The Eye
The eye forms a visual image and
projects it onto the sensory receptors
(photoreceptors) of the retina.
ACCESSORY STRUCTURES
Anatomy and Physiology Text and Laboratory Workbook, Stephen G.
Davenport, Copyright 2006, All Rights Reserved, no part of this publication can
be used for any commercial purpose. Permission requests should be
addressed to Stephen G. Davenport, Link Publishing, P.O. Box 15562, San
Antonio, TX, 78212
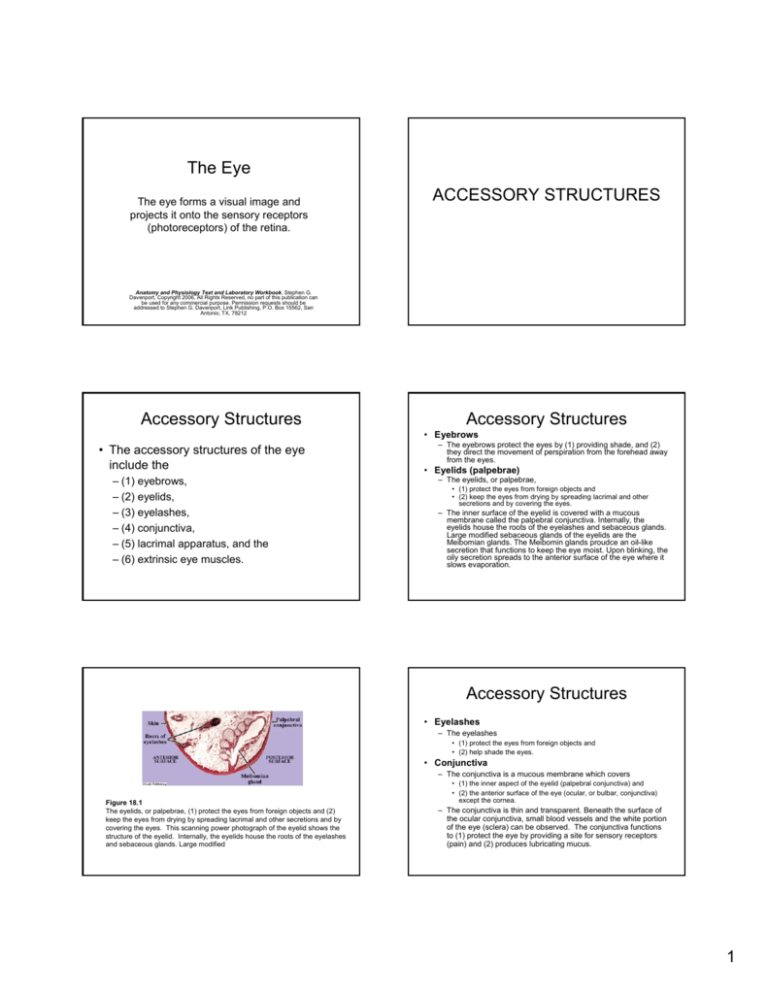
Accessory Structures
Accessory Structures
• Eyebrows
• The accessory structures of the eye
include the
– (1) eyebrows,
– (2) eyelids,
– (3) eyelashes,
– (4) conjunctiva,
– (5) lacrimal apparatus, and the
– (6) extrinsic eye muscles.
– The eyebrows protect the eyes by (1) providing shade, and (2)
they direct the movement of perspiration from the forehead away
from the eyes.
• Eyelids (palpebrae)
– The eyelids, or palpebrae,
• (1) protect the eyes from foreign objects and
• (2) keep the eyes from drying by spreading lacrimal and other
secretions and by covering the eyes.
– The inner surface of the eyelid is covered with a mucous
membrane called the palpebral conjunctiva. Internally, the
eyelids house the roots of the eyelashes and sebaceous glands.
Large modified sebaceous glands of the eyelids are the
Meibomian glands. The Meibomin glands proudce an oil-like
secretion that functions to keep the eye moist. Upon blinking, the
oily secretion spreads to the anterior surface of the eye where it
slows evaporation.
Accessory Structures
• Eyelashes
– The eyelashes
• (1) protect the eyes from foreign objects and
• (2) help shade the eyes.
• Conjunctiva
– The conjunctiva is a mucous membrane which covers
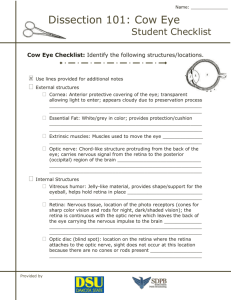
Figure 18.1
The eyelids, or palpebrae, (1) protect the eyes from foreign objects and (2)
keep the eyes from drying by spreading lacrimal and other secretions and by
covering the eyes. This scanning power photograph of the eyelid shows the
structure of the eyelid. Internally, the eyelids house the roots of the eyelashes
and sebaceous glands. Large modified
• (1) the inner aspect of the eyelid (palpebral conjunctiva) and
• (2) the anterior surface of the eye (ocular, or bulbar, conjunctiva)
except the cornea.
– The conjunctiva is thin and transparent. Beneath the surface of
the ocular conjunctiva, small blood vessels and the white portion
of the eye (sclera) can be observed. The conjunctiva functions
to (1) protect the eye by providing a site for sensory receptors
(pain) and (2) produces lubricating mucus.
1
Accessory Structures
• Lacrimal apparatus
– Each eye has a lacrimal apparatus. A lacrimal apparatus
consists of the
• (1) lacrimal gland and
• (2) the structures which drain the secretions (tears) from the
lacrimal apparatus.
Figure 18.2
The accessory structures of the eye include the eyebrows,
eyelids, eyelashes, conjunctiva, lacrimal apparatus, and the
extrinsic eye muscles.
– Each lacrimal gland is located superiorly and laterally to each
eyeball.
– Lacrimal secretions (tears) from a lacrimal gland flow onto the
upper conjunctiva through several small lacrimal ducts. Tears
pass medially over the anterior surface of the eyeball and enter
two small openings (lacrimal puncta), one located at each
medial margin of each eyelid.
– Each lacrimal punctum opens into a lacrimal canal, which
drains into the lacrimal sac. Each lacrimal sac drains into a
nasolacrimal duct, which enters the nasal cavity at the inferior
nasal meatus (chamber under the bone called the inferior nasal
concha).
Accessory Structures
• Extrinsic eye muscles
The six muscles which move the eyeball are called the
extrinsic eye muscles. Four of the six muscles are
named rectus muscles, and the two other muscles are
named oblique muscles.
– The rectus muscles are further named by their position as the
•
•
•
•
Figure 18.3
A lacrimal apparatus consists of the (1) lacrimal gland
and (2) the structures which drain the secretions
(tears) from the lacrimal apparatus.
Figure 18.4
The six muscles which move the eyeball are called the extrinsic eye
muscles. Four of the six muscles are named rectus muscles, and the two
other muscles are named oblique muscles.
(1) superior rectus,
(2) inferior rectus,
(3) medial rectus, and
(4) lateral rectus muscle, and
– the oblique muscles are named the
• (5) superior oblique and the
• (6) inferior oblique muscle.
Figure 18.5
The six extrinsic muscles of the eye function in movements of the eye as
shown in the photograph of the preserved sheep eye.
