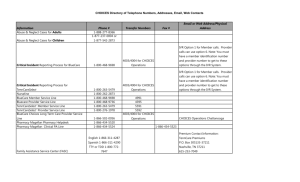
CHOICES Directory of Telephone Numbers, Addresses, Email, Web
advertisement
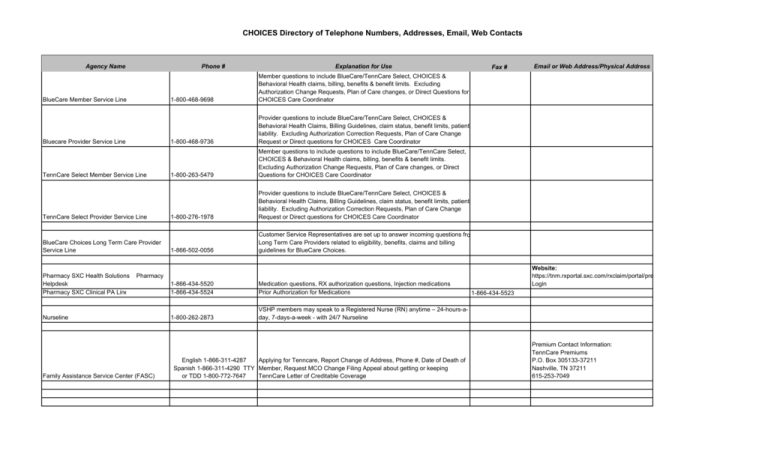
CHOICES Directory of Telephone Numbers, Addresses, Email, Web Contacts Agency Name Phone # BlueCare Member Service Line Bluecare Provider Service Line TennCare Select Member Service Line TennCare Select Provider Service Line BlueCare Choices Long Term Care Provider Service Line Pharmacy SXC Health Solutions Helpdesk Pharmacy SXC Clinical PA Line Explanation for Use 1-800-468-9698 Member questions to include BlueCare/TennCare Select, CHOICES & Behavioral Health claims, billing, benefits & benefit limits. Excluding Authorization Change Requests, Plan of Care changes, or Direct Questions for CHOICES Care Coordinator 1-800-468-9736 Provider questions to include BlueCare/TennCare Select, CHOICES & Behavioral Health Claims, Billing Guidelines, claim status, benefit limits, patient liability. Excluding Authorization Correction Requests, Plan of Care Change Request or Direct questions for CHOICES Care Coordinator 1-800-263-5479 Member questions to include questions to include BlueCare/TennCare Select, CHOICES & Behavioral Health claims, billing, benefits & benefit limits. Excluding Authorization Change Requests, Plan of Care changes, or Direct Questions for CHOICES Care Coordinator 1-800-276-1978 Provider questions to include BlueCare/TennCare Select, CHOICES & Behavioral Health Claims, Billing Guidelines, claim status, benefit limits, patient liability. Excluding Authorization Correction Requests, Plan of Care Change Request or Direct questions for CHOICES Care Coordinator 1-866-502-0056 Customer Service Representatives are set up to answer incoming questions fro Long Term Care Providers related to eligibility, benefits, claims and billing guidelines for BlueCare Choices. Fax # Website: https://tnm.rxportal.sxc.com/rxclaim/portal/pre Login Pharmacy Nurseline Family Assistance Service Center (FASC) 1-866-434-5520 1-866-434-5524 Medication questions, RX authorization questions, Injection medications Prior Authorization for Medications 1-800-262-2873 VSHP members may speak to a Registered Nurse (RN) anytime – 24-hours-aday, 7-days-a-week - with 24/7 Nurseline English 1-866-311-4287 Applying for Tenncare, Report Change of Address, Phone #, Date of Death of Spanish 1-866-311-4290 TTY Member, Request MCO Change Filing Appeal about getting or keeping or TDD 1-800-772-7647 TennCare Letter of Creditable Coverage Email or Web Address/Physical Address 1-866-434-5523 Premium Contact Information: TennCare Premiums P.O. Box 305133-37211 Nashville, TN 37211 615-253-7049 CHOICES Directory of Telephone Numbers, Addresses, Email, Web Contacts Agency Name Choices Direct Lines Rings to Nashville/Green Hills Office Phone # Explanation for Use Fax # Email or Web Address/Physical Address or IVR Options BlueCare CHOICES Member Care Coordination 1-888-747-8955 Line CHOICES Member Care Coordinators (HCCs) Coordinate ALL Medicaid services for the elderly and disabled – physical, behavioral and long-term care. Note: This line is also for general CHOICES Inquiries, authorization status, authorization change requests and plan of care information for the BlueCare CHOICES Member. All claim status & claim billing questions should go through the BlueCare Member Service Line @ 1-800-468-9698 or BlueCare Provider Service Line @ 1-800-468-9736 (615) 386-8589 providerauthissues_GM@bcbst.com TennCare Select CHOICES Member Care Coordination Line Choices Member Care Coordinators (HCCs) Coordinates ALL Medicaid services for the elderly and disabled – physical, behavioral and long-term care. Note: This line is also for general CHOICES Inquiries, authorization status, authorization change requests and plan of care information for the BlueCare CHOICES Member. (615) 386-8589 providerauthissues_GM@bcbst.com 1-800-782-2433 When a member and their caregivers have problems or complaints about care or a service Provider they should report this to the assigned Care Coordinator at th phone number or the member may also call the Tennessee Area Agency on Aging and Disability Office (AAAD) at 1-866-836-6678 to register his or her complaint. The member has 30 days after a denial is received to file an appeal. Usually, the appeal is decided within 90 days after it is filed. If the member can’t wait 90 days for health care or medicine and it is an emergency, the appeal can be decided sooner—usually within 31 days (but sometimes up to 45 days). This can be processed faster if the member has his or her doctor sign off on the appeal statement before it is sent in. CHOICES Member Complaint/Grievance1st Step CHOICES Member Complaint/Grievance2nd Step if Step 1 doesn't resolve the issue call (TennCare Solutions Unit) 1-800-782-2433 (Nashville Office) 1-800-878-3792 The member or caregiver can contact the TennCare Solutions Unit if their issue is not resolved by the Care Coordinator during the first step or the complaint is against the Care Coordinator, and the Care Coordinator's Supervisor or Manager is not able to rectify the issue by assigning another Care Coordinator. Note: The member has 30 days after a denial is received to file an appeal. Usually, the appeal is decided within 90 days after it is filed. If the member can’t wait 90 days for health care or medicine and it is an emergency, the appeal can be decided sooner—usually within 31 days (but sometimes up to 45 days). This can be processed faster if the member has his or her doctor sign off on the appeal statement before it is sent in. CHOICES Directory of Telephone Numbers, Addresses, Email, Web Contacts Agency Name CHOICES Member Complaints, Grievance Phone # 1-800-468-9698 Explanation for Use Fax # (615) 386-8589 1-888-747-8955 Critical Incidents should be reported immediately to the Care Coordination Line. Critical Incidents include but are not limited to the following: Unexpected death of CHOICES member, suspected mental or physical abuse, theft for financial exploitation, severe injury, medication error, sexual abuse or suspected sexual abuse, abuse and neglect, or suspected abuse and neglect. Abuse & Neglect Cases for Adults 1-888-277-8366 Suspected abuse, neglect and exploitation of members who are adults must be immediately reported to the Care Coordination Line with 24 hours of the incident, as well as to this number Abuse & Neglect Cases for Children 1-877-237-0004 or 1-877-542-2873 Suspected abuse, neglect and exploitation of members who are adults must be immediately reported to the Care Coordination Line with 24 hours of the incident as well as one of these contacts Critical Incident Reporting Process Phone # For people who do not already have Medicaid, this is the number they may call to speak with someone who can tell them more about CHOICES. Note: If the caller is not already enrolled with current TennCare benefits, he or she will have to go through the application process to see if benefits can be approved. Area Agencies on Aging and Disability Area Agencies on Aging and Disability (AAAD)/Single Point of Entry (SPOE) 1-866-836-6678 This number rings to a AAAD in the member's region Aging Commission of the Mid-South (901) 324-6333 AAAD contact for Memphis, TN (901) 327-7755 First TN Dev. District (423) 928-0224 AAAD contact for Johnson City, TN (423) 928-5209 East TN Human Resource Agency (865) 691-2551 ext. 216 AAAD contact for Knoxville, TN (865) 531-7216 Southeast TN Dev. District (423) 266-5781 AAAD contact for Chattanooga, TN (423) 424-4225 Upper Cumberland Dev. Distric (931) 432-4111 AAAD contact for Cookeville, TN (931) 432-6010 Greater Nashville Regional Counc (615) 862-8828 AAAD contact for Nashville, TN (615) 862-8840 South Central TN Dev. District (931) 381-2040 AAAD contact for Columbia, TN (931) 381-2053 Northwest Dev. District (731) 587-4213 AAAD contact for Martin, TN (731) 588-5833 Southwest TN Dev. District (731) 668-7112 AAAD contact for Jackson, TN (731) 668-6438 Email or Web Address/Physical Address CHOICES Directory of Telephone Numbers, Addresses, Email, Web Contacts Agency Name 1-800-357-0395 Explanation for Use Question applications or to check status of credentialing, add a new office location to their contract Provider Network Service Department 1-800-924-7141 If an in-state provider is inquiring about the status of a