Prevalon® Pressure-Relieving Heel Protector
Goes on in seconds for a
secure, comfortable fit
HEEL PROTECTION
For use with calf circumference
of 10”-18” (25cm-46cm)
Heel Pressure Ulcer Staging Guide
(Inside out)
Do not overtighten straps
Sequential compression
device compatible.
Make sure tubing is not
kinked or compressed
against patient’s skin.
1
Pull boot up around foot.
2
Make sure patient’s
heel is floated.
Wrap stretch panels
around boot.
3
Adjust straps.
Do not overtighten.
To reorder, contact Sage Customer Service 800-323-2220
www.sageproducts.com
21233D © Sage Products Inc. 2011
#7300
reorder #
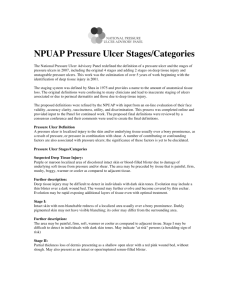
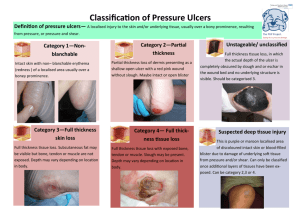
STAGE 2
STAGE 3
Partial thickness loss of
dermis; presents as
shallow open ulcer with a
red pink wound bed, no
slough present. May be
an intactor open/ruptured
serum-filled blister.
Full thickness tissue loss.
May be able to see
subcutaneous fat; can
NOT see bone, tendon or
muscle. Slough may be
present but you can still
see the depth of tissue
loss. Undermining and
tunneling may be present.
Copyright © 2008 Evonne Fowler, RN, CNS, CWOCN and Suzy Scott, RN, MSN, CWOCN.
Head Over Heels: Best Practices for Preventing Heel Ulcers, poster presented at the Symposium on Advanced
Wound Care, San Diego, CA April, 2008. All rights reserved. Reproduce with permission.
..........................................
Non-blanchable redness
of intact skin in a localized
area, usually over a bony
prominence. Darkly
pigmented skin may not
blanch; its color may differ
from surronging tissue.
..........................................
......................................
STAGE I
STAGE 4
UNSTAGEABLE
Full thickness tissue loss
with exposed bone,
tendon or muscle. May
have slough or eschar
but still can see base of
wound. Undermining and
tunneling often present.
Full thickness tissue loss
but the wound bed is
covered by slough
(yellow, tan, gray, green
or brown) and/or eschar
(tan, brown or black).
SUSPECTED DEEP
TISSUE INJURY
Local area of purple or
maroon discolored in tact
skin or blood-blister due
to damage of underlying
soft tissue from pressure
and/or shear. The area
may be preceded by
tissue that is painful, firm,
mushy, boggy, warmer or
cooler as compared to
adjacent tissue.
Comfort Shield®
Barrier Cream Cloths
ONE STEP
Cleans + Treats + Protects
Hypoallergenic
Durable
INCONTINENCE CARE
Skin Care for
Incontinent Persons
Incontinence-Associated Dermatitis
Intervention Tool
1. Cleanse incontinence ASAP and
apply barrier.
2. Document condition of skin at least
once every shift in nurseʼs notes.
3. Notify primary care provider when
skin injury occurs and collaborate
on the plan of care.
4. Consider use of external catheter
or fecal collector.
5. Consider short term use of urinary
catheter only if necessary.
Simple Interventions. Extraordinary Outcomes.
To reorder, contact Sage Customer Service
Ultra soft, rinse-free
Copyright © 2008 Joan Junkin. All rights reserved. Please send request for permissions to
IADIT@medbiopub.com.
1. Bliss DZ, Zehrer C, Savik K, et al. Incontinence-Associated Skin Damage in Nursing Home
Residents: A Secondary Analysis of a Prospective, Multicenter Study. Ost/Wound Mgmt.
2006;52:46–55. 2. Institute for Healthcare Improvement. Prevent Pressure Ulcers: How-To Guide.
May 2007. Available at: http://www.ihi.org/nr/rdonlyres/5ababb51-93b3-4d88-ae19be88b7d96858/0/pressureulcerhowtoguide.doc, accessed 10/21/07. 3. Gray M, Bliss DB, ErmerSeltun J, et al. Incontinence-associated Dermatitis: A Consensus. JWOCN. 2007;34:45-54.
800-323-2220
www.sageproducts.com
xxxx
21250C © Sage Products Inc. 2011
reorder #
DEFINITION
HIGH-RISK
MODERATE IAD
SEVERE IAD
FUNGAL APPEARING RASH
Skin exposed to stool and/or urine is dry, intact, and
not blistered, but is pink or red with diffuse (not
sharply defined), often irregular borders. In darker
skin tones, it might be more difficult to visualize color
changes (white or yellow color) and palpation may
be more useful.
Affected skin is bright or angry red – in darker skin tones, it may appear
white or yellow.
Affected skin is red with areas of denudement (partial thickness skin loss)
and oozing/bleeding. In dark skinned patients, the skin tones may be white
or yellow.
This may occur in addition to any level of IAD skin injury.
Palpation may reveal a warmer temperature
compared to skin not exposed. People with adequate
sensation and the ability to communicate may
complain of burning, stinging, or other pain.
