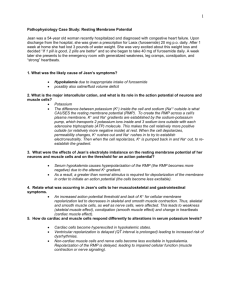
The Neuromuscular Junction
advertisement

Neuromuscular Junction Lecture Notes These notes supplement the lectures and cover background material that will help place the experiments in context. © University of Minnesota Version: July, 2011 Table of Contents 1 Muscle Contraction: cardiac, smooth and skeletal_________________________ 3 2 The Neuromuscular Junction ________________________________________ 13 3 Membrane Resting Potential _________________________________________ 21 4 NMJ References ___________________________________________________ 29 5 Readings _________________________________________________________ 31 NMJ Lecture Notes 1 1 Muscle Contraction: cardiac, smooth and skeletal 1. Types On the basis of structure, contractile properties and control mechanisms, three types of muscle can be identified: 1) skeletal muscle, 2) smooth muscle and 3) cardiac muscle. Although there are significant differences between these muscle types, the forcegenerating mechanisms are similar. Skeletal Muscle: most skeletal muscle is attached to bone and its contraction is responsible for supporting and moving the skeleton. The contraction of these muscles is initiated by action potential propagating down motoneurons to the muscle and can be under voluntary control. Smooth Muscle: sheets of smooth muscle surround various hollow organs and tubes (e.g., stomach, intestines, urinary bladder, uterus, blood vessels and airways). Contraction of these cells may propel the luminal contents through the organ or regulate internal flows by changing tube diameters. Single and groups of smooth muscle cells are also found distributed throughout organs and perform various other functions: e.g., iris of the eye and attachment of hair. Smooth muscle contraction can be spontaneous or controlled by: the autonomic nervous system, hormones and other chemical signals. Cardiac Muscle: The muscle of the heart surrounds four pumping NMJ Lecture Notes 3 chambers. Contraction of cardiac muscle provides the impetus for the movement of blood through the pulmonary and systemic circulatory systems. Spontaneous cycling of an intrinsic pacemaker triggers each heartbeat (or contraction). However the autonomic nervous system and circulating hormones modulate the frequency of this activation. 2. Structure and Function of Skeletal Muscle If one sections through a skeletal muscle, one can observed that it is organized into bundles of fibers call fascicles. The individual muscle fibers, multinucleated cells, contain long slender structures called myofibrils. These are made of myofilaments, which are organized into sarcomeres, the functional unit of contractions. Both skeletal and cardiac muscle have a striated appearance under a light microscope, due to the organization of the myofilaments. Each myofibril is composed of thick and thin filaments arranged in a repeating pattern along their length. thick filaments are composed primarily of the protein myosin and the thin filaments are made up the three proteins, troponin, tropomyosin and actin. It is the cyclic binding between myosin heads of the thick filament and actin of the thin filaments, crossbridge formation, that allows of force production or muscle shortening. It should be noted, that there exist other proteins within sarcomere which have recently been shown to have a role in contractile function, e.g., the elastic protein titan (also known as connectin). 3. The Motor Unit A single motor unit consists of one motor neuron and all of the muscle fibers it innervates. The cell bodies of motor neurons are located within the brainstem or spinal cord. The axons of these neurons are myelinated and large in diameter, and thus are able to propagate action potentials at high velocities. Once an alpha motor neuron is activated to produce an action potential, all of the fibers innervated by this neuron are activated and contract simultaneously. Each motor unit is made up of one type of muscle fibers: i.e., slow twitch, fast-twitch fatigable or fast-twitch fatigue resistant. NMJ Lecture Notes 4 4. Excitation-Contraction Coupling This refers to the sequence of events by which an action potential in the plasma membrane of the muscle fiber leads to force production via an increase in intracellular calcium and crossbridge formation and turn-over. Excitation begins at the neuromuscular junction and then the action potential spreads over the surface membrane and inward into the fiber via the transverse tubule system (invaginations of the sarcolemma). This inward excitation activates calcium release from the sarcoplasmic reticulum. The calcium then binds to the thin filament and crossbridge formation occurs. NMJ Lecture Notes 5 4. The Neuromuscular Junction Each branch of a motoneuron forms a single junction with a muscle fiber. The myelin sheath surrounding the motor axon ends near the surface of the muscle fiber and the axon divides into a number of short processes that lie embedded in grooves on the muscle-fiber surface. This region of the sarcolemma (muscle membrane) is known as the motor end plate. Acetylcholine is the neurotransmitter in these synapses. End-plate potentials (EPPs) can be recorded at the motor end plate when the presynaptic membrane is activated to release vesicles containing the acetylcholine. Steps in neuromuscular transmission: 1) nerve action potential. 2) calcium entry into the presynaptic terminus. 3) release of Ach quanta. 4) diffusion of Ach across cleft. 5) combination of Ach with post-synaptic receptors and Ach breakdown via esterase. 6) opening of Na+/K+ channels (cation channels). 7) postsynaptic membrane depolarization (EPP). 