Cultural Competence - Background and Benefits
advertisement
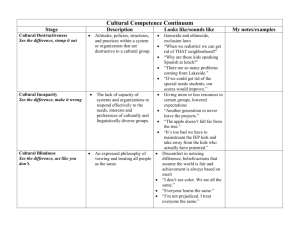
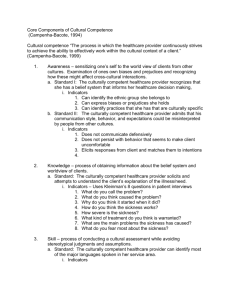
HealthStream Regulatory Script Cultural Competence: Background and Benefits Release Date: August 2010 HLC Version: 603 Lesson 1: Introduction Lesson 2: Cultural Competence Lesson 3: Clinical and Legal Significance of Cultural Competence Lesson 4: Theory of Cultural Competence Lesson 5: Practice of Cultural Competence Lesson 1: Introduction 1001 Introduction Welcome to the introductory lesson on the background and benefits of cultural competence. This lesson provides the course rationale, goals, and outline. As your partner, HealthStream strives to provide its customers with excellence in regulatory learning solutions. As new guidelines are continually issued by regulatory agencies, we work to update courses, as needed, in a timely manner. Since responsibility for complying with new guidelines remains with your organization, HealthStream encourages you to routinely check all relevant regulatory agencies directly for the latest updates for clinical/organizational guidelines. If you have concerns about any aspect of the safety or quality of patient care in your organization, be aware that you may report these concerns directly to The Joint Commission. Point 1 of 4 2 1002 Course Rationale The United States is culturally diverse: • More than 28 million Americans were born outside of the United States. • Forty-seven million Americans do not speak English at home. • Over 300 different languages are spoken in the United States. Healthcare providers will see patients from many backgrounds. Learning about how to give culturally competent care will allow you to: • Optimize your care for all patients • Maintain compliance with laws and recommendations This is the first course in a two-part series on cultural competence. Point 2 of 4 1003 Course Goals After completing this course, you should be able to: • Describe the clinical outcomes associated with cultural competence • Detail the outcomes associated with lack of cultural competence • Identify laws and recommendations about cultural competence • Recognize key terms related to cultural competence • Recall “typical” characteristics of selected cultural groups NO IMAGE Point 3 of 4 1004 Course Outline This introductory lesson gave the course rationale and goals. Lesson 2 will introduce culturally competent care. Lesson 3 will discuss the clinical and legal aspects of cultural competence. Lesson 4 will cover the theory of cultural competence. Lesson 5 will discuss the practice of cultural competence. Point 4 of 4 Lesson 2: Cultural Competence 2001 Introduction Welcome to the lesson introducing cultural competence. This lesson will define cultural competence. It also will introduce culturally competent care and using cultural understanding. Point 1 of 6 2002 Cultural Competence In the healthcare setting, cultural competence refers to the ability to provide optimal medical care to members of various cultural groups. This ability rests on a set of: • Attitudes • Skills • Policies • Practices This set of qualities makes it easier for providers to: • Understand their patients • Communicate with their patients The end result is optimal care for all patients. Point 2 of 6 2003 The Culturally Competent Provider Providers must be able to provide healthcare to: • Patients who do not speak English • Patients from different cultures Providers must understand the patient’s: • Values • Beliefs • Attitudes • Practices • Communication patterns Point 3 of 6 2004 Using Cultural Understanding Providers use their understanding of the patient’s culture to: • Improve medical care • Correct disparities [ glossary] in health status Failure to provide culturally competent care leads to: • Less-than-optimal care for many patients • Elevated rates of disease and mortality among certain populations Point 4 of 6 2005 Review Select the answer that best fits the question. Correct answer: B Cultural competence refers to the ability to provide medical care to different cultural groups. Providing culturally competent care leads to health disparities. a. True b. False Feedback for A: Incorrect. Culturally competent care leads to optimal health care for all patients. Feedback for B: Correct. Culturally competent care leads to optimal health care for all patients. Point 5 of 6 2006 Summary You have completed the lesson on culturally competent care. NO IMAGE Remember: • Cultural competence refers to the ability to provide medical care to different cultural groups. • Providers need a set of attitudes, skills, policies, and practices to more effectively communicate with their patients. • Providers need to understand the patient’s values, beliefs, attitudes, behaviors, and practices. • Providing culturally competent care leads to better patient care. Point 6 of 6 Lesson 3: Clinical and Legal Significance 3001 Introduction Welcome to the lesson on the clinical and legal significance of culturally competent care. This lesson will discuss the benefits of cultural diversity as well as applicable laws and regulations. Point 1 of 17 3002 Cultural Competence and the Practice of Medicine Today Cultural competence is a necessity. Unfortunately, many providers guide their delivery of care by: • Stereotypes • Biases As a result, racial and ethnic minorities tend to receive lower quality care than similar non-minorities. This can have health consequences. Point 2 of 17 3003 Cultural Competence and Quality of Care (1) In what ways do minorities receive lower quality care? CLICK TO REVEAL Lack of cultural competence can lead to: • Lack of medical care • Misdiagnosis • Inappropriate testing • Suboptimal disease screening Lack of medical care Cultural minorities may choose not to seek medical care. They may fear being misunderstood or treated disrespectfully. Click on each to learn more. Misdiagnosis Patients