NTWC Safe Clinical Practice Bulletin (Nov 2013, Volume 29)
advertisement

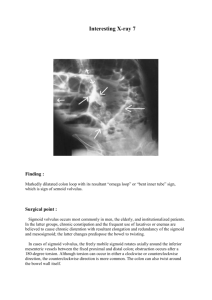
Nov 2013, Volume 29 Message of the Editor: Intestinal obstruction poses a great challenge to our colleagues. They may be found in surgical, medical or ICU settings. Diagnosis of the causes is complex and the management may be difficult. In the current issue of the bulletin, pseudoobstruction is often a forgotten category with a long list of differentials. Extensive investigations may be futile and diagnosis is usually by exclusion. Dr. Hung presented a clear algorithm on the usual management. In real life, it has to be multidisciplinary involving ICU, surgeons, GI physicians and radiologists. Is it mechanical obstruction? A patient was admitted because of abdominal distension and pain for 1 week. He had past history of DM, HT and AF on aspirin. On admission, the patient was obese. There was no fever, P=85(AF), BP=130/80. Abdomen was markedly distended. No surgical scar was evident and no cough impulse was demonstrated in the hernia orfices. There was tenderness without guarding in the central abdomen. There was no organomegaly. Bowel sound was sluggish. PR examination showed loaded rectum with brown stool. The patient was treated with IVF and NG suction. AXR revealed dilated small and large bowel. Urgent CT showed same finding with no definite transit point and there was edema of small bowel wall with possible decrease in perfusion. There mild metabolic acidosis. In view of persistent pain, the resident on-call decided for laparotomy. Intra-operative finding was bowel dilatation without ischemic change. No organic pathology was identified. The abdomen was closed with moderate difficulty. The patient ran a stormy postop course and died of pneumonia and multi-organ failure on postop day 10. Disclaimer: All the cases that are included in this Bulletin have been adopted from sources including but not limited to: international Journal publications, MPS casebook, AIRS cases from NTWC and other clusters. All the details have been modified to preserve the anonymity of the persons involved. Please send all comments and enquiries to Dr Lawrence LAI (Email: lsw448@ha.org.hk). 1 Comments of Dr L F Hung, TMH Associate Consultant (Surgery) This patient was suffering from acute colonic pseudo-obstruction (ACPO). ACPO is a clinical condition of acute large bowel obstruction without mechanical blockage. ACPO occurs most often in hospitalized patients with serious underlying medical and surgical conditions. The pathogenesis of ACPO is not completely understood, it is associated with systemic disease or disease of autonomic plexuses, other causes include laxative abuse, diabetes, hypothyroidism, systemic sclerosis or psychiatric drug treatment. ACPO can be diagnosed on the basis of CT findings that show extensive colonic dilatation without an obstructive lesion. A transitional zone may be present in some cases. CT also helps to identify any colonic ischaemia or perforation resulted from ACPO. Alternatively, colonoscopy can be used to exclude mechanical obstruction. Early recognition and appropriate management are critical to minimizing morbidity and mortality. The guideline for the treatment of ACPO suggested by the American Society of Gastrointestinal Endoscopy is as follow: Supportive management includes nothing by mouth, intravenous fluids and correct electrolytes imbalances. Nasogastric suction and rectal tube decompression. Serial physical examinations and daily abdominal radiographs help closely monitor the progress of the patient. Majority of patient (77-96%) will show clinical improvement on conservative management. Joint care among surgeons, intensivists and physicians is required. Neostigmine, a reversible acetylcholinesterase inhibitor, indirectly stimulates muscarinic receptors, thereby enhancing colonic motor activity, inducing colonic propulsion and accelerating transit. Randomized controlled trial showed that 94% patients who received neostigmine had clinical response. Colonic decompression is the initial invasive procedure of choice for patients who showed no improvement after 24–48 hours of supportive therapy, and who have failed neostigmine treatment. Rectal tube placement is recommended at the time of colonoscopy to improve the therapeutic benefit. The overall clinical success of colonoscopic decompression was 88%. Surgical management is reserved for patients with signs of colonic ischemia or perforation or who fail endoscopic and pharmacologic efforts. Surgical intervention is associated with significant morbidity and mortality (30%), likely related to the severity of the patients’ underlying medical condition. In cases of ischemic or perforated bowel, segmental or subtotal resection is indicated, with either exteriorisation or primary anastomosis. Take Home Message While most of the intestinal obstructions are mechanical in origin, one should have high index of suspicion of colonic pseudo-obstruction in patients with multiple co-morbidities. Majority of patients show response to non-surgical management (nasogastric tube suction, neostigmine, colonoscopy with rectal tube insertion). Surgical management is reserved for those who fails and complication occurs. Delay or inappropriate management may lead to significant morbidity and mortality. Disclaimer: All the cases that are included in this Bulletin have been adopted from sources including but not limited to: international Journal publications, MPS casebook, AIRS cases from NTWC and other clusters. All the details have been modified to preserve the anonymity of the persons involved. Please send all comments and enquiries to Dr Lawrence LAI (Email: lsw448@ha.org.hk). 2