Page 1 Exam I Exam II Today: A. Kidney anatomy B. Kidney
advertisement
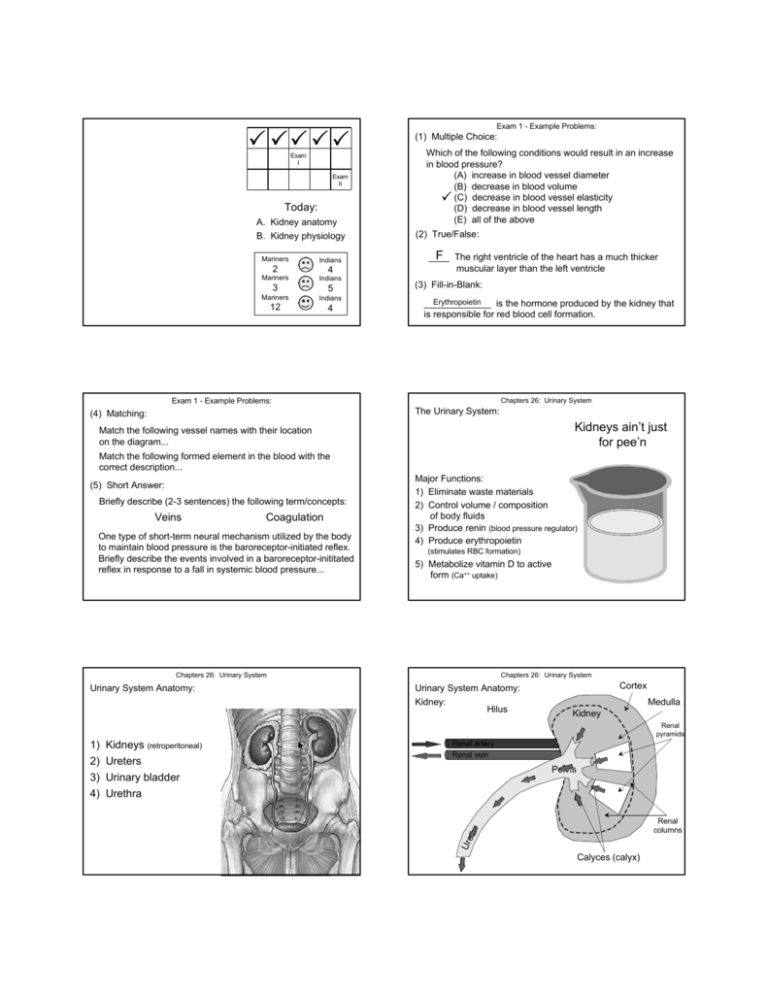
P PP P P Exam I Exam II Today: A. Kidney anatomy B. Kidney physiology Mariners Indians 2 4 Mariners Indians 3 5 Mariners Indians 12 4 Exam 1 - Example Problems: (1) Multiple Choice: Which of the following conditions would result in an increase in blood pressure? (A) increase in blood vessel diameter (B) decrease in blood volume P (C) decrease in blood vessel elasticity (D) decrease in blood vessel length (E) all of the above (2) True/False: F The right ventricle of the heart has a much thicker ____ muscular layer than the left ventricle (3) Fill-in-Blank: Erythropoietin _____________ is the hormone produced by the kidney that is responsible for red blood cell formation. Exam 1 - Example Problems: Chapters 26: Urinary System The Urinary System: (4) Matching: Kidneys ain’t just for pee’n Match the following vessel names with their location on the diagram... Match the following formed element in the blood with the correct description... (5) Short Answer: Briefly describe (2-3 sentences) the following term/concepts: Veins Coagulation One type of short-term neural mechanism utilized by the body to maintain blood pressure is the baroreceptor-initiated reflex. Briefly describe the events involved in a baroreceptor-inititated reflex in response to a fall in systemic blood pressure... Major Functions: 1) Eliminate waste materials 2) Control volume / composition of body fluids 3) Produce renin (blood pressure regulator) 4) Produce erythropoietin (stimulates RBC formation) 5) Metabolize vitamin D to active form (Ca++ uptake) Chapters 26: Urinary System Urinary System Anatomy: Chapters 26: Urinary System Urinary System Anatomy: Kidney: Hilus Cortex Medulla Kidney Renal pyramids Kidneys (retroperitoneal) Ureters Urinary bladder Urethra Pelvis Renal columns Ure ter 1) 2) 3) 4) Renal artery Renal vein Calyces (calyx) Chapters 26: Urinary System Urinary System Anatomy: Blood Supply to Kidneys: • 1/4 of cardiac output delivered to kidneys • 0.25 x 5 L/min = 1.25 L/min • Kidneys only 0.5 % of total body mass Nephron: Functional unit of the kidney (urine formation) • ~ 1 million / kidney • Filter ~ 200 L of blood plasma / day Chapters 26: Urinary System Urinary System Anatomy: Nephron Anatomy: 1) Glomerulus • Network of capillaries (filtration site) • Tightly wound coil (> surface area) 2) Tubule • Location where filtrate → urine • Produce ~ 1 - 1.5 L of urine / day • 99% of filtrate returned to blood Chapters 26: Urinary System Urinary System Anatomy: Nephron Tubule Anatomy: 1) Bowman’s Capsule • Expanded proximal end of tubule • Surrounds glomerulus • Outer layer = Simple squamous epithelium • Inner layer = Podocytes (foot cells) • Filtration slits = Area between podocytes Filtrate enters tubule through slits / fenestrations Chapters 26: Urinary System Urinary System Anatomy: Nephron Tubule Anatomy: 4) Distal Tubule • Simple cuboidal epithelium (w/o microvilli) • Acid/base balance (pH) • Secretion of materials into tubule (K+, H+, drugs) • Target region of ADH and aldosterone 5) Collecting Duct • Simple cuboidal epithelium • Collects almost completely formed urine • ~ 3x [solute] of blood Chapters 26: Urinary System Urinary System Anatomy: Nephron Tubule Anatomy: 2) Proximal Tubule • Adjacent to Bowman’s capsule • Simple cuboidal epithelium (microvilli) • ~ 80 % of reabsorption occurs here 3) Loop of Henle • Ascending and descending portions • Simple squamous epithelium • Water conservation Chapters 26: Urinary System (Figure 26.4) Chapters 26: Urinary System Chapters 26: Urinary System Urinary System Anatomy: Types of Nephrons: 1) Cortical Nephrons (85%): • Located entirely in the cortex • Short loops of Henle 2) Juxtamedullary Nephrons (15%): • Bowman’s capsule in cortex; loop of Henle in medulla • Long loops of Henle Chapters 26: Urinary System Urinary System Anatomy: Blood Supply to Nephrons: Chapters 26: Urinary System Urinary System Physiology: Glomerular capillaries Afferent arteriole Urinary System Anatomy: Blood Supply to Nephrons: • 2 capillary networks in series: 1) Glomerulus (filtration) 2) Peritubular capillaries (reabsorption) • Single day → kidneys filter 60x normal blood plasma volume present • Consume 20 - 25 % of all oxygen at rest Efferent arteriole • Filtrate = all blood borne solutes except proteins Urine = metabolic waste and unneeded solutes • Major processes in urine formation: 1) Glomerular filtration (glomeruli) Bowman’s capsule Peritubular capillaries Interlobular artery 2) Tubular reabsorption (renal tubules) 3) Tubular secretion (renal tubules) Tubule Chapters 26: Urinary System Chapters 26: Urinary System Urinary System Physiology: Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force Urine Formation: Filtration Reabsorption Secretion Urine Production (to interlobular veins) Chapters 26: Urinary System Chapters 26: Urinary System Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force Colloid Osmotic Pressure Net Filtration Rate Capsular Hydrostatic Pressure = Chapters 26: Urinary System Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force 55 mm Hg - (15 mm Hg + 30 mm Hg) Chapters 26: Urinary System (Figure 26.9) Glomerular Hydrostatic Pressure Colloid Osmotic Pressure Net Filtration Rate Glomerular Hydrostatic Pressure Capsular Hydrostatic Pressure = 10 mm Hg Chapters 26: Urinary System Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force 2) Molecules filtered < 3 nm diameter • Water, glucose, amino acids, ions, nitrogenous waste • Blood cells / proteins too large Chapters 26: Urinary System Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force 2) Molecules filtered < 3 nm diameter Capillary endothelial cell Basement Membrane Podocytes Filtration membrane Filtration slits Water, glucose, amino acids, ions, nitrogenous waste Chapters 26: Urinary System Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force 2) Molecules filtered < 3 nm diameter 3) Glomerular filtration rate (GFR): • Volume of fluid filtered into Bowman’s capsule / minute • Normal adult = 120-150 ml/min • Factors governing filtration rate: 1) Surface area 2) Filtration membrane permeability 3) Net filtration pressure (↓15% GHP = no filtration) Chapters 26: Urinary System Chapters 26: Urinary System Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force 2) Molecules filtered < 3 nm diameter 3) Glomerular filtration rate (GFR): • Regulation of GFR: a) Myogenic control (intrinsic) • Afferent arteriole diameter directly related to flow in vessel ↑ BP = ↓ BP = ↑ constriction of afferent arteriole Smooth muscle relaxes = Afferent arteriole dilates Chapters 26: Urinary System Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force 2) Molecules filtered < 3 nm diameter 3) Glomerular filtration rate (GFR): • Regulation of GFR: a) Myogenic control (intrinsic) b) Tubuloglomerular feedback mechanism (intrinsic) • Macula densa cells (distal tubules) monitor: a) Rate of fluid flow in tubules b) level of Na+ in tubules Chapters 26: Urinary System Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force 2) Molecules filtered < 3 nm diameter 3) Glomerular filtration rate (GFR): • Regulation of GFR: a) Myogenic control (intrinsic) b) Tubuloglomerular feedback mechanism (intrinsic) • Macula densa cells (distal tubules) monitor: a) Rate of fluid flow in tubules b) level of Na+ in tubules • ↓ flow / ↓ osmolarity = vasodilation (afferent arteriole) • ↑ flow / ↑ osmolarity, vasoconstriction (afferent art.) Chapters 26: Urinary System Urinary System Physiology: Glomerular Filtration: 1) Blood pressure = driving force 2) Molecules filtered < 3 nm diameter 3) Glomerular filtration rate (GFR): • Regulation of GFR: a) Myogenic control (intrinsic) b) Tubuloglomerular feedback mechanism (intrinsic) c) Sympathetic nervous system (extrinsic) d) Renin-angtiotensin mechanism (extrinsic) • Juxtaglomerular cells monitor blood pressure • If BP ↓, release renin into blood (↑ BP) Chapters 26: Urinary System Chapters 26: Urinary System Urinary System Physiology: Urine Formation: Filtration Reabsorption Chapters 26: Urinary System Urinary System Physiology: Tubular Reabsorption: • Return of fluid from renal tubules to blood • ~ 80% of water & solutes reabsorbed at proximal tubule 1) Active processes: • Chemicals moved against gradient • Requires ATP (pumps in epithelial cell membranes) • Substances = Glucose, amino acids, most cations (e.g. Na+) 2) Passive processes: • Chemicals move down gradients (diffusion) • Gradients established across epithelial membranes Chapters 26: Urinary System Assisting movement into blood: • Highly permeable basement membrane • Low blood pressure and high [protein] in capillary Transport Maximum (Tm) Ø Diabetes Solvent Drag Obligatory water reabsorption (Figure 26.12) Chapters 26: Urinary System Urinary System Physiology: Tubular Reabsorption: Absorptive Capabilities of Tubules: Proximal Convoluted Tubule Glucose (100%) Amino acids (100%) Na+ (~ 70%) Water (~ 70%) HCO3- (~ 90%) Cl- (~ 50%) Chapters 26: Urinary System Urinary System Physiology: Tubular Reabsorption: Non-reabsorbed Substances: • End products of protein / nucleic acid metabolism Loop of Henle Distal Convoluted Tubule & Collecting Duct Na+ (~ 25%) Water (~ 25%) Cl- (~ 35%) Na+ (hormone dependent) Water (hormone dependent) Cl- (hormone dependent) • Urea*, creatinine, uric acid* • Not reabsorbed because: (1) Lack protein carriers (2) Not lipid soluble (3) Too large to pass through membrane pores Chapters 26: Urinary System Urinary System Physiology: Chapters 26: Urinary System Urinary System Physiology: Tubular Secretion: • Movement of material from capillary / tubule cells to filtrate • Proximal tubules / distal tubules / collecting ducts • Function: 1) Eliminating substances not in filtrate (e.g. antibiotics) Urine Formation: Filtration Reabsorption Secretion 2) Eliminating substances reabsorbed (e.g. urea) 3) Eliminating excess K+ (collecting ducts) 4) Balancing pH (proximal / distal tubules)