This is painful whether or not the person can communicate the pain.
Skin is not erythematous or
warmer than nearby skin
but may show scars or color
changes from previous IAD
episodes and/or healed
pressure ulcer(s).
Person not able to
adequately care for self or
communicate need and is
incontinent of liquid stool at
least 3 times in 24 hours.1
INTERVENTION
EARLY IAD
Skin usually appears shiny and moist with weeping or pinpoint areas of
bleeding. Raised areas or small blisters may be noted.
Small areas of skin loss (dime size) if any.
Skin layers may be stripped off as the oozing protein is sticky and adheres
to any dry surface.
Usually spots are noted near edges of red areas (white or yellow areas in
dark skinned patients) that may appear as pimples or just flat red (white or
yellow) spots.
Person may report itching which may be intense.
1. Use a disposable barrier cloth containing cleanser, moisturizer and protectant.2
< Include treatments from box to left plus:
< Include treatments from box to left plus:
2. If barrier cloths not available, use acidic cleanser (6.5 or lower), not soap (soap
is too alkaline); cleanse gently (soak for a minute or two – no scrubbing); and
apply a protectant (ie: dimethicone, liquid skin barrier or petrolatum).
5. Consider applying a zinc oxide-based product for weepy or bleeding areas 3 times a
day and whenever stooling occurs.
10. Position the person semiprone BID to expose affected skin to air.
Ask primary care provider to order an anti-fungal powder or ointment. Avoid
creams in the case of IAD because they add moisture to a moisture damaged
area (main ingredient is water).
11. Consider treatments that reduce moisture: low air loss mattress/overlay, more
frequent turning, astringents such as Domeboro soaks.
1. If using powder, lightly dust powder to affected areas. Seal with ointment or
liquid skin barrier to prevent caking.
12. Consider the air flow type underpads (without plastic backing).
2. Continue the treatments based on the level of IAD.
3. If briefs or underpads are used, allow skin to be exposed to air. Use
containment briefs only for sitting in chair or ambulating – not while in bed.
6. Apply the ointment to a non-adherent dressing (such as anorectal dressing for cleft,
Telfa for flat areas, or ABD pad for larger areas) and gently place on injured skin to
avoid rubbing. Do not use tape or other adhesive dressings.
4. Manage the cause of incontinence: a) Determine why the patient is incontinent.
Check for urinary tract infection, b) Consider timed toileting or a bladder or
bowel program, c) Refer to incontinence specialist if no success.3
7. If using zinc oxide paste, do not scrub the paste completely off with the next cleaning.
Gently soak stool off top then apply new paste covered dressing to area.
8. If denuded areas remain to be healed after inflammation is reduced, consider BTC
ointment (balsam of peru, trypsin, castor oil) but remember balsam of peru is proinflammatory.
9. Consult WOCN if available.
3. Assess for thrush (oral fungal infection) and ask for treatment if present.
4. For women with fungal rash, ask health care provider to evaluate for vaginal
fungal infection and ask for treatment if needed.
5. Assess skin folds, including under breasts, under pannus, and in groin.
6. If no improvement, culture area for possible bacterial infection.
Prevalon® Pressure-Relieving Heel Protector with
Integrated Foot and Leg Stabilizer Wedge
Goes on in seconds for a secure, comfortable fit
HEEL PROTECTION
For use with calf circumference
of 10”-18” (25cm-46cm)
Heel Pressure Ulcer Staging Guide
1
Pull boot up around foot.
2
Adjust Wedge.
3
Wrap stretch panels
around boot.
4
Adjust straps.
Do not overtighten.
To reorder, contact Sage Customer Service 800-323-2220
www.sageproducts.com
21251C © Sage Products Inc. 2011
#7355
reorder #
STAGE 2
STAGE 3
Partial thickness loss of
dermis; presents as
shallow open ulcer with a
red pink wound bed, no
slough present. May be
an intactor open/ruptured
serum-filled blister.
Full thickness tissue loss.
May be able to see
subcutaneous fat; can
NOT see bone, tendon or
muscle. Slough may be
present but you can still
see the depth of tissue
loss. Undermining and
tunneling may be present.
Copyright © 2008 Evonne Fowler, RN, CNS, CWOCN and Suzy Scott, RN, MSN, CWOCN.
Head Over Heels: Best Practices for Preventing Heel Ulcers, poster presented at the Symposium on Advanced
Wound Care, San Diego, CA April, 2008. All rights reserved. Reproduce with permission.
..........................................
Non-blanchable redness
of intact skin in a localized
area, usually over a bony
prominence. Darkly
pigmented skin may not
blanch; its color may differ
from surronging tissue.
..........................................
......................................
STAGE I
STAGE 4
UNSTAGEABLE
Full thickness tissue loss
with exposed bone,
tendon or muscle. May
have slough or eschar
but still can see base of
wound. Undermining and
tunneling often present.
Full thickness tissue loss
but the wound bed is
covered by slough
(yellow, tan, gray, green
or brown) and/or eschar
(tan, brown or black).
SUSPECTED DEEP
TISSUE INJURY
Local area of purple or
maroon discolored in tact
skin or blood-blister due
to damage of underlying
soft tissue from pressure
and/or shear. The area
may be preceded by
tissue that is painful, firm,
mushy, boggy, warmer or
cooler as compared to
adjacent tissue.
