Human Reproduction, Vol.28, No.7 pp. 1890– 1898, 2013
Advanced Access publication on May 12, 2013 doi:10.1093/humrep/det112
ORIGINAL ARTICLE Reproductive endocrinology
Paracetamol, aspirin and indomethacin
display endocrine disrupting properties
in the adult human testis in vitro
O. Albert 1,2, C. Desdoits-Lethimonier 1,2, L. Lesné 1,2, A. Legrand 1,2,
F. Guillé 3, K. Bensalah 4, N. Dejucq-Rainsford 1,2, and B. Jégou 1,2,5,*
1
Inserm (Institut national de la santé et de la recherche médicale), IRSET, U1085, Campus de Beaulieu, Rennes CEDEX F-35042, France
Université de Rennes I, Campus de Beaulieu, Rennes CEDEX F-35042, France 3Centre de Lutte contre le cancer Eugène Marquis, rue de la
Bataille Flandres-Dunkerque CS44229, Rennes CEDEX F-35042, France 4Centre Hospitalier Universitaire de Pontchaillou, Service Urologie,
2 rue Henri Le Guilloux, Rennes CEDEX 9 35033, France 5EHESP School of Public Health, Rennes CEDEX F-35043, France
2
Submitted on January 11, 2013; resubmitted on March 15, 2013; accepted on March 20, 2013
study question: Do mild analgesics affect the endocrine system of the human adult testis?
summary answer: Mild analgesics induce multiple endocrine disturbances in the human adult testis in vitro.
what is known already: Mild analgesics have recently been incriminated as potential endocrine disruptors. Studies of the effects
of these widely used molecules on the androgenic status of men are limited and somewhat contradictory. This prompted us to investigate
whether these compounds could alter the adult human testicular function. We therefore assessed in parallel the effects of paracetamol,
aspirin and indomethacin on organo-cultured adult human testis and on the NCI-H295R steroid-producing human cell line.
study design, size, duration: Adult human testis explants or NCI-H295R adrenocortical human cells were cultured with 1024
or 1025 M paracetamol, aspirin or indomethacin for 24 –48 h. The effect of 1025 M ketoconazole, used as an anti-androgenic reference
molecule, was also assessed.
participants/materials, setting, methods: Testes were obtained from prostate cancer patients, who had not received
any hormone therapy. The protocol was approved by the local ethics committee of Rennes, France and informed consent was given by the
donors. Only testes displaying spermatogenesis, as assessed by transillumination, were used in this study. Hormone levels in the culture
media were determined by radioimmunoassay (testosterone, insulin-like factor 3), Enzyme-Linked Immunosorbent Assay (inhibin B) or
Enzyme Immunosorbent Assay [prostaglandin (PG) D2, and PGE2]. Tissues were observed and cells counted using classical immunohistochemical methods.
main results and the role of chance: The three mild analgesics caused multiple endocrine disturbances in the adult
human testis. This was particularly apparent in the interstitial compartment. Effective doses were in the same range as those measured in
blood plasma following standard analgesic treatment. The production of testosterone and insulin-like factor 3 by Leydig cells was altered
by exposure to all these drugs. Inhibin B production by Sertoli cells was marginally affected by aspirin only. Our experiments also revealed
that mild analgesics display direct anti-PG activity, which varied depending on the drug used, the dose and the duration of exposure. Nevertheless, associations between the alteration of the PG and testosterone profiles were not systematically observed, suggesting that a combination of mechanisms of endocrine disruption is at play.
limitations, reasons for caution: Our studies were performed in vitro.
wider implications of the findings: We provide the first evidence that direct exposure to mild analgesics can result in
multiple endocrine disturbances in the human adult testis. Caution, concerning the consumption of mild analgesics by men, should be
strengthened, particularly in high-risk population subgroups such as elite athletes.
study funding/competing interest(s): This work was funded by Inserm (Institut national de la santé et de la recherche
médicale), EHESP (Ecole des Hautes Etudes en Santé Publique), Ministère de l’Enseignement Supérieur et de la Recherche, Région Bretagne
and Agence Nationale de sécurité du médicament et des produits de santé (IMPACTESTIS, Project no. AAP-2012-037). The authors declare
they have no competing interests, be it financial, personal or professional.
& The Author 2013. Published by Oxford University Press on behalf of the European Society of Human Reproduction and Embryology. All rights reserved.
For Permissions, please email: journals.permissions@oup.com
Downloaded from http://humrep.oxfordjournals.org/ by guest on September 10, 2015
*Correspondence address. Tel: +33-2-23-23-69-11; Fax: +33-2-23-23-50-55; E-mail: bernard.jegou@inserm.fr
1891
Mild analgesics and the adult human testis
Key words: paracetamol / aspirin / indomethacin / human testis / endocrine disruption
Introduction
Materials and Methods
Organotypic cultures of human testis
explants
The protocol was approved by the local ethics committee of Rennes,
France and informed consent was given by the donors. Testes were
Immunostaining
Immunohistochemistry with formaldehyde-fixed, paraffin-embedded
tissues was used to estimate the number of Leydig cells/1000 interstitial
cells in control and treated explants. Testis explant sections (5 mm
thick) were deparaffinized, rehydrated, antigen-retrieved for 20 min at
+808C in EGTA buffer (pH 9), and washed three times in 0.05 mol/l Trisbuffered saline (TBS, pH 7.4). Endogenous peroxidases were inactivated
with a 10-min treatment in TBS – 0.3% H2O2. Non-specific binding sites
were blocked in TBS supplemented with 10% goat serum (Sigma-Aldrich,
Saint Louis, MO, USA) and the samples were incubated overnight at +48C
with the primary rabbit antibody directed against CYP11A1 (Sigma Prestige Antibodies, Saint Louis, MO, USA) diluted 1/250 in DAKO REAL
antibody diluent (DAKO A/S, Trappes, France). The slides were rinsed
several times in TBS and incubated for 1 h with a biotinylated goat antirabbit secondary antibody (1/500; DAKO A/S) then for 20 min with a
Vectastain Avidin:Biotinylated enzyme Complex (ABC; Vector, Burlingame, USA). Bound antibody was visualized as a brown precipitate of
3,3′ -diaminobenzidine (DAKO). The reaction was stopped by immersion
in water. To exclude peritubular cells from interstitial cells, the peritubular
cells were labeled with a smooth muscle actin primary antibody produced
in mouse (DAKO A/S) and diluted 1/500. After a 2-h incubation at 378C,
the slides were rinsed three times in TBS, incubated with an anti-mouse
secondary antibody produced in rabbit (DAKO A/S) at room temperature
Downloaded from http://humrep.oxfordjournals.org/ by guest on September 10, 2015
Paracetamol and over-the-counter non-steroidal anti-inflammatory
drugs (NSAIDs), herein referred to collectively as mild analgesics,
are among the most sold pharmaceutical drugs worldwide. These
molecules have excellent reputations within the general population
and are widely used for self-medication and prophylaxis, and are
also present in the environment (Verlicchi et al., 2012). However,
they are often mis- or over-consumed, including in population subgroups, such as elite athletes, to prevent pain and treat injuries (Gorsline and Kaeding, 2005; Ziltener et al., 2010). The risks associated with
the misuse of mild analgesics, such as hepatotoxicity (Bessone, 2010),
cardiovascular side effects (Chan et al., 2006) or inducing asthma (Jenkins
et al., 2004) are well known. Recent findings indicate that paracetamol
and NSAIDs have endocrine disruptive potential during fetal life.
Indeed, several independent epidemiological studies indicate the existence of a significant association between the intake of paracetamol
alone or combined with NSAIDs during pregnancy, and an increased
risk of cryptorchidism in newborn boys (Berkowitz and Lapinski, 1996;
Jensen et al., 2010; Kristensen et al., 2011b; Snijder et al., 2012). Mild
analgesics were also found to display anti-androgenic effects in the rat
fetal testis both in utero and in vitro (Kristensen et al., 2011a,b).
During adulthood, a number of deleterious effects of aspirin and
NSAIDs exposure on testicular function have also been described.
Indeed, abnormal spermatogenesis was observed in adult rats following
aspirin exposure (Scott and Persaud, 1977; Biswas et al., 1978). Prolonged (.15 days) administration of 1–2.5 mg/day indomethacin
(Saksena et al., 1975) or of 5 mg/100 g body weight aspirin (Didolkar
et al., 1980) to adult rats also decreased their plasma testosterone
levels and, respectively, decreased or increased LH secretion. In mice,
administration of 600 mg/kg body weight paracetamol caused degeneration of spermatids as early as 6-h post-treatment (Placke et al., 1987).
In a placebo-controlled single-blinded study with normal male
volunteers, aspirin treatment inhibited the human androgenic response to human chorionic gonadotrophin (hCG; Conte et al.,
1999). Originally designed to explore the involvement of cyclooxygenase (COX) metabolites in the regulation of human testis steroidogenesis, this study implicates prostaglandins (PGs) and COX inhibitors in
the observed endocrine disruption, and echoes recent findings
showing that many putative endocrine disruptors inhibit PG synthesis
(Kristensen et al., 2011a).
Here, the direct effects of paracetamol, aspirin and indomethacin
exposure on the adult human testis were investigated. To this end,
an experimental approach recently validated for the study of endocrine disruption, based on the analysis of both whole human testis
in organotypic culture and the NCI-H295R human steroidogenic cell
line (Desdoits-Lethimonier et al., 2012), was used.
obtained from prostate cancer patients (average age: 79.8 + 5.6 years),
who had not received any hormone therapy. Testes were transported
on ice immediately following an orchidectomy and processed as previously
described (Roulet et al., 2006; Desdoits-Lethimonier et al., 2012). Only
testes displaying spermatogenesis, as assessed by transillumination, were
used in this study.
The following procedure is referred to as TEXAS for Testis EXplants
ASsay. Testicular tissues were fragmented in phosphate-buffered saline
into explants of about 3 mm3. In each well of 12-well plates, four explants
were placed onto a polyethylene terephthalate insert (Falcon Labware;
Becton Dickinson, Lincoln Park, NJ, USA) and cultured in 1 ml of
medium at the air/liquid interface (Dulbecco’s Minimal Essential
Medium; Sigma-Aldrich, Saint Quentin Fallavier, France) as described in
Roulet et al. (2006). The testis explants were cultured in media containing
1025 – 1024 M of paracetamol (purity . 99%; Sigma-Aldrich), aspirin
(purity . 99%; Sigma-Aldrich) or indomethacin (purity . 99%; SigmaAldrich) in 0.1% dimethyl sulphoxide (DMSO), or 0.1% DMSO as a
control. Ketoconazole (Sigma-Aldrich), an orally active broad-spectrum
anti-fungal agent of the imidazole family used in the treatment of skin
and anti-fungal infections, was also used at 1025 M in 0.1% DMSO as a
positive control (Desdoits-Lethimonier et al., 2012). For each donor
explants were exposed to all the pharmaceutical drugs of interest and at
all concentrations indicated; each condition was replicated at least six
times for testosterone, at least four times for INSL3, inhibin B at 48 h
and PGD2, and three times for inhibin B 24 h and PGE2. The explants
were incubated for 24 or 48 h in a humidified atmosphere containing
5% CO2 at 348C. The media were then collected, divided into three aliquots and stored at 2808C until hormone assays and analysis. On the
day of collection, four testis explants were either fixed in neutral buffer
with 4% formaldehyde (immunochemistry) or in Bouin’s fixative for 2 h
at +48C. For in situ analyses, testicular explants were dehydrated by
immersion in a series of graduated alcohol concentrations (Citadelw,
Thermo Fisher Scientific), embedded in paraffin, sliced into 5-mm thick
sections and stored at +48C until immunostaining.
1892
for 1 h, and then for 15 min with the ABC complex. Bound antibody was
visualized in red with 3-amino-9-ethyl carbazole (Beckman Coulter, Marseille, France). Sections were counterstained with hematoxylin and
mounted in aqueous mount. CYP11A1-immunopositive cells and interstitial cells were counted in 500 fields using the Computer-Assisted Stereology Toolbox (CAST) Grid system (Olympus, Copenhagen, Denmark) with
a light microscope (Olympus BX S1).
Culture of the NCI-H295R cell line
and treatment
Measurement of testosterone levels
Testosterone in the culture media of both culture systems was assayed
in duplicate using a commercial radioimmunoassay (RIA) based on
competitive binding with I125-labeled testosterone (Immunotech,
Beckman Coulter, Villepinte, France), according to the manufacturer’s
recommendations. Standard curve interpolation was used and the
results were expressed in nanograms per milliliter. The intra- and interassay coefficients of variation for serum samples were ≤8.6 and 11.9%,
respectively. Testis explants produced an average + SEM of 7.7 +
1.15 ng/ml/explant testosterone after 24 h of culture, and 12.05 +
1.39 ng/ml/explant after 48 h. Control NCI-H295R cells produced an
average of 1.21 + 0.0.08 ng/ml/well after 24 h of culture, and 2.08 +
0.13 ng/ml/well after 48 h.
Measurement of INSL3 levels
INSL3 in the culture media of the TEXAS was assayed in duplicate using a
commercial RIA (RK-035-27, Phoenix France, Strasbourg, France) according to the manufacturer’s instructions. Each sample was diluted 4-fold in
RIA buffer prior to RIA reactions. The intra- and inter-assay coefficients
of variation were ≤15 and 7%, respectively, and the lower limit of detection was 20.17 pg/ml. Control testis explants produced an average of
0.53 + 0.66 ng/ml/explant INSL3 after 24 h of culture, and 0.39 +
0.52 ng/ml/explant after 48 h.
Measurement of inhibin B levels
Inhibin B was assayed in the culture media of the TEXAS using a commercial Enzyme-linked immunosorbent Assay (ELISA) kit (DSL-10-84100
Active, Beckman Coulter, Villepinte, France) according to the manufacturer’s instructions. Each sample was diluted 2-fold in sample diluent
solution prior to reactions. The intra- and inter-assay coefficients of variation for serum samples were ≤5.6 and 7.6%, respectively. Control testis
explants produced an average of 0.18 + 0.17 ng/ml/explant inhibin B
after 24 h of culture, and 0.30 + 0.36 ng/ml/explant after 48 h.
Measurement of PG levels
PGs D2 and E2 were assayed in the culture media of the TEXAS using
commercial Enzyme Immunosorbent Assay (EIA) kits (PGD2-MOX EIA
Kit, no. 512011 and PGE2 EIA Kit Monoclonal, no. 514010, respectively,
Cayman, MI, USA) according to the manufacturer’s instructions. Each
sample was diluted 3 to 5-fold in sample diluent solution prior to
reactions. The lower limits of detection were 3.1 and 15 pg/ml,
respectively. Control testis explants produced an average of 0.024 +
0.018 ng/ml/explant PGD2 and 1.33 + 1.52 ng/ml/explant PGE2 after
24 h of culture.
Statistical analysis
All reported values are means + SEM. For the two culture systems, values
are expressed as percentages of the control value: each replicate in each
condition was expressed as a percentage of the mean of control values,
and then the mean for each condition was calculated for each donor.
Finally, the mean + SEM of all donors was calculated and were analyzed
with the non-parametric signed-rank Mann – Whitney test. A P-value
equal or inferior to 0.05 was considered statistically significant.
Results
Mild analgesics and human testis morphology
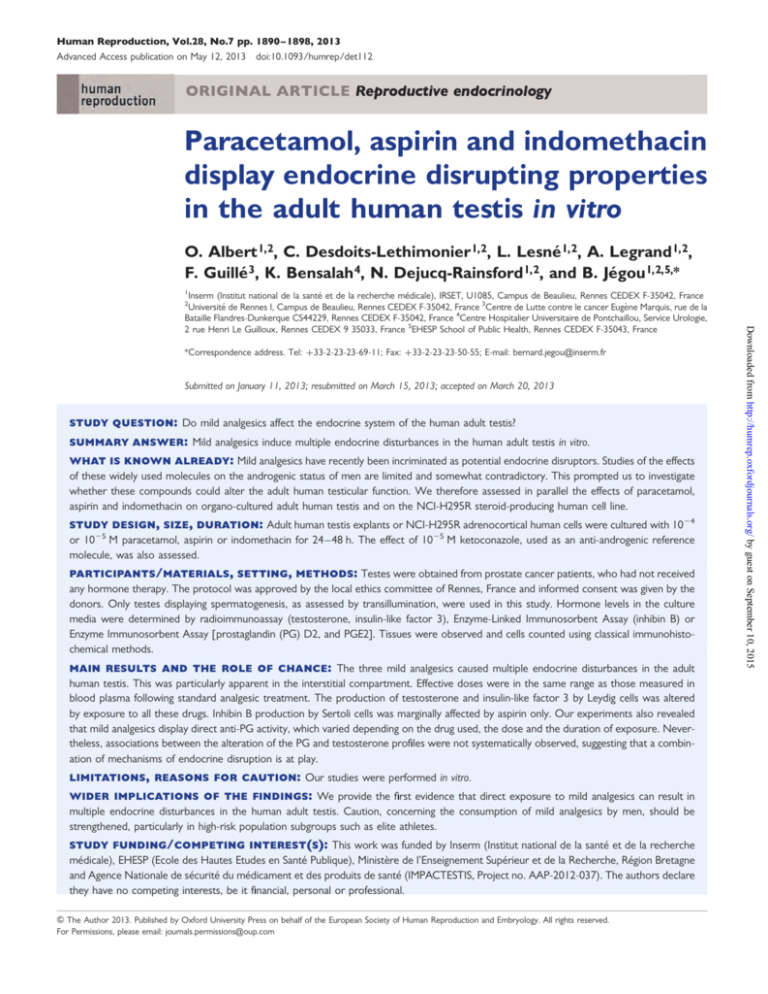
Exposure to mild analgesics had no obvious effect on the gross morphology of testis explants (Fig. 1). None of the treatments caused any
global alteration of the seminiferous epithelium. Cell counts indicated
that none of the treatments with mild analgesics significantly decreased
the Leydig cell number (Fig. 2): after 24 h of exposure, the number of
Leydig cells was significantly higher in samples treated with 1024 M
aspirin and 1025 M indomethacin than in controls (by 29 and 22%, respectively; P , 0.05).
Mild analgesics and testosterone production
by the human testis
When all the six independent experiments were taken into consideration, treatment with 1025 M ketoconazole significantly decreased
testosterone concentrations in the culture medium by 60% after 24 h,
and by 69% after 48 h of exposure relative to control values (Fig. 3;
P , 0.01). Exposure to 1025 and 1024 M paracetamol significantly
decreased testosterone secretion after 24 h by 18 and 30%, respectively
(Fig. 3; P , 0.01); 1024 M indomethacin also significantly decreased
testosterone production after 24 h by 14% (Fig. 3; P , 0.05). A 24-h
exposure to 1025 M aspirin and indomethacin induced decreasing
trends of testosterone production by 19 and 12%, respectively, which
did not reach statistical significance at P , 0.05 (Fig. 3). Following 48 h
of exposure, none of the mild analgesics significantly decreased
testosterone concentrations at the doses tested (Fig. 3).
When the experiments were considered individually, in each of the
six independent experiments, the majority of the samples exposed for
24 h to the analgesics responded by a testosterone production that
was below the control level (Supplementary data S1). After 48 h of
exposure to the analgesics, if a majority of samples exposed to the
Downloaded from http://humrep.oxfordjournals.org/ by guest on September 10, 2015
To reinforce the TEXAS approach as recently shown (DesdoitsLethimonier et al., 2012), we also used the following procedure which is
referred to as CELIAS for CEll LIne ASsay. The NCI-H295R human adrenocortical cell line, which expresses steroidogenic enzymes and produces
steroids, has previously been used to study anti-androgenic compounds
(Gracia et al., 2006) and was provided by Dr Feige (INSERM U878,
Grenoble, France). As previously described by Desdoits et al. (2012),
cells were grown for 1 –10 passages in 75-cm2 flasks with 10 ml of supplemented medium at 378C under a 5% CO2 atmosphere. The supplemented medium was RPMI medium 1640 (RPMI, Roswell Parrk Memorial
Institure; Sigma-Aldrich) with 1% ITS plus (ITS: Insulin, human Tranferrin
and Selenous acid; Becton Dickinson, Le Pont de Claix, France), 2%
fetal bovine serum (Eurobio, Courtaboeuf, France) and antibiotics. The
cells were then sub-cultured at a density of 106 cells/well in a 12-well
culture plate, and were incubated for 5 days. The medium was then
replaced with 1 ml of serum-free RPMI 1640 containing 0.01% bovine
serum albumin and 0.1% DMSO or 1025 M ketoconazole, or 1025 –
1024 M paracetamol, aspirin or indomethacin in 0.1% DMSO and the
culture continued for 24 or 48 h. The media were collected and divided
into three aliquots, which were stored at 2808C until hormone assays.
Albert et al.
Mild analgesics and the adult human testis
1893
conazole (B) or of 1025 M or 1024 M concentration of the test compound, namely paracetamol (C and D, respectively), aspirin (E and F, respectively) or indomethacin (G and H, respectively). Testis explants were fixed in Bouin fixative and stained with hematoxilin – eosin. No change in the gross
morphology of the testis was apparent.
Figure 2 Effects of a 24-h exposure to 1025 M ketoconazole (KT),
or 1025 or 1024 M paracetamol, aspirin or indomethacin on the
number of Leydig cells in human testicular explants. Each bar represents the mean + SEM of three independent experiments with
tissues from different donors. The number of Cyp11A1+ cells/
1000 interstitial cells is expressed as a percentage of the control
value; the difference from control (100%) is given in brackets where
it is significant. *P , 0.05 by the non-parametric signed-rank Mann –
Whitney test on unpaired data. NS, not significant.
Figure 3 Time- and dose-dependent effects of 1025 M ketoconazole (KT), and 1025 and 1024 M paracetamol, aspirin or indomethacin on testosterone production by human testicular explants. Each
bar represents the mean + SEM of six independent experiments
with samples from different donors. The difference from control
(100%) is given in brackets where it is significant. *P , 0.05,
**P , 0.01 by non-parametric signed-rank Mann– Whitney test on
unpaired data. NS, not significant.
Downloaded from http://humrep.oxfordjournals.org/ by guest on September 10, 2015
Figure 1 Light micrographs of areas of human testis explants after 48 h in culture in the presence of 1025 M DMSO (Control; A), 1025 M keto-
1894
Albert et al.
analgesics displayed a production of testosterone lower than the
control level in a majority of experiments (4 out of 6), the patterns
of responses were generally more contrasted than at 24 h, and
larger intra- and inter-individual variations in testosterone production
were seen (Supplementary data S1). This explained why when all the
data of 48 h of exposure were globally analyzed, no significant differences were seen with the analgesics (Fig. 3).
Mild analgesics and testosterone production
by the NCI-H295R cell line
Figure 5 Effects of 1025 M ketoconazole (KT), or 1025 – 1024 M
paracetamol, aspirin or indomethacin on INSL3 production by
human testicular explants. Values are means + SEM of four independent experiments with samples from different donors. The difference
from control (100%) is given in brackets where it is significant.
*P , 0.05 by non-parametric signed-rank Mann –Whitney test on unpaired data. NS, not significant.
Mild analgesics and INSL3 production
by the human testis
Neither ketoconazole nor paracetamol had a significant effect on
INSL3 production (Fig. 5). INSL3 levels were 22 and 33% lower following 24 h of exposure to 1025 and 1024 M aspirin, respectively,
than in controls (Fig. 5; P , 0.05). A 24-h exposure to 1024 M indomethacin also significantly decreased INSL3 production by 34% (Fig. 5;
P , 0.05). A 24-h exposure to 1025 M indomethacin did not significantly reduce INSL3 production (216%, NS at P , 0.05). INSL3 concentrations after 48 h of exposure to any of the treatments were not
significantly different from control values.
Mild analgesics and inhibin B production
by the human testis
Exposure for 24 h to 1025 M aspirin decreased inhibin B production
by 11% (P , 0.05). None of the other treatments had a significant
effect on inhibin B secretion by testis explants in culture, irrespective
of the dose and the time of exposure tested (Fig. 6).
Mild analgesics and PG synthesis
by the human testis
Figure 4 Time- and dose-dependent effects of 1025 M ketocona25
24
zole (KT), 10 and 10 M paracetamol, aspirin or indomethacin on
testosterone production by NCI-H295R cells. The cells were treated
for 24 or 48 h with 1025 M ketoconazole (KT), or 1025 – 1024 M
paracetamol, aspirin or indomethacin. Values for testosterone are
expressed as percentages of the control value. Each bar represents
the mean + SEM of 3 (24 h) to 6 (48 h) experiments. The difference
from control (100%) is given in brackets where it is significant.
*P , 0.05, **P , 0.01 and ***P , 0.001 by non-parametric
signed-rank Mann– Whitney test on unpaired data. NS, not significant;
ND, not detected.
Following 24 h of exposure to 1025 M ketoconazole, PGD2 concentrations were more than doubled compared with the control values,
and PGE2 concentrations were 78% higher (Fig. 7; P , 0.05). After
24 h, all of the mild analgesic treatments, except for 1025 M paracetamol, resulted in significantly lower than control concentrations of both
PGD2 (by 28% for 1024 M paracetamol; by 28 and 57% for 1025 and
1024 M aspirin, respectively; by 79 and 75% for 1025 and 1024 M
indomethacin, respectively; P , 0.05) and PGE2 (by 38% for 1024 M
paracetamol; by 29 and 65% for 1025 and 1024 M aspirin, respectively; by 95 and 96% for 1025 and 1024 M indomethacin, respectively;
P , 0.05).
Downloaded from http://humrep.oxfordjournals.org/ by guest on September 10, 2015
Testosterone production was inhibited in a time-dependent manner
by 1025 M ketoconazole (Fig. 4). Exposure to 1025 M paracetamol
inhibited testosterone production by 13% after 48 h (P , 0.01), but
testosterone levels after 24 h were not significantly different from
those in controls. In contrast, following 24 h of treatment with
1024 M paracetamol, the testosterone concentration was significantly
lower than in controls (210%; P , 0.05). After 48 h, the difference
was not significant anymore (212%; Fig. 4). Exposure to 1025 and
1024 M aspirin significantly reduced testosterone production after
24 h (by 18 and 17%, respectively; P , 0.05) and after 48 h (by
14%; P , 0.001 and 12%; P , 0.05, respectively). Testosterone production was markedly and significantly reduced by both 1025 and
1024 M indomethacin after 24 h (by 31 and 37%, respectively; P ,
0.05) and after 48 h (by 41%; P , 0.001 and 43%; P , 0.05,
respectively).
1895
Mild analgesics and the adult human testis
Discussion
Figure 6 Effects of 1025 M ketoconazole (KT), or 1025 – 1024 M
Figure 7 Effects of a 24-h exposure to 1025 M ketoconazole (KT),
or 1025 – 1024 M paracetamol, aspirin or indomethacin on PGD2 and
PGE2 productions by human testicular explants. Values are means +
SEM of 3 (PGE2) or 4 (PGD2) independent experiments with samples
from different donors. The difference from control (100%) is given in
brackets where it is significant. *P , 0.05 by non-parametric
signed-rank Mann –Whitney test on unpaired data. NS, not significant.
Downloaded from http://humrep.oxfordjournals.org/ by guest on September 10, 2015
paracetamol, aspirin or indomethacin on inhibin B production by
human testicular explants. Values are means + SEM of 3 (24 h) or
4 (48 h) independent experiments with samples from different
donors. The difference from control (100%) is given in brackets
where it is significant. *P , 0.05 by non-parametric signed-rank
Mann –Whitney test on unpaired data. NS, not significant.
Mild analgesics have recently been incriminated by several epidemiological and toxicological studies to act as endocrine disruptors
during human fetal life (Berkowitz and Lapinski, 1996; Jensen et al.,
2010; Kristensen et al., 2011b, 2012; Snijder et al., 2012).
We report that mild analgesics at pharmaceutical doses can directly
cause multiple endocrine disturbances in the human adult testis, particularly in the interstitial compartment. The three molecules tested
exerted both anti-androgenic and anti-prostaglandinic effects,
somehow differing according to their nature, and to some extent,
according to their dose. Paracetamol appeared to be the weaker inhibitor of PG secretion, and not to disrupt INSL3 production,
whereas INSL3 production was inhibited by aspirin and 1024 M indomethacin. Consistent with the anti-androgenic effect on cultured
human testis, and as a validation for these observations, we found
that mild analgesics also reduced steroidogenesis by 10–43% from
the control values in human steroid-producing NCI-H295R cells.
According to the literature, a standard dose of 1 g paracetamol
results in the serum concentration in adult men peaking 48 min after
administration at 11 mg/ml, which corresponds to 7.3 × 1025 M
(Prescott, 1980). A 600 mg dose intake of aspirin per os was found
to lead to a maximal serum concentration of 2.1024 M in adult men
(Dalvi et al., 1985). Two hours after a single oral administration of
100 mg indomethacin, the plasma concentration in healthy adult
men peaks at 6 mg/ml, which corresponds to 1.7 1025 M (Emori
et al., 1976). As the testicular concentrations of paracetamol and
NSAIDs are unknown in adult men, we used these pharmacokinetic
data as an estimate of the human exposure in order to select the concentrations at which to test these mild analgesics: 1025 and 1024 M.
For all doses and drugs, the anti-androgenic effects on the testis
explants declined between 24 and 48 h of exposure. This might be
due to the increased variability in testosterone levels measured after
48 h of exposure. However, such a transient anti-androgenic effect
has similarly been observed for phthalates using the same culture
model (Desdoits-Lethimonier et al., 2012). The latter study revealed
that human adult testis explants have the ability to biotransform
some xenobiotics. Therefore, it is also possible that the mild analgesics
added to the TEXAS system were at least partly metabolized between
24 and 48 h of incubation by the explants. This issue requires further
investigation. Furthermore, it cannot be excluded that an hydrolysis of
aspirin in water may also occur to explain the fading of its effects
between 24 and 48 h, but this remains to be assessed.
In our experiments, the direct exposure of the human testis to mild
analgesics had no effect on the gross morphology of the testis. As mild
analgesics did not impact the number of Leydig cells, the hormonal disruptions observed cannot be attributed to their death. In contrast,
1024 M aspirin and 1025 M indomethacin induced an apparent increase in the relative proportion of Leydig cells in the interstitial
tissue, the origin of which is unknown.
The well-documented anti-inflammatory properties of aspirin and
indomethacin result from their specific ability to inhibit the COX
site of Prostaglandin H2 synthetase (PGHS), an enzyme that transforms arachidonic acid into a number of PG inflammation mediators
(Vane and Botting, 1996). Extractions and RIAs of PGE and PGF2a
have demonstrated the expression of the PG system within the
adult human testis (Carpenter et al., 1978), and both PG receptors
1896
INSL3, an hormone responsible for the first phase of testicular
descent in mammals, is produced by both fetal and adult Leydig
cells (Nef and Parada, 1999; Bay et al., 2011). Unlike testosterone
and PGs, which were affected by all the treatments, INSL3 production
was only significantly decreased by the two concentrations of aspirin
tested and by the higher concentration of indomethacin. This is the
first report of INSL3 disruption in adult human testis following exposure to chemical agents: in the same experimental setting, the effects of
phthalates on Leydig cells remained restricted to their steroidogenic
capabilities (Desdoits-Lethimonier et al., 2012). The role of INSL3 in
normal adult testicular physiology is poorly understood, despite its
constitutive expression (Mitchell et al., 2012). INSL3 may play a role
in germ cell maintenance, affect other tissues such as prostate,
kidney or thyroid (for review, Ivell and Anand-Ivell, 2009) and contribute to bone metabolism (Ferlin et al., 2008). Thus, the consequences
of endocrine disruption that affects the ability of Leydig cells to
produce INSL3 will remain obscure until the role(s) of this hormone
is (are) better known.
The only hormone that remained almost totally unaffected by a
direct exposure to mild analgesics was the Sertoli cell product
inhibin B. Indeed, the inhibition of its production by a 24-h exposure
to 1025 M aspirin was weak (211%; Fig. 6). In similar conditions,
inhibin B production was unaffected by the exposure to phthalates
(Desdoits-Lethimonier et al., 2012). Although PGE2 and PGI2 are
synthesized by Sertoli cells in adult rats (Cooper and Carpenter,
1987), before this work their presence in adult human Sertoli cells
has never been explored, and nothing is known about their link, if
any, with Sertoli cell products. Inhibin B secretion by rat Sertoli cells
is regulated by the inflammation mediator IL-1b (Okuma et al.,
2005), and IL-1b induces COX-2 in various tissues, including Leydig
cells in infertile men (Matzkin et al., 2010); therefore, the aspirinspecific inhibition of inhibin B production may be a consequence of
a putative link between the PG system and inhibin B production by
Sertoli cells. However, this suggestion is speculative at this stage.
We report the first evidence that direct exposure to mild analgesics
can result in several endocrine disturbances, causing an unbalance in the
hormonal activity of the adult testis in short-term culture. The active
doses of analgesics were of the same order of magnitude as plasma
concentrations during standard analgesic intake. Our study demonstrates that the testicular PG system is highly susceptible to these molecules. However, the interactions between different testicular hormones
under COX-disruptive conditions, in particular the relationship between
PGs and testosterone, remain unclear. Our findings are consistent with
the concerns recently raised both by epidemiological studies on mild
analgesic consumption and by in vitro experiments on the potential
targeting of PGs by endocrine disruptors. The present in vitro results
highlight the risks associated with the abusive use of mild analgesics
for the testicular endocrine system in men.
Supplementary data
Supplementary data are available at http://humrep.oxfordjournals.org/.
Acknowledgements
We thank Damien Le Bot for technical support and Cécile Chevrier
for statistical advice.
Downloaded from http://humrep.oxfordjournals.org/ by guest on September 10, 2015
and synthetases have been found in human Leydig cells (Tokugawa
et al., 1998; Schell et al., 2007). PGs are also produced by the adult
rat total testis (Carpenter et al., 1974) and Sertoli cells (Cooper and
Carpenter, 1987), and Sertoli cells express PGE2 and PGF2 receptors
(Ishikawa and Morris, 2006). PGs are also abundant in human semen,
but are believed to originate mostly from the seminal vesicles
(Gerozissis et al., 1982).
The implication of paracetamol in the PG biosynthesis pathway
is less obvious than that of aspirin and indomethacin. Paracetamol
may specifically inhibit the peroxidase site of PGHS (Anderson,
2008), but its mechanism of action is still controversial. It was recently suggested that paracetamol may act on the endocannabinoid system via the TRPA1 receptor pathway (Andersson et al.,
2011), and this would explain why a higher concentration of paracetamol than of aspirin or indomethacin was needed to affect PG
synthesis.
A few experiments have explored the existence of a relationship
between PG production and steroidogenesis in both rats and primates. Several studies based on in vivo administration of PGE2 and/
or PGF2a reported an inhibition of steroidogenesis in the adult rat
(Saksena et al., 1973; Didolkar et al., 1981; Fuchs and Chantharaksri,
1981; Sawada et al., 1994; Gunnarsson et al., 2004) and more specifically of the androgenic response to LH (Fuchs and Chantharaksri,
1981; Marinero et al., 1996) or hCG (Romanelli et al., 1995).
However, injection of PGF2a into male rhesus monkeys was followed
by an abrupt and almost immediate increase in the production of both
testosterone and LH (Kimball et al., 1979). To date, very little is
known about the relationship between the PG system and steroidogenesis in men. Healthy male volunteers treated with 800 mg of
aspirin daily for 7 days showed a decreased androgenic response to
hCG stimulation (Conte et al., 1999). Oligospermic patients given
25– 100 mg indomethacin for 30 –90 days displayed increased
plasma FSH and LH concentrations and decreased plasma testosterone concentrations (Barkay et al., 1984). In contrast, healthy young
men treated with 25 mg of indomethacin for 14 days displayed unchanged testosterone, LH and FSH levels (Knuth et al., 1989). The
relationships between the PG system and steroidogenesis, therefore,
seem to be governed by complex hormonal balance mechanisms
involving gonadotrophins, which remain to be elucidated. The poor
or unresponsiveness of the human testis to LH or hCG stimulation
in vitro (Huhtaniemi et al., 1982; Roulet et al., 2006)—attributed to
the lower numbers of LH receptors present in the human compared
with the rat testis (Huhtaniemi et al., 1982)—prevented us from exploring this aspect of testicular physiology in response to mild
analgesics.
In the TEXAS system, the testosterone decrease induced by mild
analgesics appeared to be uncoupled from PG production. Indeed, although aspirin and indomethacin treatments were associated with
major anti-PG effects, only paracetamol and 1024 M indomethacin significantly inhibited testosterone production. The opposite occurred
with 1025 M ketoconazole, for which a sharp inhibition of testosterone production and a substantial increase of PG synthesis were
observed. Whether or not this increase in PG synthesis was a consequence of the germ cell loss induced by ketoconazole remains to be
elucidated. In any case, it cannot be excluded that mild analgesics
could act on steroidogenesis via both a PG-dependent and independent pathway.
Albert et al.
Mild analgesics and the adult human testis
Authors’ roles
B.J. and N.D-R. designed the research; O.A., C.D. and L.L. performed
the research; F.G. and K.B. supervised and performed orchidectomies;
A.L. contributed to critical discussion. All authors contributed to critically reviewing the draft manuscript. All authors saw and approved the
final version of the report.
Funding
This work was funded by Inserm (Institut national de la santé et de la
recherche médicale), EHESP (Ecole des Hautes Etudes en Santé Publique), Ministère de l’Enseignement Supérieur et de la Recherche,
Région Bretagne and Agence Nationale de Sécurité du Médicament
et des produits de santé (IMPACTESTIS, Project no. AAP-2012-037).
The authors declare they have no competing interests, be it financial,
personal or professional.
References
Anderson BJ. Paracetamol (Acetaminophen): mechanisms of action.
Paediatr Anaesth 2008;18:915 – 921.
Andersson DA, Gentry C, Alenmyr L, Killander D, Lewis SE, Andersson A,
Bucher B, Galzi JL, Sterner O, Bevan S et al. TRPA1 mediates spinal
antinociception induced by acetaminophen and the cannabinoid
Delta(9)-tetrahydrocannabiorcol. Nat Commun 2011;2:551.
Barkay J, Harpaz-Kerpel S, Ben-Ezra S, Gordon S, Zuckerman H. The
prostaglandin inhibitor effect of antiinflammatory drugs in the therapy
of male infertility. Fertil Steril 1984;42:406 – 411.
Bay K, Main KM, Toppari J, Skakkebaek NE. Testicular descent: INSL3,
testosterone, genes and the intrauterine milieu. Nat Rev Urol 2011;
8:187 – 196.
Berkowitz GS, Lapinski RH. Risk factors for cryptorchidism: a nested
case-control study. Paediatr Perinat Epidemiol 1996;10:39 – 51.
Bessone F. Non-steroidal anti-inflammatory drugs: what is the actual risk of
liver damage? World J Gastroenterol 2010;16:5651 – 5661.
Biswas NM, Sanyal S, Patra PB. Antispermatogenic effect of aspirin and its
prevention by prostaglandin E2. Andrologia 1978;10:137 – 141.
Carpenter MP. Prostaglandins of rat testis. Lipids 1974;9:397 – 406.
Carpenter MP, Robinson RD, Thuy LP. Prostaglandin metabolism by
human testis. Lipids 1978;13:308 – 311.
Chan AT, Manson JE, Albert CM, Chae CU, Rexrode KM, Curhan GC,
Rimm EB, Willett WC, Fuchs CS. Nonsteroidal antiinflammatory
drugs, acetaminophen, and the risk of cardiovascular events.
Circulation 2006;113:1578 – 1587.
Conte D, Romanelli F, Fillo S, Guidetti L, Isidori A, Franceschi F, Latini M,
di Luigi L. Aspirin inhibits androgen response to chorionic gonadotropin
in humans. Am J Physiol 1999;277:E1032– E1037.
Cooper DR, Carpenter MP. Sertoli-cell prostaglandin synthesis. Effects of
(follitropin) differentiation and dietary vitamin E. Biochem J 1987;
241:847– 855.
Dalvi SS, Gupta KC, Pohujani SM, Vaidya AB, Satoskar RS. Bioavailability of
aspirin after oral and rectal administration in volunteers and patients
with fever. J Postgrad Med 1985;31:192– 195.
Desdoits-Lethimonier C, Albert O, Le Bizec B, Perdu E, Zalko D,
Courant F, Lesne L, Guille F, Dejucq-Rainsford N, Jegou B. Human
testis steroidogenesis is inhibited by phthalates. Hum Reprod 2012;
27:1451– 1459.
Didolkar AK, Gurjar A, Joshi UM, Sheth AR, Roychowdhury D. Effects of
aspirin on blood plasma levels of testosterone, LH and FSH in maturing
male rats. Int J Androl 1980;3:312– 318.
Didolkar AK, Gurjar A, Joshi UM, Sheth AR, Roychowdhury D. Effect of
prostaglandins A-1, E-2 and F-2 alpha on blood plasma levels of
testosterone, LH and FSH in male rats. Andrologia 1981;13:50 – 55.
Emori HW, Paulus H, Bluestone R, Champion GD, Pearson C.
Indomethacin serum concentrations in man. Effects of dosage, food,
and antacid. Ann Rheum Dis 1976;35:333 – 338.
Ferlin A, Pepe A, Gianesello L, Garolla A, Feng S, Giannini S, Zaccolo M,
Facciolli A, Morello R, Agoulnik AI et al. Mutations in the insulin-like
factor 3 receptor are associated with osteoporosis. J Bone Miner Res
2008;23:683 – 693.
Fuchs AR, Chantharaksri U. Prostaglandin F2alpha regulation of LHstimulated testosterone production in rat testis. Biol Reprod 1981;
25:492– 501.
Gerozissis K, Jouannet P, Soufir JC, Dray F. Origin of prostaglandins in
human semen. J Reprod Fertil 1982;65:401 – 404.
Gorsline RT, Kaeding CC. The use of NSAIDs and nutritional supplements
in athletes with osteoarthritis: prevalence, benefits, and consequences.
Clin Sports Med 2005;24:71– 82.
Gracia T, Hilscherova K, Jones PD, Newsted JL, Zhang X, Hecker M,
Higley EB, Sanderson JT, Yu RM, Wu RS et al. The H295R system for
evaluation of endocrine-disrupting effects. Ecotoxicol Environ Saf 2006;
65:293– 305.
Gunnarsson D, Svensson M, Selstam G, Nordberg G. Pronounced
induction of testicular PGF(2 alpha) and suppression of testosterone
by cadmium-prevention by zinc. Toxicology 2004;200:49 – 58.
Huhtaniemi I, Bolton N, Leinonen P, Kontturi M, Vihko R. Testicular
luteinizing hormone receptor content and in vitro stimulation of cyclic
adenosine 3′ ,5′ -monophosphate and steroid production: a comparison
between man and rat. J Clin Endocrinol Metab 1982;55:882 – 889.
Ishikawa T, Morris PL. A multistep kinase-based sertoli cell autocrineamplifying loop regulates prostaglandins, their receptors, and
cytokines. Endocrinology 2006;147:1706– 1716.
Ivell R, Anand-Ivell R. Biology of insulin-like factor 3 in human
reproduction. Hum Reprod Update 2009;15:463 – 476.
Jenkins C, Costello J, Hodge L. Systematic review of prevalence of aspirin
induced asthma and its implications for clinical practice. Br Med J 2004;
328:434.
Jensen MS, Rebordosa C, Thulstrup AM, Toft G, Sorensen HT, Bonde JP,
Henriksen TB, Olsen J. Maternal use of acetaminophen, ibuprofen, and
acetylsalicylic acid during pregnancy and risk of cryptorchidism.
Epidemiology 2010;21:779– 785.
Kimball FA, Kirton KT, Forbes AD, Frielink RD, Porteus SE, Wilks JW,
Mohberg NR, Turner LF. Serum FSH, LH and testosterone in the
male rhesus following prostaglandin injection. Prostaglandins 1979;
18:117– 126.
Knuth UA, Kuhne J, Crosby J, Bals-Pratsch M, Kelly RW, Nieschlag E.
Indomethacin and oxaprozin lower seminal prostaglandin levels but do
not influence sperm motion characteristics and serum hormones of
young healthy men in a placebo-controlled double-blind trial. J Androl
1989;10:108 – 119.
Kristensen DM, Skalkam ML, Audouze K, Lesne L, DesdoitsLethimonier C, Frederiksen H, Brunak S, Skakkebaek NE, Jegou B,
Hansen JB et al. Many putative endocrine disruptors inhibit
prostaglandin synthesis. Environ Health Perspect 2011a;119:534 – 541.
Kristensen DM, Hass U, Lesne L, Lottrup G, Jacobsen PR,
Desdoits-Lethimonier C, Boberg J, Petersen JH, Toppari J, Jensen TK
et al. Intrauterine exposure to mild analgesics is a risk factor for
Downloaded from http://humrep.oxfordjournals.org/ by guest on September 10, 2015
Conflict of interest
1897
1898
application for basic or clinical research. Hum Reprod 2006;
21:1564 – 1575.
Saksena SK, el-Safoury S, Bartke A. Prostaglandins E2 and F2 decrease
plasma testosterone levels in male rats. Prostaglandins 1973;4:
235 – 242.
Saksena SK, Lau IF, Bartke A, Chang MC. Effect of indomethacin on blood
plasma levels of LH and testosterone in male rats. J Reprod Fertil 1975;
42:311 – 317.
Sawada T, Asada M, Mori J. Effects of single and repeated administration of
prostaglandin F2 alpha on secretion of testosterone by male rats.
Prostaglandins 1994;47:345 – 352.
Schell C, Frungieri MB, Albrecht M, Gonzalez-Calvar SI, Kohn FM,
Calandra RS, Mayerhofer A. A prostaglandin D2 system in the human
testis. Fertil Steril 2007;88:233– 236.
Scott JE, Persaud TV. Morphological and enzyme histochemical changes in
the reproductive tract of the male rat induced by acetylsalicylic acid. Acta
Histochem 1977;60:228 – 246.
Snijder CA, Kortenkamp A, Steegers EA, Jaddoe VW, Hofman A, Hass U,
Burdorf A. Intrauterine exposure to mild analgesics during pregnancy
and the occurrence of cryptorchidism and hypospadia in the offspring:
the Generation R Study. Hum Reprod 2012;27:1191 – 1201.
Tokugawa Y, Kunishige I, Kubota Y, Shimoya K, Nobunaga T, Kimura T,
Saji F, Murata Y, Eguchi N, Oda H et al. Lipocalin-type prostaglandin
D synthase in human male reproductive organs and seminal plasma.
Biol Reprod 1998;58:600 – 607.
Vane JR, Botting RM. Mechanism of action of anti-inflammatory drugs.
Scand J Rheumatol Suppl 1996;102:9 – 21.
Verlicchi P, Al Aukidy M, Zambello E. Occurrence of pharmaceutical
compounds in urban wastewater: removal, mass load and environmental
risk after a secondary treatment—a review. Sci Total Environ 2012;
429:123–155.
Ziltener JL, Leal S, Fournier PE. Non-steroidal anti-inflammatory drugs
for athletes: an update. Ann Phys Rehabil Med 2010;53:278 – 282,
282 – 278.
Downloaded from http://humrep.oxfordjournals.org/ by guest on September 10, 2015
development of male reproductive disorders in human and rat. Hum
Reprod 2011b;26:235 – 244.
Kristensen DM, Lesne L, Le Fol V, Desdoits-Lethimonier C, DejucqRainsford N, Leffers H, Jegou B. Paracetamol (acetaminophen), aspirin
(acetylsalicylic acid) and indomethacin are anti-androgenic in the rat
foetal testis. Int J Androl 2012;35:377– 384.
Marinero MJ, Colas B, Prieto JC, Lopez-Ruiz MP. Different sites of action of
arachidonic acid on steroidogenesis in rat Leydig cells. Mol Cell Endocrinol
1996;118:193 – 200.
Matzkin ME, Mayerhofer A, Rossi SP, Gonzalez B, Gonzalez CR, GonzalezCalvar SI, Terradas C, Ponzio R, Puigdomenech E, Levalle O et al.
Cyclooxygenase-2 in testes of infertile men: evidence for the
induction of prostaglandin synthesis by interleukin-1beta. Fertil Steril
2010;94:1933 – 1936.
Mitchell RT, Childs AJ, Anderson RA, van den Driesche S, Saunders PT,
McKinnell C, Wallace WH, Kelnar CJ, Sharpe RM. Do phthalates
affect steroidogenesis by the human fetal testis? Exposure of human
fetal testis xenografts to di-n-butyl phthalate. J Clin Endocrinol Metab
2012;97:E341– E348.
Nef S, Parada LF. Cryptorchidism in mice mutant for Insl3. Nat Genet
1999;22:295 – 299.
Okuma Y, O’Connor AE, Muir JA, Stanton PG, de Kretser DM,
Hedger MP. Regulation of activin A and inhibin B secretion by
inflammatory mediators in adult rat Sertoli cell cultures. J Endocrinol
2005;187:125 – 134.
Placke ME, Wyand DS, Cohen SD. Extrahepatic lesions induced by
acetaminophen in the mouse. Toxicol Pathol 1987;15:381 – 387.
Prescott LF. Kinetics and metabolism of paracetamol and phenacetin. Br J
Clin Pharmacol 1980;10(Suppl. 2):291S –298S.
Romanelli F, Valenca M, Conte D, Isidori A, Negro-Vilar A. Arachidonic
acid and its metabolites effects on testosterone production by rat
Leydig cells. J Endocrinol Invest 1995;18:186 – 193.
Roulet V, Denis H, Staub C, Le Tortorec A, Delaleu B, Satie AP, Patard JJ,
Jegou B, Dejucq-Rainsford N. Human testis in organotypic culture:
Albert et al.