15_Gade_CNV
advertisement
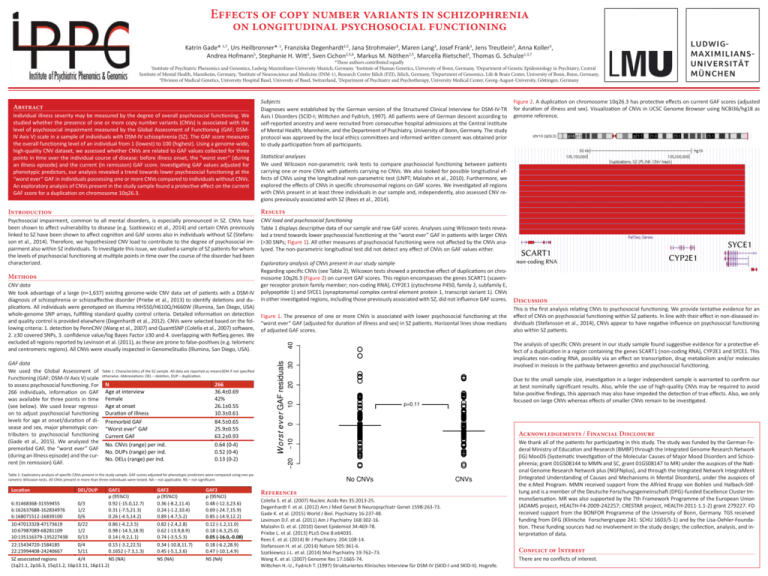
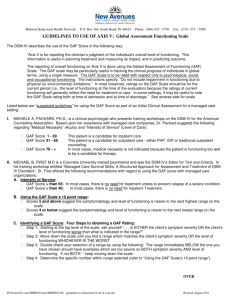
Effects of copy number variants in schizophrenia on longitudinal psychosocial functioning Katrin Gade* 1,7, Urs Heilbronner* 1, Franziska Degenhardt2,5, Jana Strohmaier3, Maren Lang3, Josef Frank3, Jens Treutlein3, Anna Koller5, Andrea Hofmann5, Stephanie H. Witt3, Sven Cichon2,5,6, Markus M. Nöthen2,5, Marcella Rietschel3, Thomas G. Schulze1,3,7 *These authors contributed equally 1 Institute of Psychiatric Phenomics and Genomics, Ludwig-Maximilians-University Munich, Germany. 2Institute of Human Genetics, University of Bonn, Germany, 3Department of Genetic Epidemiology in Psychiatry, Central Institute of Mental Health, Mannheim, Germany, 4Institute of Neuroscience and Medicine (INM-1), Research Centre Jülich (FZJ), Jülich, Germany, 5Department of Genomics, Life & Brain Center, University of Bonn, Bonn, Germany, 6 Division of Medical Genetics, University Hospital Basel, University of Basel, Switzerland, 7Department of Psychiatry and Psychotherapy, University Medical Center, Georg-August-University, Göttingen, Germany Abstract Individual illness severity may be measured by the degree of overall psychosocial functioning. We studied whether the presence of one or more copy number variants (CNVs) is associated with the level of psychosocial impairment measured by the Global Assessment of Functioning (GAF; DSMIV Axis V) scale in a sample of individuals with DSM-IV schizophrenia (SZ). The GAF score measures the overall functioning level of an individual from 1 (lowest) to 100 (highest). Using a genome-wide, high-quality CNV dataset, we assessed whether CNVs are related to GAF values collected for three points in time over the individual course of disease: before illness onset, the “worst ever” (during an illness episode) and the current (in remission) GAF score. Investigating GAF values adjusted for phenotypic predictors, our analysis revealed a trend towards lower psychosocial functioning at the “worst ever” GAF in individuals possessing one or more CNVs compared to individuals without CNVs. An exploratory analysis of CNVs present in the study sample found a protective effect on the current GAF score for a duplication on chromosome 10q26.3. Subjects Diagnoses were established by the German version of the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID-I; Wittchen and Fydrich, 1997). All patients were of German descent according to self-reported ancestry and were recruited from consecutive hospital admissions at the Central Institute of Mental Health, Mannheim, and the Department of Psychiatry, University of Bonn, Germany. The study protocol was approved by the local ethics committees and informed written consent was obtained prior to study participation from all participants. Statistical analyses We used Wilcoxon non-parametric rank tests to compare psychosocial functioning between patients carrying one or more CNVs with patients carrying no CNVs. We also looked for possible longitudinal effects of CNVs using the longitudinal non-parametric test (LNPT; Malzahn et al., 2010). Furthermore, we explored the effects of CNVs in specific chromosomal regions on GAF scores. We investigated all regions with CNVs present in at least three individuals in our sample and, independently, also assessed CNV regions previously associated with SZ (Rees et al., 2014). Results N Age at interview Female Age at onset Duraon of illness Premorbid GAF “Worst ever” GAF Current GAF No. CNVs (range) per ind. No. DUPs (range) per ind. No. DELs (range) per ind. 266 36.4±0.69 42% 26.1±0.55 10.3±0.61 84.5±0.65 25.9±0.55 63.2±0.93 0.64 (0-4) 0.52 (0-4) 0.13 (0-2) GAF1 p (95%CI) 6:31468368-31559455 0/3 0.92 (-15.0,12.7) 6:162637688-162834976 1/2 0.31 (-7.5,21.3) 6:168071512-16839100 0/6 0.26 (-4.5,14.2) 10:47013328-47173619 0/22 0.86 (-4.2,3.5) 10:67987089-68281109 