newly diagnosed patient with MM, even those older than age 70 years,
should be considered a candidate for an AHSCT. Eligibility
criteria vary by institution. Referral to a transplantation center,
most often based on proximity and insurance contracting,
should be made early in the treatment process when considering AHSCT (National Comprehensive Cancer Network [NCCN],
2013; Palumbo et al., 2011). More than 150 medical institutions
Transplantation Phase
Post-collection interval:
days to months
Diagnosis
Autologous Versus Allogeneic Hematopoietic
Stem Cell Transplantation
u
Day 0
Day –2 and Day –1
Stem
Conditioning Cell Infusion
Post-Transplantation Phase
Day +17
to Day +28
Discharge
Day +100
Evaluation
u u u u
• Disease restaging and
baseline evaluation
• Patient and caregiver
AHSCT education
• Establish peripheral or
central venous access.
• Daily apheresis to AHSC
collection goal
• Day +5 to day +10
blood count nadir
• Day +10 to day +14
engraftment
• Transplantation sideeffect management
• Possible consolidation
or maintenance therapy
• Possible tandem transplantation
• Disease and treatment side-effect
monitoring and management
• Immunizations
• Disease monitoring
• Managing disease relapse
• End-of-life care
Pretransplantation phase: Weeks to months prior to transplantation. Community providers are responsible for care.
Transplantation phase: Up to eight weeks. AHSC harvesting may be included or independent of transplantation phase. Transplantation center is
responsible for care.
Post-Transplantation phase: Ongoing following discharge. Community providers are responsible for care. Day +100 evaluation takes place at the
transplantation center.
AHSCT—autologous hematopoietic stem cell transplantation
FIGURE 1. Phrases and Terminology of Transplantation
Note. Based on information from Antin & Yolin Raley, 2009; Buschell & Kapustay, 2009; Kumar, 2009; Tariman, 2010.
14
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
u Collection: Apheresis is a procedure allowing for CD34-positive cell
selection and can take 4–6 hours. The number of sessions is variable
depending on the overall goal of collection and daily stem cell yield.
Time ranges from 1–10 days. Once collected, the cells are cryopreserved in a medium of DMSO to prevent cell breakdown and may be
stored for an indefinite period of time.
u Collection
Goal: A minimum of two million CD34-positive cells
(2 x 106 CD34-positive cells per kg of recipient weight) is generally
accepted, but higher yields can result in more rapid bone marrow
recovery following HDC. With the availability of plerixafor, stem cell
harvesting has become more predictable and mobilization failure is
less frequent. Plerixafor has been shown to improve cell yield, reduce
number of apheresis sessions, and provide timely engraftment following HDC. The number of transplantations planned is physician- and
patient-dependent; therefore, the goal is variable.
u Conditioning: The preparative regimen used to treat the underlying
disease prior to AHSCT is referred to as conditioning. In multiple myeloma, melphalan is the chemotherapy agent of choice and is given as
an IV infusion. The standard dose is 200 mg/m2, but dose reductions
may be made for impaired renal function, advanced age, or comorbid
conditions.
u Engraftment: Blood count recovery, or engraftment, may be seen as
early as 10 days following AHSC infusion. Engraftment is established
when absolute neutrophils are greater than 500 cells per dl for three
consecutive days, or greater than 1,000 cells per dl for one day, and
platelets remain greater than 20,000 mm3 independent of transfusion for
at least seven days.
u Mobilization: Stimulation and movement of AHSC from the bone
marrow into the peripheral blood is known as mobilization. Methods
include using G-CSF as a single agent, with or without chemotherapy
or with or without plerixafor. This may take 1–2 weeks depending on
the approach. Venous access is necessary for apheresis, either via peripheral veins, if access is sufficient, or the placement of a dialysis-like
central venous catheter may be required.
u Stem Cell Infusion: The day of infusion, or transplantation, is commonly
referred to as day 0. The previously cryopreserved AHSCs are thawed and
infused via central venous access. The actual infusion can take as long as
an hour depending on the number of frozen bags of AHSC product. There
may be other activities as part of the infusion (i.e., hydration) that will
result in a day-long procedure. The patient will have a distinctive odor
after the infusion from the DMSO preservative.
u Transplantation Side-Effect Management: Anticipated side effects
from the HDC include alopecia, gastrointestinal toxicity (nausea, vomiting,
diarrhea, anorexia, mucositis), and bone marrow ablation (pancytopenia).
Antiemetics, hydration, pain management, antibiotics, and transfusion
support are necessary during the acute post-transplantation phase.
AHSCT—autologous hematopoietic stem cell transplantation; DMSO—dimethyl sulfoxide; G-CSF—granulocyte–colony-stimulating factor; HDC—highdose chemotherapy
FIGURE 2. Terminology of the Mobilization, Collection, and Transplantation Processes
Note. Based on information from Antin & Yolin Raley, 2009; Buschell & Kapustay, 2009; DiPersio, Stadtmauer, et al., 2009; DiPersio, Uy, et al., 2009; Gertz
et al., 2009; Giralt et al., 2009; Tariman, 2010.
exist in the United States that perform AHSCT (Blood and
Marrow Transplant Information Network, 2013; Center for
International Blood and Marrow Transplantation, 2013).
Each institution has specific protocols for pretransplantation
screening, evaluation, consultation, and treatment planning.
Transplantation eligibility is largely based on age, performance
status, and desire to undergo the procedure (see Figure 3). The
screening and approval process may take weeks to months.
Ultimately, transplantation eligibility should be determined by
a transplantation specialist.
Once a patient is diagnosed with active MM, the patient will
initiate a treatment plan that includes chemotherapy. The goal
is to effectively suppress the malignant clone and optimally
reach a complete response prior to the collection of stem cells.
Patients with MM who are eligible for transplantation should not
receive regimens containing melphalan prior to stem cell collection because it can interfere with stem cell mobilization (Cavo
et al., 2011; Giralt et al., 2009). Novel therapies (thalidomide,
lenalidomide, pomalidomide, bortezomib, and carfilzomib),
in combination with dexamethasone or standard chemotherapeutic agents, have demonstrated improved response rates
(RR) and overall survival (OS) in patients with MM and are
considered acceptable regimens prior to HSCT (Cavallo et al.,
2011; Kyle & Rajkumar, 2009; Lacy et al., 2012; NCCN, 2013;
Sonneveld, Asselbergs, et al., 2012). For those patients deemed
transplantation ineligible, melphalan and other alkylating
agents in combination with novel agents have shown significant
responses and improved OS (Palumbo et al., 2011; Rajkumar et
al., 2010; San Miguel et al., 2008). A number of clinical trials that
include initial therapy, supportive care, maintenance, or treatment of relapse in the clinical trial setting currently are being
conducted. Participation in clinical trials should be considered
at all phases of treatment when possible.
AHSC collection and transplantation is a multistep process.
The timing for stem cell collection is individualized based on
the transplantation plan. For example, a patient may collect
stem cells for storage purposes and continue with current therapy, or collect stem cells with the intent to proceed directly to
AHSCT. Patients who previously collected and stored stem cells
will proceed with HDC and AHSCT when clinically indicated
without repeating the collection process. Certain side effects
and clinical implications are common to therapies used at each
stage of the process (see Table 1). Preparing for all phases of
the transplantation process can be overwhelming for patients.
Figure 4 and Appendix A provide considerations and Internet
resources that may assist patients and caregivers.
Post-Transplantation Recovery
The post-transplantation period begins after recovery from
acute toxicity of the HDC, including blood count recovery
(Kelley, McBride, Randolph, & Leum, 2000; Williams, 2004).
This period of time has become obscured because of the many
discharge options and individualized practices at each transplantation center. Patient acuity at time of discharge is higher
than in years past, and the care of the patient with MM who has
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Overview for Nontransplantation Nurses
15
received AHSCT often is complex (Bevans, 2009). The majority
of post-transplantation care becomes the responsibility of nontransplantation practitioners and caregivers. Patients anticipate
the return home from the transplantation center, but also may
experience anxiety in the transition.
The International Myeloma Foundation Nurse Leadership
Board has compiled a summary of guidelines, recommendations, and clinical management strategies intended to optimize
the quality of life (QOL) of patients undergoing transplantation and to minimize adverse events during the immediate
post-transplantation period. The goal is to assist the community-based healthcare team, including oncology healthcare
providers, to ease the transition from transplantation center to
community, relieve anxieties, and provide information to guide
the recovery of the patient after AHSCT. While reviewing these
guidelines, note that QOL may improve over time. In several
studies, transplantation-related symptoms and QOL improved
or surpassed the pretransplantation level when measured at
6–12 months (Chao et al., 1992; Lyons et al., 2011; McQuellon
et al., 1998; Saleh & Brockopp, 2001; Schulmeister, Quiett, &
Mayer, 2005).
Yes
Active myeloma
Active Disease?
End Organ Damage?
Calcium
Renal
Anemia
Bones
Therapy indicated
Considerations for the
Nontransplantation Oncology Nurse
Discharge guidelines vary among transplantation centers, but
generally include suggested management of psychological and
physical needs of the patient. Although patients and their caregivers receive extensive education verbally and in writing prior to
their discharge from the transplantation center, the amount of
information may be overwhelming, and specific details forgotten. Therefore, ongoing educational reinforcement is essential
for both patients and their caregivers. Familiarity with the discharge procedures and post-transplantation policies at the particular transplantation center from which the patient has been
discharged will allow for reinforcement of key concepts when
healthcare providers meet with patients and their families. If not
provided to the patient at discharge, written instructions can be
requested from the transplantation center to help guide care.
Long-term survivorship issues also should be considered when
caring for the patients with MM post-transplantation. Guidelines
addressing fertility, sexuality, renal aspects, bone health, health
maintenance, and mobility and safety can be found in a previous
supplement to the Clinical Journal of Oncology Nursing from the
International Myeloma Foundation Nurse Leadership Board (Bilotti et al., 2011; Bilotti, Gleason,
No
& McNeill, 2011; Faiman, Mangan,
Spong, & Tariman, 2011; Miceli,
Colson, Faiman, Miller, & TariSmoldering myeloma
man, 2011; Richards, Bertolotti,
Doss, & McCullagh, 2011; Rome,
Jenkins, & Lilleby, 2011).
No therapy indicated
Post-Transplantation Needs
Yes
Transplantation Eligible
Induction Regimens
•BorDex
•Bor/Cy/Dex
•Bor/Len/Dex
•Car/Len/Dex
•Bor/Dox/Dex
•Len/Dex
•Bor/Thal/Dex
Transplantation
Candidate?
Considerations
• Age
• Performance status
• Comorbidity
• Prognostic factors
• Patient preference
• Insurance coverage
No
Non-Transplantation Eligible
Induction Regimens
• Mel/Pred plus Bor, Len, or Thal
• Bor/Len/Dex
• Len/low Dex
• Cy/Bor/Dex
Consideration
Stem cell harvest after 4–6 cycles
Autologous hematopoietic
stem cell transplantation
Consideration
Continued or maintenance therapy
Bor—bortezomib; Car—carfilzomib; Cy—cyclophosphamide; Dex—dexamethasone; Dox—doxorubicin;
Len—lenalidomide; Mel—melphalan; Pred—prednisone; Thal—thalidomide
FIGURE 3. Treatment Algorithm for Newly Diagnosed Multiple Myeloma
Note. Based on information from Mikhael et al., 2013; National Comprehensive Cancer Network, 2013.
16
The psychological impact of
AHSCT should not be overlooked.
Patients often describe the “let
down” feeling after working hard
before and during the transplantation, and many reflect on the
events leading up to the transplantation and the details of the
transplantation after being discharged. Transplantation recovery
can be associated with physical
setbacks as well as social strain
on the caregiver and family. In
fact, post-transplantation psychological issues may present greater
challenges than the medical needs
of the patient for the communitybased healthcare team (Cooke,
Gemmill, Kravits, & Grant, 2009).
The estimated rate of depression following stem cell transplantation ranges from 25%–50%. Depression affects physical health,
can increase symptom-related
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
distress, decrease survival, and has been associated with a higher incidence of suicide. Early identification of the symptoms of
depression will allow the post-transplantation healthcare team
to intervene early and refer the patient for more intensive services, such as psychiatric or social services and referral back
to the transplantation center. In some cases, antidepressive
medications may be necessary. Caregivers and family members
should be made aware of the frequency of post-transplantation
depression, signs and symptoms they should report, and how
best to contact the appropriate healthcare provider (Cooke et
al., 2009).
Post-Transplantation Symptom Management
Symptom management is vital for patients after stem cell
transplantation. Persistent symptoms of HDC-related toxicity are
common even after the patient has returned home (see Table 2).
TABLE 1. Common Multiple Myeloma Therapies, Side Effects, and Clinical Implications
Potential Side
Effects and Toxicities
Drug, Class, Route
Clinical Implication
Additional Informationa
Myeloma Therapy Medications
Bortezomib
Proteasome inhibitor
IV or SQ administration
MS, PN, diarrhea or constipation, irritation or erythema at
injection site; VZV activation
Monitor CBC, monitor PN symptoms,
bowel management; use antiviral
prophylaxis
Used as combination therapy or single agent;
consider SQ administration to reduce PN
Carfilzomib
Proteasome inhibitor
IV administration
Fatigue, anemia, thrombocytopenia, nausea, diarrhea, dyspnea, and fever
Monitor CBC and liver function tests.
Prevent tumor lysis syndrome via PO
and IV hydration; premedicate with
dexamethasone in the first cycle
Approved for patients who have had two or
more prior therapies, including bortezomib and
an immunomodulatory agent
Lenalidomide
Immunomodulator
Oral administration
MS, thromboembolic event
when combined with steroids,
and skin rash
Monitor CBC, bowel management,
dose adjust for renal impairment;
thromboembolic event prophylaxis
Used as combination therapy or as single-agent
maintenance; hold for two weeks prior to
autologous hematopoietic stem cell collection
Melphalan
Alkylator
IV or oral administration
For conventional doses, MS; for
high doses, myeloablation, GI
disturbance, and alopecia
Monitor CBC
Should be avoided prior to autologous hematopoietic stem cell collection; long-term use
can cause myelodysplasia
Pomalidomide
Immunomodulator
Oral administration
MS and thromboembolic event
Monitor CBC, bowel management;
thromboembolic event prophylaxis
Approved for patients who have had two or
more prior therapies, including bortezomib and
an immunomodulatory agent
Thalidomide
Immunomodulator
Oral administration
MS, thromboembolic event
when combined with steroids,
PN, and constipation
Monitor CBC, bowel management;
thromboembolic event prophylaxis
Used in combination with dexamethasone
Supportive Care Medications
G-CSF/filgrastim
Cytokine
SQ administration
Joint and bone pain; increased
white blood cells
Assess and medicate for pain.
Management of neutropenia; autologous hematopoietic stem cell mobilization
Pamidronate
Bisphosphonate
IV administration
Initial phase reaction, hyperalbuminuria, and osteonecrosis
of the jaw
Dental evaluation prior to start (if
possible), regular dental cleaning;
avoid invasive dental procedure
while receiving treatment
Inhibition of bone resorption and associated
hypercalcemia. See ASCO and IMWG guidelines for duration of use. May be held during
transplantation and resumed after.
Plerixafor
Chemokine inhibitor
SQ administration
Diarrhea and erythema at
injection site
Bowel management
Used in combination with G-CSF for stem cell
mobilization
Zoledronic acid
Bisphosphonate
IV administration
Initial phase reaction, hyperalbuminuria, and osteonecrosis
of the jaw
Dental evaluation prior to start (if
possible), regular dental cleaning;
avoid invasive dental procedure
while receiving treatment
Inhibition of bone resorption and associated
hypercalcemia. See ASCO and IMWG guidelines for duration of use. May be held during
transplantation and resumed after.
a
See package insert for a complete listing of possible side effects. Practical use of medications may differ from U.S. Food and Drug Administrationapproved indications and is done at the discretion of a licensed provider.
ASCO—American Society of Clinical Oncology; CBC—complete blood count; G-CSF—granulocyte–colony-stimulating factor; GI—gastrointestinal;
IMWG—International Myeloma Working Group; MS—myelosuppression; PN—peripheral neuropathy; SQ—subcutaneous; VZV—varicella zoster virus
Note. Based on information from Amgen Inc., 2013; Bertolotti et al., 2008; Bilotti, Gleason, et al., 2011; Bristol-Myers Squibb, 2005; Celgene Corporation, 2013a, 2013b, 2013c; Genzyme: A Sanofi Company, 2010; GlaxoSmithKline, 2008; Kumar, 2009; Millennium: The Takeda Oncology Company, 2012;
Novartis Pharmaceuticals, 2012a, 2012b; Onyx Pharmaceuticals, 2012.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Overview for Nontransplantation Nurses
17
Post-Transplantation Infection Risk and Prevention
Post-transplantation infection is a major cause of morbidity
and mortality. Although the patient’s white blood cell count and
absolute neutrophil count may be within the normal range, the
cells are functionally abnormal, placing the patient at increased
risk for infection. In addition, continued physical weakness and
malnutrition make recovery from a new infection difficult. Therefore, prophylactic antibiotics to prevent post-transplantation
infections, such as invasive pneumococcal infection and pneumocystis pneumonia, are recommended for as long as one year following AHSCT (Tomblyn et al., 2009). Early detection and prompt
intervention for infection is essential in caring for patients with
MM (Palumbo et al., 2012). Careful assessment of the skin, lungs,
gastrointestinal, renal, and skeletal systems are needed in identifying infection. Vital signs should be monitored at each clinic visit
and patients should monitor their own vital signs as instructed by
their care provider. Potential post-transplantation infections and
preventions are listed in Table 3.
Frequent and meticulous hand washing by the patients and
those they come in contact with is very important to prevent the
transfer of infection. Many transplantation centers recommend
that patients wear a mask when coming into a clinic or hospital
for appointments. Patients may be advised to avoid public places
such as restaurants, movies, or shopping malls. The suspension
of these precautions will vary by individual centers and should
be discussed in detail with the transplantation center.
u American Cancer Society
Information on disease types and available support
www.cancer.org
u Be the Match: National Marrow Donor Program
Transplantation-related information for patients and caregivers
www.marrow.org
u BMT Information Network
Transplantation-related information for patients and caregivers
www.BMTInfoNet.org
u Caring Bridge
A site to create a personal blog or journal that can be shared with
family and friends
www.caringbridge.org
u International Myeloma Foundation
Information about myeloma, research, and available support
www.myeloma.org
u Leukemia and Lymphoma Society
Information on disease types and available support
www.lls.org
u Multiple Myeloma Research Foundation
Information about myeloma, research and available support
www.themmrf.org
u National Bone Marrow Transplant Link
Transplantation-related information for patients and caregivers
www.nbmtlink.org
u National Cancer Institute
Information on disease types and research
www.cancer.gov
Note. Website addresses and content can change; therefore, the information should be reviewed before sharing with patients.
FIGURE 4. Web Resources
18
Implications for Practice
u
Include healthcare professionals from a number of clinical settings to best address the multidisciplinary approach required
to manage multiple myeloma.
u
Become familiar with the autologous hematopoietic stem cell
transplantation process, as it remains an important treatment
option for multiple myeloma.
u
Incorporate guidelines for post-transplantation management
in the community setting to promote quality of life and
improve survival for patients.
Recommendations concerning personal hygiene, home maintenance, and cleanliness also may be provided by the transplantation center to further reduce the risk of infection. Guidelines for
laundering clothes and housekeeping, particularly facilities used
by the patient, are commonly provided. Specific policies regarding personal hygiene also are often recommended. It must be kept
in mind that the patient may not be able to perform some of these
duties independently in the first months following HSCT, emphasizing the need to include caregivers in the education process
(Antin & Yolin Raley, 2009). The role of caregivers in the recovery
of patients with HSCT is discussed in greater detail by Kurtin, Lilleby, and Spong (2013) on pages 25–32 of this supplement.
Because of the risk of food-borne infection, specific nutritional
and dietary guidelines may be mandated by the transplantation
center. Nutritional recommendations and restrictions may begin
at the start of HDC and continue after discharge. In general, the
Advisory Committee on Immune Practices recommends foods
that have been refrigerated, pasteurized, or well-cooked for
patients during the post-transplantation period (Antin & Yolin
Raley, 2009; Tomblyn et al., 2009).
Smoking tobacco is prohibited after an AHSCT for many
reasons. People who smoke are at increased risk for developing
pneumonia as well as pulmonary and cardiovascular toxicity
related to AHSCT. Marijuana use is prohibited because of the
heightened risk of fungal infection associated with inhalation.
Alcohol consumption also is restricted because of its potential
effect on the liver, platelets, and immune function (Sipsas &
Kontoyiannis, 2008; Tichelli et al., 2008; Versteeg, Slot, van der
Velden, & van der Weijden, 2008).
Post-Transplantation Immunizations
The transplantation process results in a loss of T and B lymphocytes which, in turn, causes loss of immune memory. Immune
memory is shaped by the culmination of exposure to infectious
agents, environmental antigens, and vaccines during a person’s
lifetime (Kroger, Sumaya, Pickering, & Atkinson, 2011; Stadtmauer et al., 2011). Therefore, patients require reimmunization.
Post-transplantation immunizations vary by institution. Based
on the Centers for Disease Control and Prevention and Advisory
Committee on Immune Practices recommendations, non-live
vaccines may be administered as early as three months posttransplantation. Live-attenuated vaccines may be administered
two years following transplantation in immune-competent
people (Tomblyn et al., 2009). An example of an immunization
schedule can be found in Table 4.
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
TABLE 2. Post-Transplantation Symptoms, Clinical Findings, and Management Strategies
Symptom
Clinical Findings and Risk Factors
Management Strategies
Anorexia
Weight loss, taste changes, change in performance
status, fatigue, nausea and vomiting, and diarrhea
Review medications for possible source.
Medical nutritional therapies: oral nutritional supplements, IV hydration
Small frequent meals, calorie counts, weekly weight, nutritional consult
Reinforce improvement with time.
Adjust medications as needed.
Treat underlying cause (e.g., medication for nausea and vomiting).
Anxiety and
depression
Fatigue, exhaustion, difficulty sleeping, difficulty
concentrating, restlessness, irritability and impatience, recurrent thoughts of diagnosis and treatment, and anorexia
Listen to and validate concerns.
