Servei de Farmacologia Clínica
advertisement

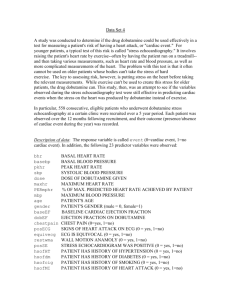
Servei de Farmacologia Clínica ® Levosimendan (Simdax ) for the treatment of patients with severe heart failure (HF) exacerbation Pharmacological characteristics Levosimendan is a positive inotrope. It increases calcium sensitivity in contractile myofilaments during systole. It has been suggested that the effect is reduced or lost during diastole and therefore would not alter myocardial relaxation or increase energy expenditure. An arterial (systemic and coronary) and venous vasodilator effect is also attributed to the drug, as it opens the ATP-dependant potassium channels and the selective inhibition of phosphodiesterase III. It is eliminated by hepatic metabolism and has an elimination half-life of one hour. However, one of its metabolites is active and has a more prolonged elimination half-life (75 to 80 hours); it has been suggested that some of its haemodynamic effects persist beyond the end of its infusion. Efficacy Table 1 includes information regarding four clinical trials with levosimendan. The first two, which involved patients with acute exacerbation of chronic heart failure (HF) resulting from ischemic or idiopathic heart disease, assessed haemodynamic effects. In the third trial, the incidence of hypotension and/or myocardial ischemia was evaluated in patients with recent acute myocardial infarction (five days prior) who had heart failure and needed intravenous positive inotropic therapy. In general, the differences in haemodynamic endpoints with short infusion durations (between 6 and 24 hours) favoured levosimendan as opposed to the placebo. Levosimendan was again favoured over dobutamine in a comparative study. In two of the studies, mortality was lower with levosimendan, but it was connected with a secondary endpoint. Patients treated with levosimendan showed improvements in dyspnoea in only one of the trials. The SURVIVE study was recently published and is the first clinical trial designed to evaluate mortality. It included 1,327 patients admitted for acute exacerbation of HF who required inotropic drugs, essentially, patients in NYHA functional class IV. Levosimendan (loading dose and infusion for up to 24 hours) was compared with dobutamine (infusion for a minimum of 24 hours) and no significant differences in mortality were observed in the first six months of the study (26% with levosimendan and 28% with dobutamine, RR=0.91; CI 95% 0.74-1.13). There were no differences in secondary endpoints either, such as mortality at 31 days, cardiovascular mortality at 6 months, dyspnoea or overall clinical evaluation; only plasma concentrations of B-type natriuretic peptide decreased more in patients treated with levosimendan. The results of two other clinical trials are known, but have yet to be published. The CASINO study included patients admitted with HF in NYHA functional class IV. However, it was interrupted before the scheduled finishing time (when 299 patients had been included instead of the anticipated 600) because the effects on mortality were favourable to levosimendan. At six months, mortality was significantly lower with levosimendan (15.3%) than with both dobutamine and the placebo (39.6 and 24.7%, respectively). Although the results were presented at a conference in 2004, the complete study has not yet been 2 published. Furthermore, it is not clear what the primary endpoint was or whether a correct intention-to-treat analysis was carried out. The REVIVE-2 trial involving 600 patients with similar characteristics has not been published either. The proportion of patients who experienced an improvement in clinical symptoms during hospitalisation (combined endpoint from the NYHA functional class and an overall evaluation) was 6% higher with levosimendan than with placebo, and the proportion that worsened was 7% less (p=0.015, for the group). In this study, more patients died at 90 days in the group treated with levosimendan than in the placebo group, although the differences are not statistically significant (45 and 35 patients, respectively). The levosimendan infusion was 24 hours in both studies. Study No. of patients (duration) Treatments Primary endpoint Slawsky et al (2000) 146 (6 h) Levosimendan (bolus of 6 μg/kg followed by 0.1-0.4 μg/kg per min) vs placebo . % of patients with: ↑ 25% EVa or ↓ of the PCPb at 6 hrs . Differences favouring levosimendan EV: 56% vs 4%; p<0.001 PCP: 43% vs 15%; p<0.001 LIDO (2002) 203 (24 h) Levosimendan (bolus of 24 μg/kg followed by 0.1-0.4 μg/kg per min) vs dobutamine (5 μg/kg per min) . % of patients with: ↑ 30% EVa and ↓ 25% of the PCPb at 24 hrs . Differences favouring levosimendan (28% vs. 15%, p=0.022) . mortality at 31 and 180 daysc: 8% vs 17%; p=0.049 26% vs 38%; p=0.029 P Results RUSSLAN (2002) 504 (6 h) Levosimendan 6 μg/kg and 0.1 μg/kg /min or 12 μg/kg and 0.2 μg/kg/min or 24 μg/kg and 0.2 μg/kg/min or 12 μg/kg and 0.4 μg/kg/min or placebo . % with hypotension or ischemia at 6 hrs . No differences . 