Breech Birth case studies
advertisement

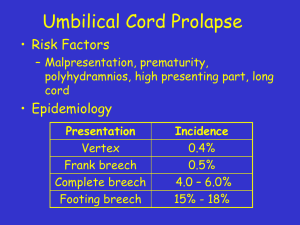
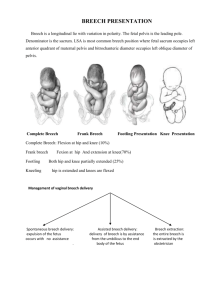
By Joy Horner RM. RGN. Dip H.Ed. From breeches meaning trousers. So breech presentation can be feet, knees or bottom-first entry into the world. 25% at 28 weeks weeks 3-4% at term We miss about 30% of breech presentations on palpation. So we need the skills to attend any woman with a breech presenting baby. Normal breech birth “A breech presentation is normal, it is just not typical. This is really important to remember: breech is not an abnormality. And a normal labour and a spontaneous birth are not excluded just because the presenting part is breech (although not all breeches can or should be born vaginally). Even though many babies presenting by the breech can and should be born normally, caesarean section is currently the most common mode of delivery (irrespective of clinical indicators). However, the fact that caesarian section has become the accepted practice for breech births does not mean that it is the only acceptable option”. Cord prolapse Head entrapment more with preterm births Cord compression Injury to brain or skull if sudden decompression – more in pre term birth Injury to skull/ spinal cord due to positioning during delivery of the after coming head Damage to internal organs Other contraindications to vaginal birth (e.g. Placenta praevia, compromised fetal condition). clinically inadequate pelvis. footling or kneeling breech presentation. large baby (larger than 3800 g). growth-restricted baby (smaller than 2000g). hyperextended fetal neck in labour. lack of presence of a clinician trained in vaginal breech delivery. previous caesarean section. (RCOG, 2006) Spontaneous onset anytime after about the 37th week. No augmentation if labour is slow or there is poor progress - caesarean section. Mother encouraged to assume positions of choice during the first stage. Fetal heart listened to frequently with a Pinard stethoscope or a hand held Doppler Sonic aid. Food and drink encouraged, but remembering that women in strong progressing labour rarely want to eat. Membranes not ruptured artificially. Vaginal examinations restricted to avoid accidental rupturing of the membranes. If, and when spontaneous rupture occurs conduct a vaginal examination as soon as possible. Second stage by maternal propulsion and spontaneous expulsive efforts guided by the attendant if judged appropriate. Mother encouraged to be in an all-fours position. No routine episiotomy. Third stage without chemical or mechanical assistance, usually managed according to woman's wishes. (Cronk 1988) Birth Joy Ltd 2009 © Birth Joy Ltd 2009 © Birth Joy Ltd 2009 © Birth Joy Ltd 2009 © Birth Joy Ltd 2009 © Birth joy Ltd 2009 © Birth Joy Ltd 2009 © Birth Joy Ltd 2009 © Birth Joy Ltd 2009 © Birth joy Ltd 2009 © Birth Joy Ltd 2009 © Birth Joy Ltd 2009 Birth Joy Ltd 2009 © Birth Joy Ltd 2008 © Since the Term Breech Trial (TBT. Also known as the Hannah trial) in 2000 caesarean section has been commonly recommended for women carrying a breech presenting baby. It appeared to indicate caesarean birth was safer for babies. A follow up study 4 years later found that at 2 years of age there were almost identical risks of death or neurodevelopmental delay in children. PREMODA study 2006 Goffinet et al produced a study 4 times larger than the term breech trial. It showed no difference in perinatal mortality or serious neonatal morbidity between planned trial of labour and planned caesarean groups. If a breech presentation is diagnosed in pregnancy in the UK, ECV is offered. If baby does not turn then caesarean, or trial of vaginal breech “delivery” are given as options. Some women do not wish their birth to be controlled and trust the power of their own body to be able to give birth. Some breeches are undiagnosed until labour. Unfortunately, since the publication of the flawed Term Breech Trial, midwives and doctors have had less chance to attend spontaneous breech births, so clinical skills have been lost. Those midwives who’ve been practicing for many years before the TBT have learnt the skills to assist women birth their breech presenting babies. Such a midwife is my mentor, Mary Cronk. The Term Breech Trial set out to test the safety of two treatments: ‘caesarean section’ and ‘vaginal breech birth.’ The researchers in the Term Breech Trial used the word ‘vaginal breech birth’ but the concept that they have of what that phrase is very different to the concept that midwives and some obstetricians, particularly Northern European ones, hold for the same phrase. The safety of spontaneous vaginal breech birth was not tested by the Term Breech Trial and therefore, the results of the trial cannot be applied to women having spontaneous vaginal breech births attended by skilled and experienced maternity care providers. (Fahey, Katherine 2011) Unbiased information sharing Time to discuss options. Explain and offer ECV Place of breech birth needs access to theatres Skilled staff availability? Maternal choice not coersion. MATERNAL Abnormality of uterus, septum/fibroids. Oligo/polyhydramnios Placenta previa. Family history Primip/strong abdominal muscles. FETAL Prematurity. Multiple pregnancy. Hydrocephalus, spina bifeda. Brittle bones, downs syndrome. Tight/short cord. 60-70% of term breeches Risk of cord prolapse 0.5% (cephalic 0.4%) Cord can get compressed between legs an abdomen. More common in primips with strong muscles (Frye 2004) 10% of all breeches Cord prolapse risk 4-6% (Frye 2004). A recent observational study of non-frank breech presentations found a high rate of cord prolapse (5.6%) but no increase in abnormal labour nor impaired perinatal outcome. (RCOG). 