Referral to social services, psychiatry, and support groups
Pharmacologic: anti-anxiety medication, antidepressants
Complementary and alternative medicine therapy: relaxation therapy, mild exercise such as walking
Diarrhea
Increased frequency of bowel movements, abdominal cramps, dehydration, and decrease in weight
Review medications for possible source (i.e., antibiotics, narcotic withdrawal).
Electrolyte evaluation
Stool sample for enteric pathogens (i.e. Clostridium difficile)
Anti-diarrheal medication
Appropriate fluid and electrolyte replacement
Adjust diet for food sensitivities: milk products, certain spicy foods, nutritional
supplements, fatty foods, chocolate
Antibiotics as needed; adjust medications as needed
Fatigue
Decrease in energy, inability to complete tasks,
insomnia or hypersomnia, not feeling rested after
sleeping at night, and generalized weakness
Review medications that may cause fatigue.
Assess for anemia.
Mild exercise such as walking
Potentially decrease or discontinue medications that cause fatigue.
Counsel patient on sleep hygiene, such as minimizing napping or staying in bed
throughout the day.
Erythropoietin medication if indicated and after obtaining written consent
Red blood cell transfusion, if needed
Fever
Diarrhea, muscle weakness, fatigue, confusion, and
seizures
Panculture, chest x-ray, and CBC with differential and platelets
Prophylactic antibiotics if neutropenic; therapeutic antibiotics if culture positive
Acetaminophen, IV hydration, symptom management
Monitor for fever greater than 101.3°F (and lower temperatures if patients are
not feeling well), blood pressure declining from baseline and tachycardia
Nausea and
vomiting
Anorexia, nausea and vomiting, weight loss, and
diminished skin turgor
Quantify episodes of emesis.
Assess fluid and electrolyte status.
Review medications for antiemetics and medications that may cause nausea and
vomiting.
Adjust medications if possible and as needed.
IV or oral hydration and replace electrolytes as needed
Pain
Assess for new or existing pain symptoms, current
pain medication, assess for pain related to infection, and assess for symptoms of depression or
anxiety
Appropriate pain medication regimen: long-acting pain medication together
with breakthrough pain medication, doses titrated to effectiveness
Consider imaging for source of new or worsening pain
Consult with appropriate specialty, if indicated
PN
Paresthesias, impaired proprioception, pain, and
sensory deficits; patients at increased risk: those
with a history of diabetes, alcohol use, vitamin B12
deficiency, paraneoplastic syndrome, and vascular
insufficiency
Baseline assessment of PN, description of PN symptoms, previous chemotherapy,
current medications, neurologic examination including sensory and motor use
Safety evaluation and nutritional assessment
Treatment of neuropathic pain: medications, acupuncture, massage, medications
Promote safety with use of assistive devices: cane, orthotics, wheelchair.
Physical therapy and activity; massage
Thrombosis
(DVT or PE)
Painful, swollen and erythematous extremity (most
often lower extremity), shortness of breath, tachycardia, chest pain, and HTN; patients at increased
risk: those with obesity, diabetes, cardiovascular
disease, HTN, hyperlipidemia, immunomodulatory
agents with concurrent high-dose steroids, anthracyclines, ESAs, hospitalizations, and immobility
Prevention: thromboprophylaxis for all patients at risk
Full therapeutic anticoagulation for any patients with more than two risk factors
If DVT or PE is suspected: Doppler ultrasound of suspected extremity
High-resolution chest CT with PE protocol if PE is suspected
Medication to treat thrombosis: low molecular weight heparin, warfarin, and
alternative anticoagulants
Consult with coagulation specialist if appropriate.
CBC—complete blood count; CT—computed tomography; DVT—deep vein thrombosis; ESA—erythropoietin-stimulating agent; HTN—hypertension;
PE—pulmonary embolus; PN—peripheral neuropathy
Note. Based on information from Antin & Yolin Raley, 2008; Eaton & Tipton, 2010; Rodriguez, 2010a.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Overview for Nontransplantation Nurses
19
Post-Transplantation Medication Considerations
Polypharmacy during transplantation is common and can be
confusing. Therefore, many transplantation teams will provide
patients and their families with a medication chart to help track
and maintain the dose and the administration of scheduled and
“as needed” medications. Pretransplantation and transplantationspecific medications are added, discontinued, and adjusted frequently according to the patient’s needs during the acute care
phase of the transplantation. Hypertension and hyperglycemic
management regimens, in particular, often require modifications
during the transplantation process. A list of discharge medications should be provided to the patient as well as to the discharge
facility or homecare agency and the patient’s referring oncologist
involved in the patient’s care. Patients may be restricted from
taking certain over-the-counter medications such as nonsteroidal
anti-inflammatory drugs and supplements because of drug interactions, organ toxicity, or interference with therapy. Medications
must be taken as prescribed and medication changes should be
discussed with the staff at the transplantation center.
Disease Management Following Autologous
Hematopoietic Stem Cell Transplantation
Although AHSCT remains an important treatment strategy
for patients with MM, relapse of MM is inevitable for the majority of patients. The timing is unpredictable and relapse can
occur at any time following AHSCT, ranging from months to
years. Those considered at high risk based on stage of disease
and cytogenetics are at greater risk of early relapse (Mikhael
et al., 2013; Palumbo & Cavallo, 2012). Providing patients with
the clear message is important so that when progression does
occur, they understand that it does not necessarily indicate
end of life, but, rather, a time for change in therapy. Determining the optimal time to next therapy remains a controversial
issue following AHSCT, and several studies are ongoing. Data
TABLE 3. Common Transplantation Infections and Prevention
Infection
Type of Infection
Prevention
Bordetella pertussis
(whooping cough)
Community-acquired bacterial respiratory
infection
If exposed, prevention and treatment available (azithromycin or SMX/
TMP)
If hospitalized, proper precautions should be taken to avoid transmitting to others. A cellular vaccine is recommended.
Community respiratory
viruses: RSV, influenza,
adenovirus, and parainfluenza
Viral infections that can progress to bronchitis
or pneumonia
RSV is more common in infants, but can be
seen in older adults and ICHs.
Influenza accounts for about 20% of respiratory viral infection in patients who receive a
transplantation.
Adenovirus may manifest as a diarrheal illness.
Handwashing; ICHs should wear a mask, clean hard surfaces with
anti-infective wash, and avoid crowds and people with respiratory
symptoms.
If hospitalized, proper precautions should be taken to avoid transmitting to others.
Antiviral medication may be available. Inactivated influenza vaccine
should be administered to the patient and direct caregivers unless
contraindicated.
Do not use the live inhaled version. May begin as early as 3–6
months post-transplantation and every year of life.
Pneumocystis carinii pneumonia (renamed as PJP)
Protozoal infection that can develop in ICHs.
ICHs and patients with AHSCT may develop PJP
if prophylaxis is not provided; can occur early
after transplantation, particularly if the patient
has been heavily treated beforehand.
SMX/TMP, atovaquone, dapsone, or aerosolized pentamidine, depending on allergy profile
Prophylaxis for 3–6 months following AHSCT
Streptococcus pneumonia
or invasive pneumococcal
infection
A gram-positive encapsulated organism that
can cause sudden and serious systemic infection in patients following AHSCT.
Considered a late transplantation complication
and is common in patients with multiple myeloma because of decreased humoral immunity
Penicillin or doxycycline, depending on allergy profile
Prophylaxis for 12 months following AHSCT, until revaccinated
Pneumococcal vaccine should be administered as a 7-valent or
23-valent vaccine as early as 3–6 months post-transplantation.
Viridans streptococci
Organism found commonly in the oral cavity
Greatest concern during times of oral mucositis
Quinolone therapy for neutropenic state longer than seven days.
VZV (shingles)
Primary infection, commonly known as chicken
pox. VZV persists in the sensory nerve ganglia.
Reactivation is common in older adults or ICHs.
Acyclovir or valacyclovir therapy for one year or while on active treatment
Also prevents herpes simplex virus, type I and II
The shingles vaccine is a live virus and currently not recommended for
patients with multiple myeloma.
AHSCT—autologous hematopoietic stem cell transplantation; ICH—immunocompromised host; PJP—Pneumocystis jiroveci pneumonia; RSV—respiratory syncytial virus; SMX/TMP—sulfamethoxazole/trimethoprim; VZV—varicella zoster virus
Note. Schedule and use vary between transplantation centers.
Note. No live vaccines should be given in the first year following transplantation.
Note. Based on information from Antin & Yolin Raley, 2009; Centers for Disease Control and Prevention, 2012; Cordonnier et al., 2010; Stadtmauer et
al., 2011; Tomblyn et al., 2009.
20
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
TABLE 4. Post-Transplantation Immunization Schedule
Organism
Vaccine
Time
Post-HSCT
to Initiate Vaccine
Dose and Route
Comments
Inactivated Vaccines
Pneumococcal
PCV7/
PPSV23
3–6 months
0.5 ml IM or SQ
Can be given six months post-transplantation
Pertussis, tetanus, diptheria
DTAP
6–12 months
0.5 m. IM
Can be given six months post-transplantation
Haemophilus influenzae
type B
HIB
6–12 months
0.5 ml IM
Can be given six months post-transplantation
Hepatitis B
–
6–12 months
1 ml IM
Administer to patients who are hepatitis B virus negative.
Meningococcus
–
6–12 months
0.5 ml SQ
Recommended in areas with an increase in meningococcus
Influenza
–
4–6 months
0.5 ml IM (the
nasal version is live
and, therefore, not
recommended)
Give annually as available in the autumn months. May
administer four months post-transplantation; however, two
doses of the vaccine are suggested.
0.5 ml SQ
MMR should not be given if the patient is immunosuppressed.
Live Virus Vaccines
Measles, mumps, and
rubella
MMR
24 months
Varicella zoster virus
(shingles)
Zoster
vaccine
Not currently
recommended.
Clinical trials are
ongoing.
–
Not currently recommended; inactivated version is under
investigation. Prevention with antiviral medication is recommended.
HSCT—hematopoietic stem cell transplantation; IM—intramuscular; SQ—subcutaneous
Note. Based on information from Cordonnier et al., 2010; Kroger et al., 2011; Ljungman et al., 2009; Tomblyn et al., 2009.
regarding the use of maintenance therapy following HSCT for
MM continue to be reported. Attal et al. (2012) reported improvement in progression-free survival (PFS) following AHSCT
using lenalidomide as maintenance therapy but no increase in
OS. McCarthy et al. (2012) also reported an increase in PFS as
well as a longer OS. Bortezomib can be used as maintenance posttransplantation as well, and may be associated with improvement
in PFS (Sonneveld, Schmidt-Wolf, et al., 2012).
Conclusion
Care of the patient following AHSCT is complex, however,
expected side effects of HDC usually are manageable. Although
consistent objectives and goals are in place for AHSCT recipients, care must be individualized based on pretransplantation
treatment toxicities and transplantation-related side effects.
Community oncology professionals play a critical role in the
collaborative management of the patient with MM throughout
the treatment continuum. Consistent communication among
the patient, the referring center, and the transplantation center
is vital to ensure all testing, insurance approval, and support
services are in place prior to starting the transplantation process.
Post-transplantation guidelines are not standardized, and recommendations for post-transplantation care vary between transplantation centers. These factors add to the challenge of caring
for the transplantation patient in a community-based setting.
All providers should assist in supporting the patient and family members through the transplantation journey. Discharge
is an exciting time for the patient, but also can be physically
challenging and emotionally overwhelming. Community providers are instrumental in monitoring and managing posttransplantation concerns. Understanding the AHSCT rationale,
process, and needs of the patient post-transplantation will improve the QOL for the patient undergoing transplantation and
impact OS. Maintaining a collaborative management approach
with consistent communication between the transplantation
center and community healthcare provider team will improve
overall outcomes for patients undergoing transplantation.
The authors gratefully acknowledge Brian G.M. Durie, MD,
Robert A. Kyle, MD, and Diane P. Moran, RN, MA, EdM, senior
vice president of strategic planning at the International Myeloma
Foundation, for their critical review of the manuscript.
References
Amgen Inc. (2013). Neupogen® ( filgrastim) [Package insert].
Retrieved from http://pi.amgen.com/united_states/neupogen/
neupogen_pi_hcp_english.pdf
Antin, J., & Yolin Raley, D. (2009). Infectious disease, stem cell
sources. In J. Antin & D. Yolin Raley (Eds.), Manual of stem cell
and bone marrow transplantation (pp. 100–120). Cambridge,
MA: Cambridge University Press.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Overview for Nontransplantation Nurses
21
Attal, M. (1996). A prospective, randomized trial of autologous bone
marrow transplantation and chemotherapy in multiple myeloma.
New England Journal of Medicine, 335, 91–97. doi:10.1056/
NEJM199607113350204
Attal, M., Lauwers-Cances, V., Marit, G., Caillot, D., Moreau, P.,
Facon, T., . . . Harousseau, J.L. (2012). Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. New
England Journal of Medicine, 366, 1782–1791. doi:10.1056/
NEJMoa1114138
Bensinger, W.I. (2009). Role of autologous and allogeneic stem cell
transplantation in myeloma. Leukemia, 23, 442–448. doi:10.1038/
leu.2008.396
Bertolotti, P., Bilotti, E., Colson, K., Curran, K., Doss, D., Faiman,
B., . . . Westphal, J. (2008). Management of side effects of novel
therapies for multiple myeloma: Consensus statements developed by the International Myeloma Foundation’s Nurse Leadership Board. Clinical Journal of Oncology Nursing, 12(3, Suppl.),
9–12. doi:10.1188/08.CJON.S1.9-12
Bevans, M. (2009). Advances in stem cell transplantation. Seminars in
Oncology Nursing, 25, 120–128. doi: 10.1016/j.soncn.2009.03.006
Bilotti, E., Faiman, B.M., Richards, T.A., Tariman, J.D. Miceli, T.S.,
Rome, S.I., & the International Myeloma Foundation Nurse Leadership Board. (2011). Survivorship care guidelines for patients
living with multiple myeloma: Consensus statements of the International Myeloma Foundation Nurse Leadership Board. Clinical
Journal of Oncology Nursing, 15(Suppl., 1), 5–8. doi:10.1188/11
.S1.CJON.5-8
Bilotti, E., Gleason, C.L., & McNeill, A. (2011). Routine health maintenance in patients living with multiple myeloma: Survivorship
care plan of the International Myeloma Foundation Nurse Leadership Board. Clinical Journal of Oncology Nursing, 15(Suppl.,
1), 25–40. doi:10.1188/11.S1.CJON.25-40
Blood and Marrow Transplant Information Network. (2013). Transplant center search form. Retrieved from http://www.bmtinfonet
.org/centersearch?tid=613&treatment=All&field_addr_state_value
_many_to_one=All&field_tc_unit_value=All
Bristol-Myers Squibb. (2005). Cytoxan® (cyclophosphamide tablets) [Package insert]. Retrieved from http://packageinserts
.bms.com/pi/pi_cytoxan.pdf
Buschell, P.C., & Kapustay, P.M. (Eds.). (2009). Stem cell transplantation. A clinical textbook. Pittsburgh, PA: Oncology Nursing Society.
Cavallo, F., Bringhen, S., Milone, G., Ben-Yehuda, D., Nagler, A., Calabrese, E., & Palumbo, A. (2011). Stem cell mobilization in patients
with newly diagnosed multiple myeloma after lenalidomide induction therapy. Leukemia, 25, 1627–1631. doi:10.1038/leu.2011.131
Cavo, M., Rajkumar, S.V., Palumbo, A., Moreau, P., Orlowski, R.,
Bladé, J., . . . International Myeloma Working Group. (2011).
International Myeloma Working Group consensus approach to
the treatment of multiple myeloma patients who are candidates
for autologous stem cell transplantation. Blood, 117, 6063–6073.
doi:10.1182/blood-2011-02-297325
Celgene Corporation. (2013a). Pomalyst® (pomalidomide) [Prescribing information]. Retrieved from http://www.pomalyst.com/
docs/prescribing_information.pdf
Celgene Corporation. (2013b). Revlimid® (lenalidomide) [Prescribing information]. Retrieved from http://www.revlimid.com/
pdf/MCL_PI.pdf
Celgene Corporation. (2013c). Thalomid® (thalidomide) [Prescribing information]. Retrieved from http://www.thalomid.com/
pdf/Thalomid_PI.pdf
Center for International Blood and Marrow Transplantation. (2013).
22
Participating transplant centers. Retrieved from http://www
.cibmtr.org/about/WhoWeAre/Centers/Pages/index.aspx
Centers for Disease Control and Prevention. (2012). Respiratory
syncytial virus infection. Retrieved from http://www.cdc.gov/rsv
Chao, N.J., Tierney, D.K., Bloom, J.R., Long, G.D., Barr, T.A., Stallbaum, B.A., . . . Blume, K.G. (1992). Dynamic assessment of
quality of life after autologous bone marrow transplantation.
Blood, 80, 825–830.
Cooke, L., Gemmill, R., Kravits, K., & Grant, M. (2009). Psychological issues of stem cell transplant. Seminars in Oncology Nursing,
25, 139–150.
Cordonnier, C., Labopin, M., Chesnel, V., Ribaud, P., Cámara Rde,
L., Martino, R., . . . Ljungman, P. (2010). Immune response to
the 23-valent polysaccharide pneumococcal vaccine after the
7-valent conjugate vaccine in allogeneic stem cell transplant
recipients: Results from the EBMT IDWOPO1 trial. Vaccine, 28,
2730–2734. doi:10.1016/j.vaccine.2010.01.025
DiPersio, J.F., Stadtmauer, E.A., Nademanee, A., Micallef, I.N., Stiff,
P.J., Kaufman, J.L., . . . Calandra, G. (2009). Plerixafor and G-CSF
versus placebo and G-CSF to mobilize hematopoietic stem cells
for autologous stem cell transplantation in patients with multiple
myeloma. Blood, 113, 5720–5726.
DiPersio, J.F., Uy, G.L., Yasothan, U., & Kirkpatrick, P. (2009).
Plerixafor. Nature Reviews. Drug Discovery, 8, 105–107.
Durie, B.G., Harousseau, J.L., Miguel, J.S., Bladé, J., Barlogie, B.,
Anderson, K., . . . Rajkumar, S.V. (2006). International uniform response criteria for multiple myeloma. Leukemia, 20, 1467–1473.
doi:10.1038/sj.leu.2404284
Eaton, L.E., & Tipton, J.M. (2010). A guide to oncology symptom
management. Pittsburgh, PA: Oncology Nursing Society.
Faiman, B., Miceli, T., Noonan, K., & Lilleby, K. (2013). Clinical updates in blood and marrow transplantation in multiple myeloma.
Clinical Journal of Oncology Nursing, 17(Suppl., 2), 33–41.
Faiman, B.M., Mangan, P., Spong, J., & Tariman, J.D. (2011). Renal
complications in multiple myeloma and related disorders: Survivorship care plan of the International Myeloma Foundation
Nurse Leadership Board. Clinical Journal of Oncology Nursing,
15(Suppl., 1), 66–76. doi:10.1188/11.CJON.S1.66-76
Genzyme: A Sanofi Company. (2010). Mozobil® (plerixafor injection)
[Prescribing information]. Retrieved from http://www.mozobil
.com/document/Package_Insert.pdf
Gertz, M.A., Kumar, S.K., Lacy, M.Q., Dispenzieri, A., Hayman, S.R.,
Buadi, F.K., . . . Litzow, M.R. (2009). Comparison of high-dose CY
and growth factor with growth factor alone for mobilization of
stem cells for transplantation in patients with multiple myeloma.
Bone Marrow Transplant, 43, 619–625.
GlaxoSmithKline. (2008). Alkeran® (melphalan hydrochloride)
[Prescribing information]. Retrieved from http://dailymed.nlm
.nih.gov/dailymed/archives/fdaDrugInfo.cfm?archiveid=13952
Giralt, S., Stadtmauer, E.A., Harousseau, J.L., Palumbo, A., Bensinger,
W., Comenzo, R.L., . . . Durie, B.G. (2009). International Myeloma
Working Group (IMWG) consensus statement and guidelines
regarding the current status of stem cell collection and high-dose
therapy for multiple myeloma and the role of plerixafor (AMD
3100). Leukemia, 23, 1904–1912. doi:10.1038/leu.2009.127
Kapustay, P.M., & Buchsel, P.C. (2009). Process, complications, and
management of peripheral stem cell transplantation. In P.C. Buchsel & P.M. Kapustay (Eds.), Stem cell transplantation: A clinical
textbook (pp. 5.1–5.28). Pittsburgh, PA: Oncology Nursing Society.
Kelley, C.H., McBride, L.H., Randolph, S.R., & Leum, E. (2000). Home
care of peripheral blood stem cell transplantation recipients. In
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
P.C. Buchsel & P.M. Kapustay (Eds.), Stem cell transplantation:
A clinical textbook (pp. 131–136). Pittsburgh, PA: Oncology
Nursing Society.
Kroger, A., Sumaya, C., Pickering, L., & Atkinson, W. (2011). General recommendations on immunization: Recommendations of
the Advisory Committee on Immunization Practices (ACIP).
Morbidity and Mortality Weekly Report, 60(2), 1–64.
Kumar, S. (2009). Stem cell transplantation for multiple myeloma.
Current Opinions in Oncology, 21, 162–170. doi:10.1097/CCO
.0b013e328324bc04
Kurtin, S.A., Lilleby, K., & Spong, J. (2013). Caregivers of multiple
myeloma survivors. Clinical Journal of Oncology Nursing,
17(Suppl., 2), 25–32.
Kyle, R.A., Gertz, M.A., Witzig, T.E., Lust, J.A., Lacy, M.Q., Dispenzieri, A., . . . Greipp, P.R. (2003). Review of 1,027 patients with
newly diagnosed multiple myeloma. Mayo Clinic Proceedings,
78, 21–33. doi:10.4065/78.1.21
Kyle, R.A., & Rajkumar, S.V. (2009). Criteria for diagnosis, staging,
risk stratification, and response assessment of multiple myeloma.