HEEL PROTECTION
Heel Pressure Ulcer Staging Guide
Simple Interventions. Extraordinary Outcomes.
* Developed by Christine Baker, RN, MSN, CWOCN, APN
Taken from Poster, Head Over Heels: Best Practices for
Preventing Heel Ulcers, presented at the Symposium on
Advanced Wound Care, San Diego, CA, April, 2008.
To reorder, contact Sage Customer Service
800-323-2220
www.sageproducts.com
21252C © Sage Products Inc. 2011
#7355
reorder #
STAGE 2
STAGE 3
Partial thickness loss of
dermis; presents as
shallow open ulcer with a
red pink wound bed, no
slough present. May be
an intactor open/ruptured
serum-filled blister.
Full thickness tissue loss.
May be able to see
subcutaneous fat; can
NOT see bone, tendon or
muscle. Slough may be
present but you can still
see the depth of tissue
loss. Undermining and
tunneling may be present.
Copyright © 2008 Evonne Fowler, RN, CNS, CWOCN and Suzy Scott, RN, MSN, CWOCN.
Head Over Heels: Best Practices for Preventing Heel Ulcers, poster presented at the Symposium on Advanced
Wound Care, San Diego, CA April, 2008. All rights reserved. Reproduce with permission.
..........................................
Non-blanchable redness
of intact skin in a localized
area, usually over a bony
prominence. Darkly
pigmented skin may not
blanch; its color may differ
from surronging tissue.
..........................................
......................................
STAGE I
STAGE 4
UNSTAGEABLE
Full thickness tissue loss
with exposed bone,
tendon or muscle. May
have slough or eschar
but still can see base of
wound. Undermining and
tunneling often present.
Full thickness tissue loss
but the wound bed is
covered by slough
(yellow, tan, gray, green
or brown) and/or eschar
(tan, brown or black).
SUSPECTED DEEP
TISSUE INJURY
Local area of purple or
maroon discolored in tact
skin or blood-blister due
to damage of underlying
soft tissue from pressure
and/or shear. The area
may be preceded by
tissue that is painful, firm,
mushy, boggy, warmer or
cooler as compared to
adjacent tissue.
see individual product package(s) for complete information
STEP 2: ORAL CLEANSING RECOMMENDATIONS
Score of 5
Score of 6 to 10
Score of 11 to 20
NO OBSERVED DYSFUNCTION,
MILD DYSFUNCTION
MODERATE TO SEVERE DYSFUNCTION
but at possible risk for alteration in integrity,
function, or comfort of oral cavity.
of integrity, function, or comfort of oral cavity.
of integrity, function, or comfort of oral cavity.
1. Perform oral assessment on admission and
once daily.
2. Remove and brush dentures 2 times daily
(same time as oral care).
3. Perform oral care 4 times daily (after meals,
at bedtime).
4. Use Ultra-Soft Toothbrush and Sodium
Bicarbonate Mouthpaste to clean teeth, gums
and entire oral mucosa.
1. Perform oral assessment on admission and 2 times
daily (AM and PM).
2. Remove and brush dentures 2 times daily (same
time as oral care); leave out if irritating.
3. Perform oral care 6 to 12 times daily.
4. Use Ultra-Soft Toothbrush and Sodium Bicarbonate
Mouthpaste to clean teeth, gums and entire oral
mucosa. If painful or risk of bleeding, use Toothette®
Plus Swabs.
1. Perform oral assessment on admission and 3
times daily.
2. Remove dentures (and leave out).
3. Perform oral care 12 times daily.
4. Use Toothette® Plus Swabs and Sodium
Bicarbonate Mouthpaste, Perox-A-Mint® Solution
or Antiseptic Oral Rinse to clean teeth, gums and
entire oral mucosa.
For patients requiring suction, use Suction
Swabs or Suction Brushes.
5. Rinse with Perox-A-Mint® Solution, Antiseptic
Oral Rinse or water.
6. Apply Mouth Moisturizer to lips and oral mucosa
to lubricate and moisturize
For patients requiring suction, use Suction Swabs or
Suction Brushes.
5. Rinse with Perox-A-Mint® Solution, Antiseptic Oral
Rinse or water.
6. Apply Mouth Moisturizer to lips and oral mucosa to
lubricate and moisturize (frequently; after oral care
and 4 times daily minimum).
Product Reorder #s
Product Reorder #s
ORAL HYGIENE
Oral Cavity Assessment Tool
and Recommended Care Guide
For patients requiring suction, use Suction Swabs
or Suction Brushes.
5. Rinse with Perox-A-Mint® Solution, Antiseptic Oral
Rinse or water.
6. Apply Mouth Moisturizer to lips and oral mucosa to
lubricate and moisturize (every 1 to 2 hours; after
oral care and as needed).
Product Reorder #s
xxxx
reorder #
Directions:
begin upon admission
STEP 1: ORAL ASSESSMENT
• Determine rating for each category.
• Add up ratings.
• Implement interventions based on total score.
Note: Use Universal Precautions during oral
assessment and intervention. Refer to your facility
policy and procedure for oral cavity exams. With
all oral care, be especially cautious to prevent
aspiration with patients who have a compromised
gag reflex. If assessment determines a potential
need for cultures, protective agents, topical
anesthetics or medications, consult a physician.