8) muscle action potential. NMJ Lecture Notes 6 5. Molecular Mechanism of Contraction Excitation of the sarcolemma and transversetubule system causes activation of a population of voltage-gate calcium channels located in the tubules themselves. The channels also known as the dihydropyridine receptors signals, by yet some unknown mechanism, the adjacent calcium-release channels on the sarcoplasmic reticulum (ryanodine receptors) to allow calcium to be released from this storage site. Hence, the intracellular [Ca2+] increases (i.e., sarcoplasmic concentration) which then diffuses and binds to troponin on the thin filaments which allows for crossbridge formation between actin and myosin by removing the steric interaction imposed by tropomyosin. Shown to the right is the association between changes in intracellular [Ca2+] and force. The change in Ca concentration is detected using a fluorescent calcium indicator dye so that changes in relative light is related to changes in calcium concentration. Note that a rise in calcium precedes force production and intracellular [Ca2+] decrease well before force. NMJ Lecture Notes 7 Functional Overview A neuromuscular junction sends excitatory signals from the CNS via the neurotransmitter, acetylcholine which binds to nicotinic receptors on the post-synaptic membrane. The binding causes a local change in the voltage of the sarcolemma affecting neighboring channels (Na+ to enter and eventually K+ to flow out). This ion movement produces the action potential which propagates along the sarcolemma and inward via the transverse tubule system. This rapid voltage change initiates the gating of dihydropyridine receptors which in turn causes the release of calcium from the sarcoplasmic reticulum via the ryanodine receptors. The released calcium binds to troponin inducing a conformation change in tropomyosin, also a component of the contractile apparatus, which in turn allows crossbridge formation between actin and myosin (an energy dependent process). The crossbridge formation leads to muscle fiber shortening and the generation of force. Crossbridge cycling will proceed until calcium dissociates from troponin and the inhibitory influence of tropomyosin is reestablished. The dissociation occurs because calcium release stops and its active uptake (requiring ATP) into the sarcoplasmic reticulum causes a reduction. 7. Metabolic pathways producing the ATP utilized during muscle contraction There are three primary ways a muscle fiber can form ATP during contractile activity: 1) phosphorylation of ADP by creatine phosphate; 2) oxidative phosphorylation of ADP in NMJ Lecture Notes 8 mitochondria (need myoglobin for oxygen transfer); or 3) substrate phosphorylation of ADP, primarily by the glycolytic pathway in the cytosol (forming lactic acid). The phosphorylation of ADP by creatine phosphate provides a very rapid means of forming ATP at the onset of contractile activity. In a resting muscle fiber, the concentration of ATP is always greater than ADP leading to the reformation of creatine phosphate. During rest muscle fibers build up a concentration of creatine phosphate to a level approximately five times that of ATP. 6. Force production: the frequency of stimulation and the length-tension relationship The amount of tension developed by a muscle fiber and thus its strength can be altered not only by the frequency of stimulation, but also by changing the length of the fiber prior to or during contraction. If the frequency of stimulation increase such that relaxation in not complete force will begin to superimpose. Eventually the frequency of stimulation becomes high enough that NMJ Lecture Notes 9 the force becomes fused. Further increase in the frequency will cause more force to be produced until eventually a maximum is reached. If one stretches skeletal or cardiac muscle the magnitude of subsequent contractions will be altered. If the muscle is unloaded, i.e., the sarcomere spacing compressed, there is little force or shortening that can occur. Skeletal muscle has an optimal length (l0) at which force is maximal due to the greatest possible numbers of crossbridges can be formed. Most muscles in the human body are attached so to have near their optimal length at rest. Because skeletal muscle can shorten allowances need to be made for the sarcolemma to also conform to this changes without being damaged. Structural proteins are present which link the myofilaments to the surface membrane and extracellular matrix. One of these proteins is dystrophin which is lacking is patients with Muscular Dystrophy. 7. Contraction in Smooth Muscle This type of muscle lacks cross-striated banding patterns and the nerves which can innervate it arise from the autonomic nervous system. Nevertheless, smooth muscle also uses cross-bridge movements between actin and myosin molecules to produce force. NMJ Lecture Notes 10 Each smooth-muscle fiber is a spindle-shaped cell with a diameter ranging between 2 and 10 µm. Smooth muscle cells have only a single nucleus and can continue to divide. Two types of filaments are present in the cytoplasm: thick filaments containing myosin and thin composed of actin. The actin filaments are anchored either to the plasma membrane or to cytoplasmic structures known as dense bodies, the smooth muscle equivalent to zlines. Tension produced by smooth muscle also varies with length, but the range of length and amount of shortening that smooth muscle can achieve is greater than skeletal muscle. The pathways leading to an increase in cytoplasmic [Ca2+] and to force generation differs significantly between smooth and skeletal muscle. Crossbridges in smooth muscle can form once myosin is phosphorylated by a calcium dependent process (enzyme). There are two sources of calcium which leads to an increase in cytoplasmic concentration prior to contractions: 1) the sarcoplasmic reticulum , and 2) extracellular calcium. NMJ Lecture Notes 11 Some smooth muscle will generate action potentials, but they differ from skeletal muscle in that Ca2+ is the primary ion responsible for the membrane depolarization. Some cells spontaneously produce action potential and have pacemaker like properties. Other types of smooth muscle are innervated by nerves. The released neurotransmitter can be released onto varicosities along the fibers or in spaces between fibers which then requires greater diffusion of the neurotransmitter to the receptor sited. In addition in certain multiunit smooth muscle arrangements, excitation may be initiated on some cells via innervation and then transmitted to additional cells via gap junctions between cells. 