can be misdiagnosed if they are not understood. This is most likely in patients with limited English proficiency (LEP). [glossary] Inappropriate testing Providers may not order needed tests if they do not understand the patient’s symptoms. Alternatively, providers may overcompensate by ordering too many tests. Suboptimal disease screening Some diseases are associated with certain minority groups. The physician must be aware of this to offer appropriate screening. Point 3 of 17 3004 Cultural Competence and Quality of Care (2) Other problems include: • Noncompliance • Reaction to drugs • Conflicting drugs Click on each to learn more. CLICK TO REVEAL Noncompliance Cultural minorities may not follow the advice of medical providers. They may not trust or understand the provider’s instructions fully. This can cause problems in the correct usage of medications or other treatments. Reaction to drugs Racial and ethnic background may affect how a patient responds to a drug. Most drug doses are based on studies of Caucasian patients. Conflicting drugs Patients may be using traditional remedies. This may lead to harmful drug interactions. wjPoint 4 of 17 3005 Cultural Competence and Health Disparities Cross-cultural health disparities may result when care is not culturally competent. For example: • African-Americans are at increased risk for: o Breast, lung, and colorectal cancer mortality o Infant mortality o Flu mortality o Heart-disease mortality o Diabetes o HIV/AIDS o Obesity • Native Americans are at increased risk for: o Infant mortality o Flu mortality o Colorectal-cancer mortality o Obesity • Hispanics/Latinos are at increased risk for: o Diabetes o HIV/AIDS Point 5 of 17 3006 Potential Benefits of Cultural Competence: Clinical (1) What are the potential benefits of cultural competence in the healthcare setting? Benefits include: • More successful patient education • Increased likelihood that minorities will seek healthcare • Fewer diagnostic errors • More appropriate diagnostic testing and screening • Fewer harmful drug interactions • Greater patient compliance • Expanded choices and access to high-quality clinicians • Equality of healthcare outcomes Point 6 of 17 3007 Quality of Care, Health Disparities, and Clinical Outcomes: Summary Effects of Culturally Competent and Non-Competent Care on Cultural Minority Patient Health Cultural Competence Lack of Cultural Competence Increased likelihood that minorities will seek healthcare Lack of medical care Fewer diagnostic errors Misdiagnosis More appropriate testing and screening Inappropriate testing and suboptimal disease screening Greater patient compliance Noncompliance Fewer harmful drug interactions Drug reactions and interactions Equalization of cross-cultural health disparities Health disparities Expanded choices and access to high-quality clinicians Limited healthcare choices More successful patient education Limited/ineffective patient education Point 7 of 17 3008 Potential Benefits of Cultural Competence: Legal and Regulatory Cultural competence also improves compliance with relevant laws and recommendations. These include: • Title VI of the Civil Rights Act of 1964 • The Joint Commission • U.S. Department of Health and Human Services (HHS) Office of Minority Health (OMH) recommendations for national standards on culturally and linguistically [glossary] appropriate services (CLAS) Let’s take a closer look at each. Point 8 of 17 3009 Title VI Title VI of the Civil Rights Act of 1964 requires any health- or social- service organization that receives federal funding to provide language assistance to any patient with limited English proficiency (LEP). Language assistance assures that: • The LEP patient is able to communicate relevant information to the provider. • The provider is able to understand the LEP patient. • The LEP patient is able to understand all necessary information. This includes a description of services and benefits available. • The LEP patient is able to receive eligible services. Point 9 of 17 3010 The Joint Commission Position The Joint Commission considers culturally competent care an important healthcare safety and quality issue. Many standards address issues related to culturally competent care. Those directly addressing cultural competence include: • Standard RI.01.01.01 • Standard RI.01.01.03 Other standards provide organizational supports for culturally competent care. Let’s take a closer look at Standards RI.01.01.01 and RI.01.01.03. Point 10 of 17 3011 The Joint Commission Position: Standard RI.01.01.01 The Joint Commission Standard RI.01.01.01 states that an organization should respect a patient’s rights. This includes their cultural: • Values • Beliefs • Preferences Patients also have a right to: • Personal dignity • Religious or other spiritual practices Point 11 of 17 3012 The Joint Commission Position: Standard RI.01.01.03 Standard RI.01.01.03 addresses a patient’s right to effective communication. Element 1 of this standard states that written information about patient rights must be appropriate to : • The population served • The language of the patient • The patient’s ability to understand Element 2 addresses provision of interpretation and translation services, if needed. Element 3 requires hospitals to meet the communication needs of a patient with hearing, speech, vision, or cognitive impairments. Point 12 of 17 3013 The Joint Commission Position: Hospitals, Language, and Culture Study CLICK TO REVEAL In January 2004, The Joint Commission started a project on cultural competence. Over a 30-month period, they collected data from 60 different hospitals. The ability of these hospitals to address patient language and culture issues was determined. Two reports have been published: • Exploring Cultural and Linguistic Services in the Nation’s Hospitals (in 2007) • One Size Does Not Fit All: Meeting the Health Care Needs of Diverse Populations (in 2008) Click on each report for information about the recommendations each makes for hospitals. Exploring Cultural and Linguistic Services in the Nation’s Hospitals This report recommends that hospitals should: • Consider establishing a centralized program for language and culture • Have policies regarding the provision of language services • Assess interpreter proficiency in the target language and English • Train staff and physicians about accessing services • Improve dialogue • Implement uniform data collection One Size Does Not Fit All: Meeting the Health Care Needs of Diverse Populations This report recommends that hospitals should: • Identify the needs of the population they serve • Assess how well the needs of patients are being met • Bring together people from across the hospital to discuss cultural and language issues • Implement a continuous process of assessment, monitoring, and evaluation of needs and services • Implement practices for building a foundation of cultural competence • Implement practices for collecting and using data to improve services • Implement practices for accommodating the needs of specific populations • Implement practices for establishing internal and external collaborations Point 13 of 17 3014 CLAS Standards The U.S. Department of Health and Human Services Office of Minority Health has 14 recommendations for national standards on culturally and linguistically appropriate services (CLAS). These recommendations address: • Culturally representative staffing • Staff education and training • Language-assistance services and materials • Organizational self-assessment • Data collection • Cross-cultural conflict and grievance processes The goals are to: • Correct healthcare disparities • Improve medical services The CLAS standards for language assistance (Standards 4, 5, 6, 7) are required for hospitals receiving federal funding. Point 14 of 17 3015 Review Drag and drop each of the terms in the word bank to its proper place in the table. Cultural competence is characterized by: Effective communication Thorough understanding of individual patients Willingness to learn Lack of cultural competence is characterized by: Use of stereotypes Biased delivery of healthcare Making assumptions about patients Point 15 of 17 3016 Review Select the answer that best fits the question. Correct answer: D Which of the following requires or recommends that hospitals provide language assistance to LEP clients: a. CLAS standards b. Title VI of the Civil Rights Act of 1964 c. The Joint Commission standards on cultural competence d. All of the above Feedback for A: Not quite. All of these require or recommend that hospitals provide assistance to clients that have problems speaking English. Feedback for B: Not quite. All of these require or recommend that hospitals provide assistance to clients that have problems speaking English. Feedback for C: Not quite. All of these require or recommend that hospitals provide assistance to clients that have problems speaking English. Feedback for D: Correct. All of these require or recommend that hospitals provide assistance to clients that have problems speaking English. Point 16 of 17 3017 Summary You have completed the lesson on the clinical and legal significance of cultural competence. NO IMAGE Remember: • Cultural competence is often lacking in the practice of medicine today. This leads to adverse patient outcomes and health inequality. • Delivering medical services in a culturally competent way has many benefits for patients. • Title VI of the Civil Rights Act requires any health- or social- service organization that receives federal funding to provide effective language assistance to LEP patients/clients. • The Joint Commission requires accredited hospitals to respect a patient’s rights and dignity. • The OMH released national standards on culturally and linguistically appropriate services (CLAS). CLAS 4-7 are requirements. Point 17 of 17 Lesson 4: Theory of Cultural Competence 4001 Introduction Welcome to the lesson on theory of cultural competence. This lesson will include a discussion of values, worldview, time orientation, and traditional social structure. The culture of western medicine will also be reviewed. Point 1 of 17 4002 Understanding Patients How can healthcare providers understand their patients? Useful information includes the patient’s healthcare-related: • Beliefs • Attitudes • Behaviors • Practices Many of these arise from the patient’s underlying: • Values • Worldview • Time orientation • Traditional social structure Let’s take a closer look at each of these four underlying characteristics. Point 2 of 17 4003 Understanding Patients: Values A value is anything important to an individual or a culture. For example, in the United States, we tend to value: • Money • Freedom • Privacy • Health/fitness • Physical appearance Values drive behavior. Understanding a patient’s values can help you understand his or her behavior. Understanding allows you to respond to a patient’s behavior in a respectful, effective way. Point 3 of 17 4004 Understanding Values: An Example Mr. C is a 45-year-old patient under the care of Nurse Jones. Mr. C’s family members wish to participate in his care. Nurse Jones responds with irritation and annoyance. She does not understand why the C family does not abide by visiting hours. They do not understand the importance of self-care for the patient. Mr. C explains that his family values family loyalty and duty. He tells Nurse Jones that his wife and children would feel guilt and dishonor if they did not assist him. Nurse Jones now understands that the C family is not ignoring her instructions. She can find ways to allow the family to help the patient. Point 4 of 17 4005 Understanding Patients: Worldview (1) A person’s worldview consists of his or her basic assumptions about the nature of reality. Most people believe their worldview without