Adapted with permission from Beck, S.L., Oral Exam Guide 1991.
Simple Interventions. Extraordinary Outcomes.
To reorder, contact Sage Customer Service
800-323-2220
www.sageproducts.com
21299C © Sage Products Inc. 2011
CATEGORY
1
2
3
4
RATING
Smooth, pink, moist,
and intact
Slightly wrinkled and dry;
one or more isolated
reddened areas
Dry and somewhat swollen;
may have one or two isolated
blisters; inflammatory line
of demarcation
Extremely dry and edematous;
entire lip inflamed; generalized blisters or
ulceration
1 2 3 4
Smooth, pink, moist,
and intact
Pale and slightly dry; one
or two isolated lesions,
blisters, or reddened areas
Dry and somewhat swollen;
generalized redness; more than two
isolated lesions, blisters, or
reddened areas
Extremely dry and edematous;
entire mucosa very red and inflamed;
multiple confluent ulcers
1 2 3 4
Smooth, pink, moist,
and intact
Slightly dry; one or two
isolated reddened areas;
papillae prominent
particularly at base
Dry and somewhat swollen;
generalized redness but tip
and papillae are redder; one or two
isolated lesions or blisters
Extremely dry and edematous; thick and
engorged; entire tongue quite inflamed; tip
very red and demarcated with coating;
multiple blisters or ulcers
Teeth
Clean; no debris
Minimal debris; mostly
between teeth
Moderate debris clinging to
half of visible enamel
Covered with debris
1 2 3 4
Saliva
Thin, watery, plentiful
Increased in amount
Scanty; may be thicker
than normal
Thick and ropy, viscid,
or mucoid
1 2 3 4
Lips
Gingiva and
oral mucosa
Tongue
See back for recommended oral care summaries.
TOTAL SCORE:
1 2 3 4
Prevalon® Petite Pressure-Relieving Heel Protector
Goes on in seconds for a
secure, comfortable fit
HEEL PROTECTION
For use with calf circumference of 6”-10” (15cm-25cm)
and for feet smaller than 9.31 in. / 23.65 cm in length
Heel Pressure Ulcer Staging Guide
(Inside out)
Do not overtighten straps
Sequential compression
device compatible.
Make sure tubing is not
kinked or compressed
against patient’s skin.
1
Pull boot up around foot.
2
Make sure patient’s
heel is floated.
Wrap stretch panels
around boot.
3
Adjust straps.
Do not overtighten.
To reorder, contact Sage Customer Service 800-323-2220
www.sageproducts.com
21362B © Sage Products Inc. 2011
#7310/#7312
reorder #
STAGE 2
STAGE 3
Partial thickness loss of
dermis; presents as
shallow open ulcer with a
red pink wound bed, no
slough present. May be
an intactor open/ruptured
serum-filled blister.
Full thickness tissue loss.
May be able to see
subcutaneous fat; can
NOT see bone, tendon or
muscle. Slough may be
present but you can still
see the depth of tissue
loss. Undermining and
tunneling may be present.
Copyright © 2008 Evonne Fowler, RN, CNS, CWOCN and Suzy Scott, RN, MSN, CWOCN.
Head Over Heels: Best Practices for Preventing Heel Ulcers, poster presented at the Symposium on Advanced
Wound Care, San Diego, CA April, 2008. All rights reserved. Reproduce with permission.
..........................................
Non-blanchable redness
of intact skin in a localized
area, usually over a bony
prominence. Darkly
pigmented skin may not
blanch; its color may differ
from surronging tissue.
..........................................
......................................
STAGE I
STAGE 4
UNSTAGEABLE
Full thickness tissue loss
with exposed bone,
tendon or muscle. May
have slough or eschar
but still can see base of
wound. Undermining and
tunneling often present.
Full thickness tissue loss
but the wound bed is
covered by slough
(yellow, tan, gray, green
or brown) and/or eschar
(tan, brown or black).
SUSPECTED DEEP
TISSUE INJURY
Local area of purple or
maroon discolored in tact
skin or blood-blister due
to damage of underlying
soft tissue from pressure
and/or shear. The area
may be preceded by
tissue that is painful, firm,
mushy, boggy, warmer or
cooler as compared to
adjacent tissue.
Prevalon® XL Pressure-Relieving Heel Protector with
Integrated Foot and Leg Stabilizer Wedge
Goes on in seconds for a secure, comfortable fit
HEEL PROTECTION
For use with calf circumference
of 18”-24” (46cm-61cm)
Heel Pressure Ulcer Staging Guide
1
Pull boot up around foot.
2
Adjust Wedge.
3
Wrap stretch panels
around boot.
4
Adjust straps.
Do not overtighten.
To reorder, contact Sage Customer Service 800-323-2220
www.sageproducts.com
21363B © Sage Products Inc. 2011
#7382
reorder #
STAGE 2
STAGE 3
Partial thickness loss of
dermis; presents as
shallow open ulcer with a
red pink wound bed, no
slough present. May be
an intactor open/ruptured
serum-filled blister.
Full thickness tissue loss.
May be able to see
subcutaneous fat; can
NOT see bone, tendon or
muscle. Slough may be
present but you can still
see the depth of tissue
loss. Undermining and
tunneling may be present.
Copyright © 2008 Evonne Fowler, RN, CNS, CWOCN and Suzy Scott, RN, MSN, CWOCN.
Head Over Heels: Best Practices for Preventing Heel Ulcers, poster presented at the Symposium on Advanced
Wound Care, San Diego, CA April, 2008. All rights reserved. Reproduce with permission.
..........................................
Non-blanchable redness
of intact skin in a localized
area, usually over a bony
prominence. Darkly
pigmented skin may not
blanch; its color may differ
from surronging tissue.
..........................................
......................................
STAGE I
STAGE 4
UNSTAGEABLE
Full thickness tissue loss
with exposed bone,
tendon or muscle. May
have slough or eschar
but still can see base of
wound. Undermining and
tunneling often present.
Full thickness tissue loss
but the wound bed is
covered by slough
(yellow, tan, gray, green
or brown) and/or eschar
(tan, brown or black).
SUSPECTED DEEP
TISSUE INJURY
Local area of purple or
maroon discolored in tact
skin or blood-blister due
to damage of underlying
soft tissue from pressure
and/or shear. The area
may be preceded by
tissue that is painful, firm,
mushy, boggy, warmer or
cooler as compared to
adjacent tissue.
HEEL PROTECTION
Heel Pressure Ulcer Staging Guide
Simple Interventions. Extraordinary Outcomes.
* Developed by Christine Baker, RN, MSN, CWOCN, APN
Taken from Poster, Head Over Heels: Best Practices for
Preventing Heel Ulcers, presented at the Symposium on
Advanced Wound Care, San Diego, CA, April, 2008.
To reorder, contact Sage Customer Service
800-323-2220
www.sageproducts.com
#7300
21617 © Sage Products Inc. 2011
reorder #
STAGE 2
STAGE 3
Partial thickness loss of
dermis; presents as
shallow open ulcer with a
red pink wound bed, no
slough present. May be
an intactor open/ruptured
serum-filled blister.
Full thickness tissue loss.
May be able to see
subcutaneous fat; can
NOT see bone, tendon or
muscle. Slough may be
present but you can still
see the depth of tissue
loss. Undermining and
tunneling may be present.
Copyright © 2008 Evonne Fowler, RN, CNS, CWOCN and Suzy Scott, RN, MSN, CWOCN.
Head Over Heels: Best Practices for Preventing Heel Ulcers, poster presented at the Symposium on Advanced
Wound Care, San Diego, CA April, 2008. All rights reserved. Reproduce with permission.
..........................................
Non-blanchable redness
of intact skin in a localized
area, usually over a bony
prominence. Darkly
pigmented skin may not
blanch; its color may differ
from surronging tissue.
..........................................
......................................
STAGE I
STAGE 4
UNSTAGEABLE
Full thickness tissue loss
with exposed bone,
tendon or muscle. May
have slough or eschar
but still can see base of
wound. Undermining and
tunneling often present.
Full thickness tissue loss
but the wound bed is
covered by slough
(yellow, tan, gray, green
or brown) and/or eschar
(tan, brown or black).
SUSPECTED DEEP
TISSUE INJURY
Local area of purple or
maroon discolored in tact
skin or blood-blister due
to damage of underlying
soft tissue from pressure
and/or shear. The area
may be preceded by
tissue that is painful, firm,
mushy, boggy, warmer or
cooler as compared to
adjacent tissue.
HEEL PROTECTION
Heel Pressure Ulcer Staging Guide
Simple Interventions. Extraordinary Outcomes.
* Developed by Christine Baker, RN, MSN, CWOCN, APN
Taken from Poster, Head Over Heels: Best Practices for
Preventing Heel Ulcers, presented at the Symposium on
Advanced Wound Care, San Diego, CA, April, 2008.
To reorder, contact Sage Customer Service
800-323-2220
www.sageproducts.com
21618 © Sage Products Inc. 2011
#7310/#7312
reorder #
STAGE 2
STAGE 3
Partial thickness loss of
dermis; presents as
shallow open ulcer with a
red pink wound bed, no
slough present. May be
an intactor open/ruptured
serum-filled blister.
Full thickness tissue loss.
May be able to see
subcutaneous fat; can
NOT see bone, tendon or
muscle. Slough may be
present but you can still
see the depth of tissue
loss. Undermining and
tunneling may be present.
Copyright © 2008 Evonne Fowler, RN, CNS, CWOCN and Suzy Scott, RN, MSN, CWOCN.
Head Over Heels: Best Practices for Preventing Heel Ulcers, poster presented at the Symposium on Advanced
Wound Care, San Diego, CA April, 2008. All rights reserved. Reproduce with permission.
..........................................
Non-blanchable redness
of intact skin in a localized
area, usually over a bony
prominence. Darkly
pigmented skin may not
blanch; its color may differ
from surronging tissue.
..........................................
......................................
STAGE I
STAGE 4
UNSTAGEABLE
Full thickness tissue loss
with exposed bone,
tendon or muscle. May
have slough or eschar
but still can see base of
wound. Undermining and
tunneling often present.
Full thickness tissue loss
but the wound bed is
covered by slough
(yellow, tan, gray, green
or brown) and/or eschar
(tan, brown or black).