8. Cardiac Muscle The cardiac-muscle cells of the myocardium are arranged in layers that are tightly bound together and completely encircle the blood-filled chambers. Cardiac muscle combines the properties of both skeletal muscle and smooth muscle. The cells are striated as the result of an arrangement of thick myosin and thin actin filaments. However, cardiac cells are considerably shorter than skeletal muscle fibers and have several branching processes. Adjacent cells are joined end to end at structures called intercalated disks, within which are desmosomes that hold the cells together and to which the myofibrils are attached. Approximately 1 percent of cardiac-muscle tissue have specialized features that form the conducting system of the heart. They send information to the contractile cells via gap junctions. The conducting system initiates the heartbeat and helps spread the impulse rapidly through the heart. The heart receives a rich supply of sympathetic (norepinephrine) and parasympathetic (acetylcholine) innervation contained in the vagus nerve. On-Line Muscle References The excellent chapter on muscle from Vander, Sherman & Luciano's Human Physiology text, one of the most widely used physiology texts in the world. The chapter from the 2004 edition is available online at www.me.umn.edu/labs/hmd/lab/docs/widmaier_samplech9.pdf The Dept of Radiology at the University of Washington has an excellent upper and lower extremity Muscle Atlas with images suitable for presentations. The site has a simple and free copyright form to use the images for academic purposes. www.rad.washington.edu/atlas2/ Medline Plus has an excellent section on muscle disorders. www.nlm.nih.gov/medlineplus/muscledisorders.html NMJ Lecture Notes 12 2 The Neuromuscular Junction Each branch of a motoneuron forms a single junction with a muscle fiber. The myelin sheath surrounding the motor axon ends near the surface of the muscle fiber and the axon divides into a number of short processes that lie embedded in grooves on the muscle-fiber surface. This region of the sarcolemma (muscle cell membrane) is known as the motor end plate. Acetylcholine is the neurotransmitter in these synapses. End-plate potentials (EPPs) can be recorded at the motor end plate when the presynaptic membrane is activated to release vesicles containing the acetylcholine. 1) Nerve and muscle have separate, intact, plasmalemmas, which are separated by a 50 nm gap (500Å) known as the synaptic cleft. NMJ Lecture Notes 13 2) An unmyelinated motoneuron terminal (i.e. presynaptic end of the axon) sits in a specialized groove of the skeletal muscle fiber to form the neuromuscular end plate. a) There is only one presynaptic nerve per muscle fiber. b) Each motoneuron has several ending; each innervates only one muscle fiber. c) All of the muscle fibers in a given motor unit contract in unison when their motoneuron fires an action potential. d) All muscle fibers in a motor unit are of the same fiber type (either all-slow or fast twitch). 3) The junction or end plate region of the skeletal muscle fiber is specialized and different from the rest of the plasmalemma. a) Synaptic infoldings of the plasmalemma in the cleft greatly increase the membrane surface area. b) Receptors (protein molecules) for acetylcholine (ACHR) are located near the cleft edge of the infoldings. In denervated muscle fibers, the ACHRs spread of the entire muscle plasmalemma (sarcolemma). i) The skeletal neuromuscular junction ACHR is nicotinic sensitive receptor. ii) The nicotinic ACHR structure is well characterized (i.e., cloned and sequenced) iii) In its protein moiety, the ACHR contains: (1) Binding sites for acetylcholine (ACH) and like molecules (agonists and antagonists). (2) Ligand-gated cation channel (3) Several types of modulator sites NMJ Lecture Notes 14 c) The are 5 subunits of the ACHR: 2 alpha, beta, gamma and epsilon. d) The channel and the ACH binding sites are on the alpha subunits. e) The ACHR is a non-specific cation channel which opens and closes in response to ACH binding and unbinding (insensitive to TTX or TEA) i) In the presence of an elevated [ACH] in the cleft ACH binds to the extracellular side of the receptor and the channel opens. Fast 2[A] + [R] < -- > [AR] + [A] < -- > A2R < -- > A2R* closed closed closed open Reaction Channel States: AR Desensitized A2 R desensitized ii) The binding of the 2 ACH molecules to a single receptor elicits positive cooperativity. iii) When the ACHR channel opens at a normal muscle fiber resting membrane potential, Em =90 mV, the net current through the channel is inward and depolarizing. iv) ACH unbinds from the ACHR after the channel closes when the [ACH] in the endplate decreases due to diffusion from the cleft and is broken down by an acetylcholinesterase (ACHE). Prolonged ACH (> 100 msec) stimulation leads to inactivation of the channels through a change to the desensitized state. v) Then the end plate channel opens, net current (I) from all cations in inward: this positive charge (q+) movement through the myoplasm to the surrounding sarcolemma cause a capacitate change (depolarization) which then affects the gating of the voltage-sensitive Na+ and K+ channels. vi) vii) ACHRs can be irreversibly blocked by the snake poison Curare block binding of ACH to its receptors. Curare is a non-activating or non-depolarizing block. viii) ix) Nicotine acts at the NMJ and binds to the ACHR. There are substances, which mimic ACH, but are not readily broken down by ACHE, thus that cause and initial opening of the channel and then NMJ Lecture Notes 15 inactivation through desensitization. Succinylcholine is one of these depolarizing muscle relaxants. 4) The nerve terminal has vesicles (50 nm in diameter) containing ACH which fuse with the plasmalemma and release ACH into the cleft after the nerve AP depolarizes the membrane and Ca2+ enters through channels in the nerve terminal. a) Formation of ACH in nerve terminal. AcetylCoA + Choline Acetyl Transferase ------------------------ > ACH + CoA b) ACH is stored in vesicles in the nerve terminal. c) Quantum: Smallest amount of ACH released. Probably the amount of ACH in a “standard” presynaptic vesicle is: Quantum = 2,000 to 10,000 ACH molecules. 