29% of all breeches with 1020% being footlings. Kneeling rarest at 5% of term breeches. More common with pre term birth. Baby has more manoeuvring ability as body not splinted by legs. Risk of cord prolapse 15-18% if footling, more commonly in pre-term or small babies. Less risk of cord compression if cord prolapse. Early rupture of membranes more likely.(Frye 2004). ECV Moxabustion Accupuncture Breech tilt positions rebozo Hypnosis Handstands in pool Cold on fundus Shining light/playing music near symphysis pubis. It’s important women choose their own birthing position to best birth their babies. Most women naturally adopt a kneeling or on all fours position. Maybe to feel grounded. “The 28 percent increase in the pelvic outlet – 1cm in the transverse diameter and 2cm in the anterior-posterior diameter of active birthing is greater than that which is normally achieved by symphysiotomy, which, primarily, increases the transverse diameters by 1cm.” (Banks, 2007) “I find that this is the best position for mother, baby and midwife. Gravity is doing what many of the old textbooks tell the operator to do; lifting the baby up by the heels, over the mothers pubis when she is in the lithotomy position, on hands and knees it happens by gravity.” (Cronk 2012) Less need for manoeuvres as illustrated by Frank Louwen’s work. Therefore less potential to harm the breech baby. Other upright positions? Ve’s? Continual or intermittant monitoring? Palpation/descent of presenting part Observing pattern of labour Maternal observations Documentation Monitor fetal heart frequently Monitor descent of presenting part. Progress with every contraction. If no progress prepare to assist. Observe colour and tone of baby and fullness of cord. Document times of presenting part visible, rumping, legs, arms and head born. Document any manouvers needed and resussitation. Birth Joy Ltd 2007 © Birth Joy Ltd 2007 © Breech babies often suffer a short period of cord compression during the second stage and have lower Apgar scores. Be prepared to resuscitate with cord intact if possible. Explain to parents what is happening and why. WOMAN A Primip Age 27 Healthy BMI Born breech herself Baby extended breech Failed ECV Planned homebirth WOMAN B Primip Age 25 Healthy BMI Baby extended breech No ECV Planned homebirth WOMAN A Spontaneous onset at term SROM 1st stage good progress No pain relief Intermittent monitoring, no decelerations. 2nd stage fast after presenting part visible. WOMAN B Spontaneous onset at term SROM 1st stage good progress No pain relief Intermittent monitoring, no decelerations 2nd stage slow progress after presenting part visible. WOMAN A No pushing Footling presentation Proceeded rapidly No manouvers needed Asked to push for head Stargazer. 5 rescue breaths apgars WOMAN B Spontaneous pushing Baby birthed bottom and legs slowly Cord compressed between legs and body. Arms delivered lovesetts Head deflexed, caught on sacral promontory, unable to reach for mauricaeucronk. Other manoeuvres The Mauriceau-Smellie-Veit manoeuvre should be considered, if necessary, displacing the head upwards and rotating to the oblique diameter to facilitate engagement. Easily performed on all fours Suprapubic pressure by an assistant can be used to assist flexion of the head (mother in supine position) WOMAN AND BABY A 2nd degree tear. Bloodloss. Feeding problems. Baby eventually fully breastfed. No residual problems WOMAN AND BABY B Episiotomy. Baby transferred for cooling. Home fully breastfed day 10. No residual problems. At this point there is compression of the umbilical cord between head and maternal pelvis. Head usually in flexed position and flexes more as baby lifts it’s legs if in good condition. Monitor colour and tone of baby and fullness of cord, and be ready to control speed of birth of head. Perform manoeuvres immediately - if baby in poor condition. Birth Joy Ltd 2010 © 1. 2. 3. 4. 5. 