Leukemia, 23, 3–9. doi:10.1038/leu.2008.291
Lacy, M., Kumar, S., LaPlant, B., Laumann, K., Gertz, M., & Hayman,
S. (2012). Pomalidomide plus low-dose dexamethasone (pom/
dex) in relapsed myeloma: Long term follow up and factors predicting outcome in 345 patients [Abstract 201]. Blood, 120, 4176.
Ljungman, P., Cordonnier, C., Englund, J., Machado, C.M., Storek, J.,
Small, T., . . . Centers for Disease Control and Prevention. (2009).
Vaccination of hematopoietic cell transplant recipients. Bone
Marrow Transplantation, 44, 521–526. doi:10.1038/bmt.2009.263
Lokhorst, H., Einsele, H., Vesole, D., Bruno, B., Miguel, J., PérezSimon, J.A., . . . Bensinger, W. (2010). International Myeloma
Working Group consensus statement regarding the current status of allogeneic stem-cell transplantation for multiple myeloma.
Journal of Clinical Oncology, 28, 4521–4530.
Lyons, D.K., Hull, J.G., Root, L.D., Kimtis, E., Shaal, A.D., Sterans,
D.M., . . . Ahles, T.A. (2011). A pilot study of activity engagement
in the first six months after stem cell transplantation. Oncology
Nursing Forum, 38, 75–83. doi:10.1188/11.ONF.75-83
Mangan, P. (2010). Patient assessment. In J.D. Tariman (Ed.), Multiple myeloma: A textbook for nurses (pp. 55–75). Pittsburgh,
PA: Oncology Nursing Society.
McCarthy, P.L., Owzar, K., Hofmeister, C.C., Hurd, D.D., Hassoun, H.,
Richardson, P.G., . . . Linker, C. (2012). Lenalidomide after stemcell transplantation for multiple myeloma. New England Journal
of Medicine, 366, 1770–1781. doi:10.1056/NEJMoa 1114083
McQuellon, R.P., Russell, G.B., Rambo, T.D., Craven, B.L., Radford,
J., Perry, J.J., . . . Hurd, D.D. (1998). Quality of life and psychological distress of bone marrow transplant recipients: The time
trajectory to recovery over the first year. Bone Marrow Transplantation, 21, 477–486. doi:10.1038/sj.bmt.1701115
Miceli, T.S., Colson, K., Faiman, B.M., Miller, K., & Tariman, J.D.
(2011). Maintaining bone health in patients with multiple myeloma: Survivorship care plan of the International Myeloma
Foundation Nurse Leadership Board. Clinical Journal of Oncology Nursing, 15(Suppl., 1), 9–23. doi:10.1188/11.S1.CJON.9-23
Mikhael, J.R., Dingli, D., Roy, V., Reeder, C.B., Buadi, F.K., Hayman,
S.R., . . . Lacy, M.Q. (2013). Management of newly diagnosed
symptomatic multiple myeloma: Updated Mayo Stratification of
Myeloma and Risk-Adapted Therapy (mSMART) consensus guidelines 2013. Mayo Clinical Proceedings, 88, 360–376.
Millennium: The Takeda Oncology Company. (2012). Velcade®
(bortezomib) [Prescribing information]. Retrieved from http://
w w w.velcade.com/Files/PDFs/ VELCADE _PRESCRIBING_
INFORMATION.pdf
National Comprehensive Cancer Network. (2013). Clinical Practice Guidelines in Oncology: Multiple myeloma. Retrieved
from http://www.nccn.org/professionals/physician_gls/pdf/
myeloma.pdf
Novartis Pharmaceuticals. (2012a). Aredia® (pamidronate disodium) [Prescribing information]. Retrieved from http://www
.pharma.us.novartis.com/product/pi/pdf/aredia.pdf
Novartis Pharmaceuticals. (2012b). Zometa® (zoledronic acid)
[Prescribing information]. Retrieved from http://www.pharma
.us.novartis.com/product/pi/pdf/Zometa.pdf
Onyx Pharmaceuticals. (2012). Kyprolis® (carfilzomib) [Prescribing information]. Retrieved from http://kyprolis.com/Content/
pdf/PrescribingInformation.pdf
Palumbo, A., & Anderson, K. (2011). Multiple myeloma. New England
Journal of Medicine, 364, 1046–1060. doi:10.1056/NEJMra1011442
Palumbo, A., Bladé, J., Boccadoro, M., Palladino, C., Davies, F.,
Dimopoulos, M., . . . San Miguel, J. (2012). How to manage neutropenia in multiple myeloma. Clinical Lymphoma Myeloma
and Leukemia, 12, 5–11.
Palumbo, A., Bringhen, S., Ludwig, H., Dimopoulos, M.A., Bladé, J.,
Mateos, M.V., . . . Sonneveld, P. (2011). Personalized therapy in
multiple myeloma according to patient age and vulnerability: A
report of the European Myeloma Network (EMN). Blood, 118,
4519–4529. doi:10.1182/blood-2011-06-358812
Palumbo, A., & Cavallo, F. (2012). Have drug combinations supplanted stem cell transplantation in myeloma? Blood, 120,
4692–4698. doi:10.1182/blood-2012-05-423202
Pasquini, M.C., & Wang, Z. (2011). Current use and outcome of hematopoietic stem cell transplantation: CIBMTR summary slides,
2011. Retrieved from http://www.cibmtr.org/ReferenceCenter/
SlidesReports/SummarySlides/Pages/index.aspx
Rajkumar, S.V., Jacobus, S., Callander, N.S., Fonseca, R., Vesole,
D.H., Williams, M.E., . . . Greipp, P.R. (2010). Lenalidomide plus
high-dose dexamethasone versus lenalidomide plus low-dose
dexamethasone as initial therapy for newly diagnosed multiple
myeloma: An open-label randomised controlled trial. Lancet
Oncology, 11, 29–37. doi:10.1016/S1470-2045(09)70284-0
Richards, T.A., Bertolotti, P.A., Doss, D., & McCullagh, E.J. (2011).
Sexual dysfunction in multiple myeloma: Survivorship care plan
of the International Myeloma Foundation Nurse Leadership
Board. Clinical Journal of Oncology Nursing, 15(Suppl., 1),
53–65. doi:10.1188/11.CJON.S1.53-65
Rodriguez, A. (2010a). Management and evaluation of patients
receiving high dose therapy with stem cell transplant. In J.D.
Tariman (Ed.), Multiple myeloma: A textbook for nurses (pp.
155–172). Pittsburgh, PA: Oncology Nursing Society.
Rodriguez, A. (2010b). Treatment of newly diagnosed, transplanteligible patients. In J.D. Tariman (Ed.), Multiple myeloma: A
textbook for nurses (pp. 109–124). Pittsburgh, PA: Oncology
Nursing Society.
Rome, S.I., Jenkins, B.S., & Lilleby, K.E. (2011). Mobility and safety
in the multiple myeloma survivor: Survivorship care plan of the
International Myeloma Foundation Nurse Leadership Board.
Clinical Journal of Oncology Nursing, 15(Suppl., 1), 41–52.
doi:10.1188/11.S1.CJON.41-52
Saleh, U.S., & Brockopp, D.Y. (2001). Quality of life one year following bone marrow transplantation: Psychometric evaluation
of the quality of life in bone marrow transplant survivors tool.
Oncology Nursing Forum, 28, 1457–1464.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Overview for Nontransplantation Nurses
23
San Miguel, J.F., Schlag, R., Khuageva, N.K., Dimopoulos, M.A.,
Shpilberg, O., Kropff, M., . . . Richardson, P.G. (2008). Bortezomib plus melphalan and prednisone for initial treatment
of multiple myeloma. New England Journal of Medicine, 359,
906–917. doi:10.1056/NEJMoa0801479
Schulmeister, L., Quiett, K., & Mayer, K. (2005). Quality of life,
quality of care, and patient satisfaction: Perceptions of patients
undergoing outpatient autologous stem cell transplantation.
Oncology Nursing Forum, 32, 57–67. doi:10.1188/05.ONF.57-67
Sipsas, N.V., & Kontoyiannis, D.P. (2008). Occupation, lifestyle,
diet, and invasive fungal infections. Infection, 36, 515–525.
doi:10.1007/s15010-008-8129-5
Sonneveld, P., Asselbergs, E., Zweegman, S., Van Der Holt, B.,
Kersten, M., Vellenga, E., . . . Lokhorst, H. (2012). Carfilzomib
combined with thalidomide and dexamethasone (ctd) is a highly
effective induction and consolidation treatment in newly diagnosed patients with multiple myeloma (mm) who are transplant
candidate [Abstract 333]. Blood, 120(21). Retrieved from http://
myeloma.org/ArticlePage.action?articleId=3622
Sonneveld, P., Schmidt-Wolf, I., van der Holt, B., El Jarari, L.,
Bertsch, U., Salwender, H., . . . Goldschmidt, H. (2012). Bortezomib induction and maintenance treatment in patients with newly
diagnosed multiple myeloma: Results of the randomized phase
III HOVON-65/ GMMG-HD4 trial. Journal of Clinical Oncology,
30, 2946–2955.
Stadtmauer, E.A., Vogl, D.T., Luning Prak, E., Boyer, J., Aqui, N.A.,
Rapoport, A.P., . . . Sullivan, K.E. (2011). Transfer of influenza
vaccine-primed costimulated autologous T cells after stem cell
transplantation for multiple myeloma leads to reconstitution of
influenza immunity: Results of randomized clinical trial. Blood,
117, 63–71. doi:10.1182/blood-2010-07-296822
Tariman, J. (2010). Multiple myeloma: A textbook for nurses.
Pittsburgh, PA: Oncology Nursing Society.
Tichelli, A., Passweg, J., Wojcik, D., Rovo, A., Harousseau, J.L.,
Masszi, T., . . . Socie, G. (2008). Late cardiovascular events after
allogeneic hematopoietic stem cell transplantation: A retrospective multicenter study of the Late Effects Working Party of the
European Group for Blood and Marrow Transplantation. Haematologica, 93, 1203–1210. doi:10.3324/haematol.12949
Tomblyn, M., Chiller, T., Einsele, H., Gress, R., Sepkowitz, K.,
Storek, J., . . . Boeckh, M.J. (2009). Guidelines for preventing infectious complications among hematopoietic cell transplantation
recipients: A global perspective. Biology of Blood and Marrow
Transplantation, 15, 1143–1238. doi:10.1016/j.bbmt.2009.06.019
Versteeg, P.A., Slot, D.E., van der Velden, U., & van der Weijden,
G.A. (2008). Effect of cannabis usage on the oral environment:
A review. International Journal of Dental Hygiene, 6, 315–320.
Williams, L. (2004). Post-transplant follow-up. In S. Ezzone (Ed.),
Hematopoietic stem cell transplantation: A manual for nursing
practice (pp. 207–220). Pittsburgh, PA: Oncology Nursing Society.
At the Transplantation Center
Follow-Up Care
Consider bringing these items to the transplantation center consultation
• Medical records (i.e., radiology on disc, laboratory results, bone marrow reports)
• List of previous chemotherapy and dates received
• Current and recently taken medications (both prescribed and supplements)
• Questions for the physician
Long-term follow-up plan of action
Plan to return to the transplantation center
near day 100 post-transplantation for a full
evaluation. This may be a 2–3 day visit. Posttransplantation immunization may be recommended at 12, 14, and 24 months following
transplantation.
Important paperwork to bring
Medical Leave of Absence (MLOA), Family Medical Leave Act (FMLA), and insurance benefits.
Notify your employer of MLOA and complete FMLA forms. Forms need to be completed for patient and caregivers. Anticipated time for processing is eight weeks.
Suggested items to bring for your stay
Comfortable clothing, sedentary activities, multi-unit pill dispenser, personal items of comfort, and cell phone
In the Community
While away from home . . .
• Arrange for caregiver support while at the transplantation center. Caregivers may be rotated. Investigate housing options near the transplantation center.
• Arrange for child and pet care.
• Arrange for care of your home while you are away and assistance when you return after
transplantation (i.e., yard maintenance, mail delivery, and utilities).
Seek help with household chores and activities of daily living
• Assistance with cleaning, paying bills, grocery shopping, laundry
• Assistance with bathing, dressing, meal preparation, and transportation (medical appointments, shopping, pharmacy)
• Encouragement regarding oral intake, ambulation, and strengthening
Fundraising
Out-of-pocket expenses add up quickly. Consider hosting a fundraising event in your community to help cover healthcare costs.
Oral medication management
Administering scheduled and as needed medications, refills, and renewals
IV fluids and medications
In some situations, home infusion of medications
for specific conditions (i.e., dehydration, infection,
low magnesium) may be ordered by the healthcare provider.
Symptom monitoring
Fever, bruising, bleeding, new onset of pain
(bone or nerve); changes in energy, appetite,
weight (up or down), bowel function, and bladder function. Know your contact information—
who to call, where to go.
Patient advocate
Communicate with healthcare providers, employers, family and friends; consider creating a
blog to keep friends and family informed
Central line care
This varies from institution to institution. Instructions will be provided by the transplantation center.
APPENDIX A. Preparation and Activity Considerations for Patients With Multiple Myeloma Undergoing Hematopoietic
Stem Cell Transplantation
24
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
n Article
Caregivers of Multiple Myeloma Survivors
Sandra Kurtin, RN, MS, AOCN®, ANP-C, Kathryn Lilleby, RN, and Jacy Spong, RN, BSN, OCN®
Patients living with multiple myeloma (MM) face complex decisions throughout their journey
relative to their diagnosis, options for treatment, and how their disease and treatment choices
may affect them physically, emotionally, financially, and spiritually. Patients considering a hematopoietic stem cell transplantation face specific self-management challenges. The availability of a
reliable caregiver is a prerequisite to transplantation eligibility. Currently, the majority of clinical
management is episodic and provided in the outpatient setting. Therefore, the bulk of care for
patients living with MM is provided by the patient together with his or her caregivers. Caregivers
face similar challenges to those faced by the patient living with MM. They are required to take
© Fuse/Thinkstock
in complex information, perform often complicated or technical procedures such as line care or
injections, assist the patient with activities of daily living, and attend the myriad of appointments required. Understanding the
dynamics of the patient-caregiver relationship, the strengths and weaknesses unique to that relationship, common elements
of caregiver stress or strain, and available tools and strategies to promote a sense of control and enhance self-management
skills may improve the health-related quality of life for both the patient with MM and his or her caregiver.
Sandra Kurtin, RN, MS, AOCN®, ANP-C, is a nurse practitioner and clinical assistant professor of medicine in the Hematology/Oncology Division of Arizona Cancer
Center in Tucson; Kathryn Lilleby, RN, is a research clinical nurse at the Fred Hutchinson Cancer Research Center in Seattle, WA; and Jacy Spong, RN, BSN, OCN®,
is an RN coordinator at the Mayo Clinic in Scottsdale, AZ. The authors received editorial support from Alita Anderson, MD, with Eubio Medical Communications
in preparation of this article supported by Sanofi Oncology. The authors are fully responsible for content and editorial decisions about this article. Kurtin serves as
a consultant for Celgene Corporation, Novartis Pharmaceuticals, Millennium: The Takeda Oncology Company, and Onyx Pharmaceuticals. Lilleby and Spong have
no financial relationships to disclose. The content of this article has been reviewed by independent peer reviewers to ensure that it is balanced, objective, and
free from commercial bias. No financial relationships relevant to the content of this article have been disclosed by the independent peer reviewers or editorial
staff. Kurtin can be reached at sandra.kurtin@uahealth.com, with copy to editor at CJONEditor@ons.org. (Submitted July 2013. Revision submitted September
2013. Accepted for publication September 12, 2013.)
Digital Object Identifier:10.1188/13.CJON.S2.25-32
L
iving with multiple myeloma (MM), either as a patient
or as a caregiver, implies a need to adapt to the requirements of the diagnosis, how it affects the individual
patient, and what changes are necessary to support
the patient, including treatment and supportive care.
The patients and caregivers spend the majority of their time at
home and receive the bulk of their health care in the outpatient
setting. Therefore, assimilating complex information, often very
rapidly, and developing skills for self-management of many complex processes is expected. The complexity of self-management
skills and behaviors of patients and caregivers varies based on
the individual disease attributes, the treatment plan, the general
health of the patient, and social and financial situations unique
to each patient. The chronic disease trajectory of MM is characterized by variability in survival and time to progression or
relapse. Each relapse brings new challenges, and each episode
of care creates patient and caregiver vulnerability. Patients
considering a hematopoietic stem cell transplantation (HSCT)
face specific self-management challenges. The availability of a
reliable caregiver is a prerequisite to transplantation eligibility.
The diagnosis of MM, as with most cancer diagnoses, is
a life-changing event. For the caregiver, whether formal or
informal, this includes the uncertainty associated with a complex diagnosis, the fear of losing a loved one, and the often
immediate need to provide skilled care, emotional support,
and assistance with day-to-day necessities. Caregivers are most
often relatives of the patient, but also may be friends, acquaintances, or volunteers. The number of caregivers and how they
interact with the patient will vary, and all caregivers will experience some level of stress and feelings of uncertainty. In addition
to struggling to find a unique role in supporting the patient,
the caregiver also is dealing with his or her own feelings about
the patient’s diagnosis with an incurable disease, the often sudden change in day-to-day activities, and the uncertainty about
the ability to provide care for the patient. Having unexpected
changes in the plan of care based on changes in the patient status is not uncommon, which adds to the stress for both the patient and the caregiver. Understanding the role of the caregiver
in patients living with MM (including those undergoing HSCT),
the dynamics of the patient-caregiver relationship, and the key
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Caregivers of Multiple Myeloma Survivors
25
elements of caregiver stress are necessary to effectively support
both patients with MM and caregivers. The majority of patients
with MM are older adults, requiring a working knowledge of
the unique needs of the older adult for effective management.
For younger patients, considering the change in family dynamics is necessary, as are the common challenges of managing a
family with children while managing the care requirements for
the patient. Optimal patient outcomes require the development
of tools and strategies to support caregivers of MM survivors.
Preparing the Patient and Caregiver
for Self-Management
The overall goal for the treatment of MM remains an early and
sustained complete response (CR) with an acceptable level of
toxicity and quality of life (QOL) (Palumbo & Cavallo, 2012).
Achieving a CR has been identified as a key factor in improved
progression-free survival and overall survival (OS); however,
achieving a CR does not imply eradication of the malignant
clone. The improvement in OS over time is attributed primarily
to novel agents, with patients exposed to these agents achieving statistically significant longer survival compared to those
who have not (Palumbo & Anderson, 2011). HSCT remains an
important treatment option for MM in patients eligible for transplantation. This approach to therapy requires planning and
collaboration among multiple healthcare providers, the patients,
and their caregivers to allow adequate preparation for treatment,
follow-up, and effective management of the expected treatmentemergent adverse events (TEAEs). Proactive and aggressive
TEAE management is critical to allowing continuation of each
treatment long enough to obtain and maintain an optimal
response. Early identification and prompt intervention of common TEAEs will limit the severity of treatment and reduce the
probability of patients discontinuing treatment prematurely.
With the majority of care provided in the outpatient setting,
patients and their caregivers are expected to take a primary role
in the self-management of their disease, including early identification and reporting of TEAEs. Some of the key elements of the
caregiver role are provided in Figure 1. Many informal caregivers
may feel inadequately prepared to assume responsibility for these
tasks because of a lack of knowledge, the presence of health
problems themselves, or preexisting dynamics between the patient and the caregiver (van Ryn et al., 2011). This may increase
caregiver stress and contribute to a sense of loss of control.
Patient and family education with consistent information,
frequent reinforcement of key concepts, and active participation of the patient and family is critical to optimizing outcomes
(Kurtin & Demakos, 2010). Communicating clearly to the
patients, and their caregivers, as well as to any collaborating
providers, will reduce the anxiety associated with expected
TEAEs and encourage consistency in the approach to management. Patients and caregivers should be encouraged to keep a
binder that includes important contact information, a patient
medical history, medications, supportive care resources, and a
log of their treatment plan, blood counts, transfusion history,
TEAEs, and how they were treated. This will provide an invaluable tool for not only the patient and caregiver, but also the
healthcare team.
26
Direct Care
• Monitoring and reporting or recording treatment side effects
• Administering medications
• Deciding whether to call a healthcare provider
• Deciding whether medicine is needed
• Performing technical procedures: dressing changes, line care
• Communicating with healthcare providers
Care Coordination and Life Management
• Transportation
• Accompanying the patient to appointments
• Communication to other family members, friends; being a gate
keeper and advocate
• Household maintenance, financial management, shopping, cooking
• Availability for emergencies
• Completing medical forms, keeping track of bills, applications for
assistance
• Engaging the healthcare system
Emotional Support
• Balancing medical expectations while maintaining hope
• Listening
• Providing reassurance
FIGURE 1. Key Elements of the Caregiver Role
Individualizing patient and caregiver education also will
encourage effective self-management behaviors. The average
American reads at an eighth-grade level; however, most patient
education materials are written well above that level (Fagerlin,
Zikmund-Fisher, & Ubel, 2011). Visits to healthcare professionals often last 15–20 minutes, making it difficult to communicate
complex ideas in a way that the patient and family will be able to
understand, synthesize, and apply to informed care decisions.
Healthcare professionals expect patients, family members, or
other designated caregivers to assume a primary role in managing the illnesses (including managing TEAEs), reporting signs
and symptoms, communicating among providers, and continuing to take an active role in decision making (Kurtin, 2012).
However, patients with multiple health problems may have difficulty understanding the complexity of balancing their cancer
treatment with the continued management of existing illnesses.
The most common toxicity associated with all active therapies for MM, including a transplantation, is myelosuppression
(Kurtin & Bilotti, 2013). Infections, neutropenic fevers, and
bleeding are the most common reasons patients seek emergency treatment following transplantation and are a major cause
of morbidity and mortality. Although the definition of engraftment suggests adequate bone marrow function for outpatient
management, many centers are conducting the majority of
care for patients undergoing autologous HSCT (AHSCT) in the
outpatient setting. Setting expectations for expected cytopenias and the anticipated time to recovery, providing concrete
criteria for monitoring and reporting the signs and symptoms
that require immediate attention, and developing standards
for interventions will provide reassurance to the patient, promote early identification and treatment of infections, and limit
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
hospitalizations. Each preparative regimen, ongoing treatment,
and supportive care plan will carry specific recommendations
for frequency of clinic visits, laboratory monitoring, ancillary
testing, and supportive care. An individualized plan for monitoring and managing TEAEs should be prepared, discussed, and
updated throughout the transplantation process to assist the
patient and his or her caregiver in self-management.