question. This can lead to ethnocentrism [glossary]. Ethnocentrism is the belief that: • One’s own way is right and natural • Other ways are inferior, unnatural, uncivilized, etc. The opposite of ethnocentrism is cultural relativism [glossary]. Cultural relativism: • Looks at behavior and beliefs in their cultural context • Accepts that other ways may be different, but equally valid Point 5 of 17 4006 Understanding Patients: Worldview (2) Western healthcare tends to be ethnocentric. It is assumed that: • Western approaches to healing are best • Other methods are not to be trusted or accepted Cultural competence demands cultural relativism. Healthcare providers must be willing to: • Acknowledge the validity of other methods • Incorporate traditional or folk medicine into treatment plans as needed Point 6 of 17 4007 Understanding Worldview: An Example According to the worldview of Western medicine, infection is caused by microorganisms. Ms. P believes that her bacterial pneumonia is the result of an imbalance of “hot” and “cold” in her body. Western medicine would insist that antibiotics can cure bacterial pneumonia. But, antibiotics are unlikely to help Ms. P: • Ms. P may not take the antibiotics because she believes that they will not help. • Even if Ms. P takes antibiotics, she may not reach a true state of healing. She will not believe she has corrected the underlying problem of heat/cold imbalance. In other words, a patient’s beliefs must always be considered. Accommodating beliefs while treating the body will: • Help ensure compliance • Help ensure full healing Point 7 of 17 4008 Understanding Patients: Time Orientation Time orientation has two aspects: • Emphasis on past, present, or future • Attention to clock time Let’s take a closer look at each. Point 8 of 17 4009 Time Orientation: Past, Present, or Future Persons with a past-time orientation tend to: • Be traditional • Do things the way they have always been done Persons with a present-time orientation tend to: • Look to today • Make few plans or provisions for the future Persons with a future-time orientation tend to: • Place trust and faith in technologic innovations • Plan for the future Point 9 of 17 4010 Past, Present, or Future Time: An Example Western healthcare tends to be future-focused. Preventive medicine is emphasized. Follow-up care is given. New techniques and medications are adopted. Patients with a more present focus may not comply with preventative health measures. For example, it may be difficult for them to remember to take medication each day. Point 10 of 17 4011 Time Orientation: Clock Time Some people pay careful attention to the passage of time, according to the clock. Others mark time by activities. Western healthcare is clock-focused. For example, you are late for your 10:15 appointment if you arrive at 11:00. Patients who are not clock-focused would consider both 11:00 and 10:15 “mid-morning.” They would not worry about being late. Point 11 of 17 4012 Understanding Patients: Social Structure In terms of power, authority, and opportunity, a social structure may be egalitarian or hierarchical [glossary}. In an egalitarian society, such as the United States, all people are inherently equal. In a hierarchical society, people are not equal. Social status is based on characteristics such as age, sex, lineage, or occupation. Point 12 of 17 4013 Understanding Social Structure: An Example In Western healthcare, all competent adult patients have equal authority and power to make healthcare decisions for themselves. In a hierarchical structure: • Husbands may make healthcare decisions for their wives and children. • A patient may expect the provider to make treatment decisions for him or her. Social structure is often related to religious belief. Point 13 of 17 4014 Understanding Social Structure: Family Structure A patient’s family structure may determine who makes healthcare decisions. There are seven family structures: • Traditional Nuclear Family • Nuclear Dyad Family • Extended Family • Skip Generation Family • Alternative Family • Single Parent Family • Reconstituted or Blended Family A family structure may also be: • Matriarchal • Patriarchal CLICK TO REVEAL A traditional nuclear family is composed of a married man and woman and their biological or adopted child or children. A nuclear dyad consists of a man and woman only. An extended family is composed of two or more adults from different generations. Children, aunts, uncles, cousins, grandparents, etc. may be included. In a skip generation family, children are raised by their grandparents. An alternative family is composed of a same-sex couple and children. A single parent family is composed of a single adult and their children. A reconstituted or blended family is composed of two parents, their biological or adopted children, and their children from previous marriages or relationships. In a matriarchal family, the family head is a female. In a patriarchal family, the family head is male. Point 14 of 17 4015 Review Select the answer that best fits the question. Correct answer: B Which of the following best supports the development of cultural competence? a. Ethnocentrism b. Cultural relativism c. Future time orientation d. Observed family behavior Feedback for A: Incorrect. Cultural competence demands acceptance that other ways are equally valid. The correct answer is B. Feedback for B: Correct. Cultural competence demands acceptance that other ways are equally valid. Feedback for C: Incorrect. Cultural competence demands acceptance that other ways are equally valid. The correct answer is B. Feedback for D: Incorrect. Cultural competence demands acceptance that other ways are equally valid. The correct answer is B. Point 15 of 17 4016 Review Drag and drop each of the terms in the word bank to its proper place in the table. A person with a… Past-time orientation Present-time orientation