6. If baby in good condition, good tone, full cord heart rate >100 progress should resume with baby’s leg flexion to flex head. If baby in poor condition, colour pale, heart rate <100, limp DO NOT REMAIN HANDS OFF! Attempt to flex head with mother on all fours (Mauricaeu Cronk manouver, ask mother to push Being upright tightens abdominal muscles and aids flexion. Frye 2004 Lay mother down to manually flex head with suprapubic pressure. (RCOG 2006) Lift torso and rotate to bring head into the transverse diameter if stuck at the brim (explained to me by Gail Tully 2012) Positions which open the pelvis may be useful eg. Supported squat. DO NOT APPLY TRACTION. Shawn Walker breech birth network In the seventh Annual Report of the Confidential Enquiry into Stillbirth and Deaths in Infancy, the most avoidable factor in causing breech stillbirths and death among breech babies was suboptimal care in labour. In cases where the cardiotocograph was available for review, there was clinical evidence of hypoxia in all but one case before delivery and delays in staff response to fetal compromise occurred in nearly 75% of cases. These delays ranged from 30 minutes to 10 hours. Consultants were informed in only 50% of these cases before delivery. Clinical inexperience at the time of delivery exacerbated the risk for an already hypoxic baby in some cases. Trauma was the sole cause of death in only one case. Any woman who gives birth vaginally with breech presentation should be cared for by an attendant with suitable experience. Good communication between practitioners is important. In recent years in the UK, there has been a reduced number of vaginal breech deliveries managed by an increased number of trainees. Alternative methods of training need to be introduced (such as videos, models and scenario teaching). Simulation training has been shown to improve performance in the management of a simulated vaginal breech delivery (CNST criterion 5.2.1). A video-recorded teaching aid on vaginal breech delivery and symphysiotomy is available in the World Health Organization Reproductive Health Library (available from rhl@who.int; www.rhlibrary.com). (RCOG Guideline No. 20b) The most important thing to remember in spontaneous breech birth is that the labour should progress well and baby’s condition should be monitored frequently. Skilled, calm confident birth attendants are needed. The midwife (and doctor if present) should practice watchful, hands-off waiting, unless help is clearly required. This may be due to slow progress (eg. no advance with the next contraction), or poor tone in the baby, which prevents him from helping himself to be born, indicating the need to achieve a swift delivery. Hands off the breech does not mean fail to help if help is needed! “Remember women’s bodies don’t go wrong. Sometimes some labours need some help” Mary Cronk 2012 Don't push a breech through the pelvis with oxytocic drugs. No inductions, no augmentations Don't pull a breech baby down through the pelvis - No breech extractions. Consider whether vaginal examination is necessary. If labour isn't progressing in the first stage consider the need for Caesarean section. Keep your hands off a breech that is birthing spontaneously - sit on them if necessary! Breech babies should birth by maternal effort NOT traction. If any delay in the second stage consider manoeuvres to facilitate delivery, or caesarean. Be ready to resuscitate baby if needed. Practice breech mechanisms so you can help if needed. Volunteering to support women planning vaginal breech birth. Teaching other midwives and doulas how to support women in breech birth choices. Write articles about normal breech birth. Join the Breech Birth Network at www.breechbirth.org.uk Possible NHS breech clinics offering women informed choice, scans and ECV. ACOG 2010. Mode of Term Singleton Breech Delivery ACOG committee opinion Number 340, July 2006 Reaffirmed 2010 (Replaces No. 265, December 2001). Banks M, 2001 Breech birth beyond the term breech trial www.birthspirit.co.nz Cronk M, 1998. Hands off the breech. Practicing Midwife 1 (6), 13-15. Evans J, 2005. Breech Birth – What are my options? AIMS Press. Evans J, February 2012. Understanding physiological breech birth. Essentially MIDIRS, Volume 3, Number 2. Evans J, March 2012. The Last Piece in the Breech Birth Jigsaw? Essentially MIDIRS, Volume 3, Number 3. Fahey. K Do the findings of the Term Breech Trial apply to spontaneous breech birth? Women and Birth Volume 24, Issue 1 , Pages 1-2, March 2011. Frye A, 2004. Holistic Midwifery, Vol. II: Care of the mother and baby from the onset of labor through the first hours after birth. Portland: Labrys Press. Hannah ME, HannahWJ 2000 planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Lancet, 356 (9239):1375-1383. Kotaska A, et al, 2009. Vaginal delivery of breech presentation. SOGC Clinical Practice Guideline No. 226. J Obstet Gynaecol Can 31(6), 557–66. Royal College of Obstetricians and Gynaecologists, 2006. The Management of Breech Presentation, Green-top Guideline No. 20b. London: RCOG. Volume 15 number 3 march 2012. Walker S 2012. Breech birth: an unusual Normal. The practicing midwife, volume 15, number 3. On line resources http://www.aims.org.uk/Journal/Vol10No3/handOffbreech.htm accessed 09/10/12 http://www.breechbirth.org.uk/ accessed 3/11/12 http://www.jpaget.nhs.uk/section.php?id=22331 accessed 01/10/12 http://www.rcmnormalbirth.org.uk/stories/do-as-you-would-be-done-by/normal-breech-birth accessed 09/10/12