Impact of Patient Quality of Life
on the Caregiver
Caregiving intensity will vary throughout the MM disease
continuum based on a number of treatment-, disease-, and
patient-related factors. Similarly, health-related QOL (HRQOL)
for the patient also will vary. Understanding factors that impact
HRQOL for the patient with MM is necessary for understanding the variability in caregiver stress and QOL throughout the
disease and treatment trajectory, and will provide guidance in
developing tools and strategies for support of the caregiver.
Patients who receive an AHSCT can generally expect to return to or surpass pretransplantation physical and emotional
role function and QOL. Patients with anxiety, depression, and
symptom distress prior to transplantation are more likely to
experience these same symptoms in the post-transplantation
period, and women are more likely to experience posttransplantation depression overall (Wells, Booth-Jones, & Jacobsen, 2009). In addition, women generally return to work later
than men and are less likely to return to work overall than men
(Kirchohoff, Leisenring, & Syrjala, 2010). Older adult patients
are more likely to adapt socially following transplantation (Sherman, Simonton, Latif, Plante, & Anaissie, 2009). Understanding
these elements of patient HRQOL is essential to anticipating and
evaluating potential caregiver strain and caregiver QOL.
Langer, Yi, Storer, and Syrjala (2010) conducted a prospective
longitudinal study evaluating marital adjustment, satisfaction,
and dissolution among 121 patients undergoing HSCT and 117
spouses at six time points starting with the pretransplantation
evaluation period through five years of follow-up. Fifty-nine of
the 121 initially married patients with a participating spouse
survived to five years with only 7% (n = 4, two male, two female
patients) of the marriages ending in dissolution. Interestingly,
female spouses reported a higher rate of relationship maladjustment at all time points in the study. The authors suggest that these
findings specific to female spouses of male patients may reflect
societal norms in which females are expected to be caregivers,
the tendency for female caregivers to provide the care without
enlisting the help of family and friends, and the fact that women
in general are more likely to be affected by the physical and psychological distress of their male partner/patient (Langer et al.,
2010). The ability of the caregiver to adapt to the multitude of
stressors inherent in the process of HSCT for patients with MM
has been shown to affect family relationships important to the
post-transplantation adjustment of the patient (Fife, Monahan,
Abonour, Wood, & Stump, 2009).
Although at least 20 different assessment tools exist for screening adult caregivers of patients undergoing HSCT, the impact
of caregiver strain or burnout on patient outcomes is not well
researched in the MM and HSCT literature (Wulff-Burchfield,
Jagasia, & Savani, 2013). Concepts gleaned from studies in other
high-risk populations, including the mentally ill and frail older
adults, suggest caregiver stress or burnout may negatively affect mortality, frequency of hospitalizations, and adherence to
treatment routines (Wulff-Burchfield et al., 2013). Assessment
of caregiver stress should be incorporated throughout the treatment continuum. Common signs of caregiver stress include anxiety, depression, emotional distress, loss of appetite, weight loss,
fatigue, sleep disturbance, and loss of physical strength (Bevans
& Sternberg, 2012; Wulff-Burchfield et al., 2013) (see Figure 2).
Fife et al. (2009) examined factors influencing the adaptation
of caregivers of patients undergoing HSCT (N = 192) prior to
hospitalization for transplantation (T1), during the hospitalization following the stem cell infusion, about one week prior
to planned discharge (T2), and one month after discharge
(T3). The patients included varied diagnoses, including MM,
with 151 patients undergoing AHSCT (79%) and 41 patients
(21%) undergoing allogenic HSCT. The majority of caregivers participating in this study were female (72%), married
to the patient (91%), working full time (58%), and Caucasian
(93%). Emotional distress increased significantly from T1 to
T3, and coping strategies declined in that same time period.
Interestingly, the sense of personal control, spirituality, and
the caregiver-patient relationship remained stable from T1 to
T3. A greater sense of personal control (p < 0.001), spirituality
(p < 0.001), and active coping (p < 0.001) were strongly correlated with adaptation and lower levels of distress. Increased
patient symptoms (p < 0.0001), financial strain (p = 0.0033),
caregiver life changes (p < 0.0236), and avoidance as a coping
strategy (p = 0.0079) were correlated with increased levels of
distress. Avoidance was associated with negative adaptation.
Physical
Health
Problems
Pain, loss of physical strength, sleep disorders,
fatigue and exhaustion, changes in appetite, sexual
dysfunction, decreased libido, and exacerbation of
preexisting health problems
Social
Problems
Changes in usual routines and lifestyle; social isolation; reduced contact with outside family, friends,
colleagues; and changes in work status, such as
increased days off, distraction, loss of employment
Emotional
Problems
Anxiety, fear, uncertainty, despair, disbelief, depression,
sorrow and a sense of loss, loneliness, feelings of inadequacy, powerlessness, and feeling a lack of control
Financial
Problems
Loss of wages, difficulty in paying bills; lack of sick
leave; managing health claims and bills; premature use of retirement funds, often with penalty;
and inability to contribute to 401(k) with loss of
employer-matched contributions
FIGURE 2. Selected Problems Faced by Caregivers
Note. Based on information from Armoogum et al., 2013; Ferrell et al.,
2013; Fife et al., 2009; Molassiotis et al., 2011; Stenberg et al., 2010;
van Ryan et al., 2011; Wulff-Burchfield et al., 2013.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Caregivers of Multiple Myeloma Survivors
27
Implications for Practice
u
Educate caregivers about the stresses and expectations they
will face during the patient’s journey with multiple myeloma.
u
Provide assistance to caregivers of patients with multiple
myeloma by suggesting hospital and community resources to
help them cope with added responsibility.
u
Assess caregivers for impaired quality of life caused by the
physical and emotional demands of assisting the patient
through pre- and post-treatment phases of care.
These data emphasize the need to adequately assess the coping strategies, patient-caregiver dynamics and communication
patterns, and elements of spirituality (sense of meaning and
peace as well as faith) for both the patient and caregiver prior
to, during, and following HSCT. Strategies to adequately prepare
the patient and caregiver for self-management strategies will
promote a sense of personal control.
Screening the patient and caregivers, both together and
separately, for pretransplantation stressors and existing coping
behaviors, with periodic reassessment may reduce caregiver
strain by assisting with a tailored support plan. Setting realistic
Caregiver Stress–10 Symptoms identifies key stress-related symptoms often experienced by caregivers.
http://myeloma.org/SGLTools/support/Caregiver-Stress---10-Symptoms
.pdf
Caring for the Caregiver is a booklet created by the National Cancer
Institute that offers both recommendations and resources for caregivers of patients with cancer.
www.cancer.gov/cancertopics/coping/caring-for-the-caregiver
Coping Tips for Caregivers A–Z offers 26 tips from the International
Myeloma Foundation.
http://myeloma.org/images/link_thumb_nail/copingtipscaregivers.jpg
Coping With the Cost of Cancer is a comprehensive guide by the
Cancer Support Community that offers strategies, tips, and resources
for managing the financial aspects of cancer care.
http://myeloma.org/SGLTools/support/Coping-with-the-Cost-of-Care.pdf
Facing Forward: When Someone You Love Has Completed Cancer
Treatment is a booklet created by the National Cancer Institute that
shares common reactions and feelings that many caregivers experience
once treatment is over. It also shares practical tips to help caregivers
navigate through this time.
www.cancer.gov/cancertopics/coping/someone-you-love-completed
-cancer-treatment
Now You Are a Caregiver is a part of the Caregiver Resource Directory. It includes important forms, such as a daily pain journal, a medication schedule, and a fatigue journal.
www.netofcare.org/content/pdf/1-nowyouareacaregiver.pdf
Taking Care of Yourself is an article highlighting side effects that
some caregivers may experience, and strategies for their management
and prevention.
www.curetoday.com/index.cfm/fuseaction/article.show/id/2/article_id/185
FIGURE 3. Caregiver Resources
28
expectations for the patient and caregiver prior to signing the
consent for HSCT, in terms of potential physical, emotional,
social, and spiritual challenges, with expected duration of these
changes, based on the individual patient attributes and type of
transplantation, may help in identifying the needed support.
Understanding the common patient and caregiver perceptions
and associated daily activities will allow development of patientand caregiver-specific supportive care strategies. All caregivers
should be encouraged to outline their available resources including family, friends, volunteers, organizations, and Internet
resources. Female caregivers of male patients, in particular,
should be encouraged to seek tangible help from family and
friends and take breaks from caregiving.
Communication strategies between caregivers and patients
vary widely. Discordance between caregiver and patient
knowledge-seeking behaviors may add burden to the caregiver,
particularly in instances where bad news may be shared (Molassiotis, Wilson, Blair, Howe, & Cavet, 2011). The caregiver must
prepare for the possibility of an unfavorable outcome, in some
cases even death of the patient, but may be conflicted with a
need to bolster hope while continuing to help the patient manage the day-to-day tasks of living with MM. Strategies to promote
effective patient and caregiver self-management include several
key elements: consistent and clear communication that allows
the patient to make informed decisions, reinforcement of key
messages at each visit, adjustment of visit frequency to the specific phase of survivorship and healthcare needs, integration of
community programs and resources, and development of mutually determined goals (Kurtin, 2012; McCorkle et al., 2011). Key
qualities of clear communication include adequate description
of the disease and prognosis; open, honest, and timely communication; and increased patient participation in decision making
with clinician assessment of individual preferences for information (Colosia et al., 2011; Rodin et al., 2009). Communication
of risks versus benefits is perhaps one of the most complicated
processes necessary for informed decision making and consent
for treatment, including HSCT. Healthcare professional descriptions often are complex and not well understood by the patient
and family (Fagerlin et al., 2011).
Healthcare professionals can provide additional support by
allowing patients adequate time to review presented material,
if clinically possible; providing written materials in addition to
verbal explanations; identifying community-based, national, or
international resources for patient support; and incorporating
members of the multidisciplinary team in the discussion with
patients (Barry, 2011; McCorkle et al., 2011). Selected resources
for patients with MM and caregivers are included in Figure 3.
Optimally, the multidisciplinary team members will be well
informed about the individual patient situation to avoid conflicting or confusing messages. Incorporation of adult learning
principles, adaptation for language barriers, and consideration
of the spiritual and cultural needs of the patient and caregiver
are ideal.
Caregiver Self-Care
The level of distress experienced by caregivers of patients
undergoing HSCT has been shown to exceed that of the patient
themselves, and caregivers are less likely to be screened for,
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
Disease-Related Information
• Causes, disease process
• Severity and prognosis
Treatment-Related Information
• Treatment options and expected outcomes
• Expected side effects, monitoring, and treatment strategies
• Complementary and alternative therapies
• Options for a second opinion
• Insurance coverage and out-of-pocket expenses
• Nutrition and activity guidelines for the patient
• When and who to call for help
• Criteria and procedure for emergent care
• Operating policies for each setting of care: visitation, children, supplies,
expected duration of appointment or length of hospital stays
• Record keeping
Support Services
• Support groups: disease-specific, HSCT-focused, and general
• Local, regional, national, and international organizations
• Drug assistance programs
• Spiritual, religious, and cultural support
• Communication skills—providers, family, friends
• In-home assistance: skilled care, PT or OT, custodial care, household work
• Food or grocery delivery services
Caregiver Self-Care
• Maintaining a healthy lifestyle: nutrition, exercise, sleep
• Relaxation or meditation
• Intimacy or sexual health
• Spirituality
• Treatment for depression and anxiety
• How to ask for and organize help
HSCT—hematopoietic stem cell transplantation; OT—occupational therapist; PT—physical therapist
FIGURE 4. Caregiver Support and Informational Needs
seek, and receive support services (Fife et al., 2009; Langer et
al., 2010). Factors associated with caregiver distress include
avoidance behaviors, financial strain, and life changes for the
caregiver. Financial strain is inevitable for patients undergoing an HSCT. Loss of employment and, in many cases, a fear of
losing insurance is of major concern. This may present added
stress in trying to balance the needs of the patient, the need to
maintain employment, manage a household, and care for other
members of the family. If the patient is the primary wage earner,
the spouse or partner may need to seek additional employment.
Patients who are single and have limited or no access to relatives
as caregivers present a particular challenge.
Out-of-pocket expenses during treatment may be substantial
and add to financial strain. A pilot study conducted by Majhail
et al. (2013) evaluating out-of-pocket expenses for patients and
caregivers (n = 22) in the first three months following HSCT
estimated median expenses of $2,440 (range = $199–$13,769),
with those requiring temporary relocation to housing near the
transplantation center incurring higher expenses than those
who do not require relocation (median = $5,247 versus $716).
The majority of patients in this pilot study had private insurance through a managed care plan (56%), with Medicaid (20%)
and Medicare (18%) being less common (Majhail et al., 2013).
Meehan et al. (2006) estimated median out-of-pocket costs for
housing for the caregiver during the patient’s inpatient stay
to be $560. In addition to housing, copayments for visits and
medications, transportation, and food represented the most
common sources of out-of-pocket expenses in these studies.
Prior authorization for HSCT is a part of the initial screening of
patient eligibility. Similar rigor should be applied in discussion
of individual financial resources, including anticipated out-ofpocket expenses based on the region and available assistance
programs.
Sherwood et al. (2008) evaluated 80 caregivers of patients
with primary brain tumors. An increased need for assistance
with independent ADLs in patients was correlated with lost
time from work in this population of caregivers. Measures
of ADLs or independent ADLs have been incorporated into
measures of vulnerability (performance status, comorbidities,
and frailty) and are central to risk-adapted treatment selection
for patients being considered for a stem cell transplantation or
other more intensive therapies for MM (Palumbo et al., 2011).
Caregiver life change is a complex concept with wide variability. Caregiver burden is a result of the responsibilities of
caregiving (direct care, indirect care, other care responsibilities) and the changes in normal routines and lifestyle as a result
of these responsibilities (Stenberg, Ruland, & Miaskowski,
2010). All caregivers experience some level of caregiver burden and secondary effects on physical, social, and emotional
well-being. For those caregivers who continue to work, the
added burden of caregiving may affect work life and the ability to maintain employment. Several studies have identified a
number of physical, social, emotional, and spiritual elements of
caregiver burden or distress. Familiarity with these attributes
will assist in assessing caregiver distress, developing individualized support strategies, and promoting caregiver self-care (see
Figure 4).
Some of the unmet needs identified by caregivers in these
studies include managing concerns for cancer recurrence, finding out about financial support and government benefits, strategies to maintain the caregiver’s own physical and emotional
health, balancing the needs of the patient with the caregivers
own needs, sexuality and sexual health, and dealing with
other caregivers and non-caregivers (Armoogum, Richardson,
& Armes, 2013; Ferrell, Hanson, & Grant, 2013).
Conclusion
Caregivers are essential for the optimal outcomes of patients
with MM throughout the disease process, in particular during
HSCT. Active participation of caregivers, whether formal or
informal, is expected to be, yet not always, readily available or
feasible for all patients. Familiarity with local, regional, national,
and international resources together with development of local
network of support will facilitate development of an interdisciplinary and individualized supportive care plan. The vulnerability of the patients and their caregivers in the transplantation
process requires careful assessment of potential attributes or
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Caregivers of Multiple Myeloma Survivors
29
dynamics that place them at risk. Similar to the widely accepted
approach to risk-adapted treatment selection based on disease
and individual clinical attributes, an equally rigorous risk-adapted
approach must be applied to assessment and planning for both
the patient and the caregiver. Understanding the dynamics of
the patient-caregiver relationship, the strengths and weakness
unique to that relationship, common elements of caregiver
stress or strain, and available tools and strategies to promote
a sense of control and enhanced self-management skills may
improve the HRQOL for both the patient and the caregiver.
The authors gratefully acknowledge Brian G.M. Durie, MD,
Robert A. Kyle, MD, Diane P. Moran, RN, MA, EdM, senior vice
president of strategic planning, and Robin Tuohy, AS, senior director of support groups at the International Myeloma Foundation,
for their critical review of the manuscript.
References
Armoogum, J., Richardson, A., & Armes, J. (2013). A survey of
the supportive care needs of informal caregivers of adult bone
marrow transplant patients. Supportive Care in Cancer, 21,
977–986. doi:10.1007/s00520-012-1615-4
Barry, M.J. (2011). Helping patients make better personal health
decisions: The promise of patient-centered outcomes research.
JAMA, 306, 1258–1259. doi:10.1001/jama.2011.1363
Bevans, M.F., & Sternberg, E.F. (2012). Caregiving burden, stress,
and health effects among family caregivers of adult cancer patients. JAMA, 307, 398–403. doi:10.1001/jama.2012.29
Colosia, A.D., Peltz, G., Pohl, G., Liu, E., Copely-Merriman, K., Khan,
S., & Kay, J.A. (2011). A review and characterization of the various perceptions of quality cancer care. Cancer, 117, 884–896.
doi:10.1002/cncr.25644
Fagerlin, A., Zikmund-Fisher, B.J., & Ubel, P.A. (2011). Helping patients decide: Ten steps to better risk communication. Journal
of the National Cancer Institute, 103, 1436–1443. doi:10.1093/
jnci/djr318
Ferrell, B., Hanson, J., & Grant, M. (2013). An overview and evaluation of the oncology family caregiver project: Improving quality
of life and quality of care of oncology family caregivers. PsychoOncology, 22, 1645–1652. doi:10.1002/pon.3198
Fife, B.L., Monahan, P.O., Abonour, R., Wood, L.L., & Stump, T.E.
(2009). Adaptation of family caregivers during the acute phase
of adult BMT. Bone Marrow Transplantation, 43, 959–966.
doi:10.1038/bmt.2008.405
Kirchohoff, A.C., Leisenring, W., & Syrjala, K.L. (2010). Prospective
predictors of return to work in the five years after hematopoietic
cell transplantation. Journal of Cancer Survivorship, 4, 33–44.
doi:10.1007/s11764-009-0105-2
Kurtin, S. (2012). Primary care of the cancer survivor: A collaborative continuum-based model for care. In J. Payne (Ed.), Current
trends in oncology nursing (pp. 191–210). Pittsburgh, PA: Oncology Nursing Society.
Kurtin, S., & Bilotti, E. (2013). Novel agents for the treatment of
multiple myeloma: Proteasome inhibitors and immunomodulatory agents. Journal of Advanced Practice Oncology, 4, 307–321.
Kurtin, S.E., & Demakos, E.P. (2010). An update on the treatment of
myelodysplastic syndromes [Online exclusive]. Clinical Journal
of Oncology Nursing, 14, E29–E44. doi:10.1188/10.CJON.E29-E44
Langer, S.L., Yi, J.C., Storer, B.E., & Syrjala, K.L. (2010). Marital
30
adjustment, satisfaction, and dissolution among hematopoietic
stem cell transplant patients and spouses: A prospective, fiveyear longitudinal investigation. Psycho-Oncology, 19, 190–200.
doi:10.1002/pon.1542
Mahjail, N.S., Rizzo, J.D., Hahn, T., Lee, S.J., McCarthy, P.L., Ammi,
M., . . . Pederson, K. (2013). Pilot study of patient and caregiver
out-of-pocket costs of allogeneic hematopoietic cell transplantation. Bone Marrow Transplantation, 48, 865–871. doi:10.1038/
bmt.2012.248
McCorkle, R., Ercolano, E., Lazenby, M., Schulman-Green, D., Schilling, L.S., Lorig, K., & Wagner, E.H. (2011). Self-management:
Enabling and empowering patients living with cancer as a
chronic illness. CA: A Cancer Journal for Clinicians, 61, 50–62.
doi:10.3322/caac.20093
Meehan, K.R., Fitzmaurice, T., Root, L., Kimtis, E., Patchett, L., &
Hill, J. (2006). The financial requirements and time commitments of caregivers for autologous stem cell transplant recipients. Journal of Supportive Oncology, 4, 187–190.
Molassiotis, A., Wilson, B., Blair, S., Howe, T., & Cavet, J. (2011).
Living with multiple myeloma: Experiences of patients and their
informal caregivers. Supportive Care in Center, 19, 101–111.
doi:10.1007/s00520-009-0793-1
Palumbo, A., & Anderson, K. (2011). Multiple myeloma. New England Journal of Medicine, 364, 1046–1060.
Palumbo, A., Bringhen, S., Ludwig, H., Dimopoulos, M.A., Blade, J.,
Mateos, M.V., . . . Sonneveld, P. (2011). Personalized therapy in
multiple myeloma according to patient age and vulnerability: A
report of the European Myeloma Network (EMN). Blood, 118,
4519–4529. doi:10.1056/NEJMra1011442
Palumbo, A., & Cavallo, F. (2012). Have drug combinations supplanted stem cell transplantation in myeloma? Blood, 120,
4692–4698. doi:10.1182/blood-2012-05-423202
Rodin, G., Mackay, J.A., Zimmerman, C., Mayer, C., Howell, D., Katz,
M., . . . Brouwers, M. (2009). Clinician-patient communication:
A systematic review. Supportive Care in Cancer, 17, 627–644.
doi:10.1007/s00520-009-0601-y
Sherman, A.C., Simonton, S., Latif, U., Plante, T.G., & Anaissie,
E.J. (2009). Changes in quality-of-life and psychosocial adjustment among multiple myeloma patients treated with high-dose
melphalan and autologous stem cell transplantation. Biology of
Blood Marrow Transplantation, 15, 12–20. doi: 10.1016/j.bbmt
.2008.09.023
Sherwood, P.R., Donovan, H.S., Given, C.W., Lu, X., Given, B.A.,
Hricik, A., & Bradley, S. (2008). Predictors of employment and
lost hours from work in cancer caregivers. Psycho-Oncology, 17,
598–605. doi:10.1002/pon.1287
Stenberg, U., Ruland, C.M., & Miaskowski, C. (2010). Review of
the literature on the effects of caring for a patient with cancer.