2
EYE MOVEMENTS
Figure 18.6
Lateral view of the eye showing the movements
directed by the extrinsic muscles.
Eye Movements
• The medial and lateral rectus muscles function in
eye movements in the horizontal plane.
– Because the medial and lateral rectus muscles are
inserted along the horizontal axis of the eye, their
contraction produces movement along the horizontal
axis.
– The medial rectus muscle functions in eye adduction
(movement of the eye toward nose) and the lateral
rectus muscle function in eye abduction (movement of
the eye away from nose).
Eye Movements
• The remaining four muscles, the superior and inferior
rectus muscles and the superior and inferior oblique
muscles, function in movement of the eye in the vertical
plane moving the eye upward (elevation) and downward
(depression).
– Because the superior and inferior rectus muscles are not
inserted along the vertical axis of the eye, their contractions do
not produce purely vertical movements (elevation and
depression).
– When the eye is abducted, the superior and inferior rectus
muscles exert the movements of elevation and depression,
respectively.
– When the eye is fully adducted the superior and inferior oblique
muscles exert the movements of depression and elevation,
respectively.
– When the eye is in its forward position, all four muscles make
contributions to elevation and depression.
Structure of the Eyeball
STRUCTURE OF THE
EYEBALL
• The eyeball, which is mostly spherical in shape, is
housed within and is protected by the bony orbit.
Only a small portion of its anterior aspect is
exposed to the external environment.
• Externally, the eye is surrounded by protective
adipose tissue. Six muscles, the extrinsic muscles
of the eye, control the movement of the eye.
• Internally, the eye is filled with fluids (humors)
and is divided by the lens into an
– (1) anterior cavity (segment) - contains aqueous humor
– (2) posterior cavity (segment) - contains the vitreous
humor (body).
3
Structure of the Eyeball
Wall of the Eye
• The wall of the eye consists of three layers
(tunics). From outer to inner, they are the
– (1) fibrous tunic, the
– (2) vascular tunic, and the
– (3) sensory tunic.
Structure of the Eyeball
Wall of the Eye
• Fibrous tunic
– The fibrous tunic is the layer of tough dense connective tissue
that surrounds the eye. The two components of the fibrous tunic
are the sclera and the cornea.
• Vascular tunic
– The vascular tunic contains numerous blood vessels (vascular),
pigments, and the intrinsic muscles of the eye. The components
of the vascular tunic are the choroid, ciliary body, and iris. The
intrinsic muscles of the eye describe the muscles found within
the eye and include the muscles of the ciliary body, the ciliary
muscle, and the muscles of the iris.
• Neural tunic
– The neural tunic is the inner layer of the eye and is the retina.
The retina consists of an inner neural layer and an outer
pigmented layer.
Figure 18.7
The general surface anatomy of the eye is shown. The extrinsic
muscles are the six ocular muscles that move the eye.
Figure 18.9
The general anatomy of the eye as demonstrated with a horizontal section of
a preserved sheep eye. Common abnormalities shown is a preserved eye are
the presence of a translucent (or opaque) cornea and lens, and a retina that
shows surface wrinkling.
Figure 18.8
A drawing of the eye as seen in a horizontal section.
Figure 18.10
A drawing of the eye as seen in horizontal and front sections.
4
Lab Activity 2
Structure of the Eye
• Observe a microscope slide preparation of
the eye and/or the following illustrations
and photographs. The label on the slide
will usually identify the section, such as
“general section,” or showing the “optic
nerve,” and/or “fovea centralis,” etc.
Figure 18.11
Horizontal meridional section of the monkey eye
showing both the fovea centralis and the optic disc.
Sclera
• The sclera is the tough, opaque “white” portion
of the eyeball formed by fibrous connective
tissue.
FIBROUS TUNIC
– It completely surrounds the eyeball except for two
locations:
• (1) anteriorly, where it merges with the cornea and
• (2) posteriorly, where it is pierced by the optic nerve.
The outer fibrous tunic consists of the
(1) sclera and the
(2) cornea.
– The sclera functions in
• (1) providing an attachment site for the extrinsic muscles,
• (2) gives the eye shape, and
• (3) provides protection.
Cornea
• The cornea primarily functions in
– (1) allowing light into the eye,
– (2) in focusing (refraction) of light, and
– (3) protection.
Figure 18.12
The fibrous sclera forms the outer portion of the wall of the eye
except anteriorly, where it merges with the (1) cornea and (2)
posteriorly, where it is pierced by the optic nerve.
• The cornea is formed from fibrous connective tissue and
is continuous with the sclera, the corneal-scleral junction
is called the limbus.
• The cornea is the transparent anterior “window” of the
eyeball and is the eye’s primary structure for focusing
incoming light.
• The external surface of the cornea is lined with stratified
squamous epithelium (not the conjunctiva). Numerous
free nerve endings, which primarily function as pain
receptors, are located in the corneal epithelium.
• Internally, the cornea is formed from layers of
transparent collagen fibers, collectively called the
stroma.
5
VASCULAR TUNIC
Figure 18.13
The cornea is the transparent anterior “window” of
the eye and is the eye’s primary structure for
focusing incoming light.
Identify the middle vascular tunic,
which consists of the
(1) choroid,
(2) ciliary body, and
(3) iris.
Choroid
• The choroid is the highly vascular
posterior portion of the vascular tunic. Its
numerous blood vessels
– (1) supply nutrients to the fibrous and sensory
(retina) tunics, and
– (2) its pigments absorb light.
• Anteriorly, the choroid joins the ciliary
body near the anterior margin of the retina,
the ora serrata.
Ciliary Body
• The ciliary body is a region of the vascular tunic anterior
to the choroid. It consists of the
– (1) ciliary muscle and the
– (2) ciliary processes.
• Ciliary muscle
– The ciliary muscle is a ring of smooth muscle that functions in
the regulation of the shape of the lens. The epithelial surface of
the ciliary muscle is modified into folds called ciliary processes.
• Ciliary processes
– The ciliary processes are folds formed from the epithelium that
covers the ciliary muscle. The ciliary processes
Figure 18.14
The choroid is the highly vascular posterior portion of the vascular tunic.
Suspensory Ligament
• The suspensory ligament extends from the
ciliary processes to the lens. It consists of
fibers that
– (1) provide for positioning of the lens and for
– (2) the transfer of tension produced by the
ciliary muscle in the regulation of the shape of
the lens.
• (1) secrete the fluid (aqueous humor) of the anterior cavity
(segment) and
• (2) provide attachment sites for the suspensory ligament, which
attaches to the lens.
6
Iris and Pupil
• Iris
Figure 18.15
The ciliary body consists of the ciliary muscle and
the ciliary processes.
– The iris is the most anterior portion of the vascular tunic. The iris
extends anteriorly from the ciliary body and divides the anterior
cavity (segment) into the anterior (in front of iris) and posterior
(behind the iris) chambers.
– The iris regulates the amount of light that enters the eye. Two
groups of smooth muscle fibers, the dilator fibers and the
sphincter (constrictor) fibers, control the diameter of the pupil,
the central opening in the iris. The dilator fibers, which dilate, or
increase the diameter of the pupil, are controlled by the
sympathetic division of the autonomic nervous system (ANS).
