Comparison of IV Fluids
advertisement

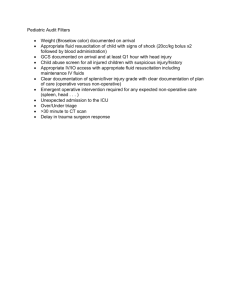
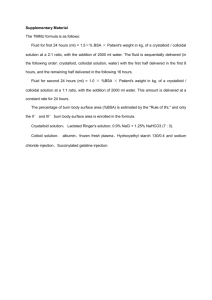
PL Detail-Document #290212 −This PL Detail-Document gives subscribers additional insight related to the Recommendations published in− PHARMACIST’S LETTER / PRESCRIBER’S LETTER February 2013 Comparison of IV Fluids The need for fluid resuscitation, or replacing blood volume with IV fluids to maintain adequate organ perfusion, is not uncommon in the hospital setting. Options include colloids such as albumin or hydroxyethyl starch (HES) and crystalloids such as normal saline (NS) or lactated Ringer’s (LR) solution. New studies such as SAFE (Saline versus Albumin Fluid Evaluation) and updated meta-analyses continue to shed light on the best choices. One often cited advantage of using colloids over crystalloids is that less volume is needed to produce the desired effect. For example, guidelines have given a 1:4 volume ratio. However, data have not consistently supported this number, with ratios often being closer to 1:1 or 1:2.1-4 Safety and cost are two major arguments against the use of colloids, along with the lack of evidence for benefit over crystalloids in many patient populations. Studies comparing IV fluids for fluid resuscitation that are underway include Albumin in Severe Sepsis (ALBIOS), Lactated Ringer Versus Albumin in Early Sepsis Therapy (RASP), and Efficacy and Safety of Colloids Versus Crystalloids for Fluid Resuscitation in Critically Ill Patients (CRISTAL). The following chart lists colloid and crystalloid products, alone with advantages, disadvantages, and evidence for use. Advantages Disadvantages Albumin 5%, 25% Fluid • Low risk for adverse reactions5 • May modulate inflammation5,6 • Colloids may provide greater intravascular volume expansion than equal volumes of crystalloids5 • Potential for allergic reactions6 • Potential for transmission of infection5 • Hyperoncotic albumin may cause kidney damage5,7 • More expensive than HES or crystalloids Dextran 40 (LMD) 10% in D5W or NS Gentran-40 Dextran 70 6% in D5W or NS Gentran-70 • Colloids may provide greater intravascular volume expansion than equal volumes of crystalloids5 • High risk for adverse reactions5 • Potential for allergic or anaphylactoid reactions5,7 • Impairs hemostasis (sometimes used as anticoagulant)4,5,7 • May cause kidney damage7 Comments • Natural colloid6 • Duration of action 12 to 24 hours5 • 25% albumin is hyperoncotic; 5% albumin is iso-oncotic5,7 • No mortality benefit over NS for fluid resuscitation in hypovolemia (SAFE)5,6,8 • A slight but nonstatistically significant benefit for albumin shown in patients with sepsis (SAFE).5 Recommended in severe sepsis and septic shock for patients who require large amounts of crystalloid.8 • May be beneficial in patients with low albumin5 • Iso-oncotic albumin may improve mortality in cardiac surgery patients2,5 • Avoid in brain trauma. May increase mortality compared with NS (SAFE).5 • Artificial colloid • Duration of action one to two hours (dextran 40)5 • Use for fluid resuscitation has fallen out of favor due to high risk of adverse reactions4 • LMD = low-molecular-weight dextran More. . . Copyright © 2013 by Therapeutic Research Center 3120 W. March Lane, Stockton, CA 95219 ~ Phone: 209-472-2240 ~ Fax: 209-472-2249 www.PharmacistsLetter.com ~ www.PrescribersLetter.com ~ www.PharmacyTechniciansLetter.com (PL Detail-Document #290212: Page 2 of 4) Fluid Advantages Disadvantages Comments 5% Dextrose (D5W) • NA • Pediatric deaths reported from hyponatremia resulting from infusion of excess volume of D5W9 • Crystalloid • Hypotonic. Isotonic in the bag, but dextrose gets metabolized almost immediately in the lining of the blood vessels, leaving free water.10 • Hypotonic solutions such as D5W are useful for patients with dehydration and adequate circulatory volume7,11 Hydroxyethyl starch (HES) • May modulate inflammation5,6 • Colloids may provide greater intravascular volume expansion than equal volumes of crystalloids5 • Potential for anaphylactoid reactions5 • May accumulate in tissue and cause prolonged itching4-7 • May impair platelet function6 • May cause kidney damage5-7 • May cause increases in serum amylase7 • More expensive than crystalloids • Synthetic colloid • Duration of action eight to 36 hours5 • 6% HES is hyperoncotic5 • Larger molecular weight than albumin2 • Adverse effects are dose-related12 • Hespan and Hextend are hetastarches. Voluven is a tetrastarch with a lower molecular weight. This is thought to reduce the risk for adverse effects; however, it has not been proven.3,4,6,12,13 • May increase mortality, need for dialysis, and bleeding compared with LR and other fluids in patients with severe sepsis (6S, etc).4,13 Not recommended for fluid resuscitation in severe sepsis and septic shock.8 • No benefit shown in critically ill patients (e.g., burns, post-op, trauma) compared with crystalloids1 • Low risk for adverse reactions5 • Crystalloids freely distribute across the vascular barrier6 • Risk for respiratory acidosis due to accumulated