Psycho-Oncology, 19, 1013–1025. doi:10.1002/pon.1670
van Ryn, M., Sanders, S., Kahn, K., van Houtven, C., Griffin, J.M.,
Martin, M., . . . Rowland, J. (2011). Objective burden, resources,
and other stressors among informal cancer caregivers: A hidden
quality issue? Psycho-Oncology, 20, 44–52. doi:10.1002/pon.1703
Wells, K.J., Booth-Jones, M., & Jacobsen, P.B. (2009). Do coping
and social support predict depression and anxiety in patients
undergoing hematopoietic stem cell transplantation? Journal
of Psychosocial Oncology, 27, 297–315.
Wulff-Burchfield, E.M., Jagasia, M., & Savani, B.N. (2013). Long-term
follow-up of informal caregivers after allo-SCT: A systematic review. Bone Marrow Transplantation, 48, 469–473. doi:10.1038/
bmt.2012.123
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
Caregiver Guide
Hematopoietic Stem Cell Transplantation for Multiple Myeloma
Y
ou or someone you know has been diagnosed with
multiple myeloma (MM) and has been considered for a
hematopoietic stem cell transplantation (HSCT). Hearing
the words HSCT or bone marrow transplantation can be
frightening. You probably have many questions.
Caregivers, described as anyone who is providing assistance to the patient diagnosed with myeloma, also are living
with myeloma. Each caregiver experience is unique, based
on the amount of care you are providing, the complexity of
the care, and how independent your loved one is.
Caregivers also can experience anxiety and depression. The
demands on you, both physical and emotional, can at times be
overwhelming. It is important that you, the caregiver, know
that you are not alone. A number of resources and healthcare
professionals are available to help you prepare for the HSCT,
organize your resources, and stay well during the process.
Several key concepts will help you manage the role of
caregiver for the patient with MM during the HSCT process.
Although your loved may have difficult days, allow the
myeloma survivor to do as much self-care as possible. This
will help them to stay active, maintain stamina, and become
independent. There will be days when your loved one needs
more help. Ask your healthcare team for guidance in balancing
their need for assistance with their capability for independence
throughout the HSCT process.
Seek support for caring for the myeloma survivor. Discuss
the day-to-day challenges of caregiving with the healthcare
team at each visit, recognize that asking for help is OK, and
seek out support and assistance from other family members
and friends to allow for breaks.
Organize your resources and assign or define specific tasks.
For example, “I need someone to take [the patient] to the clinic
on Tuesday mornings at 8 am.”
Make a list of things you need. Keep it updated as the needs
change. Continue to ask for help.
• One item that friends can assist with is creating a blue box.
Have friends organize a box of small gift items, sayings,
jokes, prayers, or good thoughts that you can take out one
by one when you’re having a blue day. In addition, explore
strategies for communicating with family and friends, assign
a gate keeper, and consider online resources: www.caring
bridge.com or www.lotsahelpinghands.com.
Know that all things are not of equal importance. Some
things need immediate attention, some things can wait; prioritize. Myeloma is a like roller coaster, with many ups and downs.
It’s not a sprint, it’s a marathon. You need to pace yourself and
deal with priorities as they come up. Sometimes “good enough”
is “good enough.”
• Group tasks by categories (i.e., work, family, household
tasks, personal care tasks, errands, and physician visits).
Do Not Let Your Insurance Lapse
If the patient carries the insurance and is going to be out of work
for a long period of time, find out if you have long-term disability or
short-term disability. You may also need to look into COBRA. Familiarize yourself with the most current laws, both local and national, that
may affect your ability to obtain health insurance.
© iStock/Thinkstock
• Create a list from your group of tasks and manage by the
level of importance.
Join a support group or attend group meetings for caregivers
and/or patients with myeloma. Talk with family, friends, clergy,
or others about your thoughts or worries instead of keeping
them inside.
Ask for help from family and friends to maintain your household.
• If your transplantation center is near your home, you may
need help with housework, yard work, home maintenance,
and other day-to-day activities needed to run a household.
If you need to relocate temporarily for the HSCT, you will
need to explore options for a house sitter and others needed
to maintain the home until you return. When you return, it is
unlikely you and the myeloma survivor will be able to maintain
the home without some help.
Ask for help in organizing care for your family members or
your pets. If you are relocating to another city for the HSCT, ask
about the policies for visitation for family members and pets.
Find out what resources are available in your home center and
in the transplantation center for support of children with a
parent who is undergoing a HSCT.
Plan ahead. You may need to consider time off work if possible. As soon as HSCT is discussed as a possible treatment
option, discuss the best time to use any time off to meet the
demands of the HSCT process (www.dol.gov/whd/regs/stat
utes/fmla.htm).
(Continued on the next page)
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Caregivers of Multiple Myeloma Survivors
31
Caregiver Guide (Continued)
Considering the impact of your loved one’s health on your
family’s finances can be a major source of anxiety.
• Contact your insurance carrier and find out exactly what
your deductables are. If you have a cap, determine what your
maximum out-of-pocket expenses are, what providers are
in network, and how out-of-network providers are handled.
Seek out a myeloma specialist or get a second opinion. If
there are no myeloma specialists in your area (50-mile radius),
petition your insurance provider that an out-of-network myeloma specialist be considered in network.
Ask for an insurance case management worker. This person
will be your point of contact for all insurance billing and questions, with no need to re-explain the entire case each time
you call. Case managers are available for all life-threatening
conditions with all insurance companies.
Every state has a state insurance department. Contact them
for unbiased insurance information and local laws. They also
provide resources for finding insurance companies, pools, filing, financial requirements, and much more.
There currently is a two-year waiting period to get on Medicare. You may qualify for supplemental Social Security disability during this period. Consider making an appointment with
your local Medicare office to help with the paperwork and requirements to avoid possible denials. If you are denied, appeal.
Ask if a Medicare representative is available who has handled
other patients diagnosed with myeloma (they will know the
proper codes and procedures to get a quicker approval). For
more information visit www.medicare.gov.
Contact your town hall for available services, including
home heating oil, electricity, school lunch programs, church
ministries, or food pantries, as needed.
If you were not in charge of handling home finances, you’ll
need to get up to speed. If you always handled the bills, be prepared to make adjustments depending on your finances.
• Remember that every bill is negotiable, including medical
bills. Call all of your creditors and let them know you or your
Organize Your Contacts
Transplantation center healthcare team and contact information
should include the following:
Center:
Address:
Phone:
Physician:
Nurse practitioner or physician assistant:
Transplant coordinator:
Social worker:
Nutritionist:
Physical therapist:
Pharmacist:
Other support:
32
Self-Care Tips and Resources
• Taking care of yourself is necessary to continue the caregiver role.
http://bmtinfonet.org/before/caregivers
• Join a support group that provides support to caregivers. Contact
the International Myeloma Foundation to locate a group near you.
www.myeloma.org
• Schedule regular medical and dental evaluations for yourself.
• Participate in activities that help to rejuvenate your energy (i.e.,
crafts, meditation, massage, and music therapy) and avoid burnout.
http://bit.ly/16jutNz
• Write in a journal to express your feelings and experiences.
• Participate in health-promotion activities, such as a healthy diet,
physical activity, and restful sleep.
• Information can be found at the National Caregiver’s Library
www.caregiverslibrary.org/home.aspx
spouse is out of work and would like to make payment arrangements. Have an amount in mind that you can afford each
month and offer that as your payment. As long as you are making payments, your account will not go to collections. Keep
your credit intact by continuing monthly payments.
• Also, you may have to reduce or cut out some services. Eating out, TV, and phone extras may need to be cut back. Use
coupons when possible.
Visit the International Myeloma Foundation website for additional information regarding possible side effects and strategies
for symptom management and wellness (www.myeloma.org).
Ask for assistance in planning for the HSCT process.
• Pretransplantation evaluation
– Time required at the transplantation center, housing options, preparation for any testing, how soon will testing
results be available, and when will the final decision to
proceed to transplantation be made
• Hospitalization
– Preparative regimen and side effects, infusion of peripheral stem cells and side effects, engraftment, common
adverse events and management, discharge criteria, visitation policies, and housing options for families
• Outpatient care
– How to prepare the home prior to discharge, frequency of
visits, expectation of the caregiver, and can the myeloma
survivor be alone?
mWhat symptoms require immediate or emergency care?
What special precautions are needed for the patient?
Are there any dietary restrictions? Specific care guidelines and any equipment needed?
mTaking a temperature, heart rate, respiratory rate, and
blood pressure; central venous catheter care; medication management; drug-drug interactions; drug-food
interactions; calendar to organize treatment schedule:
tests and clinic visits
m Log for tracking any reactions, side effects, intolerance;
make notes of drugs, dates, and describe events; resources
for drug assistance; dates medication refills are required.
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
n Article
Clinical Updates in Blood and Marrow
Transplantation in Multiple Myeloma
Beth Faiman, MSN, APRN-BC, AOCN®, Teresa Miceli, RN, BSN, OCN®, Kimberly Noonan, RN, ANP-BC,
and Kathryn Lilleby, RN
The process of hematopoietic stem cell transplantation (HSCT) is well defined, yet debate remains surrounding the role and timing of HSCT in patients with multiple myeloma (MM). Since
the 1980s, survival advances have been made with the use of newer agents by recognizing the
role of transplantation, identifying the anticipated side effects at each phase, and improving
supportive care strategies. Data support transplantation as part of the treatment strategy, but
the optimal induction regimen and timing of transplantation have yet to be defined. The general
consensus is that eligible patients should undergo autologous HSCT at some point in the treatment spectrum, preferably earlier rather than later in the disease. Allogeneic transplantation is
© tagota/iStock/Thinkstock
only recommended in the context of a clinical trial and in patients with high-risk disease. The
transplantation process can be overwhelming for patients and caregivers. Nurses play a key role in improving outcomes by
caring for patients and families throughout the transplantation experience and, therefore, need to be knowledgeable about
the process. This article is intended to expand discussion on the role of nurses in assisting patients and families undergoing
transplantation to include an overview of the acute care phase of the transplantation process.
Beth Faiman, MSN, APRN-BC, AOCN®, is a nurse practitioner in the Taussig Cancer Center at the Cleveland Clinic in Ohio; Teresa Miceli, RN, BSN, OCN ®,
is a bone marrow transplantation nurse coordinator and assistant professor of nursing in the College of Medicine in the William von Liebig Transplant
Center at the Mayo Clinic in Rochester, MN; Kimberly Noonan, RN, ANP-BC, is an adult nurse practitioner at the Dana-Farber Cancer Institute in Boston, MA;
and Kathryn Lilleby, RN, is a clinical research nurse at the Fred Hutchinson Cancer Research Center in Seattle, WA. The authors received editorial support
from Alita Anderson, MD, with Eubio Medical Communications, in preparation of this article supported by Sanofi Oncology. The authors are fully responsible
for content and editorial decisions about this article. The content of this article has been reviewed by independent peer reviewers to ensure that it is balanced, objective, and free from commercial bias. No financial relationships relevant to the content of this article have been disclosed by the authors, independent peer reviewers, or editorial staff. Mention of specific products and opinions related to those products do not indicate or imply endorsement by the
Clinical Journal of Oncology Nursing or the Oncology Nursing Society. Faiman can be reached at faimanb@ccf.org, with copy to editor at CJONEditor@ons
.org. (Submitted July 2013. Revision submitted August 2013. Accepted for publication September 12, 2013.)
Digital Object Identifier:10.1188/13.CJON.S2.33-41
T
he process of transplantation can be conceptualized
through several phases (see Figure 1). Each phase
carries with it distinct considerations and management strategies to optimize the overall process. Years
of clinical research and experience have provided
knowledge of when challenges, side effects, and appropriate
interventions can occur. Thus, an experienced transplantation team can anticipate patient needs during the acute phase.
Long-term side effects and complications can occur and require
the attention of community-based practitioners, as well. This
article will cover considerations within each phase, with a
focus on autologous hematopoietic stem cell transplantation
(AHSCT) and should be used in conjunction with the Miceli
et al. (2013) article in this supplement to get a broad picture
of the transplantation experience. Allogeneic transplantation,
which should only be considered in the context of a clinical
trial, is highlighted in the “Special Interest” sidebar on page 35.
Phase 0: Induction or Initial Treatment
Following a confirmed diagnosis of symptomatic multiple myeloma (MM), the patient begins induction chemotherapy. The
goals of induction therapy are to induce a tumor response and
decrease symptoms by reducing disease burden (Giralt, 2012).
Response to therapy is classified based on the reduction of myeloma protein from baseline. A complete response is the best
surrogate marker for progression-free survival (Chanan-Khan
& Giralt, 2010). A complete response occurs when patients
achieve negative immunofixation of the serum and urine, experience the disappearance of any soft tissue plasmacytomas, and
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Clinical Updates in Transplantation 33
White Blood Count
al., 2009). Use of CD34+ cells has resulted in reduced
transfusion needs and a shorter engraftment period
following transplantation. Therefore, this has become
the preferred source of progenitor cells (versus bone
marrow) (Williams, Zimmerman, Grad, & Mick, 1993)
and will be discussed in the current article.
Above
normala
Normalb
Nadirc
Melphalan
Day –2, –1
AHSCT
Day 0
Blood count nadir
Day +5 to +7
Engraftment
Day +10 or +14
Mobilization
The process of stimulating the bone marrow to
release HSCs into the peripheral blood is called mobilization. Methods to mobilize HSCs from the bone
marrow into the peripheral blood include the use of
cytokine growth factors, such as granulocyte–colonyc
100 mcl
stimulating factor (G-CSF) (e.g., filgrastim), alone or
in combination with chemotherapy or the CXCR4Figure 1. Timeline Schema for the Conditioning Regimen
binding agent plerixafor. For some patients, the use
for Autologous Hematopoietic Stem Cell Transplantation (AHSCT)
of G-CSF alone may mobilize adequate HSCs (Giralt
Note. Based on information from Antin & Yolin Raley, 2009; Rodriguez, 2010.
et al., 2009). The approach may be effective for patients younger than 65 years who have not received
melphalan or prolonged use of lenalidomide (Giralt et
reduce the number of plasma cells present in the bone marrow
al., 2009). Key side effects of cytokine growth factors include leuto 5% or less (Durie et al., 2006). Improved response rates can
kocytosis, bone pain, myalgias, and flu-like symptoms. In addition,
be seen with the newer therapies, such as lenalidomide, bortsome patients may develop a low-grade fever (Amgen Inc., 2013).
ezomib, and carfilzomib, followed by AHSCT (Jakubowiak et al.,
For others, chemotherapy may be added to assist with the mo2012; Richardson et al., 2010; Rosiñol et al., 2012).
bilization process and used as an additional treatment option prior
To date, the optimal timing of transplantation cannot be deto transplantation, particularly if optimal response has not been
fined. Considerations include patient performance status, organ
achieved. Although several different chemotherapies are eligible
function, response to therapy, financial limitations, and the
for use during the HSC mobilization process, including etoposide
overall treatment plan. Participation in a well-designed clinical
and paclitaxel, cyclophosphamide is used most frequently (Giralt
trial also should be considered to help identify the best inducet al., 2009). Common side effects related to high doses of cyclotion therapy, transplantation timing, and maintenance therapy
phosphamide include nausea, alopecia, and myelosuppression. At
for each MM subgroup. When considering transplantation as
the doses used for mobilization, patients rarely will experience
part of the treatment plan, using stem cell–sparing induction
mucositis or hemorrhagic cystitis. However, patients are encourregimens, which are less damaging to the hematopoietic stem
aged to drink plenty of fluids to reduce the risk of bladder toxicity
cells (HSCs), is important. Some antimyeloma therapies (e.g.,
(Rodriguez, 2010). They also must report to the nurse or provider
alkylating agents) can damage stem cells and negatively impact
a fever greater than 38.3°C (101°F) or a persistent fever of 38°C
the ability to collect adequate amounts of peripheral blood HSCs
(100.4°F) when at blood count nadir (white blood count less than
for transplantation. In particular, the prolonged use of melphalan
100 mcl) (Palumbo et al., 2012). Nadir from cyclophosphamide,
should be avoided in patients eligible for transplantation (Cavo et
when used in combination with G-CSF for the purpose of HSC
al., 2011; Giralt et al., 2009). Possible pretransplantation combinamobilization, is predictable and typically of short duration (8–12
tions for induction therapy are outlined in Miceli et al. (2013) and
days) (Giralt et al., 2009).
will not be discussed here.
The newest approach to stem cell mobilization is the use of
plerixafor with G-CSF. Plerixafor is a bicyclam molecule that
binds to the CXCR4 receptor site, the stem cell honing site in
the bone marrow stroma. Plerixafor temporarily blocks the
SDF-1a signaling pathway necessary to bind CD34+ cells to the
A key component of the transplantation process is the acquisibone marrow, promoting circulation of the CD34+ cells into
tion of pluripotent HSCs. The sources of HSCs for transplantation
the peripheral blood. Plerixafor in combination with G-CSF
are autologous (self-donation), syngeneic (identical sibling), and
was approved by the U.S. Food and Drug Administration in
allogeneic (related or unrelated donation). As mentioned earlier,
December 2008 for stem cell mobilization in autologous donors
HSCs can be retrieved from the bone marrow, cord blood, or
with non-Hodgkin lymphoma and MM (DiPersio, Uy, Yasothan,
peripheral blood (Antin & Yolin Raley, 2009). Peripheral blood
& Kirkpatrick, 2009; Flomenberg et al., 2005; National Cancer
has become the most-used source for HSC collection (Pasquini &
Institute, 2013). Side effects associated with plerixafor include
Wang, 2011). CD34+ cells are progenitor cells with the capacity
leukocytosis, thrombocytopenia, diarrhea, nausea, erythema
to differentiate and repopulate myeloid and lymphoid cell lines
at the injection site, and fatigue (Genzyme Corporation, 2010).
following bone marrow ablation after high-dose chemotherapy.
The combination of plerixafor and G-CSF has been shown to
They are measured in cells per deciliter (cells/dl) to the power of
be more effective at mobilizing HSCs than G-CSF alone (DiPer106 (million) based on recipient weight (i.e., collection yield of 3.2
sio, Stadtmauer, et al., 2009). Using G-CSF in conjunction with
x 106 CD34+ cells/kg recipient weight) (DisPersio, Stadtmauer, et
Stage and Days After Pretransplantation Regimen Chemotherapy
a
Greater than 10,000 mcl
b
Baseline
Patient timeline
4,000–10,000 mcl
Phase 1: Collection Process
34
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
plerixafor results in higher success rates for mobilizing more
stem cells while undergoing fewer apheresis procedures. As a
result, more patients achieve the minimum and target amounts
of stem cells needed for transplantation. Use of plerixafor also
has significantly reduced the number of mobilization failures.
Even patients who previously failed to effectively mobilize HSCs
have been successful with the use of plerixafor, allowing more
patients to proceed to transplantation (Calandra et al., 2008;
Gopal et al., 2012).
The cost of two common HSC mobilization approaches
has been compared in the literature (Gertz, Wolf, Micallef, &
Gastineau, 2010; Micallef et al., 2013). Investigators at Memorial
Sloan-Kettering Cancer Center in New York, NY, and the Mayo
Clinic in Rochester, MN, performed a retrospective analysis of
all patients with MM treated from November 2008 to March 2011
who received cyclophosphamide plus G-CSF or plerixafor plus
G-CSF as the first-line mobilization regimen. Plerixafor was more
cost effective than the more widely used cyclophosphamide.
Plerixafor plus G-CSF costs less than cyclophosphamide plus
G-CSF because plerixafor requires fewer days of apheresis (Adel
et al., 2011). Another reason for lower cost is that patients who
use plerixafor are less likely to require hospitalization because of
infections. Despite the cost of the medication, the notable benefits for successful mobilization make it a cost-effective option,
particularly for patients at risk for mobilization failure (Gertz et
al., 2010; Micallef et al., 2013).
The combined mobilization regimen of G-CSF and plerixafor
should begin four days prior to planned harvest. G-CSF is given
at a dose of 10 mcg/kg daily, by subcutaneous injection, beginning on day –4. The recommended dose of plerixafor is 0.24
mg/kg given by subcutaneous injection about 11 hours prior to
each planned apheresis session, beginning on day –1. The dose
of plerixafor should not exceed 40 mg per day, and should be
adjusted for creatinine clearance less than 50 ml per minute
(Genzyme Corporation, 2010). One study suggested that the
administration of plerixafor 17 hours prior to collection, rather
than 11 hours, was as effective and more convenient for patients
and nurses (Harvey et al., 2011).
Collection
The goal of collection is to procure a sufficient number of
HSCs for reconstitution of hematopoietic function after highdose chemotherapy (HDC) is administered to eradicate the
MM. Cells are collected via apheresis using a large bore catheter in a process that separates blood components and selects
specific cells for use. Although the ideal stem cell collection
goal is greater than 3 x 106 CD34+ cells/kg of recipient weight,
2 x 106 CD34+ cells/kg of recipient weight offers a minimum
goal when HSC yield is low. Greater cell counts allow for faster
recovery of hematopoiesis. Some patients may want to store
additional cells for a future transplantation (Gertz et al., 2010;
Giralt et al., 2009).
Once collected, the cells are cryopreserved in a medium of
dimethyl sulfoxide (DMSO) to prevent cell breakdown, and may
be stored for an indefinite period of time (Antin & Yolin Raley,
2009; Gertz et al., 2010). Stem cell collection can occur days,
months, or even years prior to HDC, but typically occurs early in
the diagnosis to ensure adequate collections before patients are
exposed to extended chemotherapy (Antin & Yolin Raley, 2009;
Gertz et al., 2010).
Phase 2: Pre-Engraftment
The decision to proceed directly to HDC and AHSCT is individualized based on many patient-specific factors (see Figure
2). It may follow the mobilization and collection phase for
early transplantation, or may be postponed until a later date at
Special Interest:
HSCT, Allogeneic HSCT, and Acute GVHD
Allogeneic HSCT uses HDC similar to autologous HSCT, but instead uses
HSCs from a donor. The donor cells are used to reconstitute the bone marrow
function after HDC while producing a new immune system in the recipient.
The new immune function can provide a graft-versus-tumor benefit, but is
associated with high treatment-related mortality from intensive conditioning regimens, infection associated with immunosuppression, and GVHD.