5) The NMJ cleft is filled with extracellular fluid and ground substance, which also contains the enzyme acetylcholinesterase (ACHE). ACHE ACH -------------- > Acetate + Choline 6) ACHE acts only on unbound ACH. Acetate and choline are transported back into the nerve terminal. Acetate is converted to acetylCoA (in mitochondria) and then combines with choline to reform ACH. a) Organophosphates inhibit ACHE and thus prolong ACH lifetime. Inhibitors of ACHE are: physostigmine and neostigmine, which are used clinically to reverse neuromuscular blockage. Characteristics of ACH release: 1) As a result of AP depolarization, Ca2+ enters the nerve terminal through a voltagegated channel. a) 4 Ca2+ act cooperatively to release one quantum. b) Reducing extracellular Ca2+ reduces ACH release. NMJ Lecture Notes 16 c) Mg2+ competes with Ca2+ and does not active ACH release; increasing extracellular Mg2+ decreases ACH release. 2) One nerve AP causes the release of approximately 300 quanta (vesicles) 1 AP ------ > 300 quanta released ----------- > 1,500,000 ACh molecules (assuming 5,000 ACH/quantum) Some of this ACH diffuses out from the cleft and some is broken down by ACHE: approximately 200,000 molecules bind to ACHR to open channels in the endplates. 3) Factors which alter or block nerve APs will alter ACH release: a) Local anesthetics (e.g., procaine) inhibit voltage-gated Na+ channels and interfere with AP transmission in the nerve. Some local anesthetics also act on the ACHR by promoting desensitization and/or by blocking the channel. b) An increase [K]o causes prolonged depolarization of the nerve and thus partial inactivation of the voltage-gated Na+ channels, thus alters AP transmission. Hemicholinium inhibits uptake of choline into the nerve terminus and thus decreases ACH production and storage. The result is decreases ACH/quantum. Botulinum toxins block the release of ACH from the nerve terminals (i.e., paralysis from bad tuns). Characteristics of the End Plate Potential (EPP): 1) Opening of the end plate channels and the subsequent net inward current sets up a transient depolarization of the sarcolemma adjacent to the end plate. a) The end plate potential (EPP) spreads electrotonically and thus decrements in amplitude with distance from the end plate region. The EPP itself in not propagated but serves as the stimulus to drive the Em to threshold for an AP to be initiated. The EPP can be seen in isolation of an AP by treating the muscle fibers with tetrodotoxin (TTX) which blocks the voltage-gated Na+ channels. b) The EPP brings the adjacent sarcolemma to and beyond threshold: the voltagegated channels in the non-endplate region of the membrane are then responsible for the propagation of the AP throughout the length of the muscle fiber. c) EPPs last approximately 5-10 msec. d) Normally: 1 nerve AP -- > 1 EPP -- > 1 muscle AP -- > a single twitch . NMJ Lecture Notes 17 e) The typical EPP amplitude is –30 mV, which represents current through approximately 100,000 open ACH endplate channels. NMJ Lecture Notes 18 2) Mini-EPPS (MEPPs) occur spontaneously independent of the nerve AP, although membrane depolarization increases and hyperpolarization decreases their frequency of occurrence. a) Are due to the release of quantum = approximately 5,000 ACH molecules. b) Amplitudes are approximately 0.5 to 1 mV. c) Ca2+ and Mg2+ do not alter the magnitude or time course of MEPPs, but due alters the number released. NMJ Lecture Notes 19 Review: Steps in neuromuscular transmission: 1) nerve action potential. 2) calcium entry into the presynaptic terminus. 3) release of Ach quanta. 4) diffusion of Ach across cleft. 5) combination of Ach with post-synaptic receptors and Ach breakdown via esterase. 6) opening of Na+/K+ channels (cation channels). 7) postsynaptic membrane depolarization (EPP). 8) muscle action potential. NMJ Lecture Notes 20 3 Membrane Resting Potential The nervous system uses electrical signals to communicate over relatively enormous 'biological distances'. It does so with speed and accuracy, and deals in a vast traffic of signals distributed to millions of cells. Present-day emphasis on the nerve membrane and the resting potential is far more than a political dogma to bedevil the student. For in understanding these processes, we glimpse the basic strategy used by neurons to carry-on their mission of information processing. This strategy--sometimes loosely called the ionic hypothesis - appears to be common to all nerve cells, and to be a specialization of the general phenomenon of irritability present in all cells from the dawn of life. Our knowledge of the, subject is by no means complete, but sufficient elements have been assembled to allow the conclusion that this strategy itself is a remarkably simple one, but also elegant in that there is a capacity for many individual variations on a common theme. The necessary elements appear to be: 1) the presence of an ionselective, semi-permeable membrane; 2) the ability of the cell to concentrate different amounts of sodium, potassium and chloride across the membrane, 3) passive physical forces of diffusion and electrical gradients; and 4) an active process (principally operating on sodium and potassium ions), that aids in maintaining the various ionic concentration profiles. 