SUSPECTED DEEP
TISSUE INJURY
Local area of purple or
maroon discolored in tact
skin or blood-blister due
to damage of underlying
soft tissue from pressure
and/or shear. The area
may be preceded by
tissue that is painful, firm,
mushy, boggy, warmer or
cooler as compared to
adjacent tissue.
HEEL PROTECTION
Heel Pressure Ulcer Staging Guide
Simple Interventions. Extraordinary Outcomes.
* Developed by Christine Baker, RN, MSN, CWOCN, APN
Taken from Poster, Head Over Heels: Best Practices for
Preventing Heel Ulcers, presented at the Symposium on
Advanced Wound Care, San Diego, CA, April, 2008.
To reorder, contact Sage Customer Service
800-323-2220
www.sageproducts.com
#7382
21619 © Sage Products Inc. 2011
reorder #
STAGE 2
STAGE 3
Partial thickness loss of
dermis; presents as
shallow open ulcer with a
red pink wound bed, no
slough present. May be
an intactor open/ruptured
serum-filled blister.
Full thickness tissue loss.
May be able to see
subcutaneous fat; can
NOT see bone, tendon or
muscle. Slough may be
present but you can still
see the depth of tissue
loss. Undermining and
tunneling may be present.
Copyright © 2008 Evonne Fowler, RN, CNS, CWOCN and Suzy Scott, RN, MSN, CWOCN.
Head Over Heels: Best Practices for Preventing Heel Ulcers, poster presented at the Symposium on Advanced
Wound Care, San Diego, CA April, 2008. All rights reserved. Reproduce with permission.
..........................................
Non-blanchable redness
of intact skin in a localized
area, usually over a bony
prominence. Darkly
pigmented skin may not
blanch; its color may differ
from surronging tissue.
..........................................
......................................
STAGE I
STAGE 4
UNSTAGEABLE
Full thickness tissue loss
with exposed bone,
tendon or muscle. May
have slough or eschar
but still can see base of
wound. Undermining and
tunneling often present.
Full thickness tissue loss
but the wound bed is
covered by slough
(yellow, tan, gray, green
or brown) and/or eschar
(tan, brown or black).
SUSPECTED DEEP
TISSUE INJURY
Local area of purple or
maroon discolored in tact
skin or blood-blister due
to damage of underlying
soft tissue from pressure
and/or shear. The area
may be preceded by
tissue that is painful, firm,
mushy, boggy, warmer or
cooler as compared to
adjacent tissue.
Prevalon Turn & Position System
®
Helps protect patients and staff!
1
Sacral Protection
• For single patient use only.
• Weight capacity: 350 lbs./160 kg.
2
4
Instructions for Use & Staging Guide
5
Sacrum
1
1
3
Place Prevalon Turn
and Position System
under patient.
CAUTION:
2
3
Position 30-Degree
Wedges to offload
sacrum.
Pull handles to turn
patient.
• DO NOT use Prevalon Turn and Position System to lift patients.
• Patient repositioning should always be performed following your facility’s safe patient handling policies & procedures.
• Periodically check product for signs of wear. Replace if product is damaged.
4
Adjust head of bed to
desired angle. Attach
Anti- Shear Strap on
Glide Sheet to Fastener
Strip on bed frame.
5
Product stays under
patient. Always ready
for next turn.
To reorder, contact Sage Customer Service
800-323-2220 / www.sageproducts.com
21703 © Sage Products Inc. 2012
#7200
reorder#
Stage I:
Non-blanchable
Erythema
Intact skin with nonblanchable redness of a
localized area usually over
a bony prominence. Darkly
pigmented skin may not
have visible blanching; its
color may differ from the
surrounding area.
Stage II:
Partial Thickness
of dermis
Partial thickness loss of
dermis presenting as a
shallow open ulcer with
a red pink wound bed,
without slough. May also
present as an intact or
open/ruptured serumfilled blister.
Reference: “European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Pressure Ulcer
Prevention & Treatment of: Quick Reference Guide.” Washington, DC: National Pressure Ulcer Advisory Panel, 2009.
Photos Used with permission of the National Pressure Ulcer Advisory Panel, March 2012
Stage III:
Full Thickness
tissue Loss
Full thickness tissue loss.
Subcutaneous fat may be
visible but bone, tendon or
muscle are not exposed.
Slough may be present
but does not obscure the
depth of tissue loss. May
include undermining and
tunneling.
Stage IV:
Full Thickness
Tissue Loss
Full thickness tissue
loss with exposed bone,
tendon or muscle. Slough
or eschar may be present.
Often include undermining
and tunneling
Suspected Deep
Tissue Injury –
Depth Unknown
Purple or maroon localized
area of discolored intact skin
or blood-filled blister due to
damage of underlying soft
tissue from pressure and/
or shear. The area may be
preceded by tissue that
is painful, firm, mushy,
boggy, warmer or cooler as
compared to adjacent tissue.
Prevalon Turn & Position System 2.0
®
Helps protect patients and staff!
SACRAL PROTECTION
• For single patient use only.
• Weight capacity: 550 lbs./250 kg.
1
3
5
7
2
4
6
8
1
Make sure bed brakes are locked, bed
is flat (if patient condition allows) and at
waist level. Always follow your facility’s
safe patient handling policies and
procedures.