Acute GVHD is a major complication of allogeneic HSCT associated with
significant morbidity and mortality. GVHD occurs when donor-derived cells
recognize recipient tissue as foreign and mount an immune attack against
the patient’s own tissues, which occurs in 40%–60% of patients undergoing
allogeneic HSCT. Although GVHD is a complication of transplantation, it also
is considered a treatment for multiple myeloma. As GVHD occurs, graftversus-myeloma causes an antitumor effect mediated by the donor graft.
Clinical manifestations of acute GVHD can be seen in the immune system,
skin, gut, and liver. Transplantation recipients with acute GVHD may present
with rash (81%), gut (54%), and liver (50%) symptoms. Acute GVHD has
a significant impact on the immune system. Immune reconstitution is an
integral part in the prevention of opportunistic infections, and infection is
the most frequent cause of death in transplantation recipients who experience acute GVHD. Not only does prolonged myelosuppression occur in these
patients, thymic involution and hypogammaglobulinemia further weaken
the immune system.
A skin rash often is the initial symptom associated with acute GVHD.
The rash typically is described as maculopapular, and often begins in the
anterior or posterior torso, neck, palmar and plantar surfaces, and ears. The
typical rash can range from a sunburn-like appearance to desquamating
and peeling skin.
The symptoms of gastrointestinal acute GVHD include nausea, emesis,
diarrhea, abdominal cramping, and pain. Hematochezia, ileus, and anorexia
are other notable side effects associated with acute GVHD.
Liver acute GVHD is caused by damage to the bile canaliculi, which can
cause cholestasis with hyperbilirubinemia and elevated alkaline phosphatase. The severity of liver acute GVHD is based on the serum bilirubin.
Ruling out other causes of organ dysfunction, such as drug toxicity (skin,
gut, liver), viral infection (gut, liver), and sinusoidal obstructive syndrome
(liver) is important. Prevention of acute GVHD begins with donor selection
and continues with immunosuppressive medication to decrease T-cell
activation and proliferation.
Common medications used in the prevention and treatment of GVHD
include cyclosporine, methotrexate, mycophenolate mofetil, steroids, sirolimus, and tacrolimus. In addition, bortezomib is an experimental medication
for this use.
GVHD—graft-versus-host disease; HDC—high-dose chemotherapy;
HSCT—hematopoietic stem cell transplantation
Note. Based on information from Antin & Yolin Raley, 2009; El-Cheikh
et al., 2013; Koreth et al., 2012; Laffan & Biedrzycki, 2006; Lokhorst et al.,
2010; Martin et al., 1990; Mattson, 2007; Pallera & Schwartzberg, 2004;
Sung & Chao, 2013.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Clinical Updates in Transplantation 35
the time of relapse (Kumar, 2009). If chemotherapy is used for
stem cell mobilization, some centers may delay HDC to allow
recovery and avoid the added risk of marrow toxicity.
The amount of time to undergo Phase 2 (pre-engraftment)
typically is measured in weeks. The process includes three components: conditioning, stem cell infusion, and supportive therapy
through engraftment (Antin & Yolin Raley, 2009). During this
time, the recipient may be an inpatient at the transplantation
center for three to four weeks, requiring geographic relocation
if the transplantation center is not near the patient’s home. Some
centers perform the AHSCT process in the outpatient department,
which requires a trained caregiver (Kurtin, Lilleby, & Spong,
2013) and daily clinic visits to monitor side effects.
Conditioning
The therapy used prior to HSCT is referred to as conditioning.
The term refers to the process of getting the bone marrow in condition to receive new cells. In patients with MM, high-dose melphalan (HDM) is the chemotherapy agent of choice (Bensinger,
2009). Total body irradiation is no longer routinely used as part
of the conditioning regimen because of increased toxicity without survival benefit (Moreau et al., 2002). The standard dose of
high-dose melphalan is 200 mg/m2 via infusion. Dose reductions
Age
u Chronologic age does not eliminate transplantation as a treatment
option; consider physiologic age for determining eligibility.
Cardiac
u Left ventricular ejection fraction (LVEF) greater than 50%
u If LVEF is less than 50% or history of heart failure exists, evaluation
and intervention to optimize heart function are recommended.
Disease
u High risk versus standard risk
u Responding to therapy or progressing on therapy
Performance Status
u Karnofsky Performance Score (KPS) or Eastern Cooperative Oncology
Group (ECOG) provide guidance of performance status; generally,
KPS greater than 60% or ECOG performance status greater than 3 is
needed to proceed to transplantation.
Pulmonary
u Adequate lung function (diffusion capacity of the lung for carbon
monoxide) greater than 50%
u Discontinuation of tobacco products
u Treat underlying pulmonary process, including infection.
Renal Insufficiency or Failure
u If on dialysis or if creatinine clearance is less than 50 ml per minute,
medications will be renal-dose adjusted; dialysis does not preclude
transplantation as a treatment option.
Socioeconomic Factors
u Financial: Insurance coverage (e.g., private, Medicaid, Medicare)
u Social: Caregiver support during and following transplantation
u Personal philosophy: Does the patient want to undergo transplantation? Are they accepting of transfusion support?
Figure 2. Factors to Consider When Determining
Eligibility for Transplantation
Note. Based on information from Antin & Yolin Raley, 2009; Palumbo
et al., 2012.
36
are made if patients have impaired renal function, advanced age,
or comorbid conditions. A 24-hour rest period often is planned
after high-dose melphalan and before HSC infusion to avoid the
risk of cytotoxicity on newly infused HSC (Talamo et al., 2012).
Stem Cell Infusion
At this stage of the process, the previously cryopreserved HSCs
are systematically thawed and infused into the patient via a central venous catheter. The day of infusion is commonly referred
to as “Day 0.” The actual infusion can take an hour or longer,
depending on the number of frozen bags of stem cell product
to administer. The patient will have a distinctive odor after the
infusion because of the DMSO preservative, which is most noticeable with respiration and voiding. The odor has been described
as similar to creamed corn or garlic, and gradually diminishes in
two or three days. Patients also can taste the DMSO. Various studies have been conducted to attempt to decrease this unpleasant
effect. Some patients have sucked on an orange or lemon during
the infusion to decrease the taste of the DMSO (Potter, Eisenberg,
Cain, & Berry, 2011). Other activities that are part of the infusion,
such as hydration and frequent vital sign monitoring, will result
in a day-long procedure (Antin & Yolin Raley, 2009).
Supportive Therapy
Although pretransplantation testing is designed to preclude
patients with baseline renal, liver, cardiac, and pulmonary dysfunction from transplantation, end-organ complications may
occur during the pre-engraftment phase of the transplantation
process (Laffan & Biedrzycki, 2006; Pallera & Schwartzberg,
2004). HDM and AHSCT are associated with expected side effects
such as alopecia, gastrointestinal (GI) toxicities, and bone marrow
ablation. The side effects of HDM are not present at the time of
chemotherapy infusion, but are delayed as rapidly dividing cells
are damaged from the effects of HDC. Complications of end-organ
toxicity and life-threatening side effects may cause mortality not
related to relapsed disease (Sorror, 2010), such as infectious issues
and pulmonary complications. Anticipated side effects and other
pre-engraftment complications are discussed in the following
sections. An overview of common side effects associated with
MM therapies and post-transplantation symptoms also can be
found in Tables 1 and 2 on pages 17 and 19 in Miceli et al. (2013).
Alopecia: Psychosocial support and counseling regarding hair
loss is important for men and women (Hesketh et al., 2004). Use
of a wig or head gear may be comforting as well as functional
to provide safety and warmth. The expense of a wig may be
covered by insurance if ordered as a hair prosthetic.
Gastrointestinal toxicities: GI toxicity may include mucositis,
esophagitis, nausea, vomiting, and diarrhea. Antiemetic therapy,
hydration, and pain medication often are needed for management
(Antin & Yolin Raley, 2009; Rodriguez, 2010). Patients experiencing GI toxicities may develop weight loss, anorexia, dehydration,
and infection (Pallera & Schwartzberg, 2004; Rodriguez, 2010).
Mucositis is a common side effect of HDM. A study compared
sucking on ice chips versus swishing saline prior to and for two
hours following the melphalan infusion to reduce the severity
and duration of mucositis by decreasing the circulation of the
chemotherapy through the oral tissues. The findings were significant in that the incidence of grade 3–4 mucositis was only
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
Table 1. Potential Gastrointestinal Symptoms and Treatments
Toxicity
Etiology
Intervention
Abdominal pain
Bowel obstruction
Infection
Acute graft-versus-host disease
Venocclusive disease (VOD) or sinusoidal obstructive syndrome (SOS)
Surgical assessment and interventions
Appropriate antibiotics or antifungals
Immunosuppressive therapy changes, as indicated
Supportive care if VOD or SOS develops
• No standard treatment exists; however, several antithrombotic agents such as heparin or defibrotide are used.
• Other treatment strategies include prostaglandin, antithrombin III concentrate, activated protein C, and prednisone.
Acute graftversus-host
disease
Donor cells in allogeneic transplantationa
Prophylactic immunosuppression and consider modifying immunosuppressive therapy
Supportive therapy
Monitor for infection
Anorexia
Chemotherapy
Acute graft-versus-host disease
Often temporary in the pre-engraftment phase
Supportive care with hydration, electrolyte replacement, and nutritional support
Immunosuppressive therapy, as indicated
Antibiotics, antifungals, or antiviral therapy
Infection
Diarrhea
Chemotherapy
Infection
Acute graft-versus-host disease
Bowel obstruction
Supportive care consisting of electrolyte replacement and hydration
Infections such as Clostridium difficile should be treated with the appropriate antibiotics.
Immunosuppressive therapy
Glucose
abnormalities
Increase in glucose needs caused by
infection, steroids
Decrease in glucose caused by anorexia,
diarrhea, nausea, and vomiting
If increase in glucose, consider insulin replacement and treat cause.
Mucositis
Chemotherapy
Infection
Pain medication as needed
Supportive therapy consisting of hydration or electrolyte replacement
Nausea and
vomiting
Chemotherapy
Acute graft-versus-host disease
Infection
Antiemetic therapy
Immunosuppression prophylaxis ordered and modified as indicated
Antibiotics, antifungals, or antiviral prophylaxis may be ordered and changed as indicated.
If hypoglycemia, treat cause and administer glucose as indicated.
Occurs less often with autologous stem cell transplantation
Note. Based on information from Miceli et al., 2013; Pallera & Schwartzberg, 2004; Tuncer et al., 2012.
a
14% in the ice chip group compared to 74% in the saline group
(Lilleby et al., 2006). Although the results support the use of ice
chips to decrease oral mucositis during melphalan infusion, not
all centers currently use this practice.
GI toxicities can be multifactorial, and all aspects of the
symptoms should be considered. For example, a transplantation
recipient may report pain from oral mucositis. The intervention
may consist of oral care and pain management. Medication used
to control pain potentially could cause nausea and constipation,
creating a clinical challenge for the nursing staff caring for
the patient. The goal of supportive care is not only to alleviate
symptoms, but also to prevent additional GI problems such
as ileus, anorexia, and infection (Cooke, Grant, & Gemmill,
2012). Inability to maintain oral intake because of GI toxicity
may require the patient to be admitted to the hospital for closer
monitoring and medication administration. Supportive care
guidelines vary with each transplantation center (see Table 1).
Myelosuppression: When bone marrow ablation occurs, patients experience profound pancytopenia for about 10–14 days.
Anemia and thrombocytopenia are managed by transfusion
support based on laboratory parameters and patient symptoms.
Transplantation recipients receiving HDC will develop severe
neutropenia and are at risk for infection and sepsis. Infection risk
is based on the type of transplantation, source of hematopoietic
cells, underlying disease, disease status, conditioning regimen,
prior infections, and environmental exposure to micro-organisms
(Bevans et al., 2009). Antibiotics for bacteria, viruses, and
fungi are used prophylactically when the absolute neutrophil
count is less than 500 cells/dl, as well as therapeutically for
febrile neutropenia or occult infection (Subramanian, 2011).
Common sources of infection include central line infections,
GI infections such as Clostridium difficile (C. diff ), and skin
infections. However, enteric organisms (Escherichia coli)
and opportunistic infections such as Pneumocystis jiroveci
also are common during this time (Pallera & Schwartzberg,
2004). Figure 3 lists infectious organisms commonly seen in
transplantation recipients during the pre-engraftment period.
Many transplantation centers attempt to minimize infection by
recommending a low-pathogen environment. Most centers use a
Laminair flow filtration system to provide such an environment
(Solomon et al., 2010).
Renal dysfunction: Renal failure can occur at any time throughout
the spectrum of the AHSCT process. When renal problems occur
before stem cell engraftment, the cause can be multifactorial.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Clinical Updates in Transplantation 37
•
•
•
•
•
•
•
•
Bacteria
Acinetobacter
Coagulase-negative or
positive staphylococcus
Enterococcus
Escherichia coli
Klebsiella
Lactobacillus
Pseudomonas
Streptococcus
•
•
•
•
•
•
•
•
Viruses
Aspergillus
Candida
Cytomegalovirus
Fungi
Herpes simplex
Parainfluenza
Respiratory syncytial
virus
Rhinovirus
Surveillance of Potential Infectious Agents in the AHSCT Setting
• Pretransplantation viral studies are essential to identify patients
at risk for viral infections.
• Surveillance cultures (e.g., nose and throat, stool) to identify
bacterial colonization
• Galactomannan assay test to identify invasive aspergillus also
may be considered.
AHSCT—autologous hematopoietic stem cell transplantation
FIGURE 3. Infectious Organisms Commonly Seen
During Pre-Engraftment and Surveillance Suggestions
Note. Based on information from Pallera & Schwartzberg, 2004; Versluys et al., 2010; Weinstock et al., 2007.
The source of the problem often is linked to nephrotoxic medication such as antibiotics, antihypertensives, chemotherapy, or
antifungal agents. Acute renal failure from tubular necrosis may
develop. Dehydration from diarrhea, nausea and vomiting, or
anorexia also could cause impaired renal function. Other causes
of renal problems in the early phase of transplantation include
sepsis or relapsed MM (Pallera & Schwartzberg, 2004).
Pulmonary complications: Pulmonary complications are estimated to occur in 30%–60% of hematopoietic transplantation recipients. Certain chemotherapy agents can cause pulmonary complications in the early phase of transplantation. Pre-engraftment
pulmonary complications include pulmonary edema, bronchiolitis obliterans, and pneumonia (Blombery et al., 2011).
Common organisms causing pneumonia are listed in Table 3 of
Miceli et al. (2013) on page 20 of this supplement.
Diffuse alveolar hemorrhage (DAH) is characterized by multilobular culture-negative lung injury. An estimated 5% of all
HSCT recipients develop DAH, with an estimated mortality rate
of 30%–60%. Presenting symptoms include acute shortness of
breath, hemoptysis, fever, chest pain, and cough. Risk factors
include older age, total body irradiation, severe mucositis, renal insufficiency, and white blood cell recovery. The definitive
diagnosis of DAH is made by identifying bloody return on bronchoalveolar lavage. Early diagnosis is imperative, and treatment
consists of corticosteroids and supportive care (Lara & Schwartz,
2010; Pallera & Schwartzberg, 2004).
The pre-engraftment phase of transplantation clearly represents many clinical challenges for oncology nurses, including infection, GI toxicities, myelosuppression, and renal and pulmonary
complications. Recognition of these problems and appropriate
intervention will potentially prevent significant harm to patients
with MM during this phase of the transplantation process.
38
Phase 3: Engraftment
The time it takes for HSCs to migrate from the peripheral
blood to the bone marrow and begin to grow is called blood
count recovery or engraftment. Engraftment is established
when the absolute neutrophil count is greater than 500 cells/
dl for three consecutive days or greater than 1,000 cells/dl
for one day, and platelets remain greater than 20,000 cells/
dl, independent of platelet transfusions for at least seven days
(DiPersio, Stadtmauer, et al., 2009). About three weeks (days
+17 to +25) following infusion of HSCs, most acute toxicities,
including myelosuppression related to the HDC, have resolved
(Russell et al., 2013). Once the patient has no evidence of infection, has demonstrated engraftment, and establishes the ability
to maintain oral hydration and nutrition, arrangements can be
made for discharge (Pallera & Schwartzberg, 2004).
Phase 4: Post-Transplantation
As discussed in Miceli et al. (2013), the definition of posttransplantation has become less clear as more patients are
being managed as outpatients during the acute phase of their
transplantation course. For purposes of this discussion, posttransplantation refers to the time when patients leave the inpatient transplantation center and return to their home community.
Additional discussion regarding the post-transplantation phase is
included in Miceli et al (2013).
Phase 5: Late Effects
Advances in the science of HSCT, as well as advances in supportive care, have improved long-term survival of transplantation
recipients. Survivors, however, are at risk for developing late
complications secondary to pre-, peri-, and post-transplantation
exposures. Those complications may lead to significant morbidity, mortality, and impaired quality of life (Majhail & Rizzo, 2013).
Long-term complications of AHSCT can be extensive and
complicated. Every organ is potentially affected, and long-term
follow-up guidelines are in place for screening and prevention
of long-term transplantation complications. Some of the late
complications include infection, as well as respiratory, ocular,
oral, hepatic, renal, skeletal, neurologic, cardiac, and vascular
complications (Majhail & Rizzo, 2013). Secondary primary
malignancies also are a late complication for transplantation
recipients (Thomas et al., 2012). Risk factors associated with the
Implications for Practice
u
Consider all factors when determining patient eligibility for
transplantation.
uGain
knowledge of supportive care strategies within each
phase, including special considerations for allogeneic recipients, to increase the well-being and survival of patients.
u
Anticipate short- and long-term side effects with prompt
identification and intervention, when appropriate.
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
development of secondary malignancies include total body irradiation, primary disease, male gender, and pretransplantation
therapy. Although many late complications are associated with
allogeneic recipients, such as chronic graft-versus-host disease
(cGVHD), autologous recipients are at risk for late complications as well (Majhail & Rizzo, 2013) (see Table 2).
Even long after the transplantation has taken place, the risk of
infection in the patient is estimated to be 20 times higher than
reported in the general population (Savani, Griffith, Jagasia, &
Lee, 2011). Common bacterial infections include pneumococcal,
streptococcal, and hemophilus organisms. Common viral infections include cytomegalovirus and reactivation of varicella zoster.
Hepatitis B or C also can occur (Savani et al., 2011). Please refer
to Miceli et al. (2013) of this supplement for more information
and guidelines for treatment of infection.
Cardiovascular disease is another late complication of transplantation. Dyslipidemia, hypertension, diabetes, and kidney
disease are associated with cardiovascular complications. The
incidence of cardiovascular disease increases after transplantation and is thought to be related to GVHD, use of immunosuppressant agents, and the cumulative effects of chemotherapy.
Other cardiovascular complications include cardiomyopathies,
arrhythmias, or valvular dysfunction (Majhail et al., 2012; Savani
et al., 2011).
Although guidelines are in place to monitor for long-term
complications, barriers exist to implementing the guidelines
(Burkhart, Wade, & Lesperance, 2013). Insurance coverage and
insufficient reimbursement for screening appear to be major barriers. Lack of awareness and inadequate communication about
the guidelines are other reasons for guideline nonadherence.
identify potential problems and implement strategies to manage the care of patients experiencing transplantation-related
complications, both short- and long-term. Knowledge of the
expected side effects and nursing interventions at each phase
of the transplantation process will help patients and caregivers through this challenging process, improve outcomes, and
enhance quality of life.
The authors gratefully acknowledge Brian G.M. Durie, MD,
Robert A. Kyle, MD, and Diane P. Moran, RN, MA, EdM, senior
vice president of strategic planning at the International Myeloma
Foundation, for their critical review of the manuscript.
Table 2. Screening and Preventive Practices
for Long-Term Survivors After AHSCT
Organ
Cardiac or
vascular
Education of heart-healthy lifestyle
Endocarditis prophylaxis
Early interventions for cardiovascular problems
Monitor ferritin at one year for iron overload.
Endocrine or
fertility
Monitor thyroid function test.
Referral to appropriate specialist
Birth control if indicated
Immune system
Immunization
Pneumocystis jiroveci pneumonia and antiviral
prophylaxis
Monitor for encapsulated organisms.
Liver
Monitor liver function tests.
Consider liver biopsy if indicated.
Viral load monitoring and liver biopsy in patients
with known hepatitis B or C
Monitor serum ferritin at one year.
Musculoskeletal
Consider chronic graft-versus-host disease changes.
Encourage activity.
Vitamin D and calcium replacement
Consider bisphosphonate therapy.
Consider dual photon densitometry at one year.
Respiratory
Constant physical examination for pulmonary
complications
Smoking cessation
Ocular
Schedule regular ophthalmology examinations.
Oral
Schedule regular dental examinations.
Ongoing oral examinations
Renal
Aggressively manage hypertension.
Monitor renal function.
Secondary
malignancies
Educate patients regarding risks adding to cancer
diagnosis (e.g., smoking, sun exposure).
Follow general population recommendations for
cancer screening.
Consider second malignancies based on symptoms.
Monitor blood work on a regular basis, specifically
complete blood cell levels.
Implications for Nursing Practice
The role of HSCT in patients with MM is complex from the
selection process to side effects and long-term management.
Nurses play a critical role in the care of patients with MM
because the nurse will anticipate and manage side effects and
provide education and support to patients and caregivers. An
enhanced understanding of the process is necessary to meet
the needs of patients and caregivers.
Conclusion
HSCT remains an important treatment option for patients
with MM. Eligibility is based on many factors and should be
determined by the transplantation provider. Overall, the procedure is well tolerated in the autologous setting, with a low
mortality rate in patients with MM (Kumar, 2009). Treatmentrelated mortality is much greater in the allogeneic setting;
therefore, it is only recommended in the context of a clinical
trial with a focus on individuals with high-risk disease characteristics. The goal of transplantation is to reinforce the response
achieved by induction therapy and improve progression-free
survival and overall survival. Acute and manageable side effects
are an expected part of the transplantation process, with an
anticipated period of post-transplantation recovery. Survivors
of HSCT are at risk for developing complications for the remainder of their lives. Nurses must have adequate information to
Screening Consideration
AHSCT—autologous hematopoietic stem cell transplantation
Note. Based on information from Majhail & Rizzo, 2013; Savani et al.,
2011.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Clinical Updates in Transplantation 39
References
Adel, N.G., Duck, E., Collum, K., Mccullagh, E., Reich, L., Landau,
H., . . . Hassoun, H. (2011). Cost analysis of using plerixafor plus
G-CSF versus cyclophosphamide plus G-CSF for autologous stem
cell mobilization in multiple myeloma patients treated at Memorial Sloan-Kettering Cancer Center [Abstract 3537]. ASH Annual
Meeting Abstracts, 118, 4059.