1) The Nerve Membrane. The nerve membrane has been extolled to you in biochemistry, biology and physiology, so we will not dwell in detail on it here. Suffice it to say that there exists a membrane composed basically of a bi-layer of lipid leaflets embedded in which at various distances are proteins. Many of these proteins have water permeable pores or channels in them which allow one or more ion species through. Some of these channel-bearing proteins are "gated" (can open and close as the result of something that forces a change in their structure), some are theorized to be passive and always open. These latter channels are what are called “resting channels", and we will concentrate on these, as it is thought they are responsible for the resting permeability of the membrane and therefore for the resting potential. The "gated" channels operate to produce changes in the membrane potential and therefore mediate information exchanges.1 In the absence of any active -information processing, the nerve membrane maintains a potential difference between the inside of the cell and outside of some 70 to 90 millivolts, with the inside negative (1 mV = 10-3 volts), and this voltage difference is called the 1 No one has ever "seen" a resting channel, and there are various alternative explanations that could account for the passive, resting permeability of the membrane. For instance, gated channels that flicker open and closed on a probabilistic basis could account for much of the resting permeability However, for present didactic reasons, it is easier to just theorize that resting channels exist. NMJ Lecture Notes 21 resting potential. 70 millivolts may seem like a very small electrical force compared to the 120 volts of city power you may have painfully sampled on occasion, but this 70 mV is acting across a correspondingly small distance. To obtain a "feel" for the actual force one has to look at the ratio of the resting potential to the thickness of the membrane. 70 mV across an approximately 100 membrane corresponds to a force of 70,000 volts/centimeter. This is more than adequate to make proteins with charged groups imbedded in the membrane stand-up and salute!2 Indeed, such a powerful electrical field can and does regulate the three- dimensional configuration of some of the gated membrane protein channels ("voltage gated channels") causing them to open and/or close depending on voltage changes that occur across the membrane. 2) Ionic Profiles. The typical mammalian extracellular solution contains about 120 mM (millimoles) of sodium, 4 mM of potassium and 124 mM of chloride ions. Inside the cell, the relative concentrations are almost reversed. We find about 12 mm of sodium, 110 mM of potassium and 9 mM of chloride ions. There are sufficient, large, impermeable anions (bicarbonate, glutamate, aspartate and organo-phosphates and -COOgroups of cellular proteins) to bring the sum total of negative charges inside about equal to the number of negative ions outside. Thus from a macroscopic view, the inside and outside contain an almost equal number of both positive and negative ions. The table below sums up the ion concentrations: Sodium Potassium Chloride "A” Inside Outside 12 mM 110 mM 9 mM ~(113 mM) 120 mM 4mM 124 mM -- Ratio of outside/inside 10 0.0363 13.78 -- From a macroscopic view, then, the inside and outside contain an almost equal number of both positive and negative ions. There must exist, however, a small imbalance of charge immediately across the membrane or there would be no resting potential. It should be emphasized though, that the required amount of excess negative charge inside, separated from the outside by less than 100 Angstroms, is almost immeasurably small. In fact, the ability of small amounts of charge to produce significant voltage changes across the nerve membrane is one of the great utilities of the system: small amounts of charge migrating the small distance across the membrane introduce very rapid, precise changes in voltage 3) Passive Physical Forces of Diffusion and Voltage: The Nernst Fquation. Given the ionic profiles, we are faced with explaining how they lead to the resting potential. As a first step, consider what the situation would be if the membrane were permeable only to one ion species (had only one kind of protein channel that was permeable to only one kind of ion). Taking potassium (K+) first, the relatively large 1 Ả = 10-8 cm., 100 Ả = 10-6 cm. To scale the membrane and voltage to recognizable dimensions, multiply both the membrane thickness and the voltage by 106. This gives I cm. for the membrane now, and 70 x 10-3 xIO6 =7o x 103 volts = 70,000 volts for the scaled electric field. 2 NMJ Lecture Notes 22 concentration of the K+ ions on the inside should cause K+ ions to diffuse outward toward the more dilute solution of K+ ions outside. Every ion of K+ that diffuses across the membrane will carry a positive charge with it, leaving behind an excess of negative charge. It is just this separation of charges which will produce an electric field, or potential. Moreover, increasing the number of charges which are separated, will tend to impede subsequent, positively charged K+ ions from diffusing outward. Indeed, it can be shown that an equilibrium will soon be reached such that the electrical field will exactly oppose the force of diffusion! In this state, as many potassium ions are attracted across the membrane from outside to inside by excess negative charges, as are shoved from inside to outside by the force of diffusion. The quantitative expression of this balance is the Nernst Equation for the single ion species. E RT Co ln zF Ci C RT 2.3 log o zF Ci where Co = outside concentration; Ci = inside concentration; z = the charge(valence) of the ion; and 2.3 RT/F = 61.5 mV, at 37C. Substituting in the concentration values for potassium, we get: K 4 E K 61.5 log o 61.5 log 61.5 log( 0.04) 61.5 x 1.44 90mV 110 Ki EK = -90 mV if the membrane were permeable only to potassium ions. In other words, a voltage difference of -90 mV would exactly oppose the diffusion force for the listed ionic concentrations of potassium across the nerve cell membrane. This is called the equilibrium potential for potassium. Looking at chloride, we obtain3 Cl Cl ECl 61.5 log o 61.5 log i 70mV Cli Clo This would be the value of the membrane potential if the membrane were permeable only to chloride ions. For sodium, the equilibrium potential is Na 120 E Na 61.5 log o 61.5 log 61.5 log(10) 61.5mV 12 Nai That is, the membrane potential would be 61.5 millivolts, inside positive, if the membrane were permeable only to sodium ions. 3 Note that multiplying a log ratio by –1 simply reverses the position of the numerator and denominator. This is an algebraic trick