How Do We Best Prevent
advertisement
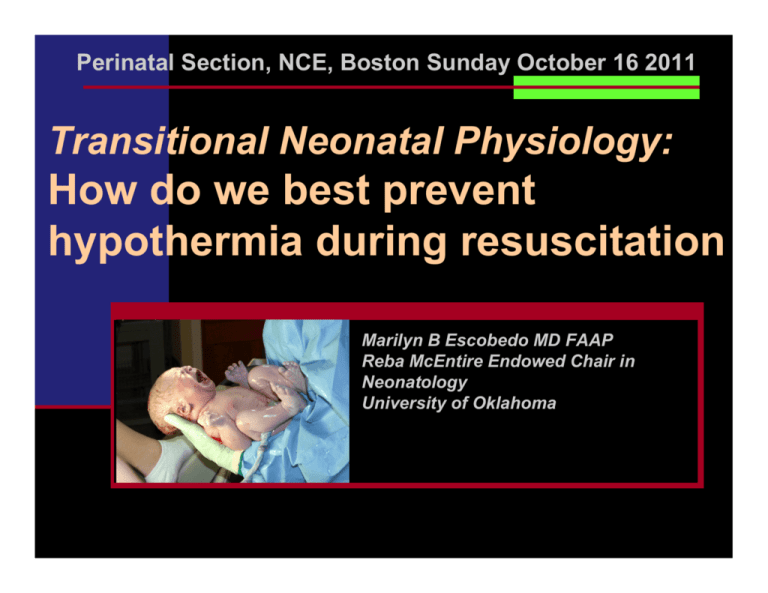
Perinatal Section, NCE, Boston Sunday October 16 2011 Transitional Neonatal Physiology: How do we best prevent hypothermia during resuscitation Marilyn B Escobedo MD FAAP Reba McEntire Endowed Chair in Neonatology University of Oklahoma University of Oklahoma, Children’s Hospital I have nothing to disclose Learning Objectives Recall the transitional physiology of thermal regulation in the neonate Review the vulnerability of the ELGAN to excessive morbidity and mortality of hypothermia Be updated on the multiple factors that may threaten thermal integrity Become familiar with multiple methods to affect better thermal outcomes in the vulnerable group. Background About 10% of babies require some resuscitation at birth 1% need extensive resuscitation ALL need attention to thermal integrity ELGANs are the MOST vulnerable. A few words On the physiology of thermoregulation… The relationship between frogs and humans has long been debated…… How is a baby not a frog? Homeotherms increase their metabolic rate in response to cooling. Poikilotherms decrease their metabolic rate in response to cooling How is a baby not a frog? This was an evolutionary LEAP Poikiolotherms vs homeotherms Homeotherms have 2-3 times metabolic rate Homeothermy demands that heat production precisely compensates losses to the environment The human baby maintains his body temperature with energy – The human baby maintains his body temperature with energy – The human baby maintains his body temperature with energy – What is the thermoneutral zone in humans? Unclothed resting adult—23-28 C (73 F) Unclothed full term neonate—32-35 C (90 F) Unclothed 1 Kg preterm neonate– 35 C (95 F) WHO, 1997, Safe Motherhood: Thermal Protection of the Newborn, a Practical Guide PHYSICS OF HEAT TRANSFER How does this apply to the DR? LOSSES Radiation – Cold walls, all solid furnishings of the theatre, poor muscle tone increasing surface area exposed Conduction – cold blankets, instruments, mattresses Convection-Vents from HVAC system, Movement of personnel, Doors, Gases Evaporation- Amniotic fluid, no clothing How does this apply to the DR? INTERVENTIONS Radiation – Increase room temperature in advance, use radiant warmer for care Conduction – warm blankets, exothermic mattresses Convection-Design appropriate HVAC system, Be aware of movement of personnel, doors, gases, use transport incubator Evaporation- Dry or place barriers to evaporation on body and head WHEN do we need to intervene? How do we intervene? When do we intervene? To whom to we apply these techniques? Do they change outcome? Is it just theoretically important? Reduction in Mortality by Reducing Hypothermia Budin, Pierre in The Nursling Comparison of Mortality in the Maternite( the Usual standard of care) with The Tarnier ( the preventive approach to Hypothermia) 100 90 80 70 60 50 40 30 20 10 0 <32 3233.5 Silverman to Costeloe Survival significantly higher in incubators kept at 32 C. vs 29 C ( Silverman1958) Survival significantly higher in radiantly heated incubators vs convectively heated due to stability of the environmental temp ( Silverman1963) Survival improved in computer controlled SKIN temperature environment (1976 Ahlgren) Hypothermia remains an independent risk factor for mortality in very small preterm babies (Costeloe 2000) Admission temps <35 C in 40% of infants <26 wks How do we best defend the tiny baby’s thermal integrity? McCall, Alderdice, Halliday Jenkins Vohra 2010 Cochrane Review Barrier Methods to prevent evaporative heat loss Polyethylene occlusive wrapping of ELGANs immediately upon delivery (Vohra, et al J Pediatr 2004, HeLP study Decreases the incidence of hypothermia Increases the NICU admission temperature Fewer