Future-time orientation Tends to: Do things the way they have always been done. Look to today. Trust technological innovations. Point 16 of 17 4017 Summary You have completed the lesson on theory of cultural competence. NO IMAGE Remember: • A value is anything important to an individual or culture. • A person’s worldview consists of his or her basic assumptions about the nature of reality. • Western medicine tends to be ethnocentric. Cultural competence demands cultural relativism. • Time orientation has two aspects: emphasis on past, present, or future, and level of attention to clock time. • A social structure may be egalitarian or hierarchical. • Cultural values, worldview, time orientation, and social structure can shape healthcare-related attitudes, beliefs, behaviors, and practices. • You need to understand a patient’s values, worldview, time orientation, and social structure to provide quality patient care. Point 17 of 17 Lesson 5: Practice of Cultural Competence 5001 Introduction Welcome to the lesson on the practice of cultural competence. This lesson will discuss stereotypes, generalizations, and characteristics of selected cultural groups. Point 1 of 22 5002 Culture Groups Let’s look at how cultural characteristics influence a patient’s healthcare-related attitudes and behaviors. Important note: The cultural characteristics given are generalizations. They indicate common trends and patterns. Generalizations should NEVER be used to stereotype. Do not assume that the patient fits the generalizations assigned to his or her culture group! Point 2 of 22 5003 Culture Groups: African-American (1) Religion is important in the lives of African-Americans. Patients should be given time and privacy to pray. Clergy should be allowed to participate in the patient’s care. The head-of-household is often a woman. Other relatives and friends may be included in the patient’s extended family. African-Americans tend to have a present-time orientation. Providers should emphasize the importance of prevention. Point 3 of 22 5004 Culture Groups: African-American (2) African-Americans may refer to “high blood” or “low blood.” You need to determine what symptom the patient is describing. You also must be sure that you use words the patient understands. Be sure you both have a common understanding of the words used to describe medical conditions. The tradition of herbal remedies is strong in the African-American culture. Ask patients if they are taking any herbal remedies. This will avoid drug interactions. Remember! These are generalizations. They should not be used to stereotype any patient. These also are selected examples only. Point 4 of 22 5005 Culture Groups: Anglo-American (1) Anglo-American patients expect to be informed of the details of their condition. They value direct eye contact, privacy, and emotional control. They may expect nurses to provide psychosocial [glossary] care. Patients in this culture group generally make healthcare decisions for themselves. Parents make decisions for their minor children. They value self-care. Poverty may lead to a present-time orientation. These patients may not comply with preventive medical advice. Middle- and upper-class Anglo-Americans tend to have a future focus. They are likely to comply with preventative medical advice. Point 5 of 22 5006 Culture Groups: Anglo-American (2) Anglo-Americans often prefer biomedicine. [ glossary] They also may use alternative approaches. Ask about herbal remedies and other complementary medicine. Patients in this group expect an aggressive approach to treatment. They assume that treatment will focus on killing germs. They may demand antibiotics, even when unnecessary. Remember! These are generalizations. Do not stereotype any individual patient. These also are selected examples only. Point 6 of 22 5007 Culture Groups: Asian (1) To show respect, Asian patients may avoid eye contact with the provider. They also may agree with their provider. Agreement does not always indicate understanding. Agreement may not indicate an intention to comply with the treatment plan. Avoid yes or no questions. Ask for responses that demonstrate understanding. Always stress the importance of compliance. Men may make healthcare decisions for their wives. Family members will expect to be involved in treatment decisions and patient care. Allow family to care for the patient as much as possible. Point 7 of 22 5008 Culture Groups: Asian (2) Asian patients may not express pain. Pain medication should be offered when appropriate. This should be done even if the patient does not request it. Family members may wish to protect a patient from hearing a poor prognosis or terminal diagnosis. Ask the patient which family member(s) should receive information about his or her condition. Coining [glossary] and cupping [glossary] are traditional medical practices in many Asian cultures. They should not be mistaken for signs of abuse. Remember! These are generalizations. Do not stereotype any patient. These also are selected examples only. Point 8 of 22 5009 Culture Groups: East Indian East Indians may consider direct eye contact rude or disrespectful. Silence may indicate acceptance or approval. Family members are likely to take over the activities of daily living for a patient. Unless patient self-care is medically necessary, allow this expression. The Sikh religion forbids cutting or shaving head or facial hair. Consult with patients before surgical prep. Remember! These are generalizations. Do not stereotype any patient. These also are selected examples only. Point 9 of 22 5010 Culture Groups: Hispanic/Latino (1) Hispanic/Latinos place high value on: • Direct eye contact • Friendly physical contact • Friendly interpersonal interaction It is appropriate to maintain a friendly manner with Latino patients. Ask patients about their families and interests before focusing on health-related issues. Children