employed to keep minus signs out of textbook equations. Its end result here is that the equilibrium expression for chloride has the inside and outside concentrations reversed when compared with K+ and Na+. NMJ Lecture Notes 23 Looking at the values obtained we can draw a number of conclusions about the actual state of affairs. First, the actual resting potential of -70 mV agrees well with the chloride equilibrium potential. This implies that chloride is distributed passively across the membrane. If we artificially pass current into the cell to change the resting potential, chloride concentrations will also change (over a period of time) such that they will balance out the right hand side of the Nernst equation to equal the artificially imposed resting potential. Nothing is acting on chloride other than the forces of diffusion and voltage. Second, neither potassium nor sodium appear to be in equilibrium. We would predict that with a resting potential of -70 mV and the given concentrations of Na and K, a small amount of potassium should tend to diffuse out of the cell and a much larger amount of Na should diffuse into the cell if both ions were equally permeable to the membrane. In fact, potassium permeates the resting cell membrane about 50 times more readily than sodium, and about an equal amount of potassium tends to diffuse out as sodium goes in. Our third, conclusion is that given the figures on sodium and potassium, some force other than the passive forces of diffusion and electrical field is necessary to maintain the measured quantity of potassium so high (and that of sodium so low) inside the cell. This is where the role of the sodium-potassium 'pump' (sometimes just called the 'sodium pump") figures in. Active transport in terms of the ATP-dependent sodiumpotassium 'pump' is constantly at work to maintain the K+ and Na+ concentrations at their stated values. This is homeostasis in action. The Na-K active transport may be considered as a background process in that the pump cranks along, using cellular energy to maintain the K+ and Na+ gradients constant. If something happens to transiently change the leakage rates of these two ions, it is known that the pump will speed up a little bit or slow down a little bit to catch things back-up within a few seconds or minutes, thereby maintaining the desired gradients. Indeed, the ATP-ase activity of the sodium-potassium coupled transport is one of the principle homeostatic mechanisms of most cell membranes studied. Present studies are moving closer to physically characterizing the structure and exact function of this system. One other thing to note: by exchanging one Na+ for one K+ ion, the pump is "electrically neutral"; i.e., it does not change the charge concentration across the membrane, and therefore it does not contribute directly to either the resting potential or to changes in the resting potential. It works indirectly by maintaining the differential ion concentrations, which in turn exert their passive forces as expressed in the Nernst equation above and in the Goldman- Hodgkin-Katz equation explained below.4 4 There are actually a number of different, generic Na-K pumps and for most of them, the exchange ratios are not exactly 1:1. In these cases, the pumps are considered "electrogenic" in that they do contribute directly to the resting potential via unequal pumping ratios, but they still continue to contribute indirectly as well by maintaining ionic gradients. The electrogenic effects of all such pumps studied are actually minor ones, however, and they contribute only a few mV of potential. Much is made of them in many recent texts, unfortunately, as they are a more recent and "hot" research discovery topic, and authors of textbooks tend to overplay new things. Students should be as astute as we are, however, and realize that this aspect, while exciting to study in the research laboratory, should not detract from the basic concept and utility of the over-all homeostatic process, which is to maintain the constant ionic concentration gradients across the membrane. NMJ Lecture Notes 24 The Goldman-Hodgkin-Katz Equation. We are still left with the question, why 70 millivolts for the resting potential? A clue to the answer lies in realizing that the cell membrane is not permeable to just one ion species but is instead permeable to all three major ions, Na, K and Cl. We must quantitatively account for the relative permeabilities of these ions in order to understand why -70 mV, and to do that we have to go beyond the Nernst equation. If one were to stir a small quantity of oranges and a large quantity of grapefruit on a platform with many holes the size of oranges and only a very few large enough for grapefruit, the net result would be that more oranges than grapefruit would fall through. The same principle holds for relative permeability of ions. The relative permeability of the membrane to the various charged ions will determine which ion species is most important in carrying charges across the membrane, and therefore which of the ion species will have the greatest influence on 'setting' the resting membrane potential. The mathematics of the diffusion process gets complicated in so doing, but the three men named above were able, over about 10 years time of independent and of collaborative effort, to mold a relatively simple expression which considers both concentrations and permeabilities. This is the GHK Equation, expressed as E RT Pk K o PNa Nao PClCli ln F Pk K i PNa Nai PClClo where: PK = 1 x 10-6 (membrane permeability of potassium compared to free diffusion) PCl = 1 x 10-6 (membrane permeability of chloride compared to free diffusion) PNa = 2 x 10-8 (membrane permeability of sodium compared to free diffusion) Note that the Goldman-Hodgkin-Katz equation gives a potential for the steady-state condition where as many plus charges are flowing out across the membrane as are flowing in. The same is true for minus charges. Only chloride is in thermodynamic equilibrium, and the resting potential is a steady-state potential defined as no net flow of charge. It is assumed, of