The sphincter (constrictor) fibers, which decrease the diameter of
the pupil, are controlled by the parasympathetic division of the
ANS.
• Pupil
– The pupil is the central opening in the iris.
SENSORY TUNIC (RETINA)
The sensory tunic, or retina, is the
inner tunic of the eye.
Figure 18.16
The iris extends anteriorly from the ciliary body and
divides the anterior cavity (segment) into the anterior (in
front of iris) and posterior (behind the iris) chambers.
Sensory Tunic
• The retina consists of the
– (1) inner neural (nervous) layer and an
– (2) outer pigmented layer.
• The neural layer of the retina consists of
three major groups of cells. From outer to
inner the cell layers are the
– (1) photoreceptors,
– (2) bipolar cells, and
– (3) the ganglion cells.
Figure 18.17
The neural layer of the retina consists of three major
groups of cells.
7
Neural Layer – Seven Layers
• A more detailed description of the retina divides
the neural portion of the retina into seven layers.
From outer to inner the layers are the
–
–
–
–
–
–
–
(1) rods and cones,
(2) outer nuclear layer,
(3) outer plexiform layer,
(4) inner nuclear layer,
(5) inner plexiform layer,
(6) ganglion cell layer, and
(7) the layer of optic nerve fibers.
Figure 18.18
A detailed description of the retina divides the neural
portion of the retina into seven layers.
Sensory Tunic
• Plexiform Layers
– The plexiform layers are regions that contain nerve
fibrils (axons and dendrites) and synapses.
• Retina – Outer Layer
Figure 18.19
Detailed description of the retina of the monkey eye.
– The outermost layer of the neural retina, the layer of
rods and cones.
– This layer contains the light receptive elements of the
photoreceptors that are either “rod” or “cone” shaped.
– The nuclei of the photoreceptors are located in the
outer nuclear layer of the retina.
– The photoreceptors terminate with synapses to the
bipolar cells in the outer plexiform layer.
Retina
• Retina – Outer Layer
– The rods do not respond to different wavelengths of
light (color), thus, are only responsible for producing
images without color (black and white). Rods also
perform best under low light conditions.
– Cones function in color reception and perform best
under higher light than allowed for rods. There are
three varieties of cones,
• (1) red sensitive cones,
• (2) green sensitive cones, and
• (3) blue sensitive cones.
– Even though each cone is most sensitive in its named
wavelength, overlapping sensitivity produces
responses for the full color spectrum.
Figure 18.20
The outermost layer of the neural retina consists of the rods
and cones. Named by their shape, rods do not result in color
discrimination. Color discrimination is produced by the
overlapping sensitivities of the three types of cones, the red
cones, the blue cones, and the green cones.
8
Bipolar and Ganglion Cells
• Bipolar Cells
– Bipolar cells are neurons that have two processes
associated with their cell body.
– Their receptive portions (dendrites) are found in the
outer plexiform layer associated with the
photoreceptors (and amacrine cells).
– The bipolar cells terminate with synapses to the
ganglion cells in the inner plexiform layer.
• Ganglion Cells
– The receptive portion of the ganglion cells is in the
inner plexiform layer where they synapse with bipolar
cells (and horizontal cells).
– The axons of the ganglion cells form the layer called
the ganglion nerve fibers (ganglion axons ) that
converge at the optic disc to form the optic nerve.
Macula Lutea
• The macula lutea is a region of the retina
which contains only cones.
– The fovea centralis is located at the center of
the macula lutea.
– Ophthalmologists and opticians routinely
examine the macula lutea for pathology
during eye examinations. An ophthalmoscopic
view of the macula lutea reveals it to be a
dark area lateral to the optic disc, the exit
point of the optic nerve.
Fovea Centralis
• The fovea centralis is a small pit located at
the center of the macula lutea.
– In humans the fovea centralis contains only
cones and is the area of most acute vision.
– The visual axis, the focal point of light through
the eye, falls directly upon the fovea centralis.
Figure 18.21
A photograph of the back of the eye as seen through an
opthalmoscope.
Figure 18.23
A scanning power view of the fovea centralis (and
wall) of the monkey eye.
Figure 18.22
The fovea centralis is a small pit located at the center of
the macula lutea. The fovea centralis is the area of most
acute vision. The visual axis, the focal point of light
through the eye, falls directly upon the fovea centralis.
9
Optic Disc (Blind spot)
• The optic disc consists of axons of the
ganglion cells (layer of nerve fibers) that
converge and exit the eye as the optic
nerve.
– The optic disc is called the blind spot because
it does not contain photoreceptors (retina is
absent at this location).
Figure 18.24
Low and high power views of the fovea centralis (nonhuman).
Optic Disc (Blind spot)
• Ophthalmologists and opticians routinely
examine the optic disc for pathology during eye
examinations.
Figure 18.25
The optic disc consists of axons of the ganglion cells (layer of
nerve fibers) that converge and exit the eye as the optic nerve
– The normal optic disc is observed as a white area
with a slight depression called the optic cup.
– Also seen at the optic disc are the central artery and
vein, two major blood vessels that vascularize a major
portion of the retina by routing through the optic
nerve.
– The outer retina (photoreceptors) receive most of
their vascular supply from the choroid, and the inner
retina (bipolar and ganglion cells) are vascularized by
the central artery and vein.
SEGMENTS AND
CHAMBERS
Figure 18.26
The optic disc as seen through an ophthalmoscope. The
normal optic disc is observed as a white area with a slight
depression called the optic cup. Also, seen at the optic disc
are the central artery and vein.
10
Segments and Chambers
• Anterior cavity (segment)
– The anterior cavity (segment) is the cavity anterior to
the lens. It contains aqueous humor and is divided by
the iris into the anterior and posterior chambers.
• Anterior chamber
– The anterior chamber is the division of the anterior
cavity that is anterior to the iris (and posterior to the
cornea). It contains aqueous humor.
• Posterior chamber
Segments and Chambers
• Posterior cavity (segment)
– The posterior cavity (segment) is the cavity
located posterior to the lens. The posterior
cavity contains the fluid called vitreous humor
(body). Because the vitreous humor is firm
and gelatinous, the term body is frequently
used to replace “humor” (fluid).
– The posterior chamber is the division of the anterior
cavity that is posterior to the iris (and anterior to the
lens). It contains aqueous humor.
AQUEOUS HUMOR –
Location, production, and
reabsorption
Figure 18.27
The anterior and posterior chambers are named in reference
to the iris. Both chambers contain aqueous humor.
Aqueous Humor
• The aqueous humor is the fluid in the anterior
cavity (segment).
• Aqueous humor is produced at the ciliary
processes by capillary filtration.
• From the ciliary process, the aqueous humor
flows into the posterior chamber, then passes
through the pupil into the anterior chamber.
• From the anterior chamber, aqueous humor
enters into the scleral venous sinus (canal of
Schlemm) at the inner junction of the sclera and
the cornea, then enters venous circulation.
Figure 18.28
The aqueous humor is the fluid in the anterior cavity
(segment). It is produced at the ciliary processes by capillary
filtration and reabsorbed at the scleral venous sinus.
11
Lens
• The lens is a biconvex structure formed of layers
of cells called lens fibers.
LENS
– The lens functions in the focusing of light onto the
retina.
