Pressure Ulcer Staging Definitions A. Stage I Pressure Ulcer: Intact
advertisement
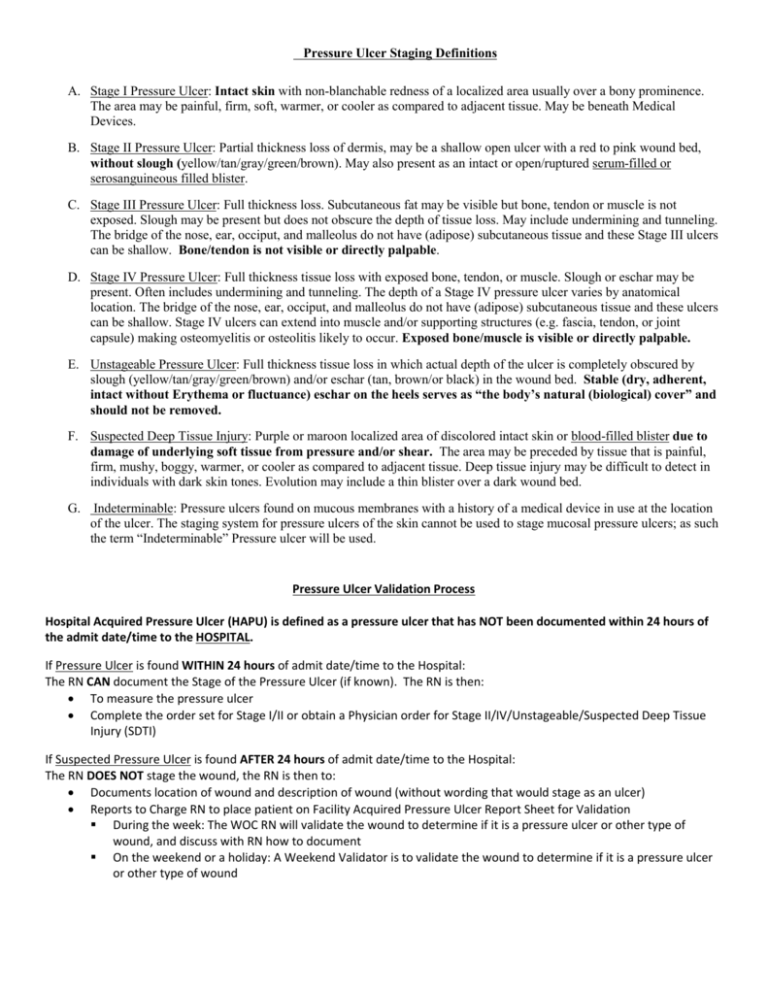
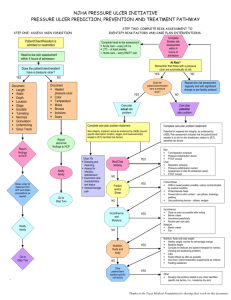
Pressure Ulcer Staging Definitions A. Stage I Pressure Ulcer: Intact skin with non-blanchable redness of a localized area usually over a bony prominence. The area may be painful, firm, soft, warmer, or cooler as compared to adjacent tissue. May be beneath Medical Devices. B. Stage II Pressure Ulcer: Partial thickness loss of dermis, may be a shallow open ulcer with a red to pink wound bed, without slough (yellow/tan/gray/green/brown). May also present as an intact or open/ruptured serum-filled or serosanguineous filled blister. C. Stage III Pressure Ulcer: Full thickness loss. Subcutaneous fat may be visible but bone, tendon or muscle is not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling. The bridge of the nose, ear, occiput, and malleolus do not have (adipose) subcutaneous tissue and these Stage III ulcers can be shallow. Bone/tendon is not visible or directly palpable. D. Stage IV Pressure Ulcer: Full thickness tissue loss with exposed bone, tendon, or muscle. Slough or eschar may be present. Often includes undermining and tunneling. The depth of a Stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput, and malleolus do not have (adipose) subcutaneous tissue and these ulcers can be shallow. Stage IV ulcers can extend into muscle and/or supporting structures (e.g. fascia, tendon, or joint capsule) making osteomyelitis or osteolitis likely to occur. Exposed bone/muscle is visible or directly palpable. E. Unstageable Pressure Ulcer: Full thickness tissue loss in which actual depth of the ulcer is completely obscured by slough (yellow/tan/gray/green/brown) and/or eschar (tan, brown/or black) in the wound bed. Stable (dry, adherent, intact without Erythema or fluctuance) eschar on the heels serves as “the body’s natural (biological) cover” and should not be removed. F. Suspected Deep Tissue Injury: Purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer, or cooler as compared to adjacent tissue. Deep tissue injury may be difficult to detect in individuals with dark skin tones. Evolution may include a thin blister over a dark wound bed. G. Indeterminable: Pressure ulcers found on mucous membranes with a history of a medical device in use at the location of the ulcer. The staging system for pressure ulcers of the skin cannot be used to stage mucosal pressure ulcers; as such the term “Indeterminable” Pressure ulcer will be used. Pressure Ulcer Validation Process Hospital Acquired Pressure Ulcer (HAPU) is defined as a pressure ulcer that has NOT been documented within 24 hours of the admit date/time to the HOSPITAL. If Pressure Ulcer is found WITHIN 24 hours of admit date/time to the Hospital: The RN CAN document the Stage of the Pressure Ulcer (if known). The RN is then: To measure the pressure ulcer Complete the order set for Stage I/II or obtain a Physician order for Stage II/IV/Unstageable/Suspected Deep Tissue Injury (SDTI) If Suspected Pressure Ulcer is found AFTER 24 hours of admit date/time to the Hospital: The RN DOES NOT stage the wound, the RN is then to: Documents location of wound and description of wound (without wording that would stage as an ulcer) Reports to Charge RN to place patient on Facility Acquired Pressure Ulcer Report Sheet for Validation During the week: The WOC RN will validate the wound to determine if it is a pressure ulcer or other type of wound, and discuss with RN how to document On the weekend or a holiday: A Weekend Validator is to validate the wound to determine if it is a pressure ulcer or other type of wound