course, that the concentration profiles remain constant due to the active transport of Na and K by the sodium- potassium pump. In fact, membrane permeabilities of both K and Na are so low that a nerve axon can be metabolically poisoned to block active transport, and the concentration profiles will change measurably only after many minutes or hours (depending on the diameter and volume of the fiber). While not dwelling excessively on mathematics, it is instructive to play a few algebraic games with the G-H-K equation to illustrate the relative importance of the terms within the brackets. Divide all terms upstairs and down by PK. (This does not change the equation, as PK/PK = 1, but it allows for rearrangement of terms). NMJ Lecture Notes 25 PNa P Na o Cl Cl i K o RT PK PK E ln F P P K i Na Nai Cl Cl o PK PK Now, disregard the terms with chloride, since we know that chloride will passively distribute its concentration to agree with whatever K and Na determine. (You might try calculating E with and without deleting the chloride term to convince yourself of this). Finally, if you get tired of writing PNa/PK, let this quantity be b, substitute it in, and we obtain: E K o bNao RT K o bNao ln 61.5 log F K i bNai K i bNai Note that in the resting state, b is small because PNa is about 50 times smaller than PK which divides it in the term. If you substitute in the concentrations, you will see that the potassium concentration dominates (because Na terms are multiplied by about .02). We expect, and we do find, that changing extracellular K concentration will greatly affect the resting membrane potential while changing extracellular Na causes little change. The Strategy. One last feature remains to be considered, and herein lies the insight into the basic strategy employed by the neuron in affecting voltage changes as its information signaling mechanism. Since Na and K are, in fact, not in thermodynamic equilibrium, and because the cell will maintain the ionic profiles cited above, a small change in the membrane's permeability to either K or Na will cause the trans-membrane potential to change. The resting state is, then, a true source of potential energy. Increase sodium permeability for a fraction of a second, and the cell will depolarize (become less negative inside or less polarized) towards the sodium equilibrium potential. Increase PK and the membrane will hyperpolarize (become more negative or more polarized) towards the potassium equilibrium potential. Few ions need to flow (and these will generally be handled over the long haul by active transport). The concentrations remain effectively the same, but the membrane potential will fluctuate rapidly towards the equilibrium potential of whatever ion appears to dominate in the equation. Figure 1 at the end of this essay summarizes the situation. The change in permeability may be brought about by chemicals acting on chemically gated channels in the membrane (as it is in synaptic transmission), or it may be that forced changes in the electrical field across the membrane may trigger a voltage gated channel (as is the case for the action potential). The permeabilities of both Na and K may either increase (by opening gated channels) or decrease (by blocking resting channels), they may do so simultaneously or in sequence, as there are a large number of different, chemically gated and voltage gated channels. Other ions (chloride for instance, calcium in cases such as in cardiac muscle) may also figure into the permeability changes, but NMJ Lecture Notes 26 they do so in the same manner as sodium and potassium. In other words, the equation can be extended within the brackets to incorporate other ion species, and while it makes the equation more complicated to look at, the strategy by which membrane potential is changed remains the same. What isn't known is all the physical details of the different types of channels. We do know that the major ion species all have membrane proteins which are pretty much selective to each of them, and this makes common sense in considering how exquisite and important is the control over permeabilities. Moreover, there are some channels that are equally permeable to both Na and K (try putting b = 1 into the GHK equation and predicting what direction the membrane potential will go when this type of gated channel opens up). We also know that the permeability sensitivity of neuronal membranes to various chemicals or to changes in electrical potential varies from cell to cell (i.e., different cells have different kinds of gated channels) and indeed, varies across the different parts of each neuron. Thus different drugs may affect different neurons or may block permeability changes on only a specific part of the neuron because of the drug's effect on a specific channel. Modern research now accepts the overall concepts given here, and the exciting new research emphasis is exactly concentrating on understanding the proteins that make up the gated channels. Considerable progress has been made on a few of these: the sodium ion channel that is voltage gated and responsible for action potentials in nerve axons has been isolated, cloned and sequenced; the acetylcholine receptor of the neuromuscular junction, which contains a large channel that lets both Na and K through simultaneously, has been isolated, purified, and sequenced; in addition numerous antibodies that bind to specific parts of this protein have been made and used to help us understand its threedimensional structure. Other channels have been sufficiently isolated to allow for their placement into "artificial" membranes in such a way as to make study of them easier. Understanding these channels better should lead to a more complete understanding of membrane. As pathologies of some channels lead to specific disease syndromes, understanding their structure should eventually lead to better clinical control of the diseases. As an example, auto immune attack on the above mentioned acetylcholine receptor leads to the disease called myasthenia gravis, and you will hear more about this later in the course. As the molecular