Rheumatoid Arthritis
advertisement
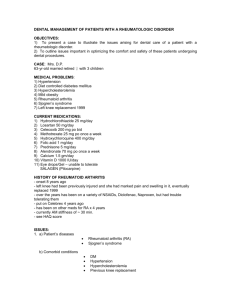
Rheumatoid Arthritis 1 Rheumatoid Arthritis Priscilla Garcia, Jennifer Klocki, Reina Ligeralde, and Dorinda Thomas Riverside Community College Rheumatoid Arthritis 2 Abstract A clinician will encounter medically compromised patients on a regular basis. The importance of medical and dental management must be taken into consideration. Patients that present with rheumatoid arthritis need to be evaluated and assessed to accommodate their specific oral health care needs. This paper will address in detail the medically compromised rheumatoid arthritis patient and the dental and medical management along with treatment planning considerations. Rheumatoid Arthritis 3 Rheumatoid Arthritis Rheumatoid arthritis (RA) is an autoimmune disease of unknown origin that is characterized by symmetric inflammation of the joints, especially of the hands, feet, and knees (Little, Falace, Miller, & Rhodus, 2008). The overall understanding of the mechanisms of RA is constantly evolving through research. The incidence and prevalence, etiology, signs and symptoms, dental and medical management of the patient, and treatment planning considerations and modifications will be addressed. Incidence and Prevalence The estimates of prevalence range from 1-2% of the population (Little et al., 2008). Disease onset usually occurs from ages 35-50 years old (Little et al.). Treister and Glick (1999) stated that fifty percent of people with RA become unable to work within the decade after the onset of disease. The long-term prognosis for people with an abrupt onset of disease is similar to that for people with a gradual disease onset (Little et al.). The course and severity of RA is unpredictable, but the disorder is characterized by remissions and exacerbations (Little et al.). Etiology The etiology of RA is unknown, although evidence seems to implicate an interrelationship of infectious agents, genetics, and autoimmunity (Little et al, 2008.). Women are affected approximately three times more than men (Little et al.). This implies the involvement of sex hormones in the sensitivity of the disease. Other possible predisposing factors include psychosocial stress, education, and socioeconomic status (Little et al.). Signs and Symptoms A patient will first experience fatigue and weakness with joint muscle aches, followed by painful joint swelling of the hands and feet, which begins with several joints and then progresses Rheumatoid Arthritis 4 to others symmetrically (Little et al., 2008). Joint involvement gradually progresses to immobility, contractures, subluxation, deviation, and other deformities (Little et al.). Characteristic features include pain aggravated by movement, generalized stiffness after inactivity, and morning stiffness lasting longer than one hour (Little et al.). The joints that are most commonly affected include the fingers, wrists, feet, ankles, knees, elbows, and TMJ in up to 75% of patients (Little et al.). Extra-articular manifestations may include rheumatoid nodules, vasculitis, skin ulcers, Sjögren’s syndrome, interstitial lung disease, pericarditis, C-spine instability, entrapment neuropathies, and ischemic neuropathies (Little et al.). Dental and Medical Management of Patient The importance of proper diagnosis, particularly in the early stages, can prevent lifelong complications (Little et al., 2008). Treatment is palliative as there is no cure for the disease (Little et al.). Treatment goals are to reduce joint inflammation and swelling, relieve pain and stiffness, and encourage normal function (Little et al.). This is accomplished by patient education, rest, exercise, physical therapy, NSAIDs, and other drugs (Little et al.). Drugs for management of RA have been divided into those used primarily for control of joint pain and swelling, and those intended to limit joint damage and improve long-term outcome (Little et al., 2008). NSAIDs inhibit proinflammatory prostaglandins and are used to treat pain, swelling, and stiffness but have no effect on the disease course or the risk of joint damage (Little et al.). Aspirin is the most effective and safest drug for patients (Little et al.). Disease-modifying antirheumatic drugs (DMARDs) are used to control disease and limit joint damage (Little et al.). Gold compounds, antimalarials used with aspirin or corticosteroids, and immunosuppressive therapy may be necessary (Little et al.). Surgical management such as arthroplasty, reconstruction, synovectomy, and total joint replacement is often required (Little et al.). Rheumatoid Arthritis 5 The dental hygienist must understand the complications associated with the drugs taken for RA. Aspirin taken with corticosteroids will prolong bleeding so the hygienist will want to obtain a bleeding time (Hupp, Williams, & Firriolo, 2006). Patients taking DMARDS will need white and red blood cell counts because DMARDS suppress bone marrow (Hupp et al.). The patient taking corticosteroids over an extended period will have immunosuppression (Hupp et al.). Knowledge of these drugs allows the hygienist to be aware of the patient's needs. During treatment, the dental hygienist should make an effort to provide comfort for the patient. Pillows or rolled towels can help support the patient’s limbs (Little et al., 2008). In cases of TMJ arthritis, a bite block may be helpful. The patient should be allowed to frequently change positions during the short appointment to aid in comfort (Little et al.). Treatment Planning Considerations and Modifications The RA patient has a difficult time doing daily tasks that may seem simple to non-RA patients. The dental hygienist must customize oral hygiene instruction to correspond with patient needs. Altering toothbrush handles and oral hygiene aids improves the patient’s oral home-care and enhances the patient's oral prognosis. Bicycle handle sleeves can be used to improve the RA patient's reduced grip strength on the toothbrush (Montandon, Pinelli, & Fais, 2006). Conclusion RA is a debilitating disease that affects many arenas of the patient's life, including the patient's oral health care. As a result, the clinician should be aware of medical and dental modifications necessary to alleviate the difficulties faced by the RA patient. Through evervigilant research into new and innovative techniques, the clinician can better address the needs of a large and growing segment of the population. Rheumatoid Arthritis 6 References Hupp, J. R., Williams, T. P., & Firriolo, F. J. (2006). Dental Clinical Advisor. St. Louis, MO: Mosby Elsevier. Little, J. W., Falace, D. A., Miller, C. S., & Rhodus, N. L. (2008). Dental Management of the Medically Compromised Patient (7th ed.). St. Louis, MO: Mosby Elsevier. Montandon, A. A. B., Pinelli, L. A. P., & Fais, L. M. G. (2006, December). Quality of life and oral hygiene in older people with manual functional limitations. Journal of Dental Education, 70(12), 1261-1262. Treister, N., & Glick, M. (1999, May). Rheumatoid arthritis: A review and suggested dental care considerations. The Journal of the American Dental Association, 130(5), 689-698.