deaths (all hypothermic) but NS Prevention of Evap Heat Loss ALL the RCTs of occlusive wrapping of the very preterm baby with food grade plastic wrap Showed improved temperatures on admission to NICU of almost 1degree C Reduced the incidence of hypothermia Some have studied effects on Acid base balance RDS IVH NEC O2 need LOS None have shown an effect on Mortality Second barrier to reduction of evap loss of heat: HATS Second barrier to reduction of evap loss of heat: HATS Stockinette Hat studies by Roberts ( >31 wks) Plastic hat study by Trevisunuto Plastic hat study in progress by Wyckoff Woolen hats studied in terms ( Coles 1979; Stothers 1981; and Chaput de Saintonge 1979) NEEDS STUDY Conductive heat transfer Exothermic warming mattressess THERMAL MATTRESS vs PLASTIC WRAP RCT < 28 week Thermal warming mattresses Compared to plastic wrap Reduced hypothermia ( <0.01) Raised NICU adm temp Allowed more direct access Improved visualization Less cumbersome to apply Thermal defense of extremely low gestational age newborns during resuscitation: exothermic mattresses vs polyethylene wrap Simon Dannaway Escobedo et al J Perinatology 2010 Various Studies of warming mattresses—all positive Brennan 1996 RCT Singh 2009 Cohort, historical Almeida 2009 RCT Ibrahim 2010 Retrospective Review Caveat!! Positive transfer of radiant heat Manuel radiant warmer International Standard requires power cut and alarm if total output has been > 10mW/cm2 for >15 minutes Most warmers will have shut off before the usual 20- 30 minute resuscitation of VLBW Servo-controlled radiant warmer should probably be used or team member should be assigned to monitor temp to avoid highs and lows (Rich, Leone, Finer in Clinics in Perinatology Mar 2010) Reducing radiant heat losses beyond the warmer Delivery room temperature needs to be kept at the WHO standard of 25 degrees C or higher (mid 70s F) Environmental Temps: Birthing and Surgical Suite WHO recommendation for 25 C or greater No references Knobel (2005) post hoc analysis Subjects born in room temps > 26 had higher mean admission temps than those in =<26 Cramer (2005) Positive relationship between DR temp and NICU admission temp Kent (2008) changed environmental temp from 20 to 25-28 C along with other interventions and showed a positive effect on T. Humidified and Heated Air during Resuscitation te Pas AB. Lopriore E. Dito I. Morley CJ. Walther FJ. Pediatrics. 125(6):e1427-32, 2010 Jun. Prospective study of <33 wks "heated" cohort used heated and humidified gas during resuscitation vs “cold” cohort Temperature at admission in the NICU 35.9 vs 36.4 ( P < .0001). Normothermia (36.5 degrees C-37.5 degrees C) occurred less often in the cold cohort than in the heated cohort (12% vs 43%; P < .0001). The use of heated and humidified air during respiratory support in very preterm infants just after birth reduced the postnatal decrease in temperature What about hyperthermia? As core temperatures increase O2 consumption rises again. This is stressful for any neonate with ELGANs more susceptible If preterms also have CNS injury, the possibility of hyperthemia exacerbating the injury may exist. The evidence shows we should be preventing hypothermia. The VON report for 2010 shows a rate of about ½ of VLBWs with admission temps <36.5 C and about ¼ < 36 C Why aren’t we doing better? TIPQC- Tennessee Initiative Incidence of Hypothermia (< 36 C) on Admission to NICU MUSC 2010 Robin L. Kissinger, PhD, APRN, NNP-BC; David J. Annabale, MD Thermal Defense for Preterms Reasonable Evidence Plastic bag with hats Thermal mattresses Emerging considerations Hats Heated gases Radiant warmer The role of the delivery room temperature Effective and consistent application HOME DELIVERY IS FOR PIZZA!!!!!!! UNDERWATER BIRTH IS FOR WHALES!!! questions?