biology of this receptor gets better understood, means for curing this disease becomes increasingly probable. That may be as it 'is, and one can get very excited about the research. What is just as exciting, however, is that we now understand the basic functional concepts underlying the membrane potential and how it is controlled. As explained above, it really isn't all that complicated, but it is an elegant system in its purity, efficiency and in the number of combinations and permutations that can lead from it. Indeed, understanding the membrane potential and the natural strategy for controlling it through permeability changes really reduces much the rest of basic neurophysiology to practical examples, and that should make any student of this subject happy! NMJ Lecture Notes 27 Potential (mV) 70 60 50 40 30 20 10 0 -10 -20 -30 -40 -50 -60 -70 -80 -90 -100 61.5 mV ENa Depolarization > 0.02 Resting (PNa/PK) = 0.02 Hyperpolarization < 0.02 EK Figure 1. The membrane potential depends on its relative permeability to ions. Permeability, and thus the membrane voltage, changes as voltage-dependent or chemically-dependent gated channels open and close. At the resting potential, PNa/PK = 0.02. When the ratio becomes larger than 0.02 (i.e. increases or decreases), depolarization results. When the ratio becomes less than 0.02 ( decreases or increases), hyperpolarization results. The two equilibrium potentials, E = 61.5 mV and E = -90 mV, set the upper and lower limits of the possible potential changes. NMJ Lecture Notes 28 4 NMJ References If you want to read more about neuromuscular physiology, try these references. Vander A, Sherman J, Luciano D (2001). Human Physiology: The Mechanisms of Body Function, 8th ed. McGraw-Hill. An excellent overview of human physiology. Covers everything, but has nice sections on nerve and muscle. Used in the core undergrad intro to physiology courses (PHYSL 3051, 6051) at the University of Minnesota. Kandel E, Schwartz J, Jessell T (2000). Principles of Neural Science, 4th ed. McGrawHill. The bible of neurosciences. Excellent chapters on nerve and the NMJ. Every student of the neurosciences should own this book. Hodgkin A (1992). Chance and Design. Cambridge University Press. Short autobiography of one author of the Hodgkin-Huxley equations. A wonderful book about his work, starting as a student, which elucidated the ionic basis of neuronal and muscle excitability. Koch, C (1999). Biophysics of Computation. Oxford University Press. Reference for biophysics of neurons. Chapters 1-4, 6 and 8 of particular interest for this week. Hille, B (2001) Ion Channels of Excitable Membranes. 3rd Ed. Sinauer, Sunderland , Mass. Standard textbook and reference on ion channels. Oakley B, Schafer R (1978) Experimental Neurobiology: A Laboratory Manual, University of Michigan Press. One of the only step-by-step guides on methods of basic neuroscience experiments. Out of print. If you get lucky, you might find one in a used book stores. Loeb G, Gans C (1986). Electromyography for Experimentalists. University of Chicago Press. Excellent coverage of experimental equipment for neurosciences, including how to build your own. The book is a little old, but most of the information is still valid. Adrian RH (1956) The effect of internal and external potassium concentration on the membrane potential of frog muscle. J Physiol 133:631-658. NMJ Lecture Notes 29 The classic paper on this topic. Included in the readings section of these lecture notes. Magleby KI (1984) Neuromuscular transmission. In: The Anatomy, Physiology, and Biochemistry of Muscle. Chapter 13, pp. 393-418. Coverage of the NMJ, classic experiments on recording EPPS and MEPPs. Included in the readings section of these lecture notes. Matthews, G.G. (1998). Cellular Physiology of Nerve and Muscle. 3rd ed. Blackwell Science. Excellent overview of the principles at work in excitable cells. Textbook used for Univ of Minn physiology courses. Aidley, D. (1998). The Physiology of Excitable Cells. 4th ed. Cambridge Univ. Press Excellent overview of the principles at work in nerve and muscle cells. NMJ Lecture Notes 30 5 Readings This section contains primary source material that should be read prior to the course. Contents Adrian RH (1956) The effect of internal and external potassium concentration on the membrane potential of frog muscle. J Physiol 133:631-658. A classic paper on how potassium concentration changes change the resting potential of a membrane. You will be doing a similar experiment in this course. Magleby KL (1984) Neuromuscular transmission. In: The Anatomy, Physiology, and Biochemistry of Muscle. Chapter 13, pp. 393-418. Coverage of the NMJ, classic experiments on recording EPPS and MEPPs. Relevant to all microelectrode recording experiments you will do this week. Included in the readings section of these lecture notes. Engle AE (1994). Congenital myasthenic syndromes. In Neurologic Clinics of North America, 12(2):401-437. Overview of NMJ disorders. You only need to skim this one. Durfee, W.K. and P.A. Iaizzo. Rehabilitation and muscle testing. In: Encyclopedia of Medical Devices and Instrumentation, 2nd ed . J.G. Webster, ed., Vol 6, pp 62-71, Hoboken, John Wiley & Sons, 2006. Review of clinical human muscle force testing. (available on-line at www.me.umn.edu/~wkdurfee/publications/wiley-chap-2006.pdf NMJ Lecture Notes 31 **Note to handout assembler: Replace this page with the following articles: Adrian RH (1956) The effect of internal and external potassium concentration on the membrane potential of frog muscle. J Physiol 133:631-658. Magleby KL (1984) Neuromuscular transmission. In: The Anatomy, Physiology, and Biochemistry of Muscle. Chapter 13, pp. 393-418. Engle AE (1994). Congenital myasthenic syndromes. In Neurologic Clinics of North America, 12(2):401-437. Durfee, W.K. and P.A. Iaizzo. Rehabilitation and muscle testing. In: Encyclopedia of Medical Devices and Instrumentation, 2nd ed . J.G. Webster, ed., Vol 6, pp 62-71, Hoboken, John Wiley & Sons, 2006. (available on-line at www.me.umn.edu/~wkdurfee/publications/wiley-chap-2006.pdf) NMJ Lecture Notes 33