– The lens is attached to the suspensory ligament,
which transfers tension from the ciliary muscle to the
capsule of the lens. Contraction and relaxation of the
ciliary muscle function in the regulation of the shape
(curvature) of the lens.
– Changing the curvature of the lens changes its
refraction (bending light), thus allowing focusing of
light onto area of the retina of acute vision, the fovea
centralis.
DISSECTION OF THE EYE (SHEEP)
Figure 18.29
The lens is a biconvex structure formed of layers of cells called lens
fibers. The lens functions in the focusing of light onto the retina.
EXTERNAL ANATOMY
12
Figure 18.30
A sketch of the eye showing its general external anatomy.
Figure 18.31
The preserved sheep eye. Usually, specimens are not
supplied with eyelids and eyelashes. A large quantity of
adipose tissue normally surrounds and protects the eye.
Eyelashes
(usually not present on dissection specimens)
• Eyelashes are the fringe of hairs that
extend across the edge of the eyelid.
– Eyelashes function to protect the eye from the
entrance of foreign substances such as sweat.
Acting like levers, eyelashes enhance touch
and promote the blink reflex.
Figure 18.32
The anterior surface of a sheep eye after the removal of most of the
adipose tissue to expose the extrinsic eye muscles. Some
preserved eyes have a translucent (permits passage of light but
image is blurred) cornea, which allows the identification of the iris.
Usually, the cornea is opaque (does not transmit light).
Eyelids
(usually not present on dissection specimens)
• The two eyelids (palpebrae) are folds of skin and
muscle that can cover the anterior surface of the
eye.
– The inner surface of the eyelids is covered with a
mucous membrane, the palpebral conjunctiva. The
eyelids house the eyelashes at their margins and
contain numerous sebaceous glands, the Meibomian
glands.
– The eyelids function to protect the eye from drying
and from damage from foreign substances.
Cornea
• The cornea of preserved eyes always appears cloudy.
Depending upon the specimen, the cornea may be
slightly translucent, thus, the iris may be observed
beneath the cornea’s surface. However, the cornea is
usually totally opaque on preserved eyes.
• In the normal eye, the cornea is the transparent anterior
“window” of the eye.
– The cornea is the eye’s primary structure for focusing incoming
light.
– The cornea is formed from fibrous connective tissue and is
continuous with the sclera, the corneal-scleral junction is called
the limbus.
– The external surface of the cornea is lined with stratified
squamous epithelium (not the conjunctiva).
– The cornea primarily functions in
• (1) allowing light into the eye,
• (2) in focusing (refraction) of light, and
• (3) protection.
13
Conjunctiva
• The conjunctiva is a mucous membrane which
covers
– (1) the inner aspect of the eyelid (palpebral
conjunctiva) and
– (2) the anterior surface of the eye (ocular, or bulbar,
conjunctiva) except the cornea.
– The conjunctiva is thin and transparent. Beneath the
surface of the ocular conjunctiva, small blood vessels
and the white portion of the eye (sclera) can be
observed.
– The conjunctiva functions to
• (1) protect the eye by providing a site for sensory receptors
(pain) and
• (2) produces lubricating mucus.
Sclera
• The sclera is the tough, opaque “white”
portion of the eyeball formed by fibrous
connective tissue. It completely surrounds
the eyeball except for two locations:
• (1) anteriorly, at the location of the cornea and
• (2) posteriorly, where it is pierced by the optic
nerve.
– The sclera functions in
• (1) providing an attachment site for the extrinsic
muscles,
• (2) gives the eye shape, and
• (3) provides protection.
Extrinsic eye muscles
• The six muscles which move the eye are
collectively called the extrinsic eye muscles.
– The extrinsic muscles are surrounded by adipose
tissue and are identified by their reddish color and
firm texture.
– Four of the six muscles are named rectus muscles,
and the two other muscles are named oblique
muscles.
– The rectus muscles are further named by their
position as the (1) superior rectus, (2) inferior rectus,
(3) medial rectus, and (4) lateral rectus muscle, and
– The oblique muscles are named the (5) superior
oblique and the (6) inferior oblique muscle.
Figure 18.33
The six muscles which move the eye are collectively called the extrinsic eye
muscles. The extrinsic muscles are surrounded by adipose tissue and are
identified by their reddish color and firm texture.
Optic Nerve
• The optic nerve originates at the
convergence of retinal (ganglion cells)
axons at the posterior wall of the eye.
– The optic nerve is slightly medial to the visual
axis and extends slightly superiorly to exit the
orbit of the eye at the optic foramen of the
sphenoid bone.
– Usually, on preserved specimens the optic
nerve is cut short and is seen as a white rodlike stub.
Figure 18.34
The optic nerve originates at the convergence of retinal (ganglion
cells) axons at the posterior wall of the eye. The optic nerve is
usually cut short and is seen as a white rod-like stub.
14
INTERNAL ANATOMY
Figure 18.35
Section the eye in a frontal plane to make approximately equal
halves, an anterior portion and a posterior portion.
Vitreous Humor
ANTERIOR PORTION OF
THE CUT EYE
Position the anterior portion
of the eye so that you are
observing its interior.
• The vitreous humor (body) is the clear
gelatinous substance that occupies the
posterior cavity (segment), the space
between the lens and the retina.
• Function of the vitreous humor include
– (1) giving the eye shape,
– (2) protecting the eye by absorbing shock,
and
– (3) supporting the retina against the wall of
the eye.
STEP 1
CAREFULLY REMOVE THE
VITREOUS HUMOR
Figure 18.36
A sketch of the anterior portion of the dissected sheep
eye as seen immediately after sectioning. The vitreous
humor (body) has been removed.
15
Lens
• In the normal eye, the lens is a crystal clear
elastic biconvex structure formed of layers of
cells called lens fibers.
– In the preserved eye the lens is hard and opaque.
– The lens functions in the focusing of light onto the
retina.
– It is attached to the suspensory ligament, which
transfers tension from the ciliary muscle for the
regulation of shape (curvature) of the lens.
– Changing the curvature of the lens changes its
refraction (bending light), thus allowing focusing of
light onto area of the retina of acute vision, the fovea
centralis. The suspensory ligament is too small to be
observed on the dissection.
Figure 18.37
The anterior portion of the dissected sheep eye as
seen immediately after sectioning. The vitreous humor
(body) has not been removed.
Ciliary Body
• The ciliary body, is a region of the vascular tunic anterior
to the choroid. It consists of the (1) ciliary muscle and
the (2) ciliary processes.
• Ciliary muscle
– The ciliary muscle is a ring of smooth muscle that functions in
the regulation of the shape of the lens. The epithelial surface of
the ciliary muscle is modified into folds called ciliary processes.
•
Ciliary processes
– The ciliary processes are folds formed from the epithelium that
covers the ciliary muscle. The ciliary processes
• (1) secrete the fluid (aqueous humor) of the anterior cavity
(segment) and
• (2) provide attachment sites for the suspensory ligament.
Retina
• Observe the inner layer, the retina.
– In the preserved eye the retina is thin,
translucent, and detached forming numerous
wrinkles.
– The retina functions as the neural layer of the
eye, converting the energy of light into
electrical energy.
CUT WALL OF THE EYE
The wall of the eye that surrounds the
posterior cavity (segment) consists of three
layers, from inner to outer, the (1) retina, (2)
choroid, and (3) the sclera.