2
Lower bed rail closest to you. Unfold Glide
Sheet with Body Pad alongside of supine
patient. Tag on underside of Glide Sheet
should be unfolded toward head of bed.
Align upper edge of Glide Sheet with
patient’s shoulders.
CAUTION:
3
4
Roll patient away from you onto their side.
Tuck Glide Sheet with Body Pad under
patient and unroll toward you. Raise bed
rail. Repeat on other side. Using black
handles, align the patient’s hips with the
hip indicator on the bed.
Place Wedge with label side up. Lift edge
of Glide Sheet and gently push wedge
under patient, allowing Wedge to initiate
patient turning movement.
5
6
Place Anchor Wedge with label side up.
Grasp Anchor and slide under patient’s
thighs. Wedges should be approximately 8
in/20 cm apart at the sacrum. Gently push
Wedge under patient, allowing Wedge
to initiate patient turning movement. Pull
Anchor taut on other side of bed.
With both hands, grasp black handles on
Glide Sheet near patient’s hips. Gently
PULL (don’t lift) until patient is positioned
at desired angle. Once positioned, sacrum
should be offloaded.
• DO NOT use Prevalon Turn and Position System to lift patients.
• Patient repositioning should always be performed following your facility’s safe patient handling policies & procedures.
• Periodically check product for signs of wear. Replace if product is damaged.
7
8
Instructions for Use & Staging Guide
To reposition patient, remove Body
Wedges by grabbing corner and rotating
wedge out. Refer to your facility’s protocol
for frequency of repositioning.
Boost Straps may be used to assist in
repositioning. Always follow recommended
posture and technique. Locate orange
straps on Glide Sheet. Slide both hands
through strap loops until they are wrapped
around your wrists/forearms. Grasp the
straight part of each
To reorder, contact Sage Customer Service
800-323-2220 / www.sageproducts.com
22284 © 2014 Sage Products LLC
STAGE I:
NON-BLANCHABLE
ERYTHEMA
Intact skin with nonblanchable redness of a
localized area usually over
a bony prominence. Darkly
pigmented skin may not
have visible blanching; its
color may differ from the
surrounding area.
STAGE II:
PARTIAL THICKNESS
OF DERMIS
Partial thickness loss of
dermis presenting as a
shallow open ulcer with
a red pink wound bed,
without slough. May also
present as an intact or
open/ruptured serumfilled blister.
Reference: “European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory
Panel. Pressure Ulcer Prevention & Treatment of: Quick Reference Guide.” Washington, DC:
National Pressure Ulcer Advisory Panel, 2009.
Photos Used with permission of the National Pressure Ulcer Advisory Panel, March 2012
STAGE III:
FULL THICKNESS
TISSUE LOSS
Full thickness tissue loss.
Subcutaneous fat may be
visible but bone, tendon or
muscle are not exposed.
Slough may be present but
does not obscure the depth
of tissue loss. May include
undermining and tunneling.
STAGE IV:
FULL THICKNESS
TISSUE LOSS
Full thickness tissue loss
with exposed bone, tendon
or muscle. Slough or eschar
may be present. Often
include undermining and
tunneling
SUSPECTED DEEP
TISSUE INJURY –
DEPTH UNKNOWN
Purple or maroon localized
area of discolored intact skin
or blood-filled blister due to
damage of underlying soft
tissue from pressure and/
or shear. The area may be
preceded by tissue that is
painful, firm, mushy, boggy,
warmer or cooler as compared
to adjacent tissue.
Prevalon Turn & Position System
®
Helps protect patients and staff!
SACRAL PROTECTION
• For single patient use only.
• Weight capacity: 800 lbs./362 kg.
1
3
5
7
2
4
6
8
1
Mattress cover takes the place of fitted/flat
sheet. Place the two black elastic corner
straps around underside of mattress at
head of bed.
2
Attach all 4 black corner straps loosely.
Disconnect the short end of black side
straps and loop around restraint target or
other points of attachment. Fasten straps
loosely to part of frame that moves during
bed adjustment. Tighten all straps securely
and make sure Mattress Cover is taut.
CAUTION:
3
Align upper edge of Glide Sheet with
patient’s shoulders. Roll patient away from
you onto his/her side. Tuck Glide Sheet
with Body Pad under patient and unroll
towards you. Raise bed rail.
4
Repeat on other side and center patient
on bed. Attach Anti-Shear Strap on Glide
Sheet to the Mattress Cover.
5
6
Insert Body Wedges blue side up/gray
side down between Mattress Cover and
Glide Sheet by sliding over fabric flap on
Mattress Cover. Fabric flap should be
folded down over white hook and loop
fastener when inserting Wedges. First
Wedge goes under patient’s back. Second
Wedge goes under patient’s thigh.
Grasp black handles on Glide Sheet and
gently PULL (don’t lift) patient across bed
horizontally toward you until patient is
angled between 20-30° on Body Wedges.
• DO NOT use Prevalon Turn and Position System to lift patients.
• Patient repositioning should always be performed following your facility’s safe patient handling policies & procedures.
• Periodically check product for signs of wear. Replace if product is damaged.
7
8
Instructions for Use & Staging Guide
As patient is positioned, fabric flap will
fold back and Wedges will lock into place
on hook and loop fastener. Underside of
Glide Sheet can also be adhered to hook
and loop fastener on outside of Wedges.
When positioned correctly, sacrum should
be offloaded (free from contact). Prevent
patient’s heels and head from dragging
across bed during repositioning. Smooth
out any wrinkles in Glide Sheet and Body
Pad. Raise bed rails.
Adjust head of bed to desired angle.
To reorder, contact Sage Customer Service
800-323-2220 / www.sageproducts.com
22107 © Sage Products LLC 2013
STAGE I:
NON-BLANCHABLE
ERYTHEMA
Intact skin with nonblanchable redness of a
localized area usually over
a bony prominence. Darkly
pigmented skin may not
have visible blanching; its
color may differ from the
surrounding area.
STAGE II:
PARTIAL THICKNESS
OF DERMIS
Partial thickness loss of
dermis presenting as a
shallow open ulcer with
a red pink wound bed,
without slough. May also
present as an intact or
open/ruptured serumfilled blister.
Reference: “European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory
Panel. Pressure Ulcer Prevention & Treatment of: Quick Reference Guide.” Washington, DC:
National Pressure Ulcer Advisory Panel, 2009.
Photos Used with permission of the National Pressure Ulcer Advisory Panel, March 2012
STAGE III:
FULL THICKNESS
TISSUE LOSS
Full thickness tissue loss.
Subcutaneous fat may be
visible but bone, tendon or
muscle are not exposed.
Slough may be present but
does not obscure the depth
of tissue loss. May include
undermining and tunneling.
STAGE IV:
FULL THICKNESS
TISSUE LOSS
Full thickness tissue loss
with exposed bone, tendon
or muscle. Slough or eschar
may be present. Often
include undermining and
tunneling
SUSPECTED DEEP
TISSUE INJURY –
DEPTH UNKNOWN
Purple or maroon localized
area of discolored intact skin
or blood-filled blister due to
damage of underlying soft
tissue from pressure and/
or shear. The area may be
preceded by tissue that is
painful, firm, mushy, boggy,
warmer or cooler as compared
to adjacent tissue.
Prevalon Seated Positioning System
Helps protect patients and staff
®
SACRAL PROTECTION
• For single patient use only.
• Weight capacity: 350 lbs/160 kg
Instructions for Use & Staging Guide
1
2
3
4
Sacral Sitting
1
Prior to Positioning Patient:
Position chair with space behind the chair
for clinician(s) access. Lock chair brakes.
Place SPS on chair seat, with product tag
at the back of the seat, facing up. Tuck
slightly into chair crease. The clear air
chambers should be in direct contact with
the chair surface.
2
Make sure the top layer of SPS is fully
extended over the front of the seat.
Keep handles accessible (not under
patient). Cover SPS with the Microclimate
Management Pad.
3
Patient Positioning:
Following patient handling policy/
procedures, assist patient onto chair
and SPS.
4
When patient is safely seated, brace a
foot or leg on the back of the chair for
support. Simultaneously pull handles
until the patient slides back into chair,
in the upright seated position. Secure
handles behind chair so they are safely
out of the way.
Proper Sitting
CAUTION:
• DO NOT use Prevalon Seated Positioning System to lift patients.
• Patient repositioning should always be performed following your facility’s safe patient handling policies & procedures.
• Periodically check product for signs of wear. Replace if product is damaged.
• DO NOT launder. Wipe clean with a damp cloth.
• Only use with standard hospital chair, or rolling chair with brakes.
• Not recommended for use with a wheelchair.
To reorder, contact Sage Customer Service
800-323-2220 / www.sageproducts.com
22185 © Sage Products LLC 2013
STAGE I:
NON-BLANCHABLE
ERYTHEMA
Intact skin with nonblanchable redness of a
localized area usually over
a bony prominence. Darkly
pigmented skin may not
have visible blanching; its
color may differ from the
surrounding area.
STAGE II:
PARTIAL THICKNESS
OF DERMIS
Partial thickness loss of
dermis presenting as a
shallow open ulcer with a
red pink wound bed, without
slough. May also present as
an intact or open/ruptured
serumfilled blister.
Reference: “European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory
Panel. Pressure Ulcer Prevention & Treatment of: Quick Reference Guide.” Washington, DC:
National Pressure Ulcer Advisory Panel, 2009.
Photos Used with permission of the National Pressure Ulcer Advisory Panel, March 2012
STAGE III:
FULL THICKNESS
TISSUE LOSS
Full thickness tissue loss.
Subcutaneous fat may be
visible but bone, tendon or
muscle are not exposed.
Slough may be present but
does not obscure the depth
of tissue loss. May include
undermining and tunneling.
STAGE IV:
FULL THICKNESS
TISSUE LOSS
Full thickness tissue loss
with exposed bone, tendon
or muscle. Slough or eschar
may be present. Often
include undermining and
tunneling.
SUSPECTED DEEP
TISSUE INJURY –
DEPTH UNKNOWN
Purple or maroon localized
area of discolored intact skin
or blood-filled blister due to
damage of underlying soft
tissue from pressure and/
or shear. The area may be
preceded by tissue that is
painful, firm, mushy, boggy,
warmer or cooler as compared
to adjacent tissue.