CO214 • Risk for hyperkalemia (has 4 mEq/L potassium)5,7 • Impaired metabolism of lactate to bicarbonate in patients with severe liver disease10 • Crystalloid • Duration of action one to four hours5 • Slightly hypotonic5 • Considered equally effective as normal saline11 • May be preferred for hemorrhagic shock because large volumes will not cause hyperchloremic metabolic acidosis, as with NS7,11 • Because of slight hypotonicity, might increase risk of brain swelling in brain trauma13,15 6% HES 200/0.5 in NS Hespan (U.S.), 6% HES 200/0.5 in lactated electrolyte solution Hextend, 6% HES 130/0.4 in NS Voluven Lactated Ringer’s (LR) More. . . Copyright © 2013 by Therapeutic Research Center 3120 W. March Lane, Stockton, CA 95219 ~ Phone: 209-472-2240 ~ Fax: 209-472-2249 www.PharmacistsLetter.com ~ www.PrescribersLetter.com ~ www.PharmacyTechniciansLetter.com (PL Detail-Document #290212: Page 3 of 4) Fluid 0.9% NaCl Normal saline (NS) Advantages • Low risk for adverse reactions5 Disadvantages • Crystalloids freely distribute across the vascular barrier6 • Risk of hypernatremia and hyperchloremic metabolic acidosis7,14 Comments • Crystalloid • Duration of action one to four hours5 • Isotonic • No mortality benefit of 4% albumin over NS for fluid replacement in hypovolemia (SAFE)5,6,8 • Considered equally effective as LR. Preferred over LR for patients with brain trauma.11 • No evidence that hypertonic saline (e.g., 3%) is better than NS for fluid resuscitation7,11 • Hypotonic solutions such as D5W/ 1/2 NS are useful for patients with dehydration and adequate circulatory volume7,11 Users of this PL Detail-Document are cautioned to use their own professional judgment and consult any other necessary or appropriate sources prior to making clinical judgments based on the content of this document. Our editors have researched the information with input from experts, government agencies, and national organizations. Information and internet links in this article were current as of the date of publication. More. . . Copyright © 2013 by Therapeutic Research Center 3120 W. March Lane, Stockton, CA 95219 ~ Phone: 209-472-2240 ~ Fax: 209-472-2249 www.PharmacistsLetter.com ~ www.PrescribersLetter.com ~ www.PharmacyTechniciansLetter.com (PL Detail-Document #290212: Page 4 of 4) Project Leader in preparation of this PL DetailDocument: Stacy A. Hester, R.Ph., BCPS, Assistant Editor 9. References 1. 2. 3. 4. 5. 6. 7. 8. Perel P, Roberts I. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev 2012;(6):CD000567. Han J, Martin GS. Rational or rationalized choices in fluid resuscitation? Crit Care 2010;14:1006. Hartog CS, Kohl M, Reinhart K. A systematic review of third-generation hydroxyethyl starch (HES 130/0.4) in resuscitation: safety not adequately addressed. Anesth Analg 2011;112:635-45. Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 2012;367:124-34. Kruer RM, Ensor CR. Colloids in the intensive care unit. Am J Health Syst Pharm 2012;69:1635-42. Strunden MS, Heckel K, Goetz AE, Reuter DA. Perioperative fluid and volume management: physiological basis, tools and strategies. Ann Intensive Care 2011;1:2. Talbert RL, DiPiro JT, Matzke GR, et al. Hypovolemic shock. In: Talbert RL, DiPiro JT, Matzke GR, et al, Eds. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. New York: McGraw-Hill;2011. Surviving Sepsis Campaign. Hemodynamic support and adjunctive therapy. 10. 11. 12. 13. 14. 15. http://survivingsepsis.org/Guidelines/Pages/default.a spx. (Accessed January 15, 2013). Plain D5W or hypotonic saline solution post-op could result in acute hyponatremia and death in healthy children. ISMP Medication Safety Alert! August 13, 2009. http://www.ismp.org/newsletters/acutecare/articles/2 0090813.asp. (Accessed January 15, 2013). Rosenthal K. Tonicity and IV fluids. Resource Nurse. http://www.resourcenurse.com/feature_tonicity_fluids .html. (Accessed January 15, 2013). Intravenous fluid resuscitation. The Merck Manual. July 2012. http://www.merckmanuals.com/profes sional/critical_care_medicine/shock_and_fluid_resus citation/intravenous_fluid_resuscitation.html. (Accessed January 15, 2013). Traynor K. Trauma experts urge cautious use of i.v. fluids. Am J Health Syst Pharm 2012;69:1846,1848. Vincent JL, Gottin L. Type of fluid in severe sepsis and septic shock. Minerva Anestesiol 2011;77:11906. The great fluid debate revisited. Medscape Critical Care (2008). http://www.medscape.org/viewarticle /572584. (Accessed January 15, 2013). Ropper AH. Hyperosmolar therapy for raised intracranial pressure. N Engl J Med 2012;367:74652. Cite this document as follows: PL Detail-Document, Comparison of IV Fluids. Pharmacist’s Letter/Prescriber’s Letter. February 2013. Evidence and Recommendations You Can Trust… 3120 West March Lane, Stockton, CA 95219 ~ TEL (209) 472-2240 ~ FAX (209) 472-2249 Copyright © 2013 by Therapeutic Research Center Subscribers to the Letter can get PL Detail-Documents, like this one, on any topic covered in any issue by going to www.PharmacistsLetter.com, www.PrescribersLetter.com, or www.PharmacyTechniciansLetter.com