Choroid
• Carefully pull the retina away from its overlying
layer, the choroid.
– The choroid is dark (purple-black) in color.
– The functions of the choroid include
• (1) supplying a portion of the retina’s blood supply, and
• (2) absorbing light.
– A specialized region of the choroid seen in the
posterior portion of the cut eye is the tapetum
lucidum, an iridescent blue region that reflects light
back to the retina.
• The tapetum lucidum is present in animals with eyes
modified for enhanced night vision.
16
Sclera
• Carefully pull the choroid away from its
overlying layer, the sclera.
– The sclera is the white outer layer of the eye’s
wall.
– The sclera is formed of fibrous connective
tissue.
– The functions of the sclera include
STEP 2
REMOVE THE LENS FROM
THE CILIARY BODY
• (1) protection and
• (2) giving the eye shape.
Figure 18.38
Remove the lens from the ciliary body to
expose the posterior surface of the iris and
the cornea.
Figure 18.39
A translucent lens from a freshly preserved sheep eye is
shown placed on text. The biconvex lens converges light rays
and produces an image that is magnified.
Iris
• The iris is the most anterior portion of the
vascular tunic.
– Removing the lens from the ciliary body exposes its
darkly pigmented posterior surface.
– The pupil is the central opening in the iris.
– The posterior surface of the cornea is observed
through the pupil.
– The function of the iris is to regulate the amount of
light entering the eye.
ANTERIOR CAVITY
(SEGMENT)
• Constriction and dilation of the muscles of the iris produces a
corresponding constriction and dilation of the pupil.
17
Anterior Cavity
• Removal of the lens exposes the anterior cavity, the
cavity anterior to the lens. It contains aqueous humor
and is divided by the iris into the anterior and posterior
chambers.
• Anterior chamber
– Observe the anterior chamber, the division of the anterior cavity
that is anterior to the iris and posterior to the cornea. The
anterior chamber contains aqueous humor.
• Posterior chamber
– Observe the posterior chamber, the division of the anterior cavity
that is posterior to the iris and anterior to the lens. The location of
the lens on the eye specimen is observed by the margin of the
ciliary body. The anterior chamber contains aqueous humor.
Figure 18.40
Sketch of the anterior portion of the eye
after removal of the lens.
STEP 3
REMOVE THE IRIS AND
CILIARY BODY
Figure 18.41
Removal of the lens from the ciliary body exposes the
posterior surface of the iris, the pupil, and the
posterior surface of the cornea.
Removal of Iris and Ciliary Body
• Observe the posterior surface of the
portion remove with the forceps and
identify the (1) ciliary body, (2) posterior
surface of the iris, (3) pupil, (4) retina, and
(5) choroid.
• Rotate the specimen to expose its anterior
surface and identify the anterior surface of
the (1) iris, (2) pupil, and (3) choroid.
Figure 18.42
Grab the ciliary body and the iris with forceps and pull the
structures out of the anterior portion of the eye.
18
Figure 18.43
The portion removed with forceps reveals the details of the ciliary body and
iris. Rotation of the specimen reveals the anterior surface of the iris
Figure 18.44
The cornea and sclera form the outer fibrous tunic of the eye.
POSTERIOR PORTION OF
THE CUT EYE
STEP 1
CAREFULLY REMOVE THE
VITREOUS HUMOR
Position the posterior half of the
eyeball so that you are observing its
interior.
Retina
• After removal of the vitreous humor, identify the
retina.
Figure 18.45
The vitreous humor (body) is a gelatinous
substance that occupies the posterior
cavity, the area posterior to the lens.
– The retina functions as the neural layer (tunic) of the
eye, converting light energy into electrical energy,
nerve impulses.
– On the eye specimen, the retina usually appears as a
thin wrinkled (detached) thin membrane. Notice that
the retina is firmly attached to a white round structure,
the optic disc.
– The optic disc is the point where retinal axons
converge and pierce the wall of the eye as the optic
nerve. The optic disc is also called the blind spot as it
is void of the retina.
19
Choroid
• Observe the choroid, the middle pigmented
vascular layer of the wall of the eye.
– The choroid functions to absorb light and through its
numerous blood vessels is a vascular supply for the
sclera and retina.
– The choroid is located directly outside of the retina.
Probe the retina away from the pigmented choroid. A
portion of the choroid, the tapetum lucidum, is an
iridescent blue.
– The tapetum lucidum is found in animals adapted for
night vision (not humans) as it reflects light back onto
the retina.
Figure 18.46
A sketch of the posterior portion of the cut eye, with the
vitreous humor (body) removed. The layers of the wall of
the eye are sectioned to show their positions.
PHYSIOLOGY OF VISION
Figure 18.47
The posterior portion of the cut eye, with the vitreous
humor (body) removed. The layers of the wall have
been separated to show their positions.
Light
• Light is a form of energy, electromagnetic
radiation, that is transmitted in waves.
LIGHT
Light is a form of energy,
electromagnetic radiation, that is
transmitted in waves.
– The energy of light is called a photon, thus,
light is considered to be a transmission of
photons in waves.
– The waves of visible light are of different
lengths (wavelengths), and if separated as
with a prism, produce a color spectrum.
20
Light
• The visual receptors (photoreceptors) of the eye, the
rods and cones, are sensitive to the portion of the
electromagnetic spectrum called visible light.
Figure 18.48
Photograph of the visible spectrum projected by a prism. A prism
separates light by its wavelength and forms the color spectrum.
– Usually, light enters the eye as reflected light. Reflection of light
is the return (or bouncing) of light from a surface. When light
strikes an object, the object may reflect all wavelengths, absorb
some, or absorb all of the wavelengths. The light waves that are
reflected from the object give the object its color.
– For example, a red object is seen as red because the object
absorbs all the wavelengths except red. The red wavelengths
are reflected and strike the color photoreceptors (red sensitive
cones) of the retina. White results when all waves are reflected
from an object and black results when all waves are absorbed by
an object.
Light and Cones
• The color receptors of the retina are the cones.
• Three color sensitive cones are found in the
retina,
– (1) red sensitive,
– (2) green sensitive, and
– (3) blue sensitive and
• The cones function in the interpretation of the
additive primary colors, red, blue and green
(RGB).
– The ability to determine color relies on the amount of
stimulation of the three different types of color cones.
Figure 18.49
Three types of cones, red sensitive, blue sensitive, and green sensitive are
responsible for the perception of color. Each cone is most sensitive in its named
region of the color spectrum. The amount of stimulation of each of the three
types of cones gives the ability to detect light in the full visible spectrum.
Lab Activity 4
Color Blindness Test
• Color blindness is the inability to distinguish certain or all
colors of light.
– Color blindness results because of one, two, or all color sensitive
cones being nonfunctional. The most common type of color
blindness is red/green color blindness and is more common in
males than females (the genes for the red/green pigments are
located of the X chromosome).
• Obtain an Ishihara Test Chart Book and perform the
color blindness exam.
– Depending upon the test books available, the test is usually for
total color blindness and/or red/green color blindness. The test is
best performed in a daylight illuminated room. Typically, the test
discriminates color blindness by using different dyes on each
plate. Thus, when plates are made by using more than one dye,
color blind subjects identify different numbers on the same plate.
Figure 18.50
Color blindness test charts are typically made by using more than one dye in
the production of the numbers on each test chart, thus, depending upon the
type of color blindness, subjects will identify different numbers. Shown in
this figure are three test plates, each with a number 70 in a primary color
corresponding to the three most sensitive cones, blue, red, and green.
21
Light Refraction
•
LIGHT REFRACTION
Light travels in a straight line and when reflected
from an object travels away from the object in many
directions.
– A primary function of the eye is to bend (refract) light so that the
light (image) falls in sharp focus on the retina’s area of most
acute vision, the fovea centralis.
– Light is bent, or refracted, when it is deflected from a straight
path as it passes obliquely from one transparent medium into
another transparent medium and its speed (velocity) changes.
For example, when light passes obliquely from air into glass, its
velocity changes and the light is directed into another straight
line.
– Typical structures used to refract light are lenses. The curved
surfaces of lenses are the points of refraction. The more the
surface is curved the more the light is refracted. Plates of glass
with flat surfaces, such as windows, do not refract light. Two
common refractive lenses are convex and concave lenses.
Convex Lens
• Convex lenses are lenses that are thicker in the
middle than at their periphery.
Figure 18.51
Refraction occurs when light passes obliquely from one transparent medium
into another transparent medium. Two areas of refraction are shown in the
photograph of a straw in a glass of water. One area of refraction is at the
surface of the water (as light passes from air to water) and the other as at the
side (curved surface) of the glass (as light passes from air-glass-water).
– Convex lenses are commonly called converging
lenses as they function to refract light inward. They
converge light from a distant source and focus it to a
point, commonly called a focal point (length).
– Increasing lens convexity, increases the refraction of
the lens.
– The greater the refraction of the lens, the shorter the
focal length. The shorter the focal length the stronger
the lens.
Concave Lens
• A concave lens has the opposite effect of
a convex lens. Concave lenses are thicker
at their periphery than in the middle.
– Concave lenses are commonly called
diverging lenses as they function to refract
light outward, and do not form a focal point.
Figure 18.52
A convex lens is commonly called a converging
lens. A convex lens converges light to a point,
commonly called a focal point (length).
22
LIGHT REFRACTION ONTO
THE RETINA
Figure 18.53
A concave lens is commonly called a diverging lens. A
concave lens refracts light outward.
Refraction onto Retina
• The two major refractory structures of the eye
are the cornea and the lens.
• Cornea
– The cornea is the primary refractory structure of the
eye, with most refraction occurring as light enters at
its anterior surface. The cornea converges light rays
inward where they are further refracted as they pass
through the anterior and then posterior surfaces of the
lens.
• Lens
– The lens functions to dynamically focus light (by
changes in its shape) onto the fovea centralis of the
retina. The shape of the cornea, thus, its refraction
does not change.
Accommodation
Distant Objects
• Light from distant objects enters the eye
as nearly parallel waves and do not
require the eye to undergo
accommodation.
– When the ciliary muscles are relaxed, the eye
is accommodated (focused) for the far point of
vision. The normal human eye has a far point
of vision of 20 feet.
– Thus, viewing an object at 20 feet or more
does not require the eye to accommodate.
Accommodation
• Accommodation is the ability of the eye to adjust
its focal length and is achieved by the ciliary
body and the lens.
– Changes in focal length are necessary to adjust
incoming light waves to fall upon the fovea centralis.
– The shape of the lens, thus its focal length, is
changed by the contraction and relaxation of the
ciliary muscle. The outer elastic covering of the lens,
the lens capsule, is attached to the ciliary muscle by
the suspensory ligament.
– Changes in tension produced by the contraction and
relaxation of the ciliary muscles changes the shape
(convexity) of the lens.
Accommodation
Near Objects
• Light from near objects (closer than 20 feet)
requires eye accommodation because the light
waves are not as parallel.
– The closer the image the less parallel the light waves
and the more the eye must accommodate.
– With decreasing distance from the eye, the ciliary
muscle contracts more and more, pulling inward
toward the lens, thus, reducing tension upon the
suspensory ligament.
– With reduced tension, the elastic capsule of the lens
recoils and the lens becomes more convex (thicker
in the center) producing a shorter focal length.
– The shortest distance at which the eye can focus is
the near point of vision.
23
VISUAL ACUITY
Figure 18.54
At the left of the illustration, the ciliary muscle of the dissected sheep eye is
shown to illustrate the resulting increasing lens convexity resulting from the
contraction of the ciliary muscle. At the right, a sectional sketch illustrates the
necessity of changing lens convexity to focus light onto the fovea centralis of
the retina.
Visual Acuity
Visual acuity is a person’s sharpness of visual detail.
– The eye that produces normal visual acuity (sharp focus at 20
feet) is described as emmetropic.
– Abnormal visual acuity results from abnormal structural features
of the eye that cause the visual axis (image) not be focused on
the fovea centralis of the retina at 20 feet.
– Twenty feet is used to describe and to test for visual acuity
because it is the distance where the lens is not accommodated
(shape changed by the activity of the ciliary muscle).
– Common abnormal structural features include the abnormally
shaped eyeball, such as having either a too short or too long
eyeball, or an eyeball that has either an abnormally curved
lens and/or cornea.
– Two common visual abnormalities that involve the abnormally
shaped eyeball are hyperopia and myopia. A common visual
abnormality that involves the abnormally shaped cornea and/or
lens is astigmatism.
Hyperopia
• Hyperopia, or farsightedness, results when
the eyeball is too short and the point of
focus is behind of the fovea centralis.
– Individuals with hyperopia can focus on
distant objects but the eye cannot focus on
near objects.
– If eyeglasses are prescribed as the solution
for hyperopia, a converging lens, such as a
convex lens, is the type of lens used.
Myopia
Myopia, or nearsightedness, results withe
the eyeball is too long and the point of
focus is in front of the fovea centralis.
ASTIGMATISM
– Individuals with myopia can focus on near
objects but the eye cannot focus on far
objects.
– If eyeglasses are prescribed as the solution
for myopia, a diverging lens, such as a
concave lens is the type of lens used.
24
Astigmatism
• Astigmatism is a visual condition that results
when light rays are not focused evenly onto the
retina because of an irregular curvature of the
cornea and/or lens.
– If the cornea is described as perfectly dome shaped,
like half of a basketball, then a corneal astigmatism
might be described as the cornea in an oblong shape
like half a football (football is sectioned along its
length).
– A nonsymmetrical shape can produce more than one
focal point, resulting in an image that is blurred and
distorted.
– If eyeglasses are prescribed as the solution for
astigmatism, a lens is prescribed with a corrective
area to match the area of the cornea and/or lens that
is astigmatic.
Figure 18.55
A perfectly symmetrical cornea produces only one focal
point. A cornea that is elongated in one axis and
compressed in the other axis produces two focal points.
VISUAL TESTS
Figure 18.56
Common abnormal structural features
include the abnormally shaped eyeball,
such as having either a too short or too
long eyeball, or an eyeball that has
either an abnormally curved lens and/or
cornea. Two common visual
abnormalities that involve the abnormally
shaped eyeball are hyperopia and
myopia. A common visual abnormality
that involves the abnormally shaped
cornea and/or lens is astigmatism.
Visual Acuity
• Visual acuity is measured by the person’s ability to read
print of a certain size at a distance of 20 feet.
– The test distance of twenty feet is used as a standard because it
is at this distance the lens of a normal eye (emmetropic) does
not change shape for focusing (point of far vision).
– The visual acuity test compares what the test subject can read at
the standard test distance of 20 feet to what a person with
normal vision reads at the distance specified on the test chart. A
visual acuity measurement is written to the side of each line on
the test chart. The top number of the visual acuity reading is the
test distance, and will always be 20 feet. The bottom number is
the distance at which a person with normal vision, emmetropic,
reads the line.
Visual Acuity
– For example, if you can read to the line that specifies 20/100,
this means that you read at 20 feet (standard test distance) what
a person with normal vision reads at 100 feet.
– Interpreting this reading indicates that you are nearsighted
(myopic). If your visual acuity is normal (emmetropic), you can
read the test print at the test distance of 20 feet that a person
with normal vision can read at 20 feet.
– Thus, your vision is 20/20. If you can read the letters specified
for 20/10 feet, then you read at 20 feet what a person with
normal vision can read at 10 feet. This reading would indicate
that you are slightly farsighted (hyperopic).
25
Lab Activity 5
Test for Visual Acuity
• Procedure
In a well-illuminated room stand 20 feet from the visual
acuity screening test page (if a test page is not available,
the above illustration can be used). \
Figure 18.57
The visual acuity screening test uses a standard test distance of 20 feet
and print of different sizes to determine visual acuity. The top number of
the visual acuity reading is the test distance, and will always be 20 feet.
The bottom number is the distance at which a person with normal vision,
emmetropic, reads the line.
– Start with the top of the test page, which normally indicates
20/200 and read the lines downward. Have someone verify your
results.
– Test one eye at a time by holding a cover in front of the other
eye.
– If you wear eyeglasses, first test your eyes with your glasses and
then without.
– If you wear contacts, test your eyes with them.
• Results
– Record in the worksheet the visual acuity reading for the last line
that you could accurately read.
Lab Activity 6
Test for Astigmatism
• Astigmatism can be tested by observing a
test card which consists of converging
radial lines.
– If no astigmatism exists, all of the radial lines
will be of equal sharpness.
– However, if astigmatism exists, lines will be
distorted in areas that correspond to the
unequal curvature of the cornea and/or lens
Lab Activity 6
Test for Astigmatism
• Procedure
– In a well-illuminated room, stand about three feet away from an
astigmatism screening illustration (if one is not available use the
above illustration).
– Test one eye at a time by holding a cover in front of the other
eye.
– Look directly at the center of the illustration.
– If you wear eyeglasses, first test your eyes with your glasses and
then without.
– If you wear contacts, test your eyes with them.
• Results
– An astigmatism is indicated if any of the radial lines appear
distorted and blurred. Record your results in the worksheet.
Lab Activity 6
Test for Astigmatism
• Test for the Optic Disc (blind spot)
•
The optic disc (blind spot) is formed by
the convergence of the fibers (axons) of
the ganglion cells of the retina. The axons
pierce the posterior wall of the eye and
exit to form the optic nerve. The optic disc
(blind spot) contains no photoreceptors
and is demonstrated by the failure of the
retina to produce an image at its location.
Figure 18.58
An astigmatism test chart of radial lines. An astigmatism produces distortion
and blurring of the radial lines. The numbers are used to identify the plane of
the astigmatism.
26
Lab Activity 7
Test for the Optic Disc (blind spot)
• The optic disc (blind spot) is formed by the
convergence of the fibers (axons) of the
ganglion cells of the retina.
– The axons pierce the posterior wall of the eye
and exit to form the optic nerve.
– The optic disc (blind spot) contains no
photoreceptors and is demonstrated by the
failure of the retina to produce an image at its
location.
Figure 18.59
The optic disc (blind spot) is formed by the convergence of the
fibers (axons) of the ganglion cells of the retina.
Lab Activity 7
Test for the Optic Disc (blind spot)
• Procedure
– The blind spot (optic disc) is easy to demonstrate by observing
two near objects points printed on paper, the eye is focused on
one object and the other object is placed in the lateral visual
field.
– The object in the lateral visual field is the point used to
demonstrate the blind spot because it is focused by the lens to
the medial retinal surface (see the above illustration) where the
blind spot (optic disc) is located.
– As the image is moved away (or toward) the eye, the image in
the lateral visual field is moved across the medial retinal surface.
– When the image moves across the blind spot (optic disc) the
image disappears because the blind spot (optic disc) lacks the
retina.
Figure 18.60
A dot and square can be used to
demonstrate the blind spot (optic disc).
Test for the Optic Disc (blind spot)
Test for the Right Eye:
Test for the Optic Disc (blind spot)
Test for the Left Eye:
• 1. Close your left eye
• 2. Hold this page a couple of inches from your right eye
and observe the above illustration of the dot and square.
• 3. Position the “dot” directly in front of the right eye.
Looking directly at the “dot,” the “square” will be
observed in your peripheral vision.
• 4. While keeping the “dot” sharply in focus, move the
page slowly away from your right eye.
• 5. When the page is about 5 -7 inches from the eye,
the “square,” seen in peripheral vision, should
completely disappear from your visual field.
• 1. Close your right eye
• 2. Hold this page a couple of inches from your left eye
and observe the above illustration of the dot and square.
• 3. Position the “square” directly in front of the left eye.
Looking directly at the “square,” the “dot” will be
observed in your peripheral vision.
• 4. While keeping the “dot” sharply in focus, move the
page slowly away from your right eye.
• 5. When the page is about 5 -7 inches from the eye,
the “dot,” seen in peripheral vision, should completely
disappear from your visual field.
27
Lab Activity 7
Test for the Near Point of Vision
• The normal lens of the eye is extremely flexible.
It can be stretched, becoming flatter and less
curved, or it can recoil and become thicker and
more curved.
– When the ciliary muscle contracts, tension on the lens
is reduced.
– The lens recoils and becomes thicker and more
curved.
– Increasing convexity of the lens allows focusing on
near objects. When maximum convexity the lens is
reached the lens is adjusted for the near point of
focus.
Lab Activity 7
Test for the Near Point of Vision
• With aging, the lens gradually loses its
elasticity and loses its ability to recoil.
– The loss of elasticity results in the lens
remaining flatter and the near point advancing
away from the eye.
– The loss of lens elasticity with advancing near
point of focus results in presbyopia,
farsightedness due to advancing age.
• The near point of focus is the shortest distance
at which the eye can sharply form a focused
image.
Lab Activity 7
Test for the Near Point of Vision
• The following illustration is an overview
showing an increased distance for the
near point of focus with increasing age,
predicted near point.
• The ten year span between the ages of 30
and 40 shows the most dramatic increases
in the changes in the near point of focus.
Figure 18.61
An overview of the changes in the near
point of focus with advancing age.
Lab Activity 7
Test for the Near Point of Vision
Left eye
• Procedure
– 1. Close your right eye.
– 2. Hold this page at arm’s length and focus on
this letter, “ R .”
– 3. While focusing on the letter “R” bring the
page toward your eye until the letter “R” just
becomes blurred.
– 4. Measure this distance in inches and record
the measurement in the worksheet.
Lab Activity 7
Test for the Near Point of Vision
Right eye
• Procedure
– 1. Close your left eye.
– 2. Hold this page at arm’s length and again
focus on the letter “R.”
– 3. Bring the page toward your eye until the
letter “R” just becomes blurred.
– 4. Measure this distance in inches and record
the measurement in the worksheet.
28
Retina
RETINA and Photoreceptors
• The retina consists of two regions, (1) an inner
neural layer and (2) an outer pigmented layer.
• Inner Neural Layer
– The inner neural layer consists of three cellular layers
from inner to outer the (1) ganglion cells, (2) the
bipolar cells and (3) the photoreceptors.
• Outer Pigmented Layer
– The outer pigmented layer consists of cells that
function in absorption of light and phagocytosis of
cellular fragments from the rods and cones.
Photoreceptors
• The photoreceptors are the rods and the
cones of the retina.
Figure 18.62
The retina is divided into the neural and pigmented
layers.
– From the pigmented layer inward, the
photoreceptors of the retina are organized
into an
•
•
•
•
(1) outer segment,
(2) an inner segment,
(3) the nuclear layer, and
(4) fibers of the outer plexiform layer.
Photoreceptors
• Outer segment
– The outer segments of the photoreceptors are closely associated
with the pigmented layer of the retina and contain the visual
pigments.
• Inner segment
– The outer segments are continuous with the inner segments.
The inner segments are the cytoplasmic rich areas of the
photoreceptors that contains most of the organelles.
• Nuclear region
– The inner segments are continuous with the nuclear region. The
nuclear region (layer) mostly contains the nuclei of the
photoreceptors.
• Fibers of the plexiform layer
– The nuclear region is continuous with the outer plexiform layer.
The outer region of the outer plexiform layer contains fibers
(axons) of the photoreceptors. The photoreceptors fibers (of the
outer plexiform layer) synapse with bipolar cells and amacrine
cells.
Figure 18.63
Photoreceptors of the retina are the rods and cones. The photoreceptors are
organized into an (1) outer segment, (2) an inner segment, (3) the nuclear
layer, and (4) fibers of the outer plexiform layer.
29
Visual Pigments
VISUAL PIGMENTS
• Rhodopsin is the light absorbing purple pigment of rods
and cones. Rhodopsin consists of two components,
retinal and opsin.
• Retinal
– Retinal (derivative of vitamin A) is the specific component of
rhodopsin that functions in light absorption. Opsin is the protein
portion of rhodopsin and functions as an enzyme. There are
three different derivatives of the opsin that is found in rods. Each
of these different opsins is associated with its corresponding
color sensitive (RGB) type of cone.
– Retinal forms two different structural arrangements (isomers).
When bound to opsin, retinal has a bent shape called 11-cis
retinal. When detached from opsin, retinal is in a straight form
called all-trans retinal.
Visual Pigments
Figure 18.64
The visual pigment retinal exists either as the l1-trans isomer or the alltrans isomer. Light energy converts ll-trans retinal to all-trans retinal.
• When ll-trans retinal is struck by light (photon energy), it
changes to a linear form called all-trans retinal, and it
detaches from opsin.
• This light dependent stage of photoreception begins the
series of events that lead to the generation of nerve
impulses of the optic nerve as opsin is free to function as
an enzyme.
• The conversion of 11-trans retinal to all-trans retinal is
called bleaching of the pigment (pigment becomes
clear).
• The regeneration of 11-cis retinal occurs in the dark
(does not require light) and is an enzymatically driven
reaction requiring ATP.
• Once all-trans retinal is converted to 11-cis retinal (or 11cis retinal is derived from vitamin A), 11-cis retinal joins
opsin to regenerate rhodopsin.
TRANSDUCTION OF LIGHT
Figure 18.65
Light energy causes 11-cis retinal to change to all-trans retinal (bleaching of the
pigment) and detach from opsin. Regeneration of the pigment occurs when alltrans retinal is converted back to 11-cis retinal in an ATP enzymatically driven
reaction. Rhodopsin is formed with the recombining of 11-cis retinal and opsin.
30
Transduction of Light
Transduction of Light
• The reactions of light striking rhodopsin begin
the process (transduction) of converting the
energy of light into nervous signals, nerve
impulses.
• When light strikes the 11-cis retinal portion of
rhodopsin, 11-cis retinal is converted to all-trans
retinal and the pigment is detached from opsin.
• Opsin now works as an enzyme that sets into
action a series of reactions that result in
hyperpolarization (inhibition) of the
photoreceptors.
• In dark, the photoreceptors are constantly releasing
neurotransmitter onto the bipolar cells at inhibitory
synapses.
• Thus, the bipolar cells are constantly in a state of
inhibition. When the photoreceptors are hyperpolarized,
the release of neurotransmitter onto the bipolar cells is
reduced.
• Reducing the release of neurotransmitter decreases the
inhibition, thus, causing an excitation of the bipolar cells.
• The bipolar cells stimulate the ganglion cells, which then
generate action potentials (nerve impulses) that are
transmitted through the optic nerve.
Optic Nerve
Pathway to the Brain
• Optic nerves
Optic Nerve
Pathway to the Brain
– Each optic nerve originates at the posterior wall of the
eye (optic disc) with the convergence of the ganglion
nerve fibers. The optic nerves are projected to the
inferior surface of the brain where the meet at the
optic chiasma.
• Optic chiasma
– The optic chiasma is the point where the two optic
nerves meet and the fibers (axons) from the medial
surface of each retina cross over to the opposite side.
The fibers form the optic tracts.
Optic Nerve
Pathway to the Brain
• Optic tracts
– The optic tracts originate at the optic chiasma. Each
optic tract contains fibers that originate from the
lateral aspect of its respective eye, and contains
fibers that originate from the medial aspect of the
opposite eye. The optic tracts continue to the
thalamus, the midbrain, and the hypothalamus.
• Thalamus
– The thalamus is the brain’s major relay center of
sensory input. Most of the fibers from the optic tracts
synapse with neurons in the thalamus (optic radiation
fibers) that deliver retinal informal to the visual cortex
of the brain’s occipital lobes.
Optic Nerve
Pathway to the Brain
• Midbrain
– Some fibers from the optic tract enter the midbrain for
visual reflexes, especially the pupillary reflexes and
reflexes of the extrinsic eye muscles.
• Hypothalamus
– Some fibers from the optic tract that enter the
hypothalamus and function to establish biorhythms,
especially responses to day and night intervals.
31
VISUAL FIELDS
Figure 18.66
The optic nerves meet at the optic chiasma where the fibers
from the medial surface of each retina cross over to the
opposite side. The fibers form the optic tracts, which send
fibers to the thalamus, midbrain, and hypothalamus.
Visual Fields
• The medial aspect of the retina receives light
from the lateral visual field, and the lateral
aspect of the retina receives information from
the medial visual fields.
– Thus, the right optic tract carries information from the
left visual field (lateral retinal surface of right eye and
medial retinal surface of left eye), and the
– Left optic tract carries information from the right visual
field (medial retinal surface of right eye and lateral
retinal surface of left eye).
Figure 18.67
Visual fields and neural pathways of the eyes.
32