1/2 0.98 (-14.5,18.9) 10:135116379-135227438 0/13 0.14 (-9.2,1.1) 22:15434720-1584185 0/4 0.15 (-3.2,22.5) 22:23994408-24240667 5/11 0.1652 (-7.3,1.3) SZ associated regions 4/4 NS (NA) (1q21.1, 2p16.3, 15q11.2, 16p13.11, 16p11.2) GAF2 p (95%CI) 0.36 (-8.2,11.4) 0.24 (-1.2,10.4) 0.89 (-4.7,5.2) 0.82 (-2.4,2.8) 0.62 (-13.9,8.9) 0.74 (-3.5,5.3) 0.34 (-10.8,11.7) 0.45 (-5.1,3.6) NS (NA) GAF3 p (95%CI) 0.48 (-12.3,23.6) 0.69 (-24.7,15.9) 0.85 (-14.9,12.2) 0.12 (-1.2,11.0) 0.18 (-6.3,25.0) 0.05 (-16.0,-0.08) 0.18 (-6.2,28.9) 0.47 (-10.1,4.9) NS (NA) 40 30 Due to the small sample size, investigation in a larger independent sample is warranted to confirm our at best nominally significant results. Also, while the use of high-quality CNVs may be required to avoid false-positive findings, this approach may also have impeded the detection of true effects. Also, we only focused on large CNVs whereas effects of smaller CNVs remain to be investigated. p=0.11 Acknowledgements / Financial Disclosure Table 2. Exploratory analysis of specific CNVs present in the study sample. GAF scores adjusted for phenotypic predictors were compared using non-parametric Wilcoxon tests. All CNVs present in more than three individuals were tested. NA – not applicable, NS – not significant. DEL/DUP The analysis of specific CNVs present in our study sample found suggestive evidence for a protective effect of a duplication in a region containing the genes SCART1 (non-coding RNA), CYP2E1 and SYCE1. This implicates non-coding RNA, possibly via an effect on transcription, drug metabolism and/or molecules involved in meiosis in the pathway between genetics and psychosocial functioning. 20 Table 1. Characteristics of the SZ sample. All data are reported as mean±SEM if not specified otherwise. Abbreviations: DEL – deletion, DUP – duplication. Figure 1. The presence of one or more CNVs is associated with lower psychosocial functioning at the “worst ever” GAF (adjusted for duration of illness and sex) in SZ patients. Horizontal lines show medians of adjusted GAF scores. This is the first analysis relating CNVs to psychosocial functioning. We provide tentative evidence for an effect of CNVs on psychosocial functioning within SZ patients. In line with their effect in non-diseased individuals (Stefansson et al., 2014), CNVs appear to have negative influence on psychosocial functioning also within SZ patients. 10 GAF data We used the Global Assessment of Functioning (GAF; DSM-IV Axis V) scale to assess psychosocial functioning. For 266 individuals, information on GAF was available for three points in time (see below). We used linear regression to adjust psychosocial functioning levels for age at onset/duration of disease and sex, major phenotypic contributers to psychosocial functioning (Gade et al., 2015). We analyzed the premorbid GAF, the “worst ever” GAF (during an illness episode) and the current (in remission) GAF. Discussion 0 CNV data We took advantage of a large (n=1,637) existing genome-wide CNV data set of patients with a DSM-IV diagnosis of schizophrenia or schizoaffective disorder (Priebe et al., 2013) to identify deletions and duplications. All individuals were genotyped on Illumina HH550/H610Q/H660W (lllumina, San Diego, USA) whole-genome SNP arrays, fulfilling standard quality control criteria. Detailed information on detection and quality control is provided elsewhere (Degenhardt et al., 2012). CNVs were selected based on the following criteria: 1. detection by PennCNV (Wang et al., 2007) and QuantiSNP (Colella et al., 2007) software, 2. ≥30 covered SNPs, 3. confidence value/log Bayes Factor ≥30 and 4. overlapping with RefSeq genes. We excluded all regions reported by Levinson et al. (2011), as these are prone to false-positives (e.g. telomeric and centromeric regions). All CNVs were visually inspected in GenomeStudio (lllumina, San Diego, USA). Exploratory