13.4% with grouped levosimendan doses Vs 10.8%; p=0.456d . ↓ in mortality at 180 days with levosimendanc: 22.6% vs 31.4% SURVIVE (2007) 1,327 (24 h) Levosimendan (12 μg/kg bolus followed by 0-0.1 μg/kg/min) . Mortality due to any cause at 180 days . No significant differences in mortality (26% with levosimendan and 28% with dobutamine) vs dobutamine 5 μg /kg/min a b c EV: ejection volume, PCP: pulmonary capillary pressure, refers to a retrospectively-analysed d secondary endpoint, a dose relationship was observed (19% with the highest levosimendan dose). Toxicity In the LIDO trial, a comparative study with dobutamine, the total incidence of adverse effects was similar. Angina, thoracic pain and myocardial ischemia, as well as the proportion of patients with arrhythmias, was more frequent with dobutamine. There was a tendency of more hypotension and headaches with levosimendan, while there was more treatment termination due to adverse effects with dobutamine. An increase in heart rate (average of 11 beats per min) was documented with the highest dose (24 μg/kg bolus and 0.4 μg/kg/min infusion), but not for the lower doses. In the SURVIVE trial, the incidence of serious adverse effects and overall incidences were similar in both groups. This was also the case in the proportion of patients with hypotension. The presence of hypokalemia, auricular fibrillation, headaches and extrasystoles were more frequent with levosimendan than with dobutamine, whereas with dobutamine, there were more patients with a clinical diagnosis of HF (but not with congestive HF, which was similar in both groups). 3 Approved indications, dose and cost • Approved indications: short-term treatment of severe acute exacerbation of chronic HF and for situations in which conventional treatment is not sufficient or when inotropic assistance is required • Authorisation procedure: mutual recognition • Recommended dose is an initial 6 to 12 μg/kg in 10 minutes, followed by 0.1 μg/kg/min for 24 hours. The infusion speed can be modified based on response, between 0.05 and 0.2 μg/kg/min • Cost: the cost of one 5 ml vial with 2.5 mg/ml is € 700.64. For a 60 kg patient, the cost of a 24-hour treatment varies between € 504 and 521 if the infusion is 0.1 μg/kg/min. With dobutamine (5-10 μg/kg/min), the cost is around € 9-18. Comparison of alternatives (dobutamine) Advantages and disadvantages of levosimendan Efficacy Haemodynamic effects Symptoms Mortality Toxicity Convenience Cost Advantage (in a single comparative study with dobutamine) Similar (no differences in the published trial) Similar (no differences in the published trial) Similar (different profile) Similar Disadvantage Conclusion With the currently available data, we do not believe that levosimendan, in comparison with dobutamine, offers any advantages regarding mortality or symptoms. The incidence of adverse effects is similar, although the profile is slightly different and the cost is higher. For the moment, at least until all the information from the two studies pending publication is made available, it does not appear to offer any relevant advantages. References 1. Moiseyev VS, Poder P, Andrejevs N, Ruda MY, Golikov AP, Lazebnik LB, et al. Safety and efficacy of a novel calcium sensitizer, levosimendan, in patients with left ventricular failure due to an acute myocardial infarction. A randomized, placebo-controlled, double-blind study (RUSSLAN). Eur Heart J 2002;23:1.42232. http://eurheartj.oxfordjournals.org/cgi/reprint/23/18/1422 2. Follath F, Cleland JGF, Just H, Papp JGY, Scholz H, Peuhkurinen K, et al. Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low-output heart failure (the LIDO study): a randomised double-blind trial. Lancet 2002;360:196-202. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=12133 653 3. Jain P, Massie BM, Gattis WA, Klein L, Gheorghiade M. Current medical treatment for the exacerbation of chronic heart failure resulting in hospitalization. Am Heart J 2003;145:s3-s17. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=12594 447 4 4. Singh BN, Lilleberg J, Sandell EP, Ylonen V, Lehtonen L, Toivonen L. Effects of levosimendan on cardiac arrhythmia: electrophysiologic and ambulatory electrocardiographic findings in phase II and phase III clinical studies in cardiac failure. Am J Cardiol 1999;83:161-201. 5. Slawsky MT, Colucci WS, Gottlieb SS, Greenberg BH, Haeusslein E, Hare J, et al. Acute hemodynamic and clinical effects of levosimendan in patients with severe heart failure. Study Investigators. Circulation 2000;31:2.222-27. http://circ.ahajournals.org/cgi/content/full/102/18/2222 6. Nieminen MS, Akkila J, Hasenfuss G, Kleber FX, Lehtonen LA, Mitrovic V, et al. Hemodynamic and neurohumoral effects of continuous infusion of levosimendan in patients with congestive heart failure. J Am Coll Cardiol 2000;36:1903-12. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=11092 663 7. Mebazaa A, Nieminen MS, Packer M, Cohen-Solal A, Kleber FX, Pocock SJ, et al. Levosimendan vs dobutamine for patients with acute descompensated heart failure. The SURVIVE randomized trial. JAMA 2007;297:1883-91. http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=17473298& ordinalpos=1&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum 8. Cleeland JGF, Freemantle N, Coletta A, Clark AL. Clinical trials update from the American Heart Association: REPAIR-AMI, ASTAMI, JELIS, MEGA. REVIVE-II, SURVIVE, and PROACTIVE. Eur J Heart Fail 2006;8:105-10. http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=16387630& ordinalpos=2&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum 9. Cleland JG, Ghosh J, Freemantle N, Kaye GC, Nasir M, Clark AL, Coletta AP. Clinical trials update and cumulative meta-analyses from the American College of Cardiology: WATCH, SCD-HeFT, DINAMIT, CASINO, INSPIRE, STRATUS-US, RIO-Lipids and cardiac resynchronisation therapy in heart failure. Eur J Heart Fail 2004;6:501-8. http://www.ncbi.nlm.nih.gov/sites/entrez?Db=pubmed&Cmd=ShowDetailView&TermToSearch=16387630& ordinalpos=2&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum