A Cesarean Hysterectomy for Invading Placenta Percreta
advertisement
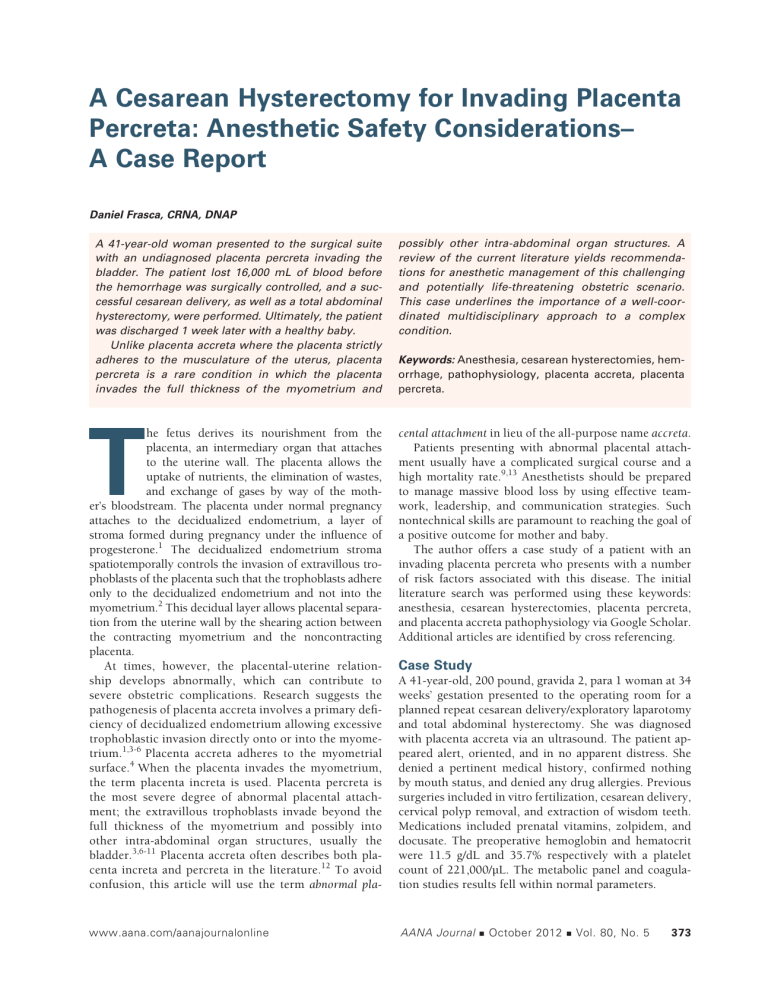
A Cesarean Hysterectomy for Invading Placenta Percreta: Anesthetic Safety Considerations– A Case Report Daniel Frasca, CRNA, DNAP A 41-year-old woman presented to the surgical suite with an undiagnosed placenta percreta invading the bladder. The patient lost 16,000 mL of blood before the hemorrhage was surgically controlled, and a successful cesarean delivery, as well as a total abdominal hysterectomy, were performed. Ultimately, the patient was discharged 1 week later with a healthy baby. Unlike placenta accreta where the placenta strictly adheres to the musculature of the uterus, placenta percreta is a rare condition in which the placenta invades the full thickness of the myometrium and T possibly other intra-abdominal organ structures. A review of the current literature yields recommendations for anesthetic management of this challenging and potentially life-threatening obstetric scenario. This case underlines the importance of a well-coordinated multidisciplinary approach to a complex condition. Keywords: Anesthesia, cesarean hysterectomies, hemorrhage, pathophysiology, placenta accreta, placenta percreta. he fetus derives its nourishment from the placenta, an intermediary organ that attaches to the uterine wall. The placenta allows the uptake of nutrients, the elimination of wastes, and exchange of gases by way of the mother’s bloodstream. The placenta under normal pregnancy attaches to the decidualized endometrium, a layer of stroma formed during pregnancy under the influence of progesterone.1 The decidualized endometrium stroma spatiotemporally controls the invasion of extravillous trophoblasts of the placenta such that the trophoblasts adhere only to the decidualized endometrium and not into the myometrium.2 This decidual layer allows placental separation from the uterine wall by the shearing action between the contracting myometrium and the noncontracting placenta. At times, however, the placental-uterine relationship develops abnormally, which can contribute to severe obstetric complications. Research suggests the pathogenesis of placenta accreta involves a primary deficiency of decidualized endometrium allowing excessive trophoblastic invasion directly onto or into the myometrium.1,3-6 Placenta accreta adheres to the myometrial surface.4 When the placenta invades the myometrium, the term placenta increta is used. Placenta percreta is the most severe degree of abnormal placental attachment; the extravillous trophoblasts invade beyond the full thickness of the myometrium and possibly into other intra-abdominal organ structures, usually the bladder.3,6-11 Placenta accreta often describes both placenta increta and percreta in the literature.12 To avoid confusion, this article will use the term abnormal pla- cental attachment in lieu of the all-purpose name accreta. Patients presenting with abnormal placental attachment usually have a complicated surgical course and a high mortality rate.9,13 Anesthetists should be prepared to manage massive blood loss by using effective teamwork, leadership, and communication strategies. Such nontechnical skills are paramount to reaching the goal of a positive outcome for mother and baby. The author offers a case study of a patient with an invading placenta percreta who presents with a number of risk factors associated with this disease. The initial literature search was performed using these keywords: anesthesia, cesarean hysterectomies, placenta percreta, and placenta accreta pathophysiology via Google Scholar. Additional articles are identified by cross referencing. www.aana.com/aanajournalonline AANA Journal Case Study A 41-year-old, 200 pound, gravida 2, para 1 woman at 34 weeks’ gestation presented to the operating room for a planned repeat cesarean delivery/exploratory laparotomy and total abdominal hysterectomy. She was diagnosed with placenta accreta via an ultrasound. The patient appeared alert, oriented, and in no apparent distress. She denied a pertinent medical history, confirmed nothing by mouth status, and denied any drug allergies. Previous surgeries included in vitro fertilization, cesarean delivery, cervical polyp removal, and extraction of wisdom teeth. Medications included prenatal vitamins, zolpidem, and docusate. The preoperative hemoglobin and hematocrit were 11.5 g/dL and 35.7% respectively with a platelet count of 221,000/µL. The metabolic panel and coagulation studies results fell within normal parameters. October 2012 Vol. 80, No. 5 373 The obstetrician admitted the patient at 32 weeks’ gestation with oligohydramnios and a tentative diagnosis of placenta accreta. Ultrasound suggested no other organ involvement, and there were no signs of hematuria or lower urinary tract symptoms. Bed rest had been prescribed. At 34.3 weeks’ gestation, the patient experienced irregular uterine contractions and bright red vaginal bleeding. The patient, originally scheduled for delivery the next day, immediately proceeded to surgery. The anesthesia team consisted of 2 anesthesiologists, 2 nurse anesthetists, and 2 nurse anesthesia students. This group assigned 1 anesthesiologist to head and organize the anesthesia care among the anesthesia team. The responsibility of airway management and the maintenance of anesthesia was given to the primary nurse anesthetist. The student registered nurse anesthetists (SRNAs) charted and acted as runners for blood products, laboratory tests, and supplies. The other anesthesia staff helped with administering fluids and blood products, drawing blood specimens for laboratory evaluation, and acting as an extra pair of hands. The primary anesthesiologist and nurse anesthetist performed a history and physical, verified that informed consent was obtained, and addressed the patient’s questions and concerns. Four units of packed red blood cells (PRBCs) were brought into the surgical suite and checked per hospital protocol, and an order to keep 2 U ahead was given to the blood bank. The primary nurse anesthetist administered 30 mL of citric acid/sodium citrate by mouth and 10 mg of metoclopramide intravenously (IV) to the patient. Cefazolin, 2 g, was administered with the intravenous fluid. The SRNA, under the guidance of the primary nurse anesthetist, preoxygenated the patient by mask for 5 minutes. After the surgical staff prepped and draped the patient, the anesthesia team performed a rapid sequence induction with cricoid pressure. The anesthesiologist administered 40 mg of etomidate and 200 mg of succinylcholine through a 16-gauge peripheral intravenous line. The SRNA unsuccessfully intubated the patient with the first laryngoscopy. A second attempt by the primary nurse anesthetist was successful and atraumatic with a grade 2 view of the vocal cords. The anesthesiologist inserted a 9 French catheter into the subclavian vein immediately before incision, and a left radial arterial line was placed simultaneously. Isoflurane and fentanyl were used for anesthetic maintenance and rocuronium was used for paralysis throughout the case. The patient underwent a classical fundal cesarean delivery and delivered a viable neonate. The surgeon explored the abdomen noting the placenta extended through the uterine wall and into the bladder base, and a diagnosis of placenta percreta was made. The uterus was closed, at which time intra-abdominal hemorrhage commenced emanating from the uterus and placental perforation site. Subsequently, the obstetrical team con- 374 AANA Journal October 2012 Vol. 80, No. 5 sisting of 2 general obstetricians emergently consulted a gynecologic oncologist who assumed the directing role of lead surgeon. The surgical team considered the hemorrhage to be life threatening and promptly initiated a massive blood transfusion. The patient proceeded to lose approximately 16,000 mL of blood over the next 3 hours. The hemoglobin dropped to a low of 5.4 g/dL (Table 1) and pH decreased to 7.21 with a base deficit of 9. The coagulation studies, which were within normal limits preoperatively, changed appreciably to a prothrombin time of 20.8 seconds, an international normalized ratio (INR) of 1.8, a fibrinogen level of 157 mg/dL, and a D-dimer of 984 ng/mL. In all, 22 U of PRBCs, 12 U of platelets, 8 U of fresh frozen plasma (FFP), and 12,000 mL of crystalloid were administered (Table 2). Ten units of cryoprecipitate and 90 µg/kg of factor VIIa were also given for disseminated intravascular coagulation (DIC)-like signs and symptoms. The acidosis was controlled with sodium bicarbonate, and the electrolytes were rebalanced with the administration of potassium and calcium chloride. Throughout surgery, the anesthesia team maintained the patient’s systolic blood pressure above 90 mm Hg with intermittent boluses of phenylephrine as needed. Urine output remained above 3 mL/kg/h with a total urine output of 1,200 mL. The surgeons controlled the hemorrhage via a hysterectomy and a bilateral salpingo-oophorectomy, and the case proceeded as planned with the addition of a partial cystectomy performed by the urologist. By the conclusion of the case, the hemoglobin returned to a value of 11.2 g/dL. The coagulation panel also returned to normal with a prothrombin time of 12.8 seconds, INR of 1.1, and fibrinogen level of 427 mg/dL. The team transferred the intubated and sedated patient to the intensive care unit with stable vital signs. She was extubated the next day and discharged home 1 week later. Discussion The series accreta, increta, and percreta represent abnormalities of placentation, by which placental villi or trophoblasts respectively attach, invade, and even penetrate the myometrium.8,10,14,15 Placenta percreta invading into the bladder presents as a very rare obstetrical condition with an incidence of 0.3 to 1 per 10,000 births.13,16 Surgical management is extremely difficult with a maternal mortality rate of 5.6% to 10% secondary to hemorrhage, infection, and damage to adjacent organs.9,16-17 Any abnormal placental attachment is thought to occur because of an absence or the deficiency of the Nitabuch’s layer of the decidua. Because of this deficiency, the placenta does not separate cleanly from the uterus after delivery and maternal hemorrhage ensues.5 Some studies posit that this decrease in decidua occurs after trauma to the uterus secondary to cesarean deliveries and curettage.9,14,17 Clark et al18 state a uterine scar www.aana.com/aanajournalonline Preoperative Hemoglobin PT/INR Perioperative Postoperative 11.5 g/dL 5.4 g/dL 11.2 g/dL WNL 20.8 s/1.8 12.8 s/1.1 Table 1. Hemoglobin and Coagulation Studies Abbreviations: PT, prothrombin time; INR, international normalized ratio; WNL, within normal limits. predisposes a patient to the development of abnormal placental attachment in later pregnancies and Breen et al8 observe that the absence of decidua is a constant pathologic feature for both placenta accreta and placenta previa. Breen et al8 take it a step further and proposes any event adversely affecting the endometrium could result in placenta accreta. The general consensus in the literature suggests the incidence of abnormal placenta attachment is rising secondarily to certain risk factors. These risk factors include increased age of the mother during pregnancy, multiple pregnancies, previous cesarean deliveries, previous curettages, Asherman syndrome, and the presence of placenta previa.6,13,19,20 The mother in this particular case study presented with a number of associated risk factors including advanced age, a previous pregnancy, and subsequent cesarean delivery, as well as prior uterine procedures. All women presenting with placenta previa combined with uterine scarring should be evaluated for abnormal placentation.4,5,10,21 Clark et al18 state there is an 11-fold increase of placenta previa with women greater than the age of 40 compared to those under age 20. Clark et al18 note that between 1977 and 1983 of 97,799 delivering patients at L.A. County Women’s Hospital, placenta previa was diagnosed in 0.3% (292 patients). The chance of placenta accreta is 5% in women with concomitant previa and an unscarred uterus. The incidence jumps to 67% with 4 prior cesarean deliveries and the diagnosis of placenta previa.18 In 1997, Miller et al14 performed a retrospective analysis and found the occurrence of placenta accreta rising from an incidence of 1 per 4,027 in 1985 to approximately 1 per 2,500 deliveries in 1994. Following this trend, cesarean deliveries also increased from 4.5% in 1965 to 26.1% in 2002. The cesarean delivery rate in developed countries now exceeds 30%, and in the United States the rate of cesarean deliveries has risen by 53% over the past 10 years.3,4 Wu et al22 found the incidence of placenta accreta increased concomitantly from 1 per 30,000 in the 1930s to 1960s to 1 per 2,500 in the 1980s. Wu et al,22 in a retrospective review at the University of Chicago, found over a 20-year period (1982-2002) an incidence of accreta at 1 per 533 pregnancies. The Society for Maternal-Fetal Medicine reports the incidence of placenta accreta has increased from 0.8 per 1,000 deliveries in the 1980s to 3 per 1,000 deliveries in the last decade and is rapidly becoming a major cause of obstetric complications worldwide.10 Although there is some disparity among these numbers between the various researchers, they all relate the same message: a steep rise in the frequency of abnormal placental placement. Miller et al14 place the risk of placenta accreta at 10% in the presence of placenta previa. Clark et al18 find the risk of having placenta accreta rises from 24% with patients having 1 cesarean delivery to 67% in patients who have 3 or more prior cesarean deliveries when placenta previa was present. Miller et al14 state in their report 89% of patients found with placenta accreta also had coexisting placenta previa. Seventy-three percent of patients with placenta accreta have a history of greater than 1 cesarean delivery. Researchers also often associate placenta accreta with placenta previa and multiple cesarean deliveries in women who have a history of dilation and curettage.3,4,14 Conversely, Kamani et al15 believe that at least part of the increase in incidence of abnormal placental attachment is probably a reflection of better reporting. Breen et al8 report a survey of data beginning in 1891 to 1972 showing the incidence of placenta accreta, increta, and percreta anywhere from 0 per 70,000 deliveries to 1 per 540 deliveries. Breen’s own institution reports 1 placenta accreta per 2,700 deliveries. This study includes 40 patients diagnosed with placenta accreta, increta, and percreta. The average age of the patient was 29.5 years and 30% of the diagnosed patients had previous cesarean deliveries. Early signs and symptoms of placenta percreta are nonspecific and may not be found until a sentinel event such as antepartum hemorrhage or spontaneous uterine rupture takes place.13,23 Taefi et al24 present a case in which a 39-year-old patient with 6 prior cesarean deliveries and a history of dilation and curettage developed gross hematuria with eventual hemorrhage. They found www.aana.com/aanajournalonline AANA Journal PRBCs 22 U Platelets 12 pack FFP 8U Cryoprecipitate 10 U Coagulation factor VIIa 90 µg/kg Crystalloid 12,000 mL Blood loss 16,000 mL Table 2. Fluids and Blood Products Abbreviations: PRBCs, packed red blood cells; FFP, fresh frozen plasma. October 2012 Vol. 80, No. 5 375 a placenta percreta invading into the bladder only after an exploratory laparotomy was performed. Definitive diagnosis of placenta accreta, increta, and percreta cannot be made until after delivery and a tentative diagnosis of accreta is usually not made until the third trimester; however, clinicians are able to identify patients at risk early in the pregnancy.8,15 Patients who fall into an at-risk category such as a history of multiple parity, multiple cesarean deliveries, prior curettage, advanced age, and a diagnosis of placenta previa require more aggressive surveillance.14,17 Clark et al18 find an increased association of accreta with a history of low transverse uterine incision and placenta previa. Placenta accretas are often found in the anterior region of the uterus in close association with previous cesarean incisions.11 Regardless of the risk factors, women with suspected placenta accreta should be scheduled for an elective cesarean delivery in an institution with an up-to-date surgical facility and an experienced multidisciplinary care team.10,25 Mothers presenting with placenta accreta, as well as their fetuses, have a complicated surgical course and a high mortality rate.9,13 One reason for this high morbidity and death rate is that definitive diagnosis of placenta accreta is difficult to elicit before surgery and many times recognized only after hemorrhage or uterine rupture.16,23,26 The importance of early diagnosis cannot be overemphasized. The single greatest factor affecting outcome is early recognition.15 Doppler flow studies, magnetic resonance imaging, as well as vaginal and abdominal ultrasound examinations, should be initiated early for patients who have a high suspicion of abnormal placentation secondary to a significant obstetric history. Although definitive diagnosis is not confirmed until after surgery, these diagnostic tools yield encouraging results and allow time for effective medical management and the coordination of a well-organized surgical team. This allows for a delivery in an elective setting.3,4,10,13,16,17,27 Teamwork is essential to the effective management of an obstetric emergency. A multidisciplinary effort consisting of an experienced surgical and anesthesia team, neonatal care team, blood bank, and laboratory personnel, as well as intensive care unit staff, is vital for optimal management of the patient and fetus.4,10,13,16,28 A gynecological oncologist, interventional radiologist, and urologist may need to be readily available.3,4,9 A surgical plan and prior communication of this plan between the teams are paramount. A disorganized, leaderless extended care team creates confusion, miscommunication, and misinterpretation of pertinent facts, which may lead to an increase in morbidity and mortality. The anesthetist’s role is to maintain the patient’s vital functions, replace blood volume, and if applicable, assume the responsibility as the team leader and coordinator of duties. The surgeon and anesthetist must communicate regularly throughout the case. The obstetrician has the best sight of the field 376 AANA Journal October 2012 Vol. 80, No. 5 and should continually relay to the anesthesia team the best estimate of blood loss. The anesthetist has the most knowledge and understanding of the patient’s hemodynamic status and may need to ask the surgeon for a surgical break with tamponade to catch up with blood loss.28 Placenta accreta is responsible for up to 50% of cesarean hysterectomies, most of which are unplanned, and is now the most common cause for cesarean hysterectomy in developed countries. Excessive blood loss is a major concern of cesarean hysterectomies, and the extent of blood loss is almost always underestimated in these obstetric patients.5,28 Blood products should always be available, and communication with the blood bank should be initiated early lest the elective case change to an urgent case. Retrospectively, in the case presented above, the order for 4 U of blood and keeping 2 U ahead was too conservative. Fortunately, the blood bank was able to keep up with the demand. Hunter and Kleiman13 routinely set up 10 units of PRBCs, 4 units of FFP, and a 10-pack of platelets in suspected cases. Hull and Resnik4 believe all obstetric units should have an obstetric hemorrhage protocol. All patients are cross matched for 10 units of PRBCs, 4 units of FFP, and a 10 pack of platelets. Because of an increased chance of bleeding after 36 weeks, patients should be scheduled for delivery around 34 to 35 weeks’ gestation. But even with early diagnosis, blood loss remains high.29 Plauché et al,30 after analyzing 108 cases of cesarean hysterectomies, found blood transfusions were needed in 66.6% of emergency cesarean hysterectomies versus only 11.8% in elective cases. Weiniger et al26 in a prospective and observational study strongly suggested anesthetists be ready for massive blood loss with all suspected placenta accretas. Hudon et al31 in 1998 found the average blood loss for abnormal placental attachment at 3,000 to 5,000 mL. Gallos et al28 state 90% of patients with placenta percreta lose greater than 3,000 mL of blood, and O’Brien et al17 found the median blood transfusion for placenta percreta to be 7 units of PRBCs. Angstmann et al32 reported in some cesarean hysterectomies a 10 L or more blood loss. Recent studies of massive blood transfusion from battlefield trauma support a 1:1 ratio in the transfusion of PRBCs and FFP/platelets to reduce mortality.4,10,33 This recommendation suggests that when an anesthetist is confronted with a patient presenting with abnormal placentation, a more aggressive use of FFP and platelets may improve outcome compared to standard replacement protocols. Techniques to decrease blood loss and control bleeding vary, but all serve to help restore hemodynamic stability. These techniques include manual compression or cross clamping the aorta, oxytocics administration, utilizing cell saver, hemodilution, bilateral iliac artery occlusion/embolization, and factor VIIa administration to name a few.6,9,13,15,28,29,34 Cell saver is controversial in www.aana.com/aanajournalonline obstetric patients though recent data attest to its safety.6 Gallos et al28 states cell saver is quick, inexpensive, and no cross matching is necessary. However, the major drawback is the potential introduction of fetal hemoglobin into the mother’s blood stream. The most important treatment for minimizing blood loss is a hysterectomy with the implanted placenta left in place. Cesarean delivery with a total abdominal hysterectomy is the preferred approach.8,9,11,14 Nevertheless, this management is associated with significant risk of lethal hemorrhage.34 Another option to minimizing blood loss favors the more conservative approach of leaving the placenta and uterus in situ, closing the abdomen, and letting the placenta reabsorb over a period of weeks.11 Clinicians reserve this option for patients who want to preserve fertility, present as Jehovah’s Witnesses, or have no active bleeding. Although decreased bleeding is a benefit of this treatment, placental reabsorption carries an increased risk of sepsis and hemorrhage postoperatively necessitating a total abdominal hysterectomy in an emergency setting and thereby increasing the risk of serious complications.34 Some researchers feel the use of methotrexate and iliac artery embolization and/or balloon occlusion facilitate a positive outcome with the conservative approach of placental reabsorption, though the literature varies with results.21,35 After the delivery, clinicians should follow the patient’s beta human chorionic gonadotropin until normalized to monitor placental reabsorption progress. Patients who decide on the conservative approach may need to be watched closely for bleeding and infection for up to 5 months.19 Most anesthesia providers choose general anesthesia as the anesthetic of choice for patients undergoing cesarean hysterectomies.15,36 In this case study, the anesthesia team and the obstetric team deliberated the best strategy for the anesthetic course and planned for a general anesthetic. Regional anesthesia was not considered in the best interest of this particular patient for 2 main reasons; the airway would not be secure allowing for a strong possibility of rescuing the airway during a demanding anesthetic course and because hemorrhage was a significant concern. Regional anesthesia for patients presenting with abnormal placentation is controversial. Hunter and Kleiman13 demonstrated no excessive bleeding with regional anesthesia when compared with general anesthesia in this population. If regional anesthesia is chosen, an epidural catheter is the preferred technique. Oyelese and Smulian9 and Gallos et al28 found regional anesthesia safe for patients who have abnormal placentation with the caveat that general anesthesia should be initiated at the first signs of significant blood loss. Regardless of the anesthetic technique, adequate intravenous access and invasive monitoring are crucial to a successful outcome. At a minimum, 2 large bore IVs are needed for fluid resuscitation, however, a central line with catheter access is preferred. An arterial line is useful for continuous blood pressure measurements and access to serial blood sampling for blood gasses and laboratory analysis. A rapid infusion device and/or pressure bags should be readily available in the suite. Vasoactive medications, blood products, and fluid warmers must be available and set up ahead of time. Body warming devices should be placed on the patient before incision.15 Expect complications such as DIC, surgical injury, invasive tissue to the ureter and bladder, adult respiratory distress syndrome, infection, and multisystem organ failure.5,9,10,28 www.aana.com/aanajournalonline AANA Journal Conclusion Patients presenting with abnormal placentation have a complicated surgical course and a high mortality rate. The general consensus in the literature suggests the incidence of abnormal placental attachment is rising secondarily to the increasing incidence of risk factors. These include increased maternal age, multiple pregnancies, previous cesarean deliveries, previous curettages, and the presence of placenta previa. The incidence of abnormal placentation is rare but rising and is responsible for up to 50% of cesarean hysterectomies, the majority of which are unplanned. The single greatest factor affecting a positive patient outcome is early recognition. This allows time for the organization of teamwork, leadership, and communication between services, which is paramount to reaching the goal of an optimal outcome for both mother and baby. In conclusion, anesthetists must have plenty of assistance and be prepared for massive blood loss in all cases of abnormal placentation. Adequate amounts of blood products should be set up before surgery with an order to keep ahead for at least 4 U PRBCs. At a minimum, 2 large bore IV catheters (16 gauge or larger) should be in place for the procedure. General anesthesia is the anesthetic of choice for patients undergoing cesarean hysterectomies for placenta accreta. The author offers a case study of a patient with an invading placenta percreta who presented with a number of risk factors associated with this disease as an example of a successful way to manage this complex population. REFERENCES 1. Tantbirojn P, Crum CP, Parast MM. Pathophysiology of placenta creta: the role of decidua and extravillous trophoblast. Placenta. 2008; 29(7):639-645. 2. Yoshino O, Osuga Y, Hirota Y, et al. Endometrial stromal cells undergoing decidualization down regulate their properties to produce proinflammatory cytokines in response to interleukin-1 beta via reduced p38 mitogen-activated protein kinase phosphorylation. J Clin Endocrinol Metab. 2003;88(5):2236-2241. 3. Russo M, Krenz EI, Hart SR, Kirsch D. Multidisciplinary approach to the management of placenta accreta. Ochsner J. 2011;11(1):84. 4. Hull AD, Resnik R. Placenta accreta and postpartum hemorrhage. Clin Obstet Gynecol. 2010;53(1):228-236. 5. Silver RM. Delivery after previous cesarean: long-term maternal October 2012 Vol. 80, No. 5 377 outcomes. Semin Perinatol. 2010;34(4):258-266. 6. Kuczkowski KM. Anesthesia for the repeat cesarean section in the parturient with abnormal placentation: what does an obstetrician need to know? Arch Gynecol Obstet. 2006;273(6):319-321. 7. Litwin MS, Loughlin KR, Benson CB, Droege GF, Richie JP. Placenta percreta invading the urinary bladder. Br J Urol. 1989;64(3):283-286. 8. Breen JL, Neubecker R, Gregori CA, Franklin JE Jr. Placenta accreta, increta, and percreta: a survey of 40 cases. Obstet Gynecol. 1977;49 (1):43-47. 9. Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol. 2006;107(4):927-941. 10. Belfort MA. Society for Maternal-Fetal Medicine. Clinical opinion: placenta accreta. Am J Obstet Gynecol. 2010;203(5):430-439. 11. Jaraquemada JMP, Pesaresi M, Nassif JC, Hermosid S. Anterior placenta percreta: surgical approach, hemostasis, and uterine repair. Acta Obstet Gynecol Scand. 2004;83(8):738-744. 12. Fox H. Placenta accreta, 1945-1969. Obstet Gynecol Surv. 1972;27: 475-490. 13. Hunter T, Kleiman S. Anaesthesia for caesarean hysterectomy in a patient with a preoperative diagnosis of placenta percreta with invasion of the urinary bladder. Can J Anesth. 1996;43(3):246-248. 14. Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177(1):210-214. 15. Kamani AA, Gambling DR, Christilaw J, Flanagan ML. Anaesthetic management of patients with placenta accreta. Can J Anesth. 1987; 34(6):613-617. 16. Ng MK, Jack GS, Bolton DM, Lawrentschuk N. Placenta percreta with urinary tract Involvement: the case for a multidisciplinary approach. Urology. 2009;74(4):778-782. 17. O’Brien JM, Barton JR, Donaldson ES. The management of placenta percreta: conservative and operative strategies. Am J Obstet Gynecol. 1996;175(6):1632-1638. 18. Clark SL, Koonings PP, Phelan JP. Placenta previa/accreta and prior cesarean section. Obstet Gynecol. 1985;66(1):89-92. 19. Lee PS, Bakelaar R, Fitpatrick CB, Ellestad SC, Havrilesky LJ, Secord AA. Medical and surgical treatment of placenta percreta to optimize bladder preservation. Obstet Gynecol. 2008;112(2):421-424. 20. Khong TY. The pathology of placenta accreta, a worldwide epidemic. J Clin Pathol. 2008;61(12):1243-1246. 21. Shevell T, Malone FD. Management of obstetric hemorrhage. Semin Perinatol. 2003;27(1):86-104. 22. Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twentyyear analysis. Am J Obstet Gynecol. 2005;192(5):1458-1461. 23. LeMaire WJ, Louisy C, Dalessandri K, Muschenheim F. Placenta percreta with spontaneous rupture of an unscarred uterus in the second trimester. Obstet Gynecol. 2001;98(5):927-929. 378 AANA Journal October 2012 Vol. 80, No. 5 24. Taefi P, Kaiser TF, Sheffer JB, Courey NG, Hodson JM. Placenta percreta with bladder invasion and massive hemorrhage: report of a case. Obstet Gynecol. 1970;36(5):686-687. 25. Eller AG, Bennett MA, Sharshiner M, et al. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet Gynecol. 2011;117(2 Pt 1):331-337. 26. Weiniger CF, Elram T, Ginosar Y, Mankuta D, Weissman C, Ezra Y. Anaesthetic management of placenta accreta: use of a pre-operative high and low suspicion classification. Anaesthesia. 2005;60(11):10791084. 27. Thorp JM Jr, Councell RB, Sandridge DA, Wiest HH. Antepartum diagnosis of placenta previa percreta by magnetic resonance imaging. Obstet Gynecol. 1992;80(3 Pt 2):506-508. 28. Gallos G, Redai I, Smiley RM. The role of the anesthesiologist in management of obstetric hemorrhage. Semin Perinatol. 2009;33(2):116-123. 29. Pelosi MA 3rd, Pelosi MA. Modified cesarean hysterectomy for placenta previa percreta with bladder invasion: retrovesical lower uterine segment bypass. Obstet Gynecol. 1999;93(5 Pt 2):830-833. 30. Plauché WC, Gruich FG, Bourgeois MO. Hysterectomy at the time of cesarean section: analysis of 108 cases. Obstet Gynecol. 1981;58(4): 459-464. 31. Hudon L, Belfort MA, Broome DR. Diagnosis and management of placenta percreta: a review. Obstet Gynecol Surv. 1998;53(8):509-517. 32. Angstmann T, Gard G, Harrington T, Ward E, Thomson A, Giles W. Surgical management of placenta accreta: a cohort series and suggested approach. Am J Obstet Gynecol. 2010;202(1):38. 33. Borgman MA, Spinella PC, Perkins JG, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63(4):805-813. 34. Shih JC, Liu KL, Shyu MK. Temporary balloon occlusion of the common iliac artery: new approach to bleeding control during cesarean hysterectomy for placenta percreta. Am J Obstet Gynecol. 2005;193(5):1756-1758. 35. Hays AM, Worley KC, Roberts SR. Conservative management of placenta percreta: experiences in two cases. Obstet Gynecol. 2008;112 (2 Pt 2):425-426. 36. American Society of Anesthesiologists Task Force on Obstetrical Anesthesia. Practice guidelines for obstetric anesthesia: a report by the American Society of Anesthesiologists Task Force on Obstetrical Anesthesia: Task Force on Obstetrical Anesthesia. Anesthesiology. 2007;106(4):843-863. AUTHOR Daniel Frasca, CRNA, DNAP, is a staff CRNA and student coordinator at St. Mary’s Hospital, Bons Secours, West End Anesthesia Group, Richmond, Virginia. Email: dpfrasca1960@comcast.net. www.aana.com/aanajournalonline