analysis of CNVs present in our study sample Regarding specific CNVs (see Table 2), Wilcoxon tests showed a protective effect of duplications on chromosome 10q26.3 (Figure 2) on current GAF scores. This region encompasses the genes SCART1 (scavenger receptor protein family member; non-coding RNA), CYP2E1 (cytochrome P450, family 2, subfamily E, polypeptide 1) and SYCE1 (synaptonemal complex central element protein 1, transcript variant 1). CNVs in other investigated regions, including those previously associated with SZ, did not influence GAF scores. −10 Methods CNV load and psychosocial functioning Table 1 displays descriptive data of our sample and raw GAF scores. Analyses using Wilcoxon tests revealed a trend towards lower psychosocial functioning at the “worst ever” GAF in patients with larger CNVs (>30 SNPs; Figure 1). All other measures of psychosocial functioning were not affected by the CNVs analyzed. The non-parametric longitudinal test did not detect any effect of CNVs on GAF values either. −20 Psychosocial impairment, common to all mental disorders, is especially pronounced in SZ. CNVs have been shown to affect vulnerability to disease (e.g. Szatkiewicz et al., 2014) and certain CNVs previously linked to SZ have been shown to affect cognition and GAF scores also in individuals without SZ (Stefansson et al., 2014). Therefore, we hypothesized CNV load to contribute to the degree of psychosocial impairment also within SZ individuals. To investigate this issue, we studied a sample of SZ patients for whom the levels of psychosocial functioning at multiple points in time over the course of the disorder had been characterized. W orst ever GAF residuals Introduction Locaon Figure 2. A duplication on chromosome 10q26.3 has protective effects on current GAF scores (adjusted for duration of illness and sex). Visualization of CNVs in UCSC Genome Browser using NCBI36/hg18 as genome reference. No CNVs CNVs References Colella S. et al. (2007) Nucleic Acids Res 35:2013-25. Degenhardt F. et al. (2012) Am J Med Genet B Neuropsychiatr Genet 159B:263-73. Gade K. et al. (2015) World J Biol. Psychiatry 16:237-48. Levinson D.F. et al. (2011) Am J Psychiatry 168:302-16. Malzahn D. et al. (2010) Genet Epidemiol 34:469-78. Priebe L. et al. (2013) PLoS One 8:e64035. Rees E. et al. (2014) Br J Psychiatry. 204:108-14. Stefansson H. et al. (2014) Nature 505:361-6. Szatkiewicz J.L. et al. (2014) Mol Psychiatry 19:762–73. Wang K. et al. (2007) Genome Res 17:1665-74. Wittchen H.-U., Fydrich T. (1997) Strukturiertes Klinisches Interview für DSM-IV (SKID-I und SKID-II). Hogrefe. We thank all of the patients for participating in this study. The study was funded by the German Federal Ministry of Education and Research (BMBF) through the Integrated Genome Research Network (IG) MooDS (Systematic Investigation of the Molecular Causes of Major Mood Disorders and Schizophrenia; grant 01GS08144 to MMN and SC, grant 01GS08147 to MR) under the auspices of the National Genome Research Network plus (NGFNplus), and through the Integrated Network IntegraMent (Integrated Understanding of Causes and Mechanisms in Mental Disorders), under the auspices of the e:Med Program. MMN received support from the Alfried Krupp von Bohlen und Halbach-Stiftung and is a member of the Deutsche Forschungsgemeinschaft (DFG)-funded Excellence Cluster ImmunoSensation. MR was also supported by the 7th Framework Programme of the European Union (ADAMS project, HEALTH-F4-2009-242257; CRESTAR project, HEALTH-2011-1.1-2) grant 279227. FD received support from the BONFOR Programme of the University of Bonn, Germany. TGS received funding from DFG (Klinische Forschergruppe 241: SCHU 1603/5-1) and by the Lisa-Oehler-Foundation. These funding sources had no involvement in the study design; the collection, analysis, and interpretation of data. Conflict of Interest There are no conflicts of interest.