recently submitted BlueCare/TennCareSelect contract, they should be referred to the Provider Network Service Department . Buffy Bass-Douglas Nathan Key Sheldon House (423) 535-3856 (615) 760-8707 (901) 544-2170 CHOICES Network Representative for East Grand Region CHOICES Network Representative for Middle Grand Region CHOICES Network Representative for West Grand Region Credentialing Contact Information Phone # Dial-Up Modem Hyper Terminal Connection Email or Web Address/Physical Address Buffy_Bass_Douglas@bcbst.com Nathan_Key@bcbst.com Sheldon_House@bcbst.com Electronic Visit Verification System is required to be used for CHOICES Home and Community Based Service Provider Billing for Adult Day Care, Attendant Care, Companion Care, Home Delivered Meals, Home Maker Services, In-Home Respite and Personal Care Electronic Visit Verification System (EVV) Sandata Fax # 1-877-526-0516 Provides technical support for HCBS providers. When providers use the EVV System, all claims will transmit to Sandata via the EVV System. Once claim information is collected from providers, Sandata will submit all EVV providers’ claims to VSHP via the secure File Transfer Protocol (FTP) connection. Note: Providers will need a dial-up modem and or hyper terminal connection if they would like to receive Proof of Timely Filing and Reject Reason Reports. Note: If a claim is rejected due to an error on the provider or Sandata's part, the provider will need to obtain the explanation from the E-business Service Center and call Sandata to have the problem with the claim corrected and then Sandata will have to resubmit the claim. (423) 535-5717 Providers will need a dial-up modem and if they would like to receive Proof of Timely Filing and Reject Reason Reports. The phone line does not have to be a dedicated line. www.bcbst.com/providers/ecomm/technicalinformation.shtml (423) 535-5717 Providers will need a dial-up modem and or hyper terminal connection if they would like to receive Proof of Timely Filing and Reject Reason Reports HyperTerminal is a tool that lets you connect to other computers, Internet telnet sites, bulletin board services, online services, and host computers, using either your modem or a null modem cable. Email: ecomm_techsupport@bcbst.com CHOICES Directory of Telephone Numbers, Addresses, Email, Web Contacts Agency Name Phone # Explanation for Use Fax # Email or Web Address/Physical Address 1-800-924-7141 E-Business Solutions can assist providers with electronic claims issues to confirm if electronic claims transmission is completed correctly, resolve issues with the claims transmission and provide claims number and explanation for rejected claims. E-Business Solutions also works with the Web Portal Email: ecomm_contracts@bcbst.com or Configurations Email: ecomm_sysconfig@bcbst.com Web: www.bcbst.com/providers/ecomm/ 1-800-924-7141 E-Business Solutions can handle the contracting for providers who want to be set up to file claims electronically. They can answer enrollment status questions for the electronic process, as well as answer claim submission questions. Email: ecomm_contracts@bcbst.com or Configurations Email: ecomm_sysconfig@bcbst.com BlueAccess Providers may register for BlueAccess on the BCBST website. BlueAccess enables providers to view information in a secure, online environment, just as it appears right now in the customer service computer system, along with viewing remittance advices. Web: www.bcbst.com Electronic Clearing House The method for HCBS providers to use an Electronic Clearing House to file claims for the following services: Assisted Care Living Facilities, Assistive Technology, Critical Adult Care Homes, Minor Home Modification, Nursing Facilities, Person Emergency Response Systems (PERS), and Pest Control E-Business Solutions Provider Contracting Paper Claims BlueCare Claims Service Center can be used to submit paper claims Provider Administration Manuals These manuals contain the provider contracting information for CHOICES Providers along with specific billing guidelines BlueCare Claims Service Center 1 Cameron Hill Cr, Ste 0002, Chattanooga, TN 37402-0002 Web: www.vshptn.com or www.bcbst.com