Triglyceride-Rich Lipoproteins and Cardiovascular Disease
advertisement

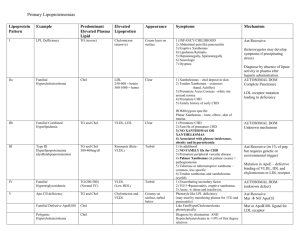
TriglycerideTriglyceride-Rich Lipoproteins and Cardiovascular Disease Tao Wang, Ph.D. Otsuka Maryland Research Institute Rockville, Maryland, USA Plaque of Coronary Atherosclerosis Endothelial Cells Basement Membrane Lipids Smooth Muscle Cells Adventitia Media Intima Lipid Accumulation Fatty Core of Plaque Thrombosis Fat Swollen Muscle Cells Fibrous Cap of Plaque 1 Triglycerides and CHD Risk A metameta-analysis of prospective population studies (multivariate model) Men PROCAM CSCHDS N= 2,536 2,966 3,395 4,129 4,407 4,860 Summary 22,293 FHS WCGS ROG LRC Women FHS LRC 2,969 3,376 Summary 6,345 0.5 1.0 2.0 3.0 5.0 Relative Risk From Hokanson JE, Austin MS. J Cardiovascular Risk 1996;3:213-9. Combined Effects of Cholesterol and Triglycerides on Risk of Fatal Myocardial Infarction in the AMORIS Study From Walldius G, et al. Blood Pressure 1992; 1 (Suppl. 1): 35-42. 2 Association between Hypertriglyceridemia and Cardiovascular Disease via Other Mechanisms Small, Dense LDL Oxidized Lipoproteins TG Remnant Lipoproteins CVD Reduced HDL Thrombogenic Factors Triglyceride Concentration as an Estimate of Total TriglycerideTriglyceride-rich Lipoproteins Triglycerides Chylomicrons VLDL VLDL remnants Chylomicron remnants Remnant Lipoproteins IDL LDL 3 Questions on the Use of Triglyceride To Assess CHD Risk • Should it be measured? • What does it mean? • Should it be treated if elevated? • What are the treatments for elevated TG? Limitations of Using Triglyceride To Assess CHD Risk • Lack of independent effects • Patients with grossly elevated plasma triglyceride concentration (e.g., type I or V hyperlipoproteinemia) are not typically associated with higher CHD risk • Measurement is fraught with problems • Reflection of total triglyceride-rich lipoproteins which are very heterogeneous 4 TriglycerideTriglyceride-rich Lipoproteins and Their Components Neither cholesterol nor triglyceride is freely circulated in blood. They are carried by lipoproteins. Different lipoproteins have different atherogenic potentials. LDL-C Atherosclerosis Progression HDL-C Atherosclerosis Regression Cholesterol Lipoprotein Remnants Atherosclerosis Progression VLDL-C & Chylomicrons ? Triglycerides Metabolism of TriglycerideTriglyceride-rich Lipoproteins Peripheral circulation CM remnants CM B48 B E B A A EC E A C HDL A E C B100 E C Lipoprotein lipase C EC B C E B B E C E C ApoB/E ApoB/E receptors E C VLDL Liver VLDL remnants E B E C E B B C IDL LDL 5 Key Steps in Metabolism of TriglycerideTriglyceride-Rich Lipoproteins Peripheral circulation CM remnants CM B A B E E CC EC A E A C HDL Lipoprotein lipase E C C B C VLDL E E B C 1. Exchange of apo C with HDL Apo C-II is an essential cofactor for lipoprotein lipase 2. Hydrolysis by lipoprotein lipase Chylomicrons and VLDL are depleted with TG and enriched in cholesterol. They are transformed to chylomicron remnants and VLDL remnants, respectively. 3. Removal of apo C from remnants and enrichment with remnants with apo E Apo E is a ligand for apo B/E receptors which remove lipoprotein remnants from circulation, whereas Apo C-III impairs this process Liver B E EC ApoB/E ApoB/E receptors E B C VLDL remnants E Physical and Chemical Properties of Lipoprotein Remnants • Smaller and denser • Have altered eletrophoretic mobility • Depleted with triglycerides and enriched in cholesterol • Enriched in apo E Words of caution: All these properties are relative to their lipoprotein precursors. Remnants are a group of very heterogeneous lipoproteins. They are probably best described by their physiological properties than their physical or chemical properties. 6 Biological Effects of Lipoprotein Remnants • Impair endothelium-dependent vasorelaxation • More likely to be retained by heparan sulfate proteoglycans within the arterial intima • Bind to chylomicron receptors on macrophages and being taken up without modification • Enhance in vitro aggregation of platelets Measurement of Lipoprotein Remnants • Ultracentrifugation: mostly for IDL • Agarose gel electrophoresis: mostly for double pre-beta, or beta VLDL • Calculation: VLDL-C / TG or (VLDL-C - 0.17 x TG) / 0.521 • Polyacrylamide gel electrophoresis: mostly for “mid-band”, which is similar to IDL • Chemical precipitation followed by apo C measurement • Immunoseparation of remnant-like particles (RLP): mostly for apo-E enriched chylomicron remnants and VLDL remnants. 7 Measurement of IDL by Ultracentrifugation d = 1.019 kg/L d = 1.006 kg/L T6 Chylomicron + VLDL T9 IDL B6 LDL B9 HDL IDL = B6 - B9 Measurement of betabeta-VLDL by Ultracentrifugation followed by Agarose Gel Electrophoresis Normal Normal Type III HDL VLDL LDL 6 m 6 6 m m 06 6 6 ru 0 00 eru .00 .00 eru 00 .00 1 1. S <1 >1 S Se < 1. > 1. < > d d d d d d β-VLDL Measurement of β -VLDL requires the use of both ultracentrifugation (separation based on hydrated density) and agarose gel electrophoresis (separation based on charges) 8 Lipoprotein Measurement by LipoPhor HDL LDL VLDL VLDL LDL HDL IDL VLDL LDL IDL (“mid-band”) HDL LipoPhor is a commercial product based on polyacrylamide gel electrophoresis which separates lipoproteins by charge and molecule size Principle of the RLPRLP-Cholesterol Assay Immunoseparation Gel + Test Sample RLP LDL + nascent VLDL HDL Sepharose 4B + anti-apo B-100 Sepharose 4B + anti-apo A-1 Incubation at RT for 2 hours Cholesterol Quantification 9 RLPRLP-C as an Independent Risk Factor for CHD Variable p OR Hypertension < 0.0001 3.72 Age > 65 yr < 0.0001 2.66 0.0001 2.14 < 0.0005 2.17 < 0.01 1.59 0.71 1.07 HDL-C < 35 mg/dL Sex th RLP-C > 75 %ile LDL-C > 130 mg/dL # of CHD Patients = 213, # of Control = 2761 from cycle 4 of the Framingham Offspring Study RLPRLP-C Values in “Normolipidemic” CAD Patients 6.6 mg/dL All CAD cases and controls had total cholesterol < 240 mg/dL and TG < 200 mg/dL From Devaraj, et al. Am J Med 1998;104:445-50. 10 RLPRLP-C Values in Type II Diabetic Patients with or without Macrovascular Diseases Control (N = 24) Type II DM without MVD (N =24) Type II DM with MVD (N = 24) Age (yr) 55.4 ± 7.2 57.3 ± 7.4 60.0 ± 6.5 BMI (kg/m²) 27.5 ± 6.8 31.6 ± 6.0 31.7 ± 7.8 Cholesterol (mmol/L) 5.1 ± 0.8 5.0 ± 1.2 4.9 ± 0.9 TG (mmol/L) 1.3 ± 0.5 1.9 ± 1.2 1.6 ± 1.0 LDL-C (mmol/L) 3.4 ± 0.8 3.2 ± 1.0 3.2 ± 0.9 HDL-C (mmol/L) 1.3 ± 0.4 1.1 ± 0.3 1.2 ± 0.4 RLP-C (mmol/L) 0.15 ± 0.06 0.20 ± 0.10 0.23 ± 0.08 a,b RLP-C/TG 0.06 ± 0.03 0.06 ± 0.02 0.08 ± 0.03 b,c a,b: Compared with controls: a, p < 0.05 ; b, p < 0.005 c: Compared with type II DM without MVD: p < 0.05 From Hirany, et al. Clin Chem 2000;46:667-72. Predictability of Future Coronary Events By RLPRLP-C 135 patients with pre-existing CAD were followed-up for up to 3 years. Elevated RLP-C concentrations were the only independent predictor for future coronary events in a multivariate Cox proportional hazard analysis model including stenosis of the left main artery, number of diseased arteries, age, gender, history of smoking, diabetes mellitus, hypertension, hypercholesterolemia, low HDL-C, high LDL-C and hypertriglyceridemia. From Kugiyama, et al. Circulation 1999;99:2858-60. 11 Conclusions • Hypertriglyceridemia has been found to be associated with increased CHD risk. But the independent effect was not proven. • Triglyceride concentrations only reflect total triglyceride-rich lipoproteins. Measurement of more atherogenic lipoprotein remnants offers better performance in assessing CHD risk. • Lipoprotein remnants can be measured by ultracentrifugation, agarose gel electrophoresis, polyacrylamide gel electrophoresis and immunoseparation. Each method measures a unique fraction of lipoprotein remnants. • Lipoprotein remnants isolated by the RLP-Cholesterol Assay have been found to have atherogenic properties in in vitro experiments and proven to be an independent risk factor for CHD in clinical studies. • Measurement of lipoprotein remnants provides additional information on individuals’ risk for CHD. It should not be used to replace other other lipid and lipoprotein tests. 12