Amgen Inc. (2013). Neupogen® (filgrastim) [Package insert]. Retrieved from http://pi.amgen.com/united_states/neupogen/neupo
gen_pi_hcp_english.pdf
Antin, J.H., & Yolin Raley, D. (2009). Stem cell sources. In J.H.
Antin & D. Yolin Raley (Eds.), Manual of stem cell and bone
marrow transplantation (pp. 9–15). New York, NY: Cambridge
University Press.
Bensinger, W.I. (2009). Role of autologous and allogeneic stem cell
transplantation in myeloma. Leukemia, 23, 442–448.
Bevans, M., Tierney, D.K., Bruch, C., Burgunder, M., Castro, K., Ford,
R., . . . Schmit-Pokorny, K. (2009). Hematopoietic stem cell transplantation nursing: A practice variation study [Online exclusive].
Oncology Nursing Forum, 36, E317–E325. doi:10.1188/09.ONF
.E317-E325
Blombery, P., Prince, H.M., Worth, L.J., Main, J., Yang, M., Wood,
E.M., & Westerman, D.A. (2011). Prophylactic intravenous immunoglobulin during autologous haematopoietic stem cell transplantation for multiple myeloma is not associated with reduced
infectious complications. Annals of Hematology, 90, 1167–1172.
doi:10.1007/s00277-011-1275-3
Burkhart, M.C., Wade, J., & Lesperance, V. (2013). Evidence-based
guideline recommendations: Post-hematopoietic stem cell transplantation [Online exclusive]. Clinical Journal of Oncology
Nursing, 17, E63–E67. doi:10.1188/13.CJON.E63-E67
Calandra, G., McCarty, J., McGuirk, J., Tricot, G., Crocker, S.A.,
Badel, K., . . . Bridger, G. (2008). AMD3100 plus G-CSF can successfully mobilize CD34+ cells from non-Hodgkin’s lymphoma,
Hodgkin’s disease and multiple myeloma patients previously
failing mobilization with chemotherapy and/or cytokine treatment: Compassionate use data. Bone Marrow Transplantation,
41, 331–338. doi:10.1038/sj.bmt.1705908
Cavo, M., Rajkumar, S.V., Palumbo, A., Moreau, P., Orlowski, R.,
Bladé, J., . . . Lonial, S. (2011). International Myeloma Working
Group consensus approach to the treatment of multiple myeloma
patients who are candidates for autologous stem cell transplantation. Blood, 117, 6063–6073. doi:10.1182/blood-2011-02-297325
Chanan-Khan, A.A., & Giralt, S. (2010). Importance of achieving
a complete response in multiple myeloma, and the impact of
novel agents. Journal of Clinical Oncology, 28, 2612–2624.
doi:10.1200/JCO.2009.25.4520
Cooke, L., Grant, M., & Gemmill, R. (2012). Discharge needs of
allogeneic transplantation recipients [Online exclusive]. Clinical
Journal of Oncology Nursing, 16, E142–E149. doi:10.1188/12
.CJON.E142-E149
DiPersio, J.F., Stadtmauer, E.A., Nademanee, A., Micallef, I.N., Stiff,
P.J., Kaufman, J.L., . . . Calandra, G. (2009). Plerixafor and G-CSF
versus placebo and G-CSF to mobilize hematopoietic stem cells
for autologous stem cell transplantation in patients with multiple
myeloma. Blood, 113, 5720–5726.
DiPersio, J.F., Uy, G.L., Yasothan, U., & Kirkpatrick, P. (2009). Plerixafor. Nature Reviews. Drug Discovery, 8, 105–107.
Durie, B.G., Harousseau, J.L., Miguel, J.S., Bladé, J., Barlogie, B.,
Anderson, K., . . . Rajkumar, S.V. (2006). International uniform response criteria for multiple myeloma. Leukemia, 20, 1467–1473.
40
El-Cheikh, J., Crocchiolo, R., Furst, S., Stoppa, A.M., Ladaique,
P., Faucher, C., . . . Blaise, D. (2013). Long-term outcome after
allogeneic stem cell transplantation with reduced-intensity conditioning in patients with multiple myeloma. American Journal
of Hematology, 88, 370–374. doi:10.1002/ajh.23412
Flomenberg, N., Devine, S.M., DiPersio, J.F., Liesveld, J.L., McCarty,
J.M., Rowley, S.D., . . . Calandra, G. (2005). The use of AMD3100
plus G-CSF for autologous hematopoietic progenitor cell mobilization is superior to G-CSF alone. Blood, 106, 1867–1874.
Genzyme Corporation. (2010). Mozobil® (plerixafor injection)
[Package insert]. Retrieved from http://www.mozobil.com/
document/Package_Insert.pdf
Gertz, M.A., Wolf, R.C., Micallef, I.N., & Gastineau, D.A. (2010). Clinical
impact and resource utilization after stem cell mobilization failure
in patients with multiple myeloma and lymphoma. Bone Marrow
Transplantation, 45, 1396–1403. doi:10.1038/bmt.2009.370
Giralt, S. (2012). Stem cell transplantation for multiple myeloma:
Current and future status. Hematology, 17(Suppl. 1), S117–S120.
Giralt, S., Stadtmauer, E.A., Harousseau, J.L., Palumbo, A., Bensinger,
W., Comenzo, R.L., . . . Durie, B.G. (2009). International Myeloma
Working Group (IMWG) consensus statement and guidelines
regarding the current status of stem cell collection and high-dose
therapy for multiple myeloma and the role of plerixafor (AMD
3100). Leukemia, 23, 1904–1912. doi:10.1038/leu.2009.127
Gopal, A.K., Harami, M., Mayor, J., Macebeo, M., Linenberger, M.,
Bensinger, W.I., & Holmberg, L. (2012). The effective use of
plerixafor as a real-time rescue strategy for patients poorly mobilizing autologous CD34(+) cells. Journal of Clinical Apheresis,
27(2), 81–77. doi:10.1002/jca.21206
Harvey, R.D., Lonial, S., Renfroe, H., Sinha, R., Flowers, C.R.,
Lechowicz, M.J., . . . Kaufman, J.L. (2011). Temporal changes in
plerixafor administration do not impact hematopoietic stem cell
mobilization efficacy: Results of a prospective clinical trial [Abstract 2988]. Retrieved from https://ash.confex.com/ash/2011/
webprogram/Paper35916.html
Hesketh, P.J., Batchelor, D., Golant, M., Lyman, G.H., Rhodes, N., &
Yardley, D. (2004). Chemotherapy-induced alopecia: Psychosocial
impact and therapeutic approaches. Supportive Care in Cancer,
12, 543–554.
Jakubowiak, A.J., Dytfeld, D., Griffith, K.A., Lebovic, D., Vesole,
D.H., Jagannath, S., . . . Vij, R. (2012). A phase 1/2 study of
carfilzomib in combination with lenalidomide and low-dose
dexamethasone as a frontline treatment for multiple myeloma.
Blood, 120, 1801–1809. doi:10.1182/blood-2012-04-422683
Koreth, J., Stevenson, K.E., Kim, H.T., McDonough, S.M., Bindra,
B., Armand, P., . . . Alyea, E.P., 3rd. (2012). Bortezomib-based
graft-versus-host disease prophylaxis in HLA-mismatched unrelated donor transplantation. Journal of Clinical Oncology, 30,
3202–3208. doi:10.1200/JCO.2012.42.0984
Kumar, S. (2009). Stem cell transplantation for multiple myeloma. Current Opinion in Oncology, 21, 162–170. doi:10.1097/CCO.0b013e
328324bc04
Kurtin, S., Lilleby, K., & Spong, J. (2013). Caregivers of multiple
myeloma survivors. Clinical Journal of Oncology Nursing,
17(Suppl., 2), 25–32.
Laffan, A., & Biedrzycki, B. (2006). Immune reconstitution: The
foundation for safe living after an allogeneic hematopoietic stem
cell transplantation. Clinical Journal of Oncology Nursing, 10,
787–794. doi:10.1188/06.CJON.787-794
Lara, A.R., & Schwartz, M.I. (2010). Diffuse alveolar hemorrhage.
Chest, 137, 1164–1171. doi:10.1378/chest.08-2084
Lilleby, K., Garcia, P., Gooley, T., McDonnell, P., Taber, R., Holmberg,
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
L., . . . Bensinger, W. (2006). A prospective, randomized study
of cryotherapy during administration of high-dose melphalan to
decrease the severity and duration of oral mucositis in patients
with multiple myeloma undergoing autologous peripheral blood
stem cell transplantation. Bone Marrow Transplantation, 37,
1031–1035. doi:10.1038/sj.bmt.1705384
Lokhorst, H., Einsele, H., Vesole, D., Bruno, B., San Miguel, J., PérezSimon, J.A., . . . Bensinger, W. (2010). International Myeloma Working Group consensus statement regarding the current status of
allogeneic stem-cell transplantation for multiple myeloma. Journal
of Clinical Oncology, 28, 4521–4530. doi:10.1200/JCO.2010.29.7929
Majhail, N.S., Rizzo, J.D., Lee, S.J., Aljurf, M., Atsuta, Y., Bonfim, C.,
. . . Tichelli, A. (2012). Recommended screening and preventive practices for long-term survivors after hematopoietic cell
transplantation. Bone Marrow Transplantation, 47, 337–341.
doi:10.1038/bmt.2012.5
Majhail, N.S., & Rizzo, J.D. (2013). Surviving the cure: Long term
followup of hematopoietic cell transplant recipients. Bone Marrow Transplantation, 48, 1145–1151. doi:10.1038/bmt.2012.258
Martin, P.J., Schoch, G., Fisher, L., Byers, V., Anasetti, C., Appelbaum, F.R., . . . Sanders, J.E. (1990). A retrospective analysis of
therapy for acute graft-versus-host disease: Initial treatment.
Blood, 76, 1464–1472.
Mattson, M.R. (2007). Graft-versus-host disease: Review and nursing implications. Clinical Journal of Oncology Nursing, 11,
325–328. doi:10.1188/07.CJON.325-328
Micallef, I.N., Sinha, S., Gastineau, D.A., Wolf, R., Inwards, D.J.,
Gertz, M.A., . . . Kumar, S. (2013). Cost-effectiveness analysis of
a risk-adapted algorithm of plerixafor use for autologous peripheral blood stem cell mobilization. Biology of Blood and Marrow
Transplantation, 19, 87–93. doi:10.1016/j.bbmt.2012.08.010
Miceli, T., Lilleby, K., Noonan, K., Kurtin, S., Faiman, B., & Mangan,
P.A. (2013). Autologous hematopoietic stem cell transplantation
for patients with multiple myeloma: An overview for nurses in
community practice. Clinical Journal of Oncology Nursing,
17(Suppl., 2), 13–24.
Moreau, P., Facon, T., Attal, M., Hulin, C., Michallet, M., Maloisel, F.,
. . . Harousseau, J.L. (2002). Comparison of 200 mg/m2 melphalan and 8 Gy total body irradiation plus 140 mg/m2 melphalan
as conditioning regimens for peripheral blood stem cell transplantation in patients with newly diagnosed multiple myeloma:
Final analysis of the Intergroupe Francophone du Myélome 9502
randomized trial. Blood, 99, 731–735. doi:10.1182/blood.V99.3.731
National Cancer Institute. (2013). FDA approval for plerixafor.
Retrieved from http://www.cancer.gov/cancertopics/druginfo/
fda-plerixafor
Pallera, A.M., & Schwartzberg, L.S. (2004). Managing the toxicity
of hematopoietic stem cell transplant. Journal of Supportive
Oncology, 2, 223–237.
Palumbo, A., Bladé, J., Boccadoro, M., Palladino, C., Davies, F., Dimopoulos, M., . . . San Miguel, J. (2012). How to manage neutropenia in multiple myeloma. Clinical Lymphoma, Myeloma and
Leukemia, 12(1), 5–11. doi:10.1016/j.clml.2011.11.001
Pasquini, M.C., & Wang, Z. (2011). Current use and outcome of hematopoietic stem cell transplantation: CIBMTR summary slides,
2011. Retrieved from http://www.cibmtr.org/ReferenceCenter/
SlidesReports/SummarySlides/Pages/index.aspx
Potter, P., Eisenberg, S., Cain, K.C., & Berry, D.L. (2011). Orange
interventions for symptoms associated with dimethyl sulfoxide
during stem cell reinfusions: A feasibility study. Cancer Nursing,
34, 361–368. doi:10.1097/NCC.0b013e31820641a5
Richardson, P.G., Weller, E., Lonial, S., Jakubowiak, A.J., Jagannath,
S., Raje, N.S., . . . Anderson, K.C. (2010). Lenalidomide, bortezomib, and dexamethasone combination therapy in patients
with newly diagnosed multiple myeloma. Blood, 116, 679–686.
doi:10.1182/blood-2010-02-268862
Rodriguez, A.L. (2010). Management and evaluation of patients
receiving high-dose chemotherapy with stem cell transplantation. In J.D. Tariman (Ed.), Multiple myeloma: A textbook for
nurses (pp. 155–172), Pittsburgh PA: Oncology Nursing Society.
Rosiñol, L., Oriol, A., Teruel, A.I., Hernández, D., López-Jiménez, J., de
la Rubia, J., . . . Bladé, J. (2012). Superiority of bortezomib, thalidomide, and dexamethasone (VTD) as induction pretransplantation
therapy in multiple myeloma: A randomized phase 3 PETHEMA/
GEM study. Blood, 120, 1589–1596.
Russell, N., Douglas, K., Ho, A.D., Mohty, M., Carlson, K., Ossenkoppele, G.J., . . . Chabannon, C. (2013). Plerixafor and granulocyte
colony-stimulating factor for first-line steady-state autologous
peripheral blood stem cell mobilization in lymphoma and
multiple myeloma: Results of the prospective PREDICT trial.
Haematologica, 98, 172–178. doi:10.3324/haematol.2012.071456
Savani, B.N., Griffith, M.L., Jagasia, S., & Lee, S.J. (2011). How I treat
late effects in adults after allogeneic stem cell transplantation.
Blood, 117, 3002–3007. doi:10.1182/blood-2010-10-263095
Solomon, S.R., Matthews, R.H., Barreras, A.M., Bashey, A., Manion,
K.L., McNutt, K., . . . Holland, H.K. (2010). Outpatient myeloablative allo-SCT: A comprehensive approach yields decreased
hospital utilization and low TRM. Bone Marrow Transplantation, 45, 468–475. doi:10.1038/bmt.2009.234
Sorror, M.L. (2010). Comorbidities and hematopoietic cell transplantation outcomes. Hematology, 2010, 237–246. doi:10.1182/
asheducation-2010.1.237
Subramanian, A.K. (2011). Antimicrobial prophylaxis regimens following transplantation. Current Opinion in Infectious Diseases,
24, 344–349. doi:10.1097/QCO.0b013e328348b379
Sung, A.D., & Chao, N.J. (2013). Concise review: Acute graft-versushost disease: Immunobiology, prevention, and treatment. Stem Cells
Translational Medicine, 2(1), 25–32. doi:10.5966/sctm.2012-0115
Talamo, G., Rakszawski, K.L., Rybka, W.B., Dolloff, N.G., Malysz,
J., Berno, T., & Zangari, M. (2012). Effect of time to infusion of
autologous stem cells (24 versus 48 hours) after high-dose melphalan in patients with multiple myeloma. European Journal of Haemoatology, 89, 145–150. doi:10.1111/j.1600-0609.2012.01795.x
Thomas, A., Mailankody, S., Korde, N., Kristinsson, S.Y., Turesson,
I., & Landgren, O. (2012). Second malignancies after multiple
myeloma: From 1960s to 2010s. Blood, 119, 2731–2737.
Tuncer, H.H., Rana, N., Milani, C., Darko, A., & Al-Homsi, S.A.
(2012). Gastrointestinal and hepatic complication of hematopoietic stem cell transplantation. World Journal of Gastroenterology, 18, 1851–1860. doi:10.3748/wjg.v18.i16.1851
Versluys, A.B., Rossen, J.W., van Ewijk, B., Schuurman, R., Bierings,
M.B., & Boelens, J.J. (2010). Strong association between respiratory viral infection early after hematopoietic stem cell transplantation and the development of life-threatening acute and chronic
alloimmune lung syndromes. Biology of Blood and Marrow
Transplantation, 16, 782–791. doi:10.1016/j.bbmt.2009.12.534
Weinstock, D.M., Conlon, M., Iovino, C., Aubrey, T., Gudiol, C.,
Riedel, E., . . . Zuccotti, G. (2007). Colonization, bloodstream
infection, and mortality caused by vancomycin-resistant enterococcus early after allogeneic hematopoietic stem cell transplant.
Biology of Blood and Marrow Transplantation, 13, 615–621.
Williams, S.F., Zimmerman, T., Grad, G., & Mick, R. (1993). Source
of stem cell rescue: Bone marrow versus peripheral blood progenitors. Journal of Hematotherapy, 2, 521–523.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Clinical Updates in Transplantation 41
n Article
Autologous Hematopoietic Stem Cell
Transplantation for Multiple Myeloma:
Frequently Asked Questions
Patricia A. Mangan, MSN, APRN-BC, Charise L. Gleason, MSN, ANP-C, AOCNP®, and Teresa Miceli, RN, BSN, OCN®
© Thinkstock.com
When caring for patients with multiple myeloma, questions often arise about the role and timing
of autologous hematopoietic stem cell transplantation. As a complement to the other articles in
this supplement, as well as to ensure that readers are provided with the insight needed to feel
comfortable speaking to patients and other practitioners about this topic, the authors address
eight frequently asked questions about common decision points in the process of autologous
hematopoietic stem cell transplantation as a treatment for patients with multiple myeloma.
Patricia A. Mangan, MSN, APRN-BC, is the nurse lead in the Department of Hematologic Malignancies and Bone Marrow and Stem Cell Transplant Programs in the
Abramson Cancer Center at the University of Pennsylvania in Philadelphia; Charise L. Gleason, MSN, ANP-C, AOCNP®, is a nurse practitioner in the Winship Cancer
Institute at Emory University in Atlanta, GA; and Teresa Miceli, RN, BSN, OCN®, is a bone marrow transplantation nurse coordinator and assistant professor of nursing
in the College of Medicine in the William von Liebig Transplant Center at the Mayo Clinic in Rochester, MN. The authors received editorial support from Alita Anderson, MD, with Eubio Medical Communications in preparation of this article supported by Sanofi Oncology. The authors are fully responsible for content and editorial
decisions about this article. Mangan is on the speakers bureaus of Celgene Corporation, Millennium: The Takeda Oncology Company, and Onyx Pharmaceuticals, and
serves as a consultant for Sanofi Oncology; and Gleason serves a consultant for Celgene Corporation. Miceli has no financial relationships to disclose. The content
of this article has been reviewed by independent peer reviewers to ensure that it is balanced, objective, and free from commercial bias. No financial relationships
relevant to the content of this article have been disclosed by the independent peer reviewers or editorial staff. Mangan can be reached at patricia.mangan@uphs
.upenn.edu, with copy to editor at CJONEditor@ons.org. (Submitted July 2013. Revision submitted September 2013. Accepted for publication September 8, 2013.)
Digital Object Identifier:10.1188/13.CJON.43-47
Who are the best candidates
for transplantation?
Multiple myeloma is the leading indication for autologous hematopoietic stem cell transplantation (AHSCT) in North America, which has become the standard of care for patients aged 65
years and younger (Gertz, Ghobrial, & Luc-Harousseau, 2009;
Giralt et al., 2009; Moreau, Avet-Loiseau, Harousseau, & Attal,
2011; Palumbo & Anderson, 2011; Palumbo, Attal, & Roussel,
2011; Pasquini & Wang, 2012). Several randomized clinical trials demonstrated a superior survival outcome for patients who
underwent high-dose melphalan and AHSCT when compared
to those who received standard-dose chemotherapeutic agents
(Attal et al., 1996; Matsui, Borrello, & Mitsiades, 2012; Palumbo,
Attal, et al., 2011). Although most of those trials were conducted
before newer agents such as lenalidomide, bortezomib, and
thalidomide were available, more recent comparative trials using lenalidomide-containing initial regimens, with or without
AHSCT, continue to demonstrate superiority of survival. One
study stated that progression-free survival (PFS) at two years is
73% with transplantation compared to 43% without transplantation (Palumbo, Cavallo, et al., 2011). With that in mind, AHSCT
should at least be considered for all patients with active multiple
myeloma who have adequate organ function and performance
status (Palumbo & Rajkumar, 2010).
AHSCT is not without risk and results in morbidity and mortality for 1%–2% of patients, usually from infection, bleeding,
or organ toxicity (Hari & McCarthy, 2013). Patients with poor
performance status are at a higher risk for these complications.
Organ dysfunction, including compromised cardiac or liver
function, as well as renal insufficiency, also predict a higher risk
of toxicity and may lead to poor outcomes (Cavo et al., 2011;
Palumbo & Anderson, 2011). Patients older than 70 years can undergo transplantation, but the incremental benefit of transplantation in this age group has not been demonstrated in randomized,
prospective clinical trials. In addition, the standard dose of melphalan (200 mg/m2) has been shown to be of increased toxicity
in patients older than 70 years with poor performance status
and other comorbidities. A risk-adapted dosing of melphalan for
patients older than aged 70 years (e.g., 140 mg/m2) and patients
with renal insufficiency (100 mg/m2) has allowed patients to
successfully undergo transplantation with acceptable toxicities
(Gertz et al., 2009). Therefore, the use of AHSCT in these populations should be conducted cautiously and with risk-adapted dose
modification of melphalan.