are highly valued and loved. Allow family members to spend as much time as possible with pediatric patients. The oldest adult male is the decision-maker. However, important decisions involve the family. Point 10 of 22 5011 Culture Groups: Hispanic/Latino (2) Hispanic/Latinos may refuse hospital foods that would upset their hot/cold body balance. Offer alternatives. Many traditional Mexican foods are high in salt and fat. Be certain to discuss nutrition. This is very important for diabetics and hypertensives [glossary]. Hispanic/Latino patients may use herbal remedies. Ask before prescribing medication. Remember! These are generalizations. Do not stereotype any patient. These also are selected examples only. Point 11 of 22 5012 Culture Groups: Middle Eastern (1) Your Middle Eastern patients may believe that communication is two-way. You may need to share information about yourself first. Then you can receive information from the patient. Sexual segregation is an important aspect of Middle Eastern culture. Assign same-sex caregivers and interpreters. Middle Eastern men may answer for their wives. Women may allow their husbands to make healthcare decisions for the family. Point 12 of 22 5013 Culture Groups: Middle Eastern (2) Islam is important to the majority of Middle Eastern people. Allow time and privacy to pray. Be aware that these patients believe that personal health is in the hands of Allah. Middle Eastern patients may avoid taking an active role in their own healthcare. Middle Easterners may expect all treatment plans to involve a prescription for medication. Remember! These are generalizations. Do not stereotype any patient. These also are selected examples only. Point 13 of 22 5014 Culture Groups: Native American (1) Patients in this group may communicate through anecdotes and metaphors [glossary]. During a conversation, the patient may pause for an extended length of time. This indicates careful consideration of the question or issue. Do not press the patient for an answer. Avoid direct eye contact. Do not speak loudly. Any illness concerns the entire family. Healthcare decisions may be made by the male head of the family, the female head of the family, or the patient. Native Americans tend not to have a clock-focused time orientation. Point 14 of 22 5015 Culture Groups: Native American (2) Native American patients may be stoic [glossary] about pain. Offer pain medication when appropriate. If a patient wears a medicine bag, [glossary] do not treat the bag casually. Do not remove it without asking the patient. Traditional healing may be an important part of any treatment plan. Accommodate traditional healers. Allow traditional rituals whenever possible. Never touch or casually admire a ritual object. Remember! These are generalizations. Do not stereotype any patient. These also are selected examples only. Point 15 of 22 5016 Culture Groups: Russian/Eastern European (1) When caring for patients in this cultural group, be firm and respectful. Make direct eye contact. Russians tend to have a high threshold for pain. They also may be stoic about pain. Offer pain medication when appropriate. Food is appreciated. A good appetite is admired. Patients and family members may offer small gifts of food or chocolate. Accept these to avoid appearing rude. Point 16 of 22 5017 Culture Groups: Russian/Eastern European (1) Russian and/or Eastern European patients may not feel comfortable with too many personal questions. They may be suspicious of providers who take notes. Smoking, excessive use of alcohol, and lack of exercise may be problematic. Remember! These are generalizations. Do not stereotype any patient. These also are selected examples only. Point 17 of 22 5018 The Culture of Western Medicine Let’s now take a brief look at the culture of Western medicine: • Western healthcare tends to standardize definitions of health and illness. Technology is believed to be allpowerful. • The practice of Western medicine stresses health maintenance and disease prevention. • Western healthcare providers are systematic and methodical. They like promptness, organization, and efficiency. They dislike tardiness, chaos, and inefficiency. • Use of jargon is common in Western healthcare. • Western healthcare providers recognize and adhere to a hierarchical system. The provider’s status is based on education, experience, and professional accomplishments. • Western healthcare observes certain routines. Point 18 of 22 5019 Review Select the answer that best fits the question. Correct answer: A Not all patients within a given cultural group fit the generalizations applicable to that group. a. True b. False Feedback for A: Correct. Generalizations indicate common trends and patterns. But, each patient is unique. Generalizations should NEVER be used to stereotype any patient. Feedback for B: Incorrect. Generalizations indicate common trends and patterns. But, each patient is unique. Generalizations should NEVER be used to stereotype any patient. Point 19 of 22 5020 Review Drag and drop each of the terms in the word bank to its proper place in the table. The following characteristic of Western healthcare… Desire for efficiency Value placed on promptness Emphasis on preventive medicine Belief in the value and efficacy of modern technology and biomedicine …may conflict with the following characteristic of certain patients: Use of long pauses during conversation, to indicate careful consideration Lack of attention to clock-time Present-time orientation Belief in the value and efficacy of traditional/folk medicine Point 20 of 22 5021 Summary You have completed the lesson on practice of cultural competence. NO IMAGE Remember: • Generalizations indicate common trends and patterns within a group. They should never be used to stereotype an individual. • Use generalizations as a starting point to: o Help understand various culture groups o Learn more about the unique values, beliefs, and practices of each patient Point 21 of 22 5022 References • U.S. Census Bureau. Population profile of the United States. Available at: http://www.census.gov/population/www/pop-profile/profile2000.html. Accessed April 13, 2010. • The provider’s guide to quality and culture. Available at: http://erc.msh.org/mainpage.cfm?file=7.0.htm&module=provider&language=English&ggroup=&mgrou p. Accessed April 13, 2010. Joint Commission. Facts about the Hospitals, Language and Culture: A Snapshot of the Nation (HLC) study. Available at: http://www.jointcommission.org/AboutUs/Fact_Sheets/facts_hlc.htm. Accessed April 13, 2010. • • • • • Office of Minority Health. National standards on culturally and linguistically appropriate services (CLAS). Available at: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=15. Accessed April 13, 2010. Galanti G. Cultural diversity in healthcare. Available at: http://www.ggalanti.com/index.html. Accessed April 13, 2010. Spector RE. Cultural Diversity in Health and Illness. 5th edition. Upper Saddle River: Prentice Hall. 2000. James C, Thomas M, Lillie-Blanton M, Garfield R. Key facts: Race, ethnicity, and medical care, 2007 update. Henry J. Kaiser Family Foundation Report. Available at: http://www.kff.org/minorityhealth/6069.cfm. Accessed April 13, 2010. Please remember that compliance is the responsibility of each organization. Provision of this list does not imply that the content of this course wholly or partially addresses the guidelines and references provided here. Point 22 of 22 Course Glossary # Term Definition coining using a coin(usually with heated oil) to vigorously rub the skin in a prescribed manner, causing a mild dermabrasion, with the goal of releasing excess force or "wind" from the body, hence restoring balance placing small, heated glasses on the skin, forming a suction that leaves a red circular mark, with the goal of drawing out a bad force inequality or difference limited English proficiency; used to describe people who do not speak English fluently Joint Commission on the Accreditation of Healthcare Organizations having to do with language the belief that one’s way of doing things is the only right way the belief that other ways may be different from one’s own, but equally valid in their cultural context a type of social organization that assumes the equality of all people, in which every individual has an equal opportunity to obtain resources and the esteem of others in leadership activities a social structure in which there are ordered groupings of people make worse cupping disparity LEP JCAHO linguistic ethnocentrism cultural relativism egalitarian hierarchical exacerbate psychosocial biomedicine hypertensive anecdote metaphor stoic medicine bag involving both psychological and social aspects the branch of medical science that applies biological and physiological principles to clinical practice a patient with high blood pressure short account of an incident a figure of speech in which an expression is used to suggest a similarity between two different things seeming unaffected by pleasure or pain a magical object used to control and direct supernatural forces; a charm Pre-Assessment 1. Providing culturally competent care can lead to all of the following EXCEPT: a. Improved medical care b. Optimal care for patients c. Decreased rates of disease and mortality among certain populations d. Increased disparities in health status Correct: D Rationale: Providers use their understanding of the patient’s culture to correct disparities in health status. 2. Mrs. Petrovich arrives at the clinic for care. She speaks broken English with a heavy accent. Which of the following statements are true about her medical care? a. She will receive the same level of care as any other patient. b. She risks having a misdiagnosis due to communication misunderstanding. c. She will be non‐compliant because she does not trust the care providers. d. All of these statements are true. e. Only B and C are true. Correct: B Rationale: Lack of cultural competence can lead to misdiagnosis if they are not understood. This is most likely in patients with Limited English Proficiency (LEP). Cultural minorities may not follow the advice of medical providers. They may not trust or understand the provider’s instructions fully. 3. Title VI of the Civil Rights Act of 1964 mandates that any health or social service agency that receives federal funding must: a. Provide language assistance to any patient with limited English proficiency (LEP). b. Provide emergency medical care to all patients regardless of their ability to pay. c. Make hiring and firing decisions without regard to race, color, or gender. d. All of the above e. None of the above Correct: A Rationale: Title VI of the Civil Rights Act of 1964 requires any health or social service agency that receives federal funding to provide language assistance to any patient with limited English proficiency. 4. Which of the following statements recognizes the appropriate view for providing culturally competent care? a. Cultural relativism: incorporating traditional or folk medicine into Western medicine treatment plans may be beneficial. b. Cultural relativism: our treatments are the most advanced and the only ones that are effective. c. Ethnocentrism: our treatments are the most advanced and the only ones that are effective. d. Ethnocentrism: incorporating traditional or folk medicine into Western medicine treatment plans may be beneficial. Correct: A Rationale: Cultural competence demands cultural relativism. Healthcare providers must be willing to incorporate traditional or folk medicine into treatment plans as needed. 5. Mr. Jackson is being treated for hypertension and has been instructed to take his antihypertensive medication every morning at 9:00 am. The clinic nurse discovers that Mr. Jackson takes his medication when he thinks about it or when he decides to get out of bed, whatever time that may be. He is demonstrating: a. Past‐time orientation b. Present‐time orientation c. Future‐time orientation d. Clock‐time orientation Correct: B Rationale: Patients with a more present focus may not comply with preventative health measures, as they do not view them as helpful or useful. Non‐compliance with preventative health recommendations such as taking medication for chronic illness may result. 6. In terms of power, authority, and opportunity an egalitarian society believes that sex, age, lineage, and occupation indicate social status. a. True b. False Correct: B Rationale: In an egalitarian society, such as the United States, all people are inherently equal. 7. The head of the household in the African‐American culture is often a woman. This family structure is known as: a. A Matriarchal family b. A Patriarchal family c. A Reconstituted family d. None of the above Correct: A Rationale: In a matriarchal family the family head is a female. 8. Your Asian patient nods her head as you describe her treatment regimen. From this behavior you can be sure that she understands and will comply with the treatment plan. a. True b. False Correct: B Rationale: To show respect, Asian patients may agree with their provider. Agreement does not always indicate understanding or indicate an intention to comply with the treatment plan. 9. Which culture may consider direct eye contact rude or disrespectful? a. Hispanic/Latino b. East Indian c. Anglo‐American d. None of the above. Correct: B Rationale: East Indians may consider direct eye contact rude or disrespectful. 10. Behaviors that would be expected of a Western medicine healthcare provider include: a. Prompt responses to questions and concerns b. Use of technology for diagnosis and treatment of conditions c. Prescribing medication for treatment of diseases such as infection or chronic illness d. All of the above e. None of the above Correct: D Rationale: In Western medicine, technology is believed to be all powerful. Healthcare providers like promptness, organization, and efficiency. The practice of Western medicine stresses health maintenance and disease prevention. Final Exam 11. Which of the following are necessary for the provider to understand in order to provide culturally competent care? a. The patient’s language b. The patient’s socioeconomic status c. The patient’s values, beliefs, and attitudes d. None of the above Correct: C Rationale: Providers need to understand the patient’s values, beliefs, attitudes, behaviors, and practices to provide culturally competent care. 12. Lack of cultural competence can lead to: a. Lack of medical care b. Misdiagnosis due to misunderstanding c. Inappropriate testing d. Suboptimal disease screening e. All of the above Correct: E Rationale: Lack of cultural competence can lead to all of the outcomes listed. 13. Health care agencies must provide language assistance to all patients when the agency is federally funded. a. True b. False Correct: A Rationale: Title VI of the Civil Rights Act of 1964 requires any health or social service agency that receives federal funding to provide language assistance to any patient with limited English proficiency. 14. Which of the following statements recognizes the appropriate view for providing culturally competent care? a. Cultural relativism: incorporating traditional or folk medicine into Western medicine treatment plans may be beneficial. b. Cultural relativism: our treatments are the most advanced and the only ones that are effective. c. Ethnocentrism: our treatments are the most advanced and the only ones that are effective. d. Ethnocentrism: incorporating traditional or folk medicine into Western medicine treatment plans may be beneficial. Correct: A Rationale: Cultural competence demands cultural relativism. Healthcare providers must be willing to incorporate traditional or folk medicine into treatment plans as needed. 15. The Joint Commission does not have standards for culturally competent care, but the expectation is that you will provide it. a. True b. False Correct: B Rationale: The Joint Commission has two standards that specifically address culturally competent care. 16. Your patient arrives for a 10:30 am appointment at 11:15 am. He is intentionally being rude and uncaring about your schedule. a. True b. False Correct: B Rationale: Some people are not clock‐focused and would consider both 10:30 and 11:15 am as mid‐morning. This patient would not worry about being late. 17. Joseph and Roxanne are raising their grandchildren. This is indicative of which family structure? a. Nuclear dyad family b. Extended family c. Skip generation family d. Alternative family Correct: C Rationale: In a skip generation family, children are raised by their grandparents. 18. Generalizations about a patient’s culture should be used to help provide culturally competent care. a. True b. False Correct: B Rationale: Generalizations should never be used to stereotype. Do not assume that the patient fits the generalizations assigned to his or her culture group. 19. Patients from which cultural group would expect you to ask about their families and interests and to maintain a friendly manner before focusing on health‐related issues? a. Middle Eastern b. Anglo‐American c. Eastern European d. Hispanic/Latino Correct: D Rationale: Hispanic/Latinos place high value on friendly interpersonal interaction. It is appropriate to maintain a friendly manner with Latino patients. 20. The practice of Western medicine recognizes and adheres to a hierarchical system. In this system, which characteristics support a provider’s status? a. Education and experience b. Professional accomplishments c. Earning potential d. A and B e. A and C f. B and C g. All of the above Correct: D Rationale: In Western medicine, the provider’s status is based on education, experience, and professional accomplishments.