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Frequently Asked Questions
43
Patients with poor risk biology, defined by cytogenetic
abnormalities such as t(4;14), del (17p), as well as high b2 microglobulin, have shorter remission duration after AHSCT.
Although this varies widely, median overall survival in the poor
risk group can range from 18–36 months (Chang et al., 2004;
Neben et al., 2010). This group of patients is the subject of clinical trials incorporating newer agents, including next-generation
immunomodulatory medications and proteasome inhibitors that
may improve overall results (Bladé, Rosiñol, Cibeira, Rovira, &
Carreras, 2010; Palumbo & Rajkumar, 2010). Participation in
clinical trials should be encouraged whenever possible.
What is the optimal timing
for transplantation?
The role of initial therapy for patients with symptomatic myeloma is to stabilize the patient, improve any organ dysfunction,
and obtain a tumor response prior to transplantation. Patients
who attain deep remissions and reversal of organ dysfunction
have the best success following AHSCT. Whether attempting to
deepen the response by extending induction therapy is beneficial
prior to stem cell transplantation is unclear. In fact, continued
initial therapy for months after attaining a response may cause
toxicity as well as decrease the stem cell yield, particularly if
the initial therapy includes alkylating agents or prolonged use
of immunomodulatory agents (Giralt et al., 2009). Although a
complete remission is obviously favorable, treatment beyond six
cycles of therapy in an attempt to achieve a deeper remission
does not definitively improve outcome (Cavo et al., 2011).
Data comparing the benefit of induction therapy followed
by high-dose melphalan and AHSCT to up-front chemotherapy alone as initial therapy for active myeloma demonstrate
improvement in PFS, response rates, and overall survival (OS)
(Attal et al., 1996; Child et al., 2003). High-dose chemotherapy
and stem cell transplantation as part of first-line therapy after
initial response has resulted in median survival of more than
five years compared to response without AHSCT (Attal et al.,
1996; Child et al., 2003). Patients undergoing transplantation
as part of their initial line of therapy have experienced longer
event-free survival and better quality of life than patients who
undergo stem cell transplantation as a late therapy, but early
transplantation has not been shown to improve overall survival
(Cavo et al., 2011; Fermand et al., 1998; Palumbo & Anderson,
2011; Palumbo, Attal, et al., 2011). On the other hand, retrospective analyses of series of patients treated with AHSCT during
their first line of therapy have reported similar outcomes as patients treated with transplantation as part of second-line therapy
(Gertz et al., 2009; Palumbo, Attal, et al., 2011). The optimal timing for transplantation continues to be an area of investigation.
An international, prospective comparison of transplantation as
first-line therapy versus second-line therapy is underway to help
clarify this issue (ClinicalTrials.gov, n.d.a.; Moreau et al., 2011).
Despite the success of high-dose melphalan and AHSCT, the
regimen is not a curative treatment, and the majority of patients
will relapse. Many strategies have been used to improve survival for patients with multiple myeloma who have undergone
AHSCT, such as tandem transplantation, second transplanta44
tion, and using newer agents (e.g., lenalidomide, bortezomib,
thalidomide) as consolidation therapy or maintenance therapy
after stem cell transplantation.
What is the role of tandem
transplantation?
Tandem autologous transplantation occurs when two autologous transplantations are performed within a period of no more
than six months. For more than two decades, patients with multiple myeloma have successfully been treated with tandem stem
cell transplantation using high-dose melphalan. One trial showed
improved PFS and OS with tandem transplantation compared to
single transplantation (Attal et al., 2003). That study suggests that
patients who either progress after the first transplantation or are
in complete remission are less likely to benefit from the second
transplantation. Patients who achieve less than a very good partial response (VGPR) but are responding and have tolerated the
first transplantation well may be the best candidates for a second
transplantation (Bladé et al., 2010; Cavo et al., 2011; Moreau et al.,
2011). A large national trial is underway to prospectively compare
single AHSCT with tandem AHSCT, which should help clarify this
issue (ClinicalTrials.gov, n.d.b.).
What is the role of salvage
transplantation?
Mobilization techniques have improved and stem cells now
can be stored for more than a decade. Salvage AHSCT has been
used for patients who have relapsed after a prior stem cell transplantation, or who had stem cells harvested and did not initially
proceed to stem cell transplantation. Response rates in the setting of relapsed and refractory myeloma are high, although the
toxicity is increased (as high as 10% mortality versus 1%–2%
mortality when AHSCT is conducted in the initial line of therapy)
(Olin et al., 2009). Response durations also tend to be shorter
(measured in months rather than years) with a second stem cell
transplantation, or one conducted in the setting of refractory
disease (Cook et al., 2011; Olin et al., 2009). Frequently, the remission induced by a stem cell transplantation acts as a bridge to
another therapy for which the patient was not eligible because
of rapid progression of disease or organ dysfunction. An intermediate dose of melphalan (100–140 mg/m2) usually is used in
this setting, keeping in mind the patient’s performance status
and organ function and implementing the same risk-adapted approaches used for initial therapy.
What is the role of consolidation therapy
after stem cell transplantation?
Despite the improvement in survival after AHSCT, a high likelihood of disease progression remains. Interest is increasing in the
role of post-transplantation consolidation using lenalidomide, bortezomib, and alkylating agents as consolidation therapy. A number
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
of trials (Cavo et al., 2011; Hari & McCarthy, 2013) have demonstrated the feasibility of this approach, and regimens such as
bortezomib, lenalidomide, and dexamethasone and bortezomib,
thalidomide, and dexamethasone for two to four cycles following
AHSCT and prior to initiation of maintenance therapy have been
well tolerated with suggestion of improved duration of response.
Preliminary results show increasing rates of complete remission
following consolidation therapy. Once again, a number of clinical trials are prospectively analyzing the incorporation of these
regimens after stem cell transplantation.
What is the role of maintenance therapy
after autologous hematopoietic stem cell
transplantation?
Although AHSCT is associated with improved remission rates
and PFS, relapse is inevitable for almost all patients. The goal of
maintenance therapy is to prolong the duration of remission,
extend OS, maintain quality of life, and reduce toxicities (Matsui et al., 2012; Moreau et al., 2011). Maintenance therapy has
been investigated since the 1990s, and a number of approaches
have been used. Alpha interferon given subcutaneously initially
showed benefit, but prospective randomized trials demonstrated
increased toxicity without a clear survival advantage (Attal et al.,
1996; Cunningham et al., 1998). Oral thalidomide also has been
used in the maintenance setting, with several randomized trials
demonstrating improved remission rates, PFS, and OS. However,
the use of thalidomide in this setting is limited because of cumulative toxicities including neurotoxicity and the development of
resistance with prolonged exposure (Cavo et al., 2011; Gertz et
al., 2009). Pulse doses of corticosteroids (prednisone or dexamethasone) also have been used after stem cell transplantation,
showing improved PFS and tolerability with intermittent administration (Berenson et al., 2002).
A number of prospective trials have assessed low-dose lenalidomide as a maintenance therapy after AHSCT. McCarthy et al.
(2012) showed significant PFS benefit in patients who received
low-dose lenalidomide (86%) versus those who did not (58%),
in addition to an OS advantage at three years of 88% versus 80%,
respectively. Attal et al. (2012) showed a PFS benefit for the lenalidomide maintenance group at four years of 43% compared
to 22% for those who did not receive lenalidomide. In those trials, lenalidomide was given until either progression or toxicity
precluded additional use. Maintenance lenalidomide was well
tolerated with a low incidence of neurotoxicity. However, the
risk of second cancers, including solid tumor and hematologic
malignancies, increased (Attal et al., 2012; McCarthy et al., 2012).
Second cancers have been observed in patients with multiple
myeloma; however, the risk has been less than 5% in previous
studies (McCarthy et al., 2012). Most recent analyses report that
the incidence of second cancers increases to 8% for patients on
lenalidomide (McCarthy et al., 2012). When compared to the risks
of progressive myeloma, the consensus remains supportive of the
use of lenalidomide as maintenance therapy. However, research
is ongoing. Efforts are now underway to identify the mechanisms
for secondary malignancies and to determine risk factors that
might reduce the likelihood of carcinogenesis (Cavo et al., 2011).
Bortezomib as part of initial and maintenance therapy has been
shown to improve outcomes when compared to a similar regimen containing thalidomide instead of bortezomib (PFS median
survival = 13 months versus 30 months; median OS = 21 months
versus 54 months, respectively) (Sonneveld et al., 2012). When
given on a weekly or biweekly schedule, bortezomib is well tolerated, although neurotoxicity remains a potential side effect. The
relative benefit of proteasome inhibitors to immunomodulatory
agents as single-agent maintenance therapy as well as in combination continues to be an area of active investigation (Palumbo
& Anderson, 2011; Sonneveld et al., 2012). The combination of
thalidomide and bortezomib, for instance, has been shown to be
well tolerated and may result in improved disease-free outcomes
(Mateos et al., 2012).
Maintenance therapy prolongs duration of remission, particularly for those who have achieved less than a VGPR. The ultimate
benefit of maintenance therapy for those who have achieved
complete remission after transplantation remains to be determined. However, increasing knowledge suggests that continued
exposure may be advantageous even for patients in complete remission by preventing proliferation of malignant plasma cells and
by maintaining a hostile bone marrow microenvironment (Giralt,
Landau, & Palumbo, 2012; Matsui et al., 2012; McCarthy et al.,
2012). Additional evaluation may clarify the use of maintenance
in the post-transplantation setting (ClinicalTrials.gov, n.d.b).
Is there a role for transplantation
in the era of novel therapies?
Since 2000, the survival of patients with multiple myeloma has
substantially improved. The median OS for patients with multiple
myeloma in 1996 was three years; in 2012, patients had a median
OS of eight years (McCarthy et al., 2012). That is a result of the
incorporation of newer agents (e.g., thalidomide, lenalidomide,
bortezomib) and the use of high-dose melphalan and AHSCT.
Given that information, the timing of high-dose melphalan and
stem cell transplantation should be considered. As noted earlier,
despite the use of lenalidomide and dexamethasone in both
groups of patients, the incorporation of high-dose therapy and
AHSCT continues to improve the survival of patients compared
to those who did not receive transplantation (Bladé et al., 2010).
That finding may be explained by the heterogeneous nature of myeloma cells and the complementary nature of the use of high-dose
alkylating agents, such as melphalan, to overcome the resistance
mechanisms in cells that are otherwise resistant to immunomodulatory agents and bortezomib. In particular, melphalan may have
a greater effect against the myeloma stem cell. Additional studies
investigating high-dose melphalan and autologous transplantation
in the era of newer agents are ongoing.
What needs to be considered when choosing
a transplantation center?
Healthcare insurance coverage should be considered when
choosing a transplantation center. The cost of transplantation
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Frequently Asked Questions
45
can be prohibitive and requires insurance approval. Patients
without insurance will require assistance from resourceful
social workers and financial counselors to successfully undergo
transplantation. Insurance carriers frequently contract with a
select group of “centers of excellence” or other transplantation
networks that they direct their patients to for evaluation; these
may or may not be geographically close to where the patient
lives. If the third-party payer does not direct the patient to a
particular transplantation center, the primary hematologist may
refer the patient to a center with which he or she has had prior
success. Geographic location and resources available within
that community also are important factors in choice of centers.
Fortunately, most regions of the country have one or more experienced centers within close proximity of the patient in need.
Ultimately, patients and their primary oncologists need to feel
comfortable with the treatment philosophy and care approach
of their transplantation team. A listing of available transplantation centers by location, disease, and statistical review can be
found at www.CIBMTR.org or www.HRSA.gov.
Summary
Since 1998, high-dose melphalan and AHSCT have been a
standard of care for patients with multiple myeloma, particularly
when administered early in the course of disease. The willingness
of patients to participate in the randomized comparative trials
has been essential to the development of successful treatment
approaches. The current practice of combining an initial (or induction) course of chemotherapy to autologous stem cell harvest
and one or two cycles of high-dose melphalan and AHSCT followed by maintenance therapy with lenalidomide or bortezomib
has resulted in unprecedented survival for this disease. A number
of questions concerning the optimal timing, best initial therapy,
post-transplantation consolidation, and maintenance therapy still
remain. Ongoing clinical trials of innovative approaches hold
great promise that these questions will be answered soon. The
ultimate result will be improved survival and quality of life for
patients with multiple myeloma.
The authors gratefully acknowledge Brian G.M. Durie, MD, and
Diane P. Moran, RN, MA, EdM, senior vice president of strategic
planning at the International Myeloma Foundation, for their
critical review of the manuscript.
References
Attal, M., Harousseau, J.L., Facon, T., Guilhot, F., Doyen, C., Fuzibet,
J.G., . . . Bataille, R. (2003). Single versus double autologous stemcell transplantation for multiple myeloma. New England Journal
of Medicine, 349, 2495–2502. doi:10.1056/NEJMoa032290
Attal, M., Harousseau, J.L., Stoppa, A.M., Sotto, J., Fuzibet, J.G.,
Rossi, J.F., . . . Bataille, R. (1996). A prospective, randomized trial
of autologous bone marrow transplantation and chemotherapy
in multiple myeloma. New England Journal of Medicine, 335,
91–97. doi:10.1056/NEJM199607113350204
Attal, M., Lauwers-Cances, V., Marit, G., Caillot, D., Moreau, P.,
Facon, T., . . . Harousseau, J.L. (2012). Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. New
46
England Journal of Medicine, 366, 1782–1791. doi:10.1056/
NEJMoa1114138
Berenson, J.R., Crowley, J.J., Grogan, T.M., Zangmeister, J., Briggs,
A.D., Mills, G.M., . . . Salmon, S.E. (2002). Maintenance therapy
with alternate-day prednisone improves survival in multiple
myeloma patients. Blood, 99, 3136–3168. doi:10.1182/blood
.V99.9.3163
Bladé, J., Rosiñol, L., Cibeira, M.T., Rovira, M., & Carreras, E. (2010).
Hematopoietic stem cell transplantation for multiple myeloma
beyond 2010. Blood, 115, 3655–3663.
Cavo, M., Rajkumar, S.V., Palumbo, A., Moreau, P., Orlowski, R.,
Bladé, J., . . . Lonial, S. (2011). International Myeloma Working
Group consensus approach to the treatment of multiple myeloma
patients who are candidates for autologous stem cell transplantation. Blood, 117, 6063–6073. doi:10.1182/blood-2011-02-297325
Chang, H., Sloan, S., Li, D., Zhuang, L., Yi, Q.L., Chen, C.I., . . . Keith
Stewart, A. (2004). The t(4;14) is associated with poor prognosis
in myeloma patients undergoing autologous stem cell transplant.
British Journal of Haematology, 125, 64–68. doi:10.1111/j.1365
-2141.2004.04867.x
Child, J.A., Morgan, G.J., Davies, F.E., Owen, R.G., Bell, S.E, Hawkins,
K., . . . Selby, P.J. (2003). High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. New England Journal
of Medicine, 348, 1875–1883. doi:10.1056/NEJMoa022340
ClinicalTrials.gov. (n.d.a). Randomized study comparing conventional dose treatment using a combination of lenalidomide, bortezomib and dexamethasone to high-dose treatment with ASCT
in the initial management of myeloma in patients up to 65 years
of age (IFM/DFCI 2009). Retrieved from http://clinicaltrials.gov/
ct2/show/NCT01191060?term=01191060&rank=1
ClinicalTrials.gov. (n.d.b). Stem cell transplant with lenalidomide
maintenance in patients with multiple myeloma (BMT CTN 0702).
Retrieved from http://clinicaltrials.gov/show/NCT01109004
Cook, G., Liakopoulou, E., Pearce, R., Cavet, J., Morgan, G.J., Kirkland, K., . . . Marks, D.I. (2011). Factors influencing the outcome
of a second autologous stem cell transplant (AHSCT) in relapsed
multiple myeloma: A study from the British Society of Blood and
Marrow Transplantation Registry. Biology of Blood and Marrow
Transplantation, 17, 1638–1645. doi:10.1016/j.bbmt.2011.04.005
Cunningham, D., Powles, R., Malpas, J., Raje, N., Milan, S., Viner,
C., . . . Gore, M. (1998). A randomized trial of maintenance interferon following high-dose chemotherapy in multiple myeloma:
Long-term follow-up results. British Journal of Haematology,
102, 495–502. doi:10.1046/j.1365-2141.1998.00795.x
Fermand, J.P., Ravaud, P., Chevret, S., Divine, M., Leblond, V.,
Belanger, C., . . . Brouet, J.C. (1998). High-dose therapy and
autologous peripheral blood stem cell transplantation in multiple
myeloma: Up-front or rescue treatment? Results of a multicenter
sequential randomized clinical trial. Blood, 92, 3131–3136.
Gertz, M.A., Ghobrial, I., & Luc-Harousseau, J. (2009). Multiple
myeloma: Biology, standard therapy, and transplant therapy.
Biology of Blood and Marrow Transplantation, 15(Suppl.),
S46–S52. doi:10.1016/j.bbmt.2008.10.006
Giralt, S., Landau, M., & Palumbo, A. (2012). Long–term myeloma
care (maintenance and second primary malignancies). HemOnc
Today, (Suppl. to Feb 2012), 11–13.
Giralt, S., Stadtmauer, E.A., Harousseau, J.L., Palumbo, A., Bensinger,
W., Comenzo, R.L., . . . Durie, B.G. (2009). International Myeloma
Working Group (IMWG) consensus statement and guidelines
regarding the current status of stem cell collection and high-dose
therapy for multiple myeloma and the role of plerixafor (AMD
3100). Leukemia, 23, 1904–1912. doi:10.1038/leu.2009.127
December 2013 • Supplement to Volume 17, Number 6 • Clinical Journal of Oncology Nursing
Hari, P.N., & McCarthy, P.L. (2013). Multiple myeloma: Future directions in autologous transplantation and novel agents. Biology
of Blood and Marrow Transplantation, 19(Suppl.), S20–S25.
doi:10.1016/j.bbmt.2012.11.002
Mateos, M.V., Oriol, A., Martínez-López, J., Gutiérrez, N., Teruel,
A.I., López de la Guía, A., . . . San-Miguel, J.F. (2012). Maintenance
therapy with bortezomib plus thalidomide or bortezomib plus
prednisone in elderly multiple myeloma patients included in
the GEM2005MAS65 trial. Blood, 120, 2581–2588. doi:10.1182/
blood-2012-05-427815
Matsui, W., Borrello, I., & Mitsiades, C. (2012). Autologous stem cell
transplantation and multiple myeloma cancer stem cells. Biology
of Blood and Marrow Transplantation, 18(Suppl.), S27–S32.
McCarthy, P.L., Owzar, K., Hofmeister, C.C., Hurd, D.D., Hassoun, H.,
Richardson, P.G., . . . Linker, C. (2012). Lenalidomide after stemcell transplantation for multiple myeloma. New England Journal
of Medicine, 366, 1770–1781. doi:10.1056/NEJMoa1114083
Moreau, P., Avet-Loiseau, H., Harousseau, J.L., & Attal, M. (2011).
Current trends in autologous stem-cell transplantation for myeloma in the era of novel therapies. Journal of Clinical Oncology, 29, 1898–1906. doi:10.1200/JCO.2010.32.5878
Neben, K., Jauch, A., Bertsch, U., Heiss, C., Hielscher, T., Seckinger, A., . . . Goldschmidt, H. (2010). Combining information
regarding chromosomal aberrations t(4;14) and del (17p13) with
the International Staging System classification allows stratification of myeloma patients undergoing autologous stem cell
transplantation. Haematologica, 95, 1150–1157. doi:10.3324/
haematol.2009.016436
Olin, R.L., Vogl, D.T., Porter, D.L., Luger, S.M., Schuster, S.J., Tsai, D.E.,
. . . Stadtmauer, E.A. (2009). Second auto-SCT is safe and effective
salvage therapy for relapsed multiple myeloma. Bone Marrow
Transplantation, 43, 417–422. doi:10.1038/bmt.2008.334
Palumbo, A., & Anderson, K. (2011). Multiple myeloma. New England Journal of Medicine, 364, 1046–1060. doi:10.1056/NEJM
ra1011442
Palumbo, A., Attal, M., & Roussel, M. (2011). Shifts in the therapeutic paradigm for patients newly diagnosed with multiple myeloma: Maintenance therapy and overall survival. Clinical Cancer
Research, 17, 1253–1263. doi:10.1158/1078-0432.CCR-10-1925
Palumbo, A., Cavallo, F., Hardan, I., , Lupo, B., Redogila, V., Levin,
M., . . . Boccadoro, M. (2011). Melphalan/prednisone/lenidomide
(MPR) versus high-dose melphalan and autologous transplantation
(MEL200)in newly diagnosed multiple myeloma (MM) patients
<65 years: Results of a randomized phase III study. Retrieved from
https://ash.confex.com/ash/2011/webprogram/Paper36073.html
Palumbo, A., & Rajkumar, S.V. (2010). Multiple myeloma: Chemotherapy or transplantation in the era of new drugs. European
Journal of Haematology, 84, 379–390. doi:10.1111/j.1600-0609
.2010.01431.x
Pasquini, M.C., & Wang, Z. (2012). Current use and outcome of hematopoietic stem cell transplantation: CIBMTR summary slides,
2012. Retrieved from http://www.cibmtr.org/ReferenceCenter/
SlidesReports/SummarySlides/Documents/SummarySlides_2012
-revised%2010%209%202013.pptx
Sonneveld, P., Schmidt-Wolf, I.G., van der Holt, B., El Jarari, L., Bertsch,
U., Salwender, H., . . . Goldschmidt, H.M. (2012). Bortezomib induction and maintenance treatment in patients with newly diagnosed
multiple myeloma: Results of the randomized phase III HOVON-65/
GMMG-HD4 trial. Journal of Clinical Oncology, 30, 2946–2955.
doi:10.1200/JCO.2011.39.6820
Clinical Journal of Oncology Nursing • Supplement to Volume 17, Number 6 • Frequently Asked Questions
47
Clinical Journal of Oncology Nursing
is an official publication of
Oncology Nursing Society
125 Enterprise Drive
Pittsburgh, PA 15275-1214 USA
+1-412-859-6100
www.ons.org
Publication of this supplement was made possible through support
from Sanofi Oncology to the International Myeloma Foundation.